Abstract
The associations among normal personality and many mental disorders are well established, but it remains unclear whether and how symptoms of schizophrenia and schizotypal traits align with the personality taxonomy. This study examined the joint factor structure of normal personality, schizotypy, and schizophrenia symptoms in people with psychotic disorders (n = 288) and never-psychotic adults (n = 257) in the Suffolk County Mental Health Project. First, we evaluated the structure of schizotypal (positive schizotypy, negative schizotypy, and mistrust) and normal traits. In both the psychotic-disorder and never-psychotic groups, the best-fitting model had 5 factors: neuroticism, extraversion, conscientiousness, agreeableness, and psychoticism. The schizotypy traits were placed on different dimensions: negative schizotypy went on (low) extraversion, whereas positive schizotypy and mistrust went on psychoticism. Next, we added symptoms to the model. Numerous alternatives were compared, and the 5-factor model remained best-fitting. Reality distortion (hallucinations and delusions) and disorganization symptoms were placed on psychoticism, and negative symptoms were placed on extraversion. Models that separated symptom dimensions from trait dimensions did not fit well, arguing that taxonomies of symptoms and traits are aligned. This is the first study to show that symptoms of psychosis, schizotypy, and normal personality reflect the same underlying dimensions. Specifically, (low) extraversion, negative schizotypy, and negative symptoms form one spectrum, whereas psychoticism, positive schizotypy, and positive and disorganized symptoms form another. This framework helps to understand the heterogeneity of psychosis and comorbidity patterns found in psychotic disorders. It also underscores the importance of traits to understanding these disorders.
Keywords: psychoticism, mistrust, detachment, positive symptoms, negative symptoms
Introduction
Trait-based paradigms, which have treated psychopathology as fully dimensional, have been useful in understanding psychopathology, particularly internalizing and externalizing disorders.1–3 The Hierarchical Taxonomy of Psychopathology (HiTOP) seeks to improve on traditional diagnostic systems, such as the Diagnostic and Statistical Manual of Mental Disorders (DSM) and International Classification of Diseases (ICD), and conceptualize psychopathology dimensionally.4 A major dimension within HiTOP is the psychotic spectrum, which ranges from normal personality to schizotypal traits to frank psychosis. Schizotypy also reflects a liability for the development of schizophrenia.5–8 The dimensional conceptualization is supported by evidence that psychotic disorders form a continuum with schizotypal traits,9–15 and schizotypal traits fit well in the personality taxonomy alongside normal traits.16,17 An alternative view of schizotypy is that it is quasi-dimensional, and previous work has not definitely resolved this issue.9,13 Some research has demonstrated that psychosis exists on a continuum with normal perceptual experiences whether examined with latent variable mixture models18 or taxometric methods.19,20 This study aims to identify where schizotypy fits within other spectra of psychopathology regardless of whether the underlying construct is dimensional or categorical. Previous research strongly supports that other psychopathology spectra included in HiTOP parallel dimensions of normal personality and extend into maladaptive extremes2,3,21–23 (although some recent research suggests that normal personality characteristics are separate from personality disorders on a genetic level24). Recent theorists have noted that personality pathology is often neglected in schizophrenia research,25 and unlike other spectra, the psychotic spectrum has not been comprehensively studied vis-à-vis the taxonomy of normal personality.
This mapping is especially complicated because psychotic symptoms are multidimensional, with structural studies finding at least 2 factors of positive and negative symptoms.26–28 The positive symptom factor includes reality distortion (delusions and hallucinations) and disorganization (bizarre behavior and formal thought disorder), and the negative symptom factor includes inexpressivity (flat affect and alogia) and avolition (avolition and asociality).29–32
Maladaptive personality traits relevant to psychosis typically are labeled schizotypy and are also multidimensional. This domain includes an array of perspectives including risk factors,5,6,33–36 prodromal signs and symptoms,37–41 maladaptive traits,42–45 and personality disorders.10,46,47 Across perspectives, schizotypy includes at least 2 dimensions, positive (anomalous perceptions and beliefs) and negative (anhedonia and social withdrawal).48,49 These dimensions also have been labeled psychoticism and detachment.4,36 Some studies observed additional factors,50–54 among which the placement of mistrust—sometimes termed suspiciousness or paranoia—has been inconsistent. Models have grouped mistrust with positive schizotypy,51,55,56 negative schizotypy,52,57 antagonism/disagreeableness,58,59 or found a separate factor,53,60–62 including large multinational studies.63
Multiple models have been proposed to organize personality, and the most studied includes 5 traits: neuroticism, extraversion, conscientiousness, agreeableness, and openness.64 Some theorists have hypothesized a link between maladaptive openness and psychoticism/positive schizotypy,65 but observed correlations are weak and often nonsignificant.66–69 Openness is largely unrelated to other forms of psychopathology,23 and neuroticism, extraversion, conscientiousness, and agreeableness have emerged as the normal personality characteristics relevant to mental disorders. Schizotypy does not fit fully into this taxonomy. Detachment typically maps onto low extraversion53,70,71 or forms a distinct dimension.51,55 In contrast, psychoticism/positive schizotypy has been consistently found to form a dimension distinct from normal personality.66–68,72–75
It is less clear how schizophrenia relates to normal personality because few investigations assessed both relatively rare psychotic disorders and normal personality. A meta-analysis of this small literature found that people with schizophrenia have lower extraversion, conscientiousness, and agreeableness, but higher neuroticism compared with healthy controls.76 Limited evidence suggests that schizophrenia correlates with psychoticism more strongly than with other traits.77 This overall profile likely masks rather different trait correlates of schizophrenia symptoms. Negative symptoms have been consistently linked to low extraversion78–81 and negative schizotypy.82 Personality correlates of positive symptoms are uncertain,83 except for a strong link of reality distortion to psychoticism/positive schizotypy.82 Personality links of disorganization are largely unknown.
