Abstract
Background
Neutrophil to lymphocyte ratio (NLR) was reported to be an independent easy‐to‐measure marker for many diseases, while the distribution of NLR in healthy population was not formally studied. So we investigated NLR in healthy people in this study.
Methods
Data include NLR, systolic pressure, diastolic pressure, and body mass index (BMI), which were collected from 3,262 healthy population. Correlations of NLR with variables were analyzed with SPSS16.0.
Results
Results demonstrated that NLR was positively associated with age (P < 0.001). The eldest age group possessed the highest NLR and the youngest age group had the lowest NLR. NLR was also slightly positively associated with systolic pressure, diastolic pressure, and BMI (P < 0.001).
Conclusion
Older people possessed relatively high NLR in healthy population.
Keywords: clinical parameter, immunity, lymphocyte, neutrophil, NLR
INTRODUCTION
Neutrophils are the main component of human periphery circulation leukocytes, which play a key role in human inflammation and disease defense 1. Neutrophils reach the infection or injury location first, followed by executing programs of phagocytosis, degranulation, and setting neutrophil extracellular traps to eliminate invaders 2. They also secrete chemokines and cytokines to attract monocytes from local area to phagocytes themselves by macrophages and transit signal to activate following adaptive immunity 2, 3. Recently, a subpopulation of neutrophils is also reported to suppress T cells mediated immune response 4. Lymphocytes are another major population of human periphery circulation leukocytes, which mainly mediate adaptive immunity including T lymphocytes mediated cellular immunity and B lymphocytes mediated humoral immunity 5, 6, 7.
With the development of immunity, more and more diseases were reported to be related to the abnormal regulation of immune system 8, 9, 10. The significance of neutrophil to lymphocyte ratio (NLR) was frequently studied because of its easy‐to‐measure characteristics. NLR was not only used as an indicator for acute viral or bacterial infection 11, 12, 13, but was also regarded as an easily measurable marker for system inflammation evaluation in some reports 14, 15. Recently, elevated NLR was reported to be an independent prognostic factor for diabetes, chronic kidney disease, heart failure, hypertension or coronary artery disease 16, 17, 18, 19, 20, 21. High NLR was also reported to be correlated with poor progression of many malignancies such as papillary thyroid carcinomas, soft tissue sarcoma, renal cell carcinoma, colon cancer, nonsmall cell lung cancer, colorectal cancer, and breast cancer et al. 22, 23, 24, 25, 26, 27, 28. As more than half of the above mentioned diseases frequently occurred in older people, we wonder whether NLR elevated in older people basically. No study about the relationship of NLR and age in normal population was reported. So we explored the possible correlation of NLR and age as well as other covariates such as systolic pressure, diastolic pressure, body mass index (BMI) and gender in this study. We found that NLR was positively associated with age, systolic pressure, diastolic pressure and BMI, but not correlated with gender.
Methodology
Ethics statement
This study was approved by the Committee for Ethical Review of Research involving human subjects at the Sun Yat‐Sen Memorial Hospital. As this study was a retrieval study based on routine clinical examination results and the data were analyzed anonymously, informed consent was waived in this study.
Study population
Data of about 3,262 healthy population including 1,568 female and 1,694 male for normal physical examination in the Sun Yat‐Sen Memorial Hospital, Sun Yat‐Sen University from January 2009 to September 2013 were collected and analyzed in this study.
Excluding criteria for healthy population: People with any signs of acute infection, chronic inflammatory disease, known malignancy, hypertension, diabetes mellitus, or any reported abnormal were excluded from this investigation.
