Abstract
Background
Schistosomiasis is a widespread public health concern in the poorest regions of the world. The principal control strategy is regular praziquantel administration to school-aged children in endemic areas. With calls for the elimination of schistosomiasis as a public health problem, expanding praziquantel delivery to all community members has been advocated. This systematic review and meta-analysis compares the impact of community-wide and child-targeted praziquantel distribution on schistosomiasis prevalence and intensity in school-aged children.
Methodology/Principal findings
We searched MEDLINE, Embase and Web of Science to identify papers that reported schistosome prevalence before and after praziquantel administration, either to children only or to all community members. Extracted data included Schistosoma species, drug administration strategy, number of treatment rounds, follow-up interval and prevalence and intensity before and after treatment. We used inverse variance weighted generalised linear models to examine the impact of mass versus targeted drug administration on prevalence reduction, and weighted boxplots to examine the impact on infection intensity reduction. This study is registered with PROSPERO, number CRD42018095377.
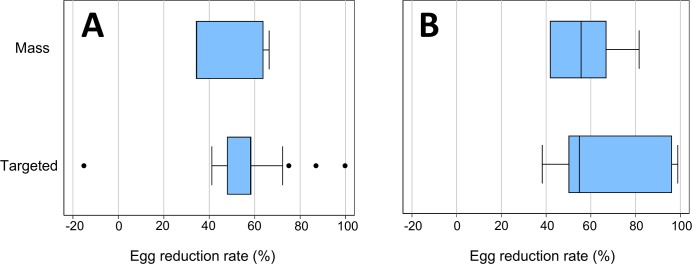
In total, 34 articles were eligible for systematic review and 28 for meta-analysis. Schistosoma mansoni was reported in 20 studies; Schistosoma haematobium in 19 studies, and Schistosoma japonicum in two studies. Results of generalised linear models showed no detectable difference between mass and targeted treatment strategies on prevalence reduction in school-aged children for S. mansoni (odds ratio 0.47, 95%CI 0.13–1.68, p = 0.227) and S. haematobium (0.41, 95%CI 0.06–3.03, p = 0.358). Box plots also showed no apparent differences in intensity reduction between the two treatment strategies.
Conclusions/Significance
The results of this meta-analysis do not support the hypothesis that community-wide treatment is more effective than targeted treatment at reducing schistosomiasis infections in children. This may be due to the relatively small number of included studies, insufficient treatment coverage, persistent infection hotspots and unmeasured confounders. Further field-based studies comparing mass and targeted treatment are required.
Author summary
Schistosomiasis is a neglected tropical disease, caused by parasitic worms, that affects more than 143 million people worldwide. Chronic infections can lead to significant morbidity including kidney damage, anaemia, malnutrition, infertility and growth impairment. School-aged children between six and 15 years are often targeted for regular treatment with praziquantel in large-scale drug delivery programs, because they suffer a disproportionate burden of morbidity. On the other hand, a mass drug delivery strategy that treats all members of the community has been suggested in a move towards elimination of schistosomiasis as a public health problem. In this systematic review, we assess the impact of community-wide versus children-only praziquantel distribution in reducing schistosomiasis infections in school-aged children. We did not detect a difference between mass and targeted treatment strategies, possibly due to factors including insufficient treatment coverage and persistent sources of reinfection. Addressing these factors may assist in optimising control programs.
Introduction
Schistosomiasis is a water-borne neglected tropical disease (NTD) that infects an estimated 143 million people worldwide [1]. Its global disease burden is estimated at 2.5 million disability-adjusted life years, and 220 million people across 52 countries live in areas endemic for schistosomiasis [1, 2]. The disease is caused by parasitic trematodes of the Schistosoma genus, hosted in freshwater Bulinus snails, and manifests in intestinal (Schistosoma mansoni, Schistosoma japonicum, Schistosoma mekongi, Schistosoma guineensis and Schistosoma intercalatum) and urogenital (Schistosoma haematobium) forms [3]. Transmission occurs when infected individuals contaminate freshwater sources with faeces or urine containing parasite eggs. The eggs hatch, releasing miracidia into the water that penetrate the host snails and develop into infective cercariae. The cercariae are released from the snails and infect humans by penetrating the skin during contact with contaminated water [4]. Infection is often endemic in rural agricultural or fishing populations with poor sanitation [4]. Chronic infections cause significant morbidity including renal damage, anaemia, malnutrition, infertility and poor physical and cognitive development. Less frequently they can cause fatal complications from renal failure, portal hypertension and bladder cancer [4].
Praziquantel, a broad-spectrum anthelminthic, has been used for over 40 years as the cornerstone of schistosomiasis control, due to its safety, low cost and efficacy against all Schistosoma species [5, 6]. The World Health Organization (WHO) recommends that school-aged children in endemic areas are treated either annually (if prevalence is above 50% in school-aged children), every two years (if prevalence is between 10% and 49% in school-aged children), or upon entering and leaving primary school (if prevalence is lower than 10% in school-aged children) [5]. The WHO recommendations additionally suggest treating special groups of at-risk adults if schistosomiasis prevalence is above 10% in school-aged children, and entire communities if prevalence in school-aged children is above 50% [5, 7]. In the WHO’s landmark roadmap for NTD control, released in 2012, schistosomiasis control targets focus exclusively on school-aged children [8]. By 2020, the WHO target is that 75% of school-aged children at risk of schistosomiasis should be receiving regular praziquantel [8]. This target was set because the donations of praziquantel were sufficient to cover only this age group [9], and the WHO wanted to indicate an attainable goal for 2020. Globally, 68% of at-risk school-aged children received praziquantel in 2017, while coverage of at-risk adults was much lower at 16.9% [2].
With calls for elimination of schistosomiasis as a public health problem, defined by the WHO as less than 1% prevalence of heavy-intensity infections among school-aged children [7, 10], the effectiveness of treatment targeted to children has been called into question [11, 12]. It has been suggested that treatment should instead be delivered community-wide, to reduce disease prevalence and transmission to children from other vulnerable members in the community [12, 13], and minimise persistent untreated populations that can significantly impact on the success of control programs [14]. Results from mathematical modelling suggest that “mass” (community-wide) treatment is more effective for controlling schistosome infection than a “targeted” (children-only) program; however, this is dependent on local epidemiological settings, including pre-control burden in adults, school enrolment rates, and transmission intensity [14]. Additionally, although the outright cost of administering treatment to the entire community is higher than treating school-aged children only, modelling has shown community-wide drug administration to be a highly cost-effective strategy across different prevalence settings [15]. With many child-targeted programs being conducted through schools, community-wide treatment strategies would have the added benefit of increasing treatment coverage of non-enrolled school-aged children [16].
The Schistosomiasis Consortium for Operational Research and Evaluation (SCORE) has been established to answer strategic questions about schistosomiasis control and elimination. A number of trials have been implemented to assess the effectiveness of different control strategies in reducing the burden of active infection [17–21]. The results of these trials have been inconsistent, with some studies finding that community-wide treatment is more effective at reducing schistosome prevalence [22], whereas others report no significant difference between community-wide and child-targeted treatment [17, 20, 21].
To our knowledge, there is no systematic synthesis comparing mass and targeted delivery strategies (see Box 1) for schistosomiasis control in terms of their impact on schistosomiasis prevalence and intensity among children. This systematic review and meta-analysis aims to address this gap. Specific aims of this study are: (a) to summarise existing literature reporting the effects of mass and targeted praziquantel distribution on schistosomiasis prevalence and intensity in school-aged children, and (b) to examine the differential effect of mass and targeted praziquantel delivery on schistosomiasis prevalence and intensity in school-aged children.
Box 1. Definitions of “mass” and “targeted” drug delivery in this paper
Throughout this paper, we refer to “mass” and “targeted” drug delivery strategies, as defined by the World Health Organization:
Mass drug administration: the entire population of a given area is given anthelminthic drugs at regular intervals, irrespective of the individual infection status [23]. This is also known as community-wide treatment.
Targeted drug administration: specific risk groups in the population (defined by age, sex or other social characteristic) are treated at regular intervals, irrespective of infection status [23]. For the purposes of this paper, targeted drug administration refers to treatment targeted specifically to children.
