Abstract
Objective
To evaluate efficacy and tolerability of adjunctive lacosamide in children and adolescents with uncontrolled focal (partial-onset) seizures.
Methods
In this double-blind trial (SP0969; NCT01921205), patients (age ≥4–<17 years) with uncontrolled focal seizures were randomized (1:1) to adjunctive lacosamide/placebo. After a 6-week titration, patients who reached the target dose range for their weight (<30 kg: 8–12 mg/kg/d oral solution; ≥30–<50 kg: 6–8 mg/kg/d oral solution; ≥50 kg: 300–400 mg/d tablets) entered a 10-week maintenance period. The primary outcome was change in focal seizure frequency per 28 days from baseline to maintenance.
Results
Three hundred forty-three patients were randomized; 306 (lacosamide 152 of 171 [88.9%]; placebo 154 of 172 [89.5%]) completed treatment (titration and maintenance). Adverse events (AEs) were the most common reasons for discontinuation during treatment (lacosamide 4.1%; placebo 5.8%). From baseline to maintenance, percent reduction in focal seizure frequency per 28 days for lacosamide (n = 170) vs placebo (n = 168) was 31.7% (p = 0.0003). During maintenance, median percent reduction in focal seizure frequency per 28 days was 51.7% for lacosamide and 21.7% for placebo. Fifty percent responder rates (≥50% reduction) were 52.9% and 33.3% (odds ratio 2.17, p = 0.0006). During treatment, treatment-emergent AEs were reported by 67.8% lacosamide-treated patients (placebo 58.1%), most commonly (≥10%) somnolence (14.0%, placebo 5.2%) and dizziness (10.5%, placebo 3.5%).
Conclusions
Adjunctive lacosamide was efficacious in reducing seizure frequency and generally well tolerated in patients (age ≥4–<17 years) with focal seizures.
ClinicalTrials.gov identifier:
Classification of evidence
This trial provides Class I evidence that for children and adolescents with uncontrolled focal seizures, adjunctive lacosamide reduces seizure frequency.
Approximately 25% to 30% of children with epilepsy have uncontrolled seizures despite antiepileptic drug (AED) treatment1; therefore, novel AED therapies are sorely needed. Lacosamide is an AED that exerts its anticonvulsant activity by selectively enhancing slow inactivation of voltage-gated sodium channels.2 It has a predictable pharmacokinetic profile with a high oral bioavailability and a low potential for clinically relevant pharmacokinetic drug-drug interactions.3 Lacosamide is indicated for the treatment of focal (partial-onset) seizures in patients ≥4 years of age in the United States and the European Union.
The efficacy, safety, and tolerability of lacosamide as adjunctive therapy and monotherapy for adults with focal seizures have been demonstrated in several randomized controlled trials4–9 and are further supported by clinical practice experience.10–12 The use of adjunctive lacosamide in children and adolescents has been investigated in open-label trials13,14 and reported in observational studies.15–20 The objective of this randomized, double-blind, placebo-controlled trial was to evaluate the efficacy and tolerability of adjunctive lacosamide in children and adolescents (≥4–<17 years of age) with uncontrolled focal seizures.
Methods
Standard protocol approvals, registrations, and patient consents
The trial was conducted in accordance with good clinical practice and the Declaration of Helsinki. The protocol and amendments were reviewed by a national, regional, or independent ethics committee or institutional review board. Each patient (when able to assent) and the parent or legal guardian provided written informed consent. The trial was registered with ClinicalTrials.gov (NCT01921205).
Patients
SP0969 was a randomized, double-blind, placebo-controlled trial conducted at 114 sites in Europe, North America, Latin America, and the Asia Pacific region. Eligibility criteria were assessed by the investigators at the screening visit. Children and adolescents (≥4–<17 years of age) were eligible for enrollment if they had a diagnosis of epilepsy with focal (partial-onset) seizures, with ≥1 prior EEG and MRI/CT scans consistent with this diagnosis. Additional inclusion criteria were uncontrolled focal seizures after an adequate course of treatment (in the opinion of the investigator) with ≥2 AEDs (concurrently or sequentially); an average of ≥2 focal seizures per 28 days, with no more than 21 days without seizures in the 8-week period before entering the baseline period, and at least 2 focal seizures during the 8-week prospective baseline; and a stable dose regimen of 1 to 3 AEDs for ≥4 weeks before the baseline period and throughout the trial. Exclusion criteria included assignment to lacosamide in a previous trial or participation in a trial of another investigational medical product or device within the previous 2 months; convulsive status epilepticus (within the previous 2 months); Lennox-Gastaut syndrome; primary generalized epilepsy; mixed seizure disorder (focal [partial] and primarily generalized seizures); exclusively febrile seizures; nocturnal seizures only; or epilepsy secondary to a progressive cerebral or neurodegenerative disease (additional criteria in supplemental Methods available from Dryad, doi.org/10.5061/dryad.kt5jj49).
Trial design
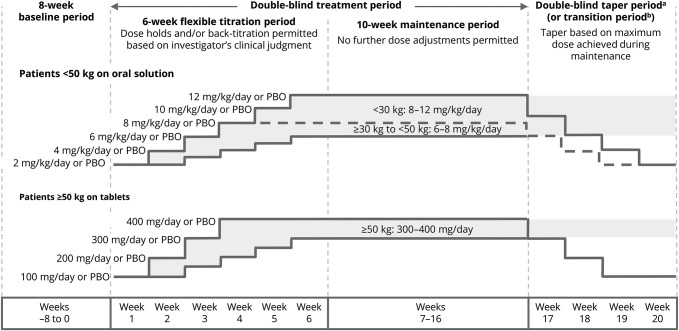
The trial consisted of an 8-week prospective baseline period, 16-week treatment period (6-week titration, 10-week maintenance), 4-week taper/transition period, and a 30-day safety follow-up period for patients not entering the open-label extension trial (EP0034; NCT01964560) (figure 1). Eligible patients were randomized (1:1) to lacosamide or placebo.
Figure 1. SP0969 trial design.
PBO = placebo. aThe highest possible dose per body weight category is shown for each taper period week. bPatients on lacosamide remained on their maintenance dose during the transition period, whereas patients in the placebo group initiated lacosamide in a double-blind fashion. On completion of the transition period, eligible patients entered the open-label extension on a weight-based dose (<30 kg: 10 mg/kg/d; ≥30–<50 kg: 6 mg/kg/d; ≥50 kg: 300 mg/d).
Trial medication was administered orally twice daily at ≈12-hour intervals. Patients weighing <50 kg initiated lacosamide or matching placebo at a dose of 2 mg/kg/d (oral solution), and those weighing ≥50 kg had a starting dose of 100 mg/d (tablets) (figure 1). Patients weighing ≥50 kg who were unwilling or unable to swallow tablets took the oral solution. A dosing syringe was used to ensure accurate administration of the oral solution. Administration of oral solution by feeding tube was permitted if needed.
After the first week of treatment, the investigator determined whether the patient could tolerate a dose increase or should remain on the current dose. Doses were increased in weekly increments of 2 mg/kg/d (oral solution; patients weighing <50 kg) or 100 mg/d (tablets; patients weighing ≥50 kg), with unlimited dose holds and/or back-titration permitted at the investigator's discretion. The target dose range for each patient was based on body weight at baseline: 8 to 12 mg/kg/d for <30 kg, 6 to 8 mg/kg/d for ≥30 kg to <50 kg, and 300 to 400 mg/d for ≥50 kg. Patients who were not able to reach the minimum target dose by the end of the 6-week titration period were withdrawn. No further dose adjustments were permitted during the 10-week maintenance period. Patients who completed the maintenance period had the option of transitioning to an open-label extension trial or tapering off their trial medication.
