Abstract
The aim of this study was to estimate the prevalence of low-back pain (LBP) and to identify the level of functional disability in elderly individuals in different populations. From January 1985 to October 2018, a search was performed using the following databases: Embase, LILACS, SciELO, Scopus, Medline, and the Web of Science. The descriptors were low-back pain, back pain, lower-back pain, prevalence, and elderly in Portuguese and English. Two independent reviewers conducted a search for studies and evaluated their methodological quality. The search strategy returned 2186 titles, and 35 were included in this review. The studies evaluated 135,059 elderly individuals aged between 60 and 102 years, and the prevalence of LBP ranged from 21% to 75%. The levels of functional disability, as well as functional difficulties, activities of daily living, and physical capacity, were identified in 60% of the studies. This review indicated a high prevalence of LBP in elderly individuals and functional disability that affects factors important for independence. However, the studies used different methodologies, suggesting that more studies be conducted with scientific accuracy, methodological quality, and low risk of bias to contribute to the proposal of preventive actions for elderly populations.
Keywords: Prevalence, Low Back Pain, Spine, Elderly, Systematic Review
INTRODUCTION
Low-back pain (LBP) is one of the most common health problems in primary care (1). LBP can be defined as any pain between the last ribs and the lower gluteal folds, with or without pain in the lower limbs (2). In addition, the duration of pain is one criterion for LBP classification. Acute LBP has a sudden onset and lasts less than six weeks, subacute LBP lasts from six to 12 weeks, and chronic LBP presents for a period greater or equal to 12 weeks (3).
It is estimated that 70% to 85% of the population will experience an episode of LBP at some point. Ninety percent of these individuals will have more than one episode (4-6). The United States spent more than $100 billion on LBP-related healthcare in 2005 (7), and these costs are expected to increase as the prevalence of back pain also increases (8).
Historically, research on LBP has primarily focused on young people and adults, while little attention has been given to the elderly population (9). There is evidence that LBP may be responsible for a large percentage of functional limitations (10), result in difficulty performing daily life activities (11), and be a risk factor for incapacity and invalidity. LBP is one of the symptoms most frequently reported by older people (12). Notwithstanding the fact that it has been identified as a major health problem, its prevalence is not well known in the elderly population (13,14).
This systematic review aims to identify, analyze and synthesize, in a systematic way, the prevalence of LBP in the elderly population.
METHODS
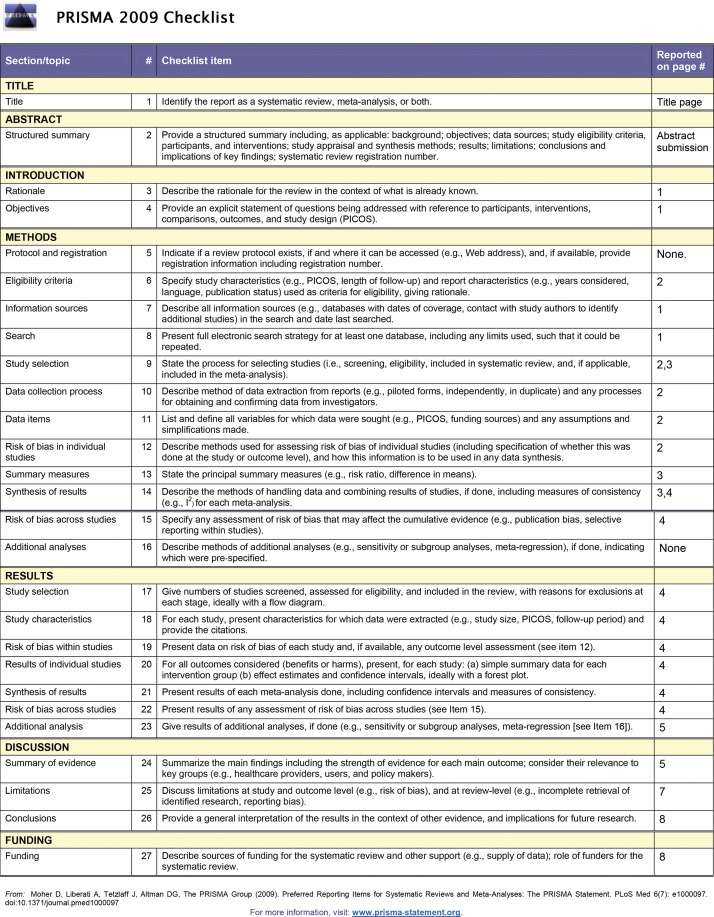
The protocol of this review is registered at PROSPERO (CRD42019118004), and the methods followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) recommendations (15).
Search Strategy and Literature Sources
Searches were performed in the following databases: Scientific Electronic Library Online (SciELO), Latin American and Caribbean Health Sciences (LILACS), US National Library of Medicine (Medline), Scopus Info Site (Scopus), the Web of Science, and Embase (Excerpta Medica).
The Health Sciences Descriptors (DeCS) and Medical Subject Headings (MeSH) used for the English search were low-back pain, back pain, lower back pain, prevalence, and elderly; for the search in Portuguese, they were low-back pain, prevalence, and elderly. For MeSH and DeCS, the operators “OR” and “AND” were used to form research topics that could be combined. The search strategy is shown in the supplementary material.
Inclusion criteria
The inclusion criteria were as follows: studies that primarily or secondarily investigated LBP prevalence among elderly individuals aged 60 years or over according to the World Health Organization (16); studies that included both sexes and individuals living in the community or institutionalized (in clinics, hospitals or public or private care institutions), regardless of duration of LBP symptoms (i.e., acute, subacute, or chronic LBP); and articles that are available in English or Portuguese.
Data extraction
Studies published in Portuguese and English with a cross-sectional design from 1985 to October 2018 were searched. Two independent reviewers (IMBS and TFS) selected studies based on the title and summary. The ones that met the eligibility criteria were analyzed and evaluated. After fully reading the selected studies, no conflicts were found between the two independent reviewers.
The descriptive data extracted and analyzed from the studies were as follows: first author/year of publication, participant’s characteristics (sex, age, population), country, instrument of collection, sample size, definition of LBP, absolute frequency of LBP, prevalence, investigated duration of LBP and functional disability level.
Risk of bias assessment
To assess the risk of bias and the methodological quality, the instrument developed by Hoy et al. was used (17). Considering that selected studies could present potential sources of bias that could influence the results (Table 2), the tool was used to assess the risk of bias of the eligible studies. This instrument allows for the verification of the risk of bias related to external and internal validity, allowing for the classification of the risk of bias as low, moderate, or high. This instrument was chosen mainly because it is easy to use, shows high interexaminer agreement, and was developed specifically to measure the risk of bias in prevalence studies of patients with LBP.
