Abstract
Background
For the forensic aim, a sensitive and specific method using headspace gas chromatography coupled with mass spectrometry (GC/MS) has been developed for the quantitative determination of ethanol in blood using n‐propanol as internal standard. GC was performed in isothermal mode with a GC run‐time of 5.0 min.
Methods
The quantification was performed using selected ions monitoring mode adopting a quantitative ion and qualifier ion for ethanol and the internal standard.
Results
The method was linear (r 2 = 0.999, in the concentration range of 39.5–1,262.9 μg/ml), specific, sensitive (limit of quantification and limit of detection of 39.5 and 0.4 μg/ml, respectively), and robust. A slightly modified method was also developed for the quantification of 50 commonly abused drunken in blood. The method used an isothermal GC program with a run‐time of 5.0 min. The quantification was performed using selected ions monitoring mode and integrating the area under the peak using n‐propanol as an internal standard. The method was linear 40–1,263 μg/ml and sensitive.
Conclusions
The method was proved superior in speed and selectivity to previously reported methods and was successfully applied to the pharmacokinetic study of ethanol.
Keywords: headspace, GC‐MS, ethanol, whole blood, n‐propanol
INTRODUCTION
Ethanol is widely considered to be the most used and abused chemical substance. As a result, measurement of ethanol is one of the most frequently performed toxicological tests. Ethanol analysis is important for both clinical and forensic purposes. Rapid and accurate analysis in the clinical setting is extremely important for patient care. For forensic purposes, ethanol is measured for workplace drug testing, investigation of driving impairment and accident investigation, and for postmortem evaluation 1. Methods for the measurement of ethanol in blood range from nonspecific and semiquantitative techniques such as osmolality and enzymatic, diffusion methods, to assays that are quantitative and specific for each particular alcohol such as gas chromatography (GC) packed or capillary or flame ionization detection or/and GC–mass spectrometry (MS; 2).
Despite limitations, enzyme‐based immunoassays are used for rapid determination of alcohol concentrations in clinical laboratories, so this method has been used in our laboratory to support clinical need, but for forensic application, GC or GC/MS should be the method of choice 3. Breath analysis is a rapid way to identify a subject with alcohol intoxication, but this test also suffers from limitation 4. Alcohol can also be measured indirectly using osmolar gap, but direct measurement of alcohol in serum or whole blood is the state‐of‐the‐art practice. For legal alcohol, caution should be taken with regard to methodology and chain of custody.
GC/MS has also been utilized for determination of alcohol concentration in serum. Dean et al. 5 reported a method for simultaneous determination of ethanol and ethyl‐d5 alcohol in serum using stable isotope GC/MS. Wasfi et al. 2 developed a sensitive and specific method using static headspace GC combined with MS for quantitative determination of ethanol in biological fluids using n‐propanol as an internal standard.
Compared with the traditional GC headspace method that must use an FID flame ionization detection and a packed column, GC/MS method is more advantageous, which is of particular importance in forensic samples suspected for presence of abused inhalants 6. So with more laboratories and affordable bench tops GC/MS instruments now, our method is of great value for the clinical and forensic purposes.
Alcohol dissolves in an aqueous environment, and because the water content of serum (about 98%) is greater than that of whole blood (about 86%), serum ethanol results are always higher than those obtained with whole blood. The serum:whole blood ethanol ratio is 1.14 (1.09–1.18) and varies slightly with hematocrit 7. Although most states have enacted laws that define intoxication while driving a motor vehicle based on whole blood ethanol levels, some states do not specify the specimen type. Therefore, laboratories that perform alcohol analysis must report the type of sample required. Several body fluids, such as venous blood, capillary blood, serum or plasma, urine (fresh void), vitreous humor, tear fluid, cerebrospinal fluid (lumbar fluid), saliva, sweat, and breath, are suitable for determination of ethanol in living subjects. Serum, plasma, or urine may be used if ethanol is assayed using enzymatic methods. Because GC analysis is used, any body fluid or tissue is suitable for analysis. Anticoagulants do not interfere with either method.
