Progressive multifocal leukoencephalopathy (PML) is a devastating demyelinating disease of the CNS, which develops almost exclusively in immunocompromised patients and is caused by JC virus (JCV), a common polyomavirus.1 So far, treatment efficacy is only modest if the compromised immune system cannot be restored.2–4 A potential treatment target is the programmed cell death protein 1 (PD-1) whose expression on CD4+ and CD8+ T lymphocytes has been shown to be elevated in patients with PML. Moreover, blocking of the PD-1 receptor resulted in increased JCV-specific T-cell immune response in a subgroup of patients with PML.5 Recently, pembrolizumab, a humanized monoclonal antibody directed against PD-1, was reported for the first time to be a promising option for PML with treatment responses in 6 of 9 patients.6,7 Here, we describe another patient with PML who did not benefit from treatment with pembrolizumab.
Case report
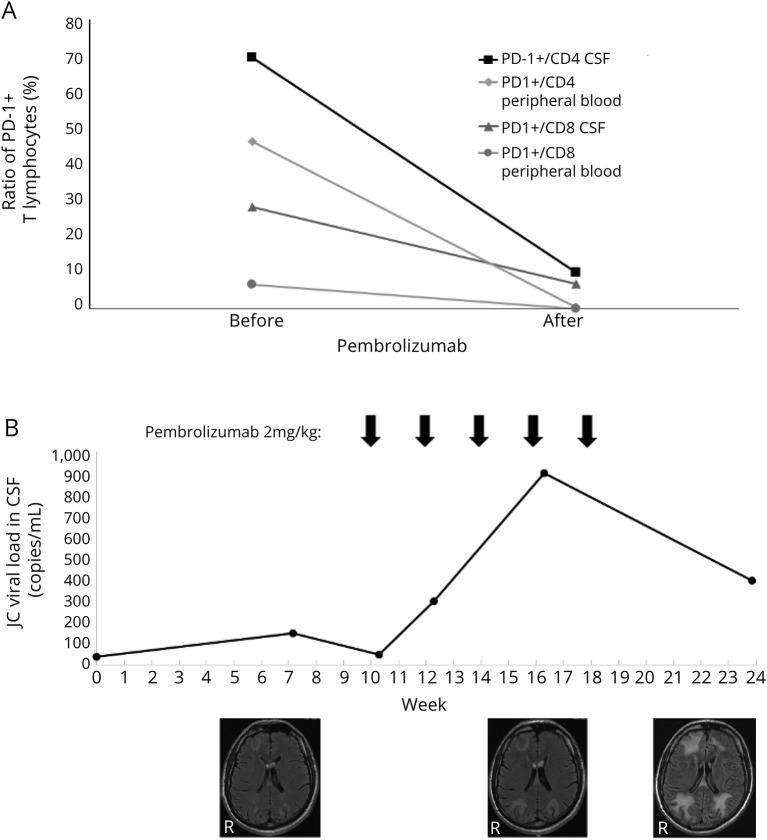
The patient is a 42-year-old man with a primary immunodeficiency (PID) syndrome diagnosed previously as common variable immunodeficiency with low natural killer cells. No mutation in a known PID gene was found by whole-exome sequencing, and he had been under immunoglobulin replacement therapy for several years. Since 2016, his previously normal CD4+ T-cell numbers started to decline, and he progressed to a late-onset combined immunodeficiency reaching 180–150 CD4+ T cells/μL in May 2018 when he developed anopia of the lower right quadrant. In August 2018, a cranial MRI showed a fluid-attenuated inversion recovery hyperintense cortical lesion of the left occipital lobe suggestive of PML. A CSF PCR detected JCV (38 copies/mL), and PML was diagnosed. In October 2018, the patient gave written informed consent to receive off-label treatment with pembrolizumab. The intervention was performed in accordance with the regulations of the Ethics Committee of the Ludwig Maximilians University of Munich. Pembrolizumab was started with 2 mg/kg biweekly. The analysis of PD-1 expression on CD4+ and CD8+ T lymphocytes in CSF and peripheral blood before and after the first course of pembrolizumab by flow cytometry showed reduced detection of PD-1 indicative of effective PD-1 blockade by pembrolizumab (figure, A). However, in the following weeks, the patient developed cortical blindness, memory disturbance, hallucinations, and aggressive behavior, whereas the CSF JC viral load and the PML lesions on MRI increased until administration of the fifth course of pembrolizumab (figure, B). There was no contrast enhancement detected on the cerebral MRIs. In February 2019, the patient developed left-sided hemiparesis and coma. Although a final evaluation had shown a decreasing trend for JC viral load in the CSF, pembrolizumab was stopped as in view of the dramatic clinical deterioration, further treatment did not seem appropriate anymore. The patient finally died under supportive care 2 weeks later.
