Abstract
The distinction between tuberculous peritonitis and peritoneal carcinomatosis is extremely difficult in patients with omental cake appearance on computed tomography and elevated CA-125 level. A 21-year-old female presented with abdominal distention, diarrhea, nausea, fever, weight loss, and night sweats. Serum CA-125 level was 563 U/L (normal range: <35 U/L) and other tumor markers were within normal range. Radiologic studies showed massive ascites, smooth minimal thickening and increased contrast enhancement of peritoneum, omental nodularities, hepatomegaly, and right pleural effusion. No underlying malignancy that could cause this condition was detected clinically and radiologically. Ultrasound-guided omental tru-cut biopsy was performed to exclude carcinomatosis peritonei. Histopathologic examination showed small-medium-sized granulomas with caseous necrosis. Molecular microbiology tests of biopsy specimens confirmed diagnosis of tuberculosis. In conclusion, tuberculous peritonitis should be in differential diagnosis of a patient with ascites, omental nodularities and elevated serum CA-125 levels.
Keywords: Carcinomatosis peritonei, Computed tomography (CT), Tuberculous peritonitis, Ovarian cancer, CA-125
Introduction
Diagnosis of tuberculous peritonitis with clinical, laboratory, and imaging findings is a difficult process. Tuberculous peritonitis accounts for 1%-2% of all cases of tuberculosis and occurs when abdominal or pelvic tuberculosis involves the peritoneum [1,2]. Tuberculous peritonitis and carcinomatosis peritonei have many common clinical, laboratory, and radiological findings [3,4]. Although the increase in serum CA-125 level is an important laboratory marker for epithelial ovarian cancer, it also increases in inflammatory conditions including tuberculous peritonitis [5,6]. It may be very difficult to differentiate between tuberculous peritonitis and carcinomatosis peritonei in a patient with ascites, peritoneal thickening, omental cake appearance, and high CA-125 level [7,8]. Often, Mycobacterium tuberculosis cannot be isolated in ascites sampling and the diagnosis is made by histopathologic examination [4,5,9]. We present a young female patient with high CA-125 level and omental cake appearance on computed tomography (CT) imaging mimicking carcinomatosis peritonei but diagnosed as tuberculous peritonitis by histopathologic examination of the ultrasound-guided omental biopsy specimens.
Case report
A 21-year-old female patient without known disease admitted to the gynecology outpatient clinic with complaints of abdominal distention and pain for last 10 days. The patient also reported a small amount of watery yellow diarrhea, nausea, fever, and night sweats during the last month and lost approximately 8 kg during this period. Abdominal and pelvic ultrasonography showed ascites, omental nodularities, and thickening. No abnormal finding was observed in bilateral ovaries and uterus. Laboratory tests showed mild normocytic anemia (hemoglobin: 11.5 g/dL, Mean Corpuscular Volume (MCV): 83.8), and a significant increase in CA-125 level (CA-125: 563 U/mL. Normal range <35 U/mL). Alpha fetoprotein and β-human chorionic gonadotropin levels were within normal limits.
Abdominopelvic CT examination showed nonloculated diffuse ascites, smooth minimal thickening of the peritoneum, omental cake appearance, and hepatomegaly (Fig. 1). No pathologic abdominopelvic lymph node was detected. There was no solid or cystic lesion in the bilateral ovaries on CT or magnetic resonance imaging (Fig. 2).
Fig. 1.

A 21-year-old female patient with abdominal distention and pain for ten days. (A) Axial contrast-enhanced abdominopelvic CT examination: peritoneal minimal smooth thickening and increased contrast enhancement (red arrow) and diffuse ascites (green arrow) are seen. (B) Axial contrast-enhanced abdominopelvic CT scan: There is an omental cake appearance (blue arrows) on the upper slices of A. (C) Coronal contrast-enhanced abdominopelvic CT scan: hepatomegaly and ascites are observed. CT, computed tomography. (Color version of figure is available online.)
