Abstract
The aim of this review is to describe long-term HIV epidemiology and prevention trends in Guangxi, a provincial-level region located along a major drug trafficking corridor in southwestern China. Between 1996 and 2006, HIV transmission in Guangxi was primarily fueled by Injection Drug Use (IDU). Since 2006, heterosexual sex has become the dominant mode of HIV transmission, followed by drug injection. Moreover, older, heterosexual adults appear to be at increased risk for HIV. The vast majority of new HIV cases are attributed to local HIV subtypes already circulating within Guangxi (93%), though imported subtypes are associated with younger age groups. Since 2011, HIV incidence in Guangxi has stabilized, due in part to HIV prevention efforts that include expanded HIV testing, antiretroviral treatment, and other intervention measures. Between 1996 and 2017, Guangxi, China experienced dramatic changes in the primary HIV transmission mode and at-risk age group. Due in part to local and National AIDS control and prevention campaigns, HIV incidence trends in Guangxi no longer appear to be increasing.
Keywords: HIV, Transmission, Injection drug use, Sexual intercourse, Antiretroviral therapy, Prevention
1. INTRODUCTION
Guangxi Zhuang Autonomous Region (Guangxi) has a population of 47 million and is one of five provincial-level autonomous regions in China (other autonomous regions include Xinjiang, Tibet, Ningxia, and Inner Mongolia). Guangxi is located in southwest China, borders Vietnam, and is in close proximity to the “Golden Triangle”, a region known for the production of illegal narcotics which sits at the intersection of Myanmar, Laos, and Thailand [1-6]. In 1996, the first HIV case in Guangxi was identified among people who inject drugs (PWID). Between 1996 and 2003, PWID represented 69% of all reported HIV cases [7]. However, in 2006, the primary transmission route in Guangxi shifted to heterosexual intercourse (Fig. 1) [8]. By the end of 2004, Guangxi had the third highest number of HIV cases reported among provincial-level regions in China [9]. In 2013, Guangxi accounted for 12% of total HIV incidence in China, while only representing less than 4% of the national population [10].
Fig. (1).
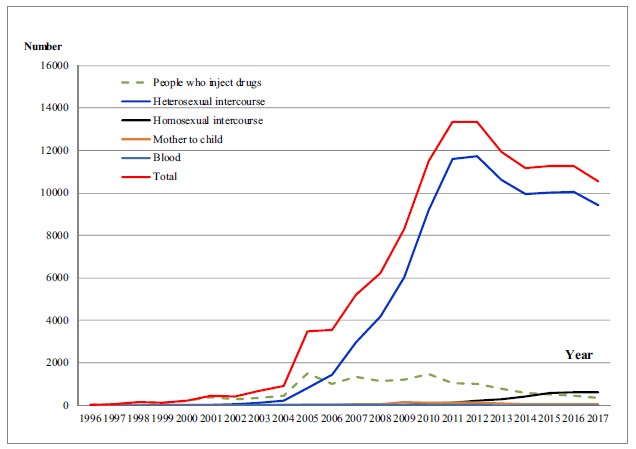
Reported HIV/AIDS cases by year and route of HIV infection in Guangxi, China.
2. HIV TRANSMISSION AND DRUG USE
Following liberation in 1949, China launched a mass anti-drug campaign that mobilized the entire nation. Consequently, serious narcotic addiction problems were largely eliminated until 1953 [4]. The use of illicit substances reemerged in China in the 1980s after China adopted an open-door policy which was associated with global drug trafficking activities [5]. These economic changes had a profound impact in Southwest China due to its close proximity to the “Golden Triangle”. The majority of heroin in China is trafficked from Myanmar (Burma), Laos, and Thailand into Yunnan and Guangxi, or from Vietnam into Guangxi, and then into other neighbor provinces (e.g., Sichuan, Guizhou, and Xinjiang and another to Guangdong, Shanghai, and Beijing) [1-6, 11-15]. From 1990 to 2009, the number of people using drugs registered by Chinese public security departments increased from 70,000 in 1990 to 1.22 million in 2009, an annual increase of 10% [6, 16]. However, the estimated number of actual people using drugs is 3-8 times the reported number [6, 16].
The first HIV case among People Who Inject Drugs (PWID) in China was reported in the southwestern province of Yunnan along the border with Burma (Myanmar) in 1989 [17]. Thereafter, the HIV epidemic among PWID rapidly spread north to other parts of the country. By 2002, HIV infection among PWID had been detected in all 31 mainland provinces, and HIV infection through injection drug use accounted for 64% of all reported HIV/AIDS cases in China [18, 19]. In 1996 when the first case of HIV was detected in Guangxi, most reported HIV cases were attributed to injection drug use. From 1996 to 2005, the number of counties in Guangxi that reported HIV cases increased from seven to all 115 [20]. In 1998, about 60% of HIV infected individuals reported sharing needles and the HIV infection prevalence among PWID at baseline was 15.4% [21]. In one study from 1998-1999, the HIV incidence among PWID increased from 2.38 to 6.86 per 100 person-years (py) [22]. Another prospective cohort study found that HIV prevalence among PWID at baseline was 25% and the HIV incidence rate was 3.1 per 100 person-years at 12 months of follow-up [23, 24]. HIV prevalence among PWID increased rapidly after 1996, with an annualized increase of 10% until 2011 [25]. (Fig. 1- 3).
Fig. (3).
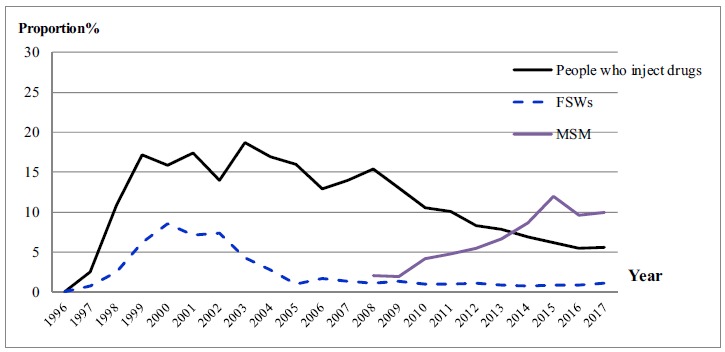
HIV prevalence over time in serial cross-sectional surveys among people who inject drugs, FSWs and MSM in Guangxi, China.
3. HIV TRANSMISSION AND SEXUAL INTERCOURSE
In response to an epidemic of Sexually Transmitted Infections (STI), China launched a nationwide STI control campaign throughout the 1950s that entailed shutting down brothels, screening and treatment of STI, and mass media education and prevention [26, 27]. By the end of 1964, syphilis infections were essentially eliminated [28, 29]. However, after adopting an open door policy and free market principles in 1978, China experienced rapid economic development, large income disparities, changing notions of sexuality, and increased commercial sex activities. The Chinese Public Security Office estimated that there were 4 to 6 million sex workers nationwide in 2000, an increase of 160-fold compared to in 1985 [28, 29]. During this same period, cases of eight reportable STIs (including syphilis and HIV) in China increased 147-fold, from 5838 to 859040 [30].
