Abstract
Background
Neutrophil gelatinase associated lipocalin (NGAL) is proposed as a biomarker of acute kidney injury (AKI). NGAL has been studied in a range of body fluids including serum and EDTA plasma. The aim of the present study was to establish relationship between serum NGAL concentrations and EDTA plasma NGAL concentrations in patients admitted to intensive care units (ICUs) and whether these determinations are directly comparable in this setting.
Methods
NGAL was measured in 40 paired samples of serum and EDTA plasma from 25 patients admitted to intensive care with a commercial particle‐enhanced turbidimetric immunoassay (The NGAL Test™, BioPorto Diagnostics A/S, Gentofte, Denmark) on a Roche Hitachi 917 (Roche‐Hitachi, Inc., Tokyo, Japan) analyzer.
Results
Serum NGAL concentrations ranged from 26.8 to 1,808 ng/ml (median 281 ng/ml, interquartile range (IQR) 453 ng/ml). EDTA plasma NGAL concentrations ranged from 25.7 to 1,752 ng/ml (median 225 ng/ml, IQR 352 ng/ml). The difference in NGAL concentrations in paired serum and EDTA plasma samples (serum– plasma) ranged from −13.8 to 321 ng/ml (median 79 ng/ml, IQR 116 ng/ml; difference from zero, P < 0.0001, Wilcoxon's signed rank test). Although serum and EDTA plasma values were correlated (Spearman's r = 0.95, P < 0.0001), Deming regression analysis showed a slope of 1.1 that was not significantly different from unity (95% confidence interval (CI) 1.0–1.1) and a highly significant intercept of 67.9 ng/ml with a wide confidence interval (95% CI 29.8–106).
Conclusion
NGAL concentration values measured in serum and EDTA plasma cannot be directly compared and should not be used as equivalents in studies of patients admitted to intensive care.
Keywords: acute kidney injury, biomarkers, neutrophil gelatinase‐associated lipocalin (NGAL), critical illness, plasma, serum
Abbreviations
- AKI
acute kidney injury
- CI
confidence interval
- EDTA
ethylenediaminetetraacetic acid
- ICU
intensive care unit
- IQR
interquartile range
- KS‐test
Kolmogorov‐Smirnov's test
- NGAL
neutrophil gelatinase‐associated lipocalin
- PASS
The Procalcitonin and Survival Study
INTRODUCTION
Neutrophil gelatinase associated lipocalin (NGAL) is a siderophore‐binding protein belonging to the lipocalin protein family 1. NGAL was first isolated from neutrophil granulocytes and shown to be released from the specific or secondary granules upon neutrophil activation 2, 3. Later, it was also found in a range of other tissues including renal tubular cells 4. In recent years, the protein has emerged as a potential biomarker of acute kidney injury (AKI). Several reports on the performance of NGAL in this respect have been published, including two meta‐analyses 5, 6. The sample materials investigated varied between heparin plasma, Ethylenediaminetetraacetic acid (EDTA) plasma, serum, and urine. A recent report found a clinically unimportant but statistically significant difference between EDTA and heparin plasma 7. No studies have investigated whether concentrations of NGAL in serum and EDTA plasma are directly interchangeable in the context of patients admitted to intensive care units (ICUs). One study investigated whether NGAL, measured by a radioimmunoassay developed for NGAL homodimer 8, could serve as a biomarker of bacterial infection 9. While a strong correlation was demonstrated between serum and plasma values, concentrations in plasma were considerably lower than in serum. However, the study did not present a direct comparison of serum and plasma NGAL in individual patients or elucidate whether the differences could be compensated. The present study was designed to investigate whether serum and plasma NGAL are directly comparable when sampled from a population of patients undergoing intensive care. If serum and EDTA plasma NGAL values are not directly comparable, it will have implications both for the interpretation of studies of NGAL in intensive care patients in which either serum or plasma has been analyzed and for the meta‐analysis of such studies. Cystatin C served as an internal control in the present study, since it is well‐established that the measured concentrations of this protein do not vary between serum and plasma 10.
