Abstract
Purpose
This study examines the utility of Video-Implemented Script Training for Aphasia (VISTA) for improving speech production and fluency in a Spanish–English bilingual speaker with aphasia.
Method
In this single-subject, multiple-baseline intervention study, VISTA was utilized to facilitate fluent and intelligible speech through training with an audiovisual speech model. Scripts were developed from personalized topics of interest, and training stimuli were tailored for speech rate and linguistic complexity. One trained script per language contained a high proportion of cognates in order to examine the potential for enhancing cross-linguistic transfer. Primary and secondary outcome measures for trained and untrained scripts were percent correct and intelligible scripted words, grammatical errors, speech rate, and total percent intelligibility.
Results
R. C. showed significant improvement in accuracy, intelligibility, and grammaticality of trained scripts. Results revealed cross-linguistic transfer for both languages of treatment. A significantly greater magnitude of cross-language transfer was observed for scripts that were not cognate dense.
Conclusions
VISTA is a viable treatment method for bilingual individuals with aphasia. Cross-linguistic transfer was diminished when incorporating scripts with a high proportion of cognates; however, this may not be true for all bilingual individuals with aphasia and should be explored with additional participants.
The current evidence base regarding the nature and treatment of aphasia caused by stroke pertains largely to monolingual English speakers (for reviews discussing treatment for bilingual speakers, see Faroqi-shah, Frymark, Mullen, & Wang, 2010; Kohnert, 2009; Murray, 2015). This is surprising considering that, in the United States alone, approximately 20% of adults speak a language other than English, with Spanish being the second most spoken and fastest growing language in the nation (LaPointe, 2011; U.S. Census Bureau, 2013, 2014). Furthermore, individuals who are Hispanic or Latinx have increased risk factors for stroke (e.g., cardiovascular disease, diabetes, and hypertension) and comprise a majority of the Spanish-speaking population in the United States. With stroke being the leading cause of aphasia, evidence-based speech and language interventions are needed to successfully treat the growing number of bilingual adults with stroke-induced aphasia.
There is currently a shortage of bilingual speech-language pathologists available to serve the growing bilingual population. In fact, only 7% of all certified speech-language pathologists (~179,000) identify as bilingual (American Speech-Language-Hearing Association, 2017). Because bilingual individuals have greater accessibility to English-only treatment, the majority of existing treatment studies have focused on methods for facilitating cross-linguistic transfer (CLT), 1 in an effort to enhance outcomes in patients' other language(s). Although there is evidence demonstrating the effectiveness of speech-language intervention in bilingual speakers with aphasia (see Faroqi-shah et al., 2010; Kohnert, 2009; Murray, 2015, for reviews), the vast majority of studies have focused on treatment for anomia, and the variables supporting CLT are not well understood. Some studies have shown that the inclusion of cross-linguistic cognates (i.e., translation equivalents that share phonological form across languages) may promote CLT following naming treatment (Kohnert, 2009). Relative to the literature base examining treatment for anomia, the evidence base for approaches targeting fluency and speech production in bilingual speakers is sparse (Caruso & Szabo, 2014), and studies have yet to examine the potential for CLT using these treatment approaches. Therefore, in this study, we sought to provide evidence for a treatment approach targeting speech production and fluency in a bilingual speaker with aphasia. We systematically manipulated the inclusion of cognates to investigate the potential for boosting CLT (see Costa, Santesteban, & Caño, 2005, for a discussion on cognate strengthening). In the following sections, we briefly review studies that have examined cognate facilitation and describe studies that have included cognates as treatment targets for bilingual speakers. We also review the literature reporting approaches intended to improve speech production and fluency in aphasia, as this literature base served as the motivation for the current study.
Cognate Facilitation
Cognate facilitation is described in the literature as a general advantage for cognate versus noncognate items that manifest as shorter latencies and/or higher accuracies across receptive and expressive tasks. With regard to bilingual speakers with aphasia, few studies have attempted to document the effects of cognates on language performance (Ferrand & Humphreys, 1996; Roberts & Deslauriers, 1999; Stadie, Springer, de Bleser, & Burk, 1995), with a handful of studies examining cognate effects following treatment. A number of theoretical models seek to describe bilingual language processing (e.g., Caramazza, 1997; Costa, 2005; Costa, Colomé, & Caramazza, 2000; de Groot, 1992; Dijkstra & van Hell, 2003; Dijkstra & van Heuven, 1998; Green, 1986; Kroll, Bobb, Misra, & Guo, 2008; Kroll & Stewart, 1994; Kroll, Van Hell, Tokowicz, & Green, 2010), and the majority of these models have the potential to explain cognate facilitation, even if cognates are not overtly described within the model (e.g., the revised hierarchical model, Kroll & Stewart, 1994; distributed representational model, e.g., Van Hell & de Groot, 1998; and cascading activation models, e.g., Costa et al., 2000).
Some models that permit spreading activation, for example, describe that bilingual speakers have a shared conceptual store with distinct lexicons (e.g., Costa et al., 2000; Kroll & Stewart, 1994; Kroll et al., 2010). When a concept is accessed, the phonological form of the selected language is activated and the nonselected form also receives some activation. Assuming that selection mechanisms are unimpaired, spreading and cascading activation models provide theoretical support for cognate facilitation. At the same time, nonselective models (i.e., models that describe automatic coactivation in both languages) could account for cognate interference, especially when an integrated lexicon is assumed (e.g., Green's [1986] control, activation, and resource framework). In these models, competition is thought to arise from the shared lexicon wherein each cognate pair is activated simultaneously and suppression or inhibition is needed to correctly select the target word in the target language. Therefore, at a theoretical level, it is plausible that cognates could either facilitate or impede transfer.
Cognates in the Treatment of Bilingual Aphasia
To date, the inclusion of cognates in treatments for bilingual speakers with aphasia has been restricted to naming intervention studies (with picture naming as the primary outcome measure). For example, Kohnert (2004; Treatment 2) reports treatment outcomes in a bilingual man with severe nonfluent aphasia. Naming treatment was provided in two phases, wherein the participant first received treatment in English, followed by treatment in Spanish. Notably, only cognates resulted in cross-language transfer (from the participant's stronger language [Spanish] to the weaker postmorbid language [English]). The intervention consisted of tasks targeting semantics and phonology (e.g., generating semantic associations to target words, writing the names of dictated training words, and confrontation naming with varied levels of cues). Similarly, Goral, Rosas, Conner, Maul, and Obler (2012) implemented a two-phase (Spanish followed by English) treatment with a multilingual speaker with nonfluent aphasia. The treatment approach consisted of semantic and phonemic cueing (e.g., semantic feature analysis, sentence generation, and rapid naming [with phonological cues]). Of the correctly named objects and actions at post-treatment, treated cognates were more likely to be accurately produced in the nontreated languages relative to noncognates.
The facilitative effect of cognate items in treatment is equivocally supported in the literature. For example, Meinzer, Obleser, Flaisch, Eulitz, and Rockstroh (2007) report the effects of treatment administered to a bilingual (German–French) man with chronic aphasia using constraint-induced aphasia therapy (i.e., communicative language games of increasing complexity that required all communication to be constrained to the spoken modality). This individual presented with prominent syntactic and word retrieval difficulties (classified as moderate “amnestic” aphasia, as measured by the Aachen Aphasia Test; Huber, Poeck, & Willmes, 1984). A post hoc examination of cognates revealed no cross-language generalization on an object-naming task administered pre- and post-treatment. Importantly, this individual was provided treatment in German only. Moreover, Kohnert (2009) proposed that the lack of CLT could be attributable to a floor effect, driven by this participant's lack of postmorbid French usage. Another study (Kurland & Falcon, 2011) examined the effects of training cognate versus noncognate items via intensive naming therapy for a Spanish–English bilingual with chronic and severe expressive aphasia. The treatment consisted of tasks including massed naming practice, word/picture matching, categorizing, and semantically cued cloze tasks. Results indicated CLT for noncognates only, leading the authors to conclude that phonological similarity of cognate items resulted in interference that adversely affected performance.
Although there are mixed findings regarding the utility of cognates as a tool to increase CLT in treatment, any gains beyond item-specific, within-language improvements are encouraging. This is especially true given that generalization of gains beyond trained items in the treatment of monolingual aphasia is often limited (e.g., Cherney, Kaye, & Vuuren, 2014; see Wisenburn & Mahoney, 2009, for a review of naming studies). Although the above studies report varying levels of detail regarding participants' speech, language, and cognitive profiles, it is possible that certain key variables might account for the conflicting outcomes regarding CLT and cognates. For example, studies that have observed CLT have treated in at least two languages (consecutively, without a washout period) and have used phonological and semantic approaches to intervention and, although participants' aphasia was severe, they could produce, minimally, single words or phrases in each of their languages. Therefore, possible explanations for the absence of cognate-based CLT might include output that is restricted to stereotyped utterances (especially in a single language) and the use of washout periods between treatment phases (i.e., Kurland & Falcon, 2011). Transfer of cognates might also be hindered by the type of intervention approach being used in treatment, as well as administration of treatment in a single language (i.e., Meinzer et al., 2007).
Treatment Approaches Intended to Improve Speech Production and Fluency
Fluency is a multidimensional construct that captures word retrieval, articulation, syntax, and prosody. Individuals with an aphasia profile described as “nonfluent” present with halting, agrammatic language, often with co-occuring motor speech impairment (apraxia of speech and/or dysarthria). Given that both linguistic and motoric factors contribute to reduced fluency of output, interventions addressing fluency in nonfluent patients may target different underlying processes. For example, some approaches target articulation at the phoneme or syllable level (e.g., sound production treatment; Wambaugh & Nessler, 2004). Other approaches have focused on production at the utterance or discourse level utilizing choral speech, choral reading, or melodic intonation (Baker, 2006; Belin et al., 1996; oral reading: Boyle, 1989; Cherney, 2010). Some interventions attempt to increase the length of individuals' utterances via expansion of linguistic content (e.g., Response Elaboration Training: Kearns, 1985; Wambaugh, Martinez, & Alegre, 2001; spoken sentence and question training: Florance & Deal, 1977), whereas others address syntactic aspects of production (e.g., Sentence Production Program for Aphasia: Helm-Estabrooks & Nicholas, 2000; Verb Network Strengthening: Edmonds, Nadeau, & Kiran, 2009; Treatment of Underlying Forms: Thompson & Shapiro, 2005).
In an approach known broadly as “script training,” dialogues or monologues are learned verbatim. Historically, the theoretical basis for script training intervention is the “instance of automaticity theory” (Logan, 1988). This theory suggests that recall of complete skilled performances induces automatic performance. Production of scripted material is thought to become more automatic as the learner relies upon recall of past instances of their performance. For this reason, material is trained in a holistic manner and repetitive practice is considered necessary to induce automaticity. Script training has the potential to target both motoric and linguistic aspects of fluency, including articulation, word retrieval, grammar, and prosody (Bilda, 2011; Cherney, Halper, Holland, & Cole, 2008; Cherney, Halper, & Kaye, 2011; Henry et al., 2018; Lee, Kaye, & Cherney, 2009; Youmans, Holland, Muñoz, & Bourgeois, 2005; Youmans, Youmans, & Hancock, 2011). Often, the clinician and the individual with aphasia will construct a personalized script that is practiced intensively to promote communication about a topic of personal interest (Goldberg, Haley, & Jacks, 2012). Participants typically progress through scripted sentences following a hierarchy of repetition, choral reading, and independent production. Script training is an effective tool for targeting the production of scripted material, resulting in an increase in accurate production of words from the target script, improved grammatical output, and increased speaking rate (Bilda, 2011; Cherney et al., 2008, 2011; Lee et al., 2009; Youmans et al., 2005, 2011).
In addition to in-person rehearsal of script content with a clinician, computer-based approaches for script training have proven beneficial (e.g., Cherney et al., 2008, 2011; Fridriksson et al., 2012; Manheim, Halper, & Cherney, 2009). One such study investigated computer-based script training that involved spoken rehearsal in conjunction with an audiovisual model using a technique called speech entrainment (Fridriksson et al., 2012). The training method required participants with nonfluent stroke-induced aphasia to speak in unison with a videotaped model of a healthy speaker (mouth only, presented on an iPod screen) reciting generic, nonpersonalized scripts. Training with this audiovisual model resulted in improved speech production, as measured by a greater variety of words, and a speech rate more closely approximating normal.