It remains unclear whether schizophrenia symptoms and schizotypy traits fit within the taxonomy of the normal model or form additional dimensions. This study sought to address this issue by performing the first-factor analysis of all relevant dimensions. First, we examined the joint structure of schizotypy and normal personality traits in psychotic-disorders and never-psychotic samples. We tested alternative models that reflect organizations suggested in the literature. Next, in the psychotic-disorders sample, we added symptoms of schizophrenia, again comparing all organizations suggested in the literature. These analyses were designed to determine whether schizophrenia symptoms, schizotypy, and normal personality fall along the same major spectra, and help to understand heterogeneity within psychotic disorders from the perspective of traits.
Methods
Participants
Data came from the Suffolk County Mental Health Project, a longitudinal epidemiologic study of first-admission patients with psychosis.84–86 The psychotic-disorders group was recruited from 12 psychiatric inpatient units of Suffolk County, NY, between 1989 and 1995. Inclusion criteria were first admission within 6 months, psychosis, ages 15–60, intelligence quotient >70, proficiency with English, resident of Suffolk County, and no apparent medical etiology for psychotic symptoms. Patients were followed over 2 decades, and 288 completed the personality assessment at the 20-year time point. The never-psychotic group (N = 257) was recruited using random digit dialing to zip codes where the psychotic disorder group resided (for sampling procedure see Velthorst et al87). The study was approved annually by the institutional review boards of Stony Brook University and participating hospitals. All participants provided written informed consent. See table 1 for the demographic characteristics of the samples. Socioeconomic status was measured with the Hollingshead Index of Socioeconomic Status.88
Table 1.
Demographic Characteristics and Psychometric Properties
| Psychotic disorders (n = 288) | Never-psychotic (n = 257) | χ2 or t (df) | Cohen’s d | |||||
|---|---|---|---|---|---|---|---|---|
| Age: M (SD) | 48.41 (9.17) | 50.39 (8.94) | 2.56 (255)* | 0.21 | ||||
| Sex: n (% female) | 130 (43.8) | 114 (44.4) | 0.03(1) | — | ||||
| Ethnicity (% Hispanic) | 39 (13.1) | 21 (8.2) | 3.40 (1) | — | ||||
| Race: n (%) | 8.96 (4) | — | ||||||
| White | 232 (78.1) | 224 (87.5) | — | — | ||||
| African American | 35 (11.8) | 16 (6.3) | — | — | ||||
| Asian | 6 (2.0) | 2 (0.8) | — | — | ||||
| Multiracial | 9 (3.0) | 6 (2.3) | — | — | ||||
| Other | 15 (5.1) | 8 (3.1) | — | — | ||||
| Employed: n (%) | 108 (36.7) | 186 (74.4) | 77.18 (1)* | |||||
| Past year GAF: M (SD) | 46.56 (17.34) | 72.75 (12.20) | 20.06 (254)* | 1.81 | ||||
| Marital status: n (%) | 111.96 (4)* | |||||||
| Never married | 132 (44.9) | 19 (7.6) | ||||||
| Married | 90 (30.6) | 176 (70.1) | ||||||
| Divorced | 49 (16.7) | 37 (14.7) | ||||||
| Separated | 15 (5.1) | 11 (4.4) | ||||||
| Widowed | 8 (2.7) | 8 (3.2) | ||||||
| Medication: n (%) | ||||||||
| Antipsychotic | 159 (54.6) | 4 (1.6) | 182.17 (1)* | — | ||||
| Antidepressant | 114 (38.4) | 27 (10.6) | 57.62 (1) * | — | ||||
| Mood stabilizer | 80 (26.9) | 2 (0.8) | 75.66 (1) * | — | ||||
| Diagnosis: n (%) | ||||||||
| Schizophrenia/schizoaffective | 137 (46.1) | — | — | — | ||||
| Bipolar disorder | 79 (26.6) | — | — | — | ||||
| Major depression | 36 (12.1) | — | — | — | ||||
| Substance use disorder | 17 (5.7) | — | — | — | ||||
| Other diagnoses | 28 (9.4) | — | — | — | ||||
| Socioeconomic status | ||||||||
| Large bus owner, major prof, exec | 11 (3.7) | NA | — | — | ||||
| Manager, med bus owner, lesser prof | 42 (14.3) | NA | — | — | ||||
| Admin, small bus owner, minor prof | 51 (17.3) | NA | — | — | ||||
| Clerical, sales technician | 55 (18.7) | |||||||
| Skilled manual | 46 (15.6) | NA | — | — | ||||
| Machine operator, semi-skilled | 43 (14.3) | NA | — | — | ||||
| Unskilled | 19 (14.6) | NA | — | — | ||||
| Not working | 27 (9.2) | NA | — | — | ||||
| Big Five Inventory | M | SD | α | M | SD | α | ||
| Neuroticism | 22.77 | 6.98 | .80 | 18.22 | 6.58 | .84 | 7.696 (529)* | 0.67 |
| Extraversion | 24.62 | 6.43 | .76 | 27.78 | 6.28 | .81 | –5.688 (523)* | 0.50 |
| Agreeableness | 36.48 | 5.87 | .75 | 38.66 | 5.08 | .76 | –4.555 (532)* | 0.40 |
| Conscientiousness | 33.61 | 6.77 | .78 | 37.56 | 5.56 | .78 | –7.207 (515)* | 0.64 |
| Schedule for Nonadaptive and Adaptive Personality | ||||||||
| Mistrust | 6.33 | 5.10 | .89 | 2.71 | 3.41 | .89 | 9.366 (512)* | 0.83 |
| Detachment | 6.54 | 4.24 | .83 | 3.85 | 3.61 | .84 | 7.748 (519)* | 0.68 |
| Eccentric perceptions | 2.97 | 3.37 | .85 | 1.36 | 1.69 | .63 | 6.821 (523)* | 0.60 |
| Scale for the Assessment of Positive/Negative Symptoms | ||||||||
| Inexpressivity | 7.52 | 9.54 | .90 | 0.94 | 2.80 | .83 | 10.561 (491)* | 0.94 |
| Avolition | 13.29 | 9.67 | .87 | 2.90 | 3.82 | .69 | 16.125 (547)* | 1.41 |
| Reality distortion | 4.10 | 7.31 | .84 | NA | ||||
| Disorganized | 4.53 | 6.43 | .77 | NA | ||||
Note: GAF, global assessment of functioning.