On the other hand, the whole blood specimens should be drawn in a gray‐top (potassium oxalate/sodium fluoride) Vacutainer. Preferably, the venipuncture site should be cleaned with an alcohol‐free disinfectant, such as aqueous benzalkonium chloride (zephiran) or povidone iodine. Samples must be well capped and preferably refrigerated to prevent loss of ethanol. No ethanol was lost from whole blood specimens stored at 0–3°C or at room temperature (22–29°C) for up to 14 days 8. For longer storage or nonsterile postmortem specimens, sodium fluoride can be used as a preservative to prevent increases in ethanol concentration because of fermentation.
Measurement of blood ethanol concentration is important for law enforcement as it is the measure for the determination of driving under the influence. Examples of punishable blood alcohol concentration limits include 80 mg/dL (0.08 gram percent) in the United States, United Kingdom, and Canada; 0.20 mg/g in Sweden; and 0.50 mg/g in most EU countries 9. However, these values have no relevance to clinical management because there is no consensus on the concentration that defines clinical intoxication.
For the forensic aim, there are few methods on the determination of ethanol in biological samples except the whole blood by GC/MS. So, this study was aimed to develop a sensitive and specific method using headspace GC/MS for the quantitative determination of ethanol in the whole blood.
EXPERIMENTAL
Reagents
Ethanol and n‐propanol were both provided by Tianjin Kemiou Chemical Reagents Development Center (Tianin City, China), HPLC grade (the purity of ethanol and n‐propanol are above 99.8%, respectively) blood samples.
Equipments and Accessories
Shimadzu GC‐MS‐QP5050A (manufactured by SHIMADZU company, Japan), Agilent HS1000 headspace injector (manufactured by Agilent Technologies, American), headspace vials, 20 ml with seal, aluminum cap, and crimper were used in this study.
Reagent Preparation
Stock solution of ethanol (7.9 mg/ml) and n‐propanol (internal standard, 16.1 mg/ml, 643.0 μg/ml, respectively) was prepared in 100 ml purified water, and stored in refrigerator at −4°C. A series of standard solutions was prepared by diluting the stock solution with 25 ml purified water, their concentrations were 79.0, 157.9, 315.7, 631.4, 1,262.9, 2,525.8 μg/ml for ethanol and 643.0 μg/ml for n‐propanol. All standard solutions and stock solutions were prepared weekly and stored in refrigerator at −4°C.
Conditions and Operation of GC‐MS
Conditions of the inlet Vapor‐liquid equilibrium temperature: 60°C; duration for vapor‐liquid equilibrium: 10.0 min. Gas‐mass spectrometer conditions. Chromatograph column: capillary column AB‐INOWAX (J&K Scientific, Beijing, China), 30 m × 0.25 mm × 0.25 μm. Column temperature: 70°C (5 min); column flow rate: high‐purified helium, 1.0 ml/min (constant flow); inlet: 200°C; detector: 200°C. Injection means—split stream sampling, split stream ratio: 25:1, mass scan range m/z 20–120, SIM selected ions monitoring: ethanol (m/z: 31, 45), n‐propanol (m/z: 31, 59), EI Electron ionization source, detector voltage: 1.0 kV.
Experiment condition
Blank blood sample
Pipette 1 ml blank whole blood confirmed with no ethanol, into the 20 ml headspace vial, cover the vial with a polytetrafluoroethylene film, silastic seal, and then pressurize the aluminum cap with a crimper, seal, and mix well. Heat the vials in the headspace inlet for 10 min at 60°C. After vapor‐liquid equilibrium under the conditions specified in Section “Recovery and Sample Stability, use air‐tight syringe to take 1.0 ml for injection (n = 3). Data are collected automatically by the machine.
Blood samples containing ethanol
Pipette 40 μl solution of ethanol (7.9 mg/ml) into 1 ml of blank whole blood sample confirmed with no ethanol to obtain the blood sample containing 315.7 μg/ml ethanol. The next procedure is described in Section “Blank blood sample.”
Blood samples containing n‐propanol
Pipette 0.5 ml n‐propanol (643.0 μg/ml) into 0.5 ml of blank whole blood sample confirmed with no ethanol to obtain the blood sample containing 321.5 μg/ml n‐propanol. The next procedure is described in Section “Blank blood sample.”