The HIV epidemic in Guangxi was initially fueled by injection drug use, but since 2006 the main mode of HIV transmission has been heterosexual sex [8]. From 2000 to 2013, the proportion of new HIV cases attributed to heterosexual sex rose from less than 10% to over 90%. This rising risk of HIV sexual transmission among the heterosexual population is alarming because it raises the potential for a more diffuse and generalized epidemic [31]. Among Female Sex Workers (FSW), HIV prevalence was above 1.0% from 1998 to 2011 but has remained below 1.0% since 2013 [32]. The age groups most afflicted by the epidemic have also shifted. In 2000, the older population (≥50 years of age) as a proportion of reported HIV cases increased from less than 4% to over 40% in 2013 (Fig. 1- 3).
Given the paucity of data on HIV risk among older individuals in China, a large-scale cross-sectional survey was conducted in 2012 to understand HIV and STI risk factors among older male clients of FSW in Guangxi, China [33-38]. This study found that the overall prevalence of HIV and syphilis infection was 3.0% and 3.2%, respectively. Factors associated with HIV or syphilis infection included recent non-commercial casual sex, >10 years of commercial sex history, >2 incidents of commercial sex in last month and aphrodisiac use [32-34]. One important finding was that 29.8% of participants used aphrodisiacs [32-34]. In 2013, a population-based prospective HIV follow-up study in three rural counties in Guangxi was conducted [35]. HIV prevalence was 0.29% among all study participants aged ≥20 years at baseline. Overall HIV incidence was 2.73 per 10000 person-years (235/860,627 PY). HIV seroconversion was associated with males, older age, and not currently being married. HIV incidence was 71.28 per 10000-years among males aged 50-69 years who had less than secondary schooling and were divorced or widowed. Heterosexual sex was the dominant transmission mode for HIV seroconversions (99.0%). Among males who seroconverted, 79% had sex with female sex workers and 18% had sex with casual sexual partners, but not sex workers. Among females who seroconverted, 62% and 37% were infected through their spouse or steady sexual partners, and casual sexual partners, respectively. This study was among the first to provide empirical evidence that current HIV prevention strategies designed primarily for key populations may be insufficient for addressing HIV transmission among the older, general population.
In China, approximately 2% to 5% of sexually active Chinese men have sex with other men. This corresponds to about 2 to 8 million men who have sex with men (MSM) in China [39]. HIV transmission among MSM is increasing at an alarming speed [40-57]. The proportion of reported HIV cases in China attributed to MSM increased from 3.5% in 2007 to 28.3% in 2015 [58, 59]. However, the proportion of reported HIV cases due to MSM remains relatively low in Guangxi. In 2013, only 2.3% of HIV cases in Guangxi were among MSM [10]. Nonetheless, annual cross-sectional surveys among MSM in Guangxi indicate that HIV prevalence increased from 2.0% in 2008 to 10.0% in 2017 [60] (Fig. 3). HIV preventative measures among MSM remain urgently needed. Mental health interventions may help reduce MSM sexual risk behaviors [61-63]. HIV risk factors among MSM in Guangxi include recent unprotected anal intercourse with commercial male partners, recent sex with female partners, past drug use, and syphilis infection [60] Figs. (1-3).
4. HIV MOLECULAR EPIDEMIOLOGY
Two different HIV subtypes have been introduced to southwest China. In the early phases of the epidemic in Yunnan among PWID, the dominant HIV subtypes were subtype B strains, including both North American-like subtype B strains and the Thailand variant of subtype B (B′ or Thai B) [64, 65]. HIV subtype C strain was similar to Indian subtype C and was first found among PWID in 1992 in Yunnan [66]. Thereafter, a circulating recombinant form (CRF) CRF01_ AE was identified in a female who came back to Yunnan after commercial sex work in Thailand in 1994 [66].
Molecular epidemiological studies indicate that HIV subtype C and subtype E among PWID probably spread from Yunnan to Baise county, Guangxi and from Vietnam into Pingxiang county in Guangxi through drug trafficking and injection drug use [67]. In 1998, the low inter-person nucleotide diversity among PWID in northern Vietnam showed that HIV subtype E was introduced recently among PWID in northern Vietnam, suggesting transborder transmission as the likely source of HIV subtype E being imported into Guangxi [68, 69]. During this period, B/C recombinants were identified among PWID from Baise county, Guangxi, a mountainous region near the Yunnan-Guangxi border, and CRF01_ AE strains were found among PWID in Nanning, the capital of Guangxi, and in Pingxiang county near the China- Vietnam border [70]. In 2000, PWID in Pingxiang and Bin-yang counties of Guangxi were found to be infected with CRF08_BC [71].
Following the rise of sexually transmitted HIV in Guangxi, China, multiple HIV subtypes were identified among HIV patients infected by heterosexual infection: CRF01_AE (80.1%), CRF07_BC (6.4%), CRF08_BC (10.2%), subtype B (1.7%), and URFs (1.7%) [72]. This study identified two large CRF01_AE clusters: one cluster originating from Vietnam among PWID and one novel cluster similar to strains from Fujian province, China. In 2008-2009, a survey in Guangxi indicated that CRF01_AE was the dominant subtype (77.6%), followed by CRF08_BC (10.7%) and CRF07_BC (7.4%), 7 unique recombinant forms, 4 subtype B (B'), and 1 subtype G [73]. Using a Bayesian discrete phylogeographic approach to analyze the transmission source of strains among recently infected HIV patients throughout Guangxi in 2012-2013, one study indicated the following subtype/CRF distribution: CRF01_AE (61.1%), CRF07_BC (18.8%), CRF08_BC (16.6%), CRF55_01B (3.1%), and subtype B' (0.4%). Recent research determined that most sequenced transmission strains were derived from already-circulating local strains (93.0%) and that only individuals 18-25 years old were significantly associated with transmission from outside Guangxi [74].
5. HIV TREATMENT AND PREVENTION
The Chinese government quickly assumed leadership and commitment of resources in responding to the growing HIV epidemic in China. The national AIDS prevention and care budget increased from 0.3 billion RMB in 2000 to 2 billion RMB in 2006. The most impactful program in the National AIDS Control Policy was the “Four Frees and One Care” program, which was implemented in 2003 and aimed to provide free voluntary counseling and testing, free antiretroviral treatment, free Prevention of Mother to Child Transmission (PMTCT), free education to AIDS orphans, and financial assistance and social support to people living with HIV [75]. Supported by this policy, harm reduction programs such as Methadone Maintenance Therapy (MMT), needle exchange, and condom promotion were implemented in 2004 [76-81].
