Abstract
Summary
We investigated the incidence trend in all major osteoporotic fractures for the whole country of Denmark between 1995 and 2010. Hip and other osteoporotic fractures declined for the general population and especially among women. But, we observed some increasing trend among men which needs more attention.
Purpose
The trend in osteoporotic fractures is varied across the globe, and there is no updated information in the case of Denmark for all major osteoporotic fractures (MOF). Thus, we investigated the incidence rates (IRs) of MOF among 50+ adults in Denmark over the period 1995–2010.
Methods
A series of cross-sectional analyses was done using the Danish National Health Service Register. Participants were 50+ adults in the full country Denmark with a MOF between 1995 and 2010. Gender- specific IRs of MOF per 10,000 person years (PYs) were estimated, in addition to IRs of individual fracture sites (hip, vertebrae, humerus, and radius/ulna), and women-to-men IR ratios for MOF.
Results
A general decline was observed in IRs of MOF for the whole population (from 169.8 per 10,000 PYs in 1995, to 148.0 in 2010), which was more pronounced among women. Thirty-one and nineteen percent of decline was observed in hip fracture rates among women and men, respectively. The trend in clinical vertebral fracture was slightly decreasing for women and increasing for men. The women-to-men rate ratio of MOF decreased noticeably from 2.93 to 2.72 during study period.
Conclusions
We observed declining trends in MOF and hip fracture for both sexes. However, a lower rate of decrease of hip fracture and an increasing trend in vertebral fracture was noticed among men. Considering our observations and the major economic burden that accompanies this devastating disease, more attention should be paid to MOF, especially in men.
Keywords: Osteoporosis, Osteoporotic fractures, Epidemiology, Incidence rates
Introduction
This article was published in error in Archives of Osteoporosis and has now been retracted [1]. Osteoporosis is a systemic metabolic skeletal disease where reduced bone mineral density would make patients susceptible to fractures, called osteoporotic (OP) fractures. Based on literature consensus, major osteoporotic fractures (MOF) include mostly hip, clinical vertebral, humerus, and forearm (radius/ulna) fractures, which altogether are a leading cause of morbidity and mortality worldwide [2]. OP fractures incurred 5.8 million lost Disability-Adjusted Life Years (DALYs) worldwide in the year 2000, of which 51% was represented by two WHO world regions Europe and the Americas [3]. The occurrence of a MOF would not only impact the well-being and function of a patient, including an elevated mortality risk, but also has substantial economic consequences [4–9]. It is estimated that in the year 2011, the associated costs of OP fractures were €36 billion in Europe, and €1.6 billion in Denmark (including both direct and productivity costs), and these costs are estimated to double by 2050 [10, 11].
The predicted increase in OP fractures has been reported in numerous countries, including the USA, China, and in worldwide projections (especially developing countries), and is in large part due to the impending aging trajectory [12–14]. A recent study in the UK with a relatively long follow-up time (1990–2012) revealed mostly a rising or steady trend for most OP fractures in both men and women [15]. However, despite the expected increase, a number of studies have identified a leveling, or decline in hip fractures in recent years [16–21]. This led the International Osteoporosis Foundation (IOF) working group on fracture to request for updates on secular trends in hip and other OP fracture incidence rates (IRs) [22]. In Danish studies, age-adjusted hip fracture IRs increased between 1977 and 1999, yet a decline, particularly in women, has been observed since 1997 [23–25]. This trend of increasing fractures up to the 1990s, with a leveling of fracture rates in the past two decades, has been noted by others [18, 19, 26]. Apart from two single year studies which surveyed the IRs of forearm and OP fractures in 2010 and 2011, respectively, and two reports on hip fracture trend until 2006 and 2010, there has never been a country-specific report on secular incidence trends in all OP fractures for Denmark [24, 25, 27, 28]. Thus, the aim of this study was to investigate the IRs of MOF among adults aged 50 years or older in Denmark over the period 1995–2010.
Methods
Data source
We used data from the registry of the Danish National Health Service. The extensive registers in Denmark cover all contacts to the health sector for all citizens, without age restriction. This includes approximately 5.2 million individuals in 1995 and 5.5 million in 2010 [29]. The unique 10-digit civil registry number allocated to each Danish citizen was used to link the population-based registries and generate a complete hospital discharge history for each patient. Data on vital status for the Danish population have been collected since 1968 in the Civil Registration System, and all inpatient contacts have been registered in the Danish National Hospital Discharge Register (NHDR) since 1977 [30]. The NHDR covers all inpatient contacts since 1977, and beginning in 1995, the NHDR captures also all outpatient visits to hospitals, outpatient clinics, and emergency room visits. The validity of the Danish National fracture records have been previously verified [31].