Patients attended weekly trial visits throughout the titration period and fortnightly visits thereafter. Throughout the trial, patients and/or their caregivers completed a daily diary of seizure activity (type and frequency). Diaries were checked by the investigators at each visit to ensure accurate and thorough completion and were used to assess efficacy outcomes. Per the trial protocol, seizure types were defined according to the International League Against Epilepsy (ILAE) 1981 criteria as simple partial (focal aware according to the ILAE 2017 classification), complex partial (focal impaired awareness), and partial evolving to secondarily generalized (focal to bilateral tonic-clonic).21,22
Outcome variables
The primary efficacy outcome was the change in focal seizure frequency per 28 days from baseline to maintenance. Secondary outcomes were the change in focal seizure frequency per 28 days from baseline to the entire treatment period (titration and maintenance combined), assessed overall and by focal (partial) seizure subtype (simple partial, complex partial, secondarily generalized); patients with a ≥50% reduction in focal seizure frequency (50% responders; maintenance); patients with a ≥25% increase in focal seizure frequency per 28 days (treatment); the proportion of seizure-free days (maintenance); and the proportion of patients who completed maintenance without a seizure (achieved seizure-free status). Other efficacy outcomes (assessed post hoc) were the median percent reduction from baseline in focal seizure frequency per 28 days (maintenance and treatment), 50% responders during treatment, and patients with a ≥75% reduction in focal seizure frequency (75% responders; maintenance and treatment).
Safety outcomes included the incidences of treatment-emergent adverse events (TEAEs), discontinuations due to TEAEs, shifts from baseline to last visit in assessments of behavior and cognitive function (Achenbach Child Behavior Checklist [CBCL]; Behavior Rating Inventory of Executive Function [BRIEF]/BRIEF-Preschool version), clinical laboratory evaluations, ECG and vital sign monitoring, and physical and neurologic examinations. The time to onset, dose at onset, and duration of somnolence and dizziness were also assessed.
Pharmacokinetic outcomes included plasma concentrations of lacosamide and concomitant AEDs based on blood samples at the screening visit, final titration and maintenance visits, and/or early termination visit. Post hoc analyses of pharmacokinetic data were performed to evaluate the plasma concentrations of concomitant AEDs during adjunctive lacosamide treatment.
Statistical analyses
Efficacy analyses comprised the full analysis set of all randomized patients who received at least 1 dose of trial medication and who had a baseline and at least 1 postbaseline assessment of seizure frequency data. Randomized patients who received at least 1 dose of trial medication were included in safety analyses (safety set). Patients who had at least 1 measurable postdose plasma sample (plasma level above the limit of quantification, with documented sampling and medication intake times) were included in pharmacokinetic analyses (pharmacokinetic–per-protocol set).
The trial was powered to detect a significant difference from baseline to maintenance between lacosamide and placebo in focal seizure frequency per 28 days. One hundred thirty-five patients per treatment arm were necessary to detect an effect size of 0.342 (placebo-subtracted difference of −0.249 and a common SD of 0.73 on the log-transformed data, equivalent to ≈22% reduction over placebo after exponentiation) with a power of 80% and a 2-sided test at a significance level of 5%. With this sample size, a 2-sided continuity-corrected χ2 test at a significance level of 5% will provide ≈87% power for assessment of the 50% responder rate, assuming responder rates of 22% and 40% for the placebo and lacosamide groups, respectively. To account for an anticipated dropout rate of ≈14%, 308 patients were planned for enrollment (154 per treatment arm). During the trial, a blinded re-estimation of sample size was performed, and the target for randomization was increased to 340 patients (supplemental Methods available from Dryad, doi.org/10.5061/dryad.kt5jj49).
Assessments of focal seizure frequency per 28 days were based on the number of days for which seizure information was provided during the specified time interval. If >10% of the diary entries were missing for a specific patient and time interval, then that patient was not included in the analyses of seizure frequency or seizure-free days during that time interval. For those who discontinued before maintenance, all available seizure frequency data from the titration period were carried forward for the maintenance period analysis. Similarly, for patients who discontinued during maintenance, all available seizure frequency data were used for the calculation of seizure frequency per 28 days during the maintenance period.
For the primary outcome, an analysis of covariance was performed on log-transformed seizure frequency with terms for treatment and pooled center and log-transformed baseline seizure frequency as a covariate. The change in focal seizure frequency for lacosamide vs placebo during maintenance was compared using least squares (LS) means, and the percent reduction over placebo was estimated. The change in focal seizure frequency per 28 days during treatment and the proportion of seizure-free days during maintenance (days with no seizures/days with lacosamide, per patient diary) were analyzed with similar methods. Responder rates were analyzed with a logistic regression model with terms for treatment and pooled center, and odds ratios with 95% confidence intervals (CIs) were calculated. Patients who discontinued before maintenance were treated as nonresponders. Descriptive analyses were performed for all other efficacy and safety outcomes.
Post hoc subgroup analyses of efficacy outcomes were performed by focal seizure subtype (including the combined category of complex partial and/or secondarily generalized seizures) and by concomitant use of sodium channel–blocking (SCB) AEDs (carbamazepine, lamotrigine, oxcarbazepine, phenytoin, and rufinamide). Post hoc subgroup analyses of TEAE data were performed by number of concomitant AEDs, and by concomitant SCB use.
Patients were included in post hoc analyses of plasma levels of concomitant AEDs if they were on a stable dose regimen of valproic acid, levetiracetam, lamotrigine, carbamazepine, topiramate, oxcarbazepine, clonazepam, or clobazam and had plasma levels above the lower limit of quantification for the selected AEDs at baseline and at least 1 postbaseline visit during treatment. For patients on oxcarbazepine, the plasma concentration of the main oxcarbazepine active metabolite 10-hydroxycarbazepine (MHD) was assessed. Patients who received >1 concomitant AED were counted once within each AED category. Repeated-measures analysis of covariance was performed, and geometric LS mean ratios (treatment/baseline) with 90% CIs were estimated for plasma concentrations. No lacosamide effect on AED concentration was concluded if the 90% CIs of the geometric LS means ratios were within the bioequivalence limit of 0.8 to 1.25.
Data availability
Underlying data from this manuscript may be requested by qualified researchers 6 months after product or indication approval in the US and/or Europe, or global development is discontinued, and 18 months after trial completion. Investigators may request access to anonymized individual patient data and redacted study documents, which may include raw datasets, analysis-ready datasets, study protocol, blank case report form, annotated case report form, statistical analysis plan, dataset specifications, and clinical study report. Before use of the data, proposals need to be approved by an independent review panel at www.clinicalstudydatarequest.com and a signed data sharing agreement will need to be executed. All documents are available in English only, for a prespecified time, typically 12 months, on a password-protected portal.
Classification of evidence
Primary research question was the following: is adjunctive lacosamide efficacious in reducing focal seizure frequency in children and adolescents with uncontrolled focal seizures?
This trial provides Class 1 evidence that adjunctive lacosamide reduced focal seizure frequency by 31.72% vs placebo (p = 0.0003).
