Abstract
Introduction
Hypoalbuminemia (<3.5 mg/dL) is an accepted marker of malnutrition, but it was unknown if low albumin remained an independent predictor of post-operative complications following primary total hip (THA) and knee (TKA) arthroplasty.
Methods
The National Surgical Quality Improvement Program (NSQIP) database was queried for patients undergoing primary THA and TKA. Propensity score-matched analysis was used to control for co-morbid conditions.
Results
Patients with low albumin demonstrated greater odds of death (by 2–21x), morbidity (by 25–51%), re-admission (by 45–54%), and increased length of stay.
Conclusion
Low albumin remains an independent predictor of adverse outcomes following primary total joint arthroplasty.
Keywords: Malnutrition, Outcomes, Primary knee arthroplasty, Primary hip arthroplasty, Albumin
1. Introduction
Total hip (THA) and knee (TKA) arthroplasty are two of the most commonly performed surgical procedures in the United States,1 and they are expected to continue to rise in volume over the coming decades.2 However, despite total joint arthroplasty (TJA) being common-place for the treatment of end-stage degenerative arthritis, major complications still occur in a minority of cases.3,4
With a focus on improving performance and post-operative outcomes, previous studies have identified pre-operative risk factors, specifically those that are modifiable and associated with complications following TJA.3,4 Pre-operative nutritional status has emerged as one such potentially modifiable risk factor. Low pre-operative serum albumin (less than 3.5 mg/dL) is a widely accepted marker of malnutrition that has been implicated as a risk factor for post-operative complications in revision TJA,5,6 and in primary TJA even after correcting for patient obesity.7, 8, 9
These studies, although effective, were limited to open access American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) data available at the time. Since 2014, the number of primary TJA cases included in the NSQIP dataset has nearly doubled. Moreover, the patient population undergoing primary TJA is evolving; since 2000, the mean patient age as well as the proportion of cases involving women have both decreased.10 Given these demographic changes, the role of a low pre-operative albumin as a true independent predictor of post-operative complications following primary TJA is unknown. Additionally, a larger NSQIP database allows for higher powered analyses to isolate the effects of pre-operative risk factors such as low albumin while still correcting for a greater number of comorbid conditions.
The purpose of this study was to use a large, multi-center prospective clinical outcomes database to determine whether low pre-operative albumin remains significantly associated with post-operative complications including death and serious morbidity following primary THA and TKA, even after correcting for several comorbid conditions. We hypothesized that low albumin would be significantly associated with an increased risk for post-operative complications following TJA. We further looked to quantify the difference in risk among THA patients compared with TKA patients.
2. Methods
The NSQIP participant use data file for 2010 to 2016 was accessed, and Current Procedural Terminology (CPT) codes were used to identify patients who underwent primary THA (27130) or primary TKA (27447). International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) coding for hip or proximal tibia and/or distal femur fracture [733.X, 820.X, 821.X, 822.X, 823.X, M80.X, M81.X, M84.X, M96.6, and S72.X] were used to exclude patients undergoing TJA as treatment for a diagnosis of prior fracture. The 2016 NSQIP participant use file contained data from 680 participating institutions. This study was reviewed and deemed exempt by our institutional review board.
Only cases that contained complete data for pre-operative albumin level were included in the final analysis. Pre-operative albumin level was examined using binary and categorical variables (Table 1).
Table 1.
Binary and categorical patient factors included in analysis.
| Patient Factors |
|---|
| Binary |
| Low albumin (<3.5 mg/dL) |
| Sex |
| Advanced age (≥70 years) |
| Outpatient ASA classification (high vs. low) |
| Obesity (BMI > 30 kg/m2) |
| Diabetes |
| Hypertension requiring medication |
| Rheumatoid arthritis (vs. osteoarthritis) |
| Current smoker |
| General Anestheisa |
| Chronic obstructive pulmonary disease |
| Chronic steroid use |
| Renal failure requiring dialysis |
| Cancer |
| Post-Traumatic |
| Low hematocrit (<30%) |
| Elevated creatinine (≥2 mg/dL) |
| Low platelets (<100 billion cells/L) |
| High bilirubin (≥2 mg/dL) |
| Categorical |
| Race |
| Functional status |
The primary outcomes for this study were death and serious medical morbidity within 30 days of the index procedure. Each primary outcome was analyzed separately for primary THA and primary TKA patients. Serious medical morbidity was defined as surgical site infection, respiratory event, cardiac event, bleeding with need for transfusion, and sepsis.
Secondary outcome measures included long operative time (>1 standard deviation above the mean), prolonged length of stay (>5 days), reoperation within 30 days, re-admission within 30 days, and discharge to a non-home facility.
Analysis was performed using Stata IC 14.2 statistical software (StataCorp, College Station, TX). Univariate analysis was performed using Pearson's chi-square test or Fisher's exact test to determine associations with pre-operative hypoalbuminemia for all categorical pre-operative characteristics and post-operative categorical outcomes. Association with seven different primary and secondary outcomes was deemed significant for p values of ≤0.007 according to Bonferroni's correction (0.05 ÷ 7 ≈ 0.007).
Propensity score matching was then used to adjust for potential confounders when determining the independent association of hypoalbuminemia with primary and secondary outcomes. In this method, “case” (low albumin) and “control” (normal albumin) groups were matched on a 1:1 basis, without replacement, using logistic regression modeling. The resulting propensity score-matched “case” and “control” groups – now similar with respect to all categorical pre-operative variables except for albumin status, and therefore free of identifiable confounding variables – were then directly compared to determine the odds conferred by hypoalbuminemia on primary and secondary outcomes.