Data of about 89 chronic hepatitis B (CHB) inpatients, 94 hepatocellular (HCC) inpatients with hepatitis B virus (HBV) infection, 109 breast cancer inpatients, 94 nodular goiter inpatients, 50 type 2 diabetes inpatients, 105 myocardial infarction (MI) inpatients 69 acute lung bacterial infection inpatients, 81 systemic lupus erythematosus (SLE) inpatients, and 66 rheumatoid arthritis (SA) inpatients in the Sun Yat‐Sen Memorial Hospital, Sun Yat‐Sen University from Jan 2009 to Sep 2013 were also randomly collected. Gender and age mated healthy control were randomly collected from the above healthy population. NLR in different diseases and their respectively mated healthy control were compared and analyzed. Data from another 185 diagnosed hypertension patients for normal physical examination in the Sun Yat‐Sen Memorial Hospital, Sun Yat‐Sen University from January 2009 to September 2013 were also collected and analyzed in this study.
Periphery NLR value calculation
EDTA‐K2 anticoagulation full blood was taken from vein. Then periphery leukocyte, neutrophil, and lymphocyte concentration was performed with standard automated clinical methodologies. The NLR value was calculated as absolute periphery neutrophil concentration divided by absolute periphery lymphocyte concentration.
Covariates
Body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters. Blood pressure was measured at the brachial artery with a hamnatodynamometer when the participant sat.
Statistical analysis
All statistical analyses were performed with SPSS version 16.0 with two‐tailed tests, and significance was defined as P values less than 0.05. Continuous variables were compared with one‐way ANOVA or independent Student's t‐test expressed in the report of mean ± standard deviation (S.D.). Correlations between variables were determined by linear regression analysis.
RESULTS
NLR Positively Correlated with Age in Healthy Population
A total of 3,262 healthy population was analyzed in this study, which included 1568 female and 1,694 male. Correlation between NLR and age was first determined by linear regression analysis. The result demonstrated that NLR was positively associated with age, the older the age, the higher the NLR (r = 0.161, P < 0.001, Pearson Correlation) (Fig. 1). Further, we stratified by analyzing the relation between NLR and age in female or male population. The results revealed that NLR correlated positively to age both in female and male population (r = 0.119, P < 0.001 for female, r = 0.200, P < 0.001 for male, Pearson Correlation) (Fig. 1).
Figure 1.
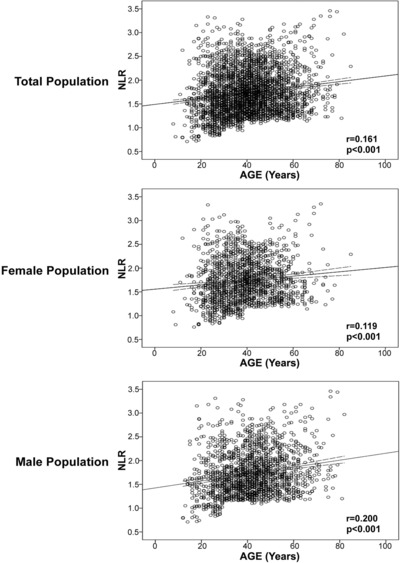
NLR correlated with age positively in healthy population. The correlation of NLR and age was analyzed with Pearson Correlation.
No Significantly Different NLR Between Female and Male in Healthy Population
As gender was reported to play different roles in different clinical parameters, we followed by analyzing the influence of gender on NRL. Seven age groups were characterized according to age (years) as well as gender, and named as <20, which included the population of less than 20 years old; 20–29, which included the population that aged between 20 years old and 29 years old, so on, 30–39, 40–49, 50–59, and 60–69; and the ≥70 group, which included the population of equal to or more than 70 years old. Then NLR at different groups between female and corresponding male was compared with Student's t‐test. Results demonstrated that no significantly different NLR was found between female and male population at each age group (Table 1).
Table 1.