Methods
Search strategy and selection criteria
This systematic review and meta-analysis was conducted according to PRISMA guidelines [24] (see S1 Checklist) and is available in PROSPERO, registration number CRD42018095377. Eligible studies were those that reported prevalence or intensity of schistosomiasis (any or all species) infection, before and after mass or targeted delivery of praziquantel. We included longitudinal studies as well as repeated cross-sectional studies in this review. Randomised controlled trials were included when randomisation was performed at the community or school level. There was no restriction on date or language of publication, geographical area, or length of study.
Studies were excluded if: treatment was delivered only to infected individuals; positive individuals were re-treated shortly after initial drug administration; all follow-up intervals (defined as the time between drug administration and examination) fell outside of a two month to 18-month timeframe; treatment intervals or follow-up times were not provided; or the drug administration strategy changed (from mass to targeted or vice versa) during the study with no interim data reported. Studies were excluded from quantitative analysis if they did not report initial and/or follow-up sample sizes.
We searched for studies through the databases MEDLINE, Embase and Web of Science on 15 February 2019. The following search terms were used: (a) disease-related terms: “Schistosomiasis” or “Bilharzia” or “Schistosoma” or “Schistosoma mansoni” or “Schistosoma haematobium” or “Schistosoma japonicum” or “Schistosoma mekongi” or “Schistosoma guineensis” or “Schistosoma intercalatum” or “Schistosome” or “Blood flukes” or “Trematode” or “Trematoda” or “Trematode infections” or “Trematode worms”, and (b) intervention-related terms: “Praziquantel” or “PZQ” or “Drug therapy” or “Chemotherapy” or “Preventive chemotherapy” or “Mass drug administration” or “Community based treatment” or “School based treatment”. The complete search strategy can be found in S1 Appendix. Additional studies were identified by hand-searching relevant review paper reference lists [14, 16, 25–31], monitoring the SCORE publication list, and contacting experts in the field.
Following de-duplication, studies were screened by title and abstract, followed by retrieval of full-text articles. All full-texts were then screened for eligibility against the study protocol. Articles published in English were examined by DMC and NEC. Articles published in languages other than English were screened by researchers fluent in those languages.
Data extraction
Data were extracted from included studies by DMC and verified by NEC. Extracted data included initial and follow-up prevalence and intensity of the reported Schistosoma species; study location, design and duration; drug administration strategy (mass or targeted); drug administration platform (school-based, fixed community site or mobile community drug distributors); drug dose; number of treatment rounds; treatment interval(s); treatment coverage; diagnostic method; and interval between drug administration and follow-up.
Where studies reported multiple treatment arms with different treatment or follow-up intervals, data from each study arm were extracted. In studies with a control group that received drug treatment only and groups with additional interventions (e.g. health education), only data from the control group were extracted.
We contacted nine authors to request additional information, including aggregated follow-up prevalence and intensity data, follow-up interval, initial and follow-up sample sizes, praziquantel dose and interim prevalence data when delivery strategies changed during the study. Additional data on the number of infected individuals and intensity of infection were received from one study [21].
Study quality was assessed using a modified version of a validated scale designed to assess risk of bias in prevalence studies [32], as reported previously [26]. Studies were assessed against nine criteria encompassing internal and external validity.
Statistical analysis
Analyses were performed using a similar methodology to our previously-reported meta-analysis comparing mass and targeted drug delivery strategies for soil-transmitted helminth infections [26]. All analyses were performed separately for each Schistosoma species.
To examine the impact of mass and targeted treatment on schistosome prevalence, an inverse variance weighted generalised linear model with robust error variances was used, in order to adjust for a number of key sources of heterogeneity. The covariates for the model were: drug administration strategy (mass or targeted); baseline prevalence; number of treatment rounds between baseline and follow-up; and follow-up interval (i.e., time between final treatment round and follow-up prevalence assessment). Treatment coverage was not included in the primary model because it was not reported in a large number of studies.
Where age-stratified prevalence was not available (two studies [33, 34]), infection prevalence in school-aged children was estimated from community prevalence using scaled age weights reported elsewhere [35]. The first reported assessment of infection prevalence and intensity was used as the baseline for all studies except one, where interim data were used as baseline because data were combined for study arms receiving treatment at different intervals for the first two years of the study [34]. Where multiple rounds of treatment were reported in one study, prevalence and intensity at the final follow-up were used. Where multiple follow-up intervals were reported, the closest to 12 months was used. Some studies were entered into the model multiple times to account for multiple species and strategies (mass or targeted) being reported [17, 21, 22, 36–41].
The outcome variable for the model was prevalence reduction (PReduc). This was defined as (p1-p2)/p1 = 1 –prevalence ratio, where p1 is the initial prevalence proportion and p2 is the post-treatment prevalence proportion. P2/p1 is the prevalence ratio (PRatio). As described previously, PReduc was truncated so that any increase between initial prevalence and follow-up prevalence would be reset to zero [26]. Coefficients were exponentiated to generate weighted odds ratios. Any study weights that were more than five times greater than the upper quartile were truncated and substituted with the threshold weight.
A secondary analysis was performed to pool prevalence reduction for each Schistosoma species. This was done by pooling PRatio, but results are reported as 1 –PRatio = PReduc (non-truncated). Results from each study were pooled using the inverse variance heterogeneity model [42]. Heterogeneity was assessed using Cochran’s Q and Higgins’ I2, with I2 greater than 50% indicating significant heterogeneity. Small-study effects were examined using Egger’s regression test (two-tailed p<0.1 indicating of asymmetry).
A number of sensitivity analyses were performed. Firstly, we added a covariate for reported treatment coverage (categorised as average of 75% coverage or greater across all treatment rounds; average of below 75% coverage across all treatment rounds; or treatment coverage not reported) to the generalised linear model. Secondly, we re-ran the generalised linear model excluding studies that reported greater than 50% initial prevalence, the cut-off for high-endemicity zones [5]. Finally, we re-ran the generalised linear model including follow-up prevalence measured after one treatment round (or closest), rather than after the final treatment round. Additionally, the generalised linear model and secondary meta-analysis were re-run using random effects model weights for comparison.
To compare intensity reduction between mass and targeted studies, given that limited data were available, simple box plots of egg reduction rates were created separately for mass and targeted studies. The box plots were weighted by sample size under the assumption that larger weights designate more accurately measured intensity reductions. Because there were insufficient studies to adjust for number of treatment rounds in this analysis, intensity reduction was calculated after one round of treatment (or closest) for consistency. Egg reduction rate was calculated using mean infection intensity at baseline and follow-up for each study, as follows: Egg reduction rate = (Mean intensitybaseline−Mean intensityfollowup)/(Mean intensitybaseline).
All meta-analyses were performed using MetaXL version 5.3 (Epigear International, Noosa, Australia). To run the generalised linear models and create the weighted box plots, Stata version 15.1 (StataCorp, College Station, TX, USA) was used.