Study design
We included patients, aged 50 years or older, who were diagnosed with a fracture in the period between 1995 and 2010. MOF were identified in accordance with the WHO/FRAX definition as hip, clinical symptomatic vertebral, humerus, or forearm (radius/ulna) fracture [32, 33]. They were clustered by site using the following International Classification of Diseases and Related Health Problems 10th Edition (ICD-10) codes: hip (S72.0-S72.2), clinical symptomatic vertebral (S12, S22.0, S22.1, S32.0, T08), humerus (S42.2-S42.4), and forearm (S52). As it is possible that the original fracture and follow-up visits or procedures may have the same ICD-10 code, we introduced a washout period to avoid double counting fractures in individuals. As 1995 was the first year of observation, we also applied a 1-year washout period prior to 1995. Thus, if a patient had a hip fracture code (ICD-10 S72.2) in 1995 and also had the same code in 1994, we did not include this in our analysis as we could not be certain that it was a new hip fracture or a recurring follow-up. After 1995, we took the first recorded fracture code in each calendar year and assessed if the patient had a previous code for the same fracture, or unspecified fracture, in the prior 365 days. If there were no codes for a prior fracture of the same type, or unspecified, in the prior 365 days, it was deemed an eligible new fracture, otherwise it was excluded. Additionally, for MOF, the first occurrence of a hip, clinical symptomatic vertebral, humerus, or forearm fracture was selected.
Statistical analysis
Population demographics for the background population in calendar years 1995–2010 were obtained online from Statistics Denmark [29]. IRs (number of fractures/10,000 person years [PYs]), and corresponding 95% confidence intervals (95% CI), were calculated by dividing all cases of first recorded fractures during the calendar year over the average number of persons alive in that calendar year. For example, to calculate the denominator for the year 2010, we first summed the number of people alive on 1 January 2010 and those alive on 1 January 2011, then divided this sum by two. Gender-specific IRs were estimated in addition to site-specific fracture rates. While we did not produce age-specific rates, we were able to standardize the IRs to the annual Danish population over the age 50, using the Statistics Denmark data. This permits a comparison to a similar age distribution. Women-to-men incidence rate ratios (IRRs) were calculated for MOF and determined by dividing the IR for women over the IR for men. The IRs were plotted over time both for MOF, as well as specific fracture sites, and the plots were examined by visual assessment. Data were analyzed using SAS version 9.3 (SAS Institute Inc. Cary, NC, USA).
Results
We identified a total of 422,380 MOF in Danish adults over 50 between 1995 and 2010, where a sum of 101,177 fractures occurred among men, and 321,203 cases among women (Table 1); thus, females sustained 76.0% of all MOF. There was a 4.5% relative increase in the total number of MOF from 1995 to 2010, although apart from a spike in 2010, the numbers were dropping until 2009. The mean age at first occurrence of a MOF was 74.1 years, and the age distribution was constant across all years.
Table 1.
Absolute number and incidence rates of major osteoporotic fractures among Danish adults aged 50+, stratified by sex and calendar year (1995–2010)
| Calendar year | Total | Men | Women | IRRW/M ratio | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of fractures | IR per 10,000 PYs | 95% CI | Number of fractures | IR per 10,000 PYs | 95% CI | Number of fractures | IR per 10,000 PYs | 95% CI | IRR W/M | 95% CI | |||||