MATERIALS AND METHODS
Study Population
We measured NGAL concentrations in 40 paired samples of serum and EDTA plasma from 25 randomly selected ICU patients included in the Procalcitonin and Survival Study (PASS). Details of the PASS and its results have been published elsewhere 11, 12. The PASS and use of the biobank were approved by the local ethical committee (ref. no. H‐KF‐272–753) and the Danish Data Protection Agency (ref. no. 2005–54–1779). Written informed consent was obtained from all patients or their legal representative before enrollment. All data and samples were collected and processed in accordance with Good Clinical Practice standards and European Union legislation (EMEA CPMP/ICH/135/95).
Samples
Serum and EDTA plasma were sampled in standard serum‐separation tubes and EDTA tubes, respectively. Both samples were drawn simultaneously and transported side‐by‐side to a tertiary laboratory for preparation. Samples were placed on ice immediately after sampling and the isolated serum and plasma were frozen to −80°C within 5 hr.
Measurements
NGAL was measured with a particle‐enhanced turbidimetric immunoassay, NGAL‐Test™ (BioPorto Diagnostics A/S). Cystatin C was measured by means of Cystatin C Immunoparticles (Dako A/S, Glostrup, Denmark). The samples were analyzed with a Roche Hitachi 917 (Roche‐Hitachi Inc.) analyzer. Both assays are validated for use on this equipment.
Statistics
Agreement between serum and EDTA plasma NGAL values was analyzed by Bland and Altman's method for nonnormally distributed data 13, 14. The distribution of continuous variables was assessed by graphical inspection of histograms and controlled by Kolmogorov‐Smirnov's (KS) test. Paired continuous data were analyzed by Wilcoxon's signed rank test and presented as medians with the 25th–75th interquartile range (IQR). Linear regression analysis was conducted using the Deming method, assuming a ratio of measurement error of one. If the fitted model had residuals with a normal distribution, standard parametric methods were used to calculate 95% confidence intervals (CI) for the parameters and regression line. To ensure that no outliers overly influence the Deming regression analysis, Passing–Bablok regression was conducted. Correlation was estimated by means of Spearman's correlation coefficient. The value of P < 0.05 was considered significant. Analyses were performed with R 2.15.1 (R Foundation for Statistical Computing, Vienna, Austria, http://r‐project.org), employing the “mcr”‐package version 1.1.
RESULTS
Two samples were excluded from analysis because NGAL concentrations were below the lower limit of quantification of the NGAL assay (25 ng/ml). The differences between serum and plasma values did not convincingly fit a normal distribution curve (KS‐test P = 0.12), and nonparametric analysis was performed. Serum NGAL values ranged from 26.8 to 1,808 ng/ml with a median of 281 ng/ml (IQR 453 ng/ml). EDTA plasma NGAL values ranged from 25.7 to 1,752 ng/ml, with a median of 225 ng/ml (IQR 352 ng/ml). The difference (serum value – EDTA plasma value) ranged from −13.8 to 321 ng/ml, and was significantly different from 0 with a median of 79.1 ng/ml (IQR 116 ng/ml, P < 0.0001, Wilcoxon's signed rank test; Fig. 1). The Deming regression line (independent variable: plasma, dependent variable: serum) had a slope of 1.1, which was not significantly different from unity (95% CI 1.0–1.1) but showed an intercept of 67.9 ng/ml that was significantly different from zero (95% CI 29.8–106 ng/ml). Passing–Bablok regression did not alter the signal of the Deming regression analysis excluding significant influence of outliers. The residuals were approximated to normality (KS‐test P = 0.69). No increased variation with higher values was observed (Fig. 1). The Spearman correlation coefficient was 0.95 (P < 0.0001). Only ten (26%) of the difference values were within ±25 ng/ml of identity, while 12 (31.6%) were within ±50 ng/ml. To investigate for random errors in the sampling, we measured cystatin C in all samples. The median difference between serum and plasma cystatin C was −0.01 mg/l (IQR 0.07, P = 0.73). This was confirmed by a regression analysis in which the slope of 0.99 (95% CI 0.97–1.01) was not significantly different from unity and the intercept of −0.03 mg/l (95% CI −0.02–0.08) was not significantly different from zero.