Table 2. Characteristics of the studies found in the systematic review with chronic low back pain prevalence.
| Author/Year | Gender | Age (years) | Population | Country | Instrument | Sample Size | Sample with LBP | Prevalence (%) | Prevalence period* | LBP Definition | Functional disability |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lavsky-Shulan et al., (1985) (26) | Both | ≥65 | Two rural counties adjacent to the county in which the University of Iowa, USA. | USA | Itself questionnaire | 3097 | 671 | 21.7 | 1 year | Not informed | Women had the most difficulty doing household chores (42.3%), while men had the most difficulty bending over (28.3%) |
| Weiner et al., (2003) (27) | Both | 73.6 | Caucasians recruited were from a random sample of Medicare beneficiaries in designated zip codes in Pittsburgh, Pennsylvania and Memphis, Tennessee, and African Americans. | USA | Itself questionnaire EPESE performance battery + Health ABC functional capacity scale | 2776 | 987 | 36 | 1 year | Back pain location was categorized as upper, middle, lower, or buttocks | Functional difficulty was more common with greater severity of LBP among both genders |
| Cecchi et al., (2006) (28) | Both | 65 | A representative cohort of persons aged 65 or more (65+) selected was from the registries of Greve in Chianti (rural area) and Bagno a Ripoli (urban area near Florence). | Italy | Itself questionnaire | 1008 | 318 | 31.5 | 1 year | Presence of frequent back pain (quite often-almost every day). | The 7.4% of the overall study population had LBP related functional limitation |
| Dellaroza et al., (2008) (29) | Both | 69.5 | Population sample of community-dwelling elderly residents in the city of São Paulo, Brazil. | Brazil | Itself questionnaire Lawton Scale | 1271 | 95 | 25.4 | ≥6 months | Lumbar region (below waist) | Dependent in the basic activities of daily living with chronic pain (33.7%) and instrumental activities of daily living (62.4%) |
| Hicks et al., (2008) (30) | Both | 81.3 | The Retirement Community Back Pain Study is a population-based survey study of adults ages 62 years or older. | USA | Itself questionnaire | 522 | 251 | 48.1 | 1 year | Not informed | Participants with LBP plus leg pain had greater disruption in physical capacity than those without LBP |
| Kovacs et al., (2008) (31) | Both | 65 | All community dwelling residents in the island of Majorca who are retired from work or 65 years or older (even if they have never worked), are invited to attend such conferences at no cost. | Spain | Roland Morris Questionnaire and Visual Analogue Scale | 1044 | 792 | 34.1 | 3 months | Pain between the costal margins and the inferior gluteal folds, usually accompanied by painful limitation of movement | In subjects with LBP, fear avoidance beliefs correlated moderately with disability |
| Dos Reis et al., (2008) (32) | Both | 69.1 | Elderly attended in the geriatrics sector of the Physical Therapy School Clinic from the Universidade Estadual of the Sudoeste of Bahia. | Brazil | Medical records | 131 | 44 | 33.6 | 3 months | Symptom referred to at the level of the pelvic girdle, generating a clinical condition of pain | Not informed |
| Woo et al., (2009) (33) | Both | 72.5±4.8 | Elderly community of the Hong Kong. | China | Itself questionnaire} Physical Activity Scale of the Elderly Grip strength | 4000 | 1569 | Total 39.2 M 39.2 F 50.3 |
1 year | Not informed | Back pain affecting activities of daily living predisposed to reduced grip strength and physical activity score |
| Holton et al., (2011) (34) | Male | 74±6 | Elderly recruited at 6 US academic medical centers in Birmingham AL, Minneapolis MN, Palo Alto, CA, Pittsburgh PA, Portland OR, and San Diego, CA. | USA | The North American Spine Society questionnaires for back and neck pain Physical Activity Scale of the Elderly | 298 | 126 | 66 | 1 year | North American Spine Society questionnaires for back and neck pain | Men with and without diffuse idiopathic skeletal hyperostosis did not vary from one another with physical activity score |
| Abegunde & Owaje, (2013) (35) | Both | ≥60 | Eldelry residents at Iseyin (urban) and Ilua (rural) of Oyo. | Nigeria | Itself questionnaire | Rural 314 Urban 316 |
253 | Rural 38.5 Urban 41.8 |
3 months | Not informed | Not informed |
| Exarchou et al., (2013) (36) | Male | 69-81 | Elderly residents of Uppsala, Malmo, Gothneburg. | Sweden | Quebec Pain Disability Scale Physical Activity Scale for the Elderly questionnaire | 1005 | 445 | 44.3 | 1 year | Not informed | Were no statistically significant differences between those with and without radiographic sacroilitis reflected by measures on physical activity, functional status and LBP |
| Figueiredo et al., (2013) (37) | Both | 72 | Healthy community-dwelling elderly in urban area | Brazil | McGill Questionnaire and Roland Morris Questionnaire | 54 | 34 | 61.8 | 1 year | Pain, tension or stiffness located in the region between the last ribs and the gluteal line | A high and positive correlation with the presence of LBP was indicated for functional disability |
| Ghanei et al., (2014) (38) | Male | 69-81 | Men aged 69-81 years enrolled in Malmo, Gothenburg and Uppsala with the primary aim to evaluate risk factors for osteoporosis and fractures. | Sweden | Visual Analog Scales for LBP, Roland Morris Questionnaire | 489 | 236 | 45 | 1 year | LBP was defined as pain in the lower back, SCI as pain emerging from the lower back with radiation to the lower extremity below the buttocks | 50% of the men with LBP + SCI + NEU reported impairment in activity of daily living due to the disorder |
| Palma et al., (2014) (39) | Both | 60-69 | Elderly registered at the Family Health Strategy of Vila São Paulo, Bauru,SP, Brazil. | Brazil | Nordic and the Roland Morris questionnaires | 360 | 246 | Total 68.3 M 25.1 F 35.1 |
1 year | Pain or discomfort in the last twelve months, not related to trauma or other problem | 67.5% of the elderly demonstrated an inappropriate functional capacity |
| Pereira et al., (2014) (40) | Both | 60-80 | Health Surveillance Network for Elderly People (REVISI), in Goiânia, Goiás State, Brazil | Brazil | Numerical Range Scale | 934 | 135 | 29.5 | 6 months | Pain in lumbar region | Not informed |
| Santos et al., (2015) (41) | Both | 86.3 | Elderly participants “Long-lived Project” Federal University of São Paulo (UNIFESP). | Brazil | Verbal Numeric Scale, Visual Numeric Scale Face Pain Scale | 330 | 61 | 32.7 | 6 months | Not informed | Not informed |
| Scherer et al., (2016) (42) | Both | 74 | Elderly residents of the cities Bonn, Dusseldorf, Frankfurt/Main, Hamburg, Jena, Leipzig, Mannheim and Munich. | Germany | Graded Chronic Pain Scale | 3189 | 1493 | M 55.2 F 41.1 |
6 months | Not informed | Not informed |
| Kherad et al., (2016) (43) | Male | 69-81 | Mister Osteoporosis (MrOS) Sweden is a multi-centre population-based study of 3,014 men aged 69-81 years, enrolled in the cities of Malmö, Gothenburg and Uppsala. | Sweden | Itself questionnaire | 3014 | 1361 | 49 | 1 year | Pain in the lower back but not specified further | Not informed |
| Marshall et al., (2016) (44) | Male | ≥65 | U.S. men enrolled in MrOS, a nationwide prospective cohort study in U.S. academic medical centers in Birmingham AL, Minneapolis MN, Palo Alto CA, Pittsburgh PA, Portland OR, and San Diego CA. | USA | Itself questionnaire | 5568 | 3707 | 67 | 1 year | Not informed | Not informed |
| Quintino et al., (2017) (45) | Both | ≥60 | Elderly people that live in the Family Health Strategy confined areas, in the neighborhood of Vila São Paulo, northern region of Bauru, São Paulo. | Brazil | Nordic questionnaire, adapted to the Brazilian culture | 363 | 200 | 55.8 | 1 year | Pain or discomfort in the last twelve months, not related to trauma or any other problem in the lumbar region | Not informed |
| Machado et al., (2018) (46) | Both | ≥65 | Households located in 15 clusters (census regions) distributed across the city of Belo Horizonte. | Brazil | Itself questionnaire Handgrip test and a walking test | 378 | 35 | 9.3 | 1 year | Pain or discomfort in the lower back lasting for at least 24 hours, and not related to feverish illness or spinal surgery | Those reporting a recent history of disabling LBP were more likely to have low level of physical activity |
| Total | 29,831 | 12,806 |
Subtitle: LBP = Low back pain;
= period prevalence investigate;
SCI = Sciatic; NEU = Neurological deficits.