Results
Patients
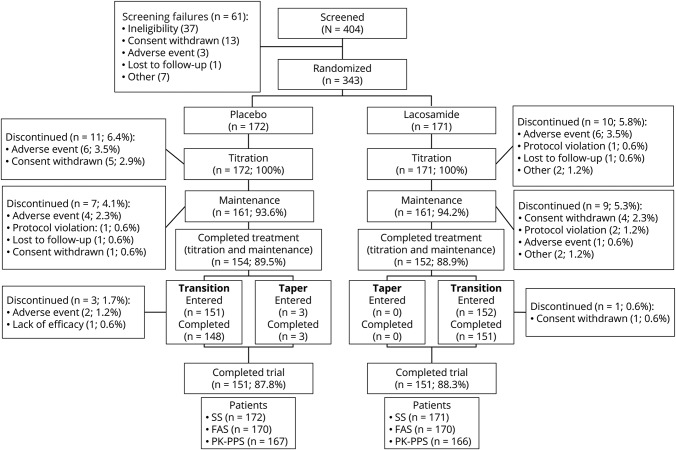
The trial was performed between August 2013 and January 2017. Three hundred forty-three patients were randomized, of whom 306 completed the treatment period and 302 completed the trial (figure 2). Adverse events (AEs) were the most common reasons for trial discontinuation during treatment (lacosamide: 7 [4.1%]; placebo: 10 [5.8%]). One hundred fifty-one (88.3%) patients on lacosamide and 148 (86.0%) patients on placebo planned to continue to the open-label extension trial.
Figure 2. Patient disposition.
FAS = full analysis set; PK-PPS = pharmacokinetic–per-protocol set; SS = safety set.
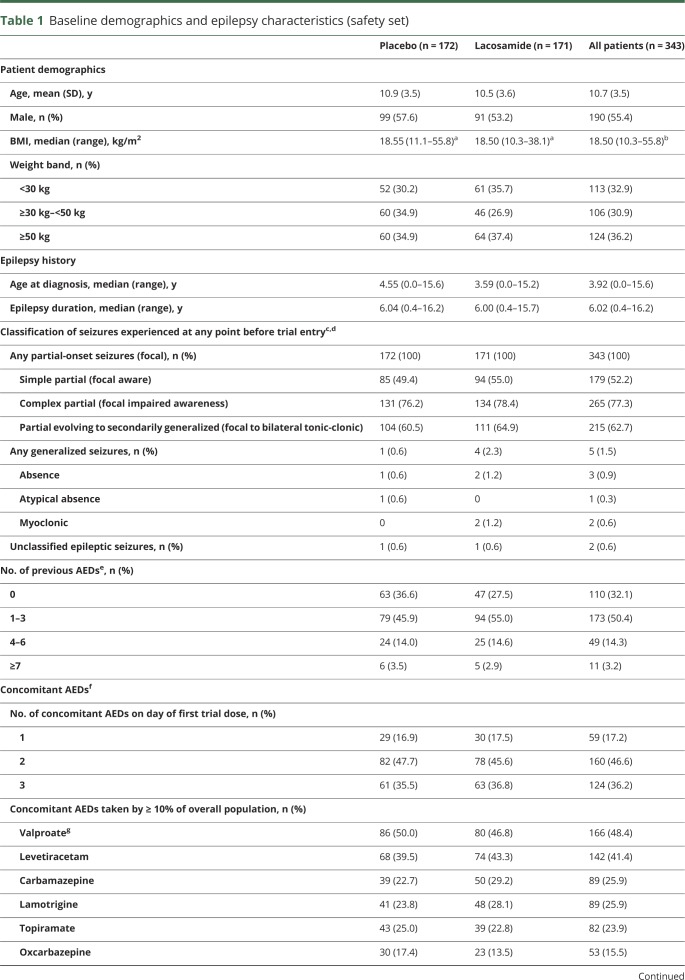
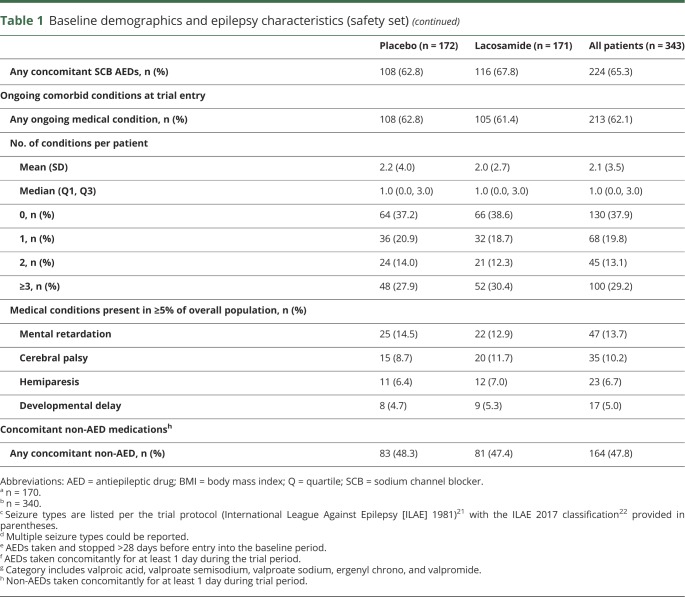
Baseline demographic data and epilepsy characteristics were similar between treatment groups (table 1). The majority of patients (267 [77.8%]) were white. Patients had a median epilepsy duration of 6.0 years and a median age at diagnosis of 3.9 years. On the day of first trial dose, the majority of patients were taking 2 or 3 concomitant AEDs (table 1). Valproate and levetiracetam were the most common concomitant AEDs. Most patients (224 [65.3%]) took at least 1 SCB AED.
Table 1.
Baseline demographics and epilepsy characteristics (safety set)
During titration, most patients (lacosamide: 142 [83.0%]; placebo: 156 [90.7%]) did not require any back-titration step. The median of the median daily dose of lacosamide during maintenance was 12 mg/kg/d for patients weighing <30 kg, 8 mg/kg/d for those weighing ≥30 to <50 kg, and 400 mg/d for those weighing ≥50 kg. One hundred (58.5%) patients on lacosamide and 161 (93.6%) on placebo reached the maximum target dose level for their weight. A higher proportion of lacosamide-treated patients with 1 concomitant AED at baseline (22 of 30 [73.3%]) than those with 2 (45 of 78 [57.7%]) or 3 (33 of 63 [52.4%]) concomitant AEDs reached their maximum target dose level. The maximum target lacosamide dose was reached by 38 of 55 (69.1%) patients not on concomitant SCB AEDs and 62 of 116 (53.4%) of those on ≥1 SCB AED.