Figure 1.
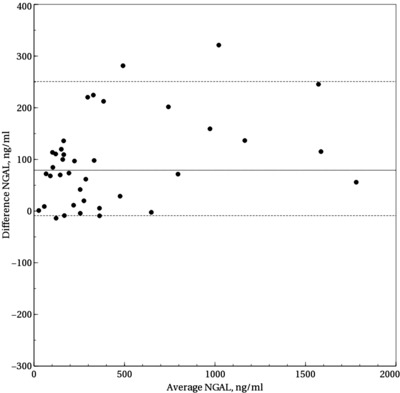
Bland–Altman plot of serum and EDTA plasma neutrophil gelatinase‐associated lipocalin (NGAL). Difference NGAL is the difference between serum and EDTA plasma NGAL concentrations. Average NGAL is the sum of serum and EDTA plasma NGAL divided by two. Solid line (—): Median. Dashed lines (‐‐‐): 5th and 95th percentiles.
DISCUSSION
The present study has demonstrated a clinically important and statistically significant bias between NGAL measured in EDTA plasma and serum. Moreover, it was impossible to correct the difference by linear regression because of wide confidence limits of the intercept estimate. Our results indicate that a significant source of variation in NGAL concentration between plasma and serum must arise in the period from sampling to measurement. Cystatin C measurement showed an almost perfect agreement between serum and plasma, making it unlikely that the findings for NGAL could be attributed to internal error. In contrast to plasma, where the coagulation process is actively inhibited, serum will likely contain proteins produced and secreted during coagulation that are not found in plasma. The reason for the excess NGAL found in serum than that found in plasma could be in vitro release from neutrophil granulocytes. Two mechanisms could contribute to this: (1) proinflammatory proteins or by‐products of coagulation released during the preparation of serum could lead to release of the NGAL‐containing secondary granule contents from neutrophil granulocytes increasing the NGAL concentration in serum; (2) depletion of calcium by EDTA in the plasma could inhibit the calcium‐dependent release of the secondary granule contents, inhibiting further release of NGAL into the EDTA plasma even if the neutrophils are activated. The latter mechanism should also lead to a difference between the NGAL concentration in heparin plasma and EDTA plasma as the calcium concentration is largely unaltered during the preparation of heparin plasma. This was, however, not found when NGAL was measured in a mixed population consisting both of patients seen at the department of chronic hemodialysis and patients admitted to an ICU 7. However, if the increased NGAL is due to degranulation of activated neutrophils inclusion of noninfected hemodialysis patients could attenuate the effect of calcium depletion. Currently, these theoretical considerations await further studies to finally confirm the precise mechanism behind the observed differences.
The release of NGAL from neutrophils during the preparation of serum and different types of plasma has not been studied. However, the release of the protein YKL‐40, which is stored together with NGAL in the secondary granules of neutrophils, has been studied in relation to plasma and serum preparation in considerable detail 15. The YKL‐40 concentrations of serum samples left for 1 hr on the clot were considerably higher than those of EDTA plasma samples, even when these had been left in contact with the blood cells for 72 hr, and successively higher serum values were obtained with increasing time in contact with the clot. It is not unlikely that the release of NGAL in blood samples will show parallel features under similar conditions. The YKL‐40 concentrations were studied in samples from healthy premenopausal women. The excess release of NGAL from neutrophils during serum preparation may be potentiated by the presence of significant bacterial infection 9.
Several proteins produced and secreted during coagulation have inflammatory properties 16, 17. The effects of proinflammatory proteins or by‐products of coagulation released during preparation of serum may sum with in vivo influences that have already primed a proportion of neutrophils to facilitate the release of their secondary granule contents during the preparation of serum. To further explore this hypothesis, studies should be specifically designed to address this question, for example, by incubating EDTA‐blood samples from patients with and without infection with by‐products of coagulation.