Standard Curve Plotting
Pipette 0.5 ml blank whole blood sample into six 20 ml headspace vials, add 0.5 ml of standard solutions (79.0, 157.9, 315.7, 631.4, 1,262.9, 2,525.8 μg/ml for ethanol and 643.0 μg/ml for n‐propanol) to six bottles, respectively, to obtain the ethanol concentration 39.5, 78.9, 157.9, 315.7, 631.4, 1,262.9 μg/ml and n‐propanol concentration 321.5 μg/ml. The vials are covered with polytetrafluoroethylene film, silastic seal, and the aluminum cap is capped by a crimper, sealed, mixed well, and heated in the headspace inlet for 10 min at 60°C. After vapor‐liquid equilibrium procedure specified in Section “Conditions and Operation of GC‐MS,” take 1.0 ml using air‐tight syringe for injection (n = 3); data are automatically collected by the machine. The Y‐axis is presented as the average peak area ratio of ethanol to the internal standard (n‐propanol). The X‐axis is presented as the ethanol level.
METHOD VALIDATION PROCEDURE
The method was validated according to the procedures set out by the FDA Guidance for Industry—Bioanalytical Method Validation procedure 10. All data were produced using analyte‐integrated peak area to internal standard (n‐propanol) integrated peak area ratios.
LOD and LOQ Determination
Limit of detection (LOD) was determined as the response that was at least three times the response compared to the blank response. Lower limit of quantification was determined as the response that was at least five times the response compared to the blank response, reproducible with a precision of 20% and an accuracy of 80–120%.
Accuracy and Precision
Prepare the samples with final ethanol concentration 78.9, 315.7, 1,262.9 (μg/ml), and n‐propanol concentration 321.5 μg/ml as low (L), mid (M), and high (H) concentrations. Determine the accuracy and precision as follows.
Accuracy was determined at 3, the different concentrations with five replicates for each concentration and the deviation of the mean result from the true value determined by calibration were expressed as a percentage.
Intraday precision was expressed as the coefficient of variation determined using the reproducibility of five replicate blood samples at three different concentrations—low (L), mid (M), and high (H) concentrations. The procedure was repeated on six different occasions to give interday data.
Recovery and Sample Stability
Recovery was determined at the low and high concentrations by comparing blood samples with solutions of ethanol dissolved in water. Recovery after storage was assessed both by storage of blood in sample tubes for 6 and 24 h at room temperature, 1 and 4 months at −80°C, and after three freeze–thaw cycles at −80°C to room temperature. Stability on the sampler was also assessed by leaving blood samples in vials, following preparation, at room temperature for 24 h.
SAMPLE INVESTIGATION
Pipette 0.5 ml whole blood samples into the 20 ml headspace vials, add 0.5 ml n‐propanol (643.0 μg/ml) the next procedure is the same as described in Section “Standard Curve Plotting.” According the peak area ratio of ethanol to the n‐propanol, the concentration of ethanol in the blood samples can be determined from the internal standard curve, and its content in the blood samples can be calculated. Two quality controls, 78.9 and 315.7 μg/ml, are detected with the samples.
RESULTS AND DISCUSSION
Under the chromatographic conditions used, there were no blank effects, and the method for ethanol was linear in the concentration range used with correlation coefficients above 0.999 (Fig. 1). The LOD was found to be 0.4 μg/ml for ethanol and the LOQ was found to be 39.5 for ethanol. Table 1 shows the accuracy (n = 6) and the intra‐assay coefficient of variation (n = 6) and interassay coefficient of variation (n = 6) evaluated at concentrations of 78.9, 315.7, and 1,262.9 μg/ml, which proved the method was sensitive, robust, and reproducible. Under the described conditions, ethanol and n‐propanol (the internal standard) identified by its retention time, respectively, were well separated with a GC run‐time of 5.0 min (Fig. 2, 3, 4). Recovery for ethanol was good (exceeding 80%) throughout the range of concentrations tested. Table 2 shows that the analytes were also stable in the variety of conditions tested.
Figure 1.

Calibration curves (n = 3, 39.5–1262.9 μg/ml) of enthanol in blood (y = 0.0016x – 0.0029; r 2 = 0.9998).