Comparing of the NLR at Different Age Groups Between Female and Male
| Number | Average Age (Years) | NLR (Mean ± S.D.) | ||||||
|---|---|---|---|---|---|---|---|---|
| Group | F | M | F | M | P value* | F | M | P value* |
| <20 | 37 | 61 | 16.4 | 16.9 | 0.408 | 1.54 ± 0.54 | 1.52 ± 0.58 | 0.814 |
| 20–29 | 309 | 241 | 25.3 | 25.6 | 0.215 | 1.63 ± 0.49 | 1.61 ± 0.51 | 0.712 |
| 30–39 | 503 | 416 | 34.7 | 34.7 | 0.714 | 1.74 ± 0.47 | 1.69 ± 0.41 | 0.053 |
| 40–49 | 423 | 548 | 43.7 | 44.2 | 0.017 | 1.79 ± 0.35 | 1.76 ± 0.43 | 0.164 |
| 50–59 | 216 | 277 | 54.0 | 53.9 | 0.662 | 1.76 ± 0.42 | 1.80 ± 0.44 | 0.977 |
| 60–69 | 67 | 118 | 63.4 | 63.5 | 0.803 | 1.78 ± 0.54 | 1.86 ± 0.50 | 0.284 |
| > = 70 | 13 | 33 | 74.5 | 74.2 | 0.748 | 1.85 ± 0.58 | 2.05 ± 0.61 | 0.173 |
F, female; M, male. *, analyzed with SPSS16.0 by T test.
Older Healthy Population Had Higher NLR
As gender did not influence NLR, we combined female and male population at the same age phase and calculated their respective NLRs. Differences among these groups were analyzed with one‐way ANOVA and the result demonstrates that older age group tends to possess higher NLR than that in younger groups (P < 0.05). The ≥ 70 age group had the highest NLR and the <20 age group possessed the lowest NLR (Table 2). NLR in any two groups was significantly different (P < 0.05) except among the groups with the age range from 40 years old to 69 years old, when compared with Post Hoc multiple comparisons Student's t‐test.
Table 2.
Comparing of the NLR Among Different Age Groups
| Number | ||||||
|---|---|---|---|---|---|---|
| Group | Total | Female (%) | Male (%) | Average Age (Years) | NLR (mean ± S.D.) | P value |
| <20 | 98 | 37.8 | 62.2 | 16.7 | 1.53 ± 0.56 | |
| 20–29 | 550 | 56.2 | 43.8 | 25.4 | 1.62 ± 0.50 | |
| 30–39 | 919 | 54.7 | 45.3 | 34.7 | 1.72 ± 0.44 | |
| 40–49 | 971 | 43.6 | 56.4 | 44.0 | 1.77 ± 0.40 | |
| 50–59 | 493 | 43.8 | 56.2 | 53.9 | 1.78 ± 0.43 | |
| 60–69 | 185 | 36.2 | 63.8 | 63.5 | 1.83 ± 0.52 | |
| > = 70 | 46 | 28.3 | 71.7 | 74.3 | 1.99 ± 0.60 | |
| Between groupsa | <0.001 | |||||
analyzed with SPSS 16.0 by ANOVA.
NLR Positively Correlated with Systolic Pressure, Diastolic Pressure, and BMI in Healthy Population
The previous results revealed that NLR positively correlated with age. We kept on analyzing the relation between NLR and other covariates with linear regression analysis in the whole population. The results demonstrated that NLR also positively correlated with systolic pressure (r = 0.092, P < 0.001, Pearson Correlation), diastolic pressure (r = 0.089, P < 0.001, Pearson Correlation) and BMI (r = 0.043, P = 0.015, Pearson Correlation) (Fig. 2). Correlations of age with systolic pressure, diastolic pressure, and BMI were also analyzed. Results demonstrated that age positively correlated with systolic pressure (r = 0.359, P < 0.001 Pearson Correlation), diastolic pressure (r = 0.280, P < 0.001, Pearson Correlation), and BMI (r = 0.257, P = 0.015, Pearson Correlation; Fig. 3) also.
Figure 2.