*P < .05.
Four participants in the never-psychotic group were excluded due to excessive missing data. Demographic information was available for 373 participants in the psychotic-disorders group at 20-year wave, 85 of whom did not provide information necessary for present analyses and were excluded. These participants did not significantly differ from the 288 included participants on age, gender, race/ethnicity, employment status, or socioeconomic status. However, the included group was more likely to have a diagnosis of schizoaffective and bipolar disorders, and less likely to have a diagnosis of drug abuse or other miscellaneous disorder. A plurality of both groups carried a diagnosis of schizophrenia. Among participants for whom some data were available, all data were missing completely at random. In all analyses, missing data were excluded pairwise.
Measures
Normal Personality traits were measured with the Conscientious, Extraversion, Agreeableness, and Neuroticism scales of the Big Five Inventory (BFI).89 The BFI is a 44-item instrument in which participants indicate how much they agree with statements on a scale from 1 (Disagree Strongly) to 5 (Agree Strongly). The BFI is the most commonly used measure of general personality, has high correlations with other measures of big 5 personalities in both psychotic and general population samples, and represents the 5 dimensions well in factor analyses.73,90 Cronbach’s alphas for all scales were >.70 in both samples (table 1).
Schizotypy was measured with the Eccentric Perceptions, Detachment, and Mistrust scales of the Schedule for Nonadaptive and Adaptive Personality (SNAP).91 The SNAP is a 375-item true/false questionnaire. The SNAP is widely used in general population samples and has impressive evidence of reliability and validity.91 Specifically, the Eccentric Perceptions scale measures odd or unusual beliefs, cognitions, and perceptual experiences and is strongly correlated with measures of psychoticism in general population samples including the Magical Ideation Scale, Perceptual Aberration Scale, Schizotypal Traits Scale-Magical Ideation Subscale, and a schizotypal personality questionnaire (SPQ)-derived unusual beliefs and experience scale (rs = .69–.73)92 and interview ratings of schizotypal personality disorder.91 The Detachment scale measures interpersonal and emotional distance and shows excellent convergence with and the Revised Social Anhedonia Scale (r = .77) and a SPQ-derived social anhedonia measure (r = .75) in a general population sample92 and interview measures of schizoid, schizotypal, and avoidant personality disorders.93 The Mistrust scale measures suspiciousness, alienation, and feelings of injustice. It is highly correlated with interview ratings of both schizotypal and paranoid personality disorder94 and other measures of mistrust including the Schizotypy Traits Scale-Paranoia Subscale (r = .80) and SPQ-Suspiciousness (r = .73) in a general population sample.92
Psychosis Symptoms were measured with the Scale for the Assessment of Positive Symptoms (SAPS)27 and the Scale for the Assessment of Negative Symptoms (SANS).95 The SAPS consists of 31 items covering 4 symptom domains and global ratings. The SANS consists of 19 items assessing 5 domains and global ratings. For both scales, symptoms are rated on a scale from 0 (None) to 5 (Severe). Previous factor analyses examined the SAPS and SANS symptom ratings and concluded that 4 dimensions are most informative: Reality Distortion, Disorganization, Inexpressivity, and Apathy/Avolition,29 consistent with numerous previous studies.30–32,96,97 The inter-rater reliability of these ratings was high for inexpressivity (intraclass correlation coefficient [ICC] = 0.79), Apathy/Avolition (ICC = 0.94), Reality Distortion (ICC = 0.95), and Disorganization (ICC = 0.85).29
Data Analyses
We used confirmatory factor analysis (CFA) to test models of traits and symptoms. We compared these models using Bayesian Information Criterion (BIC) and Akaike Information Criterion (AIC), of which BIC was primary as recommended (lower scores represent better fit).98,99 Root Mean Squared Error of Approximation (RMSEA), Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), and Standardized Root Mean Squared Residual (SRMR) were used to evaluate absolute model fit. Following conventional criteria, RMSEA and SRMR values < .10 were considered acceptable and < .05 were excellent. CFI and TLI values > .90 were acceptable and > .95 were excellent.100–102 All models were fit with Mplus, version 7.31103 using maximum likelihood estimation with robust standard errors estimation, a maximum likelihood estimator with standard errors that are robust to violations of the normality assumption.