This instrument (17) uses the following criteria: (1) representativeness of the study sample in relation to the national population to assess the generalizability of the results; (2) a sampling system that represents the target population; (3) a method for selecting the sample; (4) probability of nonresponse bias; (5) method of obtaining a response of interest; (6) definition of LBP used to select the sample; (7) reliability and validity of the tools used; (8) standardization of the collection process; (9) period of prevalence of appropriate interest; and (10) presence of error in calculation and/or reporting values of the numerator and denominator of the parameter of interest. The first four topics are related to the external validity of the study. Consequently, the other items report the risk of bias in categories relating to internal validity. At the end of the analysis, studies with at least nine criteria were classified as having a low risk of bias; studies that had between seven and eight of the criteria had a medium risk of bias; and those with less than seven of the criteria had a high risk of bias.
RESULTS
Summary of included studies
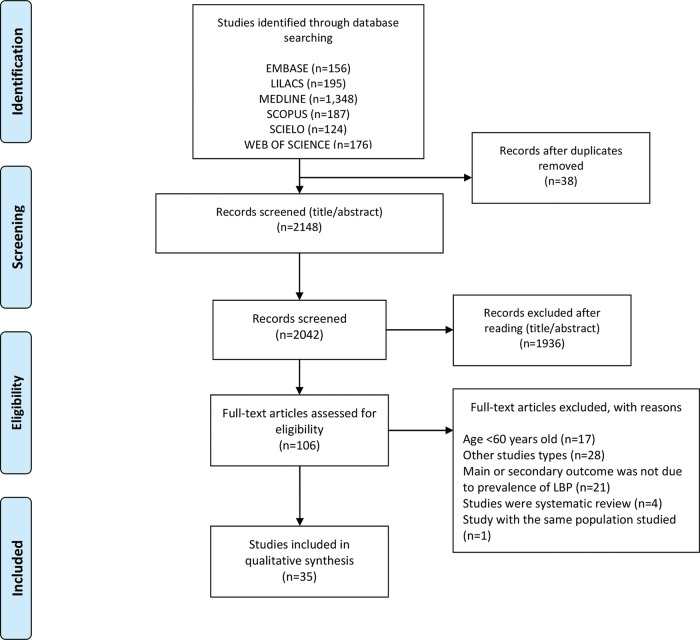
We identified 2186 titles; of these, 38 were duplicates. During the search by title and abstract, 2148 studies were selected, and 1936 were excluded after reading the summaries. One hundred six studies were selected for full-text reading, and only 35 met the eligibility criteria and were included in the systematic review (Figure 1). Because of great heterogeneity, a meta-analysis was not possible.
Figure 1. Flowchart of the included studies.
Characteristics of the studies
The prevalence of LBP among the elderly individuals ranged from 21 to 75%. These studies included a total of 135,059 elderly individuals, with sample sizes ranging from 54 to 55,690 elderly individuals, and LBP was present in 34,516 of the participants (Tables 1, 2 and 3).
Table 1. Characteristics of the studies found in the systematic review with acute low back pain prevalence.
| Author/Year | Gender | Age (years) | Population | Country | Instrument | Sample Size | Sample with LBP | Prevalence (%) | Prevalence period* | LBP Definition | Functional disability |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hartvigsen et al., (2003) (18) | Both | 80 | Interview data from the Longitudinal Study of Aging Danish Twins, dealing with a population-based sample of Danish twins aged 70-102. | Denmark | Itself questionnaire | 4486 | 1121 | Total 25 M 20 F 29 |
1 month | Not informed | 2.78 for participants with LB vs 3.16 forparticipants without LBP |
| Blay et al., (2007) (19) | Both | ≥60 | Respondents selected were from a multistage area probability sample of non-institutionalized population in the state of the Rio Grande of Sul, Brazil. | Brazil | Itself questionnaire | 6963 | 2997 | 42.5 | 1 month | Not informed | Not informed |
| Meyer et al., (2007) (20) | Both | 75 | Subjects at Centers for Medicare Medicaid Services (CMS) started the Health Outcomes Survey (HOS) collecting health status d outcomes over time in different Medicare settings. | USA | Itself questionnaire | 55.690 | 13.244 | 24.1 | 1 month | Not informed | Participants with no functional limitations was 64.7% |
| Lima et al., (2009) (21) | Both | 69.9±0.3 | Elderly residents the cities of Botucatu and Campinas; an area encompassing the cities of Itapecerica da Serra, Embu, and Taboão da Serra; and the District of Butantã, in the city of São Paulo. | Brazil | Itself questionnaire Sf-36 - Physical functioning | 1958 | 621 | 30.1 | Not informed | Not informed | With LBP (64.7%) |
| Rana et al., (2009) (22) | Both | 69.1±6.9 | Elderly residents in the rural area of the Matlab city, Dhaka. | Bangladesh | Itself questionnaire | 471 | 341 | Total 72.4 M 64.6 F 78.8 |
At exactly moment | Not informed | Not informed |
| Gálvez-Barrón et al., (2015) (23) | Both | ≥80 | Elderly non-institucionalized residents in the rural and urban area. | Spain | Face Pain Scale Katz index | 551 | 289 | Total 52.5 M 40.7 F 58.1 |
1 month | Pain in dorso-lumbar region | Functional status (median and interquartile range): Pain 1 (0-3) |
| Tomita et al., (2015) (24) | Female | 72.6±5.2 | Community-dwelling women, who were non-institutionalized and lived independently in Oshima Town, Nagasaki Prefecture. | Japan | Itself questionnaire Timed up and Go test Time of walking a 6m distance Chair Stand time Grip strengh | 278 | 61 | 22 | 1 month | Not informed | Poor physical performance and pain were significantly associated with fear of falling |
| Cedraschi et al., (2016) (25) | Both | ≥65 | Was conducted in five Swiss cantons: two French- speaking ones, Geneva and Wallis, two German-speaking ones, Bern and Basel, and the only Italian-speaking one, i.e. Ticino. | Swiss | A scale assessing LBP for use in prevalence studies | 3042 | 889 | 29 | Last month | Standardized Back Pain Definition | Not informed |
| Total | 73,439 | 18,942 | |||||||||
Subtitle: LBP = Low back pain;
= period prevalence investigate;
F = Female; M = Male.
Table 3. Characteristics of the studies found in the systematic review with prevalence period not informed.
| Author/Year | Gender | Age (years) | Population | Country | Instrument | Sample Size | Sample with LBP | Prevalence (%) | Prevalence period* | LBP Definition | Functional disability |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Liu-Ambrose et al., (2002) (47) | Female | 69.4 | Identified were from a computerized database of community-dwelling women who had been referred for bone densitometry at the BC Women’s Hospital and Health Centre Osteoporosis Program between 1996 and 2000. | Canada | Oswestry Questionnaire | 93 | 70 | 75 | Not informed | Not informed | Not informed |
| Kobuke et al., (2009) (48) | Both | ≥65 | Elderly residentes in the Nagasaki. | Japan | Itself questionnaire | 323 | 127 | M 32.8 F 43.0 |
Not informed | Not informed | Back pain were associated with chair stand difficulty |
| Peng et al., (2009) (49) | Male | 80.9±5.4 | Data of the Longitudinal Older Veterans (LOVE) study. | Taiwan | Itself questionnaire | 574 | 153 | 40.5 | Not informed | Not informed | Subjects with pain were physically independence 92.2% |
| Baek et al., (2010) (50) | Both | 76.4±5.7 | Elderly residents of the Seongnam. | South Korea | Oswestry Questionnaire | 1118 | 686 | Total 72 M 58.4 F 82.2 |
Not informed | Not informed | Not informed |
| Barros et al., (2011) (51) | Both | 60-69 | Elderly residentss of the Campinas, São Paulo. | Brazil | Itself questionnaire | 1518 | 652 | 43 | Not informed | Not informed | Not informed |
| Kim et al., (2015) (52) | Female | 75-84 | Residents in the comunnity of the Itabashi, Tokyo. | Japan | Itself questionnaire Grip strength and usual walking speed | 1399 | 399 | 28.5 | Not informed | Not informed | UI was associated with LBP, pain coupled with grip strength, and mobility limitation. |
| Total | 5025 | 2087 |
Subtitle: LBP = Low back pain;
= period prevalence investigate;
F = Female; M = Male; UI = Urinary Incontinence.