ACS NSQIP and the hospitals participating in the ACS NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
3. Results
3.1. Patient demographics
The NSQIP database included 135,013 patients who underwent primary THA and 225,123 who underwent primary TKA without preceding trauma or fracture during the time period of 2010–2016. Data on pre-operative albumin levels were available for 65,023 (48.16%) patients undergoing THA and 108,556 (48.22%) patients undergoing TKA. For both procedures, patients with low albumin were more likely to have received general anesthesia (THA: 61.59% vs. 56.36%, p < 0.001; TKA: 58.75% vs. 53.05%, p < 0.001). Demographics of both THA and TKA cohorts demonstrated significant differences with respect to sex, advanced age, race, functional status, ASA class, diabetes, hypertension, arthritis type, smoking, COPD, chronic steroid use, dialysis, cancer, anemia, elevated creatinine, and thrombocytopenia (Table 2, Table 3). Additionally, the THA cohort demonstrated a significant difference for hyperbilirubinemia (Table 2), and the TKA cohort demonstrated a significant difference for obesity (Table 3).
Table 2.
Overall demographics and comorbidities for patients undergoing primary total hip arthroplasty (THA) with known pre-operative albumin.
| Primary Total Hip Arthroplasty |
|||||||
|---|---|---|---|---|---|---|---|
| Overall (n [%]) | Alb < 3.5 (n [%]) | Alb > 3.5 (n [%]) | P | ||||
| Total | 65,023 | (100.00) | 2795 | (4.30) | 62,228 | (95.70) | |
| Sex | |||||||
| Male | 29,549 | (45.49) | 1071 | (38.33) | 28,478 | (45.81) | <.001 |
| Female | 35,410 | (54.51) | 1723 | (61.67) | 33,687 | (54.19) | |
| Age | |||||||
| <70 yr | 42,504 | (65.37) | 1447 | (51.77) | 41,057 | (65.98) | <.001 |
| ≥70 yr | 22,519 | (34.63) | 1348 | (48.23) | 21,171 | (34.02) | |
| Race | |||||||
| White | 53,605 | (89.14) | 2240 | (85.86) | 51,365 | (89.29) | <.001 |
| Black | 5260 | (8.75) | 321 | (12.30) | 4939 | (8.59) | |
| Hispanic | 805 | (1.34) | 29 | (1.11) | 776 | (1.35) | |
| Hawaiian | 126 | (0.21) | 2 | (0.08) | 124 | (0.22) | |
| American Indian | 339 | (0.56) | 17 | (0.65) | 322 | (0.56) | |
| Functional status | |||||||
| Independent | 63,293 | (97.67) | 2506 | (91.13) | 60,787 | (98.06) | <.001 |
| Partially Dependent | 1446 | (2.23) | 244 | (8.87) | 1202 | (1.94) | |
| Totally Dependent | 67 | (0.10) | 24 | (0.87) | 43 | (0.07) | |
| Outpatient | |||||||
| ASA class | |||||||
| Low | 35,919 | (55.24) | 836 | (29.91) | 35,083 | (56.38) | <.001 |
| High | 29,104 | (44.76) | 1959 | (70.09) | 27,145 | (43.62) | |
| Comorbidities | |||||||
| Obesity (BMI >30 kg/m^2) | 30,676 | (47.18) | 1291 | (46.19) | 29,385 | (47.22) | 0.285 |
| Diabetes | 8276 | (12.73) | 494 | (17.67) | 7782 | (12.51) | <.001 |
| Hypertension Medication | 38,320 | (58.93) | 1876 | (67.12) | 36,444 | (58.57) | <.001 |
| Arthritis | |||||||
| Osteoarthritis | 58,461 | (99.57) | 2103 | (98.83) | 56,358 | (99.60) | <.001 |
| Rheumatoid Arthritis | 251 | (0.43) | 25 | (1.17) | 226 | (0.40) | |
| Smoker | 8902 | (13.69) | 482 | (17.25) | 8420 | (13.53) | <.001 |
| General Anesthesia | 36,751 | (56.58) | 1717 | (61.59) | 35,034 | (56.36) | <.001 |
| COPD | 2906 | (4.47) | 263 | (9.41) | 2643 | (4.25) | <.001 |
| Chronic steroid | 2919 | (4.49) | 315 | (11.27) | 2604 | (4.18) | <.001 |
| Dialysis | 192 | (0.30) | 58 | (2.08) | 134 | (0.22) | <.001 |
| Cancer | 296 | (0.46) | 60 | (2.15) | 236 | (0.38) | <.001 |
| Low Hematocrit (<30) | 760 | (1.17) | 215 | (7.69) | 545 | (0.88) | <.001 |
| High Creatinine (≥2 mg/dL) | 922 | (1.42) | 151 | (5.40) | 771 | (1.24) | <.001 |
| Low Platelets (<100 bil cells/L) | 478 | (0.74) | 81 | (97.10) | 397 | (99.36) | <.001 |
| High Bilirubin (≥2 mg/dL) | 6306 | (9.70) | 230 | (8.23) | 6076 | (9.76) | 0.007 |
| Post-Traumatic | 367 | (0.62) | 32 | (1.50) | 335 | (0.59) | <.001 |
Table 3.