Efficacy
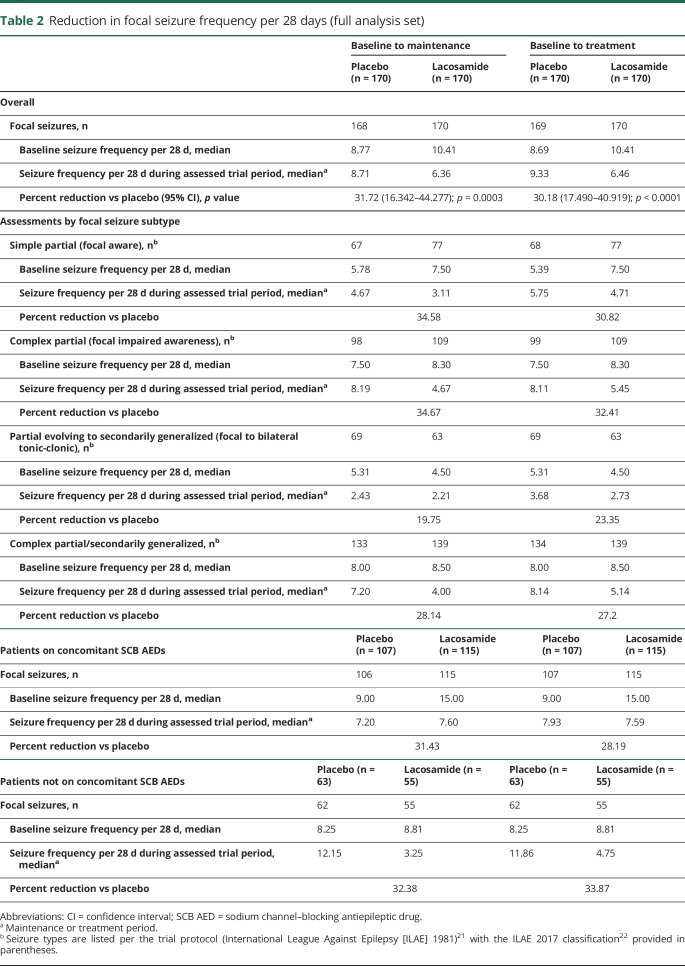
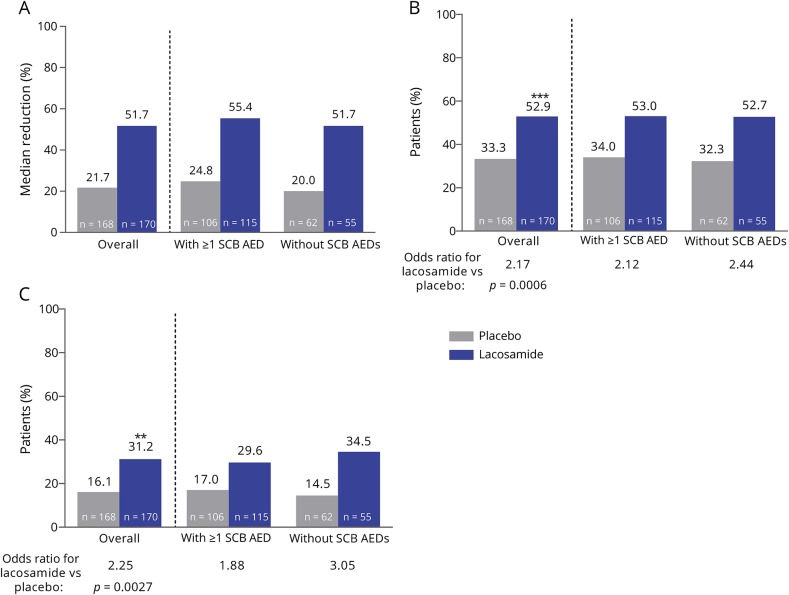
Three hundred forty patients had postbaseline seizure frequency data and were included in the full analysis set (figure 2). At baseline, the median focal seizure frequency per 28 days was 10.41 for patients randomized to lacosamide and 8.77 for those randomized to placebo (table 2). The percent reduction for lacosamide vs placebo in focal seizure frequency per 28 days was 31.72% (p = 0.0003) during maintenance and 30.18% (p < 0.0001) during treatment (table 2). The median percent reductions from baseline to maintenance in focal seizure frequency per 28 days were 51.7% and 21.7% for lacosamide and placebo, respectively (figure 3). Generally similar responses were observed during the entire treatment period (figure e-1 available from Dryad, doi.org/10.5061/dryad.kt5jj49).
Table 2.
Reduction in focal seizure frequency per 28 days (full analysis set)
Figure 3. Analyses of focal seizure frequency per 28 days during maintenance.
(A) Median percent reduction from baseline, (B) 50% responder rates, and (C) 75% responder rates, assessed for the overall population and for patients with and without concomitant sodium channel–blocking antiepileptic drugs (SCB AEDs). **p ≤ 0.01, ***p ≤ 0.001.
The proportions of 50% and 75% responders during the maintenance period were higher with lacosamide vs placebo (figure 3). The mean proportion of seizure-free days during maintenance was 0.71 on lacosamide and 0.66 on placebo (LS mean treatment difference 0.07 (95% CI 0.029–0.115, p = 0.0011). Among patients who completed maintenance, 23 of 152 (15.1%) on lacosamide and 15 of 154 (9.7%) on placebo were seizure-free. Similar proportions of patients on lacosamide (32 of 170 [18.8%]) and placebo (39 of 169 [23.1%]) had a ≥25% increase from baseline to treatment in focal seizure frequency per 28 days.
Subgroup analyses showed similar efficacy of lacosamide in patients with and without concomitant SCB AEDs (table 2 and figure 3). Assessments by focal seizure subtype showed reductions in seizure frequency per 28 days with lacosamide vs placebo in simple partial (focal aware), complex partial (focal impaired awareness), and secondarily generalized (focal to bilateral tonic-clonic) seizures, as well as reductions in the combined category of complex partial and/or secondarily generalized seizures (table 2). Higher median percent reductions from baseline in seizure frequency per 28 days and higher 50% and 75% responder rates were also observed with lacosamide vs placebo for these focal seizure subtypes (figure e-2 available from Dryad, doi.org/10.5061/dryad.kt5jj49).
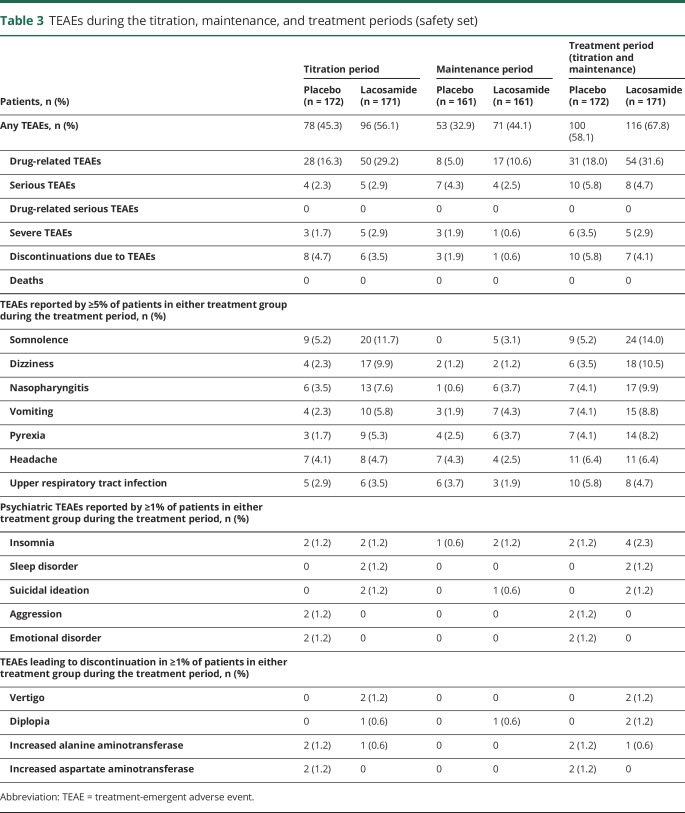
Safety and tolerability
One hundred sixteen (67.8%) patients on lacosamide and 100 (58.1%) on placebo reported TEAEs during the treatment period (table 3). As judged by the investigator, these TEAEs were drug related in 54 (31.6%) patients on lacosamide and 31 (18.0%) on placebo. Most TEAEs were mild or moderate in intensity; 5 (2.9%) patients on lacosamide and 6 (3.5%) on placebo reported severe TEAEs. In both treatment groups, the incidences of TEAEs and drug-related TEAEs were higher during titration than maintenance (table 3).
Table 3.
TEAEs during the titration, maintenance, and treatment periods (safety set)
In the lacosamide group, somnolence and dizziness were the most common TEAEs (≥10% of patients) and the most common drug-related TEAEs (≥5% of patients). Somnolence was reported by 24 (14.0%) lacosamide-treated patients (34 events) (placebo 9 [5.2%] patients, 12 events) and was considered to be drug related in 21 (12.3%) patients on lacosamide (placebo: 8 [4.7%]). All events of somnolence were mild or moderate in intensity. One patient discontinued lacosamide due to somnolence. The median time from lacosamide initiation to onset of somnolence was 24.0 days (placebo 6.0 days), with a median dose at somnolence onset of 8.0 mg/kg/d among patients in the <30 kg and 30 to <50 kg weight bands and 225 mg/d among patients weighing ≥50 kg. The median duration of somnolence during treatment was 6.0 days on lacosamide and 9.5 days on placebo.