Table 1.
The Accuracy and Precision of Three Concentrations (μg/ml) of Ethanol Measured by Headspace GC/MS
| 78.9 | 315.7 | 1,262.9 | ||
|---|---|---|---|---|
| Accuracy (n = 6), | Mean | 90.6 | 95.2 | 102.7 |
| R.R. relative recovery (%) | SD | 8.00 | 4.9 | 0.7 |
| Precision (n = 6), | Intra‐assay | 3.8 | 0.7 | 1.0 |
| RSD (%) | Interassay | 9.5 | 4.9 | 0.8 |
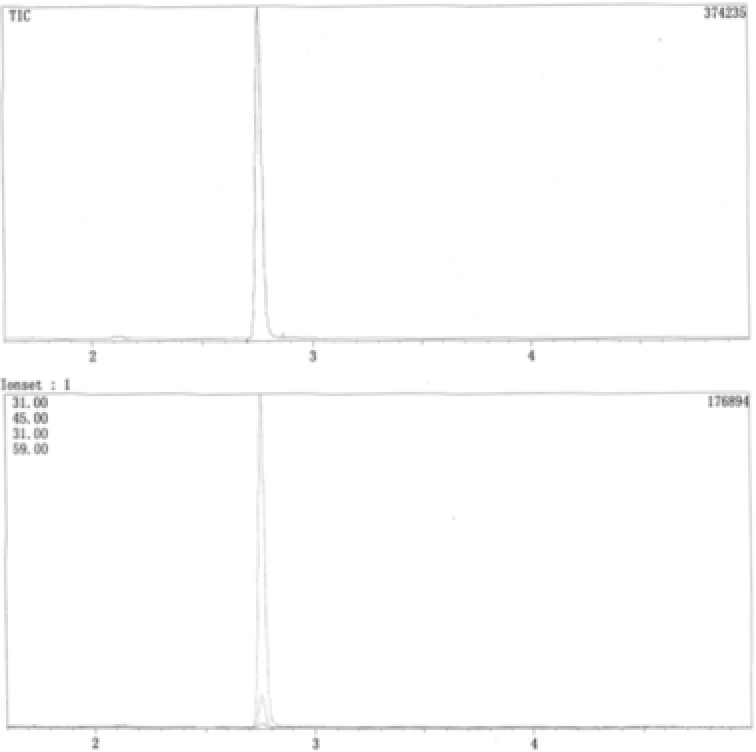
Figure 2.

Total and selected ion chromatogram of ethanol.
Figure 3.
Total and selected ion chromatogram of n‐propanol.
Figure 4.

Total and selected ion chromatogram of ethanol and n‐propanol.
Table 2.
Stability of Ethanol in Blood Samples at Room Temperature (RT), −80°C, and Through Freeze–Thaw Cycles
| Recovery (%) | ||
|---|---|---|
| 78.9 | 1,262.9 | |
| 6 h in sample tube RT | 98 | 99 |
| 24 h in sample tube RT | 92 | 94 |
| 24 h in vials RT | 101 | 98 |
| ×3 −80°C freeze–thaw cycles | 105 | 94 |
| 1 month in sample tubes −80°C | 102 | 98 |
| 4 months in sample tubes −80°C | 90 | 90 |
O'Neal et al.'s 11 study demonstrates that using t‐butanol or methyl ethyl ketone as internal standards resulted in precise ethanol determinations in postmortem blood, whether applied to procedures with packed or capillary columns with direct injection or headspace GC. Additionally, the use of these internal standards with capillary headspace GC allows for the identification of other volatiles in postmortem specimens, specifically n‐propanol, which may aid in distinguishing antemortem ingestion from postmortem synthesis of ethanol. However, for the drunk, the internal standard typically used is n‐propanol 12. As our hospital has more drunk to identify, which are nearly not postmortem specimens, we selected n‐propanol as the internal standard.
