Abstract
Objective
Infection with the bacterial pathogen Helicobacter pylori (HP) clearly results in chronic mucosal inflammation in the stomach and duodenum, which, in turn, might lead to abnormalities in gastroduodenal motility and sensitivity and is the most frequent cause of dyspepsia and peptic disease. Some studies have shown that there was a correlation between low‐grade inflammation as C‐reactive protein (CRP) and HP infection. The aim of this study was to investigate the relationship between the presence of gastritis due to HP infection and neutrophil/lymphocyte ratio (NLR), a simple and reliable indicator of inflammation.
Design
Fifty patients met the HP criteria and half of them have had severe symptoms and upper endoscopy showed atrophic gastritis, and fifty age‐ and sex‐matched control subjects with gastritis without HP infection were included in this randomized controlled trial. Patients were diagnosed to have HP according to the use of urea breath testing (UBT) and multiple biopsies. NLR was calculated from complete blood count at the time of diagnosis and before initiating the treatment to all groups.
Results
Patients with HP infection had significantly higher NLR compared to those without HP. Moreover, the patients with symptomatic HP and grade 4 gastritis had higher NLR than those asymptomatic with past history of peptic disease (P 0.007 and P 0.068, respectively). Although NLR increased as the severity of gastritis and HP symptoms increased (r = 0.564, P < 0.001), Receiver operating characteristic (ROC) Curve analysis was performed. The cut‐off level for NLR with optimal sensitivity and specificity was calculated as 1.82 (area under curve [AUC] = 0.825 [0.753–0.884], P < 0.001).
Conclusion
The present study indicated, for the first time, a significant correlation between HP infection and inflammation on the basis of NLR, a simple and reliable indicator of inflammation. Furthermore, there is an increase in NLR as the severity of gastritis with HP increases. This elevated ratio gets normalized with treatment.
Keywords: Helicobacter pylori, neutrophil/lymphocyte ratio, inflammation, peptic disease
INTRODUCTION
Helicobacter pylori (HP) is the most common chronic bacterial infection in humans 1, 2. Studies involving genetic sequence analysis suggest that humans have been infected with HP since they first migrated from Africa around 58,000 years ago 3. HP has been demonstrated worldwide and in individuals of all ages. HP is a common cause of gastric and duodenal ulcers. Conservative estimates suggest that 50% of the world's population is affected. Infection is more frequent and acquired at an earlier age in developing countries compared with industrialized nations 2. Once acquired, infection persists and may or may not produce gastroduodenal disease. The route by which infection occurs remains unknown 1, 4. Person‐to‐person transmission of HP through either fecal/oral or oral/oral exposure seems most likely 4, 5. Diagnostic testing for HP can be divided into invasive and noninvasive techniques based upon the need for endoscopy. Recommendations for diagnostic testing for HP were first proposed by the National Institutes of Health (NIH) in 1994 6. More recent guidelines were published in 2006 by the European Helicobacter Study Group (EHSG) 7 and in 2007 by the American College of Gastroenterology (ACG) 8.
Few studies have shown that there was a correlation between inflammatory mediators and the presence of HP infection. Particularly, C‐reactive protein (CRP) levels were observed to be increased in HP 9. Leukocyte activation occurs during an inflammatory reaction. Leukocytes were detected to have a role in several chronic diseases such as diabetes, hypertension, atherogenesis, and thrombus formation, and other inflammatory disorders. Along with high number of leukocytes, there is a significant relationship between neutrophil/lymphocyte ratio (NLR) and severity and prognosis of cardiovascular disease (CVD) 10. The association with NLR and helicobacter pylori has never been observed before. This study was the first to detect a relationship between HP and NLR, a simple and reliable indicator of inflammation.