Given the measures available, modeling of latent factors required creation of parcels from each scale.104 The individual items in the scales could not be used because it would have required estimating too many parameters in relation to sample size. We created 2 random parcels for each scale (ie, odd items comprising parcel 1, even items comprising parcel 2). We tested the unidimensionality assumption of parceling by conducting an exploratory factor analysis for each scale, and comparing the eigenvalues of the 1- through 4-factor solutions using a scree plot (see supplementary tables S1A and S1B). In the never-psychotic group, the slope of the scree plots suggested a unidimensional solution for all BFI and SNAP scales, with the potential exception of Conscientiousness. In the psychotic-disorders group, the slope of the scree plots for all scales suggested a single factor in each. We concluded that the random parceling approach was appropriate, given evidence for the unidimensionality in 6 of the 7 scales across both samples. Although there was evidence for multidimensionality for one scale, this finding did not replicate across samples and is inconsistent with the scale having been developed to measure a unidimensional construct.89
The first goal was to determine where schizotypy traits (ie, Detachment, Mistrust, and Eccentric Perceptions) fit within the personality taxonomy. We estimated a series of models that tested hypothesized arrangements of these traits separately in both samples. After the best-fitting model was identified, we examined measurement invariance between groups. First, a configural model was tested in which the pattern of the factor loadings matrix (free or fixed to 0) is constrained to equality between groups, but the magnitude of factor loadings and intercepts were allowed to vary between groups. Second, a metric model was tested in which the pattern and magnitude of factor loadings were constrained to be equal between groups, but the intercepts were allowed to vary. Finally, a scalar invariance model was tested in which the pattern and magnitude of factor loadings and intercepts were constrained to be equal between groups.105 Given the well-known limitations of chi-square difference testing for measurement invariance,106 we used change in CFI (ΔCFI),107 McDonald’s Noncentrality Index (Mc),108 and lower BIC109,110 to compare model fit. As recommended, we used 0.010 and 0.020 as the cutoffs for ΔCFI and Mc, respectively.106
The second goal was to test the joint factor structure of personality, schizotypy, and schizophrenia symptoms. We retained the best-fitting model from the personality and schizotypy analyses for the psychotic-disorders sample and added the SAPS and SANS parcels (the never-psychotic group was excluded because, by definition, they did not have sufficient variability in SAPS and SANS ratings). For all analyses, parcels from a given scale were assigned to factor together. Correlations between pairs of parcels can be inflated due to common source, and we modeled that by correlating the corresponding error terms in all analyses including measurement invariance.
Results
Descriptive Statistics
Compared with the never-psychotic group, the psychotic-disorders group was moderately elevated on Neuroticism, and low on Extraversion, Agreeableness, and Conscientiousness (table 1). The Eccentric Perceptions and Detachment scales were moderately elevated, and the mistrust scale was highly elevated.
Structure of Personality and Schizotypy
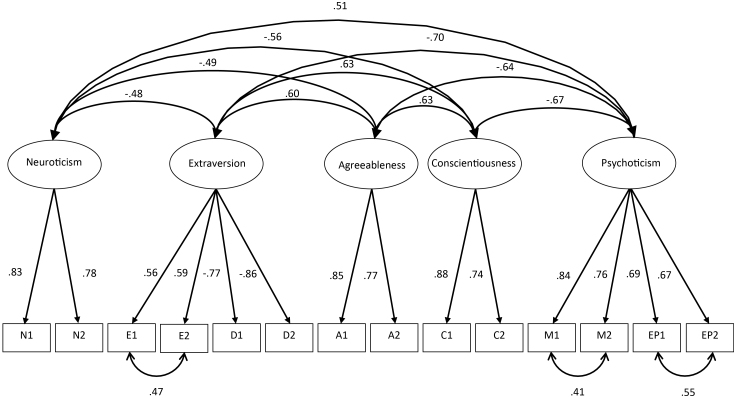
Next, we examined associations among personality and schizotypy variables in both the psychotic-disorder and never-psychotic samples (supplementary table S2A). We compared 5 models representing different arrangements of schizotypy and normal traits (table 2). The model that showed the best fit on BIC consisted of psychoticism (Eccentric Perceptions and Mistrust), extraversion (Extraversion and low Detachment), neuroticism, conscientiousness, and agreeableness factors. This model had the lowest BIC in both samples and fit well according to the RMSEA, CFI, TLI, and SRMR. The AIC showed the best fit for Model 3, which placed Mistrust on both the Psychoticism and Agreeableness factors, but only in the never-psychotic sample. Overall, Model 1 fit best on AIC in psychotic-disorders sample, fit best on the primary index (BIC) in both samples, and is the most parsimonious (figure 1).
Table 2.