| 1995 | 28,351 | 169.8 | 166.9 | 172.6 | 6323 | 82.9 | 80.0 | 85.9 | 22,028 | 242.8 | 238.2 | 247.4 | 2.93 | 2.85 | 3.01 |
| 1996 | 27,215 | 160.1 | 157.4 | 162.9 | 5908 | 75.8 | 73.1 | 78.6 | 21,307 | 231.5 | 227.1 | 236.0 | 3.05 | 2.97 | 3.14 |
| 1997 | 25,856 | 149.5 | 146.9 | 152.2 | 5850 | 73.5 | 70.9 | 76.3 | 20,006 | 214.3 | 210.1 | 218.6 | 2.91 | 2.83 | 3.00 |
| 1998 | 25,823 | 147.1 | 144.6 | 149.7 | 5850 | 72.2 | 69.6 | 74.9 | 19,973 | 211.3 | 207.1 | 215.5 | 2.93 | 2.84 | 3.01 |
| 1999 | 26,314 | 148.1 | 145.5 | 150.7 | 6141 | 74.7 | 72.1 | 77.4 | 20,173 | 211.3 | 207.1 | 215.5 | 2.83 | 2.75 | 2.91 |
| 2000 | 25,007 | 139.2 | 136.8 | 141.7 | 5925 | 71.1 | 68.6 | 73.7 | 19,082 | 198.1 | 194.1 | 202.2 | 2.79 | 2.71 | 2.87 |
| 2001 | 25,797 | 142.1 | 139.7 | 144.6 | 6004 | 71.1 | 68.6 | 73.7 | 19,793 | 203.8 | 199.8 | 207.9 | 2.87 | 2.78 | 2.95 |
| 2002 | 25,698 | 140.2 | 137.8 | 142.7 | 6211 | 72.7 | 70.2 | 75.3 | 19,487 | 199.3 | 195.3 | 203.3 | 2.74 | 2.66 | 2.82 |
| 2003 | 25,192 | 136.1 | 133.7 | 138.5 | 6198 | 71.6 | 70.0 | 75.2 | 18,994 | 192.7 | 188.8 | 196.7 | 2.69 | 2.61 | 2.77 |
| 2004 | 26,196 | 140.0 | 137.6 | 142.5 | 6446 | 73.6 | 71.0 | 76.2 | 19,750 | 198.6 | 194.7 | 202.6 | 2.70 | 2.63 | 2.78 |
| 2005 | 26,687 | 141.1 | 138.7 | 143.5 | 6603 | 74.4 | 71.8 | 77.0 | 20,084 | 200.2 | 196.2 | 204.2 | 2.69 | 2.62 | 2.77 |
| 2006 | 26,739 | 139.8 | 137.4 | 142.2 | 6558 | 72.8 | 70.4 | 75.4 | 20,181 | 199.2 | 195.4 | 203.2 | 2.74 | 2.66 | 2.81 |
| 2007 | 25,804 | 133.4 | 131.1 | 135.7 | 6538 | 71.6 | 69.2 | 74.2 | 19,266 | 188.5 | 184.7 | 192.3 | 2.63 | 2.56 | 2.71 |
| 2008 | 26,001 | 132.9 | 130.6 | 135.2 | 6569 | 71.0 | 68.6 | 73.5 | 19,432 | 188.3 | 184.6 | 192.2 | 2.65 | 2.58 | 2.73 |
| 2009 | 26,076 | 131.8 | 129.5 | 134.1 | 6681 | 71.3 | 68.9 | 73.8 | 19,395 | 186.2 | 182.5 | 190.0 | 2.61 | 2.54 | 2.69 |
| 2010 | 29,624 | 148.0 | 145.6 | 150.4 | 7372 | 77.6 | 75.1 | 80.2 | 22,252 | 211.5 | 207.5 | 215.5 | 2.72 | 2.65 | 2.80 |
| Total | 422,380 | 101,177 | 321,203 | ||||||||||||
IR incidence rate, CI confidence interval, IRRW/M women-to-men ratio of incidence rate, PYs person years
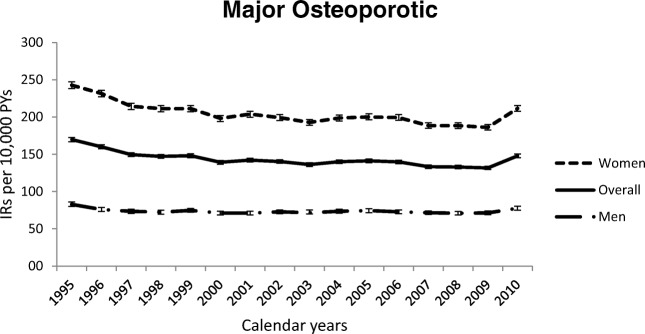
A general decline was observed in the IRs of MOF for the whole population, where IRs dropped from 169.8 per 10,000 PYs in 1995 to 148.0 in 2010 (Table 1), as visualized in Fig. 1. Among women, the rates for the MOF dropped during this 16-year study period from 242.8 to 211.5; however, it is worth mentioning that the rates had dropped even lower in the years 2008 and 2009 (IRs 188.3 and 186.2, respectively). For men, the MOF rates exhibited a smaller decrease from 82.9 in 1995 to 77.6 in 2010. The women-to-men rate ratio of MOF decreased noticeably from 2.93 (95% CI, 2.85–3.01) in 1995 to 2.72 (95% CI, 2.65–2.80) in 2010 (Table 1).
Fig. 1.
Incidence rates of major osteoporotic fractures for Danish adults aged 50+, stratified by sex and calendar year, 1995–2010. 95% confidence intervals are shown by small bars for each graph line and calendar year. IR incidence rates, PYs person years
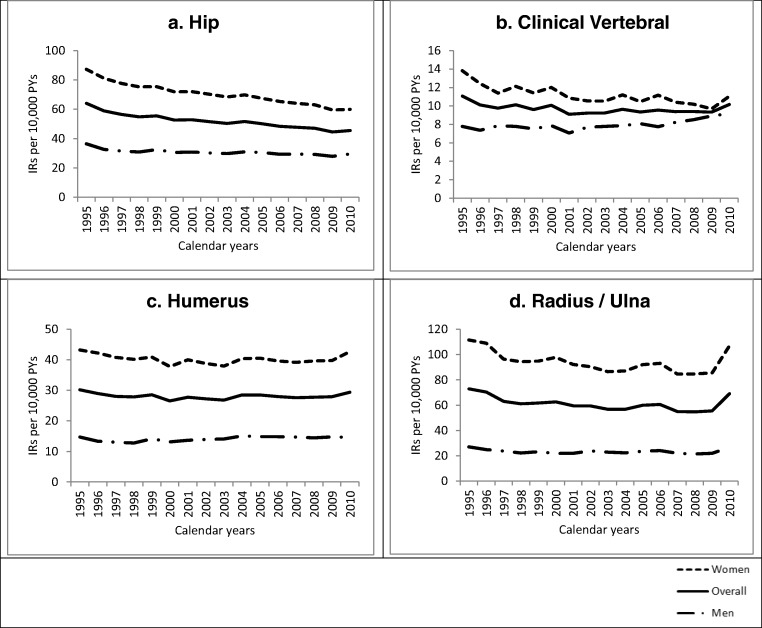
Regarding hip fractures, a total of 152,571 cases were identified, where 72.3% (110,349) of all hip fractures occurred in women, and 27.7% (42,222) occurred in men. The mean age for occurrence of hip fracture among the whole population was 80.0 years. The overall hip fracture IRs decreased during the study period, i.e., 1995 to 2010 from 64.1 per 10,000 PYs to 45.5, respectively, and this decrease was more prominent in women (Fig. 2a). We observed a 31% decline in hip fracture rates (from 87.2 to 59.9 per 10,000 PYs) among women and 19% decline (from 36.5 to 29.6 per 10,000 PYs) among men.