PATIENTS AND METHODS
Fifty patients, who had been diagnosed to have HP infection in the outpatient clinic according to established criteria for suspected HP infection, were recruited for the study. Fifty age‐ and sex‐matched subjects with gastritis without HP infection were recruited as the control group. Patients with uncontrolled hypertension, uncontrolled diabetes, renal failure, hepatic failure, and/or manifested heart disease, such as cardiac failure, coronary arterial disease, arrhythmia, and cardiac valve disease, were excluded. Similarly, patients with infection, acute stress, chronic systemic inflammatory disease, upper or lower gastrointestinal bleeding, and those who had been receiving medications affecting the number of leukocytes were excluded, as well. All the participants included in the study were informed about the study, and their oral and written consents on participating voluntarily were obtained.
HP was diagnosed according to the National Institutes of Health (NIH) in 1994 6. More recent guidelines were published in 2006 by the European Helicobacter Study Group (EHSG) 7 and in 2007 by the American College of Gastroenterology (ACG) 8.
All patients were diagnosed as having HP infection according to the use of urea breath testing (UBT) that is based upon the hydrolysis of urea by HP to produce CO2 and ammonia using the nonradioactive 13C test (Meretek, Otsuka Pharmaceuticals), A labeled carbon isotope is given by mouth; HP liberate tagged CO2 that can be detected in breath samples with sensitivity and specificity are approximately 88–95% and 95–100%, respectively. The control group had negative results. All patients’ group with positive and negative HP (100) have undergone an upper endoscopy and multiple biopsies were obtained from both the angularis incisura and the antral mucosa to confirm the diagnosis, and those with positive HP were divided in two groups of 25 each according to gastritis staging on the basis of OLGA proposal 11 and clinical symptoms, the group with nonatrophic gastritis stage I–II were asymptomatic. Only 30% have few symptoms as dyspeptic complaints, the second symptomatic group (epigastric pain, nausea, and vomiting) and positive HP have atrophic antral gastritis 80% and 20% antral and corpus gastritis stage III–IV.
Plasma glucose, urea, creatinine, total cholesterol, TG, HDL, and LDL levels were measured in the venous blood samples obtained in the morning after 8‐hr fasting. Complete blood count was studied in our hematology unit with Beckman‐Coulter Gen‐S system device (Beckman‐Coulter, USA).
Statistical Analysis
Continuous variables were defined as mean ± standard deviation, and categorical variables were given as percentages. Independent sample t‐test or Mann–Whitney U test were used for continuous variables, and chi‐square test for categorical variables. Statistical analyses were performed using Statistical Package for Social Sciences (SPSS) Version 15.0 (SPSS, Chicago, IL, USA). Any P value <0.05 was considered as statistically significant.
RESULTS
Totally, 50 patients with HP and 50 age‐ and sex‐matched subjects with gastritis without HP infection were included in the study as patient and control groups, respectively. Clinical and vital signs characteristics of both groups are summarized in Table 1. As shown in Table 2, while numbers of white blood cells (WBCs), neutrophils, and lymphocytes in the patients with HP were higher than those without HP. Platelet counts and hemoglobin levels were comparable. Patients with HP had significantly higher NLR compared to those without HP. Furthermore, NLR increased more as severity of gastritis with HP and symptoms increased (Fig. 1). In subjects without HP, NLR was detected to be significantly lower compared to those with gastritis grade I and II and asymptomatic HP and symptomatic gastritis grade III and IV (2.854, 4.048, 5.086, respectively, P < 0.001) (Fig. 1). The elevated NLR normalized after successful treatment and eradication of HP infection established according to the use of UBT only and clinical symptoms, detected two weeks after initiating therapy (P < 0.001).
Table 1.
Differences Between Various Parameters of the Groups With and Without HP
| HP (−) | HP (+) | P value | |
|---|---|---|---|
| Age (years) | 48 ± 12 | 49 ± 10 | 0.440 |
| Sex (male %) | 54 | 52 | 0.469 |
| SBP (mmHg) | 129 ± 19 | 135 ± 18 | 0.079 |
| DBP (mmHg) | 82 ± 11 | 85 ± 10 | 0.031 |
HP: Helicobacter pylori; DBP, diastolic blood pressure; SBP, systolic blood pressure.
Table 2.