Script training via speech entrainment has also been implemented in nonfluent/agrammatic primary progressive aphasia. Henry et al. (2018) implemented an approach known as Video-Implemented Script Training for Aphasia (VISTA) in a group of 10 individuals with nonfluent/agrammatic primary progressive aphasia. This approach, which individually tailors the content and speech rate of scripts, consists of twice weekly treatment sessions with the clinician and daily home practice with speech entrainment (Fridriksson et al., 2012). This study revealed robust gains in percent correct and intelligible scripted words produced, with maintenance of gains documented up to 1 year post-treatment for trained scripts. In addition, improvement in grammaticality was observed at post-treatment for trained scripts.
Script Training in Bilingual Speakers With Aphasia
Only one unpublished study has examined the effects of script training in a bilingual speaker with aphasia (Caruso & Szabo, 2014). In this study, the participant (a Spanish–English bilingual man with Broca's aphasia) received training in English for three scripts and in Spanish for one script. Although the participant was Spanish dominant prior to his stroke, he demonstrated stronger postmorbid verbal expression and a greater functional need to communicate in English; therefore, a majority of the scripts were trained in English. The content of the Spanish script was geared toward reconnecting with a network of Spanish-speaking friends with whom he had less contact after his stroke. For each script, the treatment hierarchy included choral reading, repetition, oral reading, and an independent production of the script.
The treatment consisted of 79 total 50-min sessions, occurring twice weekly, with 1 hr of daily home practice on an iPad. Home practice was facilitated by an application (Pictello), which created a digital storybook for each script. Pictello allowed the scripted lines to be paired with audio and a picture/video. If the participant tapped on the screen, an audio recording of the participant reciting the line was given as an auditory cue. Following treatment, an increase in percent correct scripted words, an increase in words produced per minute (WPM), and a decrease in omitted words were observed. However, these results were not analyzed quantitatively. Although script training has proven to be an efficacious intervention for monolingual speakers and despite promising outcomes in this single case, systematic research has not been directed toward examining these treatment techniques in bilingual individuals with speech production or syntactic deficits.
Current Study
The aim of this study was to examine the effects of VISTA (Henry et al., 2018) on fluency in a Spanish–English bilingual woman with borderline fluent aphasia (with prominent deficits in naming, syntax, and motor speech). VISTA is a script training approach that tailors the speech rate and linguistic and articulatory difficulty of scripts to each individual in an effort to ensure that the scripted material is attainable and natural for the participant.
A single-subject, multiple-baseline crossover design was used to examine the effects of treatment, wherein four trained scripts and one untrained script were assigned to each language of treatment (for a total of eight trained scripts and two untrained scripts). We predicted the following after treatment:
1. The participant would exhibit an increase in the number of correct and intelligible scripted words (primary outcome measure) on trained material.
2. The participant would display a greater degree of CLT from Spanish to English for trained, scripted material. This pattern of generalization was predicted based on greater preservation of Spanish poststroke in our participant as well as theoretical models, which suggest that the second language (L2) is supported by the first language (L1; i.e., Spanish) during learning (Kroll & Stewart, 1994; Kroll et al., 2010).
3. Treatment effects would be maintained at follow-ups (1.5 and 3.5 months post-treatment).
Furthermore, given that the cognate facilitation effect is well established in neurotypical bilingual speakers and that previous studies have demonstrated that cognates may facilitate cross-linguistic generalization for individuals with aphasia, one cognate-dense script was included in each language with the hypothesis that:
4. Cognate-dense scripts would facilitate a greater degree of cross-language transfer relative to scripts with lesser cognate density.
Lastly, secondary variables of interest included grammaticality (number of grammatical errors produced per hundred words), speech rate (i.e., WPM), and overall intelligibility (i.e., percent intelligible words). We hypothesized that:
5. Our participant would show a decrease in number of grammatical errors and an increase in speech rate and overall intelligibility for trained, scripted material.
Method
Participant R. C.
One individual (R. C.) with stroke-induced aphasia was recruited to participate in this study. R. C. was a 66-year-old, right-handed woman who suffered an aneurysm in her left middle cerebral artery and subsequent cerebrovascular accident during a left lateral frontal craniotomy. At the time of this study, R. C. was 1 year 1 month poststroke. Her native language (L1) was Spanish, and her L2 was English. Our participant gave written informed consent, and all procedures were approved by the institutional review board at The University of Texas at Austin.
Language and Social Background
To characterize our participant's language history, including her proficiency, usage, and exposure, R. C. was interviewed and asked to complete the Language Use Questionnaire (LUQ; Kiran, Peña, Bedore, & Sheng, 2010; see Table 1). Her primary communication partners (i.e., her husband and son), who were familiar with her language history and use, were also interviewed to corroborate information provided by the participant (due to the inherent limitations of self-report; Hamers & Blanc, 2000). The LUQ is a comprehensive survey that contains questions regarding the manner and timing of acquisition for both languages, with an emphasis on use and proficiency prior to onset of aphasia. The LUQ was modified for this study in order to inquire about the participant's use and proficiency subsequent to the cerebrovascular accident as well.
Table 1.
Weighted averages of self-rating and communication partner rating of language proficiency, use, and exposure (modified from the Language Use Questionnaire; Kiran et al., 2010).
| Criteria | Spanish | English | |||
|---|---|---|---|---|---|
| Age of acquisition (years) | From birth | 6 | |||
| Poststroke proficiency (out of 100%; with 100% indicating nativelike proficiency) | |||||
| Reading and comprehension | 74 | 73 | |||
| Writing/spelling | 5 | 5 | |||
| Speaking in full sentences | 20 | 15 | |||
| Relating an event | 15 | 20 | |||
| Listening/understanding | 95 | 85 | |||
| Word finding | 15 | 15 | |||
| Poststroke daily usage (out of 100%) | |||||
| Weekday | 82 | 18 | |||
| Weekend | 80 | 20 | |||
| Premorbid daily usage (out of 100%) | |||||
| Weekday | 44 | 56 | |||
| Weekend | 87 | 13 | |||
| Six months prior to stroke (out of 100%) | 50 | 50 | |||
|
Criteria |
Only Spanish |
Primarily Spanish |
Both |
Primarily English |
Only English |
| Lifetime exposure (out of 100%): | |||||
| Hearing | 37 | 27 | 18 | 9 | 9 |
| Speaking | 30 | 30 | 20 | 10 | 10 |
| Reading | 30 | 30 | 20 | 10 | 10 |
Note. Weighted averages out of 100%. Responses rounded to nearest whole number.
R. C. was an early sequential bilingual who was exposed to Spanish from birth and began learning English at 6 years of age. She immigrated to the United States from Mexico when she was 40 years old and had resided in Texas for the previous 26 years. Prior to her stroke, R. C. attended the Monterrey Institute of Technology and Higher Education in Monterrey, Mexico, and earned a Master of Business Administration degree and a bachelor's degree in accounting. Beginning in her 20s, she also spent approximately 1 month per year in the United States visiting family. Her career history included work as a certified public accountant, a professional legal translator, an accounting professor at a university in northern Mexico, and later as a lecturer for a university in Texas.
She was reported to be very proficient in both languages premorbidly and presented with a Spanish-influenced accent when speaking English. Her premorbid proficiency is also supported by her professional and linguistic history. In addition, R. C. could read, write, and speak both languages with ease. Postmorbidly, R. C. reported that suppressing Spanish was challenging for her and, for that reason, English was used with less frequency. With the exception of her position at a university in northern Mexico, English was the primary language used in her professional settings; both Spanish and English were used at home with her husband and children and when conversing with friends.
Structural Neuroimaging
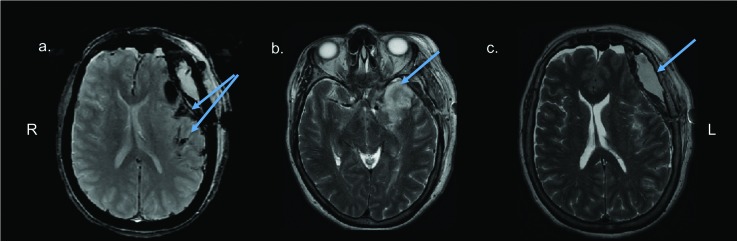
R. C. incurred a ruptured aneurysm in her left middle cerebral artery and subsequently had a second cerebrovascular accident during a left lateral frontal craniotomy. Following these events (5 days postrupture and 13 months prior to this study), a clinical magnetic resonance imaging scan was collected. Imaging revealed damage to the left perisylvian cortex and to the left anterior temporal and prefrontal regions (see Figure 1). This lesion profile is consistent with R. C.'s prominent anomia, telegraphic speech, and reported difficulty with language suppression.
Figure 1.
Clinical magnetic resonance imaging scan showing (a) lesion encompassing perisylvian cortex, (b) prominent lesion in the left anterior temporal lobe, and (c) subdural hematoma in the left prefrontal region.
Procedure
Pre-treatment Assessment
Comprehensive assessment included speech, language, and cognitive evaluations (see Table 2). At the time of her initial evaluation, R. C.'s performance on the Mini-Mental State Examination (Folstein, Folstein, & McHugh, 1975; 18, Spanish; 20, English) indicated deficits in cognition, and her performance on the Stroop task confirmed an impairment of executive function. More specifically, R. C.'s score on the Stroop task was in the impaired range (4/77, Spanish; 0/77, English; Kramer et al., 2003), and she demonstrated difficulty in correcting instances of interference during the task. With respect to her aphasia profile, R. C. presented with a borderline fluent/anomic aphasia, as discerned by her performance on the Western Aphasia Battery–Revised (WAB-R; Kertesz, 1982) and a Spanish version of the WAB-R (Aphasia Bank: Informal Spanish Translation, 2014; Aphasia Quotient [AQ] = 67.2, Spanish; 71.7, English). Her spontaneous speech was often telegraphic and halting, and she demonstrated evidence of moderate motor speech impairment. Specifically, her performance on the Apraxia of Speech Rating Scale (Strand, Duffy, Clark, & Josephs, 2014) was consistent with moderate apraxia and dysarthria (see Appendix B for individual item ratings from the Apraxia of Speech Rating Scale).
Table 2.
Speech, language, and cognitive test performance: participant R. C.
| Assessment | Pre-Tx (Spn) | Pre-Tx (Eng) | Post-Tx (Spn) | Post-Tx (Eng) | 3.5 mo. f.u. (Spn) | 3.5 mo. f.u. (Eng) |
|---|---|---|---|---|---|---|
| Mini Mental State Exam (30) | 18 | 20 | 27 | 23 | — | — |
| Stroop task (77) | ||||||
| Stroop Color Naming (no. correct/77/1 min) | 7 | 6 | 13 | 7 | — | — |
| Color Naming (uncorrected errors) | 0 | 1 | 0 | 0 | — | — |
| Color Naming (self-corrected errors) | 1 | 0 | 1 | 0 | ||
| Inhibition (no. correct/1 min) | 4 | 0 | 10 | 6 | — | — |
| Inhibition (uncorrected errors) | 2 | 3 | 1 | 2 | — | — |
| Inhibition (self-corrected errors) | 1 | 0 | 1 | 1 | ||
| Western Aphasia Battery–Aphasia Quotient (100) | 67.2 | 71.7 | 75.7 | 72.9 | 72.3 | 69.4 |
| Spontaneous Speech (20) | 13 | 13 | 13 | 14 | 13 | 13 |
| Information Content | 7 | 7 | 9 | 8 | 8 | 8 |
| Fluency | 6 | 6 | 5 | 5 | 5 | 5 |
| Auditory Verbal Comprehension (10) | 8.5 | 7.75 | 8.55 | 7.75 | 8.15 | 7.00 |
| Repetition (10) | 7.5 | 7.3 | 8.4 | 7.8 | 8.5 | 7.8 |
| Naming and Word Finding (10) | 4.6 | 7.8 | 7.9 | 6.9 | 6.5 | 6.9 |
| Boston Naming Test (60) | 17 | 19 | 37 | 25 | 41 | 22 |
| Pyramids and Palm Trees: Picture Version (shortened; 14) | — | 14 | — | — | — | — |
| Apraxia of Speech Rating Scale–Apraxia rating (0 = none, 4 = severe) | 2 | 2 | — | — | — | — |
| Apraxia of Speech Rating Scale–Dysarthria rating (0 = none, 4 = severe) | 2 | 2 | — | — | — | — |
| Northwestern Anagram Test (NAT; 12) | 4 | — | — | 8 | — | — |
| Bilingual Aphasia Test | ||||||
| Syntactic Comprehension (87) | 58 | 61 | 64 | 57 | — | — |
| Grammaticality Judgments (10) | 7 | 6 | 10 | 9 | — | — |
Note. Em dash indicates that data were not collected at the specified time point. A short version of the NAT sampling all of the grammatical structures on the assessment was used. Tx = treatment; Spn = Spanish; Eng = English; mo. = month; f.u. = follow-up.