An approach regarding complaints of LBP at different moments was found in this systematic review. Eight studies (18-25) addressed acute LBP prevalence, and 21 studies (26-46) addressed chronic LBP prevalence; however, six studies (47-52) did not specify the prevalence period investigated.
Of the 35 original studies, 26 included both sexes. The age range was from 60 to ≥86 years, and the places where the studies took place included North America (USA and Canada), South America (Brazil), Europe (Spain, Sweden, Italy, Denmark and Switzerland), Asia (Japan, South Korea, Bangladesh, Taiwan, and China), and Africa (Nigeria).
Regarding data collection instruments, a customized questionnaire was employed in 20 studies (18-22,24,26-28,32,35,43-45), and a Roland-Morris questionnaire was employed in four studies (31,36-38). The Oswestry questionnaire (47,50), the Visual Analog Scale (31,38), the Face Pain Scale (23,41), the Numeric Scale (40,41), the Physical Activity Scale of the Elderly (33,36), and the Nordic questionnaire (39,45) were employed in two studies each. The following instruments were used in only one study each: the Lawton questionnaire (29), the McGill questionnaire (36), the Quebec Pain Disability Scale (35), the Graded Chronic Pain Scale (42), the North American Spine Society Questionnaires for Back and Neck Pain (34), the Katz index (23) and medical records from a physiotherapy clinic school at the State University of Southwestern Bahia, Brazil (32).
Functional disability due to LBP was investigated in 60% of the studies, and LBP was shown to hinder functionality (18,20,21,23,27,28,30,37,39) and result in major dependence for daily living activities (24,29,48,38,52) and physical capacity (30,33,36,24,46).
The methodological quality assessment (Table 4) ranged from four to ten points. Four studies (19,25,28,42) presented methodological quality without risk of bias, and eleven studies (20,23,27,29,34,38-40,43,) were classified as a low risk of bias. Seventeen (18,21,22,24,26,30,31,33,35-37,41,45-47,51,52) were classified as having a medium risk of bias, and three studies (32,48,49) presented a high risk of bias, with scores lower than seven.
Table 4. Evaluation of the methodological quality of included studies in the systematic review.
| Author/Year | 1. Was the study’s target population a close representation of the national population in relation to relevant variables? | 2. Was the sampling frame a true or close representation of the target population? | 3. Was some form of random selection used to select the sample, OR was a census undertaken? | 4. Was the likelihood of nonresponse bias minimal? | 5. Were data collected directly from the subjects? | 6. Was an acceptable case definition used in the study? | 7. Was the study instrument that measured the parameter of interest shown to have validity and reliability? | 8. Was the same mode of data collection used for all subjects? | 9. Was the length of the shortest prevalence period for the parameter of interest appropriate? | 10. Were the numerator and denominator for the parameter of interest appropriate? | 11. Summary item on the overall risk of study bias |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hartvigsen et al., (2003) (18) | N | Y | NI | Y | Y | Y | Y | Y | Y | Y | 8 |
| Blay et al., (2007) (19) | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Meyer et al., (2007) (20) | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | 9 |
| Lima et al., (2009) (21) | Y | Y | Y | Y | Y | Y | N | Y | NI | Y | 8 |
| Rana et al., (2009) (22) | N | Y | N | Y | Y | Y | N | Y | Y | Y | 7 |
| Gálvez-Barrón et al., (2015) (23) | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | 9 |
| Tomita et al., (2015) (24) | N | Y | N | Y | Y | Y | N | Y | Y | Y | 7 |
| Cedraschi et al., (2016) (25) | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Lavsky-Shulan et al., (1985) (26) | N | Y | N | Y | Y | Y | Y | Y | NI | Y | 7 |
| Weiner et al., (2003) (27) | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 |
| Cecchi et al., (2006) (28) | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Dellaroza et al., (2008) (29) | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 |
| Hicks et al., (2008) (30) | N | Y | Y | NI | N | Y | Y | Y | Y | Y | 7 |
| Kovacs et al., (2008) (31) | N | Y | N | Y | Y | Y | Y | Y | Y | Y | 8 |
| Dos Reis et al., (2008) (32) | N | Y | N | N | Y | N | NI | Y | NI | Y | 4 |
| Woo et al., (2009) (33) | N | Y | N | Y | Y | Y | N | Y | Y | Y | 7 |
| Holton et al., (2011) (34) | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 |
| Abegunde & Owaje, (2013) (35) | N | Y | Y | Y | Y | Y | Y | Y | NI | Y | 8 |
| Exarchou et al., (2013) (36) | Y | Y | N | Y | N | Y | N | Y | Y | Y | 7 |
| Figueiredo et al., (2013) (37) | N | Y | N | NI | Y | Y | Y | Y | Y | Y | 7 |
| Ghanei et al., (2014) (38) | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 |
| Palma et al., (2014) (39) | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 |
| Pereira et al., (2014) (40) | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 |
| Santos et al., (2015) (41) | N | Y | N | Y | Y | Y | Y | Y | Y | Y | 8 |
| Scherer et al., (2016) (42) | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Kherad et al., (2016) (43) | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | 9 |
| Marshall et al., (2016) (44) | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | 9 |
| Quintino et al., (2017) (45) | N | Y | Y | N | Y | Y | Y | Y | Y | Y | 8 |
| Machado et al., (2018) (46) | N | Y | Y | N | Y | Y | Y | Y | Y | Y | 8 |
| Liu-Ambrose et al., (2002) (47) | N | Y | N | Y | Y | Y | Y | Y | NI | Y | 7 |
| Kobuke et al., (2009) (48) | N | N | N | Y | Y | Y | N | Y | NI | Y | 5 |
| Peng et al., (2009) (49) | Y | Y | N | Y | Y | Y | N | Y | NI | Y | 6 |
| Baek et al., (2010) (50) | Y | Y | Y | Y | Y | Y | Y | Y | NI | Y | 9 |
| Barros et al., (2011) (51) | Y | Y | Y | Y | Y | Y | N | Y | NI | Y | 8 |
| Kim et al., (2015) (52) | Y | Y | Y | Y | Y | Y | N | Y | NI | Y | 8 |
Subtitle: N = No = 0; Y = Yes = 1; NI = Not informed.
DISCUSSION
Among all chronic pain problems and spinal pain conditions, LBP is the most common public health, economic, and social problem. Moreover, LBP affects the population indiscriminately worldwide (53). Nevertheless, the prevalence of LBP varies according to the definitions used and the population studied (9).
This systematic review summarizes the international literature data on the prevalence of LBP in the elderly population. The results indicate a high prevalence of LBP among elderly individuals, ranging from 21.7 to 75%. Furthermore, the prevalence of LBP is high in developed countries such as Canada (18) (75%), the United States (44) (67%), Sweden (43) (49%), China (33) (39.2%) and Japan (48) (32%). LBP occurs in 43% of both men and women, differing from the mean global prevalence, which was 31% (22). This finding was also true in developing countries such as Brazil, where the prevalence was 33.6% to 68.3%. In other Brazilian studies (37,39), the small samples studied may have contributed to a high prevalence, and the samples may not have been representative of the study population.