Overall demographics and comorbidities for patients undergoing primary total knee arthroplasty (TKA) with known pre-operative albumin.
| Primary Total Knee Arthroplasty |
|||||||
|---|---|---|---|---|---|---|---|
| Overall (n [%]) | Alb < 3.5 (n [%]) | Alb > 3.5 (n [%]) | P | ||||
| Total | 108,556 | (100.00) | 4596 | (4.23) | 103,960 | (95.77) | |
| Sex | |||||||
| Male | 41,093 | (37.89) | 1424 | (31.01) | 39,669 | (38.20) | <.001 |
| Female | 67,355 | (62.11) | 3168 | (68.99) | 64,187 | (61.80) | |
| Age | |||||||
| <70 yr | 67,014 | (61.73) | 2616 | (56.92) | 64,398 | (61.94) | <.001 |
| ≥70 yr | 41,542 | (38.27) | 1980 | (43.08) | 39,562 | (38.06) | |
| Race | |||||||
| White | 89,400 | (88.79) | 3603 | (83.17) | 85,797 | (89.04) | <.001 |
| Black | 8383 | (8.33) | 631 | (14.57) | 7752 | (8.05) | |
| Hispanic | 1912 | (1.90) | 52 | (1.20) | 1860 | (1.93) | |
| Hawaiian | 265 | (0.26) | 12 | (0.28) | 253 | (0.26) | |
| American Indian | 728 | (0.72) | 34 | (0.78) | 694 | (0.72) | |
| Functional status | |||||||
| Independent | 106,398 | (98.55) | 4368 | (95.98) | 102,030 | (98.72) | |
| Partially Dependent | 1502 | (1.39) | 183 | (4.02) | 1319 | (1.28) | |
| Totally Dependent | 59 | (0.05) | 11 | (0.24) | 48 | (0.05) | |
| Outpatient | |||||||
| ASA class | |||||||
| Low | 53,516 | (49.30) | 1397 | (30.40) | 52,119 | (50.13) | <.001 |
| High | 55,040 | (50.70) | 3199 | (69.60) | 51,841 | (49.87) | |
| Comorbidities | |||||||
| Obesity (BMI >30 kg/m^2) | 69,282 | (63.82) | 3136 | (68.23) | 66,146 | (63.63) | <.001 |
| Diabetes | 20,763 | (19.13) | 1151 | (25.04) | 19,612 | (18.86) | <.001 |
| Hypertension Medication | 73,129 | (67.37) | 3363 | (73.17) | 69,766 | (67.11) | <.001 |
| Arthritis | |||||||
| Osteoarthritis | 104,897 | (99.50) | 4265 | (98.32) | 100,632 | (99.55) | <.001 |
| Rheumatoid Arthritis | 524 | (0.50) | 73 | (1.68) | 451 | (0.45) | |
| Smoker | 9508 | (8.76) | 553 | (12.03) | 8955 | (8.61) | <.001 |
| General Anesthesia | 57,784 | (53.29) | 2697 | (58.75) | 55,087 | (53.05) | <.001 |
| COPD | 4321 | (3.98) | 348 | (7.57) | 3973 | (3.82) | <.001 |
| Chronic steroid | 4575 | (4.21) | 415 | (9.03) | 4160 | (4.00) | <.001 |
| Dialysis | 211 | (0.19) | 52 | (1.13) | 159 | (0.15) | <.001 |
| Cancer | 137 | (0.13) | 13 | (0.28) | 124 | (0.12) | 0.002 |
| Low Hematocrit (<30) | 881 | (0.81) | 188 | (4.09) | 693 | (0.67) | <.001 |
| High Creatinine (≥2 mg/dL) | 1263 | (1.16) | 168 | (3.66) | 1095 | (1.05) | <.001 |
| Low Platelets (<100 bil cells/L) | 734 | (0.68) | 122 | (2.65) | 612 | (0.59) | <.001 |
| High Bilirubin (≥2 mg/dL) | 8359 | (7.70) | 322 | (7.01) | 8037 | (7.73) | 0.071 |
| Post-Traumatic | 901 | (0.85) | 41 | (0.95) | 860 | (0.85) | 0.464 |
3.2. Unmatched cohort analysis
Of patients undergoing THA, 7776 (11.96%) died or had serious morbidity; there were 102 deaths (0.16%) and 7752 (11.92%) with serious morbidities, and 2447 (3.91%) were re-admitted within 30 days. Of patients undergoing TKA, 10,036 (9.24%) died or had serious morbidity; there were 125 (0.12%) deaths and 10,005 (9.22%) with serious morbidities, and 3719 (3.56%) were re-admitted within 30 days.
Unadjusted analysis performed separately on both THA (Table A1) and TKA (Table A2) cohorts demonstrated that for both cohorts, low pre-operative albumin was associated with increased odds of death, length of stay over 5 days, discharge to facility, re-admission, reoperation, and serious morbidity including respiratory complications, bleeding requiring transfusion, and sepsis.
3.3. Propensity score-matched cohort analysis
Propensity score matching resulted in matched THA and TKA cohorts of 4692 and 8238 patients, respectively, with exactly one half of all patients in each cohort having low albumin. Significant differences originally observed in the unmatched cohorts with respect to sex, advanced age, race, functional status, ASA class, diabetes, hypertension, smoking, COPD, chronic steroid use, dialysis, cancer, anemia, elevated creatinine, thrombocytopenia, and obesity were no longer present after matching (Tables A3 and A.4).