R. C. demonstrated a moderate impairment in syntactic comprehension in both English and Spanish on the Bilingual Aphasia Test (BAT; Syntactic Comprehension subtest; Paradis & Libben, 1987) with more errors on passive sentences with subject/object word order variation (“It's the truck that pulls the car”) and similar negative passive sentences (“The truck is not pulled by the car”). A nonverbal syntax production impairment was observed in English on a shortened version of the Northwestern Anagram Test (NAT; Thompson, Weintraub, & Mesulam, 2011), with impaired performance on both canonical (3/6) and noncanonical structures (1/6).
Confrontation naming on the Boston Naming Test (BNT; Kaplan, Goodglass, & Weintraub, 2001, 2005) was impaired in both languages (17/60 items in Spanish and 19/60 items in English), and the participant produced both semantic and phonological paraphasias. R. C.'s nonverbal object semantics were preserved, as measured by her performance on the Pyramids and Palm Trees Test (100%; Breining et al., 2015; Howard & Patterson, 1992). In summary, R. C. presented with a borderline fluent aphasia profile with deficits in syntax, motor speech, and lexical retrieval.
Study Design and Treatment Approach
A single-subject, multiple-baseline experimental design was used to examine within-language gains and cross-language transfer. Using this design, we administered VISTA (Henry et al., 2018) to our participant in two phases. In the first phase, treatment was administered in Spanish, whereas the second phase consisted of treatment administered in English. The VISTA protocol included two components: (a) two weekly 1-hr sessions with a bilingual speech-language pathology graduate clinician (D. C.) and a certified bilingual speech-language pathologist (S. G.) using a hierarchy of tasks designed to promote memorization and conversational usage of scripts (see Table 3) and (b) daily homework of at least 30 min, which consisted of unison speech production with audiovisual stimuli on the iPad. Although the participant was permitted to practice for more than 30 min per day, she rarely reported practicing for more than 30 min.
Table 3.
Clinician-guided Video-Implemented Script Training for Aphasia treatment hierarchy (Henry et al., 2018).
| Participant is asked to: | |
| 1. Choose each correct script sentence from four foil sentences. | |
| 2. Put the script sentences in the correct order. | |
| 3. Read the entire script aloud. | |
| 4. Produce individual scripted sentences in response to questions. | |
| 5. Produce the entire script from memory. | |
| 6. Respond to questions with scripted sentences out of the correct order of the script. | |
| • During the second treatment session for a given script, a novel communication partner has an unscripted conversation with the participant to promote conversational usage of scripted material. | |
|
Script not loaded with cognates: Topic: My friendships My best friends are Sara, Alejandrina, Linda, and Lola. My sister supported me throughout my recovery following my stroke. My friends are just like sisters to me. Do you have any friends that are like siblings to you? |
Cognate-dense script (*cognates are underlined): Topic: My Rehabilitation My doctor is very professional and sensitive. I had an extensive operation and she facilitated my rehabilitation. I use strategies to calm my mind when I have stressful moments. Do you use strategies to reduce stress? |
|
Example foils for a scripted sentence (Step 1; correct sentence underlined): My friends are just like sisters to me. My friends are just like cousins to me. My friends are not like sisters to me. My sisters are like my friends. | |
Note. Feedback regarding articulation and grammar occurred during Steps 3–6, with targeted practice, as needed.
Script Development and Stimulus Generation
Ten scripts were developed for R. C. via a collaborative process involving the participant, her primary communication partners (i.e., her husband and son), and the clinicians. The participant selected five topics in each language, and four topics per language were pseudorandomly selected to enter treatment; of those four, one script was constructed to contain a high proportion of cognates. During the initial baseline probe and subsequent script development for a given topic, our participant provided more content than was necessary for the final scripts, which allowed us to be selective about the specific content to be included. Cognate-dense scripts (one per language) were constructed by intentionally selecting cognates generated during the initial probe and script development stage. Conversely, for scripts that were not designed to be cognate dense, we intentionally avoided selecting cognates generated during this stage. Cognate-dense scripts contained 16/34 and 14/38 cognates out of the total number of scripted words (hereafter referred to as cognate-dense scripts), as compared to other trained scripts, whose cognate count varied from 0 to 5 (M = 2.75). Two additional scripts served as untrained, within-subject controls (see Table 3).
R. C. selected functional script topics (e.g., about me, family, career) and generated content that was then modified minimally by the clinician in order to balance trained and untrained scripts for number of words, number of sentences, complexity (i.e., percentage of complex words per sentence), and readability. Ease of readability was assessed using a Flesch Kincaid reading score (Flesch, 1948). In addition, t tests revealed that trained and untrained scripts were matched on the basis of average word frequency and phonotactic probability (all ps > .05; CLEARPOND; Marian, Bartolotti, Chabal, & Shook, 2012). Scripts were limited to approximately four sentences in length, and each script followed a similar format (i.e., three statements and a question; all canonical sentence structures). In general, scripts in Spanish had a higher percentage of complex words (as measured by syllable and letter length). However, this was driven by the structure of the Spanish language, wherein a greater number of syllables may be needed to convey information relative to the English language (see Pellegrino, Coupe, & Marsico, 2011, for a discussion on information density).
After scripts were generated, home practice videos with a healthy speaker were produced. To determine the tailored rate for the audiovisual stimuli, an average of the participant's WPM was derived in each language from both a picture description task and a reading passage. R. C.'s average connected speech rate was 40 WPM. Subsequently, a female mouth model (who was a simultaneous Spanish–English bilingual speaker; S.G.) was video-recorded while reading the participant's script at R. C.'s target speech rate (using a metronome for pacing). A mouth model that spoke a Mexican dialect of Spanish was selected in order to avoid a dialectal mismatch with the patient.
Prior to the initiation of treatment, three baseline probes were collected. We collected a fixed number of baseline probes due to the practicality of collecting 10 script probes in two languages and in order to minimize repeated probing before the initiation of treatment. In the first baseline probe, the scripted material was yet to be developed. Therefore, the clinician prompted the participant with the topic of the script (i.e., “tell me about your family”). After this probe, the clinician finalized the scripted material with the participant's feedback and read the final version of the script to the participant once. On a different day, a second baseline probe was collected, wherein the clinician again prompted the participant with the topic of the script. The third and final pre-treatment probe mirrored that of the second probe. Given that the participant was not at all familiar with the scripted material in the first probing session, we used only the second and third baseline probes in our statistical analyses, because including the first baseline probe would underestimate the participant's baseline performance.
Treatment Approach
The VISTA training hierarchy (Henry et al., 2018) was used for treatment sessions with the clinicians (see Table 3 for the complete hierarchy and example scripts). Sessions progressed from structured tasks (e.g., targeting grammaticality and intelligibility) to tasks that resemble situations encountered in daily communication (e.g., using scripted sentences out of order and in conversation with novel conversational partners) in order to promote memorization and generalized conversational usage. Each of the following steps was completed per session: identifying script sentences from four foils, correctly ordering the scripted sentences, reading the script aloud, responding to questions in the scripted order, recalling the script from memory, and responding to questions out of the scripted order. Speech sound errors were targeted via visual placement cues, and grammatical errors were corrected online via modeling from the clinician.
Throughout the treatment hierarchy, if the participant made an appropriate content substitution (i.e., at the lexical level or phrase level), the clinician prompted the participant to attempt to provide the information from the script verbatim. If the participant provided the correct scripted information, then the training hierarchy continued. If the participant provided an appropriate substitution again, then the clinician would provide positive reinforcement (i.e., the clinician told the participant that they provided an appropriate, if not verbatim, response), and the participant would be reminded of their scripted sentence (i.e., “and remember the actual sentence from your script is…”).
A conversation with a novel communication partner occurred for each script at the end of the second treatment session. For this unscripted conversation, the novel communication partner was provided with the script topic, but not with the script content. The conversation partner was instructed to avoid the specific prompt used by clinicians during probes (i.e., asking the participant to “tell me about X”). During this conversation, we could not guarantee that the specific information from the trained scripts would be elicited. The purpose of this conversation was to provide the participant with the opportunity to use scripted material, if it was appropriate in their conversation. The participant was provided with the following instructions prior to engaging in the conversation: “We are going to introduce you to a new person who is going to have a conversation with you. They know that the conversation will be about X, but they don't know the information in your script. We encourage you to use parts of your script if the opportunity comes up.”
Daily speech entrainment (Fridriksson, Basilakos, Hickok, Bonilha, & Rorden, 2015; Fridriksson et al., 2012) homework occurred at the participant's place of residence using video stimuli of individualized scripts. R. C. was asked to log the number of minutes of training that she completed daily, and the clinician monitored training progress twice per week by reviewing homework logs with the patient. The participant was asked to practice for at least 30 min per day with the assigned script. During practice, R. C. attempted to speak in unison with the audiovisual model in real time using an iPad and headphones. In addition, the participant practiced articulating a list of scripted words that were difficult for her to articulate during the prior session with the clinicians.
Training Criteria
Criterion for advancement to a new script was set at 90% correct and intelligible words relative to the script target, with a minimum of two and a maximum of three treatment sessions per script. More specifically, our primary outcome measure of correct and intelligible words was defined as a word produced by R. C. that the clinician coded online as present relative to the script target (i.e., correct) and as intelligible within the context of the script topic. If the participant produced a phonemic paraphasia that did not change the meaning of the word and was clearly derived from the target word, it was considered intelligible. However, if the participant produced a semantic paraphasia, a synonym, or a lexical unit in the nontarget language, the word was not counted toward the total number of correct and intelligible scripted words. Only words produced in the language of training were considered toward the total number of correct and intelligible words.
The outcome measure of correct and intelligible words is a combined metric capturing linguistic improvement, improved speech intelligiblity, and script memorization. For this reason, we also included secondary outcome measures that assess language (i.e., number of grammatical errors per hundred words) and speech production (i.e., overall intelligibility and words per minute) separately and irrespective of script memorization. These outcome measures have been shown to be sensitive to treatment-induced improvements in a previous study (Henry et al., 2018). Production accuracy on all scripts (trained and untrained) was probed at the beginning of each treatment session. Each time the participant was prompted to recall the script from memory, the clinician provided the following prompt: “you have been practicing your family script. I want you to tell me this script from memory. Tell me about your family.” Approximately half of the scripts (always including the script currently in training) were probed in each language at the start of each treatment session, so that all scripts were probed once per week in each language.
Reliability of Primary Outcome Measure
One trained undergraduate coder, blind to study condition, used CHAT and CLAN software (MacWhinney & Snow, 1985) to transcribe all probes and to code unintelligible words. Each spoken word was coded as intelligible or unintelligible and as present or omitted relative to each scripted word. Productions that were deemed unintelligible were transcribed phonetically. If the participant self-corrected, the rectified response was counted as correct. Interrater reliability, comparing the clinician's online data collection and coder's transcription, was conducted for 25% of the total number of treatment sessions. Overall, reliability was high at 97.44%.