Only one systematic review performed in 1999, including only developed countries in the Northern Hemisphere, evaluated the prevalence of LBP among elderly individuals. This study also showed a prevalence ranging from 12.8% to 51% (age above 65 years), based on the prevalence of punctual pain, pain in the last six months and pain in the last year (13). Another systematic review of the prevalence of spinal pain among elderly individuals, including studies conducted in developed countries, presented a 20% prevalence (≥60 years) (54). However, the study did not separately analyze elderly individuals with LBP.
It was found that 46.6% of the studies included in the review defined a six-month period of LBP in the last year as chronic LBP; this definition was in accordance with one of the diagnostic criteria for research on chronic noncancer pain recommended by the taxonomy of the “International Association for Study of Pain” (55).
The most recent assessment of the global prevalence of punctual LBP comprising all age groups estimated that pain is an emerging problem in the elderly population that requires monitoring (56), especially in developing countries. Furthermore, another study reported that LBP is more frequent and is characterized by longer episodes in elderly individuals than in young adults (57).
The proportion of elderly individuals (60 years or more) in almost all developed and developing countries worldwide is increasing faster than any other age group (58). In a world report on aging and health by the World Health Organization (WHO), it was stated that the world population aged over 60 years will increase from the current 841 million to two billion by 2050, turning chronic diseases and the welfare of older people into new challenges for global public health (58,59).
Fejer et al. (60) reported that the prevalence of LBP increases until 80 years of age and then decreases slightly, except among women, who report a greater frequency of LBP than men. There are several possible explanations for the decline in pain with advancing age (from 80 years on). Not only is there an increase in life expectancy, there is also an increase in the incidence of chronic noncommunicable diseases, which leads to increased morbidity and disability (61). Pain is experience by elderly individuals due to their fragility, threatening their safety, autonomy, and independence. Pain often prevents them from performing daily life activities, as well as limits their social interactions, which are situations that considerably diminish their quality of life (62).
Consequently, pain among elderly individuals should be considered as a continuation of pain from previous years (63), while accepting that pain among the elderly population occurs as a part of aging (64). In other words, pain becomes a natural part of life; therefore, it becomes less disturbing or it is simply ignored. Finally, a decline in the prevalence of pain in the elderly population may be explained by a phenomenon of “survival of the fittest” (65).
Another aspect that can be highlighted in this review is the greater prevalence among females observed in various studies (22,23,33,39,42,47,48); the prevalence ranged from 35% to 82%. These findings confirm that women outlive men, despite suffering longer exposure to risk factors; women live with more comorbidities and experience the chronicity of clinical conditions - a phenomenon called “feminization” of old age (66). A recent systematic review showed that the prevalence of LBP seemed higher among middle-aged adults and women (56). A biopsychosocial model of chronic pain attributes sexual differences in pain to interactions between biological, psychological, and sociocultural factors (67,68). A greater sensitivity to pain among women may also partially explain higher reports of pain by women than by men (69).
Although most LBP is self-limiting, begins to improve after a few days and resolves within a month (70), some patients are susceptible to chronic LBP that leads to significant disability. Age is a well-known risk factor for chronic LBP (71), and other factors may perpetuate LBP in older adults. The understanding of these factors can help identify high-risk patients and improve their LBP management. Since older adults usually face both age-related physical and psychosocial issues, comprehensive assessments and treatments are needed to effectively manage LBP in the elderly population.
Methodological limitations, when related to external validity relevant to criterion (1) (representatives of the study sample in relation to the national population to allow for the generalizability of results), were not found in 22 studies (18,22,24,27,29,31-34,36,37,40,41,43-48). The researchers involved in these studies conducted data collection in regions or municipalities without nationally representing the target population, which would not occur if there were core studies or multicentric groups to produce representative samples. Random selection was used in 18 studies (19-21,22,24,27,29,34,35,37,41,51,53). In the remaining studies, convenience sampling was the technique of choice to obtain quick, low-cost information (58). Regarding internal validity, which was involved in this criterion (7), 53.3% of the studies (18-22,26-30,33,35,37,40,42,48,49,51,52) used their own questionnaires. These studies only questioned whether the individuals had LBP or not. Nonetheless, the lack of standardization of instruments used in data collection may have influenced the results (35).
We attempted to minimize these limitations by evaluating the methodological criteria of the eligible studies, but unlike other reviews (72,73), we did not establish a cut-off point based on this methodological evaluation to include the studies in this review.
Based on previous findings and the most recent global prevalence of occasional LBP, including all age groups (i.e., 9.4%, 95% CI 9 to 9.8) (54), this review estimates that LBP is a health problem in the elderly population. The adequate epidemiological description of LBP in the elderly can improve the distribution of resources for the clinical management of this condition, especially in developing countries (58,69,74). Data show that both the number and proportion of individuals aged older than 65 years have been increasing in most western populations (60). It is believed that LBP will lead to even greater health care costs in the future (58).
This study helped to reveal the main shortcomings of the current studies on the prevalence of LBP in the elderly population worldwide. These findings can guide actions to produce robust evidence on this topic in future studies and in clinical practice. We strongly recommend the performance of further robust studies with low risk of bias and consistent LBP definitions.
Limitations
The limitation of the study was the different definitions of LBP used in the studies, which may lead to a misunderstanding about the actual location of LBP. In addition, a uniform definition of LBP for the purpose of LBP epidemiological studies would significantly enhance our ability to compare and pool results across studies.
CONCLUSIONS
This systematic review indicates a high prevalence of LBP in the elderly population and that functional disability affects factors that are important for independence. However, the investigated studies present diverse methodologies, and different definitions of LBP were used, suggesting that more research should be carried out with scientific accuracy, methodological quality and low risk of bias to contribute towards developing preventive actions for the elderly population affected by LBP. Finally, such studies will provide information to devise public policy plans by health managers and professionals.