Differences Between the Hematologic Parameters of the Groups With and Without HP
| HP (−) | HP (+) | P value | |
|---|---|---|---|
| Hemoglobin (g/dl) | 13.5 ± 0.54 | 13.4 ± 0.52 | 0.805 |
| Platelet count (×1,000) | 294 ± 54 | 276 ± 72 | 0.212 |
| WBC | 8,528 ± 984 | 9,930 ± 1,413 | <0.001 |
| Neutrophil count | 6,039 ± 868 | 8,205 ± 1,162 | <0.001 |
| Lymphocyte count | 2,313 ± 577 | 1,610 ± 520 | <0.001 |
| NLR | 2.853 ± 0.72 | 5.086 ± 0.83 | <0.001 |
HP: Helicobacter pylori; NLR, neutrophil/lymphocyte ratio; WBC; white blood cells.
Figure 1.
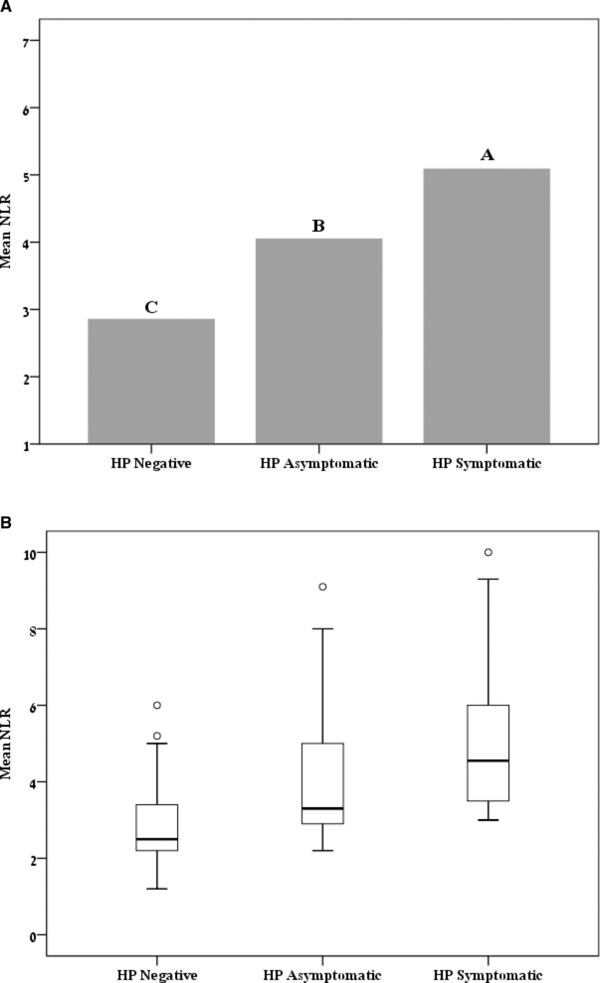
NLR in the three study groups, compared to HP(−) and HP(+) asymptomatic gastritis I–IV grade group.
Note. Different subscripts above the bars represent significant differences between groups (P < .001).
The cut‐off level for NLR with optimal sensitivity and specificity was calculated as 1.84 (area under curve [AUC] = 0.825 [0.753–0.884], P < 0.001). For that level, sensitivity was 92.8% (84.1–97.6%), and specificity was 61.9% (49.7–73.2%), positive predictive value was 70.7 (60.2–79.7), and negative predictive value was 89.8 (77.6–98.7).
DISCUSSION
The present study indicated, for the first time, a significant correlation between HP infection and inflammation on the basis of NLR, a simple and reliable indicator of inflammation. Furthermore, the correlation between the increases in the number of NLR associated with HP infection has been reported, for the first time, to our knowledge. HP is a common cause of gastric and duodenal ulcers. About 50% of the world's population is affected. Usually infection is more frequent and acquired at an earlier age in developing countries compared with industrialized nations 1. Once acquired, infection persists may produce gastroduodenal disease. In fact, HP causes more than 90% of duodenal ulcers and more than 80% of stomach ulcers 12. HP also causes gastritis, an inflammation of the stomach lining, which can lead to chronic inflammation or loss of function of the cells (atrophic gastritis). Furthermore, individuals with this infection have a —two‐ to six‐folds increased risk of developing mucosa‐associated lymphoid tissue lymphoma and stomach cancer compared to uninfected individuals 13.