Treatment Fidelity
Two trained undergraduate raters independently reviewed video recordings of 25% of the total number of treatment session in order to determine whether the clinicians followed each step of the treatment protocol correctly. For each step of the treatment hierarchy, the raters were required to make a decision as to whether or not the clinician completed each step (e.g., “did the clinician prompt the participant to choose the scripted sentence from four foils?”). After the raters reviewed each video, they calculated a percentage with the denominator representing the total number of treatment hierarchy steps. No discrepancies were found between the two raters' fidelity ratings, and fidelity scores revealed that the clinicians correctly administered treatment steps 100% of the time.
Self-Assessment and Communication Partner Assessment of Change
A post-treatment survey (modified from Henry et al., 2013) was administered to R. C. and her primary communication partners (i.e., her spouse and son) in order to query perceptions regarding the effects of treatment and potential changes in communication abilities that may have resulted from treatment (see Appendix A for survey items).
Outcome Measures and Statistical Analyses
All four Spanish scripts were trained first, followed by the four English scripts. Data collected at three time points were examined to determine the effects of treatment: pre-treatment (before any treatment began), mid-treatment (post-Spanish and pre-English treatment), and following all treatment (post-Spanish and English treatment). In addition, follow-up data were collected at 1.5 and 3.5 months post-treatment. The follow-up time point of 1.5 months was chosen because it represents the approximate duration of a single phase of treatment (i.e., the Spanish or English phase of treatment). Therefore, this follow-up time point provided us with an equivalent comparison relative to the post-treatment probe obtained for the Spanish-training phase (after the English-trained set was completed). We were also interested in assessing longer term maintenance and therefore conducted a follow-up visit at 3.5 months post-treatment.
Our primary outcome measure of correct and intelligible scripted words was calculated for trained and untrained scripts for two time points during pre-treatment (baseline), for two at mid-treatment, and for three to four time points post all training. Our measure that captured the magnitude of CLT was calculated for trained scripts at the aforementioned time points. To examine CLT, the clinicians prompted the participant to produce the trained scripts in the language not used for training (e.g., to produce Spanish-trained scripts in English).
Data analysis for our primary outcome measure occurred in two stages. In the first stage, we analyzed whether changes across time points were significant and lasting for trained scripts. In order to establish the overall treatment effect for all trained scripts combined (Spanish- and English-trained scripts), we compared pre- and post-treatment performance. To examine maintenance effects for all trained scripts combined, we compared pre-treatment performance with performance at the 1.5 and 3.5 month follow-ups. We used a nonparametric permutation test using the exactRankTest (Hothorn & Hornik, 2006) package in R (Version 3.3.2; R Core Team, 2016; n = 8), as the distribution of difference scores for paired-samples tests did not meet the assumption of normality. One-tailed tests were used to interpret pre- versus post-treatment and pre-treatment versus follow-up performance, as we predicted that treatment gains for the primary outcome measure would be significant and lasting.
In the second stage of analysis, we compared the magnitude of effect sizes across conditions. To compare treatment outcomes across conditions (Spanish trained vs. English trained, Spanish trained vs. Spanish untrained, etc.), treatment effect sizes (d statistics; Robey, Schultz, Crawford, & Sinner, 1999) were calculated for each script (with 2.6, 3.9, and 5.8 corresponding to small-, medium-, and large-sized effects, respectively; Beeson & Robey, 2006). We calculated d statistics for our primary outcome measure of correct and intelligible scripted words by taking R. C.'s performance from trained and untrained scripts for two observations during pre-treatment, two mid-treatment, three to four observations after all treatment, and two observations at follow-up (3.5 months post-treatment; see Henry et al., 2013, for a similar calculation method). Furthermore, we calculated d from the pre to the mid and post all treatment time points for Spanish-trained scripts so that we could derive Spanish performance immediately after the Spanish treatment phase, as well as following all treatment. For English-trained scripts, d was calculated from pre to post all treatment, as English scripts were targeted in the second treatment phase. Weighted effect sizes were calculated by multiplying each set's d statistic by the total number of observations, adding this weighted value across sets, and dividing by the total number of observations, in order to determine the magnitude of treatment effects for each language of treatment and for CLT (English to Spanish and Spanish to English; see Beeson & Robey, 2006, for additional calculation details). Furthermore, we conducted z tests to compare the magnitude of effect sizes calculated from each treatment condition (i.e., performance on trained vs. untrained scripts in each language; CLT of cognate-dense vs. other trained scripts). The rationale for using z tests instead of permutation tests for these comparisons was due to our limited number of observations in each language (n = 4). The z test was conducted by taking the difference between the weighted effect sizes of each condition (d) and dividing the generated difference by the square root of their combined variance.
Tests comparing effect sizes for trained scripts between languages were evaluated using two-tailed tests as we did not have specific predictions regarding these contrasts. Tests comparing effect sizes between trained and untrained scripts (at all time points) as well as between cognate loaded and other trained scripts (with regard to CLT) were evaluated using one-tailed tests due to our prediction that trained scripts would demonstrate a greater degree of CLT relative to untrained scripts and that cognate loaded scripts would demonstrate more CLT relative to scripts that were not cognate dense. CLT effects were also investigated using permutation tests. CLT effects for all trained scripts from pre- to post-treatment were evaluated using a one-tailed test as we predicted a significant CLT effect for trained material. Maintenance of CLT was assessed using a two-tailed test, as this effect was less predictable.
Additional outcome measures included grammatical errors produced per hundred words, WPM (regardless of the relevance of words produced), and overall intelligibility (percent intelligible words; regardless of whether words adhered to scripted targets), which were calculated for trained and untrained scripts for two time points during pre-treatment, mid-treatment, and post-treatment. Nonparametric permutation tests were also conducted to compare pre- versus post-treatment performance on these outcome measures for all trained scripts combined. One-tailed tests were used to evaluate the results of our additional outcome measures from pre- to post-treatment due to our a priori hypotheses that our participant would improve on these outcome measures for trained scripts. Although we calculated performance on secondary variables for untrained scripts, we were unable to conduct statistical analyses due to the limited number of untrained scripts (n = 2).
In addition to performance on untrained scripts, generalization was assessed via performance on the NAT, administered in English (Weintraub et al., 2009); on the BNT (Kaplan et al., 2001, 2005); on the WAB-R (Kertesz, 2006); and on the subtests of the BAT (Paradis & Libben, 1987), which were administered in English and Spanish. McNemar tests were used to compare pre- versus post-treatment scores on these selected language measures. Given that we did not have a priori hypotheses regarding generalization to formal language measures, we evaluated the results of these comparisons using two-tailed tests.
Results
Treatment Duration
R. C. participated in 3 months (approximately 13 weeks) of treatment, with sessions occurring twice weekly for 1 hr, for a total of 26 hr of direct contact with the clinicians. During the first 6.5 weeks, treatment was administered in Spanish, and for the remaining 6.5 weeks, treatment was administered in English. R. C. also completed at least 30 min of homework daily, totaling approximately 46.5 total hours of homework.
Primary Outcome Measure: Percent Correct and Intelligible Scripted Words
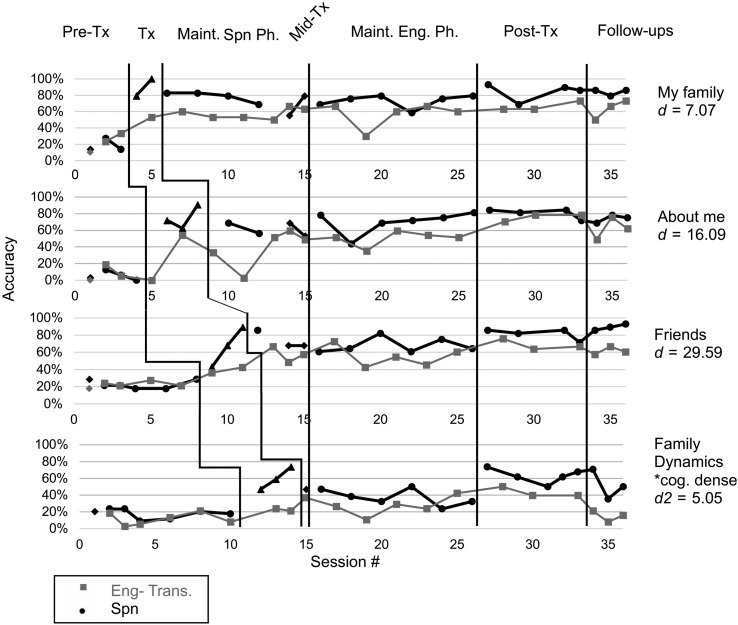
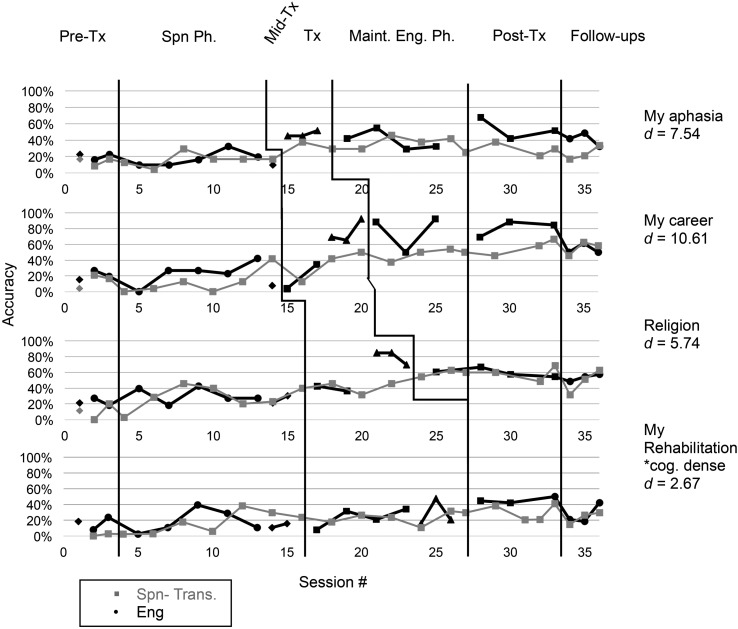
Multiple baseline data for R. C.'s performance on spontaneous speech probes for trained and untrained scripts in both languages are shown in Figures 2 (Spanish) and 3 (English). In addition, cross-language transfer of scripted material is displayed in each figure. The overall treatment effect for trained scripts (across both languages) was significant as measured by a permutation test (t = −8.96, p = .004, one-tailed). In the following section, we report results separately for Spanish- and English-trained scripts.
Figure 2.
Multiple-baseline data for R. C.'s performance during and after Video-Implemented Script Training for Aphasia for Spanish-trained scripts. Phases of treatment are indicated by vertical lines, including baseline (first/pure baseline indicated by diamond marker, which was not included in statistical analyses), treatment sessions, mid-treatment (when the language of treatment changed from Spanish to English), maintenance sessions, post-treatment probes, and follow-up visits (one probe at 1.5 months post-treatment and two probes at 3.5 months post-treatment). Tx = treatment; Ph = phase; Maint. = maintenance; Spn = Spanish; Eng = English; Trans. = Transfer; *cog-dense = cognate-dense script.
Figure 3.
Multiple-baseline data for R. C.'s performance during and after Video-Implemented Script Training for Aphasia for English-trained scripts. Phases of treatment are indicated by vertical lines, including baseline (first/pure baseline indicated by diamond marker, which was not included in statistical analyses), treatment sessions, mid-treatment (when the language of treatment changed from Spanish to English), maintenance sessions, post-treatment probes, and follow-up visits (one probe at 1.5 months post-treatment and two probes at 3.5 months post-treatment). Tx = treatment; Ph = phase; Spn = Spanish; Maint. = maintenance; Eng = English; Trans. = transfer; *cog-dense = cognate-dense script.