Fit Statistics for Models of Personality and Schizotypy
| Model | Para | BIC | AIC | χ2 (df) | RMSEA (90% CI) | CFI | TLI | SRMR |
|---|---|---|---|---|---|---|---|---|
| Never-psychotic group | ||||||||
| 1) Mistrust on psychoticism | 55 | 14 443.91 | 14 284.71 | 124.973 (64) | 0.061 (0.045–0.077) | 0.959 | 0.942 | 0.046 |
| 2) Detachment on psychoticism | 54 | 14 485.60 | 14 293.95 | 164.972 (65) | 0.077 (0.063–0.092) | 0.933 | 0.901 | 0.071 |
| 3) Mistrust on agreeableness | 56 | 14 444.11 | 14 245.36 | 120.468 (63) | 0.060 (0.043–0.076) | 0.962 | 0.945 | 0.045 |
| 4) Mistrust on neuroticism | 56 | 14 449.55 | 14 250.80 | 125.942 (63) | 0.062 (0.046–0.078) | 0.958 | 0.939 | 0.046 |
| 5) Mistrust separate factor | 58 | 14 456.69 | 14 250.84 | 122.070 (61) | 0.062 (0.046–0.078) | 0.959 | 0.939 | 0.043 |
| Psychotic-disorders droup | ||||||||
| 1) Mistrust on psychoticism | 55 | 17 803.74 | 17 602.27 | 213.726 (64) | 0.090 (0.077–0.104) | 0.919 | 0.885 | 0.055 |
| 2) Detachment on psychoticism | 55 | 17 850.10 | 17 652.30 | 265.008 (65) | 0.103 (0.091 -0.116) | 0.892 | 0.849 | 0.071 |
| 3) Mistrust on agreeableness | 56 | 17 815.68 | 17 610.55 | 221.116 (63) | 0.093 (0.080–0.107) | 0.915 | 0.877 | 0.057 |
| 4) Mistrust on neuroticism | 56 | 17 813.08 | 17 607.95 | 217.777 (63) | 0.092 (0.079–0.106) | 0.917 | 0.879 | 0.055 |
| 5) Mistrust separate factor | 58 | 17 816.44 | 17 603.99 | 210.923 (61) | 0.092 (0.079–0.106) | 0.919 | 0.879 | 0.055 |
Note: Para = number of parameters, in all models, BFI Neuroticism loads on Neuroticism, BFI-Extraversion loads on Extraversion, BFI-Conscientiousness Loads on Conscientiousness, BFI- Agreeableness Loads on Agreeableness, and SNAP Eccentric Perceptions loads on Psychoticism. 1) Mistrust on Psychoticism: SNAP Mistrust loads Psychoticism, SNAP Detachment loads on Extraversion; 2) Detachment on Psychoticism: SNAP Mistrust loads Psychoticism, SNAP Detachment crossloads on Extraversion and Psychoticism; 3) Mistrust on Agreeableness: SNAP Mistrust crossloads on Psychoticism and Agreeableness, SNAP Detachment loads on Extraversion.; 4) Mistrust on Neuroticism: SNAP Mistrusts crossloads on Psychoticism and Neuroticism, Detachment loads on Extraversion; 5) Mistrust Separate Factor: SNAP Mistrust forms separate sixth factor, Detachment loads on Extraversion. Best-fitting model is in bold. BIC, Bayesian Information Criterion; AIC, Akaike Information Criterion; RMSEA, Root Mean Squared Error of Approximation; CFI, Comparative Fit Index; TLI, Tucker-Lewis Index; BFI, Big Five Inventory; SNAP, Schedule for Nonadaptive and Adaptive Personality.
Fig. 1.
Joint confirmatory factor analysis of normal personality and schizotypy in the psychotic-disorders group. Note: N = Big Five Inventory (BFI) Neuroticism, E = BFI Extraversion, A = BFI Agreeableness, C = BFI Conscientiousness, D = Schedule for Nonadaptive and Adaptive Personality (SNAP) Detachment Subscale, M = SNAP Mistrust Subscale, EP = SNAP Eccentric Perceptions, numbers on straight lines represent standardized factor loadings, numbers on curved lines represent correlation coefficients between latent variables and residuals for manifest variables.
Measurement Invariance
As can be seen in supplementary table S3, the configural model fit the data well. The metric invariance model fit the data as well as the configural model according to ΔCFI and better according to BIC, but worse according to Mc. Because 2 of the 3 indicators suggest metric invariance, the factor structure is deemed to be invariant. Finally, the scalar invariance model fit as well as the metric model according to all 3 indices. This suggests that the indicators measure the same constructs, measure them equally well between groups, and differences in scores represent meaningful differences in trait severity, consistent with the literature on elevations of personality traits in psychosis.
Structure of Personality, Schizotypy, and Schizophrenia Symptoms
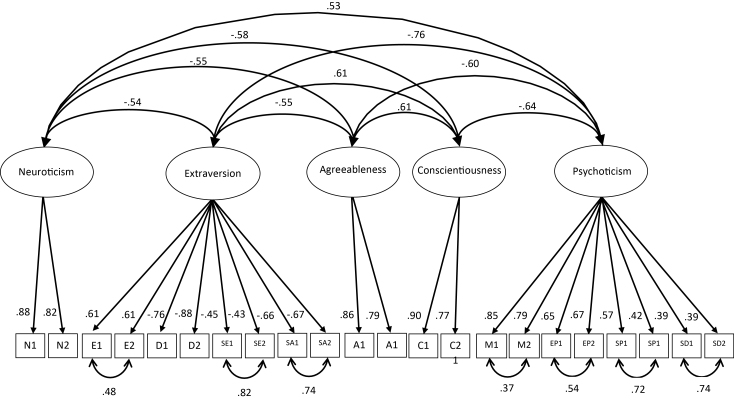
We then investigated the alignment of psychosis symptoms and personality traits (supplementary table S2B). We compared 5 competing models, all of which retained the structure from previous analyses and added symptoms in several arrangements (table 3). The model that fit best on BIC had only 5 dimensions, placing Reality Distortion and Disorganization on the Psychoticism factor, and Inexpressivity and Avolition on the (low)Extraversion/Detachment factor. Absolute indices indicated adequate fit. Additional factors for negative symptoms worsened model fit, suggesting that negative symptoms belong on the same dimension as extraversion and detachment. The AIC favored Model 3, in which Reality Distortion and Disorganized scales formed a separate, sixth factor. However, this positive symptoms factor correlated very highly with psychoticism factor (r = .78), suggesting little distinction between the 2 dimensions. Because the 5-factor model had the lowest BIC, was most parsimonious, and psychoticism and positive symptoms were so strongly correlated, we determined the 5-factor model fit the data best (figure 2).
Table 3.