Eighteen (10.5%) patients on lacosamide reported a total of 22 events of dizziness (placebo 6 [3.5%] patients, 6 events). Dizziness was considered to be drug related in 15 (8.8%) patients on lacosamide and 4 (2.3%) on placebo. All events were mild to moderate in intensity, and none led to trial discontinuation. The median time from lacosamide initiation to onset of dizziness was 26.5 days (placebo 38.5 days), with a median dose at onset of 6.0 mg/kg/d for patients weighing 30 to <50 kg and 350 mg/d for patients weighing ≥50 kg. The median duration of dizziness during treatment was 7.5 days on lacosamide and 12.5 days on placebo.
Psychiatric TEAEs were reported by 11 (6.4%) patients in each treatment group. Insomnia was the most common psychiatric TEAE, reported by 4 (2.3%) patients on lacosamide and 2 (1.2%) patients on placebo (table 3). Two patients (1.2%) treated with lacosamide had a total of 3 events of suicidal ideation. These events were mild in intensity, were resolved, and were not related to trial medication as assessed by the trial investigator. There were no suicide attempts during the trial. Severe psychiatric TEAEs were reported by 1 patient on placebo only (severe auditory hallucinations). No patients reported TEAEs related to psychotic disorders, memory impairment, amnesia, or cognitive disorders.
Similar incidences of serious TEAEs were observed in patients on lacosamide (8 [4.7%]) and placebo (10 [5.8%]), and none were considered to be drug-related (table 3). Convulsion was the only serious TEAE reported by ≥2 patients (lacosamide: 2 [1.2%]; placebo: 3 [1.7%]). A serious TEAE of syncope was reported by 1 patient while on a dose of 5.5 mg/kg/d lacosamide. This TEAE was moderate in intensity, did not lead to a dose change, and resolved. The patient experienced a second TEAE of syncope 6 days after her final lacosamide dose; this TEAE was considered to be serious but mild in intensity. Neither incident was considered to be related to lacosamide. ECG data showed a slight prolongation of the PR duration and QRS duration (table e-1 available from Dryad, doi.org/10.5061/dryad.kt5jj49). One patient had a serious TEAE of bradycardia while on a dose of 8 mg/kg/d lacosamide; this TEAE was mild in intensity, was not considered to be related to lacosamide, did not lead to a dose change, and resolved. Vital signs assessments before treatment (screening and baseline visits) showed that the patient had a supine pulse rate of 82 to 84 bpm. All supine pulse rates recorded at vital signs assessments during treatment were ≥66 bpm, except for the value recorded during the event of bradycardia (61 bpm). None of the patient's ECG parameters showed a clear increase during treatment, and most recordings showed a shortened PR duration compared to baseline (table e-2 available from Dryad, doi.org/10.5061/dryad.kt5jj49).
Few patients in either treatment group (lacosamide 7 [4.1%]; placebo 10 [5.8%]) had a TEAE that led to discontinuation during the treatment period (table 3). Discontinuation due to TEAEs was more common during titration than maintenance (table 3), with a median time to discontinuation of 36 days in the lacosamide group and 50 days in the placebo group. Vertigo and diplopia were the only TEAEs leading to discontinuation of lacosamide in ≥2 patients (diplopia [n = 1]; vertigo [n = 1]; vertigo and diplopia [n = 1]; these events were considered drug related), all of whom were receiving concomitant treatment with a SCB AED.
Analyses of tolerability by number of concomitant AEDs did not show any clear trends in the overall incidences of TEAEs, drug-related TEAEs, or discontinuations due to TEAEs (table e-3 available from Dryad, doi.org/10.5061/dryad.kt5jj49). Similar incidences of somnolence were observed in lacosamide-treated patients on 1, 2, or 3 concomitant AEDs, whereas the majority of patients who reported somnolence on placebo were taking 3 concomitant AEDs. The incidence of dizziness on lacosamide appeared to increase with an increasing number of concomitant AEDs.
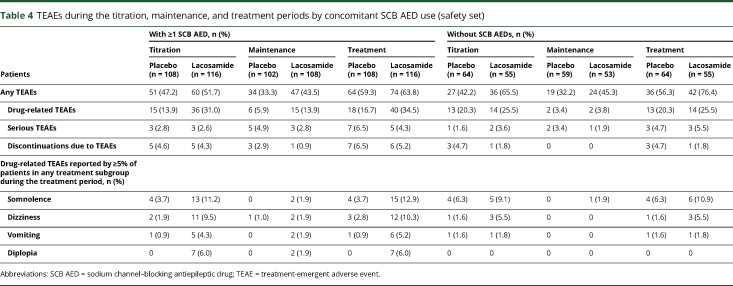
Analyses by concomitant SCB use showed a higher incidence of drug-related TEAEs in patients taking lacosamide with a concomitant SCB (34.5%; 16.7% with placebo) than in those with no SCB AEDs (25.5%; 20.3% with placebo) (table 4). The incidence of drug-related somnolence was similar in lacosamide-treated patients who were on and those not on concomitant SCB AEDs, whereas the incidence of drug-related dizziness was higher in lacosamide-treated patients who were on concomitant SCBs than in those not on SCB AEDs. Discontinuations due to TEAEs were low in lacosamide-treated patients and were similar to those of patients taking placebo regardless of whether SCB AEDs were part of the treatment regimen (on concomitant SCBs: 5.2% with lacosamide, 6.5% with placebo; not on SCB AEDs: 1.8% with lacosamide, 4.7% with placebo).
Table 4.
TEAEs during the titration, maintenance, and treatment periods by concomitant SCB AED use (safety set)
Assessments of behavior and cognitive function showed stable scores over the treatment period. Shifts from baseline to last visit in Achenbach CBCL 1.5—5 and CBCL/6—18 T-scores were similar in patients on lacosamide and on placebo (table e-4 available from Dryad, doi.org/10.5061/dryad.kt5jj49), with most patients remaining in their baseline category (normal, borderline, or clinically significant). Of those with a change in category, more improved than worsened. For the BRIEF and BRIEF-Preschool assessments, shifts in T-score findings from baseline to last visit were similar in each treatment group, with very few patients changing category (table e-5 available from Dryad, doi.org/10.5061/dryad.kt5jj49). Of those with a change in category, more patients improved than worsened.
No consistent or clinically relevant changes from baseline were observed for hematology, clinical chemistry, or endocrinology parameters, and no clinically relevant changes were observed for vital signs or ECG assessments. Pharmacokinetic data for lacosamide are shown in table e-6 (available from Dryad, doi.org/10.5061/dryad.kt5jj49). For patients on lacosamide, the geometric LS mean ratios for treatment/baseline and their 90% CIs were within the 80% to 125% limits for valproic acid, levetiracetam, lamotrigine, carbamazepine, topiramate, and oxcarbazepine (MHD) (figure e-3 available from Dryad, doi.org/10.5061/dryad.kt5jj49).
Discussion
In this double-blind placebo-controlled trial, adjunctive lacosamide was efficacious in reducing seizure frequency and was generally well tolerated in children and adolescents (age ≥4–<17 years) with uncontrolled focal seizures.
A weight-based dosing scheme was used; the maximum dose for each weight band targeted plasma levels shown to be at the upper limit of the therapeutic adjunctive dose in adults (400 mg/d).23 This weight-based dosing algorithm and flexible dose escalation during the titration period allowed physicians to tailor lacosamide treatment for each child.