APPENDIX
Search strategies data bases
MEDLINE
tw:(low back pain AND prevalence AND elderly) AND (instance:“regional“) AND (db:(“MEDLINE“) AND la:(“en” OR “pt“) AND year_cluster:(“2017” OR “2018” OR “2014” OR “2013” OR “2015” OR “2012” OR “2009” OR “2011” OR “2006” OR “2010” OR “2005” OR “2007” OR “2008” OR “2016” OR “2004” OR “2002” OR “2003” OR “2001” OR “2000” OR “1998” OR “1999” OR “1997” OR “1995” OR “1993” OR “1994” OR “1996” OR “1991” OR “1987” OR “1990” OR “1992” OR “1989” OR “1988” OR “1985“) AND type:(“article“))
EMBASE
“low back pain” OR “back pain” OR “lower back pain” AND prevalence AND elderly#1 AND (1980:py OR 1984:py OR 1985:py OR 1986:py OR 1987:py OR 1988:py OR 1989:py OR 1990:py OR 1991:py OR 1992:py OR 1993:py OR 1994:py OR 1995:py OR 1996:py OR 1997:py OR 1998:py OR 1999:py OR 2000:py OR 2001:py OR 2002:py OR 2003:py OR 2004:py OR 2005:py OR 2006:py OR 2007:py OR 2008:py OR 2009:py OR 2010:py OR 2011:py OR 2012:py OR 2013:py OR 2014:py OR 2015:py OR 2016:py OR 2017:py OR 2018:py)
SCOPUS
TITLE-ABS-KEY(“low back pain” OR “back pain” OR “lower back pain” ) AND TITLE-ABS-KEY(prevalence) AND TITLE-ABS-KEY(elderly) AND (LIMIT-TO (PUBYEAR,2018) OR LIMIT-TO (PUBYEAR,2017) OR (PUBYEAR,2016) OR LIMIT-TO (PUBYEAR,2015) LIMIT-TO (PUBYEAR,2014) OR LIMIT-TO (PUBYEAR,2013) OR LIMIT-TO (PUBYEAR,2012) OR LIMIT-TO (PUBYEAR,2011) OR LIMIT-TO (PUBYEAR,2010) OR LIMIT-TO (PUBYEAR,2009) OR LIMIT-TO (PUBYEAR,2008) OR LIMIT-TO (PUBYEAR,2007) OR LIMIT-TO (PUBYEAR,2006) OR LIMIT-TO (PUBYEAR,2005) OR LIMIT-TO (PUBYEAR,2004) OR LIMIT-TO (PUBYEAR,2003) OR LIMIT-TO (PUBYEAR,2002) OR LIMIT-TO (PUBYEAR,2001) OR LIMIT-TO (PUBYEAR,2000) OR LIMIT-TO (PUBYEAR,1999) OR LIMIT-TO (PUBYEAR,1998) OR LIMIT-TO (PUBYEAR,1997) OR LIMIT-TO (PUBYEAR,1996) OR LIMIT-TO (PUBYEAR,1995) OR LIMIT-TO (PUBYEAR,1994) OR LIMIT-TO (PUBYEAR,1993) OR LIMIT-TO (PUBYEAR,1992) OR LIMIT-TO (PUBYEAR,1990) OR LIMIT-TO (PUBYEAR,1989) OR LIMIT-TO (PUBYEAR,1988) OR LIMIT-TO (PUBYEAR,1985) OR LIMIT-TO (PUBYEAR,1980) )
SCIELO (http://search.scielo.org/)
low back pain AND prevalence AND elderly
dor lombar OR low back pain AND prevalência OR prevalence AND idoso OR elderly AND la:(“pt” OR “en“) AND year_cluster:(“2015” OR “2017” OR “2018” OR “2011” OR “2013” OR “2014” OR “2016” OR “2012” OR “2010” OR “2006” OR “2007” OR “2009” OR “2001” OR “2004” OR “2008” OR “1997” OR “2003” OR “2005“)
LILACS
“dor lombar” OR “low back pain” AND prevalência OR prevalence AND idoso OR elderly
WEB OF SCIENCE
(low back pain) AND Tópico: (prevalence) AND Tópico: (elderly) Refinado por: Idiomas: (ENGLISH OR PORTUGUESE) Tempo estipulado: 1985-2018. ĺndices: SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, ESCI.
.
AUTHOR CONTRIBUTIONS
Souza IMB designed the study, edited the manuscript and critically reviewed its final version. Sakaguchi TF acquired some of the data. Yuan SLK, Espirito-Santo AS and Matsutani LA critically reviewed the final version of the manuscript. Pereira CAB conducted the statistical analysis. Marques AP performed the data collection and analysis, and critically reviewed the final version of the manuscript. All authors read and approved the final version of the manuscript.
ACKNOWLEDGMENTS
The authors would like to thank all collaborators in the Laboratory of Professor PhD Marques for their collaboration and support since 2016.
Footnotes
No potential conflict of interest was reported.
REFERENCES
- 1.Rapoport J, Jacobs P, Bell NR, Klarenbach S. Refining the measurement of the economic burden of chronic diseases in Canada. Chronic Dis Can. 2004;25(1):13–21. [PubMed] [Google Scholar]
- 2.Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, et al. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006;15(Suppl 2):S192–300. doi: 10.1007/s00586-006-1072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martins MR, Foss MH, Santos Junior R, Zancheta M, Pires IC, Cunha AMR, et al. A eficácia da conduta do grupo de postura em pacientes com lombalgia crônica. Rev Dor. 2010;11(2):116–21. [Google Scholar]
- 4.Silva MC, Fassa AG, Valle NC. [Chronic low back pain in a Southern Brazilian adult population: prevalence and associated factors] Cad Saude Publica. 2004;20(2):377–85. doi: 10.1590/S0102-311X2004000200005. [DOI] [PubMed] [Google Scholar]
- 5.Institucionais IT. Programa Nacional de Promoção da Atividade Física “Agita Brasil”: Atividade física e sua contribuição para a qualidade de vida. Rev Saude Publica. 2002;36(2):254–6. doi: 10.1590/S0034-89102002000200022. [DOI] [PubMed] [Google Scholar]
- 6.Andersson GB. Epidemiological features of chronic low-back pain. Lancet. 1999;354(9178):581–5. doi: 10.1016/S0140-6736(99)01312-4. [DOI] [PubMed] [Google Scholar]
- 7.Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006;88(Suppl 2):21–4. doi: 10.2106/JBJS.E.01273. [DOI] [PubMed] [Google Scholar]
- 8.Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, et al. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169(3):251–8. doi: 10.1001/archinternmed.2008.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81(9):646–56. [PMC free article] [PubMed] [Google Scholar]
- 10.Edmond SL, Felson DT. Function and back symptoms in older adults. J Am Geriatr Soc. 2003;51(12):1702–9. doi: 10.1046/j.1532-5415.2003.51553.x. [DOI] [PubMed] [Google Scholar]
- 11.Cooper JK, Kohlmann T. Factors associated with health status of older Americans. Age Ageing. 2001;30(6):495–501. doi: 10.1093/ageing/30.6.495. [DOI] [PubMed] [Google Scholar]
- 12.Teixeira MJ, Teixeira WGJ, Santos FPS, Andrade DCA, Bezerra SL, Figueiró JB, et al. Epidemiologia clínica da dor músculo-esquelética. Rev Med. 2001;80(ed. esp. pt.1):1–21. [Google Scholar]
- 13.Bressler HB, Keyes WJ, Rochon PA, Badley E. The prevalence of low back pain in the elderly. A systematic review of the literature. Spine. 1999;24(17):1813–9. doi: 10.1097/00007632-199909010-00011. [DOI] [PubMed] [Google Scholar]
- 14.Gallagher RM. Low back pain, health status, and quality of life in older adults: challenge and opportunity. Pain Med. 2003;4(4):305–7. doi: 10.1111/j.1526-4637.2003.03049.x. [DOI] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG. Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9, W64. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization . Active Ageing: A Policy Framework. A Contribution of the World Health Organization to the Second United Nations World Assembly on Ageing. https://extranet.who.int/agefriendlyworld/wp-content/uploads/2014/06/WHO-Active-Ageing-Framework.pdf Available from: [Accessed Oct, 2019] [Google Scholar]
- 17.Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–9. doi: 10.1016/j.jclinepi.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 18.Hartvigsen J, Christensen K, Frederiksen H. Back pain remains a common symptom in old age. a population-based study of 4486 Danish twins aged 70-102. Eur Spine J. 2003;12(5):528–34. doi: 10.1007/s00586-003-0542-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blay SL, Andreoli SB, Gastal FL. Chronic painful physical conditions, disturbed sleep and psychiatric morbidity: results from an elderly survey. Ann Clin Psychiatry. 2007;19(3):169–74. doi: 10.1080/10401230701468099. [DOI] [PubMed] [Google Scholar]