Fit Statistics for Models of Personality, Schizotypy, and Psychosis Symptoms
| Model | Para | BIC | AIC | χ2 (df) | RMSEA (90% CI) | CFI | TLI | SRMR |
|---|---|---|---|---|---|---|---|---|
| 1) 5-Factor | 83 | 29 248.96 | 28 942.38 | 499.435 (192) | 0.073 (0.066–0.081) | 0.907 | 0.888 | 0.079 |
| 2) SANS on psychoticism | 86 | 29 266.08 | 28 948.42 | 501.192 (189) | 0.075 (0.067–0.083) | 0.905 | 0.884 | 0.078 |
| 3) 6-Factor positive | 88 | 29 250.89 | 28 925.84 | 478.805 (187) | 0.072 (0.064–0.081 | 0.912 | 0.891 | 0.073 |
| 4) 6-Factor negative | 87 | 29 274.24 | 28 952.89 | 502.395 (188) | 0.075 (0.067–0.083) | 0.905 | 0.883 | 0.097 |
| 5) 7-Factor | 93 | 29 278.37 | 28 934.86 | 479.155 (182) | 0.074 (0.066–0.082) | 0.910 | 0.886 | 0.089 |
Note: In all models, BFI Neuroticism loads on Neuroticism, BFI-Extraversion and SNAP Detachment load on Extraversion, BFI-Conscientiousness loads on Conscientiousness, BFI-Agreeableness loads on Agreeableness, and SNAP Eccentric Perceptions and SNAP Mistrust load on Psychoticism. 1) 5-Factor: SAPS Reality Distortion and SAPS Disorganized load on Psychoticism, SANS Inexpressivity and SANS Avolition load on Extraversion. 2) SANS on Psychoticism: SANS Avolition and Inexpressivity crossload on Psychoticism and Extraversion. SAPS Reality Distortion and Disorganized load on Psychoticism; 3) 6-Factor Positive: SANS Avolition and Inexpressivity load on Extraversion, SAPS Reality Distortion and Disorganized form separate sixth factor; 4) 6-Factor Negative: SAPS Reality Distortion and Disorganized load on Psychoticism, SANS Avolition and Inexpressivity form separate sixth factor; 5) 7-Factor: SAPS Reality Distortion and Disorganized for separate sixth factor, SANS Avolition and Inexpressivity form separate seventh factor. The best-fitting model is in bold. BIC, Bayesian Information Criterion; AIC, Akaike Information Criterion; RMSEA, Root Mean Squared Error of Approximation; CFI, Comparative Fit Index; TLI, Tucker-Lewis Index; BFI, Big Five Inventory; SNAP, Schedule for Nonadaptive and Adaptive Personality.
Fig. 2.
Joint confirmatory factor analysis of normal personality, schizotypy, and psychotic symptoms in the psychotic-disorders group. Note: N = Big Five Inventory (BFI) Neuroticism, E = BFI Extraversion, A = BFI Agreeableness, C = BFI Conscientiousness, D = Schedule for Nonadaptive and Adaptive Personality (SNAP) Detachment Subscale, M = SNAP Mistrust Subscale, EP = SNAP Eccentric Perceptions, SA = Scale for the Assessment of Negative Symptoms (SANS) Avolition factor, SE = SANS, Inexpressivity factor, SP = Scale for the Assessment of Positive Symptoms (SAPS), Reality Distortion factor, SD = SAPS, Disorganized factor, numbers on straight lines represent standardized factor loadings, numbers on curved lines represent correlation coefficients between latent variables and between residuals for manifest variables.
Discussion
These findings contribute to our understanding of the taxonomy of symptoms and traits associated with psychosis in several ways. First, we observed that psychoticism/positive schizotypy forms a dimension distinct from normal personality, whereas detachment/negative schizotypy is inseparable from (low) extraversion. Mistrust joined psychoticism rather than aligning with normal personality dimensions or defining a separate factor. This factor structure was invariant between groups. Second, schizophrenia symptoms fit into this structure fully and did not require additional dimensions. Positive symptoms and psychoticism formed one spectrum, whereas negative symptoms and detachment formed another. Overall, these results suggest that normal personality, schizotypy, and psychotic disorder symptoms are intertwined, and research on psychosis should consider traits as well as symptoms.
Our finding that psychoticism/positive schizotypy and positive symptoms form a coherent spectrum is consistent with previous research documenting links between them.111 It is further reinforced by prospective evidence that psychoticism predicts first onset of psychosis in general population34,112 and prodromal samples.113,114 Psychosis and psychoticism are influenced by some of the same genetic vulnerabilities115–117 and environmental factors, such as cannabis exposure, stress or trauma, and urbanicity.12,118 They also exhibit similar brain abnormalities and cognitive and social-cognitive deficits.119–121 Although the 5-factor model fit the data best according to BIC, the difference between model fit was small and may not represent a substantial difference in fit. Thus, an alternative explanation may be that positive symptoms of psychosis represent a separate factor from psychoticism. However, this model is less parsimonious, and the positive symptom factor is very strongly correlated with psychoticism (r = .78), suggesting a lack of a meaningful distinction.
Our observation that a single spectrum spans from (low)extraversion to detachment/negative schizotypy to negative symptoms is consistent with several lines of evidence. Previous research documented a strong link between detachment and (low)extraversion.44,53,70–72,122 Detachment is highly correlated with negative symptoms,37,123–126 predicts the first onset of psychosis,5,112,127–129 shares a genetic liability with schizophrenia,130,131 and is associated with similar social-cognitive deficits,132 deficits in reward processing,133–135 neurofunctional abnormalities,136,137 and cognitive deficits among others.138,139 In contrast, some evidence from previous research suggests that some aspects of negative schizotypy and negative symptoms in schizophrenia are categorical.32,140–142 One potential explanation is that low extraversion, negative schizotypy, and negative symptoms are underpinned by a dimension of risk from which dimensional traits and categorical entities emerge.