Spanish-Assigned Scripts
On Spanish-assigned scripts, R. C.'s performance was relatively stable throughout baseline probes. As treatment was implemented, she showed improvement on the script in training for the primary outcome measure of percent correct, intelligible words. R. C. did not, however, meet criterion (90% correct, intelligible words or better) on all scripts. As shown in Figure 2, R. C. met criterion on two Spanish-trained scripts within three sessions (i.e., Family and About me), achieved 89% on one script (i.e., Friends), and maintained good performance for the duration of the training period for those scripts. The participant did not meet criterion on the cognate-dense script.
Table 4 displays weighted effect sizes derived in each treatment phase. The weighted effect size observed post-treatment for Spanish-trained scripts was large at the midtreatment time point (d = 11.16) and following both phases of treatment (d = 13.76), indicating a robust, positive response to treatment. The weighed effect size for Spanish-untrained scripts was minimal at the mid-treatment time point (d = 2.48) and at the end of all treatment (d = 1.71), indicating only a slight improvement for untrained topics (see Figure 4).
Table 4.
Weighted effect sizes (d statistics) for trained scripts by language of treatment, cognate status, and treatment phase.
| Phase | Mid-Tx (post-Spanish Tx) | Post-All Tx |
|---|---|---|
| Spanish-trained scripts | ||
| All Spanish-trained | 11.16 | 13.76 |
| Trained (cognate-dense script excluded) | 14.38 | 18.83 |
| Cognate script | 0.69 | 5.05 |
| Untrained scripts | 2.48 | 1.71 |
| Transfer to English | 6.12 | 16.13 |
| Transfer to English (cognate-dense script excluded) | 7.98 | 11.30 |
| English-trained scripts | ||
| All English-trained | — | 6.64 |
| Trained (cognate-dense script excluded) | — | 7.96 |
| Cognate script | — | 2.67 |
| Untrained scripts | — | 1.68 |
| Transfer to Spanish | — | 4.68 |
| Transfer to Spanish (cognate-dense script excluded) | — | 6.17 |
Note. Post-All Tx refers to effect sizes calculated after Spanish and English phases of treatment. Em dashes denote empty cells due to the fact that English scripts were not yet trained at the mid-treatment time point. Values 2.6, 3.9, and 5.8 correspond to small-, medium-, and large-sized effects, respectively (Beeson & Robey, 2006; Robey et al., 1999). Tx = treatment.
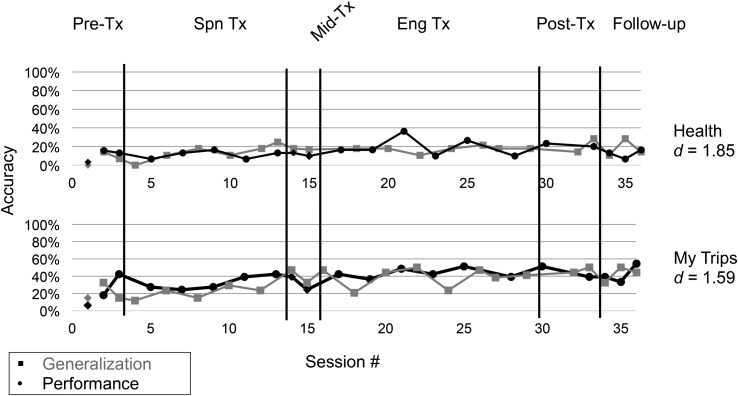
Figure 4.
Multiple-baseline data for R. C.'s performance during and after Video-Implemented Script Training for Aphasia for untrained scripts. Phases of treatment are indicated by vertical lines, including baseline (first/pure baseline indicated by diamond marker, which was not included in statistical analyses), treatment phases, mid-treatment (when the language of treatment changed from Spanish to English), post-treatment probes, and follow-up visits (one probe at 1.5 months post-treatment and two probes at 3.5 months post-treatment). Tx = treatment; Spn = Spanish; Eng = English.
A z test was used to compare the magnitude of treatment effects between trained and untrained scripts in Spanish. The z test revealed a significant difference between trained and untrained scripts, from pre- to mid-treatment (i.e., post–Spanish treatment; z = 3.53, p = .0002, one-tailed), and from pre to post all treatment (z = 4.79, p < .0001, one-tailed).
English-Assigned Scripts
On English-assigned scripts, R. C.'s performance was relatively stable over the first two pre-treatment probes, and as treatment was implemented, she showed improvement on the script in training for the primary outcome measure of percent correct, intelligible words (see Figure 3). With the exception of one script (Career), she did not meet criterion for English scripts within three sessions.
The weighted effect size for all English-assigned trained scripts was large (d = 6.64), indicating a positive response to treatment. For untrained scripts, the weighted effect size was minimal (d = 1.68), demonstrating only a slight improvement for untrained topics (see Figure 4). Regarding performance on English scripts, a z test revealed a significant difference between trained and untrained scripts from pre- to post-treatment (z = 3.26, p = .0006, one-tailed).
Comparing Effect Sizes Between Languages
A z test was used to compare the magnitude of effect sizes for scripts trained in each language. A nonsignificant difference (z = 1.74, p = .08, two-tailed) was observed when comparing the weighted effect size for Spanish-trained scripts immediately following treatment (d = 11.16) to the weighted effect size for English-trained scripts (d = 6.64). However, a significant difference (z = 2.60, p = .01, two-tailed) was observed when comparing the weighted effect size for Spanish-trained scripts following all treatment (d = 13.76) to the weighted effect size for English-trained scripts (d = 6.64).
Maintenance of Primary Outcome Measure
For all trained scripts combined, the significant improvement for our primary outcome measure from pre- to post-treatment was retained at 1.5 and 3.5 months post-treatment (relative to pre-treatment; permutation test, pre-treatment vs. 1.5 months follow-up, t = −4.94, p = .004; pre-treatment vs. 3.5 months follow-up, t = −4.89, p = .004, one-tailed).
In addition, we calculated d statistics comparing follow-up performance to baseline performance. For Spanish-trained scripts, we observed maintenance at 3.5 months post-treatment, as evidenced by an effect size (d = 14.14) that was comparable to the d statistic calculated immediately post-treatment (d = 13.76). Performance on English-trained scripts also indicated maintenance of gains at follow-up (d = 4.27, compared to post-treatment, d = 6.64). Moreover, the significant difference between trained and untrained scripts was retained for both Spanish (z = 4.66, p < .0001, one-tailed; untrained d = .11) and English (z = 1.67, p = .05, one-tailed; untrained d = 2.00) at 3.5 months post-treatment relative to baseline.
Overall Effect of CLT
A permutation test comparing performance of scripts in the untrained language from pre- to post-treatment revealed a significant CLT effect for trained scripts (both languages combined; t = −7.71, p = .004, one-tailed; pre to post each treatment phase). For this analysis, performance after each treatment phase was used in order to reduce interference of the language that was currently in treatment (i.e., transfer from Spanish to English was assessed immediately following the Spanish treatment phase). Transfer at 1.5 months post-treatment was borderline significant relative to immediately post-treatment (t = 3.16, p = .05, two-tailed); however, transfer at 3.5 months post-treatment was not significantly different relative to immediately post-treatment (t = 0.22, p = .67, two-tailed).
English Performance of Spanish-Trained Scripts
The magnitude of CLT from Spanish to English (i.e., performance in English of Spanish-trained scripts) was large (see Table 4; d = 6.12 at mid-treatment; d = 16.13 post all treatment). To examine the influence of cognates on CLT, we conducted a z test to examine potential differences in the magnitude of treatment effects between the cognate-dense script and the other trained scripts (from pre- to post-treatment). Results indicated a significantly greater magnitude of CLT for trained scripts that were not cognate dense (z = 2.82, p = .002, one-tailed).
Spanish Performance of English-Trained Scripts
A medium-sized CLT effect was observed for English to Spanish transfer (i.e., performance in Spanish of English-trained scripts; see Table 4; d = 4.68). A z test revealed a significantly greater magnitude of CLT for trained scripts that were not cognate dense (z = 1.69, p = .05, one-tailed).
Comparing Transfer Between Languages
To compare the magnitude of transfer in each linguistic direction (Spanish transfer to English and English transfer to Spanish), we conducted an additional z test directly comparing effect sizes reflecting CLT for trained scripts. The difference between effect sizes was not significant (p > .05, one-tailed), despite the fact that Spanish to English transfer generated a large effect size (d = 6.12) and that English to Spanish transfer generated a medium effect size (d = 4.68).
Additional Treatment Effects and Outcome Measures
In addition to our primary outcome measure, secondary variables of interest were as follows: grammatical errors per hundred words, speech rate, and overall intelligibility. We conducted analyses for trained scripts with both languages combined due to the limited number of observations and compared performance between the pre- and post-treatment time points.
Grammatical Errors
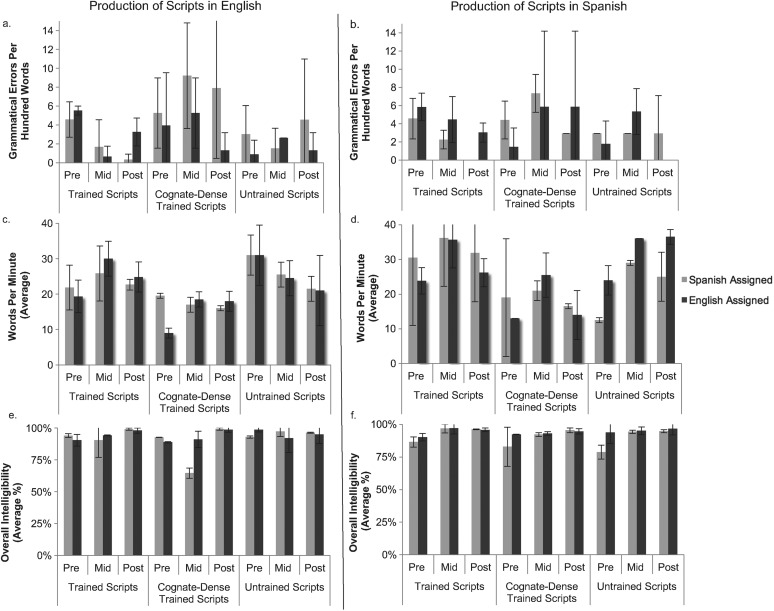
The number of grammatical errors R. C. produced per hundred words was calculated before, during, and after treatment for trained and untrained scripts. 2 In general, the participant demonstrated a reduction in grammatical errors for trained scripts (Figures 5a and 5b). However, an increase in the frequency of grammatical errors for trained cognate-dense scripts was observed. Figure 5a shows an increase in the frequency of grammatical errors for trained cognate-dense scripts at the mid-treatment time point for both English- and Spanish-assigned scripts produced in English. Figure 5b shows a similar pattern for both English- and Spanish-assigned cognate-dense scripts produced in Spanish. Nevertheless, for all trained scripts combined, a significant decrease in grammatical errors produced per hundred words was observed from pre- to post-treatment using a permutation test (t = 4.52, p = .008, one-tailed).
Figure 5.
(a) Grammatical errors produced per hundred words during R. C.'s production of scripts in English. (b) Grammatical errors produced per hundred words during R. C.'s production of scripts in Spanish. (c) Average words per minute for R. C.'s production of scripts in English. (d) Average words per minute for R. C.'s production of scripts in Spanish. (e) Average overall intelligibility for R. C.'s production of scripts in English. (f) Average overall intelligibility for R. C.'s production of scripts in Spanish. The mid-treatment time point represents data collected post–Spanish treatment and pre–English treatment. Error bars represent standard deviation, included for descriptive purposes but not used for statistical inference.
Speech Rate
The number of words R. C. produced per minute (WPM) was calculated for the pre-, mid- and post-treatment time points for trained and untrained scripts.2 R. C. demonstrated a numerical increase in WPM for most trained scripts from pre- to post-treatment; however, she did not attain a rate of greater than 37 WPM (on average) for performance on scripts produced in English or Spanish (see Figures 5c and 5d, respectively). R. C.'s lowest WPM rates occurred when producing cognate-dense scripts in each of her languages (e.g., 12–25 WPM). A permutation test revealed a nonsignificant increase in WPM from pre- to post-treatment for trained scripts (t = −1.50, p = .09, one-tailed).