Fig. 2.
Incidence rates of major osteoporotic fracture subsites (a hip, b clinical vertebral, c humerus, d radius/ulna) for Danish adults aged 50+, stratified by sex and calendar year, 1995–2010. IR incidence rates, PYs person years
The IRs over time for the other MOF subsites are provided in Fig. 2b–d. The trend for clinical vertebral fracture remained steady between 1995 and 2010, yet there was a slightly decreasing trend for women and an increasing trend for men (Fig. 2b). Overall, humerus fracture rates remained stable, and this steady state was observed among both men and women (Fig. 2c). Regarding forearm fractures, there is a declining trend for the whole study population from 1995 to 2009 (IRs dropped from 73.0 in 1995 to 55.5 in 2009), but there was a spike in 2010 (IRs 69.1) (Fig. 2d). Women followed a similar trend to the overall trend regarding radius/ulna fracture, while for men, a smaller decrease was observed. The mean age of occurrence was 72.4 years for clinical vertebral fracture, 73.6 years for humerus fracture, and 69.6 years for radius/ulna fracture. Furthermore, females sustained 61.5% of all clinical vertebral fractures, 76.4% of all humerus fractures, and 82.1% of all radius/ulna fractures.
Discussion
In this study, we observed a reduction in IRs of MOF from 1995 to 2010 in 50+ adults in Denmark, where the striking finding was a reduction in hip fracture rates in both men and women. Among women, the IRs of all MOF have been declining, with exception of a rather steady state for humerus. But in men, apart from the gradually reducing hip and forearm fracture rates, steady rates for humerus fracture and a rising trend in vertebral fracture were noticed. The results of study by Driessen et al. in 2011 complement our observed decreasing trend in MOF for Denmark [28]. Considering the aging population, these findings are interesting, as we identify a decreasing incidence of MOF between 1995 and 2011. Yet, importantly, there appears to be differences between males and females, particularly for hip fractures, in Denmark.
In general, our findings are in line with the present literature affirming a decrease in hip fracture rates in both men and women. We observed a 31% decline (from 87.2 to 59.9 per 10,000 PYs) among women and 19% decline (from 36.5 to 29.6) among men. Driessen et al. estimated even lower IRs for hip fracture in Denmark in the year 2011, as 57.1 per 10,000 PYs for women, and 29.2 for men [28]. In numerous studies from different countries, a leveling or decrease in age- and sex-specific hip fracture rates especially in the past two decades has been noticed too [16–21, 24]. For instance, Leslie et al. showed that there was a 32% reduction in hip fracture rates among women in Canada (118.6 to 80.9 per 100,000 PYs), and 25% in men (68.2 to 51.1) between 1985 and 2005 [16]. Additionally, Brauer et al. reported dropped rates from 964.2 per 100,000 PYs in 1986 to 793.5 in 2005 among 65+ women, and from 392.4 to 369.0 among 65+ men in the USA [17]. In most cases as we observed, the decrease was more profound among women, which could be hypothesized due to the higher number of women under anti-osteoporosis treatment or who received lifestyle modifications.
There are few studies that have looked at both hip and other MOF. A study in the USA made comparisons after 20 years (1989–1991 and 2009–2011), and the reported decrease in hip fracture rates in both sexes and an increase in vertebral fractures in men were concordant with our results [34]. Another study in Canada (1986–2006) identified a similar result to ours regarding a global decrease in hip fracture rates and a decrease of forearm fractures among women [35].
On the other hand, there are studies whose results are not concordant with our findings. Van der Velde et al. reported an increase of hip fracture rates in men and a steady state for women in the UK [15]; the differences could be due to a different version of ICD used for fracture classification (ICD-9 vs. 10) or a different kind of database (medical record-based Clinical Practice Research Datalink [CPRD]). A Japanese study showed not only substantially lower rates for limb OP fractures, and higher rates of vertebral cases, but also an increasing trend in hip fractures since the 1990s [36]. Two other studies from Japan and Singapore showed similar results with increasing tendencies for hip fracture over the 1990s and 2000s [37, 38]. Interestingly, there was a notable difference between East and West regarding change of rates of hip fracture in the past decades, where the exact reason for these trend discrepancies is not clear [39, 40].