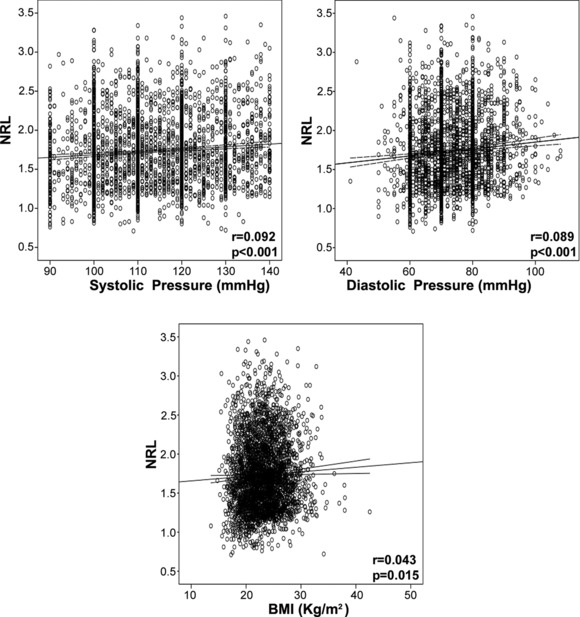
NLR positively correlated with systolic pressure, diastolic pressure and BMI in healthy population. Correlation of NLR with systolic pressure, diastolic pressure, and BMI was analyzed with Pearson Correlation.
Figure 3.
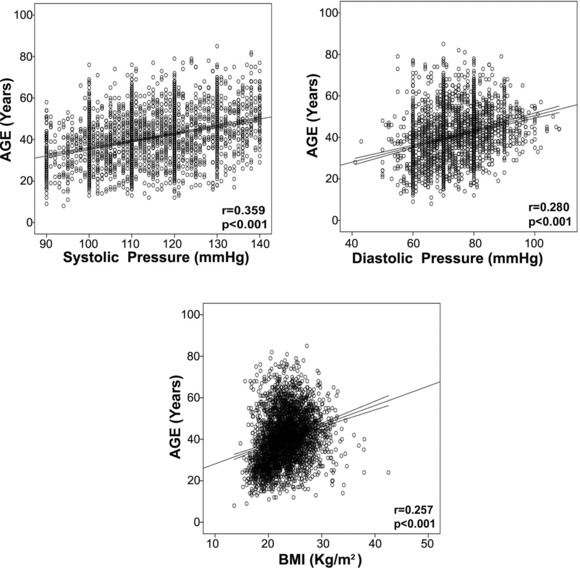
Age positively correlated with systolic pressure, diastolic pressure, and BMI in healthy population. Correlation of age with systolic pressure, diastolic pressure, and BMI was analyzed with Pearson Correlation.
NLR in Different Diseases
Further, we compared NLR in CHB, HCC with HBV infection, breast cancer, nodular goiter, type 2 diabetes, MI, acute lung bacterial infection, SLE, and SA inpatients with their respectively gender and age mated healthy control. The results demonstrated that all the analyzed patients possessed significantly higher NLR than that in healthy control (Fig. 4).
Figure 4.
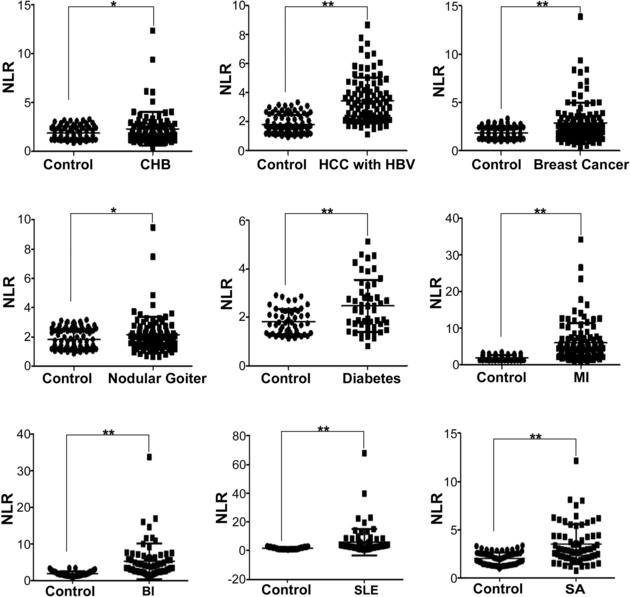
NLR in different diseases. NLR in different diseases and their mated control were analyzed with independent Student's t‐test. BI, acute lung bacterial infection.*, P <0.05; **, P < 0.01.