Despite the fact that HP mainly infects the stomach, it has been shown to play a role in the development of numerous nongastrointestinal diseases. Researchers suggest that HP induces systemic inflammation and decreases the absorption of nutrients, thereby increasing the risk of several diseases. Some of the conditions associated with HP infection include CVD, stroke, anemia, glaucoma, Alzheimer's disease, rosacea, eczema, chronic hives, diabetes, thyroid disease, and idiopathic thrombocytopenic purpura 14. Eradication treatment of HP can improve numerous conditions, and natural strategies exist to help eradicate this harmful organism.
One study found that eradication treatment of HP increased high‐density lipoprotein (HDL) cholesterol, and decreased the inflammatory markers C‐reactive protein (CRP) and fibrinogen, which are associated with atherosclerosis and CVD risk 15. Research has shown that the presence of HP antibodies were significantly more frequent in individuals with coronary artery disease (CAD) compared to healthy control subjects. In fact, the presence of antibodies was nearly double in the subjects with CAD compared to the control group, which also correlated to increased CRP levels 9. Similarly, another study showed that HP infection was related to increased arterial stiffness and increased systolic blood pressure in diabetic subjects 16.
Our study is the first to detect an association between HP and other available and simple inflammatory markers to control disease activity. This marker (NLR) can differentiate between symptomatic and asymptomatic patients therefore help us deciding who need therapy. NLR is infrequently practical, despite the simplicity of the test and availability that can be useful in various inflammatory diseases.
Previous studies have shown that WBC, leukocyte subtype, and NLR were indicators of systemic inflammation 17. Number of neutrophils is considered to be associated with formation, complexity, and activation of atheromatous plaque 18. Consistent with the literature, the present study showed that the number of neutrophils increased in HP; moreover, the number of neutrophils increased as symptoms of HP increased. The variation in the increased rate of number of lymphocytes was insignificant between the HP subjects and those without HP. That was considered to be consistent with more increase in the number of neutrophils compared to that of lymphocytes and hence increase in NLR in the conditions associated with inflammation. In a previous study, NLR was shown to be a predictor in the progression of atherosclerosis 19, 20. The study by Horne et al. found a significant association among the severity and prognosis of CVD, high WBC and NLR 10. The present study showed that NLR was strongly correlated with the presence of HP and severity of symptoms of HP infection. However, associations between NLR and HP have still yet to be investigated. NLR, a promising marker of inflammation starting to find a place in the literature, was found to be correlated with the presence and the severity of HP infection and can be useful to follow up patients after successful therapy.
CONCLUSION
It is known that systemic inflammation is involved in various chronic diseases and sometimes can be considered a major risk for development of CVD. The present study is the first report about the association of NLR with the presence of HP as chronic inflammatory disease. The results may have clinical importance, because this marker can be useful for detecting HP infection and severity, deciding about treatment time and follow‐up to ensure eradication of HP. Persestent infection with HP may be the early marker of development of cardiovascular events, we need future studies with more samples to test this marker after successful long‐term therapy.
Limitations
The most important limitation of the present study was the number of the patients included in addition to the absence of long‐term follow‐up period after treatment to check the response of therapy and variation of this marker over time.
CONFLICT OF INTEREST
None.
ETHICS APPROVAL
The study protocol was approved by signing an informed consent for blood sampling approved by the institutional committee in accordance with the Helsinki declaration.