Univariate analysis performed separately on both matched THA (Table A3) and TKA (Table A4) cohorts demonstrated that for both cohorts, low pre-operative albumin was still associated with length of stay over 5 days, discharge to non-home facility, and serious morbidity. In both cohorts, patients with low albumin had significantly longer length of stay (THA: +0.70 [0.54, 0.86] days, p < 0.001; TKA: +0.27 [0.14, 0.40] days, p < 0.001). In addition, for the THA cohort alone, low albumin was also still associated with increased odds of death and increased odds of sepsis and bleeding requiring transfusion. Mean age and operative time were no longer significantly different.
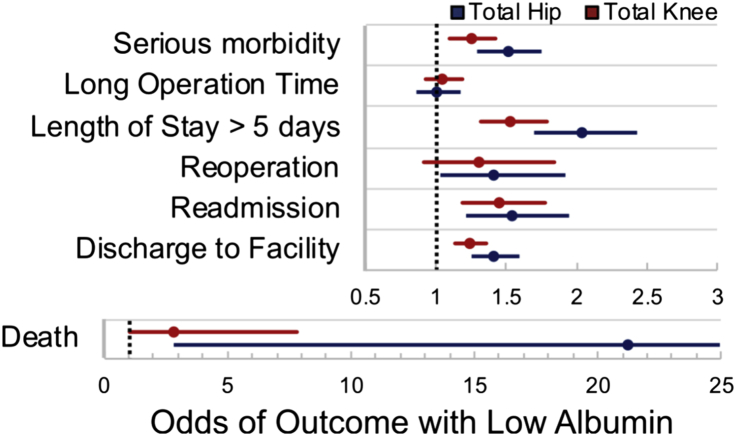
Logistic regression performed separately on both matched THA and TKA cohorts (Table 4) demonstrated that for both cohorts, low albumin remained significantly associated with serious morbidity, length of stay greater than five days, re-admission, and discharge to non-home facility. After matching, the THA cohort demonstrated a significant association between low albumin and death, but the TKA cohort did not (Fig. 1).
Table 4.
Outcomes independently associated with low albumin following primary total hip (THA) and knee (TKA) arthroplasty after application of logistic regression model in matched cohorts.
| Patients with Low Albumin | Logistic Regression – Matched Cohort |
|||||||
|---|---|---|---|---|---|---|---|---|
| Primary THA |
Primary TKA |
|||||||
| OR | 95% CI | P | OR | 95% CI | P | |||
| Death | 21.19 | 2.85 | 157.66 | 0.003 | 2.81 | 1.01 | 7.80 | 0.048 |
| Serious morbidity | 1.51 | 1.30 | 1.75 | <.001 | 1.25 | 1.09 | 1.43 | 0.001 |
| Long Operation Time | 1.01 | 0.86 | 1.18 | 0.906 | 1.05 | 0.92 | 1.19 | 0.458 |
| Length of Stay >5 days | 2.03 | 1.70 | 2.43 | <.001 | 1.53 | 1.32 | 1.79 | <.001 |
| Reoperation | 1.41 | 1.03 | 1.92 | 0.031 | 1.30 | 0.92 | 1.84 | 0.136 |
| Readmission | 1.54 | 1.21 | 1.95 | <.001 | 1.45 | 1.19 | 1.78 | <.001 |
| Discharge to Facility | 1.42 | 1.26 | 1.60 | <.001 | 1.25 | 1.14 | 1.36 | <.001 |
Fig. 1.
Forest plot of outcomes associated with low albumin following primary total hip (THA) and knee (TKA) arthroplasty after application of logistic regression model in matched cohorts. Odds ratio with 95% confidence intervals are shown.
4. Discussion
We performed a retrospective, observational analysis of a large national cohort evaluating the impact of pre-operative low albumin on 30-day post-operative complications following primary THA and TKA. Primary outcomes were death and serious morbidity; secondary outcomes were re-admission, reoperation, long operative time, discharge to non-home facility, and length of stay greater than five days. Consistent with our hypothesis, pre-operative low albumin was associated with death or serious morbidity in univariate unmatched analysis, univariate propensity score-matched analysis, and propensity-matched logistic regression analysis. In addition, even after propensity score-matching, low albumin also remained associated with greater odds of re-admission within 30 days, length of stay greater than five days, and discharge to a non-home facility.
This study has several limitations. First, and most notable, out of all patients in the NSQIP cohort undergoing TJA, only 48% had pre-operative albumin data available. The non-uniform availability of albumin data may be due in part to various provider and health system-related differences in pre-operative testing that might be expected in such a large multi-center outcomes database. However, there also exists selection bias, in that providers would be more likely to include serum albumin as part of pre-operative testing for patients that tended to be less healthy with a greater number of medical comorbidities. In addition, this study may underestimate the number of malnourished patients undergoing TJA, given that the NSQIP only reports on one nutritional marker, meanwhile neglecting other important markers such as pre-albumin, ferritin and transferrin. Additionally, NSQIP only includes outcomes up to 30 days following surgery, and potentially underestimates the effects of hypoalbuminemia beyond the 30-day period.