NLR Did Not Correlated with age in Hypertension Patients
To explore whether age and NLR was correlated in disease status, we compared their correlation in 185 diagnosed hypertension patients. The result demonstrated that age and NLR did not significantly correlated in hypertension patients (Fig. 5).
Figure 5.
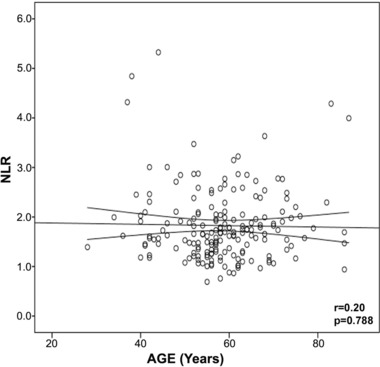
NLR and age did not significantly correlate in hypertension patients. The correlation of NLR and age was analyzed with Pearson Correlation in 185 hypertension patients.
DISCUSSION
One of the most important goals for medical research is to find convenient method or ways for disease detection, monitoring, and therapy. NLR was an easy‐to‐measure marker on clinic, and it has been reported to be related to prognosis or therapy indication for many chronic diseases and malignancies 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28. NLR would benefit greatly to patients if these results could apply to clinic after verification. However, two aspects of NLR must be resolved before it could be popularly applied to clinic. One is the clinical evaluation by the most popular patients, and the other is the basic or physical value of NLR.
However, no formal investigation was reported about the physical value of NLR, so we investigated the possible correlation of NLR distribution in healthy population in this investigation. We found that NLR positively correlated to age both in female and in male. This was logically consistent with the report that granulocytes count showed upward trend with age and lymphocyte count showed declining trend with age in another study 29. Actually, we also observed the declining trend of lymphocytes with age increase in our cohort, while we did not obtain the significance difference among these age groups as to neutrophils count (data not shown).
The observation that NLR increased positively with age might be able to explain some of the phenomena we observed in clinic, such as the phenomena that chronic infection disease and malignance developed more frequently in older people. In this investigation, we found that NLR was increased in older people. Circulating neutrophil could not only defend exotic invasion and induce inflammation, a subpopulation of which could also suppress the immune function of certain immune cytotoxic cells such as T cells 4. Circulating lymphocytes were the major immune cells that were on the surveillance of cancer development 30. So in another way, the increase of NLR in older population did not benefit the defense against malignancy, which might be one of the possible reasons that malignancy developed more frequently in the elders. Of course, we could not ignore the possibility that older people had more chance to acquire gene mutation and more environment influence on tumorigenesis.
We also found that NLR was positively associated with systolic pressure and diastolic pressure in the investigation, which was in accord with the investigation that nebivolol could decrease the blood pressure as well as NLR in a study 31. As hypertension had more possibility to induce cardiovascular disease, the positive association of NLR and systolic pressure as well as diastolic pressure might partly explain why reports about higher NLR was correlated with poor prognosis in many cardiovascular diseases 18, 20, 21. NLR was also positively associated with BMI in this investigation, which agreed with the report that decreased BMI associated with decreased NLR after gastric banding surgery 32.
Grant number: S2013010014007 (to Chaohui Duan); Grant sponsor: Province Natural Science Foundation of Guangdong, China; Grant number: 2010B030700007 (to Chaohui Duan); Grant sponsor: Province Science and Technology Project Plan and Social Development of Guangdong, China.