Figure. PD-1+ T lymphocytes, JC viral load, and MRI lesions in a patient with PML treated with pembrolizumab.
A 42-year-old man with primary immunodeficiency syndrome and PML was treated with pembrolizumab 2 mg/kg for 5 courses. (A) Before and after the first course of pembrolizumab, the percentage of PD-1+ cells of all CD4+ and CD8+ T lymphocytes was analyzed by flow cytometry in CSF and peripheral blood. Pembrolizumab treatment resulted in reduced PD-1 detection on both CD4+ and CD8+ T lymphocytes indicative of effective PD-1 blockade. (B) JC viral load in the CSF was analyzed by PCR. Structural brain damage was evaluated by FLAIR-weighted MRI. Despite the pembrolizumab treatment, the JC viral load in the CSF increased and the lesion load on MRI. A final CSF analysis after the last pembrolizumab course showed a decreasing trend of the JC viral load, but given the increasing MRI lesions and the patient's dramatic clinical deterioration at that time, further treatment did not seem appropriate anymore. FLAIR = fluid-attenuated inversion recovery; PD-1 = programmed cell death protein 1; PML = progressive multifocal leukoencephalopathy.
In summary, in our case, PML treatment with pembrolizumab failed to change the disease outcome. Because responses to pembrolizumab can happen after the fifth biweekly course,7 we do not know whether pembrolizumab is not effective in patients with PID syndromes leading to low CD4+ T cells or whether we have just started our treatment too late to stop the disease in time (previous fatal brain damage). The optimal treatment strategy for these conditions has to be further determined in larger studies.
This case report gives Class IV evidence that pembrolizumab treatment in patients with PML due to PID leading to low CD4+ T cells might not be effective in general or when given late in the disease course.
Appendix. Authors
Footnotes
Study funding
No targeted funding reported.
Disclosure
The authors report no disclosures. Disclosures available: Neurology.org/NN.
References
- 1.Major EO, Yousry TA, Clifford DB. Pathogenesis of progressive multifocal leukoencephalopathy and risks associated with treatments for multiple sclerosis: a decade of lessons learned. Lancet Neurol 2018;17:467–480. [DOI] [PubMed] [Google Scholar]
- 2.Clifford DB, Nath A, Cinque P, et al. A study of mefloquine treatment for progressive multifocal leukoencephalopathy: results and exploration of predictors of PML outcomes. J Neurovirol 2013;19:351–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jamilloux Y, Kerever S, Ferry T, Broussolle C, Honnorat J, Sève P. Treatment of progressive multifocal leukoencephalopathy with mirtazapine. Clin Drug Investig 2016;36:783–789. [DOI] [PubMed] [Google Scholar]
- 4.Marra CM, Rajicic N, Barker DE, et al. A pilot study of cidofovir for progressive multifocal leukoencephalopathy in AIDS. AIDS 2002;16:1791–1797. [DOI] [PubMed] [Google Scholar]
- 5.Tan CS, Bord E, Broge TA Jr, et al. Increased program cell death-1 expression on T lymphocytes of patients with progressive multifocal leukoencephalopathy. J Acquir Immune Defic Syndr 2012;60:244–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cortese I, Muranski P, Enose-Akahata Y, et al. Pembrolizumab treatment for progressive multifocal leukoencephalopathy. N Engl J Med 2019;380:1597–1605. [DOI] [PubMed] [Google Scholar]
- 7.Rauer S, Marks R, Urbach H, et al. Treatment of progressive multifocal leukoencephalopathy with Pembrolizumab. N Engl J Med 2019;380:1676–1677. [DOI] [PubMed] [Google Scholar]