This study also sheds light on the relations between mistrust and other traits. Our analyses placed mistrust to the psychoticism factor, suggesting it is more closely related to psychoticism than to other traits. Previous work on the placement of mistrust has produced inconsistent results.2,51–53,58,59,143–145 This finding is consistent with the traditional view of paranoia and persecutory delusions as positive symptoms and with substantial evidence indicating that paranoia is on a continuum with subclinical suspicious thoughts and pathological mistrust in personality disorders.51,143,146,147 A case could also be made that Mistrust belongs on both psychoticism and agreeableness in the never-psychotic group. The model in which mistrust crossloaded on psychoticism and agreeableness fit well than the model with mistrust only on psychoticism according to AIC, and the differences in BIC were small. However, the mistrust on psychoticism model clearly fit better in the psychotic-disorders group, and the measurement invariance analyses suggest the factor structure is statistically equivalent between groups.
This study is the first to investigate the joint taxonomy of symptoms and traits related to psychosis, but it had several limitations. Although measured with well-validated instruments, only one measure of each construct was included. This necessitated the construction of parcels for CFA. There is a lack of consensus in the literature about whether the parceling approach is appropriate for CFA.104,148,149 Some research suggests that item parceling may lead to incorrect decisions regarding the number of factors, distort relations among factors when items crossload on multiple factors, artificially inflate fit statistics, and may be especially problematic when testing measurement invariance.149 Future research could avoid this issue by including multiple measures of each construct.
Another limitation is that this study cannot comment on relations between openness and psychosis. This question was outside the scope of the present investigation. Prior research established that openness is largely unrelated to psychopathology,23,66,68 and we chose not to assess it. Moreover, cases had onset of psychosis more than 2 decades ago. Many continued to experience symptoms, but it is possible that symptom-trait associations might be different early in the illness course, and the joint taxonomy should be investigated in recent-onset samples. Work with the Positive and Negative Symptom Scale suggests a five-factor structure including positive, negative, disorganized, emotional distress, and excitement/agitation. We chose to focus on schizophrenia symptoms because mood symptoms (i.e., emotional distress and excitement/agitation) are already characterized in dimensional taxonomies and have been assigned to the internalizing spectrum.4 The current study also lacked a cross-validation sample, which could add certainty to the stability of the results.
The current research used the eccentric perceptions, mistrust, and detachment scales of the SNAP as measures of schizotypy. There is somewhat limited evidence from previous research about the validity of SNAP scores as measures of schizotypy, particularly in samples of people with schizophrenia. Although several studies have found that SNAP scores are associated schizotypy measures, the majority are non-peer reviewed publications in the form of assessment manuals and unpublished dissertations.43,91–93 Thus, the current results may not generalize to other measures of schizotypy. At the same time, the finding of the CFAs and the significant zero-order correlations among SNAP, BFI, and SAPS/SANS scores provide some evidence of the validity of SNAP scores in people with psychosis. Finally, we could not consider symptom-trait associations in the never-psychotic group because it lacked variance in positive symptoms by design.
Conclusions
These results clarify the common structure of personality, schizotypy, and schizophrenia symptoms. We found that these disorders harbor 2 fundamental spectra: psychoticism dimension defined by mistrust, positive schizotypy, and positive symptoms and detachment dimension spanning (low)extraversion, negative schizotypy, and negative symptoms. The resulting 2-spectra model helps to conceptualize heterogeneity within psychotic disorders and interpret their comorbidities. Also, neuroticism has long been established as the core of internalizing disorders, whereas (low)conscientiousness and (low)agreeableness underpin externalizing disorders. These findings highlight that traits are important in psychotic disorder as well and even brief personality assessments would substantially benefit researchers and clinicians.
Funding
National Institutes of Health (MH44801 to Evelyn Bromet and MH110434 to Roman Kotov).
Supplementary Material
Acknowledgments
The authors are indebted to efforts of study coordinators, interviewers, and psychiatrists. Special thanks to Evelyn Bromet and Laura Fochtmann for comments on the manuscript.