The Chinese National Free Antiretroviral Treatment Program (NFATP) was initiated in 2002 and has significantly reduced death in HIV patients [82-86]. From 2003-2008, free antiretroviral therapy (ART) was provided to HIV patients with CD4+ T cell counts less than 200 cells/uL. From 2008-2012, guidelines were updated so that HIV patients with CD4+ T cell counts less than 350 cells/uL could access free ART. After 2012, all HIV patients could access free ART, irrespective of their CD4 T cell count [84-86]. First-line HAART regimens before 2008 consisted of [azidothymidine (AZT) or stavudine (D4T)] + [didanosine (DDI) or lamivudine (3TC)] + [nevirapine (NVP) or efavirenz (EFV)], and then revised to consist of [tenofovir (TDF) or azidothymidine (AZT)] + lamivudine (3TC) + [efavirenz (EFV) or nevirapine (NVP)] [84-90]. This program included three phases: initiation to 2005, 2005-2007 (first scale-up), and 2008-present (further scale-up and standardization). During these three phases, Guangxi, respectively, initiated more than 190, 4100, and 57500 HIV patients (at least 18 years old) on ART by the end of 2016. The average mortality rate was 2.6 deaths per 100 person-years among HIV patients who initiated ART during 2008-2013 in Guangxi [87]. The mortality rates per 100 person-years by year post-ART initiation was 5.4 in the first year, 1.8 in the second year, 1.3 in the third year, 1.2 in the fourth year, and less than 1.0 after four years on ART. Mortality rates in this study were significantly lower than other studies in China but higher than in studies from Europe and North America [88, 91-93], especially the high mortality rate during the first year post-ART initiation. The average mortality and ART attrition rates among all patients who initiated ART between 2010 and 2015 in Guangxi were 2.63 deaths and 5.32 attritions per 100 person-years, respectively [94]. High CD4 counts (pre-ART CD4 counts >500 cells/ul) was strongly associated with attrition (stop ART or lost to follow-up). One major concern with initiating ART among patients with a high CD4+ cell count is increased risk of poor adherence [94, 95]. Improving quality of care remains a considerable challenge in ART treatment.
In order to achieve significant future reductions in HIV transmission and HIV-related mortality, China’s government implemented the World Health Organization’s 90–90–90 policy (90% of the people living with HIV know their HIV status, 90% of the people who know their HIV-positive status are accessing treatment, and 90% of the people receiving treatment have suppressed viral loads). By the end of 2017, 70.2% of the people living with HIV knew their HIV status, 76.8% of the people who knew their HIV-positive status were receiving treatment, and 96.8% of the people receiving treatment had suppressed viral loads in Guangxi [96]. An observational cohort study of HIV epidemiology and treatment databases among serodiscordant couples in Guangxi showed that HIV seroincidence rate was significantly higher among the treatment-naive group (4.2 per 100 person-years, 3.7-4.8) compared with the treatment group (1.6 per 100 person-years, 1.3-1.8) [97]. This corresponded to an overall 45% reduction in risk of HIV transmission among serodiscordant couples who were on ART treatment. Drug adherence and baseline viral load among partners in the treatment were significantly associated with an increased risk of HIV seroincidence [98]. Treatment-as-prevention was feasible on a regional scale, but comprehensive harm reduction programs are urgently needed for serodiscordant couples.
In 2006-2007, surveys in Guangxi found that after initiation of first-line ART, 99.1% of HIV patients had viral loads <1000 copies/ml and 0.0% of HIV patients had ART drug resistance after 12 months of treatment [99, 100]. A series of cross-sectional surveys among HIV patients receiving first-line ART from 2004 to 2012 in Guangxi indicated that the prevalence of virologic suppression and drug resistance was 95.4% and 2.8%, respectively [101]. Among HIV patients who had a viral load ≥1000 copies/ml, 54.5% were resistant to Non-Nucleoside Reverse Transcriptase Inhibitor (NNRTIs) drugs, 90.9% were resistant to nucleoside reverse transcriptase inhibitor (NRTIs) drugs, and 4.5% of patients had drug resistance to Protease Inhibitors (PIs). Moreover, the trend chi-square test showed that the proportion of HIV patients achieving virologic suppression increased over time from 2004 to 2012. From 2005-2010, the overall prevalence of transmitted HIV Drug Resistance (TDR) in Guangxi was 3.2% among antiretroviral-naive HIV patients [102]. A survey among patients from newly diagnosed HIV infected 16-25 years olds in Guangxi from 2009 to 2013 showed that TDR mutations were 4.6%, with 1.4%, 1.4%, and 2.3% with resistance to PIs, NRTIs, and NNRTIs, respectively [103]. These excellent treatment outcomes in Guangxi can be explained by several factors. First, provincial, prefecture, and county hospitals are all providing ART for HIV patients. One provincial hospital provides technical support and training to each prefecture hospital, which then provides technical assistance to each county hospital. Second, all HIV patients receive treatment in hospitals, while community care and outreach are provided through local health workers.
In response to the HIV epidemic, the Guangxi government launched a Guangxi AIDS Conquering Project (GACP) in 2010 [104]. In 2013, the Guangxi People’s Congress passed the “Regulations on AIDS Prevention and Control in Guangxi” to foster a supportive social environment for AIDS control. The Guangxi government integrated local initiatives with the national Four Frees and One Care AIDS control policy, thus efficiently leveraging financial and human resource investments to enhance HIV prevention education, HIV testing and counselling, surveillance, health interventions, medical care, and antiretroviral therapies. By the end of 2014, AIDS control health/management staff increased by 357 and 2015 at prefectural and county level public health institutions, respectively. The Guangxi budget for AIDS prevention and treatment was 2.1 billion Yuan RMB during 2010-2014, including national and local investments.
Since GACP was initiated in 2011, HIV prevention efforts in Guangxi were greatly enhanced to expand access to HIV testing, ART, and other intervention measures. Guangxi’s HIV testing (per 100 persons) rapidly increased from 7.1 in 2009 to 15.0 in 2016 and was more than 2.0 times that of the national average. The Guangxi ART coverage rate increased from 23% in 2009 to 50% in 2016. In addition, the number of reported HIV/AIDS cases in Guangxi decreased from 2013 to 2017. From 2009-2015, the prevalence of HIV, HCV, and syphilis among PWID decreased from 13.0% to 6.2%, 68.0% to 50.5%, and 8.5% to 5.2%, respectively [105]. Such declines coincide with an increase in the use of prevention services, methadone maintenance therapy or needle exchange, peer education, and HIV testing and knowledge of HIV status increased over time during 2009-2015. HIV prevalence also declined significantly among high-tier, middle-tier, and low-tier FSWs over time from 2010 to 2015 [106]. However, HIV prevalence increased for older age (≥50 years old) clients of FSW, particularly among older clients who prefer low-tier FSWs.
CONCLUSION
From 1996 to 2017, the dominant mode of HIV transmission in Guangxi shifted from injection drug use to heterosexual sex. This rising risk of HIV sexual transmission among the heterosexual population is alarming because it raises the potential for a more diffuse and generalized epidemic, especially among older heterosexual adults in rural areas. The local GACP initiative combined with the National AIDS Control Policy appears to have helped stabilize HIV incidence in Guangxi, but additional interventions are needed to address HIV risk among older male clients of FSW.
Fig. (2).