Results
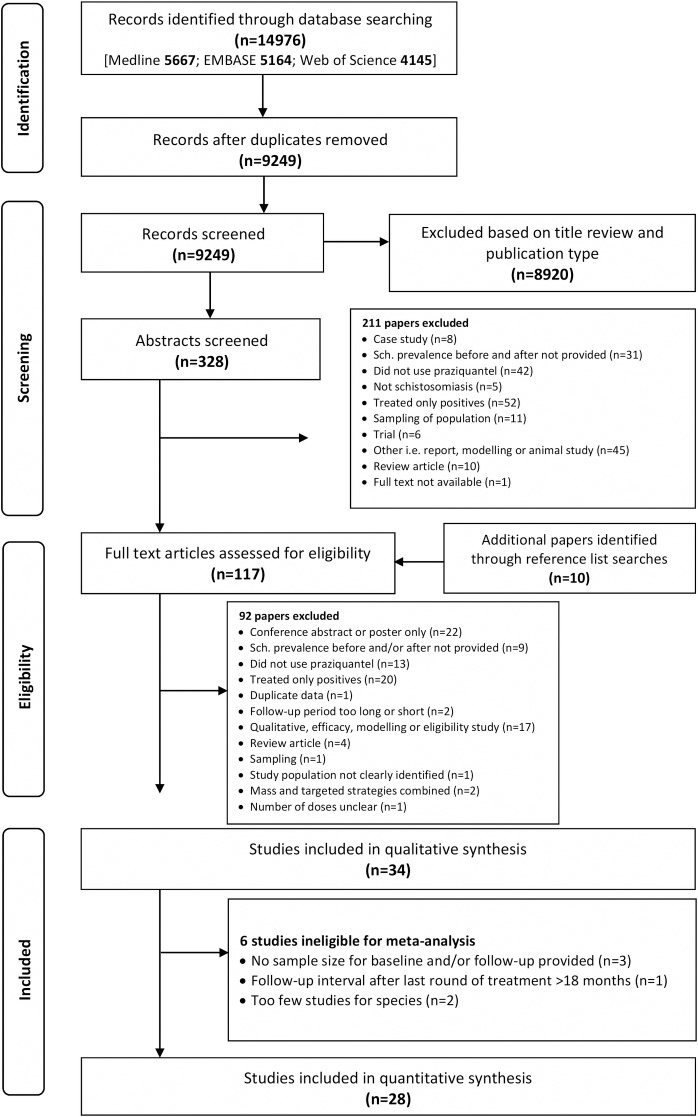
After running the search terms and removing duplicate entries, 9,249 articles were considered for the systematic review process. An additional 10 studies were added through reference list searches. Thirty-four studies met the inclusion criteria for the systematic review. Of these, 28 studies were included for meta-analysis. The screening and selection process is illustrated in Fig 1. A summary of all included studies can be found in Table 1 and S1 Table.
Fig 1. Process of selection of studies for inclusion in this synthesis.
Table 1. Characteristics of included studies for systematic review.
| Author & year | Reference | Location | Drug delivery strategy | Treatment rounds prior to final follow-up | Follow-up interval after last treatment round | Study design | Drug delivery platform(s) |
|---|---|---|---|---|---|---|---|
| Schistosoma mansoni | |||||||
| Abudho et al., 2018* | [43] | Kenya | Targeted | 4 rounds, yearly | 12 months | Repeated cross-sectional | School |
| Ahmed et al., 2012* | [44] | Sudan | Targeted | 1 round | 12 months | Longitudinal | School |
| Al Abaidani et al., 2016* | [45] | Oman | Mass | 4 rounds, yearly | 12 months | Repeated cross-sectional | Not reported |
| Assare et al., 2016* | [18] | Cote d’Ivoire | Targeted | 1 round | 11 months | RCT SCORE |
School |
| Boisier et al., 1998* | [34] | Madagascar | Mass | 4 rounds, yearly or 6 rounds, biannually (final round annual) |
12 months | Longitudinal | Not reported |
| Hodges et al., 2012* | [46] | Sierra Leone | Targeted | 1 round | 6 months | Repeated cross-sectional | School |
| Kaatano et al., 2015 | [47] | Tanzania | Mass | 4 rounds, yearly | 12 months | Repeated cross-sectional | School, fixed community site, mobile CDDs |
| Karanja et al., 2017* | [19] | Kenya | Targeted | 2 or 4 rounds, yearly or biennially | 12, 24 and 36 months | RCT SCORE |
School |
| Mwinzi et al., 2012* | [48] | Kenya | Mass | 1 round | 6 months | Repeated cross-sectional | Mobile CDDs |
| Olsen et al., 2018* | [21] | Tanzania | Both | 2 or 4 rounds, yearly or biennially | 12, 24 and 36 months | RCT SCORE |
School, fixed community site |
| Onkanga et al., 2016 | [20] | Kenya | Both | 2 rounds, yearly | 12 months | RCT SCORE |
School, mobile CDDs |
| Wanjala et al., 2013* | [49] | Kenya | Targeted | 1 round | 18 months | Longitudinal | School |
| Zhang et al., 2007* | [22] | Uganda | Botb | 2 rounds, yearly | 12 months | Longitudinal | School, mobile CDDs |
| Both Schistosoma mansoni and Schistosoma haematobium | |||||||
| Brinkmann et al., 1988* | [36] | Mali | Both | 1 round | 12 months | Repeated cross-sectional | Not reported |
| Koukounari et al., 2007* | [37] | Burkina Faso | Targeted | 1 round | 12 months | Longitudinal | School, fixed community site, mobile CDDs |
| Landoure et al., 2012* | [38] | Mali | Mass | 3 or 4 rounds, yearly (with 1 year break) | 12 and 24 months | Repeated cross-sectional | School, mobile CDDs |
| Massa et al., 2009* | [39] | Tanzania | Targeted | 1 round | 12 months | Repeated cross-sectional | School, mobile CDDs |
| Mwandawiro et al., 2019* | [40] | Kenya | Targeted | 2 or 4 rounds, yearly | 12 months | Repeated cross-sectional | School |
| Ouedraogo et al., 2016 | [50] | Burkina Faso | Targeted | 4 rounds, approximately biennially | 12 or 24 months | Repeated cross-sectional | School, fixed community site, mobile CDDs |
| Toure et al., 2008* | [41] | Burkina Faso | Targeted | 1 round | 12 and 24 months | Longitudinal | School, fixed community site, mobile CDDs |
| Schistosoma haematobium | |||||||
| Adewale et al., 2018* | [51] | Nigeria | Targeted | 1 round | 12, 24, 36, 48 and 60 months | Longitudinal | School |
| Chaula & Tarimo, 2014* | [52] | Tanzania | Targeted | 2 rounds, yearly | 12 months | Longitudinal | School |
| Garba et al., 2004* | [33] | Niger | Mass | 1 round | 10 and 28 months | Repeated cross-sectional | Not reported |
| Hopkins et al., 2002 | [53] | Nigeria | Mass | 2 rounds, yearly | 12 months | Repeated cross-sectional | Mobile CDDs |
| Janitschke et al., 1989* | [54] | Yemen | Mass | 1 round | 12 months | Repeated cross-sectional | Not reported |
| Mduluza et al., 2001* | [55] | Zimbabwe | Targeted | 7 rounds, bi-monthly | 2 months | Longitudinal | Not reported |
| N’Goran et al., 2001* | [56] | Cote d’Ivoire | Targeted | 1 round or 2 rounds, yearly | 6, 12, 18 and 24 months | Longitudinal | School |
| Pennance et al., 2016* | [57] | Tanzania | Mass | 4 rounds, biannually | 7–8 months | Repeated cross-sectional | School, mobile CDDs |
| Phillips et al., 2017* | [17] | Mozambique | Both | 2 or 4 rounds, yearly or biennially | 12, 24 and 36 months | RCT SCORE |
School, fixed community site, mobile CDDs |
| Saathoff et al., 2004* | [58] | South Africa | Targeted | 1 round | 3, 16, 41 and 53 weeks | Longitudinal | School |
| Shehata et al., 2018* | [59] | Zambia | Targeted | 1 round | 6 and 12 months | Longitudinal | School |
| Stothard et al., 2009* | [60] | Tanzania | Targeted | 2 rounds, yearly | 12 months | Repeated cross-sectional | School |
| Schistosoma japonicum | |||||||
| Lin et al., 1997 | [61] | China | Mass | 2 rounds, yearly | 12 months | Longitudinal | Fixed community site |
| Zhang et al., 1998 | [62] | China | Mass | 1 round | 12 months | Longitudinal | Not reported |
RCT = randomised controlled trial, SCORE = study conducted by Schistosomiasis Consortium for Operational Research and Evaluation, CDD = community drug distributor
*Included in meta-analysis
Characteristics of included studies
Of the 34 included studies, 13 (38.2%) reported on only S. mansoni, 12 (35.3%) reported on only S. haematobium, seven (20.6%) reported on both S. mansoni and S. haematobium, and two (5.9%) reported on S. japonicum (Table 2). For S. mansoni, nine of 20 studies (45.0%) used a mass drug administration strategy and 14 (70.0%) used a targeted strategy. Three of these studies (15.0%) reported both strategies. For S. haematobium, seven of 19 studies (36.8%) used a mass drug administration strategy and 14 (73.7%) used a targeted strategy. Two of these studies (10.5%) reported both strategies. Of the five studies that included both mass and targeted strategies, three of these were randomised controlled trials that compared mass and targeted treatment arms within the study [17, 20, 21], one study used baseline village prevalence to direct mass or targeted treatment [36], and one study presented results for individual village groups that adopted mass or targeted strategies [22]. Both studies of S. japonicum reported mass drug administration.