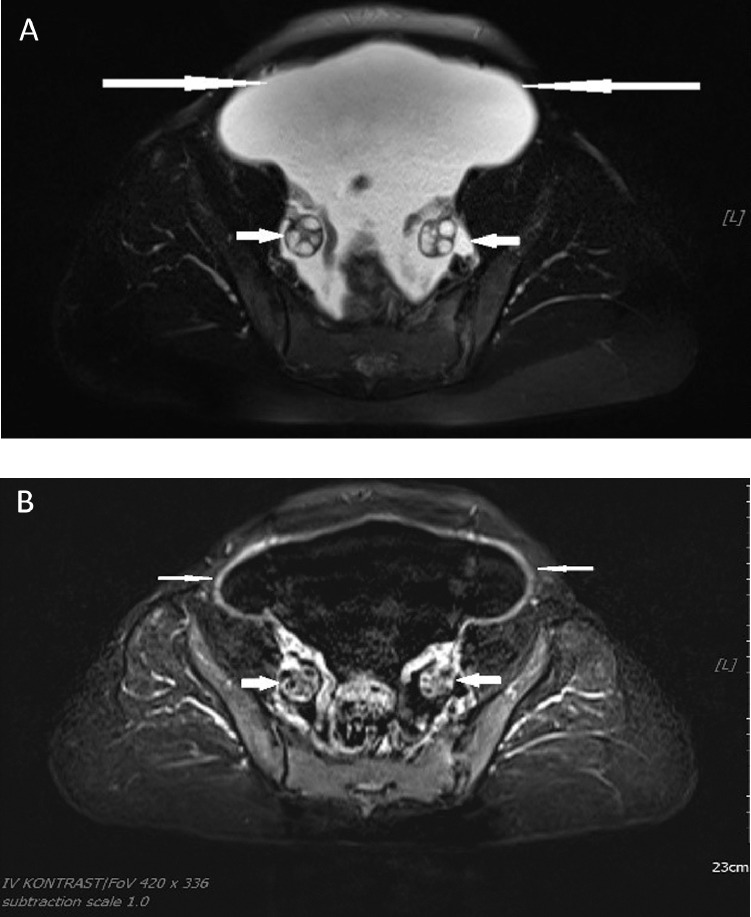
Fig. 2.
Pelvis MRI of the patient showing normal ovaries (thick arrows), diffuse ascites (long arrows), peritoneal smooth thickening, and increased contrast enhancement (thin arrows). MRI, magnetic imaging resonance.
In addition, CT imaging did not reveal any signs of malignancy originating from the stomach, appendix, small intestine and colon that may cause omental cake appearance. No solid/cystic mass was detected on patient's breast ultrasonography. Upper gastrointestinal endoscopy and colonoscopy were within normal limits. When the findings of the patient were evaluated together, tuberculous peritonitis was considered. Chest X-ray showed no abnormality except right-sided pleural effusion (Fig. 3). There were no signs of malignancy in ascites sampling. Total nucleated cells were 594, numbers of monomorphic cells were 526 and number of polymorphic cells was 68 in microliters. Acid-resistant bacilli were not detected by direct microscopy. Quantiferon test was positive. Although tuberculosis peritonitis was thought to be the primary cause of the patient's current clinical status, ultrasound-guided tru-cut biopsies from the omental cakes were performed to exclude the diagnosis of malignancy. Molecular microbiology of the biopsy materials revealed M. tuberculosis DNA.
Fig. 3.
Chest X-ray of the patient showing no abnormality except right-sided pleural effusion.
Microscopic examination of the tru-cut biopsy revealed small-medium-sized granulomatous structures composed of epithelioid histiocytes in omental tissue. Caseous necrosis was seen in the small portion of the granulomas (Fig. 4). No signs of malignancy were observed. Conventional histochemical staining for the etiology of caseified granulomas revealed no infectious agent.
Fig. 4.
Small to medium sized granuloma structures with caseification necrosis (Hematoxylin-Eosin, 200×).
When the imaging findings, molecular microbiology, and histopathologic examination were evaluated together, the diagnosis of tuberculous peritonitis was made and quadruple antituberculosis treatment including isoniazid, rifampicin, pyrazinamide, and ethambutol was started.
Discussion
The use of CT in the evaluation of peritoneal diseases is increasing day by day. The distinction between tuberculous peritonitis and peritoneal carcinomatosis is difficult in some cases because of nonspecific clinical findings and overlapping imaging findings [10,11].
CA-125, which is frequently used as a marker of ovarian cancer, is also elevated in patients with pulmonary and extrapulmonary tuberculosis. This is because CA-125 antigen is a transmembrane glycoprotein found in epithelial tissues such as pericardium, pleura, peritoneum, fallopian tubes and endometrium [12]. The increase in CA-125 level can be observed in ovarian cancer, benign ovarian diseases, and other benign gynecologic diseases as well as other malignancies [13].
The most common CT findings of tuberculous peritonitis include high-density lymphadenopathy, high-density ascites and thickening and/or nodularity of the peritoneal surfaces, mesentery, omentum, and intestinal walls. However, none of these CT findings are pathognomonic for tuberculous peritonitis and may be observed in cases of peritonitis carcinomatosis [14].
The most useful CT finding in the differentiation of tuberculous peritonitis and peritonitis carcinomatosis is the appearance of parietal peritoneum. While smooth minimal thickening and significant enhancement in peritoneum supports tuberculous peritonitis, nodular implants, and irregular peritoneal thickening suggest the diagnosis of peritonitis carcinomatosis [10].
Several studies have been reported as the gold standard in the diagnosis of tuberculous peritonitis [9]. However, it is still difficult to diagnose tuberculous peritonitis in clinical practice. While the diagnosis of pulmonary tuberculosis requires microbiological confirmation, the diagnosis of extra-pulmonary tuberculosis is often based on histopathologic examination [4,9].