Overall Intelligibility
The percentage of intelligible words produced by R. C. in response to probes was calculated before, during, and after treatment for trained and untrained scripts2 for English (see Figure 5e) and Spanish (see Figure 5f). R. C.'s overall intelligibility for all scripts in either language was above 80% at pre-treatment. Therefore, Figures 5e and 5f show only modest improvements in intelligibility for all scripts, approximating 90% or greater, except for the Spanish-assigned, cognate-dense script produced in English during the mid-treatment time point, in which intelligibility dropped to about 65% (see Figure 5e). Nevertheless, for all trained scripts, a significant increase in overall intelligibility was observed from pre- to post-treatment (permutation test, t = −6.64, p = .004, one-tailed).
Generalization: Post-Treatment and Follow-Up Assessments
To examine generalization of treatment effects, we compared performance on select language measures across time points using McNemar tests. R. C.'s performance on the BNT in English remained relatively stable, with small numerical improvements noted at post-treatment and 3.5 months post-treatment (19/60, pre-treatment; 25/60, post-treatment; 22/60, 3.5 months post-treatment). These changes were not significant (pre- to post-treatment, p = .18; before 3.5 months, p = .581). However, R. C. demonstrated significant improvement on the Spanish BNT (p < .0001; 17/60, pre-treatment; 37/60, post-treatment). This improvement was maintained at 3.5 months post-treatment (41/60; before 3.5 months, p < .0001; after 3.5 months, p = .34).
Performance on English syntax production on a short version of the NAT improved from pre- to post-treatment from a score of 4/12 (pre-treatment) to 8/12 (post-treatment); however, these changes were not significant (p = .13). Syntactic comprehension in English as measured by the BAT subtest revealed a nonsignificant change from pre- (61) to post-treatment (57/87; p = .56), with minimal improvement in Spanish (58–64/87; p = .31). Similar results were observed on the BAT Grammaticality Judgments subtest for English and Spanish. Overall, improvements (6–9, English, p = .38; 7–10, Spanish, p = .34; both scores out of 10) were not statistically significant.
R. C. also demonstrated a clinically significant improvement (≥ 5 points; Shewan & Donner, 1988) from pre- to post-treatment on the WAB-R in Spanish (AQ = 67.2–75.7), with the largest improvement observed on the Naming and Word Finding subtest. Her performance in English on the WAB-R was stable from pre- to post-treatment (AQ = 71.7–72.9). In summary, on generalization measures, R. C. showed improvement on various standardized measures from pre- to post-treatment, with Spanish performance on the BNT and WAB-R showing significant improvements.
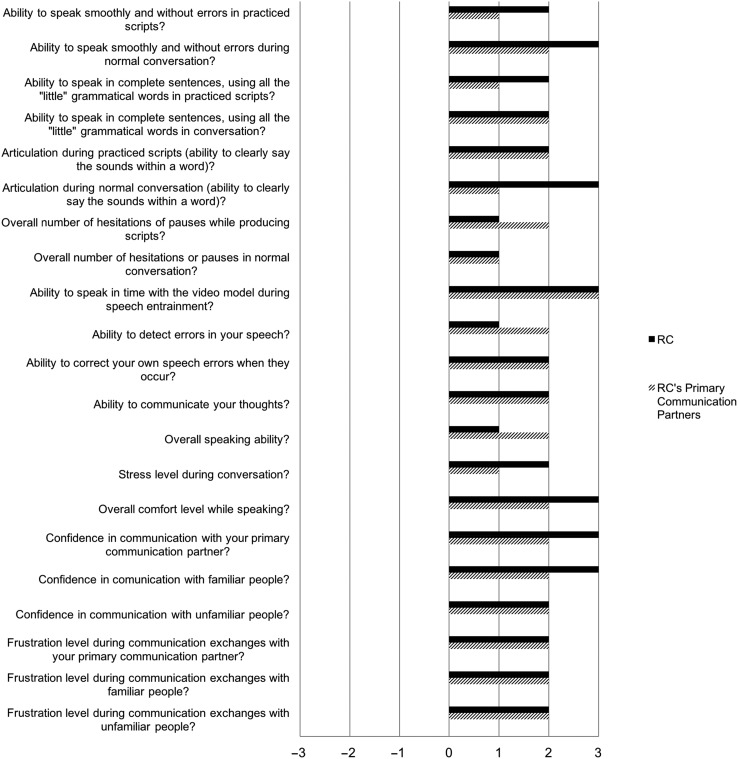
Self-Assessment and Communication Partner Assessment of Change
The items and results from the post-treatment survey are reported in Appendix A. In summary, both R. C. and her communication partners reported improvement on all items assessing treatment-specific effects (e.g., ability to speak smoothly and without errors in practiced scripts) and on items assessing changes in communication more broadly (e.g., ability to speak in complete sentences in conversation). The mean rating for R. C. was 2.1, corresponding to a rating between “better” and “a lot better,” and the mean rating for R. C.'s communication partners was 1.8, corresponding to a rating between “somewhat better” and “better.”
Discussion
To our knowledge, this is the first study to report outcomes from a script training intervention administered to a bilingual speaker with aphasia. In this study, we investigated the effectiveness of a script training protocol administered to a 66-year-old bilingual (Spanish–English) female (R. C.) with borderline fluent/anomic aphasia and concomitant motor speech impairment. The treatment approach, VISTA, utilizes scripts that are personalized in content and tailored in rate of speech for practice stimuli. In addition to within-language treatment effects, we were interested in examining CLT effects. More specifically, to examine whether cognates facilitated CLT, we manipulated cognate density so that one cognate-dense script was treated in each language.
Several hypotheses were generated regarding the potential effects of the treatment. It was predicted that R. C. would improve in the number of correct and intelligible words produced for scripted material within each language, with maintenance of gains at follow-up. It was hypothesized that greater CLT might occur from Spanish to English (our participant's L1–L2; given her cognitive-linguistic profile). Furthermore, we hypothesized that a greater magnitude of CLT would occur for scripts that contained a high proportion of cognates relative to scripts containing fewer cognates. Lastly, we hypothesized that treatment would result in an increase in speech rate, grammaticality, and overall intelligibility for trained scripts from pre- to post-treatment.
Primary Outcome Measure
Consistent with our hypothesis, a significant treatment effect was observed for our primary outcome measure of correct and intelligible scripted words (all trained scripts, combined) from pre- to post-treatment, with maintenance of gains observed at follow-up visits (1.5 and 3.5 months post-treatment). R. C. displayed a larger overall effect size for scripts treated in Spanish, as compared to scripts treated in English, and a significant difference in effect sizes was observed when comparing Spanish- and English-trained scripts following all intervention (Spanish followed by English phases). The finding that larger effect sizes resulted following treatment in the language with higher postmorbid proficiency (Spanish; also this participant's L1) is consistent with previous findings in the literature (Kohnert, 2004).
Generalization to Untrained Measures
The impact of training was strongest for trained scripts, as evidenced by a significant difference between the magnitude of treatment effects for trained versus untrained scripts at all time points. Minimal changes were observed in the untrained scripts at post-treatment relative to pre-treatment, as these scripts were not directly targeted during VISTA. In contrast, following treatment, R. C. showed within-language generalization to untrained tasks and targets in Spanish, as evidenced by her improved facility for word recall (significantly higher BNT score and clinically significant change in WAB-R score in Spanish at post-treatment relative to pre-treatment).
Generalization on these measures might be explained by the multiple facets of fluency that script training has the potential to target (i.e., word retrieval, grammar, and articulation). Generalization to a confrontation naming measure and to the Naming and Word Finding subtest of the WAB-R may reflect enhanced word retrieval conferred by repeated retrieval of scripted words during home practice and treatment sessions. In addition, prior to R. C.'s participation in our study, she had received speech therapy in English only. As such, intensive Spanish stimulation provided during treatment may have resulted in improvements in confrontation naming irrespective of the specific nature of the intervention. Nevertheless, the effects of script training on word retrieval are not well understood, with only one study reporting numerical improvements in naming on a formal measure following script training (Bilda, 2011). Accordingly, the potential relation between script training and naming warrants further investigation.
CLT
CLT was observed for treatment administered in both languages, with maintenance of transfer effects documented at 3.5 months post-treatment. Overall, our participant demonstrated bidirectional transfer for trained scripts, with a small advantage for CLT from Spanish to English. Our observation of bidirectional transfer is generally consistent with previous studies (e.g., Edmonds & Kiran, 2006; Kiran & Roberts, 2010) reporting that relatively balanced premorbid proficiency may facilitate generalization within and across languages. Training in Spanish resulted in a somewhat greater degree of unidirectional CLT to English following the Spanish treatment phase, which was amplified following the English treatment phase. This may be explained by our participant's relative difficulty with accessing and producing English (compared to Spanish). By training scripted material in her more accessible poststroke language (Spanish), production of the material in English may have benefited because scripted material provided a structure from which R. C. could base her production of English content. This is consistent with theories of L2 learning, which propose that the L1 provides a substrate for L2 learning (e.g., Kroll & Stewart, 1994; Kroll et al., 2010). Because this participant demonstrated a less robust effect for English-trained scripts, production of that material in Spanish was also rendered somewhat less successful. Moreover, although R. C. was a early sequential bilingual speaker, her first learned language was Spanish, and it is possible that she was accessing her L2 (English) via her L1, as individuals do during L2 learning.
Contrary to our hypothesis, cognate-dense scripts did not facilitate CLT. In fact, z tests revealed that, for both languages, scripts with fewer cognates demonstrated a significantly greater magnitude of CLT relative to cognate-dense scripts. The participant's lesion, which included prominent prefrontal damage, and accompanying executive function deficits (reflected in her difficulty suppressing Spanish) may have impeded the facilitation effect that is often observed with cognates. Consequently, scripts that were cognate dense may have increased competition between lexical units, thereby reducing R. C.'s ability to produce scripted material in the other language. In addition, it should be noted that previous studies that have found CLT effects for cognates provided treatment at the lexical level (Goral et al., 2012; Kohnert, 2004), whereas R. C.'s treatment targeted connected speech. Other studies in the aphasia literature have found that there are likely to be more lexical candidates competing for selection in connected speech than generative or confrontation naming, resulting in higher processing demands in narrative tasks versus picture- naming tasks (Law, Kong, Lai, & Lai, 2015; Wilshire & McCarthy, 2002). Therefore, script training intervention for an individual with language suppression difficulties might serve to boost the competition existing between cognate items.
The evidence for a facilitative cognate effect in bilingual aphasia therapy is not undisputed. As previously discussed, Kurland and Falcon (2011) reported an interference effect for cognate items following a naming intervention. The authors utilize Green's control, activation, and resource framework (Green, 1986) to account for the interference effect of the cognates, which assumes that lexical selection of the target word requires a controlled balance of excitatory and inhibitory resources. Accordingly, the cognate advantage fades when cognitive control circuits are damaged, possibly due to reduced excitatory and inhibitory resources required to either activate the target or suppress the nontarget. The impairment precludes correct selection among competing lexical units such as cognates. Therefore, it is possible that damage to cognitive control mechanisms may have impeded R. C.'s ability to transfer scripts that were cognate dense. In order to better understand the mechanisms that facilitate or impede CLT, more research should be conducted on the impact of brain injury on inhibitory mechanisms involved in language control. Of particular importance is the degree to which such impairments affect a bilingual individual's capacity to access each language and how these factors influence treatment response.
Additional Outcome Measures
Secondary variables of interest included number of grammatical errors (produced per hundred words), speech rate (WPM), and overall intelligibility. Improvements were observed for all secondary variables, although a statistically significant improvement was only observed for grammaticality and overall intelligibility. We attribute these improvements to the multifaceted nature of VISTA, which provides stimulation at linguistic as well as motoric levels of production. Cognate-dense scripts, which yielded the smallest treatment effect, also showed little to no improvement on secondary variables. As previously mentioned, it is possible that cognates increased lexical competition for R. C., which may have also slowed her production and caused her to be more errorful in her production of cognate-dense scripts.