Despite its limitations, the results of this study corroborate the findings of several retrospective studies that have described the effects of low serum albumin on post-operative outcomes following TJA.3,4,7, 8, 9 In a pooled analysis of patients undergoing either TKA or THA, Bohl et al. identified approximately 4% of patients having low albumin associated with increased length of stay and re-admission.9 That rate of hypoalbuminemia is similar to the 4.3% and 4.2% of patients undergoing THA and TKA (without pooling) observed in the present study, as are the findings regarding increased length of stay and re-admission associated with low albumin. The relationship between pre-operative low albumin and post-operative complications has also been described separately both for primary TKA4,7,11 and primary THA.3,11, 12, 13
The results of the present study highlight an opportunity for targeted intervention with a goal of optimizing pre-operative nutrition and, in patients with low albumin, allowing these values to normalize prior to elective surgical intervention.14 Previous studies have explored the benefits of pre-operative nutritional supplementation with some success.15, 16, 17, 18, 19 In a randomized controlled trial of 80 patients who underwent surgical fixation for treatment of traumatic hip fracture, post-operative intravenous and oral dietary supplementation was associated with decreased risk of fracture-related complication and decreased mortality.18 The benefits of nutritional supplementation have also been shown in non-trauma patients undergoing elective TJA. For example, in a randomized controlled trial of 162 patients undergoing primary total knee arthroplasty, patients randomized to pre-operative enrollment in a multimodal nutrition program were found to have decreased length of stay by 1.7 days.19
Despite the association with albumin, worth noting is that albumin as a marker of protein energy deficiency20 is likely merely an indicator of underlying medical unsuitability for elective surgery – colloquially described by terms such as “poor protoplasm” or “frailty”.21 Such an indicative rather than causative role of albumin has also been suggested by a previous report, in which correction of serum albumin alone did not necessarily result in improved outcomes.22
One of the most striking findings in the present study was the ∼21.2 times significantly increased odds of death associated with low albumin in patients undergoing primary THA (p = 0.003) identified by logistic regression in the matched cohort, in contrast to the ∼2.8 times increased odds in patients undergoing TKA (p = 0.048) which did not meet statistical significance (Table 4). An alternative interpretation is that pre-operative albumin may confer a greater significant mortality predisposition to patients undergoing THA as compared to TKA. A recent retrospective comparison of NSQIP outcomes following THA and TKA supports this concept, identifying increased rates of re-admission and re-operation associated with THA.11 Therefore, it is possible that the THA patient population or THA procedure itself may confer greater risk of post-operative complication, and that pre-operative optimization in the THA patient population may be of even greater importance than in patients undergoing TKA. In addition to low albumin having a greater association with increased post-operative mortality risk among THA patients compared with TKA patients, pre-operative hypoalbuminemia was associated with a greater effect on length of stay for THA patients compared with TKA patients. Pre-operative low albumin added an average 0.70 days to length of stay following THA compared to 0.36 additional days following TKA, both of which may be associated with greater healthcare costs.23 Importantly, the present study excludes total hip replacements performed following trauma, such as in the case of the geriatric hip fracture, where patients may undergo urgent surgery including total hip arthroplasty without the same level of pre-operative medical optimization as might be seen prior to elective surgery. In the geriatric hip fracture population, pre-operative low albumin may be associated with a risk of death as high as 9.94%.24
5. Conclusions
Hypoalbuminemia (<3.5 mg/dL) remains a significant independent predictor of adverse outcomes in patients undergoing primary THA and TKA, even after controlling for several comorbid conditions. The adverse effects of low albumin may be even greater in patients undergoing THA as compared to patients undergoing TKA, though risks remain elevated in both populations. The findings of this study suggest a need to limit elective surgery on patients with low albumin and consultation with a nutritionist for pre-operative optimization. Future research should determine the length of treatment and efficacy of pre-operative nutritional supplementation in mitigating these risks.
Declarations of interest
Dr. George Fryhofer has nothing to disclose.
Dr. Matthew Sloan has nothing to disclose.
Dr. Neil Sheth reports personal fees from Zimmer (consulting), personal fees from Smith and Nephew (consulting), personal fees from Medacta (consulting), and personal fees from Elsevier (royalites), all outside the submitted work.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Table A1.
| Primary Total Hip Arthroplasty – Unmatched Cohort |
|||||||
|---|---|---|---|---|---|---|---|
| Overall (n [%]) | Alb < 3.5 (n [%]) | Alb > 3.5 (n [%]) | P | ||||
| Death or serious morbidity | 7776 | (11.96) | 685 | (24.51) | 7091 | (11.40) | <.001 |
| Death | 102 | (0.16) | 32 | (1.15) | 70 | (0.11) | <.001 |
| Serious morbidity | 7752 | (11.92) | 678 | (24.26) | 7074 | (11.37) | <.001 |
| Surgical Site Infection | 7 | (0.01) | 3 | (0.11) | 4 | (0.01) | 0.002* |
| Respiratory | 131 | (0.20) | 22 | (0.79) | 109 | (0.18) | <.001 |
| Cardiac | 686 | (1.06) | 61 | (2.18) | 625 | (1.00) | <.001 |
| Bleeding | 7037 | (10.82) | 617 | (22.08) | 6420 | (10.32) | <.001 |
| Sepsis | 197 | (0.30) | 29 | (1.04) | 168 | (0.27) | <.001 |
| Long Operative Time | 9389 | (14.44) | 469 | (16.78) | 8920 | (14.33) | <.001 |
| Length of Stay > 5 days | 4856 | (7.47) | 588 | (21.04) | 4268 | (6.86) | <.001 |
| Discharge to Facility | 15,613 | (24.66) | 1178 | (43.73) | 14,435 | (23.82) | <.001 |
| Readmission Within 30 Days | 2447 | (3.91) | 225 | (8.40) | 2222 | (3.71) | <.001 |
| Required Reoperation | 1389 | (2.20) | 120 | (4.45) | 1269 | (2.10) | <.001 |
Table A2.