A clinically relevant, significant reduction in focal seizure frequency per 28 days was observed with lacosamide vs placebo from baseline to the maintenance and treatment periods. Secondary and post hoc analyses showed greater median percent reductions from baseline in focal seizure frequency, as well as higher 50% and 75% responder rates and higher seizure-freedom rates, with lacosamide compared with placebo. Lacosamide was efficacious regardless of whether SCB AEDs were part of the concomitant treatment regimen. Subgroup analyses indicated the efficacy of lacosamide across all focal seizure types. The efficacy of lacosamide observed in children and adolescents in the current trial was in line with that reported for adults with focal seizures.4–6,24 These results further support the concept of extrapolation of efficacy data from adults to the pediatric population with focal seizures.25
The 50% responder rate observed with lacosamide in children (52.9%) was consistent with that reported for adults (35%–49%); however, the 50% responder rate with placebo was somewhat higher (33.3% vs 22.6%).24 This was not unexpected because higher 50% responder rates for placebo have been observed in children compared with adults.26 In this trial, the 50% responder rate with placebo was comparable to that reported with placebo in a randomized trial of adjunctive zonisamide in children with focal seizures (31%).27
The TEAEs most commonly reported during adjunctive lacosamide treatment in children were consistent with AEs reported during lacosamide treatment in adults (somnolence, dizziness) and with infections frequently encountered in double-blind placebo-controlled trials and open-label studies of other AEDs in pediatric patients with focal seizures (nasopharyngitis, pyrexia).27–33 The incidences of nasopharyngitis and pyrexia were higher with lacosamide than placebo; however, these TEAEs mainly occurred during the titration period, with low incidences (<4% of patients) during maintenance. A similar proportion of patients on lacosamide and placebo reported psychiatric TEAEs. The incidence of serious TEAEs was similar on lacosamide and placebo, and few patients in both treatment groups reported severe TEAEs or discontinued because of TEAEs. In both treatment groups, a higher incidence of TEAEs was reported during titration than maintenance, which is consistent with data reported in adults.34 This difference was most pronounced for drug-related TEAEs, with 29% of patients on lacosamide reporting TEAEs in this category during titration vs 11% during maintenance. However, the initiation and flexible uptitration of lacosamide was generally well tolerated with few patients requiring a dose reduction or discontinuing because of TEAEs. In both treatment groups, analyses of tolerability by number of concomitant AEDs did not show any trends in the overall incidences of TEAEs, drug-related TEAEs, or discontinuations because of TEAEs.
Somnolence and dizziness were the most commonly reported TEAEs, and the most common drug-related TEAEs during adjunctive lacosamide treatment. Somnolence and dizziness occurred mainly during titration, and the duration of these TEAEs was similar between patients on lacosamide and those on placebo. In the lacosamide group, the incidence of somnolence was not related to the number of concomitant AEDs. Drug-related somnolence was reported by similar proportions of patients treated with lacosamide on concomitant SCB AEDs (12.9%) and those not on SCB AEDs (10.9%). The incidence of dizziness with lacosamide increased with the number of concomitant AEDs, and the incidence of drug-related dizziness was higher in patients on SCB AEDs (10.3%) than in those not on SCB AEDs (5.5%).
Clinical practice experience with adjunctive lacosamide has shown a better35–38 or similar39–41 tolerability profile in adult patients not on SCB AEDs compared with those on SCB AEDs. A retrospective cohort study of children and adolescents (age <21 years) with focal, generalized, or mixed epilepsy (n = 223) showed that use of an SCB AED was an independent predictor of time to lacosamide treatment failure.42 Furthermore, analyses of pooled data from double-blind placebo-controlled trials in adults showed a potential for better tolerability of adjunctive lacosamide when taken without SCB AEDs.43 Among lacosamide-treated adults on a SCB AED, discontinuations because of AEs were dose-dependent (200 mg, 5.5%; 400 mg, 14.4%; 600 mg, 31.0%) and most commonly occurred because of dizziness (7.0% of patients).43 In contrast, adjunctive lacosamide was well tolerated in the current pediatric trial regardless of whether SCB AEDs were part of the treatment regimen. Discontinuation rates were similar for lacosamide and placebo in patients with and without concomitant SCB AEDs, and no patients discontinued because of dizziness. The improved tolerability of adjunctive lacosamide in patients on SCB AEDs in the pediatric trial compared to the trials in adults may be related to the different trial designs. The pediatric trial had a flexible titration schedule with the option of back-titration steps if needed, whereas the adult trials applied forced titration to a predefined randomized dose for each patient. Individualized titration and dosing may allow optimization of tolerability of adjunctive lacosamide treatment in patients taking various AED combinations.
Children with epilepsy have an increased risk for several neurologic (e.g., cognitive impairment) and psychological (e.g., mood disorders, attention-deficit/hyperactivity disorder) disorders, some of which may be linked to the use of AEDs.44 The presence of hyperactivity or impulsivity at the time of AED treatment initiation is a predictor of behavioral side effects.45 In the current trial, scores for behavior and cognitive function (Achenbach CBCL and BRIEF) were generally stable and similar for both treatment groups, with no worsening for patients on lacosamide vs placebo; however, results for the 4- to 6-year-old group should be interpreted with caution given the small number of patients in this category. Further evaluations are needed to determine the long-term effects of lacosamide on cognition and behavior in children.
In children and adolescents (age ≥4–<17 years) with focal seizures, plasma concentrations of valproic acid, levetiracetam, lamotrigine, carbamazepine, topiramate, oxcarbazepine (MHD), clonazepam, and clobazam were not affected by concomitant lacosamide use. The data for clonazepam and clobazam should be interpreted with caution because of the small sample size. In line with data in adults,46 these pharmacokinetic analyses suggest that no dose adjustment for the respective AEDs would generally be needed when lacosamide is added to or removed from the treatment regimen.
In this randomized double-blind trial, adjunctive lacosamide was efficacious in reducing focal seizure frequency in children and adolescents (≥4 to <17 years of age) with uncontrolled focal seizures and was generally well tolerated with flexible titration and weight-based dosing. These data, together with the favorable, predictable pharmacokinetic profile of lacosamide, its low potential for clinically relevant pharmacokinetic drug-drug interactions, and bioequivalent oral (tablets or oral solution) formulations,3,47 demonstrate that lacosamide is a valuable addition to the armamentarium of licensed therapies for focal seizures in pediatric patients.
Acknowledgment
The authors thank the patients and their caregivers and the clinical project team. Armel Stockis (UCB Pharma, Braine-l'Alleud, Belgium) provided input into the post hoc analyses of pharmacokinetic data. Publication management was provided by Barbara Pelgrims, PhD (UCB Pharma, Brussels, Belgium). Deanne Dilley, UCB Pharma, Raleigh, NC, contributed to the statistical analysis.
Glossary
- AE
adverse event
- AED
antiepileptic drug
- BRIEF
Behavior Rating Inventory of Executive Function
- CBCL
Child Behavior Checklist
- CI
confidence interval
- ILAE
International League Against Epilepsy
- LS
least squares
- MHD
10-hydroxycarbazepine
- SCB
sodium channel–blocking
- TEAE
treatment-emergent adverse event
Appendix. Coinvestigators

Footnotes
Class of Evidence: NPub.org/coe
Author contributions
V. Farkas contributed to acquisition of data, analysis or interpretation of data, and drafting/revising the manuscript for content. B. Steinborn contributed to acquisition of data and drafting/revising the manuscript for content. J.R. Flamini contributed to acquisition of data, analysis or interpretation of data, and drafting/revising the manuscript for content. Y. Zhang contributed to analysis or interpretation of data, statistical analyses, and drafting/revising the manuscript for content. N. Yuen contributed to analysis or interpretation of data and drafting/revising the manuscript for content. S. Borghs, A. Bozorg, and T. Daniels contributed to trial concept or design, analysis or interpretation of data, and drafting/revising the manuscript for content. P. Martin contributed to analysis and interpretation of the post hoc pharmacokinetic data and revising the manuscript for content. H.C. Carney contributed to drafting/revising the manuscript for content. S. Dimova contributed to analysis or interpretation of data and drafting/revising the manuscript for content. I.E. Scheffer contributed to acquisition of data and drafting/revising the manuscript for content.