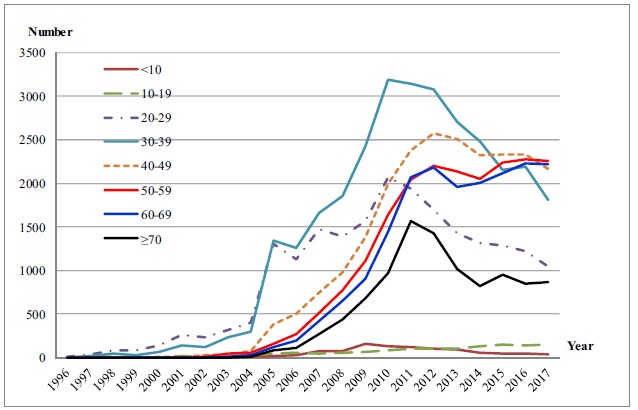
Reported HIV/AIDS cases by age (years) in Guangxi, China.
ACKNOWLEDGEMENTS
Declared none.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
This study was supported by grants from the Ministry of Science and Technology of China (2018ZX10721102-006, 2018ZX10715008), the Guangxi Medical and Health Project (Z20170126), Guangxi Science and Technology Bureau (AB16380213), Guangxi Honor Scholar, Chinese State Key Laboratory for Infectious Disease Develop Grant.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
REFERENCES
- 1.Zhang Kl K.L., Ma S.J. Epidemiology of HIV in China. BMJ. 2002;324(7341):803–804. doi: 10.1136/bmj.324.7341.803. [http://dx.doi.org/10.1136/bmj.324.7341.803]. [PMID: 11934762]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.UNAIDS Task Force on Drug Use and HIV. Drug use and HIV vulnerability: policy research study in Asia. Bangkok: UNAIDS Asia Pacific Intercountry Team; 2000. [Google Scholar]
- 3.United Nations Office on Drugs and Crime Global illicit drug trends. 2003 http://www.unodc.org
- 4.Lowinger P. The solution to narcotic addiction in the People’s Republic of China. Am. J. Drug Alcohol Abuse. 1977;4(2):165–178. doi: 10.3109/00952997709002758. [http://dx.doi.org/10.3109/00952997709002758]. [PMID: 347925]. [DOI] [PubMed] [Google Scholar]
- 5.Thomas J. HIV / AIDS in China: Migrant population, drug injection responsible for increased transmission. AIDSlink. 1998;(49):12–14. [PMID: 12293301]. [PubMed] [Google Scholar]
- 6.China Ministry of Public Security. Registered number of drug users in China updated through June of. 2009 http://www.mps.gov.cn/ n16/ n1252/n1897/n2872/2077880.html
- 7.Chinese Center for Disease Control and Prevention. Analysis of HIV/STD epidemic in 2003. Beijing, China. [Google Scholar]
- 8.Chinese Center for Disease Control and Prevention. Analysis of HIV/STD epidemic in 2006. Beijing, China [Google Scholar]
- 9.Chinese Center for Disease Control and Prevention. Analysis of HIV/STD epidemic in 2009. Beijing, China [Google Scholar]
- 10.Chinese Center for Disease Control and Prevention. Analysis of HIV/STD epidemic in 2013. Beijing, China [Google Scholar]
- 11.Ruan Y., Chen K., Hong K., et al. Community-based survey of HIV transmission modes among intravenous drug users in Sichuan, China. Sex. Transm. Dis. 2004;31(10):623–627. doi: 10.1097/01.olq.0000140018.24262.4a. [http://dx.doi.org/10.1097/01.olq.0000140018.24262.4a]. [PMID: 15389002]. [DOI] [PubMed] [Google Scholar]
- 12.Ruan Y., Qin G., Liu S., et al. HIV incidence and factors contributed to retention in a 12-month follow-up study of injection drug users in Sichuan Province, China. J. Acquir. Immune Defic. Syndr. 2005;39(4):459–463. doi: 10.1097/01.qai.0000152398.47025.0f. [http://dx.doi.org/10.1097/01.qai.0000152398.47025.0f]. [PMID: 16010170]. [DOI] [PubMed] [Google Scholar]
- 13.Zhang Y., Shan H., Trizzino J., et al. Demographic characteristics and risk behaviors associated with HIV positive injecting drug users in Xinjiang, China. J. Infect. 2007;54(3):285–290. doi: 10.1016/j.jinf.2006.06.001. [http://dx.doi.org/10.1016/j.jinf.2006.06.001]. [PMID: 16831464]. [DOI] [PubMed] [Google Scholar]
- 14.Yin L., Qin G., Qian H.Z., et al. Continued spread of HIV among injecting drug users in southern Sichuan Province, China. Harm Reduct. J. 2007;4:6. doi: 10.1186/1477-7517-4-6. [http://dx.doi.org/10.1186/1477-7517-4-6]. [PMID: 17286871]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang Y., Shan H., Trizzino J., et al. HIV incidence, retention rate, and baseline predictors of HIV incidence and retention in a prospective cohort study of injection drug users in Xinjiang, China. Int. J. Infect. Dis. 2007;11(4):318–323. doi: 10.1016/j.ijid.2006.09.001. [http://dx.doi.org/10.1016/j.ijid.2006.09.001]. [PMID: 17321184]. [DOI] [PubMed] [Google Scholar]
- 16.China N.N.C.C. Annual report on drug control in China. Beijing, China: National Narcotics Control Commission; 2002. [Google Scholar]
- 17.Ma Y., Li Z.Z., Zhao S.D. HIV was first discovered among IDUs in China. Zhonghua Liu Xing Bing Xue Za Zhi. 1990;11:184–185. [Google Scholar]
- 18.Chinese Center for Disease Control and Prevention. Analysis of HIV/STD epidemic in 2002. Beijing, China. 2002. [Google Scholar]
- 19.Chinese Center for Disease Control and Prevention. Analysis of HIV/STD epidemic in 2004. Beijing, China [Google Scholar]
- 20.Progress Report on AIDS. Prev Res 2005. [Google Scholar]
- 21.Zhang G., Zheng X., Liu W., et al. The survey of HIV prevalence among drug users in Guangxi, China]. Zhonghua Liu Xing Bing Xue Za Zhi. 2000;21(1):15–16. [PubMed] [Google Scholar]
- 22.Lai S., Liu W., Chen J., et al. Changes in HIV-1 incidence in heroin users in Guangxi Province, China. J. Acquir. Immune Defic. Syndr. 2001;26(4):365–370. doi: 10.1097/00126334-200104010-00014. [http://dx.doi.org/10.1097/00042560-200104010-00014]. [PMID: 11317080]. [DOI] [PubMed] [Google Scholar]
- 23.Wei L., Chen J., Rodolph M., et al. HIV incidence, retention, and changes of high-risk behaviors among rural injection drug users in Guangxi, China. Subst. Abus. 2006;27(4):53–61. doi: 10.1300/j465v27n04_07. [http://dx.doi.org/10.1300/J465v27n04_07]. [PMID: 17347126]. [DOI] [PubMed] [Google Scholar]
- 24.Liu W., Chen J., Rodolph M., et al. HIV prevalence among injection drug users in rural Guangxi China. Addiction. 2006;101(10):1493–1498. doi: 10.1111/j.1360-0443.2006.01557.x. [Erratum in: Addiction. 2007; 102(5): 841]. [http://dx.doi.org/10.1111/j.1360-0443.2006.01557.x]. [PMID: 16968351]. [DOI] [PubMed] [Google Scholar]
- 25.Chinese Center for Disease Control and Prevention. Analysis of HIV/STD epidemic in 2011. Beijing, China [Google Scholar]
- 26.Hu C.K.Y.G., Wang G.C., Yun G.L. Ten years of accomplishments in dermatology and venereology. Zhonghua Pifuke Zazhi. 1959;7:290–294. [Google Scholar]
- 27.Hu C.K., Ye G.Y., Chen S.T. Control and eradication of syphilis in China.; Beijing Science Conference; pp. 167–77. [Google Scholar]