- 20.Meyer T, Cooper J, Raspe H. Disabling low back pain and depressive symptoms in the community-dwelling elderly: a prospective study. Spine. 2007;32(21):2380–6. doi: 10.1097/BRS.0b013e3181557955. [DOI] [PubMed] [Google Scholar]
- 21.Lima MG, Barros MB, César CL, Goldbaum M, Carandina L, Ciconelli RM. Impact of chronic disease on quality of life among the elderly in the state of São Paulo, Brazil: a population-based study. Rev Panam Salud Publ. 2009;25(4):314–21. doi: 10.1590/S1020-49892009000400005. [DOI] [PubMed] [Google Scholar]
- 22.Rana AM, Wahlin A, Streatfield PK, Kabir ZN. Association of bone and joint diseases with health-related quality of life among older people: a population-based cross-sectional study in rural Bangladesh. Ageing Soc. 2009;29(05):727–43. doi: 10.1017/S0144686X09008411. [DOI] [Google Scholar]
- 23.Gálvez-Barrón C, Narvaiza L, Dapena MD, Macho O, Rodríguez-Molinero A. Prevalence and treatment of pain in non-institutionalized very old population: transversal study at national level. Aging Clin Exp Res. 2016;28(2):347–53. doi: 10.1007/s40520-015-0387-3. [DOI] [PubMed] [Google Scholar]
- 24.Tomita Y, Arima K, Kanagae M, Okabe T, Mizukami S, Nishimura T, et al. Association of Physical Performance and Pain With Fear of Falling Among Community-Dwelling Japanese Women Aged 65 Years and Older. Medicine. 2015;94(35):e1449. doi: 10.1097/MD.0000000000001449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cedraschi C, Luthy C, Allaz AF, Herrmann FR, Ludwig C. Low back pain and health-related quality of life in community-dwelling older adults. Eur Spine J. 2016;25(9):2822–32. doi: 10.1007/s00586-016-4483-7. [DOI] [PubMed] [Google Scholar]
- 26.Lavsky-Shulan M, Wallace RB, Kohout FJ, Lemke JH, Morris MC, Smith IM. Prevalence and functional correlates of low back pain in the elderly: the Iowa 65+ Rural Health Study. J Am Geriatr Soc. 1985;33(1):23–8. doi: 10.1111/j.1532-5415.1985.tb02855.x. [DOI] [PubMed] [Google Scholar]
- 27.Weiner DK, Haggerty CL, Kritchevsky SB, Harris T, Simonsick EM, Nevitt M, et al. How does low back pain impact physical function in independent, well-functioning older adults? Evidence from the Health ABC Cohort and implications for the future. Pain Med. 2003;4(4):311–20. doi: 10.1111/j.1526-4637.2003.03042.x. [DOI] [PubMed] [Google Scholar]
- 28.Cecchi F, Debolini P, Lova RM, Macchi C, Bandinelli S, Bartali B, et al. Epidemiology of back pain in a representative cohort of Italian persons 65 years of age and older: the InCHIANTI study. Spine. 2006;31(10):1149–55. doi: 10.1097/01.brs.0000216606.24142.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dellaroza MS, Pimenta CA, Duarte YA, Lebrão ML. [Chronic pain among elderly residents in São Paulo, Brazil: prevalence, characteristics, and association with functional capacity and mobility (SABE Study)] Cad Saude Publica. 2013;29(2):325–34. doi: 10.1590/S0102-311X2013000200019. [DOI] [PubMed] [Google Scholar]
- 30.Hicks GE, Gaines JM, Shardell M, Simonsick EM. Associations of back and leg pain with health status and functional capacity of older adults: findings from the retirement community back pain study. Arthritis Rheum. 2008;59(9):1306–13. doi: 10.1002/art.24006. [DOI] [PubMed] [Google Scholar]
- 31.Kovacs F, Noguera J, Abraira V, Royuela A, Cano A, Gil del Real MT, et al. The influence of psychological factors on low back pain-related disability in community dwelling older persons. Pain Med. 2008;9(7):871–80. doi: 10.1111/j.1526-4637.2008.00518.x. [DOI] [PubMed] [Google Scholar]
- 32.dos Reis LA, Mascarenhas CH, Marinho Filho LE, Borges PS. Lombalgia na terceira idade: distribuição e prevalência na Clínica Escola de Fisioterapia da Universidade Estadual do Sudoeste da Bahia. Rev Bras Geriatr Gerontol. 2008;11(1):93–103. doi: 10.1590/1809-9823.2008.11019. [DOI] [Google Scholar]
- 33.Woo J, Leung J, Lau E. Prevalence and correlates of musculoskeletal pain in Chinese elderly and the impact on 4-year physical function and quality of life. Public Health. 2009;123(8):549–56. doi: 10.1016/j.puhe.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 34.Holton KF, Denard PJ, Yoo JU, Kado DM, Barrett-Connor E, Marshall LM, et al.editors., editors. Diffuse idiopathic skeletal hyperostosis and its relation to back pain among older men: the MrOS Study. Semin Arthritis Rheum. 2011;41(2):131–8. doi: 10.1016/j.semarthrit.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abegunde KA, Owoaje ET. Health problems and associated risk factors in selected urban and rural elderly population groups of South-West Nigeria. Ann Afr Med. 2013;12(2):90–7. doi: 10.4103/1596-3519.112398. [DOI] [PubMed] [Google Scholar]
- 36.Exarchou S, Redlund-Johnell I, Karlsson M, Mellström D, Ohlsson C, Turesson C, et al. The prevalence of moderate to severe radiographic sacroiliitis and the correlation with health status in elderly Swedish men--the MrOS study. BMC Musculoskelet Disord. 2013;14:352. doi: 10.1186/1471-2474-14-352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Figueiredo VF, Pereira LS, Ferreira PH, Pereira AM, Amorim JS. Incapacidade funcional, sintomas depressivos e dor lombar em idosos. Fisioter Mov. 2013;26(3):549–57. doi: 10.1590/S0103-51502013000300008. [DOI] [Google Scholar]
- 38.Ghanei I, Rosengren BE, Hasserius R, Nilsson JÅ, Mellström D, Ohlsson C, et al. The prevalence and severity of low back pain and associated symptoms in 3,009 old men. Eur Spine J. 2014;23(4):814–20. doi: 10.1007/s00586-013-3139-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Palma R, de Conti MH, Quintino NM, Gatti MA, Simeão SF, de Vitta A. Functional capacity and its associated factors in the elderly with low back pain. Acta Ortop Bras. 2014;22(6):295–9. doi: 10.1590/1413-78522014220600890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pereira LV, de Vasconcelos PP, Souza LA, Pereira Gde A, Nakatani AY, Bachion MM. Prevalence and intensity of chronic pain and self-perceived health among elderly people: a population-based study. Rev Lat Am Enfermagem. 2014;22(4):662–9. doi: 10.1590/0104-1169.3591.2465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Santos FC, Moraes NS, Pastore A, Cendoroglo MS. Chronic pain in long-lived elderly: prevalence, characteristics, measurements and correlation with serum vitamin D level. Revista Dor. 2015;16(3):171–5. doi: 10.5935/1806-0013.20150034. [DOI] [Google Scholar]
- 42.Scherer M, Hansen H, Gensichen J, Mergenthal K, Riedel-Heller S, Weyerer S, et al. Association between multimorbidity patterns and chronic pain in elderly primary care patients: a cross-sectional observational study. BMC Fam Pract. 2016;17:68. doi: 10.1186/s12875-016-0468-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kherad M, Rosengren BE, Hasserius R, Nilsson JA, Redlund-Johnell I, Ohlsson C, et al. Age Ageing. 2017;8;46(1):64–71. doi: 10.1093/ageing/afw152. [DOI] [PubMed] [Google Scholar]