| Primary Total Knee Arthroplasty – Unmatched Cohort |
|||||||
|---|---|---|---|---|---|---|---|
| Overall (n [%]) | Alb < 3.5 (n [%]) | Alb > 3.5 (n [%]) | P | ||||
| Death or serious morbidity | 10,036 | (9.24) | 649 | (14.12) | 9387 | (9.03) | <.001 |
| Death | 125 | (0.12) | 17 | (0.37) | 108 | (0.10) | <.001 |
| Serious morbidity | 10,005 | (9.22) | 645 | (14.03) | 9360 | (9.00) | <.001 |
| Surgical Site Infection | 11 | (0.01) | 1 | (0.02) | 10 | (0.01) | 0.378* |
| Respiratory | 187 | (0.17) | 24 | (0.52) | 163 | (0.16) | <.001 |
| Cardiac | 18,888 | (1.74) | 102 | (2.22) | 1786 | (1.72) | 0.011 |
| Bleeding | 8089 | (7.45) | 546 | (11.88) | 7543 | (7.26) | <.001 |
| Sepsis | 221 | (0.20) | 19 | (0.41) | 202 | (0.19) | 0.001 |
| Long Operative Time | 14,587 | (13.44) | 643 | (13.99) | 13,944 | (13.41) | 0.261 |
| Length of Stay > 5 days | 7612 | (7.01) | 577 | (12.55) | 7035 | (6.77) | <.001 |
| Discharge to Facility | 29,687 | (28.17) | 1769 | (39.77) | 27,918 | (27.66) | <.001 |
| Readmission Within 30 Days | 3719 | (3.56) | 278 | (6.29) | 3441 | (3.44) | <.001 |
| Required Reoperation | 1292 | (1.23) | 90 | (2.02) | 1202 | (1.19) | <.001 |
Table A3.
| Primary THA – Matched Cohort |
|||||||
|---|---|---|---|---|---|---|---|
| Overall (no. [%]) | Alb < 3.5 (n [%]) | Alb > 3.5 (n [%]) | P | ||||
| Total | 4692 | (100.00) | 2346 | (50.00) | 2346 | (50.00) | |
| Sex | |||||||
| Male | 2346 | (50.00) | 877 | (37.38) | 871 | (37.13) | 0.856 |
| Female | 2346 | (50.00) | 1469 | (62.62) | 1475 | (62.87) | |
| Age | |||||||
| <70 yr | 2430 | (51.79) | 1215 | (51.79) | 1215 | (51.79) | 1.000 |
| ≥70 yr | 2262 | (48.21) | 1131 | (48.21) | 1131 | (48.21) | |
| Race | |||||||
| White | 4088 | (87.13) | 2044 | (87.13) | 2044 | (87.13) | 0.883 |
| Black | 548 | (11.68) | 273 | (11.64) | 275 | (11.72) | |
| Hispanic | 34 | (0.72) | 18 | (0.77) | 16 | (0.68) | |
| Hawaiian | 1 | (0.02) | 1 | (0.04) | 0 | (0.00) | |
| American Indian | 21 | (0.45) | 10 | (0.43) | 11 | (0.47) | |
| Functional status | |||||||
| Independent | 4394 | (93.65) | 2198 | (93.69) | 2196 | (93.61) | 0.940 |
| Partially Dependent | 287 | (6.12) | 142 | (6.05) | 145 | (6.18) | |
| Totally Dependent | 11 | (0.23) | 6 | (0.26) | 5 | (0.21) | |
| Outpatient | |||||||
| ASA class | |||||||
| Low | 1510 | (32.18) | 758 | (32.31) | 752 | (32.05) | 0.851 |
| High | 3182 | (67.82) | 1588 | (67.69) | 1594 | (67.95) | |
| Comorbidities | |||||||
| Obesity (BMI >30 kg/m^2) | 2218 | (47.27) | 1109 | (47.27) | 1109 | (47.27) | 1.000 |
| Diabetes | 766 | (16.33) | 381 | (16.24) | 385 | (16.41) | 0.874 |
| Hypertension Medication | 3155 | (67.24) | 1578 | (67.26) | 1577 | (67.22) | 0.975 |
| Smoker | 765 | (16.30) | 381 | (16.24) | 384 | (16.37) | 0.906 |
| COPD | 385 | (8.21) | 192 | (8.18) | 193 | (8.23) | 0.958 |
| Chronic steroid | 445 | (9.48) | 226 | (9.63) | 219 | (9.34) | 0.727 |
| Dialysis | 22 | (0.47) | 11 | (0.47) | 11 | (0.47) | 1.000 |
| Cancer | 35 | (0.75) | 18 | (0.77) | 17 | (0.72) | 0.865 |
| Low Hematocrit (<30) | 171 | (3.64) | 84 | (3.58) | 87 | (3.71) | 0.815 |
| High Creatinine (≥2 mg/dL) | 117 | (2.49) | 60 | (2.56) | 57 | (2.43) | 0.779 |
| Low Platelets (<100 bil cells/L) | 82 | (1.75) | 43 | (1.83) | 39 | (1.66) | 0.656 |
| High Bilirubin (≥2 mg/dL) | 261 | (5.56) | 132 | (5.63) | 129 | (5.50) | 0.848 |
Table A4.