- 28.Gil V.E., Wang M.S., Anderson A.F., Lin G.M., Wu Z.O. Prostitutes, prostitution and STD/HIV transmission in mainland China. Soc. Sci. Med. 1996;42(1):141–152. doi: 10.1016/0277-9536(95)00064-x. [http://dx.doi.org/10.1016/0277-9536(95)00064-X]. [PMID: 8745115]. [DOI] [PubMed] [Google Scholar]
- 29.Qian H.Z., Vermund S.H., Wang N. Risk of HIV/AIDS in China: Subpopulations of special importance. Sex. Transm. Infect. 2005;81(6):442–447. doi: 10.1136/sti.2004.014258. [http://dx.doi.org/10.1136/sti.2004.014258]. [PMID: 16326842]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gong XD, Ye SZ, Zhang GC, et al. An epidemiologic analysis of sexually transmitted diseases in China in 2000. Chin J STD/AIDS Prev Cont. 2001;7:131–134. [Google Scholar]
- 31.Shao Y., Jia Z. Challenges and opportunities for HIV/AIDS control in China. Lancet. 2012;379(9818):804. doi: 10.1016/S0140-6736(12)60349-3. [http://dx.doi.org/10.1016/S0140-6736(12)60349-3]. [PMID: 22386033]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen L., His J.H., Wu X., et al. Disparities in HIV and syphilis prevalence and risk factors between older male clients with and without steady sex partners in southwestern rural China. BMC Infect. Dis. 2017;17(1):269. doi: 10.1186/s12879-017-2367-z. [http://dx.doi.org/10.1186/s12879-017-2367-z]. [PMID: 28403825]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu X., Huang H., Tang Z., et al. Aphrodisiac use and associated factors among oder male clients of low-cost female sex workers in southwestern rural areas of China. Sex. Res. Soc. Policy. 2016;14(1):1–10. [Google Scholar]
- 34.Tang Z., Wu X., Li G., et al. Aphrodisiac use associated with HIV infection in elderly male clients of low-cost commercial sex venues in Guangxi, China: a matched case-control study. PLoS One. 2014;9(10):e109452. doi: 10.1371/journal.pone.0109452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen H., Wu X., Chen L., et al. Rapidly spreading HIV epidemic among older males and associated factors: A large-scale prospective cohort study in rural southwest China. Sex. Transm. Dis. 2018 doi: 10.1097/OLQ.0000000000000957. [Epub ahead of print]. [http://dx.doi.org/10.1097/OLQ.0000000000000957]. [PMID: 30516723]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lu H., Zhu Y., Wu X., et al. Study on the characteristics of commercial sexual behavior and the risk factors analysis of HIV infection among the old male clients, in Guangxi. Zhonghua Liu Xing Bing Xue Za Zhi. 2015;36(1):31–34. [PubMed] [Google Scholar]
- 37.Xing J., Li Y.G., Tang W., et al. HIV/AIDS epidemic among older adults in China during 2005-2012: Results from trend and spatial analysis. Clin. Infect. Dis. 2014;59(2):e53–e60. doi: 10.1093/cid/ciu214. [http://dx.doi.org/10.1093/cid/ciu214]. [PMID: 24700658]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu H., Lin X., Xu Y., Chen S., Shi J., Morisky D. Emerging HIV epidemic among older adults in Nanning, China. AIDS Patient Care STDS. 2012;26(10):565–567. doi: 10.1089/apc.2012.0227. [http://dx.doi.org/10.1089/apc.2012.0227]. [PMID: 22984779]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chow E.P.F., Wilson D.P., Zhang J., Jing J., Zhang L. Human immunodeficiency virus prevalence is increasing among men who have sex with men in China: Findings from a review and meta-analysis. Sex. Transm. Dis. 2011;38(9):845–857. doi: 10.1097/OLQ.0b013e31821a4f43. [http://dx.doi.org/10.1097/OLQ.0b013e31821a4f43]. [PMID: 21844741]. [DOI] [PubMed] [Google Scholar]
- 40.Zheng C., Xu J.J., Hu Q.H., et al. Commercial sex and risk of HIV, syphilis, and herpes simplex virus-2 among men who have sex with men in six Chinese cities. BMC Infect. Dis. 2016;16(1):765. doi: 10.1186/s12879-016-2130-x. [http://dx.doi.org/10.1186/s12879-016-2130-x]. [PMID: 28003032]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xu J.J., Zhang C., Hu Q.H., et al. Recreational drug use and risks of HIV and sexually transmitted infections among Chinese men who have sex with men: Mediation through multiple sexual partnerships. BMC Infect. Dis. 2014;14:642. doi: 10.1186/s12879-014-0642-9. [http://dx.doi.org/10.1186/s12879-014-0642-9]. [PMID: 25443542]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang X., Lan G., Shen Z., et al. HIV and syphilis prevalence trends among men who have sex with men in Guangxi, China: Yearly cross-sectional surveys, 2008-2012. BMC Infect. Dis. 2014;14:367. doi: 10.1186/1471-2334-14-367. [http://dx.doi.org/10.1186/1471-2334-14-367]. [PMID: 24993252]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lou J., Cheng J., Li Y., et al. Comparison of different strategies for controlling HIV/AIDS spreading in MSM. Infect. Dis. Model. 2018;3:293–300. doi: 10.1016/j.idm.2018.10.002. [doi: 10.1016/j.idm.2018.10.002. eCollection 2018]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li J., Peng L., Gilmour S., et al. A mathematical model of biomedical interventions for HIV prevention among men who have sex with men in China. BMC Infect. Dis. 2018;18(1):600. doi: 10.1186/s12879-018-3516-8. [http://dx.doi.org/10.1186/s12879-018-3516-8]. [PMID: 30486800]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ruan Y., Li D., Li X., et al. Relationship between syphilis and HIV infections among men who have sex with men in Beijing, China. Sex. Transm. Dis. 2007;34(8):592–597. doi: 10.1097/01.olq.0000253336.64324.ef. [http://dx.doi.org/10.1097/01.olq.0000253336.64324.ef]. [PMID: 17325622]. [DOI] [PubMed] [Google Scholar]
- 46.Zhang X., Wang C., Hengwei W., et al. Risk factors of HIV infection and prevalence of co-infections among men who have sex with men in Beijing, China. AIDS. 2007;21(Suppl. 8):S53–S57. doi: 10.1097/01.aids.0000304697.39637.4c. [http://dx.doi.org/10.1097/01.aids.0000304697.39637.4c]. [PMID: 18172392]. [DOI] [PubMed] [Google Scholar]