The finding of this study is important for the interpretation of previous studies and planning of future trials. In recent years, several studies across various patient populations and conditions, including ICU patients, have reported serum concentrations of NGAL 18, 19, 20, 21, 22, 23, 24. Our results indicate that changing the sample material from serum to plasma in ICU patients could reclassify a substantial number of patients as either NGAL positive or negative regardless of their degree of kidney injury. The range and random nature of the differences could potentially alter the results of these studies in an unpredictable manner 23, 24. Meta‐analyses of the diagnostic accuracy of NGAL in predicting AKI have pooled data from studies with NGAL measured in both serum and in plasma 5, 6. Although the majority of included studies have measured NGAL in plasma, the findings of these reviews should be re‐evaluated, that is by stratification for sample material, to ensure that they are not biased by failing to take the difference between serum and plasma concentrations into account.
CONCLUSION
The present study confirms that NGAL concentrations in serum are generally higher than those in EDTA plasma, showing a median difference of 79 ng/ml. The variation is substantial, making the correction of serum to plasma values or vice versa impossible. The difference is clinically significant. Therefore, when studying blood concentrations of NGAL in different pathological situations, the choice of the blood‐derived sample material is important. A possible mechanism for increased serum values is the in vitro release of NGAL from neutrophil granulocytes during clot formation. Further studies are needed to investigate this and its potential clinical implications. At present, the use of serum as sample material for NGAL measurement in the context of intensive care cannot be recommended if an influence of circulating neutrophils is to be discounted. Meta‐analyses of NGAL studies should take these findings into consideration when pooling data.
ACKNOWLEDGMENTS
We thank our co‐investigators in the PASS group: Central Coordinating Centre: M. L. Jakobsen, S. S. Reilev, and M. Kofoed‐Djursner; Procalcitonin Analysis and Logistics Centre: M. B. Rasmussen, C. S. v. Hallas, M. Zacho, J. Iversen, T. Leerbeck, M. Jeppesen, K. S. Hansen, and K. B. Jensen; Clinical Microbiology Management: J. D. Knudsen, A. Friis‐Møller, K. Schønning, A. Lester, H. Westh, G. Lisby, J. K. Møller, B. Bruun, J. J. Christensen, M. Arpi, K. Astvad, M. D. Bartels, J. Engberg, H. Fjeldsøe‐Nielsen, and U. S. Jensen; PASS Site Clinical Investigators: Glostrup: L. Hein, T. Mohr, D. G. Strange, P. L. Petersen, A. Ø. Lauritsen, S. Hougaard, T. Mantoni, L. Nebrich, A. Bendtsen, L. H. Andersen, F. Bærentzen, A. Eversbusch, B. Bømler, R. Martusevicius, T. Nielsen, P. M. Bådstøløkken, C. Maschmann, U. Grevstad, P. Hallas, A. Lindhardt, T. Galle, K. Graeser, E. Hohwu‐Christensen, P. Gregersen, H. C. Boesen, L.M. Pedersen, K. Thiesen, L. C. Hallengreen, I. Rye, J. Cordtz, K. R. Madsen, P. R. C. Kirkegaard, L. Findsen, L. H. Nielsen, D. H. Pedersen, J. H. Andersen, C. Albrechtsen, A. Jacobsen, T. Jansen, A. G. Jensen, H. H. Jørgensen, and M. Vazin; Gentofte: L. Lipsius, K. Thornberg, J. Nielsen, K. Thormar, M. Skielboe, B. Thage, C. Thoft, M. Uldbjerg, E. Anderlo, M. Engsig, F. Hani, R. B. Jacobsen, L. Mulla, and U. Skram; Herlev: H. Tousi, P. Søe‐Jensen, T.Waldau, T. Faber, B. Andersen, I. Gillesberg, A. Christensen, C. Hartmann, R. Albret, D. S. Dinesen, K. Gani, M. Ibsen, and N. G. Holler; Hvidovre: J. Løken, M. Steensen, J. A. Petersen, P. Carl, E. Gade, D. Solevad, C. Heiring, M. Jørgensen, K. Ekelund, A. Afshari, N. Hammer, M. Bitsch, J. S. Hansen, C. Wamberg, T. D. Clausen, R. Winkel, J. Huusom, D. L. Buck, U. Grevstad, E. Aasvang, K. Lenz, P. Mellado, H. Karacan, J. Hidestål, J. Høgagard, J. Højbjerg, J. Højlund, M. Johansen, and S. Strande; Hillerød: M. Bestle, S. Hestad, M. Østergaard, N. Wesche, S. A. Nielsen, H. Christensen, H. Blom, C. H. Jensen, K. Nielsen, I. B. Jensen, and K. A. Jeppesen; Aarhus‐Skejby: M. H. Andersen, P. Fjeldborg, A. Vestergaard, O. Viborg, and C. D. Rossau; Roskilde: N. Reiter, M. Glæemose, M. B. Wranér, C. B. Thomsen, B. Rasmussen, C. Lund‐Rasmussen, B. Bech, K. Bjerregaard, L. Spliid, L. L. W. Nielsen, and N. E. Drenck; Aarhus‐Centre: K. M. Larsen, M. Goldinger, D. Illum, C. Jessen, A. Christiansen, A. Berg, T. Elkmann, J. A. K. Pedersen, and M. Simonsen; Bispebjerg: H. Joensen, H. Alstrøm, C. Svane, and A. Engquist. BioPorto Diagnostics A/S and Dako A/S supplied analysis kits for NGAL and cystatin C measurement, respectively. TSI received a research grant from Nordsjællands Hospital – part of Copenhagen University Hospital, The Capital Region of Denmark, Denmark. Finally, we also thank the patients and the staff at the participating ICUs.
CONFLICT OF INTEREST
TSI, MHB, and JUJ have not declared conflict of interest. KB holds a position at BioPorto Diagnostics A/S, which manufactures The NGAL Test(TM) and are the inventors of patents and patent applications relating to the diagnostic use of NGAL determination. PHC holds a position at Dako A/S, which manufactures Cystatin C Immunoparticles. BioPorto Diagnostics A/S provided reagents for NGAL analysis. Dako A/S provided reagents for Cystatin C analysis. TSI and MB had full access to all data.
REFERENCES
- 1. Clerico A, Galli C, Fortunato A, et al. Neutrophil gelatinase‐associated lipocalin (NGAL) as biomarker of acute kidney injury: A review of the laboratory characteristics and clinical evidences. Clin Chem Lab Med 2012;50:1505–1517. [DOI] [PubMed] [Google Scholar]
- 2. Kjeldsen L, Johnsen AH, Sengeløv H, et al. Isolation and primary structure of NGAL, a novel protein associated with human neutrophil gelatinase. J Biol Chem 1993;268:10425–10432. [PubMed] [Google Scholar]
- 3. Kjeldsen L, Bainton DF, Sengeløv H, et al. Identification of neutrophil gelatinase‐associated lipocalin as a novel matrix protein of specific granules in human neutrophils. Blood 1994;83:799–807. [PubMed] [Google Scholar]
- 4. Kjeldsen L, Cowland JB, Borregaard N. Human neutrophil gelatinase‐associated lipocalin and homologous proteins in rat and mouse. Biochim Biophys Acta 2000;1482:272–283. [DOI] [PubMed] [Google Scholar]
- 5. Haase M, Bellomo R, Devarajan P, et al. Accuracy of neutrophil gelatinase‐associated lipocalin (NGAL) in diagnosis and prognosis in acute kidney injury: A systematic review and meta‐analysis. Am J Kidney Dis 2009;54:1012–1024. [DOI] [PubMed] [Google Scholar]
- 6. Haase M, Devarajan P, Haase‐Fielitz A, et al. The outcome of neutrophil gelatinase‐associated lipocalin‐positive subclinical acute kidney injury: a multicenter pooled analysis of prospective studies. J Am Coll Cardiol 2011;57:1752–1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bakker AJ, Syperda H. Neutrophil gelatinase‐associated lipocalin: Comparison of the use of EDTA and heparin plasma. Clin Chem Lab Med 2012;50:1679–1680. [DOI] [PubMed] [Google Scholar]
- 8. Xu SY, Petersson CG, Carlson M, et al. The development of an assay for human neutrophil lipocalin (HNL)—To be used as a specific marker of neutrophil activity in vivo and vitro. J Immunol Methods 1994;171:245–252. [DOI] [PubMed] [Google Scholar]