Application of the GC/MS method for the quantification for blood ethanol in authentic samples (n = 50) is very fast, accurate, sensitive. According to the results of abused inhalants, many drunk‐driving and accident investigation were identified. In Chengdu city of Sichuan province, three laboratories including ours could develop method for legal and clinical use. From the literature, we are the first laboratory that uses GC/MS method to determine ethanol in the whole blood. As a result, our method is very reasonable. So, our method is important for the clinical intoxication to investigate the effect of ethanol too.
CONCLUSIONS
A rapid, sensitive, and selective GC/MS method for quantification of ethanol in whole blood using n‐propanol as internal standard is reported in this study. Compared with the analytical methods reported in the literatures, the method offered satisfactory selectivity, good sensitivity with short run‐time of 5.0 min using headspace GC/MS, which are of particular advantage to high sample throughput of bioanalysis. The method was proved superior in speed and selectivity to previously reported methods and was successfully applied to the pharmacokinetic study of ethanol.
Grant sponsor: Science and Technology Pillar Program of Sichuan Province; Grant number: 2009SZ0226; Grant sponsor: Health Department of Sichuan Province; Grant number: 100491; Grant sponsor: Chengdu City Science and Technology Project; Grant number: 11PPYB010SF‐289.
REFERENCES
- 1. Winek CL, Carfagna M. Comparison of plasma, serum, and whole blood ethanol concentrations. J Anal Toxicol 1987;11:267–268. [DOI] [PubMed] [Google Scholar]
- 2. Wasfi IA, Al‐Awadhi AH, Al‐Hatali ZN, Al‐Rayami FJ, Al Katheeri NA. Rapid and sensitive static headspace gas chromatography–mass spectrometry method for the analysis of ethanol and abused inhalants in blood. J Chromatogr B 2004;799:331–336. [DOI] [PubMed] [Google Scholar]
- 3. Maeda H, Zhu BL, Ishikawa T, et al. Evaluation of postmortem ethanolconcentrations in pericardial fluid and bone marrow aspirate. Forensic Sci Int 2006;161:141–143. [DOI] [PubMed] [Google Scholar]
- 4. Currier GW, Trenton AJ, Walsh PG. Innovations: Emergency psychiatry: Relative accuracy of breath and serum alcohol readings in the psychiatric emergency service. Psychiatr Serv 2006;57:34–36. [DOI] [PubMed] [Google Scholar]
- 5. Dean RA, Thomasson HR, Dumaual N, Amann D, Li TK. Simultaneous measurement of ethanol and ethyl d5‐alcohol by stable isotope gas chromatography‐mass spectrometry. Clin Chem 1996;42:367–342. [PubMed] [Google Scholar]
- 6. Helander A, Beck O. Mass spectrometric identification of ethyl sulfate as an ethanol metabolite inhumans. Clin Chem 2004;50:936–937. [DOI] [PubMed] [Google Scholar]
- 7. Winek CL, Carfagna M. Comparison of plasma, serum, and whole blood ethanol concentrations. J Anal Toxicol 1987;11:267–268. [DOI] [PubMed] [Google Scholar]
- 8. Winek CL, Paul LJ. Effect of short term storage conditions on alcohol concentrations in blood fromliving human subjects. Clin Chem 1983;29:1959–1983. [PubMed] [Google Scholar]
- 9. Jones AW. Medicolegal alcohol determinations—Breath‐ or blood‐ alcohol concentrations? Forensic Sci Rev 2000;12:23–47. [PubMed] [Google Scholar]
- 10. Food and Drug Administration. 2001. U.S. Department of Health and Human Services, Guidance for Industry, Bioanalytical Method Validation. FDA [Available on line at http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm070107.pdf] (Accessed January 2012).
- 11. O'Neal CL, Wolf CE II, Levine B, Kunsman G, Poklis A. Gas chromatographic procedures for determination of ethanol in postmortem blood using t‐butanol and methyl ethyl ketone as internal standards. Forensic Sci Int 1996;83:31–38. [DOI] [PubMed] [Google Scholar]
- 12. Williams RH, Shah SM, Maggiore JA, Erickson TB. Simultaneous detection and quantitation of diethylene glycol, ethylene glycol, and the toxic alcohols in serum using capillary column gas chromatography. J Anal Toxicol 2000;24:621–626. [DOI] [PubMed] [Google Scholar]