| Primary TKA – Matched Cohort |
|||||||
|---|---|---|---|---|---|---|---|
| Overall (no. [%]) | Alb < 3.5 (n [%]) | Alb > 3.5 (n [%]) | P | ||||
| Total | 8238 | (100.00) | 4119 | (50.00) | 4119 | (50.00) | |
| Sex | |||||||
| Male | 2527 | (30.67) | 1264 | (30.69) | 1263 | (30.66) | 0.981 |
| Female | 5711 | (69.33) | 2855 | (69.31) | 2856 | (69.34) | 0.981 |
| Age | |||||||
| <70 yr | 4665 | (56.63) | 2335 | (56.69) | 2330 | (56.57) | 0.911 |
| ≥70 yr | 3573 | (43.37) | 1784 | (43.31) | 1789 | (43.43) | |
| Race | |||||||
| White | 6912 | (83.90) | 3455 | (83.88) | 3457 | (83.93) | 0.999 |
| Black | 1171 | (14.21) | 586 | (14.23) | 585 | (14.20) | |
| Hispanic | 91 | (1.10) | 45 | (1.09) | 46 | (1.12) | |
| Hawaiian | 17 | (0.21) | 9 | (0.22) | 8 | (0.19) | |
| American Indian | 47 | (0.57) | 24 | (0.58) | 23 | (0.56) | |
| Functional status | |||||||
| Independent | 7967 | (96.71) | 3981 | (96.65) | 3986 | (96.77) | 0.916 |
| Partially Dependent | 262 | (3.18) | 133 | (3.23) | 129 | (3.13) | |
| Totally Dependent | 9 | (0.11) | 5 | (0.12) | 4 | (0.10) | |
| Outpatient | |||||||
| ASA class | |||||||
| Low | 2539 | (30.82) | 1271 | (30.86) | 1268 | (30.78) | 0.943 |
| High | 5699 | (69.18) | 2848 | (69.14) | 2851 | (69.22) | |
| Comorbidities | |||||||
| Obesity (BMI >30 kg/m^2) | 5709 | (69.30) | 2852 | (69.24) | 2857 | (69.36) | 0.905 |
| Diabetes | 2033 | (24.68) | 1016 | (24.67) | 1017 | (24.69) | 0.980 |
| Hypertension Medication | 6083 | (73.84) | 3042 | (73.85) | 3041 | (73.83) | 0.980 |
| Smoker | 950 | (11.53) | 475 | (11.53) | 475 | (11.53) | 1.000 |
| COPD | 578 | (7.02) | 290 | (7.04) | 288 | (6.99) | 0.931 |
| Chronic steroid | 645 | (7.83) | 323 | (7.84) | 322 | (7.82) | 0.967 |
| Dialysis | 27 | (0.33) | 14 | (0.34) | 13 | (0.32) | 0.847 |
| Cancer | 12 | (0.15) | 5 | (0.15) | 6 | (0.15) | 1.000 |
| Low Hematocrit (<30) | 198 | (2.40) | 98 | (2.38) | 100 | (2.43) | 0.886 |
| High Creatinine (≥2 mg/dL) | 192 | (2.33) | 96 | (2.33) | 96 | (2.33) | 1.000 |
| Low Platelets (<100 bil cells/L) | 153 | (1.86) | 76 | (1.85) | 77 | (1.87) | 0.935 |
| High Bilirubin (≥2 mg/dL) | 394 | (4.78) | 197 | (4.78) | 197 | (4.78) | 1.000 |
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.HCUP Fast Stats. Healthcare Cost and Utilization Project (HCUP) www.hcup-us.ahrq.gov/faststats/national/inpatientcommonprocedures.jsp. Accessed 4/30/2018.
- 2.Sloan M., Premkumar A., Sheth N.P. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am Vol. 2018;100(17):1455–1460. doi: 10.2106/JBJS.17.01617. [DOI] [PubMed] [Google Scholar]
- 3.Belmont P.J., Jr., Goodman G.P., Hamilton W., Waterman B.R., Bader J.O., Schoenfeld A.J. Morbidity and mortality in the thirty-day period following total hip arthroplasty: risk factors and incidence. J Arthroplast. 2014;29(10):2025–2030. doi: 10.1016/j.arth.2014.05.015. [DOI] [PubMed] [Google Scholar]
- 4.Belmont P.J., Jr., Goodman G.P., Waterman B.R., Bader J.O., Schoenfeld A.J. Thirty-day postoperative complications and mortality following total knee arthroplasty: incidence and risk factors among a national sample of 15,321 patients. J Bone Joint Surg Am Vol. 2014;96(1):20–26. doi: 10.2106/JBJS.M.00018. [DOI] [PubMed] [Google Scholar]
- 5.Kamath A.F., Nelson C.L., Elkassabany N., Guo Z., Liu J. Low albumin is a risk factor for complications after revision total knee arthroplasty. J Knee Surg. 2017;30(3):269–275. doi: 10.1055/s-0036-1584575. [DOI] [PubMed] [Google Scholar]
- 6.Bohl D.D., Shen M.R., Kayupov E., Cvetanovich G.L., Della Valle C.J. Is hypoalbuminemia associated with septic failure and acute infection after revision total joint arthroplasty? A study of 4517 patients from the national surgical quality improvement program. J Arthroplast. 2016;31(5):963–967. doi: 10.1016/j.arth.2015.11.025. [DOI] [PubMed] [Google Scholar]