Table 2. Descriptive indicators separated by schistosome species.
|
S. mansoni (n = 20*) |
S. haematobium (n = 19*) |
S. japonicum (n = 2) |
|||
|---|---|---|---|---|---|
| Mass | Targeted | Mass | Targeted | Mass | |
| Drug delivery strategy | 9 (45%)^ | 14 (70%)^ | 7 (37%)^ | 14 (74%)^ | 2 (100%) |
| Delivery platform# | |||||
| School | 2 (22%) | 14 (100%) | 2 (29%) | 12 (86%) | - |
| Community–fixed site | 2 (22%) | 3 (21%) | 1 (14%) | 3 (21%) | 1 (50%) |
| Community–mobile unit | 5 (56%) | 4 (29%) | 4 (57%) | 4 (29%) | - |
| Not reported | 3 (33%) | - | 3 (43%) | 2 (14%) | 1 (50%) |
| Number of treatment rounds† | |||||
| 1 round | 3 (33%) | 8 (57%) | 3 (43%) | 8 (57%) | 2 (100%) |
| Multiple rounds | 7 (78%) | 7 (50%) | 5 (71%) | 8 (57%) | - |
| Follow up after final treatment round† | |||||
| Less than 12 months | 1 (11%) | 2 (14%) | 2 (29%) | 6 (43%) | - |
| 12 months | 8 (89%) | 11 (79%) | 4 (57%) | 13 (93%) | 2 (100%) |
| Greater than 12 months | 2 (22%) | 6 (43%) | 4 (57%) | 9 (64%) | - |
* These totals include seven studies that report both S. mansoni and S. haematobium.
^ Three studies for S. mansoni and two studies for S. haematobium reported both mass and targeted strategies
# Numbers add to greater than 100% because studies used more than one delivery platform.
† Number of treatment rounds and follow up after final treatment round may add to greater than 100% as this incorporates studies that have multiple treatment arms with differing values for these variables.
As shown in Table 2, studies of targeted drug distribution primarily used a school-based platform to treat school-aged children. Some studies additionally used other platforms to reach non-enrolled school-aged children, including fixed community sites at dispensary units and mobile community drug distributors. One study compared school-based and community-based drug delivery for school-aged children [39], and one study treated only preschool children, aged two to six years [55]. Two studies did not report delivery platform [36, 55]. Studies of mass drug distribution primarily conducted drug administration through mobile community drug distributors. Fixed community sites and schools were also used to distribute drugs to the entire community. Six studies did not report the delivery platform [33, 34, 36, 45, 54, 62].
The number of treatment rounds varied from one to seven rounds, with treatment intervals ranging from two to 24 months. The follow-up interval after the final treatment round ranged from three weeks to 60 months. The most common follow-up interval after the final treatment round for all three species and both drug administration strategies was 12 months (27 studies, 79.4%).
Nine potential deficiencies were assessed in terms of risk of bias (S2 Table). The most common deficiencies were a response rate of less than 75% (or not reported) in 31 studies and praziquantel not delivered to at least 75% of the population (or not reported) in 19 studies. All other deficiencies were less common.
All 22 studies of S. mansoni and S. japonicum used stool samples to determine infection prevalence and intensity; all used the Kato-Katz diagnostic method. All 19 S. haematobium studies used urine samples to determine infection prevalence and intensity. Seventeen studies (89.5%) used the urine filtration method and four studies (21.1%) used urine dipsticks; two of these studies (10.5%) used both methods.
As shown in S1 Table, the most common additional medication was albendazole (11 studies, 32.4%), with mebendazole (two studies, 5.9%) and ivermectin (one study, 2.9%) also administered. Twenty-one studies (61.8%) reported no additional medications. Health education (e.g. videos, posters, broadcasts, reading material) was reported in seven studies (20.6%). Snail control using tilapia fish or molluscicide (two studies, 5.9%) and water source improvements with pumped wells (one study, 2.9%) were also reported. Twenty-seven studies (79.4%) reported no additional interventions apart from drug delivery.
Most studies were conducted in Africa (30 studies, 88.2%), with two studies (5.9%) in the Middle East and two studies in Asia. Tanzania and Kenya (six studies (17.6%) each) were the most commonly studied countries. Fourteen studies (41.2%) used a longitudinal design, while 15 (44.1%) were repeated cross-sectional studies and five were randomised controlled trials conducted by SCORE.
Treatment coverage was reported in 20 of 34 studies (58.8%), ranging from 22.7% to 129.8% (see S1 Table). Coverage values over 100% were seen due to inaccurate estimates of population size. Sixteen of these studies (80.0%) reported coverage greater than 75% for at least one treatment round.
Schistosome prevalence was reported in all included studies, while a measure of infection intensity was reported in 30 of the 34 studies (88.2%). Four of these studies reported only the proportion of high intensity infections, and two studies reported intensity only at baseline.
Quantitative analysis
Only S. mansoni and S. haematobium had sufficient studies to perform quantitative analysis. Results from the inverse variance weighted generalised linear model are shown in Table 3.
Table 3. Odds ratio of prevalence reduction* for selected covariates, stratified by Schistosoma species (inverse variance weighted generalised linear model with robust error variance).
| Odds ratio (95% CI) | p-value | R2 | |
|---|---|---|---|
| Schistosoma mansoni | |||
| Mass (n = 7) vs targeted (n = 12) treatment | 0.47 (0.13–1.68) | 0.227 | 0.126 |
| Baseline prevalence (%) | 1.02 (0.99–1.05) | 0.292 | |
| Number of treatment rounds | 0.95 (0.64–1.42) | 0.786 | |
| Follow-up time (months) | 1.06 (0.92–1.23) | 0.390 | |
| Schistosoma haematobium | |||
| Mass (n = 6) vs targeted (n = 13) treatment | 0.41 (0.06–3.03) | 0.358 | 0.279 |
| Baseline prevalence (%) | 0.99 (0.95–1.05) | 0.926 | |
| Number of treatment rounds | 0.76 (0.49–1.20) | 0.219 | |
| Follow-up time (months) | 1.48 (0.50–4.40) | 0.452 | |
* Prevalence reduction = (Prevalencefollow-up−Prevalencebaseline) / Prevalencebaseline, truncated such that any prevalence increase was reset to zero
For S. mansoni, 19 studies were included in the model, with two studies including two treatment arms [21, 22]. There was no significant difference in prevalence reduction following mass versus targeted treatment (odds ratio (OR) 0.47, 95% confidence interval (CI) 0.13–1.68, p = 0.227). Number of treatment rounds, baseline prevalence and follow-up time were not significantly associated with prevalence reduction.
Similarly, for S. haematobium, 19 studies were included in the model, with two studies including two treatment arms [17, 36]. There was no significant difference between mass and targeted drug treatment (OR 0.41, 95% CI 0.06–3.03, p = 0.358). Baseline prevalence, number of treatment rounds, and follow-up time were not significantly associated with prevalence reduction.
Results for intensity reduction are presented in Fig 2. There are no apparent differences in median egg reduction rates between mass and targeted praziquantel delivery for either S. mansoni or S. haematobium.
Fig 2.
Boxplots of infection intensity reduction for S. mansoni (A) and S. haematobium (B) for studies using mass and targeted strategies. Studies were weighted according to their sample size.
In sensitivity analyses, adding a covariate for treatment coverage did not significantly affect the results of the generalised linear model (S3 Table). Furthermore, results remained generally robust when high-prevalence studies were excluded and when follow-up prevalence was measured after one treatment round or closest (S4 Table). For S. haematobium, when studies with greater than 50% baseline prevalence were excluded, only a very small number of studies remained, leading the model to become unstable with very wide confidence intervals.