Study funding
Supported by UCB Pharma, Brussels, Belgium.
Disclosure
V. Farkas has participated as principal investigator in UCB Pharma clinical trials. B. Steinborn has participated as principal investigator in UCB Pharma clinical trials and has acted as a speaker for UCB Pharma in Poland. J. Flamini participated as an investigator in the current clinical trial. Y. Zhang, N. Yuen, S. Borghs, A. Bozorg, T. Daniels, P. Martin, and S. Dimova are employees of UCB Pharma. H. Carney provided writing and editorial assistance toward the development of the manuscript, which was contracted by UCB Pharma. I. Scheffer serves on the editorial boards of Neurology® and Epileptic Disorders; may accrue future revenue on a pending patent on a therapeutic compound; has received speaker honoraria from Athena Diagnostics, UCB Pharma, GlaxoSmithKline, Eisai, and Transgenomic; has received scientific advisory board honoraria from Nutricia, BioMarin, and GlaxoSmithKline; has received funding for travel from Athena Diagnostics, UCB Pharma, BioMarin, and GlaxoSmithKline; and receives/has received research support from the Australian National Health and Medical Research Council, ARC, NIH, Health Research Council of New Zealand, March of Dimes, the Weizmann Institute, CURE, the US Department of Defense, and the Perpetual Charitable Trustees. Go to Neurology.org/N for full disclosures.
References
- 1.Verrotti A, Loiacono G, Coppola G, Spalice A, Mohn A, Chiarelli F. Pharmacotherapy for children and adolescents with epilepsy. Expert Opin Pharmacother 2011;12:175–194. [DOI] [PubMed] [Google Scholar]
- 2.Rogawski MA, Tofighy A, White HS, Matagne A, Wolff C. Current understanding of the mechanism of action of the antiepileptic drug lacosamide. Epilepsy Res 2015;110:189–205. [DOI] [PubMed] [Google Scholar]
- 3.Cawello W. Clinical pharmacokinetic and pharmacodynamic profile of lacosamide. Clin Pharmacokinet 2015;54:901–914. [DOI] [PubMed] [Google Scholar]
- 4.Ben-Menachem E, Biton V, Jatuzis D, Abou-Khalil B, Doty P, Rudd GD. Efficacy and safety of oral lacosamide as adjunctive therapy in adults with partial-onset seizures. Epilepsia 2007;48:1308–1317. [DOI] [PubMed] [Google Scholar]
- 5.Chung S, Sperling MR, Biton V, et al. Lacosamide as adjunctive therapy for partial-onset seizures: a randomized controlled trial. Epilepsia 2010;51:958–967. [DOI] [PubMed] [Google Scholar]
- 6.Halász P, Kälviäinen R, Mazurkiewicz-Beldzińska M, et al. Adjunctive lacosamide for partial-onset seizures: efficacy and safety results from a randomized controlled trial. Epilepsia 2009;50:443–453. [DOI] [PubMed] [Google Scholar]
- 7.Wechsler RT, Li G, French J, et al. Conversion to lacosamide monotherapy in the treatment of focal epilepsy: results from a historical-controlled, multicenter, double-blind study. Epilepsia 2014;55:1088–1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baulac M, Rosenow F, Toledo M, et al. Efficacy, safety, and tolerability of lacosamide monotherapy versus controlled-release carbamazepine in patients with newly diagnosed epilepsy: a phase 3, randomised, double-blind, non-inferiority trial. Lancet Neurol 2017;16:43–54. [DOI] [PubMed] [Google Scholar]
- 9.Hong Z, Inoue Y, Liao W, et al. Efficacy and safety of adjunctive lacosamide for the treatment of partial-onset seizures in Chinese and Japanese adults: a randomized, double-blind, placebo-controlled study. Epilepsy Res 2016;127:267–275. [DOI] [PubMed] [Google Scholar]
- 10.Runge U, Arnold S, Brandt C, et al. A noninterventional study evaluating the effectiveness and safety of lacosamide added to monotherapy in patients with epilepsy with partial-onset seizures in daily clinical practice: the VITOBA study. Epilepsia 2015;56:1921–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Steinhoff BJ, Eckhardt K, Doty P, De Backer M, Brunnert M, Schulze-Bonhage A. A long-term noninterventional safety study of adjunctive lacosamide therapy in patients with epilepsy and uncontrolled partial-onset seizures. Epilepsy Behav 2016;58:35–43. [DOI] [PubMed] [Google Scholar]
- 12.Villanueva V, Garcés M, López-Gomáriz E, et al. Early add-on lacosamide in a real-life setting: results of the REALLY study. Clin Drug Investig 2015;35:121–131. [DOI] [PubMed] [Google Scholar]
- 13.Ferreira J, Daniels T, Dilley D, Dimova S, Rice K, Byrnes W. Safety and tolerability of lacosamide as adjunctive therapy in children with partial-onset seizures. [Abstract] Eur J Paediatr Neurol 2015;19(suppl 1):S56–S57. [Google Scholar]
- 14.Yuen N, Taeter C, Beller C, Dimova S, Daniels T, Bozorg A. Long-term tolerability of adjunctive lacosamide in pediatric patients aged 4 to <16 years with focal seizures: an interim pooled analysis of data from open-label trials. Presented at the 71st Annual Meeting of the American Epilepsy Society; December 1–5, 2017; Washington, DC. Abstract 1.282. Available at: www.aesnet.org. Accessed January 30, 2019.