REFERENCES
- 1. Nathan C. Neutrophils and immunity: challenges and opportunities. Nat Rev Immunol 2006;6:173–182. [DOI] [PubMed] [Google Scholar]
- 2. Amulic B, Cazalet C, Hayes GL, Metzler KD, Zychlinsky A. Neutrophil function: from mechanisms to disease. Annu Rev Immunol 2012;30:459–489. [DOI] [PubMed] [Google Scholar]
- 3. Kolaczkowska E, Kubes P. Neutrophil recruitment and function in health and inflammation. Nat Rev Immunol 2013;13:159–175. [DOI] [PubMed] [Google Scholar]
- 4. Pillay J, Kamp VM, van Hoffen E, et al. A subset of neutrophils in human systemic inflammation inhibits T cell responses through Mac‐1. J Clin Invest 2012;122:327–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rich SS, Rich RR. Regulatory mechanisms in cell‐mediated immune responses. I. Regulation of mixed lymphocyte reactions by alloantigen‐activated thymus‐derived lymphocytes. J Exp Med 1974;140:1588–1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Finkelman FD, Mond JJ, Woods VL, et al. Effects of anti‐immunoglobulin antibodies on murine B lymphocytes and humoral immune responses. Immunol Rev 1980;52:55–74. [DOI] [PubMed] [Google Scholar]
- 7. Raff MC. T and B lymphocytes and immune responses. Nature 1973;242:19–23. [DOI] [PubMed] [Google Scholar]
- 8. Dimitrov JD, Planchais C, Roumenina LT, et al. Antibody polyreactivity in health and disease: statu variabilis. J Immunol 2013;191:993–999. [DOI] [PubMed] [Google Scholar]
- 9. Sonnenberg GF, Artis D. Innate lymphoid cell interactions with microbiota: implications for intestinal health and disease. Immunity 2012;37:601–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Goldszmid RS, Trinchieri G. The price of immunity. Nat Immunol 2012;13:932–938. [DOI] [PubMed] [Google Scholar]
- 11. Dolin R, Reichman RC, Fauci A S. Lymphocyte populations in acute viral gastroenteritis. Infect Immun 1976;14:422–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Marsh JC, Boggs DR, Cartwright GE, Wintrobe MM. Neutrophil kinetics in acute infection. J Clin Invest 1967;46:1943–1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Markar SR, Karthikesalingam A, Falzon A, Kan Y. The diagnostic value of neutrophil: lymphocyte ratio in adults with suspected acute appendicitis. Acta Chir Belg 2010;110:543–547. [PubMed] [Google Scholar]
- 14. Guthrie GJ, Charles KA, Roxburgh CS, Horgan PG, McMillan DC, Clarke SJ. The systemic inflammation‐based neutrophil‐lymphocyte ratio: experience in patients with cancer. Crit Rev Oncol Hematol 2013;88:218–230. [DOI] [PubMed] [Google Scholar]
- 15. Imtiaz F, Shafique K, Mirza SS, Ayoob Z, Vart P, Rao S. Neutrophil lymphocyte ratio as a measure of systemic inflammation in prevalent chronic diseases in Asian population. Int Arch Med 2012;5:2:s1–s6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ulu SM, Dogan M, Ahsen A, et al. Neutrophil‐to‐Lymphocyte Ratio as a Quick and Reliable Predictive Marker to Diagnose the Severity of Diabetic Retinopathy. Diabetes Technol Ther 2013;15:942–947. [DOI] [PubMed] [Google Scholar]
- 17. Solak Y, Yilmaz MI, Sonmez A, et al. Neutrophil to lymphocyte ratio independently predicts cardiovascular events in patients with chronic kidney disease. Clin Exp Nephrol 2013;17:532–540. [DOI] [PubMed] [Google Scholar]
- 18. Uthamalingam S, Patvardhan EA, Subramanian S, et al. Utility of the neutrophil to lymphocyte ratio in predicting long‐term outcomes in acute decompensated heart failure. Am J Cardiol 2011;107:433–438. [DOI] [PubMed] [Google Scholar]