REFERENCES
- 1. Cave DR. Transmission and epidemiology of Helicobacter pylori . Am J Med 1996;100(5A):12S–17S. [DOI] [PubMed] [Google Scholar]
- 2. Pounder RE, Ng D. The prevalence of Helicobacter pylori infection in different countries. Aliment Pharmacol Ther 1995;9(Suppl 2):33–39. [PubMed] [Google Scholar]
- 3. Linz, B , Balloux F, Moodley Y, et al. An African origin for the intimate association between humans and Helicobacter pylori . Nature 2007;445(7130):915–918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Megraud F. Transmission of Helicobacter pylori: Faecal‐oral versus oral‐oral route. Aliment Pharmacol Ther 1995;9(Suppl 2):85–91. [PubMed] [Google Scholar]
- 5. Perry S, de la Luz Sanchez M, Yang S, et al. Gastroenteritis and transmission of Helicobacter pylori infection in households. Emerg Infect Dis 2006;12(11):1701–1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. NIH Consensus Conference . Helicobacter pylori in peptic ulcer disease. NIH consensus development panel on Helicobacter pylori in peptic ulcer disease. JAMA 1994;272(1):65–69. [PubMed] [Google Scholar]
- 7. Malfertheiner P, Megraud F, O'Morain C, et al. Current concepts in the management of Helicobacter pylori infection: The Maastricht III Consensus Report. Gut 2007;56(6):772–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chey WD, Wong BC. American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Am J Gastroenterol 2007;102(8):1808–1825. [DOI] [PubMed] [Google Scholar]
- 9. Jha HC, Prasad J, Mittal A. High immunoglobulin A seropositivity for combined Chlamydia pneumoniae, Helicobacter pylori infection, and high‐sensitivity C‐reactive protein in coronary artery disease patients in India can serve as atherosclerotic marker. Heart Vessels 2008;23(6):390–396. [DOI] [PubMed] [Google Scholar]
- 10. Horne BD, Anderson JL, John JM, et al. Which white blood cell subtypes predict increased cardiovascular risk? J Am Coll Cardiol 2005;45(10):1638–1643. [DOI] [PubMed] [Google Scholar]
- 11. Rugge M, Meggio A, Pennelli G, et al. Gastritis staging in clinical practice: The OLGA staging system. Gut 2007;56(5):631–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Centers for Disease Control and Prevention . Helicobacter pylori 2010. Available from: http://www.cdc.gov/ncidod/aip/research/hp.html.
- 13. Centers for Disease Control and Prevention . Helicobacter pylori and Peptic Ulcer Disease 2010. Available from: http://www.cdc.gov/ulcer/keytocure.htm#illnesses.
- 14. Szlachcic A. The link between Helicobacter pylori infection and rosacea. J Eur Acad Dermatol Venereol 2002;16(4):328–333. [DOI] [PubMed] [Google Scholar]
- 15. Pellicano R, Oliaro E, Fagoonee S, et al. Clinical and biochemical parameters related to cardiovascular disease after Helicobacter pylori eradication. Int Angiol 2009;28(6):469–473. [PubMed] [Google Scholar]
- 16. Ohnishi M, Fukui M, Ishikawa T, et al. Helicobacter pylori infection and arterial stiffness in patients with type 2 diabetes mellitus. Metabolism 2008;57(12):1760–1764. [DOI] [PubMed] [Google Scholar]
- 17. Papa A, Emdin M, Passino C, Michelassi C, Battaglia D, Cocci F. Predictive value of elevated neutrophil‐lymphocyte ratio on cardiac mortality in patients with stable coronary artery disease. Clin Chim Acta 2008;395(1–2):27–31. [DOI] [PubMed] [Google Scholar]
- 18. Avanzas P, Arroyo‐Espliguero R, Cosín‐Sales J, et al. Markers of inflammation and multiple complex stenoses (pancoronary plaque vulnerability) in patients with non‐ST segment elevation acute coronary syndromes. Heart 2004;90(8):847–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kalay N, Dogdu O, Koc F, et al. Hematologic parameters and angiographic progression of coronary atherosclerosis. Angiology 2012;63(3):213–217. [DOI] [PubMed] [Google Scholar]
- 20. Pasceri V, Cammarota G, Patti G, et al. Association of virulent Helicobacter pylori strains with ischemic heart disease. Circulation 1998;97(17):1675–1679. [DOI] [PubMed] [Google Scholar]