Results of the secondary meta-analyses synthesising the non-truncated prevalence reduction estimates from individual studies are shown in Table 4. Pooled prevalence reduction is shown separately for mass and targeted studies, stratified by number of treatment rounds. There was significant heterogeneity among included studies. In targeted studies, I2 was 96.7% for S. mansoni and 98.5% for S. haematobium. In mass studies, I2 was 93.3% for S. mansoni and 98.6% for S. haematobium.
Table 4. Meta-analysis results showing pooled prevalence reduction estimates (non-truncated), shown for mass and targeted studies for each schistosome species, stratified by number of treatment rounds.
| Delivery method | Number of treatment rounds | PReduc* (95% CI) | Cochran's Q | p value (Cochran’s Q) | Number of study datasets |
|---|---|---|---|---|---|
| Schistosoma mansoni | |||||
| Mass | One round | 0.22 (-0.76–0.66) | 27.63 | <0.001 | 4 |
| Multiple rounds | 0.34 (0.07–0.53) | 36.55 | <0.001 | 3 | |
| Targeted | One round | 0.41 (0.19–0.57) | 84.34 | <0.001 | 7 |
| Multiple rounds | 0.33 (-0.33–0.67) | 235.49 | <0.001 | 5 | |
| Schistosoma haematobium | |||||
| Mass | One round | 0.57 (0.24–0.75) | 46.86 | <0.001 | 3 |
| Multiple rounds | 0.34 (-0.04–0.58) | 111.41 | <0.001 | 3 | |
| Targeted | One round | 0.69 (0.45–0.82) | 216.34 | <0.001 | 7 |
| Multiple rounds | 0.60 (-0.01–0.84) | 574.68 | <0.001 | 6 | |
*PReduc = (Prevalencefollow-up−Prevalencebaseline) / Prevalencebaseline
The results of analyses conducted using random effects weights are depicted in S5 Table and S6 Table. Re-analysis using this approach did not significantly affect study results. In terms of small study effects, Egger’s regression showed evidence of mild funnel plot asymmetry for S. mansoni (intercept -4.10, p = 0.022), but not for S. haematobium (intercept -3.03, p = 0.335).
Discussion
Treatment of schistosomiasis has been scaled up over the last decade from test-and-treat strategies towards large-scale preventive drug administration programs. Recent modelling studies predict community-wide treatment programs to be the most effective strategy for controlling infection [14, 15]. To our knowledge, this systematic review and meta-analysis is the first synthesis of its kind, comparing the effects of mass and targeted delivery strategies on schistosomiasis prevalence and intensity in school-aged children.
The results of this analysis show that based on currently published studies, there is no detectable difference between mass and targeted drug administration strategies on the reduction in S. mansoni or S. haematobium infection prevalence or intensity in school-aged children. This does not align with our hypothesis, which was supported by previously-published mathematical modelling predictions [14] and a similar meta-analysis on soil-transmitted helminths [26]. The current analysis reflects only the findings of the 28 studies that were considered, including recent cluster-randomised controlled trials conducted by the SCORE initiative that found community-wide and child-targeted treatment equally effective in reducing prevalence in S. mansoni and S. haematobium infections [17, 20, 21]. An earlier study that applied either mass or targeted treatment to different villages also found similar prevalence reductions following mass and targeted drug delivery for S. haematobium [36].
One of the most plausible reasons for these results is insufficient treatment coverage in mass drug administration programs. Compared to child-targeted programs conducted through schools, mass drug administration programs may face more challenges in reaching a majority of the population eligible for treatment. Many studies included in our review did not report treatment coverage, and among those that did, reported coverage varied widely between studies, and was often inconsistent across treatment rounds within studies. Due to the large amount of studies that did not report treatment coverage, we were unable to adjust for this in our primary analysis. However, our findings for mass versus targeted treatment did not change when we conducted a sensitivity analysis controlling for treatment coverage. Further issues with reported treatment coverage are that underestimation of the target population is common and leads to an overestimation of treatment coverage [20], and also that there may be considerable discrepancies between reported treatment coverage (those who receive tablets) and treatment compliance (those who actually ingest the tablets) [63]. Compliance is an important consideration when reporting treatment coverage; however, there is considerable heterogeneity in the defining and reporting of treatment compliance in existing literature [63].
Another potential explanation for our findings is that in some settings, school-aged children may play a dominant role in driving transmission. Infections peak in childhood, leading school-aged children to generally carry more infection than other community members [4]. Therefore, in some settings, expanding treatment programs to other community members may not have a detectable effect on transmission among school-aged children. Furthermore, it is known that in many settings, there are hotspots of infection that have a disproportionate influence on driving transmission [64]. These persistent low-prevalence populations tend to remain, regardless of the drug administration strategy or how well drug administration programs are implemented [57]. Such hotspots may explain why significant differences between mass and targeted treatment were not evident in this review.
Several limitations in this study must be acknowledged. Firstly, only a relatively small number of studies were included in meta-analysis, especially for mass treatment. Secondly, there is potential for confounding from factors we were unable to include in our model, such as water, sanitation and hygiene (WASH) conditions, socioeconomic status and treatment coverage. An important potential confounder is the proximity of the infected population to local contaminated bodies of water [22], and the frequency and duration of water contact, especially in children [18]. Several studies have shown that populations living closer to local water bodies are more likely to have a higher prevalence and rate of reinfection [19, 22, 65]. Thirdly, limitations of existing diagnostic techniques for identifying schistosome infections may have affected our findings. Both the Kato-Katz technique (used to diagnose for S. mansoni and S. japonicum infections) and urine filtration (used for S. haematobium); are known to have low sensitivity, particularly for detecting light-intensity infections in areas with low endemicity [66, 67]. This is a source of measurement error that can underestimate the actual prevalence of infection in a population, creating a non-differential misclassification and potentially biasing findings towards the null hypothesis. Finally, two included studies did not have age-stratified data available, so we used standardised weights for calculating prevalence in school-aged children. These weights were taken from a study published in 1998 [35]. The age distribution and schistosome prevalence may vary between communities and prevalence reduction among school-aged children may not reflect that of other age groups.
Our review focuses on the impact of mass and targeted drug delivery strategies on school-aged children, who are recognised as the group at highest risk of schistosomiasis-associated morbidity. However, it is important to note that expanding control programs community-wide would provide the advantage of reducing morbidity in other age groups (i.e., preschool-aged children, adolescents, and adults), in whom the burden of schistosomiasis-associated morbidity may also be significant [68, 69]. WHO guidelines currently do not recommend a baseline assessment of infection prevalence and intensity in age groups other than school-aged children [70]. However, recent mathematical modelling highlights that including a broader range of age groups in baseline assessments, as well as ongoing monitoring, is important in order to determine appropriate control strategies for defined regions [71].
Although current targets, drug donations, and operational guidelines for schistosomiasis control focus on school-aged children [8, 9, 23], the burden of schistosomiasis among both adults and preschool-aged children has been acknowledged [5, 72]. At-risk adults are recommended to receive regular praziquantel in certain epidemiological settings [5], although global coverage remains low [2]. On the other hand, preschool-aged children are not included in WHO guidelines for schistosomiasis control because the safety of praziquantel in children under 4 years of age has not been established, and because there is no suitable paediatric formulation available [72, 73]. A recent dose-ranging study identified that a single 40mg/kg dose of praziquantel can be administered safely and efficaciously in children under 5 years of age [73], and a paediatric formulation of praziquantel is currently in development [74]. Treatment of preschool-aged children could be achieved by utilising existing platforms, such as child health days, as is done for other NTDs [75], if this formulation was made available free of charge.
Our findings highlight the importance of additional strategies beyond regular drug administration in achieving community-wide control of schistosomiasis. Praziquantel remains effective at treating S. mansoni and S. haematobium [76], but due to ongoing environmental reservoirs of disease, it does not stop reinfection. Rapid reinfection can occur in endemic areas [77], indicating that treatment should be accompanied with WASH interventions to improve water and sanitation conditions and hygiene behaviours. These interventions may include provision of a safe water supply, education to end open defecation, and safe contact with contaminated bodies of water [78]. As schistosomiasis is transmitted to humans through contact with contaminated freshwater snails, and amplification of parasite numbers occurs within the intermediate host [4], snail control with molluscicide or similar treatment should also be considered [79]. Only a very small number of studies in this review included such strategies.