- 44.Marshall LM, Litwack-Harrison S, Makris UE, Kado DM, Cawthon PM, Deyo RA, et al. A Prospective Study of Back Pain and Risk of Falls Among Older Community-dwelling Men. J Gerontol A Biol Sci Med Sci. 2017;72(9):1264–9. doi: 10.1097/AJP.0000000000000564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Quintino NM, De Conti MHS, Palma R, Gatti MAN, Simeão SFAP, Vitta A. Prevalence and factors associated with low back pain in elderly registered in the Family Health Strategy. Fisioter Mov. 2017;30(2):367–77. doi: 10.1590/1980-5918.030.002.ao17. [DOI] [Google Scholar]
- 46.Machado LAC, Viana JU, da Silva SLA, Couto FGP, Mendes LP, Ferreira PH, et al. Correlates of a Recent History of Disabling Low Back Pain in Community-dwellin Older Persons: The Pain in the Elderly (PAINEL) study. Clin J Pain. 2018;34(6):515–24. doi: 10.1097/AJP.0000000000000564. [DOI] [PubMed] [Google Scholar]
- 47.Liu-Ambrose T, Eng JJ, Khan KM, Mallinson A, Carter ND, McKay HA. The influence of back pain on balance and functional mobility in 65- to 75-year-old women with osteoporosis. Osteoporos Int. 2002;13(11):868–73. doi: 10.1007/s001980200119. [DOI] [PubMed] [Google Scholar]
- 48.Kobuke Y, Abe Y, Ye Z, Honda S, Tomita M, Osaki M, et al. Association of Age, Obesity, Joint Pain, and Chewing Ability with Chair Stand Difficulty among Community-dwelling Elderly People in Nagasaki, Japan. Acta Med Nagasaki. 2009;53:65–8. doi: 10.11343/amn.53.65. [DOI] [Google Scholar]
- 49.Peng LN, Lin MH, Lai HY, Hwang SJ, Chen LK, Lan CF. Pain and health-care utilization among older men in a veterans care home. Arch Gerontol Geriatr. 2009;49(Suppl 2):S13–6. doi: 10.1016/S0167-4943(09)70006-8. [DOI] [PubMed] [Google Scholar]
- 50.Baek SR, Lim JY, Lim JY, Park JH, Lee JJ, Lee SB, et al. Prevalence of musculoskeletal pain in an elderly Korean population: results from the Korean Longitudinal Study on Health and Aging (KLoSHA) Arch Gerontol Geriatr. 2010;51(3):e46–51. doi: 10.1016/j.archger.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 51.Barros MB, Francisco PM, Lima MG, César CL. Social inequalities in health among the elderly. Cad Saude Publica. 2011;27(Suppl 2):S198–208. doi: 10.1590/S0102-311X2011001400008. [DOI] [PubMed] [Google Scholar]
- 52.Kim H, Yoshida H, Hu X, Saito K, Yoshida Y, Kim M, et al. Association between self-reported urinary incontinence and musculoskeletal conditions in community-dwelling elderly women: a cross-sectional study. Neurourol Urodyn. 2015;34(4):322–6. doi: 10.1002/nau.22567. [DOI] [PubMed] [Google Scholar]
- 53.Manchikanti L, Singh V, Datta S, Cohen SP, Hirsch JA. American Society of Interventional Pain Physicians Comprehensive review of epidemiology, scope, and impact of spinal pain. Pain Physician. 2009;12(4):E35–70. [PubMed] [Google Scholar]
- 54.Macfarlane G, Jones G, McBeth J. Wall and Melzack’s textbook of pain. 2005. Epidemiology of pain. [Google Scholar]
- 55.[No authors listed] Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl. 1986;3:S1–226. [PubMed] [Google Scholar]
- 56.Dionne CE, Dunn KM, Croft PR. Does back pain prevalence really decrease with increasing age? A systematic review. Age Ageing. 2006;35(3):229–34. doi: 10.1093/ageing/afj055. [DOI] [PubMed] [Google Scholar]
- 57.Schillewaert N, Langerak F, Duharnel T. Non probability sampling for WWW surveys: a comparison of methods. J Market Res Soc. 1998;40(4):1–13. doi: 10.1177/147078539804000403. [DOI] [Google Scholar]
- 58.Cassidy JD, Cote P, Carroll LJ, Kristman V. Incidence and course of low back pain episodes in the general population. Spine. 2005;30(24):2817–23. doi: 10.1097/01.brs.0000190448.69091.53. [DOI] [PubMed] [Google Scholar]
- 59.Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73(6):968–74. doi: 10.1136/annrheumdis-2013-204428. [DOI] [PubMed] [Google Scholar]
- 60.Fejer R, Ruhe A. What is the prevalence of musculoskeletal problems in the elderly population in developed countries? A systematic critical literature review. Chiropr Man Therap. 2012;20(1):31. doi: 10.1186/2045-709X-20-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Celich KL, Galon C. Dor crônica em idosos e sua influência nas atividades da vida diária e convivência social. Rev Bras Geriatr Gerontol. 2009;12(3):345–59. doi: 10.1590/1809-9823.2009.00004. [DOI] [Google Scholar]
- 62.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global burden of disease and risk factors. New York: Oxford University Press New York; 2006. [DOI] [Google Scholar]
- 63.Leveille SG, Zhang Y, McMullen W, Kelly-Hayes M, Felson DT. Sex differences in musculoskeletal pain in older adults. Pain. 2005;116(3):332–8. doi: 10.1016/j.pain.2005.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sjogren P, Ekholm O, Peuckmann V, Gronbaek M. Epidemiology of chronic pain in Denmark: an update. Eur J Pain. 2009;13(3):287–92. doi: 10.1016/j.ejpain.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 65.Lima e Costa MF. A saúde dos adultos na Região Metropolitana de Belo Horizonte: um estudo epidemiológico de base populacional. A saúde dos adultos na Região Metropolitana de Belo Horizonte: um estudo epidemiológico de base populacional. UFMG;: FIOCRUZ;; 2004. p. 120p. [Google Scholar]
- 66.Turk DC, Okifuji A. Psychological factors in chronic pain: evolution and revolution. J Consult Clin Psychol. 2002;70(3):678–90. doi: 10.1037/0022-006X.70.3.678. [DOI] [PubMed] [Google Scholar]
- 67.Fillingim RB. Sex, gender and pain: The biopsychosocial model in action XX vs. XY. The International Journal of Sex Differences in the Study of Health, Disease and Aging. 2003;1:98–101. [Google Scholar]
- 68.Rollman GB, Lautenbacher S. Sex differences in musculoskeletal pain. Clin J Pain. 2001;17(1):20–4. doi: 10.1097/00002508-200103000-00004. [DOI] [PubMed] [Google Scholar]
- 69.Makris UE, Fraenkel L, Han L, Leo-Summers L, Gill TM. Epidemiology of restricting back pain in community-living older persons. J Am Geriatr Soc. 2011;59(4):610–4. doi: 10.1111/j.1532-5415.2011.03329.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Klineberg E, Mazanec D, Orr D, Demicco R, Bell G, McLain R. Masquerade: medical causes of back pain. Cleve Clin J Med. 2007;74(12):905–13. doi: 10.3949/ccjm.74.12.905. [DOI] [PubMed] [Google Scholar]
- 72.Kim W, Jin YS, Lee CS, Hwang CJ, Lee SY, Chung SG, et al. Relationship between the type and amount of physical activity and low back pain in Koreans aged 50 years and older. PM R. 2014;6(10):893–9. doi: 10.1016/j.pmrj.2014.04.009. [DOI] [PubMed] [Google Scholar]
- 73.Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64(6):2028–37. doi: 10.1002/art.34347. [DOI] [PubMed] [Google Scholar]
- 74.Ferreira ML, Machado G, Latimer J, Maher C, Ferreira PH, Smeets RJ. Factors defining care-seeking in low back pain: a meta-analysis of population based surveys. Eur J Pain. 2010;14(7):747.e1–7. doi: 10.1016/j.ejpain.2009.11.005. [DOI] [PubMed] [Google Scholar]