Our study period (i.e., the 1990s and 2000s) was a crucial time span as it saw extensive developments in management of osteoporosis, including bisphosphonates coming to the market, awareness of osteoporosis management grew, and treatment guidelines underwent a number of revisions [41, 42]. Based on the guidelines for osteoporosis treatment in Denmark, the suggested daily intake of calcium for men with osteoporosis is lower than postmenopausal women at risk (800–1000 mg vs. 1000–1200 mg, respectively), but the first line treatment for both sexes is alendronate, and in case of severe disease, anabolic treatment is indicated [43, 44]. Nevertheless, osteoporosis has been traditionally considered a women’s only disease, and it could be hypothesized that a decrease in hip fractures due to preventive medication may be stronger among women than men. Numerous studies have already shown the effectiveness of anti-osteoporotic therapy (including bisphosphonates) on fracture prevention; however, there are studies which reported only a small role of these medication in the reduction of hip fracture rates [24, 45–47]. So, the extent to which anti-osteoporotic therapy may affect rates of OP fractures, or whether it could have a role in the present discrepancies among men and women, requires further investigation.
Beside anti-osteoporotic therapy, there might be other factors which contributed to the mostly declining OP fracture trend in Denmark. An increasing proportion of 50+ individuals was born after the World War II, and grew up under better nutritional states and physical activities (sport classes introduced at schools, etc.), which might help to improve their peak bone mass. Also, the next generations are being guided by physicians on the importance of bone health as we age, and this could end up in positive effects including better use of Ca/Vit D supplements, and more adherence to anti-osteoporotic therapies. These among others resulted in a lower rate of fracture despite an aging population. Still, interventions such as more ubiquitous use of devices that reduce risk of falling in frail and elderly, such as walk aids, could play a role. These hypothesized factors are beyond the scope of this study and need further investigation.
As stated above, the economic burden of OP fractures is substantial and many reports suggest this will increase over the coming years mostly because of an aging population [2, 4–9]. Studies showed that healthcare expenditures associated with an OP fracture in the USA are twice as high compared to patients only affected with osteoporosis and are threefold higher compared to the general population [9]. It has also been shown that the hospital costs of OP fractures were higher compared to similar aging ailments like myocardial infarction, stroke, or breast cancer [5]. From €1.6 billion total costs of OP fractures in Denmark in 2011, just €628 million (40.2%) was spent for men [10]; but based on our results, there was an increase in the total number of fractures in Denmark, the OP fracture rates are not declining among men with the same rate observed in women, and the women to men ratio for MOF rates were noticeably decreased from 2.93 to 2.72 between 1995 and 2010. Considering all these, it could be expected that healthcare expenditures for osteoporosis and OP fractures among men might be a more serious burden in the near future.
This study had many strengths. The database used provided the opportunity of studying all fracture cases reported to hospitals in Denmark in this time period, and it has already proved to be reliable and valid [31]. This is one of the few studies that examined not only hip but all MOF. Again, the duration of study is one of the longest in literature with 16 years of follow-up time. We were also able to stratify IRs by fracture sites. All these resulted in a comprehensive study that could be used for national and international policy-making purposes, including improvements of healthcare services, and better estimation of OP fracture-associated costs.
We had also some limitations in this study. To minimize double counting, we excluded fractures of the same type within 1 year. While this decision was made to improve the likelihood that we would capture new fractures as opposed to follow-up visits, we recognize that this may have resulted in an underestimation of the true fracture rate as we may have excluded some new fractures. In case of clinical vertebral fracture, this underestimation could be even worse, as the evidence suggests the majority of vertebral fractures do not immediately come to clinical attention [48]. On the other hand, there is this possibility that we overestimated the clinical vertebral fractures, because with advancement of spine imaging utilization in recent years, there are more chances to detect old previously unrecognized fractures, and so, some prevalent vertebral fracture might be misclassified as incident fractures. Also, our IRs were not adjusted beyond the factors explained in this article, as we were not able to examine the influence of any further mediating or confounding factor on the observed trends. Similarly, we have limited explanatory information for seemingly anomalous spikes. For example, the only explanation for the spike observed in trends of radius/ulna fracture in the year 2010 (Fig. 2d) was the record-breaking freezing winter happened in Europe in 2010 (potentially resulting in higher number of falls) [49], as no other coding or reporting issue was detected.
In conclusion, we did a series of cross-sectional analyses showing the secular trends of MOF rates in Denmark between 1995 and 2010. The results showed a general decline in MOF rates and a decreasing trend in hip fracture rates for both men and women, which is in line with the study by Driessen et al. in Denmark for the year 2011, and many other studies in Nordic and Western countries. Also, we noticed a lower rate of decrease of hip fracture trends and an increasing trend in rates of vertebral fracture among men, which was accompanied by a reducing women-to-men IRs ratio in the study period. Considering these observations and the major economic burden that accompanies this devastating disease, more attention should be paid to MOF, especially in men.