- 47.Zhang X., Li S., Li X., et al. Characterization of HIV-1 subtypes and viral antiretroviral drug resistance in men who have sex with men in Beijing, China. AIDS. 2007;21(Suppl. 8):S59–S65. doi: 10.1097/01.aids.0000304698.47261.b1. [http://dx.doi.org/10.1097/01.aids.0000304698.47261.b1]. [PMID: 18172393]. [DOI] [PubMed] [Google Scholar]
- 48.Ruan Y., Luo F., Jia Y., et al. Risk factors for syphilis and prevalence of HIV, hepatitis B and C among men who have sex with men in Beijing, China: Implications for HIV prevention. AIDS Behav. 2009;13(4):663–670. doi: 10.1007/s10461-008-9503-0. [http://dx.doi.org/10.1007/s10461-008-9503-0]. [PMID: 19082879]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ruan Y., Jia Y., Zhang X., et al. Incidence of HIV-1, syphilis, hepatitis B, and hepatitis C virus infections and predictors associated with retention in a 12-month follow-up study among men who have sex with men in Beijing, China. J. Acquir. Immune Defic. Syndr. 2009;52(5):604–610. doi: 10.1097/QAI.0b013e3181b31f5c. [http://dx.doi.org/10.1097/QAI.0b013e3181b31f5c]. [PMID: 19710617]. [DOI] [PubMed] [Google Scholar]
- 50.Li D., Jia Y., Ruan Y., et al. Correlates of incident infections for HIV, syphilis, and hepatitis B virus in a cohort of men who have sex with men in Beijing. AIDS Patient Care STDS. 2010;24(9):595–602. doi: 10.1089/apc.2010.0083. [http://dx.doi.org/10.1089/apc.2010.0083]. [PMID: 20731610]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ruan Y., Pan S.W., Chamot E., et al. Sexual mixing patterns among social networks of HIV-positive and HIV-negative Beijing men who have sex with men: A multilevel comparison using roundtable network mapping. AIDS Care. 2011;23(8):1014–1025. doi: 10.1080/09540121.2010.542127. [http://dx.doi.org/10.1080/09540121.2010.542127]. [PMID: 21400315]. [DOI] [PubMed] [Google Scholar]
- 52.Fan S., Lu H., Ma X., et al. Behavioral and serologic survey of men who have sex with men in Beijing, China: Implication for HIV intervention. AIDS Patient Care STDS. 2012;26(3):148–155. doi: 10.1089/apc.2011.0277. [http://dx.doi.org/10.1089/apc.2011.0277]. [PMID: 22248333]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li D., Li S., Liu Y., et al. HIV incidence among men who have sex with men in Beijing: A prospective cohort study. BMJ Open. 2012;2(6):e001829. doi: 10.1136/bmjopen-2012-001829. [http://dx.doi.org/10.1136/bmjopen-2012-001829]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lu H., Han Y., He X., et al. Alcohol use and HIV risk taking among Chinese MSM in Beijing. Drug Alcohol Depend. 2013;133(2):317–323. doi: 10.1016/j.drugalcdep.2013.06.013. [http://dx.doi.org/10.1016/j.drugalcdep.2013.06.013]. [PMID: 23876859]. [DOI] [PubMed] [Google Scholar]
- 55.Lou J., Blevins M., Ruan Y., et al. Modeling the impact on HIV incidence of combination prevention strategies among men who have sex with men in Beijing, China. PLoS One. 2014;9(3):e90985. doi: 10.1371/journal.pone.0090985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wu Z.L., Guan G.Y., Zhao J.H., et al. Dynamic characteristics and HIV infection of men who have sex with men from 2011 to 2017 in Yinchuan, Ningxia, China. Curr. HIV Res. 2018;16(5):364–373. doi: 10.2174/1570162X17666190119094035. [http://dx.doi.org/10.2174/1570162X17666190119094035]. [PMID: 30659545]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang N., Wu G., Lu R., et al. Investigating HIV infection and HIV incidence among chinese men who have sex with men with recent sexual debut, Chongqing, China, 2011. AIDS Behav. 2016;20(12):2976–2982. doi: 10.1007/s10461-016-1356-3. [http://dx.doi.org/10.1007/s10461-016-1356-3]. [PMID: 26979418]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chinese Center for Disease Control and Prevention. Analysis of HIV/STD epidemic in 2007, Beijing, China [Google Scholar]
- 59.Chinese Center for Disease Control and Prevention. Analysis of HIV/STD epidemic in 2015, Beijing, China [Google Scholar]
- 60.Guanghua L., Yi C., Shuai T., et al. HIV, syphilis and behavioral risk factors among men who have sex with men in a drug-using area of southwestern China: Results of 3 cross-sectional surveys from 2013 to 2015. Medicine (Baltimore) 2018;97(16):e0404. doi: 10.1097/MD.0000000000010404. [http://dx.doi.org/10.1097/MD.0000000000010404]. [PMID: 29668597]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Leluțiu-Weinberger C., Manu M., Ionescu F., et al. An mHealth intervention to improve young gay and bisexual men’s sexual, behavioral, and mental health in a structurally stigmatizing national context. JMIR Mhealth Uhealth. 2018;6(11):e183. doi: 10.2196/mhealth.9283. [http://dx.doi.org/10.2196/mhealth.9283]. [PMID: 30429117]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tao J., Vermund S.H., Lu H., et al. Impact of depression and anxiety on initiation of antiretroviral therapy among men who have sex with men with newly diagnosed HIV infections in China. AIDS Patient Care STDS. 2017;31(2):96–104. doi: 10.1089/apc.2016.0214. [http://dx.doi.org/10.1089/apc.2016.0214]. [PMID: 28170305]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tao J., Wang L., Kipp A.M., et al. Relationship of stigma and depression among newly HIV-diagnosed Chinese men who have sex with men. AIDS Behav. 2017;21(1):292–299. doi: 10.1007/s10461-016-1477-8. [http://dx.doi.org/10.1007/s10461-016-1477-8]. [PMID: 27376900]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Xia M., Kreiss J.K., Holmes K.K. Risk factors for HIV infection among drug users in Yunnan province, China: Association with intravenous drug use and protective effect of boiling reusable needles and syringes. AIDS. 1994;8(12):1701–1706. [http://dx.doi.org/10.1097/00002030-199412000-00010]. [PMID: 7888119]. [PubMed] [Google Scholar]
- 65.Cheng H., Zhang J., Capizzi J., Young N.L., Mastro T.D. HIV-1 subtype E in Yunnan, China. Lancet. 1994;344(8927):953–954. doi: 10.1016/s0140-6736(94)92304-3. [http://dx.doi.org/10.1016/S0140-6736(94)92304-3]. [PMID: 7934363]. [DOI] [PubMed] [Google Scholar]