Summary
Findings from this study indicate that script training intervention holds promise for improving speech production and fluency in bilingual speakers with aphasia. The treatment resulted in improved production of scripted material and improved facility in word retrieval and grammar. In addition to these objective gains, our participant and her communication partners reported improvements on skills related to the treatment and improvements in other factors that may influence successful communication (see Appendix A).
Our findings offer evidence that both languages can benefit from treatment, with a clear advantage for this participant's stronger postmorbid and first acquired language. Contrary to other findings (Goral et al., 2012; Kohnert, 2004), our results indicate that cognates may interfere with, rather than facilitate, target word selection regardless of the language of treatment. Whereas cognates may bolster CLT for bilinguals who do not demonstrate difficulty with inhibition or language suppression, it is possible that those who present with these deficits may not show a CLT effect for cognates.
Accordingly, clinicians delivering treatment to bilingual individuals who have cognitive–linguistic profiles similar to our participant's should be cautious when considering incorporation of a high proportion of cognates in training stimuli. It is unknown, however, whether R. C.'s lack of CLT for cognates was related to the specific treatment approach we implemented, to her cognitive–linguistic and lesion profile, or both. Thus, future studies should manipulate cognate density using different treatment approaches and should consider site of lesion (i.e., whether there is a relation between relatively spared vs. damaged regions and cognate facilitation) to discern whether a participant’s behavioral and neural profile can predict their ability to benefit from cognate inclusion.
Acknowledgments
This research was supported by Grants R03DC013403 and R01DC016291 awarded to Maya L. Henry and Grant F31DC016229 awarded to Stephanie M. Grasso by the National Institute on Deafness and Communicative Disorders. The authors would like to thank Kristin Schaffer for her assistance with completing ratings on the ASRS.
Appendix A
Self-Assessment and Communication Partner Assessment of Change
Post-treatment survey responses from R. C. and her primary communication partners. The x-axis displays ratings for each item on the survey, on the following scale: 3 = a lot better, 2 = better, 1 = somewhat better, 0 = unchanged, −1 = somewhat worse, −2 = worse, and −3 = a lot worse.
Appendix B
Ratings for Participant R. C. Using the Apraxia of Speech Rating Scale (Strand et al., 2014)
| Total of Ratings: 2 | |||
| Aphasia Severity: 2; moderate | |||
| AOS Severity: 2; moderate | |||
| Dysarthria Severity: 2; moderate | |||
| Rater 1 | Rater 2 | Consensus ratings | |
| 1 AOS: primary distinguishing features (no overlap with dysarthria or aphasia). One or more must be present for diagnosis of AOS. | |||
| 1.1 Distorted sound substitutions | 2 | 2 | |
| 1.2 Distorted sound additions (not including intrusive schwa) | 2 | 2 | |
| 1.3 Increased sound distortions or distorted sound substitutions with increased utterance length or increased syllable/word articulatory complexity | 3 | 2 | 3 |
| 1.4 Increased sound distortions or distorted sound substitutions with increased speech rate | 2 | 2 | |
| 1.5 Inaccurate (off-target in place or manner) speech AMR's (alternating motion rates, as in rapid repetition of “puh puh puh”) | 1 | 1 | |
| 1.6 Reduced words per breath group relative to maximum vowel duration | 1 | 1 | |
| 2 Distinguishing features unless dysarthria present | |||
| 2.1 Syllable segmentation within words > 1 syllable | 0d | 0d | |
| 2.2 Syllable segmentation across words in phrases/sentences | 2d | 1d | 1d |
| 2.3 Sound distortions | 3d | 3d | |
| 2.4 Slow overall speech rate | 2d | 3d | 3d |
| 2.5 Lengthened vowel &/or consonant segments | 0d | 0d | |
| 2.6 Lengthened intersegment durations (between sounds, syllables, words, or phrases; possibly filled, including intrusive schwa) | 1d | 1d | |
| 3 Distinguishing features unless aphasia present | |||
| 3.1 Deliberate, slowly sequenced, segmented, &/or distorted (including distorted substitutions) speech SMRs in comparison to speech AMRs | 2a | 2a | |
| 3.2 Audible or visible articulatory groping; speech initiation difficulty; false starts/restarts | 1a | 1a | |
| 4 Distinguishing features unless dysarthria &/or aphasia present | |||
| 4.1 Sound or syllable repetitions | 1ad | 0ad | 1ad |
| 4.2 Sound prolongations (beyond lengthened segments) | 0ad | 0ad | |
Funding Statement
This research was supported by Grants R03DC013403 and R01DC016291 awarded to Maya L. Henry and Grant F31DC016229 awarded to Stephanie M. Grasso by the National Institute on Deafness and Communicative Disorders.
Footnotes
In this article, we use the term cross-linguistic transfer, or CLT, to refer to cross-language generalization of treatment gains and reserve the term generalization to refer to within-language generalization to untrained stimuli.
For untrained scripts, performance on all secondary variables of interest remained relatively stable from pre- to post-treatment (see Figure 5).
References
- American Speech-Language-Hearing Association. (2017). Demographic profile of ASHA members providing bilingual services. Retrieved from https://www.asha.org/uploadedFiles/Demographic-Profile-Bilingual-Spanish-Service-Members.pdf
- Aphasia Bank: Informal Spanish Translation (adapted from Spanish translation of WAB). (2014). Retrieved from https://aphasia.talkbank.org/protocol/Spanish/
- Baker F. A. (2006). Modifying the melodic intonation therapy program for adults with severe non-fluent aphasia. Music Therapy, 18(2), 110–114. https://doi.org/10.1093/mtp/18.2.110 [Google Scholar]
- Beeson P. M., & Robey R. R. (2006). Evaluating single-subject treatment research: Lessons learned from the aphasia literature. Neuropsychology Review, 16(4), 161–169. https://doi.org/10.1007/s11065-006-9013-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belin P., Van Eeckhout P., Zilbovicius M., Remy P., François C., Guillaume S., … Samson Y. (1996). Recovery from nonfluent aphasia after melodic intonation therapy. American Academy of Neurology, 47, 902–905. [DOI] [PubMed] [Google Scholar]
- Bilda K. (2011). Video-based conversational script training for aphasia: A therapy study. Aphasiology, 25(2), 191–201. https://doi.org/10.1080/02687031003798254 [Google Scholar]
- Boyle M. (1989). Reducing phonemic paaphasias in the connected speech of a conduction aphasic subject. Clinical Aphasiology, 18, 379–393. [Google Scholar]
- Breining B. L., Lala T., Cuitiño M. M., Manes F., Peristeri E., Tsapkini K., … Hillis A. E. (2015). A brief assessment of object semantics in primary progressive aphasia. Aphasiology, 29(4), 488–505. https://doi.org/10.1080/02687038.2014.973360 [Google Scholar]
- Caramazza A. (1997). How many levels of processing are there in lexical access? Cognitive Neuropsychology, 14(1), 177–208. https://doi.org/10.1080/026432997381664 [Google Scholar]
- Caruso C., & Szabo G. B. (2014). Script training in a bilingual person with aphasia: A case study. Paper presented at the ASHA Convention, Orlando, FL. [Google Scholar]
- Cherney L. R. (2010). Oral reading for language in aphasia: Impact of aphasia severity on cross-modal outcomes in chronic nonfluent aphasia. Seminars in Speech and Language, 31, 42–51. https://doi.org/10.1055/s-0029-1244952 [DOI] [PubMed] [Google Scholar]
- Cherney L. R., Halper A. S., Holland A. L., & Cole R. (2008). Computerized script training for aphasia: Preliminary results. American Journal of Speech-Language Pathology, 17, 19–34. https://doi.org/10.1044/1058-0360(2008/003) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherney L. R., Halper A. S., & Kaye R. C. (2011). Computer-based script training for aphasia: Emerging themes from post-treatment interviews. Journal of Communication Disorders, 44(4), 493–501. https://doi.org/10.1016/j.jcomdis.2011.04.002 [DOI] [PubMed] [Google Scholar]
- Cherney L. R., Kaye R. C., & Van Vuuren S. (2014). Acquisition and maintenance of scripts in aphasia: A comparison of two cuing conditions. American Journal of Speech-Language Pathology, 23(2), S343–S360. https://doi.org/10.1044/2014_AJSLP-13-0097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa A. (2005). Lexical access in bilingual production. In Kroll J. F. & de Groot A. M. B. (Eds.), Handbook of bilingualism: Psycholinguistic approaches (pp. 289–307). New York, NY: Oxford University Press. [Google Scholar]
- Costa A., Colomé À., & Caramazza A. (2000). Lexical access in speech production: The bilingual case. Psicológica, 21, 403–437. [Google Scholar]
- Costa A., Santesteban M., & Caño A. (2005). On the facilitatory effects of cognate words in bilingual speech production. Brain and Language, 94, 94–103. https://doi.org/10.1016/j.bandl.2004.12.002 [DOI] [PubMed] [Google Scholar]
- De Groot A. M. B. (1992). Bilingual lexical representation: A closer look at conceptual representations. In Frost R. & Katz L. (Eds.), Orthography, phonology, morphology and meaning. Amsterdam, the Netherlands: Elsevier. [Google Scholar]
- Dijkstra T., & van Hell J. G. (2003). Testing the language mode hypothesis using trilinguals. International Journal of Bilingual Education and Bilingualism, 6(1), 2–16. https://doi.org/10.1080/13670050308667769 [Google Scholar]
- Dijkstra T., & van Heuven W. J. B. (1998). The BIA model and bilingual word recognition. In Grainger J. & Jacobs A. M. (Eds.), Scientific psychology series. Localist connectionist approaches to human cognition (pp. 189–225). Mahwah, NJ: Erlbaum. [Google Scholar]
- Edmonds L. A., & Kiran S. (2006). Effect of semantic naming treatment on crosslinguistic generalization in bilingual aphasia. Journal of Speech, Language, and Hearing Research, 49, 729–748. [DOI] [PubMed] [Google Scholar]
- Edmonds L. A., Nadeau S. E., & Kiran S. (2009). Effect of verb network strengthening treatment (VNeST) on lexical retrieval of content words in sentences in persons with aphasia. Aphasiology, 23(3), 402–424. https://doi.org/10.1080/02687030802291339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faroqi-shah Y., Frymark T., Mullen R., & Wang B. (2010). Effect of treatment for bilingual individuals with aphasia: A systematic review of the evidence. Journal of Neurolinguistics, 23(4), 319–341. https://doi.org/10.1016/j.jneuroling.2010.01.002 [Google Scholar]
- Ferrand L., & Humphreys G. W. (1996). Transfer of refractory states across languages in a global aphasic patient. Cognitive Neuropsychology, 13(8), 1163–1191. https://doi.org/10.1080/026432996381692 [Google Scholar]
- Flesch R. (1948). A new readability yardstick. Journal of Applied Psychology, 32, 221–233. [DOI] [PubMed] [Google Scholar]
- Florance C. L., & Deal J. L. (1977). A treatment protocol for nonverbal stroke patients. In Brookshire R. H. (Ed.), Clinical aphasiology (Vol. 7, pp. 59–67). Minneapolis, MN: BRK Publishers. [Google Scholar]
- Folstein M. F., Folstein S. E., & McHugh P. R. (1975). “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189–198. https://doi.org/10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- Fridriksson J., Basilakos A., Hickok G., Bonilha L., & Rorden C. (2015). ScienceDirect speech entrainment compensates for Broca's area damage. Cortex, 69, 68–75. https://doi.org/10.1016/j.cortex.2015.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fridriksson J., Hubbard H. I., Hudspeth S. G., Holland A. L., Bonilha L., Fromm D., & Rorden C. (2012). Speech entrainment enables patients with Broca's aphasia to produce fluent speech. Brain, 135(12), 3815–3829. https://doi.org/10.1093/brain/aws301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg S., Haley K. L., & Jacks A. (2012). Script training and generalization for people with aphasia. American Journal of Speech-Language Pathology, 21, 222–239. https://doi.org/10.1044/1058-0360(2012/11-0056) [DOI] [PubMed] [Google Scholar]
- Goral M., Rosas J., Conner P. S., Maul K. K., & Obler L. K. (2012). Effects of language pro fi ciency and language of the environment on aphasia therapy in a multilingual. Journal of Neurolinguistics, 25(6), 538–551. https://doi.org/10.1016/j.jneuroling.2011.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green D. W. (1986). Control, activation, and resource: A framework and a model for the control of speech in bilinguals. Brain and Language, 223, 210–223. https://doi.org/10.1016/0093-934X(86)90016-7 [DOI] [PubMed] [Google Scholar]
- Hamers J. F., & Blanc M. H. A. (2000). Bilinguality and bilingualism (2nd ed.). Cambridge, United Kingdom: Cambridge University Press. [Google Scholar]
- Helm-Estabrooks N., & Nicholas M. (2000). Sentence production program for aphasia (SPPA). Austin, TX: Pro-Ed. [Google Scholar]
- Henry M. L., Hubbard H. I., Grasso S. M., Mandelli M. L., Wilson S. M., Sathishkumar M. T., … Gorno-Tempini M. L. (2018). Retraining speech production and fluency in nonfluent/agrammatic primary progressive aphasia. Brain, 141(6), 1799–1814. https://doi.org/10.1093/brain/awy101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry M. L., Rising K., DeMarco A. T., Miller B. L., Gorno-Tempini M. L., & Beeson P. M. (2013). Examining the value of lexical retrieval treatment in primary progressive aphasia: Two positive cases. Brain and Language, 127(2), 145–156. https://doi.org/10.1016/j.bandl.2013.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hothorn T., & Hornik K. (2006). Unbiased recursive partitioning: A conditional inference framework. Journal of Computational and Graphical Statistics, 15(3), 651–674. [Google Scholar]
- Howard D., & Patterson K.E. (1992). The Pyramids and Palm Trees Test: A test of semantic access from words and pictures. Thames Valley Test Company.