- 19. Demir M. The Relationship Between Neutrophil Lymphocyte Ratio and Non‐dipper Hypertension. Clin Exp Hypertens 2013;35:570–573. [DOI] [PubMed] [Google Scholar]
- 20. Arbel Y, Finkelstein A, Halkin A, et al. Neutrophil/lymphocyte ratio is related to the severity of coronary artery disease and clinical outcome in patients undergoing angiography. Atherosclerosis 2012;225:456–460. [DOI] [PubMed] [Google Scholar]
- 21. Sahin DY, Elbasan Z, Gur M, Yildiz A, Akpinar O, Icen YK, Turkoglu C, Tekin K, Kuloglu O, Cayli M. Neutrophil to lymphocyte ratio is associated with the severity of coronary artery disease in patients with ST‐segment elevation myocardial infarction. Angiology 2013;64:423–429. [DOI] [PubMed] [Google Scholar]
- 22. Kim JY, Park T, Jeong SH, et al. Prognostic importance of baseline neutrophil to lymphocyte ratio in patients with advanced papillary thyroid carcinomas. Endocrine 2013. doi: 10.1007/s12020-013-0089-6 [DOI] [PubMed] [Google Scholar]
- 23. Szkandera J, Absenger G, Liegl‐Atzwanger B, et al. Elevated preoperative neutrophil/lymphocyte ratio is associated with poor prognosis in soft‐tissue sarcoma patients. Br J Cancer 2013;108:1677–1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ohno Y, Nakashima J, Ohori M, Hatano T, Tachibana M. Pretreatment neutrophil‐to‐lymphocyte ratio as an independent predictor of recurrence in patients with nonmetastatic renal cell carcinoma. J Urol 2010;184:873–878. [DOI] [PubMed] [Google Scholar]
- 25. Absenger G, Szkandera J, Stotz M, et al. Preoperative Neutrophil‐to‐Lymphocyte Ratio Predicts Clinical Outcome in Patients with Stage II and III Colon Cancer. Anticancer Res 2013;33:4591–4594. [PubMed] [Google Scholar]
- 26. Sarraf KM, Belcher E, Raevsky E, Nicholson AG, Goldstraw P, Lim E. Neutrophil/lymphocyte ratio and its association with survival after complete resection in non‐small cell lung cancer. J Thorac Cardiovasc Surg 2009;137:425–428. [DOI] [PubMed] [Google Scholar]
- 27. Walsh SR, Cook EJ, Goulder F, Justin TA, Keeling NJ. Neutrophil‐lymphocyte ratio as a prognostic factor in colorectal cancer. J Surg Oncol 2005;91:181–184. [DOI] [PubMed] [Google Scholar]
- 28. Noh H, Eomm M, Han A. Usefulness of pretreatment neutrophil to lymphocyte ratio in predicting disease‐specific survival in breast cancer patients. J Breast Cancer 2013;16:55–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ruggiero C, Metter EJ, Cherubini A, et al. White blood cell count and mortality in the Baltimore Longitudinal Study of Aging. J Am Coll Cardiol 2007;49:1841–1850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hamai A, Benlalam H, Meslin F, et al. Immune surveillance of human cancer: if the cytotoxic T‐lymphocytes play the music, does the tumoral system call the tune? Tissue Antigens 2010;75:1–8. [DOI] [PubMed] [Google Scholar]
- 31. Fici F, Celik T, Balta S, et al. Comparative effects of nebivolol and metoprolol on red cell distribution width and neutrophil/lymphocyte ratio in patients with newly diagnosed essential hypertension. J Cardiovasc Pharmacol 2013;62;388–393. [DOI] [PubMed] [Google Scholar]
- 32. Santos J, Salgado P, Santos C, et al. Effect of Bariatric Surgery on Weight Loss, Inflammation, Iron Metabolism, and Lipid Profile. Scand J Surg 2014;103:21–25. doi: 10.1177/1457496913490467 [DOI] [PubMed] [Google Scholar]