- 66.Luo C.C., Tian C., Hu D.J., Kai M., Dondero T., Zheng X. HIV-1 subtype C in China. Lancet. 1995;345(8956):1051–1052. doi: 10.1016/s0140-6736(95)90792-0. [http://dx.doi.org/10.1016/S0140-6736(95)90792-0]. [PMID: 7723522]. [DOI] [PubMed] [Google Scholar]
- 67.Yu X.F., Chen J., Shao Y., Beyrer C., Lai S. Two subtypes of HIV-1 among injection-drug users in southern China. Lancet. 1998;351(9111):1250. doi: 10.1016/S0140-6736(05)79316-8. [http://dx.doi.org/10.1016/S0140-6736(05)79316-8]. [PMID: 9643749]. [DOI] [PubMed] [Google Scholar]
- 68.Kato K., Shiino T., Kusagawa S., et al. Genetic similarity of HIV type 1 subtype E in a recent outbreak among injecting drug users in northern Vietnam to strains in Guangxi Province of southern China. AIDS Res. Hum. Retroviruses. 1999;15(13):1157–1168. doi: 10.1089/088922299310250. [http://dx.doi.org/10.1089/088922299310250]. [PMID: 10480629]. [DOI] [PubMed] [Google Scholar]
- 69.Yu X.F., Chen J., Shao Y., et al. Emerging HIV infections with distinct subtypes of HIV-1 infection among injection drug users from geographically separate locations in Guangxi Province, China. J. Acquir. Immune Defic. Syndr. 1999;22(2):180–188. doi: 10.1097/00126334-199910010-00011. [http://dx.doi.org/10.1097/00042560-199910010-00011]. [PMID: 10843533]. [DOI] [PubMed] [Google Scholar]
- 70.Piyasirisilp S., McCutchan F.E., Carr J.K., et al. A recent outbreak of human immunodeficiency virus type 1 infection in southern China was initiated by two highly homogeneous, geographically separated strains, circulating recombinant form AE and a novel BC recombinant. J. Virol. 2000;74(23):11286–11295. doi: 10.1128/jvi.74.23.11286-11295.2000. [http://dx.doi.org/10.1128/JVI.74.23.11286-11295.2000]. [PMID: 11070028]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Laeyendecker O., Zhang G.W., Quinn T.C., et al. Molecular epidemiology of HIV-1 subtypes in southern China. J. Acquir. Immune Defic. Syndr. 2005;38(3):356–362. [PMID: 15735457]. [PubMed] [Google Scholar]
- 72.Li L., Chen L., Liang S., et al. Subtype CRF01_AE dominate the sexually transmitted human immunodeficiency virus type 1 epidemic in Guangxi, China. J. Med. Virol. 2013;85(3):388–395. doi: 10.1002/jmv.23360. [http://dx.doi.org/10.1002/jmv.23360]. [PMID: 23341369]. [DOI] [PubMed] [Google Scholar]
- 73.Liu W., Liang S.J., Yang J.Y., et al. Distribution of HIV-1 subtypes in Guangxi Zhuang Autonomous Region, 2008-2009. Zhonghua Liu Xing Bing Xue Za Zhi. 2013;34(1):53–56. [PubMed] [Google Scholar]
- 74.Li J., Feng Y., Shen Z., et al. HIV-1 transmissions among recently infected individuals in southwest China are predominantly derived from circulating local strains. Sci. Rep. 2018;8(1):12831. doi: 10.1038/s41598-018-29201-3. [Erratum in: Sci Rep 2018; 8]. [1].[http://dx.doi.org/10.1038/s41598-018-29201-3]. [PMID: 30150680]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Han M., Chen Q., Hao Y., et al. Design and implementation of a China comprehensive AIDS response programme (China CARES), 2003-08. Int. J. Epidemiol. 2010;39(Suppl. 2):ii47–ii55. doi: 10.1093/ije/dyq212. [http://dx.doi.org/10.1093/ije/dyq212]. [PMID: 21113037]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Liu B., Sullivan S.G., Wu Z. An evaluation of needle exchange programmes in China. AIDS. 2007;21(Suppl. 8):S123–S128. doi: 10.1097/01.aids.0000304707.56670.cf. [http://dx.doi.org/10.1097/01.aids.0000304707.56670.cf]. [PMID: 18172380]. [DOI] [PubMed] [Google Scholar]
- 77.Yin W., Hao Y., Sun X., et al. Scaling up the national methadone maintenance treatment program in China: Achievements and challenges. Int. J. Epidemiol. 2010;39(Suppl. 2):ii29–ii37. doi: 10.1093/ije/dyq210. [http://dx.doi.org/10.1093/ije/dyq210]. [PMID: 21113034]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Rou K., Sullivan S.G., Liu P., Wu Z. Scaling up prevention programmes to reduce the sexual transmission of HIV in China. Int. J. Epidemiol. 2010;39(Suppl. 2):ii38–ii46. doi: 10.1093/ije/dyq211. [http://dx.doi.org/10.1093/ije/dyq211]. [PMID: 21113035]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Qian H.Z., Hao C., Ruan Y., et al. Impact of methadone on drug use and risky sex in China. J. Subst. Abuse Treat. 2008;34(4):391–397. doi: 10.1016/j.jsat.2007.07.002. [http://dx.doi.org/10.1016/j.jsat.2007.07.002]. [PMID: 17869049]. [DOI] [PubMed] [Google Scholar]
- 80.Ruan Y., Liang S., Zhu J., et al. Evaluation of harm reduction programs on seroincidence of HIV, hepatitis B and C, and syphilis among intravenous drug users in southwest China. Sex. Transm. Dis. 2013;40(4):323–328. doi: 10.1097/OLQ.0b013e31827fd4d4. [http://dx.doi.org/10.1097/OLQ.0b013e31827fd4d4]. [PMID: 23486498]. [DOI] [PubMed] [Google Scholar]
- 81.Zhang L, Liang S, Lu W, et al. HIV, syphilis, and behavioral risk factors among female sex workers before and after implementation of harm reduction programs in a high drug-using area of China. PLoS One. 2014;8;9(1):e84950.. doi: 10.1371/journal.pone.0084950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhang F., Dou Z., Ma Y., et al. Effect of earlier initiation of antiretroviral treatment and increased treatment coverage on HIV-related mortality in China: A national observational cohort study. Lancet Infect. Dis. 2011;11(7):516–524. doi: 10.1016/S1473-3099(11)70097-4. [http://dx.doi.org/10.1016/S1473-3099(11)70097-4]. [PMID: 21600849]. [DOI] [PubMed] [Google Scholar]
- 83.Zhang F, Dou Z, Ma Y, et al. Five-year outcomes of the China national free antiretroviral treatment program. Ann Intern Med. 2009;18; 151(4):241–51, W-52.. doi: 10.7326/0003-4819-151-4-200908180-00006. [DOI] [PubMed] [Google Scholar]
- 84.Zhang F. Manual of the National Free Antiretroviral Treatment. 1st ed. Beijing: People’s Medical Publishing House; 2005. [Google Scholar]
- 85.Zhang F., Wang Y., Wang J., et al. Manual of the National Free Antiretroviral Treatment. 2nd ed. Beijing: People’s Medical Publishing House; 2008. [Google Scholar]