- 9. Xu SY, Pauksen K, Venge P, et al. Serum measurements of human neutrophil lipocalin (HNL) discriminate between acute bacterial and viral infections. Scand J Clin Lab Invest 1995;55:125–131. [DOI] [PubMed] [Google Scholar]
- 10. Kyhse‐Andersen J, Schmidt C, Nordin G, et al. Serum cystatin C, determined by a rapid, automated particle‐enhanced turbidimetric method, is a better marker than serum creatinine for glomerular filtration rate. Clin Chem 1994;40:1921–1926. [PubMed] [Google Scholar]
- 11. Jensen JU, Hein L, Lundgren B, et al. Procalcitonin‐guided interventions against infections to increase early appropriate antibiotics and improve survival in the intensive care unit: A randomized trial. Crit Care Med 2011;39:2048–2058. [DOI] [PubMed] [Google Scholar]
- 12. Jensen JU, Hein L, Lundgren B, et al. Kidney failure related to broad‐spectrum antibiotics in critically ill patients: Secondary end point results from a 1200 patient randomised trial. BMJ Open 2012;2:e000635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res 1999;8:135–160. [DOI] [PubMed] [Google Scholar]
- 14. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307–310. [PubMed] [Google Scholar]
- 15. Høgdall EV, Johansen JS, Kjaer SK, et al. Stability of YKL‐40 concentration in blood samples. Scan J Clin Lab Invest 2000;60:247–251. [DOI] [PubMed] [Google Scholar]
- 16. Levi M, Van der Poll T. Two‐way interactions between inflammation and coagulation. Trends Cardiovasc Med 2005;15:254–259. [DOI] [PubMed] [Google Scholar]
- 17. Levi M, Keller TT, Van Gorp E, et al. Infection and inflammation and the coagulation system. Cardiovasc Res 2003;60:26–39. [DOI] [PubMed] [Google Scholar]
- 18. Alharazy SM, Kong N, Saidin R, et al. Serum neutrophil gelatinase‐associated lipocalin and cystatin C are early biomarkers of contrast‐induced nephropathy after coronary angiography in patients with chronic kidney disease. Angiology 2013. DOI: 10.1177/0003319713483918. [DOI] [PubMed] [Google Scholar]
- 19. Martí J, Fuster J, Solà A, et al. Prognostic value of serum neutrophil gelatinase‐associated lipocalin in metastatic and nonmetastatic colorectal cancer. World J Surg 2013;37:1103–1109. [DOI] [PubMed] [Google Scholar]
- 20. Slack AJ, McPhail MJW, Ostermann M, et al. Predicting the development of acute kidney injury in liver cirrhosis—An analysis of glomerular filtration rate, proteinuria and kidney injury biomarkers. Aliment Pharmacol Ther 2013;37:989–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mahdavi‐Mazdeh M, Abdollahi A, Nozary Heshmati B, et al. Comparison of serum and urine neutrophil gelatinase‐associated lipocalin (ngal) with serum creatinine in prediction of kidney suitability for transplantation. Nephro‐Urol Mon 2013;5:679–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mellor AJ, Woods D. Serum neutrophil gelatinase‐associated lipocalin in ballistic injuries: a comparison between blast injuries and gunshot wounds. J Crit Care 2012;27:419e1–5. [DOI] [PubMed] [Google Scholar]
- 23. Wheeler DS, Devarajan P, Ma Q, et al. Serum neutrophil gelatinase‐associated lipocalin (NGAL) as a marker of acute kidney injury in critically ill children with septic shock. Crit Care Med 2008;36:1297–1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kümpers P, Hafer C, Lukasz A, et al. Serum neutrophil gelatinase‐associated lipocalin at inception of renal replacement therapy predicts survival in critically ill patients with acute kidney injury. Crit Care 2010;14:R9. [DOI] [PMC free article] [PubMed] [Google Scholar]