In conclusion, although our analysis of current literature does not agree with mathematical modelling findings, there are limitations to existing studies and to this meta-analysis. There are further cluster-randomised controlled trials comparing strategies in development (C. King and A. Amadou, personal communication), which will provide more information on the effect of mass versus targeted treatment. Despite the findings presented here, it is nonetheless likely that mass treatment–when delivered with high coverage rates–will be more beneficial in some settings than targeted treatment for reducing infections among school-aged children. More research is needed to address issues with achieving coverage targets, implementation of WASH improvements, and addressing disease hotspots and sources of rapid reinfection. Consideration of these factors will assist with optimising control programs in the push towards eliminating schistosomiasis as a public health problem.
Supporting information
(DOC)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
The authors acknowledge the contributions of the following individuals towards this paper: Charles King, for his guidance on current SCORE initiatives and comments on an earlier draft of this manuscript; Colleen Lau, for comments on an earlier draft of this manuscript; and Yixuan Zhao, for reviewing and extracting data from Chinese papers.
Data Availability
All relevant data are within the manuscript and its Supporting Information files
Funding Statement
The authors received no specific funding for this work
References
- 1.James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet. 2018;392(10159):1789–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. Schistosomiasis and soiltransmitted helminthiases: numbers of people treated in 2017. Wkly Epidemiol Rec. 2018;93(50):681–692. [Google Scholar]
- 3.Rollinson D, Knopp S, Levitz S, Stothard JR, Tchuem Tchuente LA, Garba A, et al. Time to set the agenda for schistosomiasis elimination. Acta Trop. 2013;128(2):423–440. 10.1016/j.actatropica.2012.04.013 [DOI] [PubMed] [Google Scholar]
- 4.Colley DG, Bustinduy AL, Secor E, King CH. Human schistosomiasis. Lancet. 2014;383(9936):2253–2264. 10.1016/S0140-6736(13)61949-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO. Preventive chemotherapy in human helminthiasis: coordinated use of anthelminthic drugs in control interventions: a manual for health professionals and programme managers Crompton DWT, WHO, editors. Geneva: World Health Organization; 2006. [Google Scholar]
- 6.Kardaman MW, Amin MA, Fenwick A, Cheesmond AK, Dixon HG. A field trial using praziquantel (Biltricide) to treat Schistosoma mansoni and Schistosoma haematobium infection in Gezira, Sudan. Ann Trop Med Parasitol. 1983;77(3):297–304. 10.1080/00034983.1983.11811711 [DOI] [PubMed] [Google Scholar]
- 7.WHO. Schistosomiasis: progress report 2001–2011 and strategic plan 2012–2020. Geneva, Switzerland; 2013.
- 8.WHO. Accelerating work to overcome the global impact of neglected tropical diseases: a roadmap for implementation. 2012. [Google Scholar]
- 9.WHO. Crossing the Billion. Preventive chemotherapy for neglected tropical diseases: Lymphatic filariasis, onchocerciasis, schistosomiasis, soil-transmitted helminthiases and trachoma: World Health Organization; 2017. [Google Scholar]
- 10.WHO. Generic framework for control, elimination and eradication of neglected tropical diseases.; 2016. [Google Scholar]
- 11.Toor J, Alsallaq R, Truscott JE, Turner HC, Werkman M, Gurarie D, et al. Are We on Our Way to Achieving the 2020 Goals for Schistosomiasis Morbidity Control Using Current World Health Organization Guidelines? Clin Infect Dis. 2018;66(suppl_4):S245–S252. 10.1093/cid/ciy001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lo NC, Addiss DG, Hotez PJ, King CH, Stothard JR, Evans DS, et al. A call to strengthen the global strategy against schistosomiasis and soil-transmitted helminthiasis: the time is now. Lancet Infect Dis. 2017;17(2):E64–E69. 10.1016/S1473-3099(16)30535-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gurarie D, Yoon N, Li E, Ndeffo-Mbah M, Durham D, Phillips AE, et al. Modelling control of Schistosoma haematobium infection: predictions of the long-term impact of mass drug administration in Africa. Parasit Vectors. 2015;8(529) 10.1186/s13071-13015-11144-13073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Turner HC, Truscott JE, Bettis AA, Farrell SH, Deol AK, Whitton JM, et al. Evaluating the variation in the projected benefit of community-wide mass treatment for schistosomiasis: Implications for future economic evaluations. Parasit Vectors. 2017;10 (1)(213) 10.1186/s13071-13017-12141-13075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lo NC, Bogoch II, Blackburn BG, Raso G, N'Goran EK, Coulibaly JT, et al. Comparison of community-wide, integrated mass drug administration strategies for schistosomiasis and soil-transmitted helminthiasis: A cost-effectiveness modelling study. Lancet Glob Health. 2015;3(10):e629–e638. 10.1016/S2214-109X(15)00047-9 [DOI] [PubMed] [Google Scholar]
- 16.Burnim M, Ivy JA, King CH. Systematic review of community-based, school-based, and combined delivery modes for reaching school-aged children in mass drug administration programs for schistosomiasis. PLoS Negl Trop Dis. 2017;11(10) 10.1371/journal.pntd.0006043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Phillips AE, Gazzinelli-Guimaraes PH, Aurelio HO, Ferro J, Nala R, Clements M, et al. Assessing the benefits of five years of different approaches to treatment of urogenital schistosomiasis: A SCORE project in Northern Mozambique. PLoS Negl Trop Dis. 2017;11(12) 10.1371/journal.pntd.0006061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Assare RK, Tian-Bi YN, Yao PK, N'Guessan NA, Ouattara M, Yapi A, et al. Sustaining Control of Schistosomiasis Mansoni in Western Cote d'Ivoire: Results from a SCORE Study, One Year after Initial Praziquantel Administration. PLoS Negl Trop Dis. 2016; 10.1371/journal.pntd.0004329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karanja DMS, Awino EK, Wiegand RE, Okoth E, Abudho BO, Mwinzi PNM, et al. Cluster randomized trial comparing school-based mass drug administration schedules in areas of western Kenya with moderate initial prevalence of Schistosoma mansoni infections. PLoS Negl Trop Dis. 2017;11(10) 10.1371/journal.pntd.0006033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Onkanga IO, Mwinzi PN, Muchiri G, Andiego K, Omedo M, Karanja DM, et al. Impact of two rounds of praziquantel mass drug administration on Schistosoma mansoni infection prevalence and intensity: a comparison between community wide treatment and school based treatment in western Kenya. Int J Parasitol. 2016;46(7):439–445. 10.1016/j.ijpara.2016.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olsen A, Kinung'hi S, Magnussen P. Comparison of the Impact of Different Mass Drug Administration Strategies on Infection with Schistosoma mansoni in Mwanza Region, Tanzania-A Cluster-Randomized Controlled Trial. Am J Trop Med Hyg. 2018;99(6):1573–1579. 10.4269/ajtmh.18-0671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang Y, Koukounari A, Kabatereine N, Fleming F, Kazibwe F, Tukahebwa E, et al. Parasitological impact of 2-year preventive chemotherapy on schistosomiasis and soil-transmitted helminthiasis in Uganda. BMC Med. 2007;5(27) 10.1186/1741-7015-1185-1127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.WHO. Helminth control in school age children: a guide for managers of control programmes: World Health Organization; 2011. [Google Scholar]