- 15.Verrotti A, Loiacono G, Pizzolorusso A, et al. Lacosamide in pediatric and adult patients: comparison of efficacy and safety. Seizure 2013;22:210–216. [DOI] [PubMed] [Google Scholar]
- 16.Grosso S, Parisi P, Spalice A, Verrotti A, Balestri P. Efficacy and safety of lacosamide in infants and young children with refractory focal epilepsy. Eur J of Paediatr Neurol 2014;18:55–59. [DOI] [PubMed] [Google Scholar]
- 17.Pasha I, Kamate M, Didagi SK. Efficacy and tolerability of lacosamide as an adjunctive therapy in children with refractory partial epilepsy. Pediatr Neurol 2014;51:509–514. [DOI] [PubMed] [Google Scholar]
- 18.Gulati P, Cannell P, Ghia T, et al. Lacosamide as adjunctive therapy in treatment-resistant epilepsy in childhood. J Paediatr Child Health 2015;51:794–797. [DOI] [PubMed] [Google Scholar]
- 19.Kim JS, Kim H, Lim BC, et al. Lacosamide as an adjunctive therapy in pediatric patients with refractory focal epilepsy. Brain Dev 2014;36:510–515. [DOI] [PubMed] [Google Scholar]
- 20.Toupin JF, Lortie A, Major P, et al. Efficacy and safety of lacosamide as an adjunctive therapy for refractory focal epilepsy in paediatric patients: a retrospective single-centre study. Epileptic Disord 2015;17:436–443. [DOI] [PubMed] [Google Scholar]
- 21.Proposal for revised clinical and electroencephalographic classification of epileptic seizures: from the Commission on Classification and Terminology of the International League Against Epilepsy. Epilepsia 1981;22:489–501. [DOI] [PubMed] [Google Scholar]
- 22.Fisher RS, Cross JH, French JA, et al. Operational classification of seizure types by the International League Against Epilepsy: position paper of the ILAE Commission for Classification and Terminology. Epilepsia 2017;58:522–530. [DOI] [PubMed] [Google Scholar]
- 23.Winkler J, Schoemaker R, Stockis A. Lacosamide population pharmacokinetics in children from 6 months to 17 years of age. [Abstract] Epilepsia 2015;56(suppl 1):177–178.25534640 [Google Scholar]
- 24.Chung S, Ben-Menachem E, Sperling MR, et al. Examining the clinical utility of lacosamide: pooled analyses of three phase II/III clinical trials. CNS Drugs 2010;24:1041–1054. [DOI] [PubMed] [Google Scholar]
- 25.Pellock JM, Arzimanoglou A, D'Cruz O, et al. Extrapolating evidence of antiepileptic drug efficacy in adults to children ≥2 years of age with focal seizures: the case for disease similarity. Epilepsia 2017;58:1686–1696. [DOI] [PubMed] [Google Scholar]
- 26.Rheims S, Cucherat M, Arzimanoglou A, Ryvlin P. Greater response to placebo in children than in adults: a systematic review and meta-analysis in drug-resistant partial epilepsy. PLoS Med 2008;5:e166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guerrini R, Rosati A, Segieth J, Pellacani S, Bradshaw K, Giorgi L. A randomized phase III trial of adjunctive zonisamide in pediatric patients with partial epilepsy. Epilepsia 2013;54:1473–1480. [DOI] [PubMed] [Google Scholar]
- 28.Appleton R, Fichtner K, LaMoreaux L, et al. Gabapentin as add-on therapy in children with refractory partial seizures: a 12-week, multicentre, double-blind, placebo-controlled study: Gabapentin Paediatric Study Group. Epilepsia 1999;40:1147–1154. [DOI] [PubMed] [Google Scholar]
- 29.Appleton R, Fichtner K, LaMoreaux L, et al. Gabapentin as add-on therapy in children with refractory partial seizures: a 24-week, multicentre, open-label study. Dev Med Child Neurol 2001;43:269–273. [DOI] [PubMed] [Google Scholar]
- 30.Duchowny M, Pellock JM, Graf WD, et al. A placebo-controlled trial of lamotrigine add-on therapy for partial seizures in children: Lamictal Pediatric Partial Seizure Study Group. Neurology 1999;53:1724–1731. [DOI] [PubMed] [Google Scholar]
- 31.Elterman RD, Glauser TA, Wyllie E, Reife R, Wu SC, Pledger G. A double-blind, randomized trial of topiramate as adjunctive therapy for partial-onset seizures in children: Topiramate YP Study Group. Neurology 1999;52:1338–1344. [DOI] [PubMed] [Google Scholar]
- 32.Glauser TA, Nigro M, Sachdeo R, et al. Adjunctive therapy with oxcarbazepine in children with partial seizures: the Oxcarbazepine Pediatric Study Group. Neurology 2000;54:2237–2244. [DOI] [PubMed] [Google Scholar]
- 33.Glauser TA, Ayala R, Elterman RD, et al. Double-blind placebo-controlled trial of adjunctive levetiracetam in pediatric partial seizures. Neurology 2006;66:1654–1660. [DOI] [PubMed] [Google Scholar]
- 34.Biton V, Gil-Nagel A, Isojarvi J, Doty P, Hebert D, Fountain NB. Safety and tolerability of lacosamide as adjunctive therapy for adults with partial-onset seizures: analysis of data pooled from three randomized, double-blind, placebo-controlled clinical trials. Epilepsy Behav 2015;52:119–127. [DOI] [PubMed] [Google Scholar]
- 35.Foldvary-Schaefer N, Fong JS, Morrison S, Wang L, Bena J. Lacosamide tolerability in adult patients with partial-onset seizures: impact of planned reduction and mechanism of action of concomitant antiepileptic drugs. Epilepsy Behav 2016;57:155–160. [DOI] [PubMed] [Google Scholar]
- 36.Hoefler J, Dobesberger J, Kuchukhidze G, Walser G, Unterberger I, Trinka E. Effect of lacosamide polytherapy with other sodium channel blockers: a retrospective study. [Abstract] Epilepsy Curr 2012;12:361–362. [Google Scholar]
- 37.Kamel JT, DeGruyter MA, D'Souza WJ, Cook MJ. Clinical experience with using lacosamide for the treatment of epilepsy in a tertiary centre. Acta Neurol Scand 2013;127:149–153. [DOI] [PubMed] [Google Scholar]
- 38.Villanueva V, López-Gomáriz E, López-Trigo J, et al. Rational polytherapy with lacosamide in clinical practice: results of a Spanish cohort analysis RELACOVA. Epilepsy Behav 2012;23:298–304. [DOI] [PubMed] [Google Scholar]
- 39.Stephen LJ, Kelly K, Parker P, Brodie MJ. Adjunctive lacosamide in clinical practice: sodium blockade with a difference? Epilepsy Behav 2011;22:499–504. [DOI] [PubMed] [Google Scholar]
- 40.Harden CL, Cohn A, Lowe M, Serrano E. Initial post marketing experience with lacosamide in adult patients with epilepsy. Epilepsy Res 2012;98:260–263. [DOI] [PubMed] [Google Scholar]
- 41.Novy J, Bartolini E, Bell GS, Duncan JS, Sander JW. Long-term retention of lacosamide in a large cohort of people with medically refractory epilepsy: a single centre evaluation. Epilepsy Res 2013;106:250–256. [DOI] [PubMed] [Google Scholar]
- 42.McGinnis E, Kessler SK. Lacosamide use in children with epilepsy: retention rate and effect of concomitant sodium channel blockers in a large cohort. Epilepsia 2016;57:1416–1425. [DOI] [PubMed] [Google Scholar]
- 43.Sake JK, Hebert D, Isojärvi J, et al. A pooled analysis of lacosamide clinical trial data grouped by mechanism of action of concomitant antiepileptic drugs. CNS Drugs 2010;24:1055–1068. [DOI] [PubMed] [Google Scholar]
- 44.Wei SH, Lee WT. Comorbidity of childhood epilepsy. J Formos Med Assoc 2015;114:1031–1038. [DOI] [PubMed] [Google Scholar]
- 45.Guilfoyle SM, Follansbee-Junger K, Smith AW, et al. Antiepileptic drug behavioral side effects and baseline hyperactivity in children and adolescents with new onset epilepsy. Epilepsia 2018;59:146–154. [DOI] [PubMed] [Google Scholar]
- 46.Cawello W, Stockis A, Andreas JO, Dimova S. Advances in epilepsy treatment: lacosamide pharmacokinetic profile. Ann NY Acad Sci 2014;1329:18–32. [DOI] [PubMed] [Google Scholar]
- 47.Cawello W, Bökens H, Nickel B, Andreas JO, Halabi A. Tolerability, pharmacokinetics, and bioequivalence of the tablet and syrup formulations of lacosamide in plasma, saliva, and urine: saliva as a surrogate of pharmacokinetics in the central compartment. Epilepsia 2013;54:81–88. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Underlying data from this manuscript may be requested by qualified researchers 6 months after product or indication approval in the US and/or Europe, or global development is discontinued, and 18 months after trial completion. Investigators may request access to anonymized individual patient data and redacted study documents, which may include raw datasets, analysis-ready datasets, study protocol, blank case report form, annotated case report form, statistical analysis plan, dataset specifications, and clinical study report. Before use of the data, proposals need to be approved by an independent review panel at www.clinicalstudydatarequest.com and a signed data sharing agreement will need to be executed. All documents are available in English only, for a prespecified time, typically 12 months, on a password-protected portal.