In conclusion, tuberculous peritonitis should be in differential diagnosis of a patient with ascites and elevated serum CA-125 levels. Patients with tuberculosis peritonitis may be misdiagnosed as ovarian malignancy and may undergo unnecessary surgery. Although the appearance of omental cake primarily suggests carcinomatosis peritonei due to ovarian cancer, smooth thickening and/or significant enhancement of the peritoneum, and absence of adnexal mass should suggest tuberculous peritonitis. The production of M. tuberculosis bacilli in culture of ascites and acid-resistant staining are often negative thus biopsy specimens should be histologically examined for diagnosis.
Declaration of Competing Interest
None.
References
- 1.Koc S., Beydilli G., Tulunay G., Ocalan R., Boran N., Ozgul N. Peritoneal tuberculosis mimicking advanced ovarian cancer: a retrospective review of 22 cases. Gynecol Oncol. 2006;103:565–569. doi: 10.1016/j.ygyno.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 2.Oge T., Ozalp S.S., Yalcin O.T., Kabukcuoglu S., Kebapci M., Arik D. Peritoneal tuberculosis mimicking ovarian cancer. Eur J Obstet Gynecol Reprod Biol. 2012;162:105–108. doi: 10.1016/j.ejogrb.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 3.Shibata R., Matsufuji H., Morimoto T., Araki A., Hata J. Extraovarian primary peritoneal carcinoma in a child. Pediatr Blood Cancer. 2004;42:292–293. doi: 10.1002/pbc.10236. [DOI] [PubMed] [Google Scholar]
- 4.Protopapas A., Milingos S., Diakomanolis E., Elsheikh A., Protogerou A., Mavrommatis K. Miliary tuberculous peritonitis mimicking advanced ovarian cancer. Gynecol Obstet Invest. 2003;56:89–92. doi: 10.1159/000072919. [DOI] [PubMed] [Google Scholar]
- 5.Straughn J.M., Robertson M.W., Partridge E.E. A patient presenting with a pelvic mass, elevated CA-125, and fever. Gynecol Oncol. 2000;77:471–472. doi: 10.1006/gyno.2000.5756. [DOI] [PubMed] [Google Scholar]
- 6.Wu J.F., Li H.J., Lee P.I., Ni Y.H., Yu S.C., Chang M.H. Tuberulous peritonitis mimicking peritonitis carcinomatosis: a case report. Eur J Pediatr. 2003;162:853–855. doi: 10.1007/s00431-003-1319-3. [DOI] [PubMed] [Google Scholar]
- 7.Mpiura B., Rabinovich A., Leron E., Yanai-Inbar I., Mazor M. Peritoneal tuberculois—an uncommon disease that may deceive the gynecologist. Eur J Gynecol Oncol. 2003;110:230–234. doi: 10.1016/s0301-2115(03)00101-5. [DOI] [PubMed] [Google Scholar]
- 8.Bilgin T., Karabay A., Dolar E., Develioglu O.H. Peritoneal tuberculosis with pelvic abdominal mass, ascites and elevated CA 125 mimicking advanced ovarian carcinoma: a series of 10 cases. Int J Gynecol Cancer. 2001;11:290–294. doi: 10.1046/j.1525-1438.2001.011004290.x. [DOI] [PubMed] [Google Scholar]
- 9.Bayramicli-Uygur O., Dabak G., Dabak R. A clinical dilemma: abdominal tuberculosis. World J Gastroenterol. 2003;9:1098–1101. doi: 10.3748/wjg.v9.i5.1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rodriguez E., Pombo F. Peritoneal tuberculosis versus peritoneal carcinomatosis: distinction based on CT findings. J Comput Assist Tomogr. 1996;20:269–272. doi: 10.1097/00004728-199603000-00018. [DOI] [PubMed] [Google Scholar]
- 11.Ha H.K., Jung J.I., Lee M.S., Choi B.G., Lee M.G., Kim Y.H. CT differentiation of tuberculous peritonitis and peritoneal carcinomatosis. AJR Am J Roentgenol. 1996;167:743–748. doi: 10.2214/ajr.167.3.8751693. [DOI] [PubMed] [Google Scholar]
- 12.Yilmaz A., Ece F., Bayramgürler B., Akkaya E., Baran R. The values of Ca 125 in the evaluation of tuberculosis activity. Respir Med. 2001;95:666–669. doi: 10.1053/rmed.2001.1121. [DOI] [PubMed] [Google Scholar]
- 13.Moss E.L., Hollingworth J., Reynolds T.M. The role of CA 125 in clinical practice. J Clin Pathol. 2005;58:308–312. doi: 10.1136/jcp.2004.018077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barutcu O., Erel H.E. Abdominopelvic tuberculosis simulating disseminated ovarian carcinoma with elevated CA-125 level: report of two cases. Abdom Imag. 2002;27:465–470. doi: 10.1007/s00261-001-0072-1. [DOI] [PubMed] [Google Scholar]