- 24.Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLOS Med. 2009;6(7) 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rujeni N, Morona D, Ruberanziza E, Mazigo HD. Schistosomiasis and soil-transmitted helminthiasis in Rwanda: An update on their epidemiology and control. Infect Dis Poverty. 2017;6 (1)(8) 10.1186/s40249-40016-40212-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clarke NE, Clements ACA, Doi SA, Wang DX, Campbell SJ, Gray D, et al. Differential effect of mass deworming and targeted deworming for soil-transmitted helminth control in children: a systematic review and meta-analysis. Lancet. 2017;389(10066):287–297. 10.1016/S0140-6736(16)32123-7 [DOI] [PubMed] [Google Scholar]
- 27.Andrade G, Bertsch DJ, Gazzinelli A, King CH. Decline in infection-related morbidities following drug-mediated reductions in the intensity of Schistosoma infection: A systematic review and meta-analysis. PLoS Negl Trop Dis. 2017;11(2) 10.1371/journal.pntd.0005372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zoni AC, Catala L, Ault SK. Schistosomiasis Prevalence and Intensity of Infection in Latin America and the Caribbean Countries, 1942–2014: A Systematic Review in the Context of a Regional Elimination Goal. PLoS Negl Trop Dis. 2016;10(3) 10.1371/journal.pntd.0004493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lai YS, Biedermann P, Ekpo UF, Garba A, Mathieu E, Midzi N, et al. Spatial distribution of schistosomiasis and treatment needs in sub-Saharan Africa: a systematic review and geostatistical analysis. Lancet Infect Dis. 2015;15(8):927–940. 10.1016/S1473-3099(15)00066-3 [DOI] [PubMed] [Google Scholar]
- 30.Su J, Lu DB, Zhou X, Wang SR, Zhuge HX. Control efficacy of annual community-wide treatment against Schistosoma japonicum in China: A meta-analysis. PLoS ONE. 2013;8(11) 10.1371/journal.pone.0078509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.King CH, Olbrych SK, Soon M, Singer ME, Carter J, Colley DG. Utility of repeated praziquantel dosing in the treatment of schistosomiasis in high-risk communities in Africa: A systematic review. PLoS Negl Trop Dis. 2011;5(9) 10.1371/journal.pntd.0001321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–939. 10.1016/j.jclinepi.2011.11.014 [DOI] [PubMed] [Google Scholar]
- 33.Garba A, Campagne G, Tassie JM, Barkire A, Vera C, Sellin B, et al. Long-term impact of a mass treatment by praziquantel on morbidity due to Schistosoma haematobium in two hyperendemic villages of Niger. Bull Soc Pathol Exot. 2004;97(1):7–11. [PubMed] [Google Scholar]
- 34.Boisier P, Ramarokoto CE, Ravaoalimalala VE, Rabarijaona L, Serieye J, Esterre P. Reversibility of Schistosoma mansoni-associated morbidity after yearly mass praziquantel therapy: ultrasonographic assessment. Trans R Soc Trop Med Hyg. 1998;92(4):451–453. 10.1016/s0035-9203(98)91090-2 [DOI] [PubMed] [Google Scholar]
- 35.Guyatt HL, Brooker S, Donnelly CA. Can prevalence of infection in school-aged children be used as an index for assessing community prevalence? Parasitology. 1999;118(3):257–268. [DOI] [PubMed] [Google Scholar]
- 36.Brinkmann UK, Werler C, Traore M, Doumbia S, Diarra A. Experiences with mass chemotherapy in the control of schistosomiasis in Mali. Trop Med Parasitol. 1988;39(2):167–174. [PubMed] [Google Scholar]
- 37.Koukounari A, Gabrielli AF, Toure S, Bosque-Oliva E, Zhang Y, Sellin B, et al. Schistosoma haematobium infection and morbidity before and after large-scale administration of praziquantel in Burkina Faso. J Infect Dis. 2007;196(5):659–669. 10.1086/520515 [DOI] [PubMed] [Google Scholar]
- 38.Landoure A, Dembele R, Goita S, Kane M, Tuinsma M, Sacko M, et al. Significantly reduced intensity of infection but persistent prevalence of schistosomiasis in a highly endemic region in Mali after repeated treatment. PLoS Negl Trop Dis. 2012;6(7) 10.1371/journal.pntd.0001774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Massa K, Magnussen P, Sheshe A, Ntakamulenga R, Ndawi B, Olsen A. The effect of the community-directed treatment approach versus the school-based treatment approach on the prevalence and intensity of schistosomiasis and soil-transmitted helminthiasis among schoolchildren in Tanzania. Trans R Soc Trop Med Hyg. 2009;103(1):31–37. 10.1016/j.trstmh.2008.07.009 [DOI] [PubMed] [Google Scholar]
- 40.Mwandawiro C, Okoyo C, Kihara J, Simiyu E, Kepha S, Campbell SJ, et al. Results of a national school-based deworming programme on soil-transmitted helminths infections and schistosomiasis in Kenya: 2012–2017. Parasit Vectors. 2019;12(76) 10.1186/s13071-13019-13322-13071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Toure S, Zhang Y, Bosque-Oliva E, Ky C, Ouedraogo A, Koukounari A, et al. Two-year impact of single praziquantel treatment on infection in the national control programme on schistosomiasis in Burkina Faso. Bull World Health Organ. 2008;86(10):780–787. 10.2471/BLT.07.048694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Doi SA, Barendregt JJ, Khan S, Thalib L, Williams GM. Advances in the meta-analysis of heterogeneous clinical trials I: The inverse variance heterogeneity model. Contemp Clin Trials. 2015;45(Pt A):130–138. 10.1016/j.cct.2015.05.009 [DOI] [PubMed] [Google Scholar]
- 43.Abudho BO, Ndombi EM, Guya B, Carter JM, Riner DK, Kittur N, et al. Impact of Four Years of Annual Mass Drug Administration on Prevalence and Intensity of Schistosomiasis among Primary and High School Children in Western Kenya: A Repeated Cross-Sectional Study. Am J Trop Med Hyg. 2018;98(5):1397–1402. 10.4269/ajtmh.17-0908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ahmed AM, El Tash LA, Mohamed EY, Adam I. High levels of Schistosoma mansoni infections among schoolchildren in central Sudan one year after treatment with praziquantel. J Helminthol. 2012;86(2):228–232. 10.1017/S0022149X11000290 [DOI] [PubMed] [Google Scholar]
- 45.Al Abaidani I, Al-Abri S, Shaban M, Ghugey SL, Al Kathery S, Al-Mashikhi K, et al. Decline in transmission of schistosomiasis mansoni in Oman. Infect Dis Poverty. 2016;5(112) 10.1186/s40249-40016-40210-40241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hodges MH, Dada N, Warmsley A, Paye J, Bangura MM, Nyorkor E, et al. Mass drug administration significantly reduces infection of Schistosoma mansoni and hookworm in school children in the national control program in Sierra Leone. BMC Infect Dis. 2012;12(16) 10.1186/1471-2334-1112-1116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kaatano GM, Siza JE, Mwanga JR, Min DY, Yong TS, Chai JY, et al. Integrated Schistosomiasis and Soil-Transmitted Helminthiasis Control over Five Years on Kome Island, Tanzania. Korean J Parasitol. 2015;53(5):535–543. 10.3347/kjp.2015.53.5.535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mwinzi PN, Montgomery SP, Owaga CO, Mwanje M, Muok EM, Ayisi JG, et al. Integrated community-directed intervention for schistosomiasis and soil transmitted helminths in western Kenya—a pilot study. Parasit Vectors. 2012;5(182) 10.1186/1756-3305-1185-1182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wanjala PM, Khaemba BM, Luoba AI. Prevalence and intensity of infection of intestinal schistosomiasis and reinfection after intervention in Budalangi endemic focus of Western Kenya. Int J Trop Med. 2013;8(3):71–80. [Google Scholar]
- 50.Ouedraogo H, Drabo F, Zongo D, Bagayan M, Bamba I, Pima T, et al. Schistosomiasis in school-age children in Burkina Faso after a decade of preventive chemotherapy. Bull World Health Organ. 2016;94(1):37–45. 10.2471/BLT.15.161885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Adewale B, Mafe MA, Sulyman MA, Idowu ET, Ajayi MB, Akande DO, et al. Impact of Single Dose Praziquantel Treatment on Schistosoma haematobium Infection among School Children in an Endemic Nigerian Community. Korean J Parasitol. 2018;56(6):577–581. 10.3347/kjp.2018.56.6.577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chaula SA, Tarimo DS. Impact of praziquantel mass drug administration campaign on prevalence and intensity of Schistosoma haemamtobium among school children in Bahi district, Tanzania. Tanzan J Health Res. 2014;16(1):1–8. [DOI] [PubMed] [Google Scholar]