Compliance with ethical standards
Conflicts of interest
SA, JD, PV, and AMB declare that they have no conflicts of interest.
JB reports grants and personal fees from Eli Lilly, grants and personal fees from Amgen, and personal fees from Sanofi, outside the submitted work.
AB received a grant to her department from the Netherlands Organization for Health Research and Development to investigate a multicomponent adherence intervention in patients with a recent major osteoporotic fracture.
FV currently supervises a PhD student who is also employed with F. Hoffmann la Roche Ltd., Basel Switzerland. He has not received any reimbursements for this, and the student’s research topics are not related to this publication.
Ethical approval
This was not a clinical trial, and ethics committee approval was not required.
References
- 1.Abtahi S, Driessen JHM, Vestergaard P, van den Bergh J, Boonen A, de Vries F, Burden AM (2019) Retraction Note to: Secular trends in major osteoporotic fractures among 50+ adults in Denmark between 1995 and 2010. Archives of Osteoporosis (2019) 14:77 [DOI] [PMC free article] [PubMed]
- 2.Lad SP, Patil CG, Lad EM, Boakye M. Trends in pathological vertebral fractures in the United States: 1993 to 2004. J Neurosurg Spine. 2007;7(3):305–310. doi: 10.3171/SPI-07/09/305. [DOI] [PubMed] [Google Scholar]
- 3.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17(12):1726–1733. doi: 10.1007/s00198-006-0172-4. [DOI] [PubMed] [Google Scholar]
- 4.Briggs AM, Sun W, Miller LJ, Geelhoed E, Huska A, Inderjeeth CA. Hospitalisations, admission costs and re-fracture risk related to osteoporosis in Western Australia are substantial: a 10-year review. Aust N Z J Public Health. 2015;39(6):557–562. doi: 10.1111/1753-6405.12381. [DOI] [PubMed] [Google Scholar]
- 5.Singer A, Exuzides A, Spangler L, O'Malley C, Colby C, Johnston K, Agodoa I, Baker J, Kagan R. Burden of illness for osteoporotic fractures compared with other serious diseases among postmenopausal women in the United States. Mayo Clin Proc. 2015;90(1):53–62. doi: 10.1016/j.mayocp.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 6.Christensen L, Iqbal S, Macarios D, Badamgarav E, Harley C. Cost of fractures commonly associated with osteoporosis in a managed-care population. J Med Econ. 2010;13(2):302–313. doi: 10.3111/13696998.2010.488969. [DOI] [PubMed] [Google Scholar]
- 7.Pike C, Birnbaum HG, Schiller M, Sharma H, Burge R, Edgell ET. Direct and indirect costs of non-vertebral fracture patients with osteoporosis in the US. PharmacoEconomics. 2010;28(5):395–409. doi: 10.2165/11531040-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 8.Sasser AC, Rousculp MD, Birnbaum HG, Oster EF, Lufkin E, Mallet D. Economic burden of osteoporosis, breast cancer, and cardiovascular disease among postmenopausal women in an employed population. Womens Health Issues. 2005;15(3):97–108. doi: 10.1016/j.whi.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 9.Orsini LS, Rousculp MD, Long SR, Wang S. Health care utilization and expenditures in the United States: a study of osteoporosis-related fractures. Osteoporos Int. 2005;16(4):359–371. doi: 10.1007/s00198-004-1694-2. [DOI] [PubMed] [Google Scholar]
- 10.Hansen L, Mathiesen AS, Vestergaard P, Ehlers LH, Petersen KD. A health economic analysis of osteoporotic fractures: who carries the burden? Arch Osteoporos. 2013;8:126. doi: 10.1007/s11657-013-0126-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Compston J. Osteoporosis: social and economic impact. Radiol Clin N Am. 2010;48(3):477–482. doi: 10.1016/j.rcl.2010.02.010. [DOI] [PubMed] [Google Scholar]
- 12.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22(3):465–475. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 13.Si L, Winzenberg TM, Jiang Q, Chen M, Palmer AJ. Projection of osteoporosis-related fractures and costs in China: 2010-2050. Osteoporos Int. 2015;26(7):1929–1937. doi: 10.1007/s00198-015-3093-2. [DOI] [PubMed] [Google Scholar]