- 86.Zhang F., Wang J., Wang F.S., et al. Manual of the National Free Antiretroviral Treatment. 2nd ed. Beijing: People’s Medical Publishing House; 2012. [Google Scholar]
- 87.Shen Z., Zhu Q., Tang Z., et al. Effects of CD4 Cell Counts and Viral Load Testing on Mortality Rates in Patients with HIV Infection Receiving Antiretroviral Treatment: An Observational Cohort Study in Rural Southwest China. Clin. Infect. Dis. 2016;63(1):108–114. doi: 10.1093/cid/ciw146. [http://dx.doi.org/10.1093/cid/ciw146]. [PMID: 27001800]. [DOI] [PubMed] [Google Scholar]
- 88.Zwahlen M., Harris R., May M., et al. Mortality of HIV-infected patients starting potent antiretroviral therapy: Comparison with the general population in nine industrialized countries. Int. J. Epidemiol. 2009;38(6):1624–1633. doi: 10.1093/ije/dyp306. [http://dx.doi.org/10.1093/ije/dyp306]. [PMID: 19820106]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zhang F., Dou Z., Yu L., et al. The effect of highly active antiretroviral therapy on mortality among HIV-infected former plasma donors in China. Clin. Infect. Dis. 2008;47(6):825–833. doi: 10.1086/590945. [http://dx.doi.org/10.1086/590945]. [PMID: 18690805]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhao D.C., Wen Y., Ma Y., et al. Expansion of China’s free antiretroviral treatment program. Chin. Med. J. (Engl.) 2012;125(19):3514–3521. [PMID: 23044316]. [PubMed] [Google Scholar]
- 91.Antiretroviral Therapy for HIV Infection in Adults and Adolescents. Recommendations for a Public Health Approach. Revision; 2010. [http://www.who.int/hiv/pub/arv/adult2010/en/index.html] [PubMed] [Google Scholar]
- 92.The Joint United Nations Programme on HIV/AIDS. 90-90-90: An ambitious treatment target to help end the AIDS epidemic 2014. http://www.unaids.org/en/resources/documents/2014/90–90–90
- 93.World Health Organization. Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV 2015. http://www.who.int/hiv/pub/guidelines/earlyrelease-arv/en/ [PubMed]
- 94.Tang Z., Pan S.W., Ruan Y., et al. Effects of high CD4 cell counts on death and attrition among HIV patients receiving antiretroviral treatment: an observational cohort study. Sci. Rep. 2017;7(1):3129. doi: 10.1038/s41598-017-03384-7. [http://dx.doi.org/10.1038/s41598-017-03384-7]. [PMID: 28600549]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Pan S.W., Shen Z., Xing H., Ruan Y., Shao Y. High baseline CD4 counts and antiretroviral therapy cessation. Clin. Infect. Dis. 2018;67(4):644. doi: 10.1093/cid/ciy131. [http://dx.doi.org/10.1093/cid/ciy131]. [PMID: 29462265]. [DOI] [PubMed] [Google Scholar]
- 96.Guangxi Center for Disease Control and Prevention. Analysis of HIV/STD epidemic in. China: Guangxi; 2017. [Google Scholar]
- 97.Chen H., Yang X., Zhu Q., et al. Treatment for HIV prevention study in southwestern areas of China. Infect. Dis. Model. 2018;3:249–255. doi: 10.1016/j.idm.2018.09.007. [http://dx.doi.org/10.1016/j.idm.2018.09.007]. [PMID: 30839859]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Liu P., Tang Z., Lan G., et al. Early antiretroviral therapy on reducing HIV transmission in China: Strengths, weaknesses and next focus of the program. Sci. Rep. 2018;8(1):3431. doi: 10.1038/s41598-018-21791-2. [http://dx.doi.org/10.1038/s41598-018-21791-2]. [PMID: 29467460]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jordan M.R., Bennett D.E., Bertagnolio S., Gilks C.F., Sutherland D. World Health Organization surveys to monitor HIV drug resistance prevention and associated factors in sentinel antiretroviral treatment sites. Antivir Ther (Lond) 2008;13(Suppl. 2):15–23. [PMID: 18575188]. [PubMed] [Google Scholar]
- 100.Wang X., Yang L., Li H., et al. Factors associated with HIV virologic failure among patients on HAART for one year at three sentinel surveillance sites in China. Curr. HIV Res. 2011;9(2):103–111. doi: 10.2174/157016211795569122. [http://dx.doi.org/10.2174/157016211795569122]. [PMID: 21361864]. [DOI] [PubMed] [Google Scholar]
- 101.Liang S., Shen Z., Yan J., et al. Low virologic failure and drug resistance among HIV-infected patients receiving hospital-based ART while care and outreach through community in Guangxi, China. Front. Public Health. 2015;3:244. doi: 10.3389/fpubh.2015.00244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Li G., Liang S., Harrison T.J., et al. Prevalence of transmitted HIV-1 drug resistance remains low in Guangxi, China, eight years after scale-up of highly-active antiretroviral therapy. Intervirology. 2014;57(5):270–276. doi: 10.1159/000362366. [http://dx.doi.org/10.1159/000362366]. [PMID: 24994115]. [DOI] [PubMed] [Google Scholar]
- 103.Zhang J., Shen Z.Y., Li Z., et al. Genetic Characteristics of CRF01_AE among newly diagnosed HIV-1-infected 16- to 25-year olds in 3 geographic regions of Guangxi, China. Medicine (Baltimore) 2015;94(21):e894. doi: 10.1097/MD.0000000000000894. [http://dx.doi.org/10.1097/MD.0000000000000894]. [PMID: 26020400]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.The People’s Government of Guangxi Zhuang Autonomous Region. Implementation plan of Guangxi AIDS Conquering Project (2010-2014). 2010 [Google Scholar]
- 105.Chen Y., Tang Z., Tang S., et al. Decreasing HIV, syphilis, and hepatitis C infection after a decade of harm reduction implementation among drug users in Southwestern Areas of China. J. Stud. Alcohol Drugs. 2018;79(2):248–257. [http://dx.doi.org/10.15288/jsad.2018.79.248]. [PMID: 29553354]. [PubMed] [Google Scholar]
- 106.Chen Y., Abraham Bussell S., Shen Z., et al. declining inconsistent condom use but increasing HIV and syphilis prevalence among older male clients of female sex workers: Analysis from sentinel surveillance sites (2010-2015), Guangxi, China. Medicine (Baltimore) 2016;95(22):e3726. doi: 10.1097/MD.0000000000003726. [http://dx.doi.org/10.1097/MD.0000000000003726]. [PMID: 27258500]. [DOI] [PMC free article] [PubMed] [Google Scholar]