- 53.Hopkins DR, Eigege A, Miri ES, Gontor I, Ogah G, Umaru J, et al. Lymphatic filariasis elimination and schistosomiasis control in combination with onchocerciasis control in Nigeria. Am J Trop Med Hyg. 2002;67(3):266–272. 10.4269/ajtmh.2002.67.266 [DOI] [PubMed] [Google Scholar]
- 54.Janitschke K, Telher AA, Wachsmuth J, Jahia S. Prevalence and control of Schistosoma haematobium infections in the Amran subprovince of the Yemen Arab Republic. Trop Med Parasitol. 1989;40(2):181–184. [PubMed] [Google Scholar]
- 55.Mduluza T, Ndhlovu PD, Madziwa TM, Midzi N, Zinyama R, Turner CM, et al. The impact of repeated treatment with praziquantel of schistosomiasis in children under six years of age living in an endemic area for Schistosoma haematobium infection. Mem Inst Oswaldo Cruz. 2001;96 Suppl:157–164. 10.1590/s0074-02762001000900024 [DOI] [PubMed] [Google Scholar]
- 56.N'Goran EK, Utzinger J, N'Guessan AN, Muller I, Zamble K, Lohourignon KL, et al. Reinfection with Schistosoma haematobium following school-based chemotherapy with praziquantel in four highly endemic villages in Cote d'Ivoire. Trop Med Int Health. 2001;6(10):817–825. 10.1046/j.1365-3156.2001.00785.x [DOI] [PubMed] [Google Scholar]
- 57.Pennance T, Person B, Muhsin MA, Khamis AN, Muhsin J, Khamis IS, et al. Urogenital schistosomiasis transmission on Unguja Island, Zanzibar: Characterisation of persistent hot-spots. Parasit Vectors. 2016;9(646) 10.1186/s13071-13016-11847-13070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Saathoff E, Olsen A, Magnussen P, Becker W, Appleton CC. Patterns of Schistosoma haematobium infection, impact of praziquantel treatment and re-infection after treatment in a cohort of schoolchildren from rural KwaZulu-Natal/South Africa. BMC Infect Dis. 2004;4(40) 10.1186/1471-2334-1184-1140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shehata M, Chama M, Funjika E. Prevalence and intensity of Schistosoma haematobium infection among schoolchildren in central Zambia before and after mass treatment with a single dose of praziquantel. Trop Parasitol. 2018;8(1):12–17. 10.4103/tp.TP_32_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Stothard JR, French MD, Khamis IS, Basanez MG, Rollinson D. The epidemiology and control of urinary schistosomiasis and soil-transmitted helminthiasis in schoolchildren on Unguja Island, Zanzibar. Trans R Soc Trop Med Hyg. 2009;103(10):1031–1044. 10.1016/j.trstmh.2009.03.024 [DOI] [PubMed] [Google Scholar]
- 61.Lin D, Zhang S, Murakami H, Wu Z, Totsuya T, Gu X, et al. Impact mass chemotherapy with praziquantel on schistosomiasis control in Fanhu village, People's Republic of China. Southeast Asian J Trop Med Public Health. 1997;28(2):274–279. [PubMed] [Google Scholar]
- 62.Zhang GH WT, Wu WD, Chen YS, Tian XG. Comparative study of effect on schistosomiasis control between the targeted population treatment and the community-wide treatment. Chinese Primary Health Care. 1998:46–48. [Google Scholar]
- 63.Shuford KV, Turner HC, Anderson RM. Compliance with anthelmintic treatment in the neglected tropical diseases control programmes: a systematic review. Parasites & Vectors. 2016;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kittur N, Binder S, Campbell CH, King CH, Kinung'Hi S, Olsen A, et al. Defining persistent hotspots: Areas that fail to decrease meaningfully in prevalence after multiple years of mass drug administration with praziquantel for control of schistosomiasis. Am J Trop Med Hyg. 2017;97(6):1810–1817. 10.4269/ajtmh.17-0368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Woodhall DM, Wiegand RE, Wellman M, Matey E, Abudho B, Karanja DM, et al. Use of geospatial modeling to predict Schistosoma mansoni prevalence in Nyanza Province, Kenya. PLoS ONE. 2013;8(8) 10.1371/journal.pone.0071635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Le L, Hsieh MH. Diagnosing Urogenital Schistosomiasis: Dealing with Diminishing Returns. Trends Parasitol. 2017;33(5):378–387. 10.1016/j.pt.2016.12.009 [DOI] [PubMed] [Google Scholar]
- 67.Barenbold O, Raso G, Coulibaly JT, N'Goran EK, Utzinger J, Vounatsou P. Estimating sensitivity of the Kato-Katz technique for the diagnosis of Schistosoma mansoni and hookworm in relation to infection intensity. Plos Negl Trop Dis. 2017;11(10) 10.1371/journal.pntd.0005953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Odogwu SE, Ramamurthy NK, Kabatereine NB, Kazibwe F, Tukahebwa E, Webster JP, et al. Schistosoma mansoni in infants (aged <3 years) along the Ugandan shoreline of Lake Victoria. Ann Trop Med Parasitol. 2006;100(4):315–326. 10.1179/136485906X105552 [DOI] [PubMed] [Google Scholar]
- 69.Njenga SM, Mwandawiro CS, Muniu E, Mwanje MT, Haji FM, Bockarie MJ. Adult population as potential reservoir of NTD infections in rural villages of Kwale district, Coastal Kenya: Implications for preventive chemotherapy interventions policy. Parasit Vectors. 2011;4(175) 10.1186/1756-3305-1184-1175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.WHO. Prevention and control of schistosomiasis and soil-transmitted helminthiasis. World Health Organ Tech Rep Ser. 2002;912:i–vi, 1–57, back cover. [PubMed] [Google Scholar]
- 71.Toor J, Turner HC, Truscott JE, Werkman M, Phillips AE, Alsallaq R, et al. The design of schistosomiasis monitoring and evaluation programmes: The importance of collecting adult data to inform treatment strategies for Schistosoma mansoni. PLoS Negl Trop Dis. 2018;12(10):e0006717 10.1371/journal.pntd.0006717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.WHO. Report of a meeting to review the results of studies on the treatment of schistosomiasis in preschool-age children: World Health Organization; 2011. [Google Scholar]
- 73.Montresor A, Garba A. Treatment of preschool children for schistosomiasis. Lancet Glob Health. 2017;5(7):e640–e641. 10.1016/S2214-109X(17)30202-4 [DOI] [PubMed] [Google Scholar]
- 74.Reinhard-Rupp J, Klohe K. Developing a comprehensive response for treatment of children under 6 years of age with schistosomiasis: Research and development of a pediatric formulation of praziquantel. Infect Dis Poverty. 2017;6(122) 10.1186/s40249-40017-40336-40249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Albonico M, Allen H, Chitsulo L, Engels D, Gabrielli A-F, Savioli L. Controlling Soil-Transmitted Helminthiasis in Pre-School-Age Children through Preventive Chemotherapy. PLOS Negl Trop Dis. 2008;2(3):e126 10.1371/journal.pntd.0000126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Vale N, Gouveia MJ, Rinaldi G, Brindley PJ, Gartner F, Correia da Costa JM. Praziquantel for Schistosomiasis: Single-Drug Metabolism Revisited, Mode of Action, and Resistance. Antimicrob Agents Chemother. 2017;61(5) 10.1128/AAC.02582-02516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Secor W, Colley D. When Should the Emphasis on Schistosomiasis Control Move to Elimination? Trop Med Infect Dis. 2018;3(85) 10.3390/tropicalmed3030085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Campbell SJ, Savage GB, Gray DJ, Atkinson J-AM, Soares Magalhães RJ, Nery SV, et al. Water, Sanitation, and Hygiene (WASH): A Critical Component for Sustainable Soil-Transmitted Helminth and Schistosomiasis Control. PLOS Negl Trop Dis. 2014;8(4):e2651 10.1371/journal.pntd.0002651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.King CH, Sutherland LJ, Bertsch D. Systematic Review and Meta-analysis of the Impact of Chemical-Based Mollusciciding for Control of Schistosoma mansoni and S. haematobium Transmission. Plos Negl Trop Dis. 2015;9(12) 10.1371/journal.pntd.0004290 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files