- 14.Cooper C, Campion G, Melton LJ. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2(6):285–289. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 15.van der Velde RY, Wyers CE, Curtis EM, Geusens PPMM, van den Bergh JPW, de Vries F, Cooper C, van Staa TP, Harvey NC. Secular trends in fracture incidence in the United Kingdom between 1990 and 2012. Osteoporos Int. 2016;27(11):3197–3206. doi: 10.1007/s00198-016-3650-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leslie WD, O'Donnell S, Jean S, Lagacé C, Walsh P, Bancej C, Morin S, Hanley DA, Papaioannou A, Osteoporosis Surveillance Expert Working Group Trends in hip fracture rates in Canada. JAMA. 2009;302(8):883–889. doi: 10.1001/jama.2009.1231. [DOI] [PubMed] [Google Scholar]
- 17.Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302(14):1573–1579. doi: 10.1001/jama.2009.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dimai HP, Svedbom A, Fahrleitner-Pammer A, Pieber T, Resch H, Zwettler E, Chandran M, Borgstrom F. Epidemiology of hip fractures in Austria: evidence for a change in the secular trend. Osteoporos Int. 2011;22(2):685–692. doi: 10.1007/s00198-010-1271-9. [DOI] [PubMed] [Google Scholar]
- 19.Maravic M, Taupin P, Landais P, Roux C. Change in hip fracture incidence over the last 6 years in France. Osteoporos Int. 2011;22(3):797–801. doi: 10.1007/s00198-010-1255-9. [DOI] [PubMed] [Google Scholar]
- 20.Crisp A, Dixon T, Jones G, Cumming RG, Laslett LL, Bhatia K, Webster A, Ebeling PR. Declining incidence of osteoporotic hip fracture in Australia. Arch Osteoporos. 2012;7:179–185. doi: 10.1007/s11657-012-0095-y. [DOI] [PubMed] [Google Scholar]
- 21.Chen FP, Shyu YC, Fu TS, Sun CC, Chao AS, Tsai TL, Huang TS. Secular trends in incidence and recurrence rates of hip fracture: a nationwide population-based study. Osteoporos Int. 2017;28(3):811–818. doi: 10.1007/s00198-016-3820-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM, Melton LJ, Cummings SR, Kanis JA, IOF CSA Working Group on Fracture Epidemiology Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int. 2011;22(5):1277–1288. doi: 10.1007/s00198-011-1601-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vestergaard P, Rejnmark L, Mosekilde L. Strongly increasing incidence of hip fractures in Denmark from 1977 to 1999. Ugeskr Laeger. 2008;170(8):621–623. [PubMed] [Google Scholar]
- 24.Abrahamsen B, Vestergaard P. Declining incidence of hip fractures and the extent of use of anti-osteoporotic therapy in Denmark 1997-2006. Osteoporos Int. 2010;21(3):373–380. doi: 10.1007/s00198-009-0957-3. [DOI] [PubMed] [Google Scholar]
- 25.Rosengren BE, Björk J, Cooper C, Abrahamsen B. Recent hip fracture trends in Sweden and Denmark with age-period-cohort effects. Osteoporos Int. 2017;28(1):139–149. doi: 10.1007/s00198-016-3768-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Neuburger J, Wakeman R. Is the incidence of hip fracture increasing among older men in England? J Epidemiol Community Health. 2016;70(10):1049–1050. doi: 10.1136/jech-2015-207114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abrahamsen B, Jørgensen NR, Schwarz P. Epidemiology of forearm fractures in adults in Denmark: national age- and gender-specific incidence rates, ratio of forearm to hip fractures, and extent of surgical fracture repair in inpatients and outpatients. Osteoporos Int. 2015;26(1):67–76. doi: 10.1007/s00198-014-2831-1. [DOI] [PubMed] [Google Scholar]
- 28.Driessen JH, Hansen L, Eriksen SA, van Onzenoort HA, Henry RM, van den Bergh J, Abrahamsen B, Vestergaard P, de Vries F. The epidemiology of fractures in Denmark in 2011. Osteoporos Int. 2016;27(6):2017–2025. doi: 10.1007/s00198-016-3488-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.FOLK2: Population 1. January by sex, age, ancestry, country of origin and citizenship (1980–2017). Statistics Denmark, Accessed 23.11.2017, Available from: http://www.statbank.dk/statbank5a/default.asp?w=1366
- 30.Andersen TF, Madsen M, Jørgensen J, Mellemkjoer L, Olsen JH. The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull. 1999;46(3):263–268. [PubMed] [Google Scholar]
- 31.Hundrup YA, Høidrup S, Obel EB, Rasmussen NK. The validity of self-reported fractures among Danish female nurses: comparison with fractures registered in the Danish National Hospital Register. Scand J Public Health. 2004;32(2):136–143. doi: 10.1080/14034940310017490. [DOI] [PubMed] [Google Scholar]
- 32.WHO Scientific Group on the Assessment of Osteoporosis at Primary Health Care Level. Summary meeting report. 5–7 May 2004. Brussels, Belgium: World Health Organization; 2004:9