- Huber W., Poeck K., & Willmes K. (1984). The Aachen Aphasia Test. Advances in Neurology, 42, 291–303. [PubMed] [Google Scholar]
- Kaplan E., Goodglass H., & Weintraub S. (2001). Boston Naming Test–Second Edition (BNT-2). Austin, TX: Pro-Ed. [Google Scholar]
- Kaplan E., Goodglass H., & Weintraub S. (2005). Test de Vocabulario de Boston (2nd ed.). Madrid, Spain: Editorial Medica Panamericana. [Google Scholar]
- Kearns K. P. (Ed.). (1985). Response elaboration training for patient initiated utterances. Clinical Aphasiology, 15, 196–204. [Google Scholar]
- Kertesz A. (1982). Western Aphasia Battery Test manual. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Kertesz A. (2006). Western Aphasia Battery–Revised. San Antonio, TX: Pearson. [Google Scholar]
- Kiran S., Peña E., Bedore L., & Sheng L. (2010). Evaluating the relationship between category generation and language use and proficiency. Paper presented at the Donostia Workshop on Neurobilingualism, San Sebastian, Spain. [Google Scholar]
- Kiran S., & Roberts P. M. (2010). Semantic feature analysis treatment in Spanish–English and French–English bilingual aphasia. Aphasiology, 24, 231–261. [Google Scholar]
- Kohnert K. (2004). Cognitive and cognate-based treatments for bilingual aphasia: A case study. Brain and Language, 91, 294–302. https://doi.org/10.1016/j.bandl.2004.04.001 [DOI] [PubMed] [Google Scholar]
- Kohnert K. (2009). Cross-language generalization following treatment in bilingual speakers with aphasia: A review. Seminars in Speech and Language, 30(3), 174–186. https://doi.org/10.1055/s-0029-1225954 [DOI] [PubMed] [Google Scholar]
- Kramer J. H., Jurik J., Sha S. J., Rankin K. P., Rosen H. J., Johnson J. K., & Miller B. L. (2003). Distinctive neuropsychological patterns in frontotemporal dementia, semantic dementia and Alzheimer disease. Cognitive and Behavioral Neurology: Official Journal of the Society for Behavioral and Cognitive Neurology, 16(4), 211–218. https://doi.org/10.1097/00146965-200312000-00002 [DOI] [PubMed] [Google Scholar]
- Kroll J. F., Bobb S. C., Misra M., & Guo T. (2008). Language selection in bilingual speech: Evidence for inhibitory processes. Acta Psychologica, 128(3), 416–430. https://doi.org/10.1016/j.actpsy.2008.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroll J. F., & Stewart E. (1994). Category interference in translation and picture naming: Evidence for asymmetric connections between bilingual memory representations. Journal of Memory and Language, 33(2), 149–174. https://doi.org/10.1006/jmla.1994.1008 [Google Scholar]
- Kroll J. F., Van Hell J. G., Tokowicz N., & Green D. W. (2010). The revised hierarchical model: A critical review and assessment. Bilingualism: Language and Cognition, 13(3), 373–381. https://doi.org/10.1017/S136672891000009X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurland J., & Falcon M. (2011). Effects of cognate status and language of therapy during intensive semantic naming treatment in a case of severe nonfluent bilingual aphasia. Clinical Linguistics & Phonetics, 25(6–7), 584–600. https://doi.org/10.3109/02699206.2011.565398 [DOI] [PubMed] [Google Scholar]
- LaPointe L. (2011). Multicultural and multi-linguistic issues. In Aphasia and related neurogenic language disorders (4th ed., pp. 69–79). New York, NY: Thieme. [Google Scholar]
- Law S.-P., Kong A. P.-H., Lai L. W.-S., & Lai C. (2015). Effects of context and word class on lexical retrieval in Chinese speakers with anomic aphasia. Aphasiology, 29(1), 81–100. https://doi.org/10.1080/02687038.2014.951598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J. B., Kaye R. C., & Cherney L. R. (2009). Conversational script performance in adults with non-fluent aphasia: Treatment intensity and aphasia severity. Aphasiology, 23, 885–897. https://doi.org/10.1080/02687030802669534 [Google Scholar]
- Logan G. D. (1988). Toward an instance theory of automatization. Psychological Review, 95, 492–527. https://doi.org/10.1037/0033-295X.95.4.492 [Google Scholar]
- MacWhinney B., & Snow C. (1985). The child language data exchange system. Journal of Child Language, 12, 271–296. [DOI] [PubMed] [Google Scholar]
- Manheim L. M., Halper A. S., & Cherney L. (2009). Patient-reported changes in communication after computer-based script training for aphasia. Archives of Physical Medicine and Rehabilitation, 90(4), 623–627. https://doi.org/10.1016/j.apmr.2008.10.022 [DOI] [PubMed] [Google Scholar]
- Marian V., Bartolotti J. Chabal S., & Shook A. (2012). CLEARPOND: Cross-linguistic easy-access resource for phonological and orthographic neighborhood densities. PLOS ONE, 7(8), e43230 https://doi.org/10.1371/journal.pone.0043230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinzer M., Obleser J., Flaisch T., Eulitz C., & Rockstroh B. (2007). Recovery from aphasia as a function of language therapy in an early bilingual patient demonstrated by fMRI. Neuropsychologia, 45, 1247–1256. https://doi.org/10.1016/j.neuropsychologia.2006.10.003 [DOI] [PubMed] [Google Scholar]
- Murray L. L. (2015). Bilingual aphasia treatment: Clinical recommendations regarding secondary language treatment, cross-language transfer, and the use of language brokers await additional research. Evidence-based Communication Assessment and Intervention, 9(1), 1–6. https://doi.org/10.1080/17489539.2014.960645 [Google Scholar]
- Paradis M., & Libben G. (1987). The assessment of bilingual aphasia. Mahwah, NJ: Erlbaum. [Google Scholar]
- Pellegrino F., Coupe C., & Marsico E. (2011). A cross-language perspective on speech information rate. Language, 87(3), 539–558. [Google Scholar]
- R Core Team. (2016). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; Retrieved from http://www.R-project.org/ [Google Scholar]
- Roberts P. M., & Deslauriers L. (1999). Picture naming of cognate and non-cognate nouns in bilingual aphasia. Journal of Communication Disorders, 32(1), 1–23. https://doi.org/10.1016/S0021-9924(98)00026-4 [DOI] [PubMed] [Google Scholar]
- Robey R. R., Schultz M. C., Crawford A. B., & Sinner C. A. (1999). Review: Single-subject clinical-outcome research: Designs, data, effect sizes, and analyses. Aphasiology, 13, 445–473. https://doi.org/10.1080/026870399402028 [Google Scholar]
- Shewan C. M., & Donner A. P. (1988). A comparison of three methods to evaluate change in the spontaneous language of aphasic individuals. Journal of Communication Disorders, 21, 171–176. [DOI] [PubMed] [Google Scholar]
- Stadie N., Springer L., De Bleser R., & Burk F. (1995). Oral and written naming in a multilingual patient. In Paradis M. (Ed.), Aspects of bilingual aphasia (pp. 85–100). New York, NY: Elsevier Science. [Google Scholar]
- Strand E. A., Duffy J. R., Clark H. M., & Josephs K. (2014). The Apraxia of Speech Rating Scale: A tool for diagnosis and description of apraxia of speech. Journal of Communication Disorders, 51, 43–50. https://doi.org/10.1016/j.jcomdis.2014.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson C. K., & Shapiro L. (2005). Treating agrammatic aphasia within a linguistic framework: Treatment of underlying forms. Aphasiology, 19, 1021–1026. https://doi.org/10.1080/02687030544000227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson C. K., Weintraub S., & Mesulam M. (2011). Northwestern Anagram Test. Evanston, IL: Northwestern University; Retrieved from http://northwestern.flintbox.com/public/project/19927/ [Google Scholar]
- U.S. Census Bureau. (2013). Language use in the United States: 2011 American community survey reports. Retrieved from https://www2.census.gov/library/publications/2013/acs/acs-22/acs-22.pdf
- U.S. Census Bureau. (2014). Annual estimates of the resident population by sex, race, and hispanic origin for the United States. Retrieved from https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk
- Van Hell J. G., & De Groot A. M. B. (1998). Conceptual representation in bilingual memory. Effects of concreteness and cognate status in word association. Bilingualism: Language and Cognition, 1, 193–211. https://doi.org/10.1017/S1366728998000352 [Google Scholar]
- Wambaugh J. L., Martinez A. L., & Alegre M. N. (2001). Qualitative changes following application of modified response elaboration training with apraxic aphasic speakers. Aphasiology, 15, 965–976. https://doi.org/10.1080/02687040143000320 [Google Scholar]
- Wambaugh J. L., & Nessler C. (2004). Modification of sound production treatment for apraxia of speech: Acquisition and generalisation effects speech: Acquisition and generalisation effects. Aphasiology, 18, 407–427. https://doi.org/10.1080/02687030444000165 [Google Scholar]
- Weintraub S., Mesulam M. M., Wieneke C., Rademaker A., Rogalski E. J., & Thompson C. K. (2009). The Northwestern Anagram Test: Measuring sentence production in primary progressive aphasia. American Journal of Alzheimer's Disease and Other Dementias, 24, 408–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilshire C. E., & McCarthy R. A. (2002). Evidence for a context-sensitive word retrieval disorder in a case of nonfluent aphasia. Cognitive Neuropsychology, 19, 165–186. https://doi.org/10.1080/02643290143000169 [DOI] [PubMed] [Google Scholar]
- Wisenburn B., & Mahoney K. (2009). A meta-analysis of word-finding treatments for aphasia. Aphasiology, 23(11), 1338–1352. https://doi.org/10.1080/02687030902732745 [Google Scholar]
- Youmans G., Holland A., Muñoz M., & Bourgeois M. (2005). Script training and automaticity in two individuals with aphasia. Aphasiology, 19(3–5), 435–450. https://doi.org/10.1080/02687030444000877 [Google Scholar]
- Youmans G., Youmans S. R., & Hancock A. B. (2011). Script training treatment for adults with apraxia of speech. American Journal of Speech-Language Pathology, 20, 23–37. https://doi.org/10.1044/1058-0360(2010/09-0085) [DOI] [PubMed] [Google Scholar]