- 7.Fu M.C., McLawhorn A.S., Padgett D.E., Cross M.B. Hypoalbuminemia is a better predictor than obesity of complications after total knee arthroplasty: a propensity score-adjusted observational analysis. HSS J. 2017;13(1):66–74. doi: 10.1007/s11420-016-9518-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nelson C.L., Elkassabany N.M., Kamath A.F., Liu J. Low albumin levels, more than morbid obesity, are associated with complications after TKA. Clin Orthop Relat Res. 2015;473(10):3163–3172. doi: 10.1007/s11999-015-4333-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bohl D.D., Shen M.R., Kayupov E., Della Valle C.J. Hypoalbuminemia independently predicts surgical site infection, pneumonia, length of stay, and readmission after total joint arthroplasty. J Arthroplast. 2016;31(1):15–21. doi: 10.1016/j.arth.2015.08.028. [DOI] [PubMed] [Google Scholar]
- 10.Sloan MP N.S. AAOS 2018 Annual Meeting; Tuesday, March 6, 2018. 2018. Changing demographics in primary and revision total joint arthroplasty, 2000-2014. New Orleans, LA. [Google Scholar]
- 11.George J., Chughtai M., Khlopas A. Readmission, reoperation, and complications: total hip vs total knee arthroplasty. J Arthroplast. 2018;33(3):655–660. doi: 10.1016/j.arth.2017.09.048. [DOI] [PubMed] [Google Scholar]
- 12.Mednick R.E., Alvi H.M., Krishnan V., Lovecchio F., Manning D.W. Factors affecting readmission rates following primary total hip arthroplasty. J Bone Joint Surg Am Vol. 2014;96(14):1201–1209. doi: 10.2106/JBJS.M.00556. [DOI] [PubMed] [Google Scholar]
- 13.Walls J.D., Abraham D., Nelson C.L., Kamath A.F., Elkassabany N.M., Liu J. Hypoalbuminemia more than morbid obesity is an independent predictor of complications after total hip arthroplasty. J Arthroplast. 2015;30(12):2290–2295. doi: 10.1016/j.arth.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 14.Nussenbaum F.D., Rodriguez-Quintana D., Fish S.M., Green D.M., Cahill C.W. Implementation of preoperative screening criteria lowers infection and complication rates following elective total hip arthroplasty and total knee arthroplasty in a veteran population. J Arthroplast. 2018;33(1):10–13. doi: 10.1016/j.arth.2017.07.031. [DOI] [PubMed] [Google Scholar]
- 15.Evans D.C., Martindale R.G., Kiraly L.N., Jones C.M. Nutrition optimization prior to surgery. Nutr Clin Pract. 2014;29(1):10–21. doi: 10.1177/0884533613517006. [DOI] [PubMed] [Google Scholar]
- 16.Jie B., Jiang Z.M., Nolan M.T., Zhu S.N., Yu K., Kondrup J. Impact of preoperative nutritional support on clinical outcome in abdominal surgical patients at nutritional risk. Nutrition. 2012;28(10):1022–1027. doi: 10.1016/j.nut.2012.01.017. [DOI] [PubMed] [Google Scholar]
- 17.Delmi M., Rapin C.H., Bengoa J.M., Delmas P.D., Vasey H., Bonjour J.P. Dietary supplementation in elderly patients with fractured neck of the femur. Lancet. 1990;335(8696):1013–1016. doi: 10.1016/0140-6736(90)91073-j. [DOI] [PubMed] [Google Scholar]
- 18.Eneroth M., Olsson U.B., Thorngren K.G. Nutritional supplementation decreases hip fracture-related complications. Clin Orthop Relat Res. 2006;451:212–217. doi: 10.1097/01.blo.0000224054.86625.06. [DOI] [PubMed] [Google Scholar]
- 19.Cao G., Huang Q., Xu B., Huang Z., Xie J., Pei F. Multimodal nutritional management in primary total knee arthroplasty: a randomized controlled trial. J Arthroplast. 2017;32(11):3390–3395. doi: 10.1016/j.arth.2017.06.020. [DOI] [PubMed] [Google Scholar]
- 20.Reeds P.J., Laditan A.A. Serum albumin and transferrin protein-energy malnutrition. Their use in the assessment of marginal undernutrition and the prognosis of severe undernutrition. Br J Nutr. 1976;36(2):255–263. doi: 10.1079/bjn19760077. [DOI] [PubMed] [Google Scholar]
- 21.Smith C.R. Frailty is to predictive as Jello is to wall. J Thorac Cardiovasc Surg. 2018;156(1):177. doi: 10.1016/j.jtcvs.2018.01.068. [DOI] [PubMed] [Google Scholar]
- 22.Vanek V.W. The use of serum albumin as a prognostic or nutritional marker and the pros and cons of IV albumin therapy. Nutr Clin Pract. 1998;13(3):110–122. doi: 10.1002/j.1941-2452.1998.tb03058.x. [DOI] [PubMed] [Google Scholar]
- 23.Haas D.A., Kaplan R.S. Variation in the cost of care for primary total knee arthroplasties. Arthroplast Today. 2017;3(1):33–37. doi: 10.1016/j.artd.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bohl D.D., Shen M.R., Hannon C.P., Fillingham Y.A., Darrith B., Della Valle C.J. Serum albumin predicts survival and postoperative course following surgery for geriatric hip fracture. J Bone Joint Surg Am Vol. 2017;99(24):2110–2118. doi: 10.2106/JBJS.16.01620. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.