- 33.FRAX. WHO Fracture risk assessment tool. 2001. Accessed 29.05.2018, Available from: www.shef.ac.uk/FRAX/index.aspx
- 34.Amin S, Achenbach SJ, Atkinson EJ, Khosla S, Melton LJ., 3rd Trends in fracture incidence: a population-based study over 20 years. J Bone Miner Res. 2014;29(3):581–589. doi: 10.1002/jbmr.2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leslie WD, Sadatsafavi M, Lix LM, Azimaee M, Morin S, Metge CJ, Caetano P. Secular decreases in fracture rates 1986-2006 for Manitoba, Canada: a population-based analysis. Osteoporos Int. 2011;22(7):2137–2143. doi: 10.1007/s00198-010-1470-4. [DOI] [PubMed] [Google Scholar]
- 36.Tsukutani Y, Hagino H, Ito Y, Nagashima H. Epidemiology of fragility fractures in Sakaiminato, Japan: incidence, secular trends, and prognosis. Osteoporos Int. 2015;26(9):2249–2255. doi: 10.1007/s00198-015-3124-z. [DOI] [PubMed] [Google Scholar]
- 37.Hagino H, Furukawa K, Fujiwara S, Okano T, Katagiri H, Yamamoto K, Teshima R. Recent trends in the incidence and lifetime risk of hip fracture in Tottori, Japan. Osteoporos Int. 2009;20(4):543–548. doi: 10.1007/s00198-008-0685-0. [DOI] [PubMed] [Google Scholar]
- 38.Koh LK, Saw SM, Lee JJ, Leong KH, Lee J, National Working Committee on Osteoporosis Hip fracture incidence rates in Singapore 1991-1998. Osteoporos Int. 2001;12(4):311–318. doi: 10.1007/s001980170121. [DOI] [PubMed] [Google Scholar]
- 39.Ballane G, Cauley JA, Luckey MM, Gel-H F. Secular trends in hip fractures worldwide: opposing trends East versus West. J Bone Miner Res. 2014;29(8):1745–1755. doi: 10.1002/jbmr.2218. [DOI] [PubMed] [Google Scholar]
- 40.Curtis EM, Moon RJ, Harvey NC, Cooper C. Reprint of: the impact of fragility fracture and approaches to osteoporosis risk assessment worldwide. Int J Orthop Trauma Nurs. 2017;26:7–17. doi: 10.1016/j.ijotn.2017.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kanis JA, Delmas P, Burckhardt P, Cooper C, Torgerson D. Guidelines for diagnosis and management of osteoporosis. The European Foundation for Osteoporosis and Bone Disease. Osteoporos Int. 1997;7(4):390–406. doi: 10.1007/BF01623782. [DOI] [PubMed] [Google Scholar]
- 42.Compston J, Cooper A, Cooper C, Francis R, Kanis JA, Marsh D, McCloskey EV, Reid DM, Selby P, Wilkins M, National Osteoporosis Guideline Group (NOGG) Guidelines for the diagnosis and management of osteoporosis in postmenopausal women and men from the age of 50 years in the UK. Maturitas. 2009;62(2):105–108. doi: 10.1016/j.maturitas.2008.11.022. [DOI] [PubMed] [Google Scholar]
- 43.Danish Endocrine Society (co-endorsed by the Danish Bone Society and the National Board of Health). National Osteoporosis Guidelines: Treatment instructions for osteoporosis in women. NBV. 2016 Oct. Accessed 23.11.2017, Available from: http://www.endocrinology.dk/index.php/3-calcium-og-knoglemetaboliske-sygdomme/3-osteoporose [Danish]
- 44.Danish Endocrine Society (co-endorsed by the Danish Bone Society and the National Board of Health). National Osteoporosis Guidelines: Treatment of male osteoporosis. NBV. 2016 Oct. Accessed 23.11.2017, Available from: http://www.endocrinology.dk/index.php/3-calcium-og-knoglemetaboliske-sygdomme/nbv-endokrinologi-behandling-af-mandlig-osteoporose-sekundaer-osteoporose-mandlig-hypogonadisme-d-vitamin [Danish]
- 45.Sanderson J, Martyn-St James M, Stevens J, Goka E, Wong R, Campbell F, Selby P, Gittoes N, Davis S. Clinical effectiveness of bisphosphonates for the prevention of fragility fractures: a systematic review and network meta-analysis. Bone. 2016;89:52–58. doi: 10.1016/j.bone.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 46.Nguyen ND, Eisman JA, Nguyen TV. Anti-hip fracture efficacy of bisphosphonates: a Bayesian analysis of clinical trials. J Bone Miner Res. 2006;21(2):340–349. doi: 10.1359/JBMR.050903. [DOI] [PubMed] [Google Scholar]
- 47.Vestergaard P, Mosekilde L, Langdahl B. Fracture prevention in postmenopausal women. BMJ Clin Evid. 2011;3:2011. [PMC free article] [PubMed] [Google Scholar]
- 48.Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int. 2005;16(Suppl 2):S3–S7. doi: 10.1007/s00198-004-1702-6. [DOI] [PubMed] [Google Scholar]
- 49.Cattiaux J, Vautard R, Cassou C, Yiou P, Masson-Delmotte V, Codron F. Winter 2010 in Europe: a cold extreme in a warming climate. Geophys Res Lett. 2010;37:L20704. doi: 10.1029/2010GL044613. [DOI] [Google Scholar]