References
- 1. Røysamb E, Kendler KS, Tambs K, et al. The joint structure of DSM-IV Axis I and Axis II disorders. J Abnorm Psychol. 2011;120:198–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kotov R, Ruggero CJ, Krueger RF, Watson D, Yuan Q, Zimmerman M. New dimensions in the quantitative classification of mental illness. Arch Gen Psychiatry. 2011;68:1003–1011. [DOI] [PubMed] [Google Scholar]
- 3. Wright AG, Simms LJ. A metastructural model of mental disorders and pathological personality traits. Psychol Med. 2015;45:2309–2319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kotov R, Krueger RF, Watson D, et al. The Hierarchical Taxonomy of Psychopathology (HiTOP): a dimensional alternative to traditional nosologies. J Abnorm Psychol. 2017;126:454–477. [DOI] [PubMed] [Google Scholar]
- 5. Kwapil TR. Social anhedonia as a predictor of the development of schizophrenia-spectrum disorders. J Abnorm Psychol. 1998;107:558–565. [DOI] [PubMed] [Google Scholar]
- 6. Kwapil TR, Miller MB, Zinser MC, Chapman J, Chapman LJ. Magical ideation and social anhedonia as predictors of psychosis proneness: a partial replication. J Abnorm Psychol. 1997;106:491–495. [DOI] [PubMed] [Google Scholar]
- 7. Meehl PE. Schizotaxia, schizotypy, and schizophrenia. Am Psychol. 1962;17:827–838. [Google Scholar]
- 8. Lenzenweger MF. Psychometric high-risk paradigm, perceptual aberrations, and schizotypy: an update. Schizophr Bull. 1994;20:121–135. [DOI] [PubMed] [Google Scholar]
- 9. Claridge G, Beech T. Fully and quasi-dimensional constructions of schizotypy. In: Raine A, Lencz T, Mednick SA, eds., Schizotypal Personality. New York, NY: Cambridge University Press; 1995:192–216. [Google Scholar]
- 10. Kendler KS, McGuire M, Gruenberg AM, O’Hare A, Spellman M, Walsh D. The Roscommon Family Study. III. Schizophrenia-related personality disorders in relatives. Arch Gen Psychiatry. 1993;50:781–788. [DOI] [PubMed] [Google Scholar]
- 11. Linscott RJ, van Os J. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med. 2013;43:1133–1149. [DOI] [PubMed] [Google Scholar]
- 12. van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39:179–195. [DOI] [PubMed] [Google Scholar]
- 13. Linscott RJ, van Os J. Systematic reviews of categorical versus continuum models in psychosis: evidence for discontinuous subpopulations underlying a psychometric continuum. Implications for DSM-V, DSM-VI, and DSM-VII. Annu Rev Clin Psychol. 2010;6:391–419. [DOI] [PubMed] [Google Scholar]
- 14. van Os J, Reininghaus U. Psychosis as a transdiagnostic and extended phenotype in the general population. World Psychiatry. 2016;15:118–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nelson MT, Seal ML, Pantelis C, Phillips LJ. Evidence of a dimensional relationship between schizotypy and schizophrenia: a systematic review. Neurosci Biobehav Rev. 2013;37:317–327. [DOI] [PubMed] [Google Scholar]
- 16. Tackett JL, Silberschmidt AL, Krueger RF, Sponheim SR. A dimensional model of personality disorder: incorporating DSM Cluster A characteristics. J Abnorm Psychol. 2008;117:454–459. [DOI] [PubMed] [Google Scholar]
- 17. Watson D, Stasik SM, Ro E, Clark LA. Integrating normal and pathological personality: relating the DSM-5 trait-dimensional model to general traits of personality. Assessment. 2013;20:312–326. [DOI] [PubMed] [Google Scholar]
- 18. Miettunen J, Nordström T, Kaakinen M, Ahmed AO. Latent variable mixture modeling in psychiatric research–a review and application. Psychol Med. 2016;46:457–467. [DOI] [PubMed] [Google Scholar]
- 19. Subramaniam M, Abdin E, Vaingankar JA, Verma S, Chong SA. Latent structure of psychosis in the general population: results from the Singapore mental health study. Psychol Med. 2014;44:51–60. [DOI] [PubMed] [Google Scholar]
- 20. Ahmed AO, Buckley PF, Mabe PA. Latent structure of psychotic experiences in the general population. Acta Psychiatr Scand. 2012;125:54–65. [DOI] [PubMed] [Google Scholar]
- 21. Rubio DM, Berg-Weger M, Tebb SS. Using structural equation modeling to test for multidimensionality. Struct Eq Model. 2001;8:613–626. [Google Scholar]
- 22. Hopwood CJ, Malone JC, Ansell EB, et al. Personality assessment in DSM-5: empirical support for rating severity, style, and traits. J Pers Disord. 2011;25:305–320. [DOI] [PubMed] [Google Scholar]
- 23. Kotov R, Gamez W, Schmidt F, Watson D. Linking “big” personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychol Bull. 2010;136:768–821. [DOI] [PubMed] [Google Scholar]
- 24. Czajkowski N, Aggen SH, Krueger RF, et al. A twin study of normative personality and DSM-IV personality disorder criterion counts: evidence for separate genetic influences. Am J Psychiatry. 2018;175:649–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Simonsen E, Newton-Howes G. Personality pathology and schizophrenia. Schizophr Bull. 2018:sby053–sby053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Crow TJ. Molecular pathology of schizophrenia: more than one disease process? Br Med J. 1980;280:66–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Andreasen NC. Scale for the Asssessment of Positive Symptoms. Iowa City: University of Iowa, Department of Psychiatry; 1982. [Google Scholar]
- 28. Andreasen NC, Olsen S. Negative v positive schizophrenia. Definition and validation. Arch Gen Psychiatry. 1982;39:789–794. [DOI] [PubMed] [Google Scholar]
- 29. Kotov R, Foti D, Li K, Bromet EJ, Hajcak G, Ruggero CJ. Validating dimensions of psychosis symptomatology: neural correlates and 20-year outcomes. J Abnorm Psychol. 2016;125:1103–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kring AM, Gur RE, Blanchard JJ, Horan WP, Reise SP. The Clinical Assessment Interview for Negative Symptoms (CAINS): final development and validation. Am J Psychiatry. 2013;170:165–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Strauss GP, Hong LE, Gold JM, et al. Factor structure of the Brief Negative Symptom Scale. Schizophr Res. 2012;142:96–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Blanchard JJ, Cohen AS. The structure of negative symptoms within schizophrenia: implications for assessment. Schizophr Bull. 2006;32:238–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chapman LJ, Chapman JP. Scales for rating psychotic and psychotic-like experiences as continua. Schizophr Bull. 1980;6:477–489. [PubMed] [Google Scholar]
- 34. Chapman LJ, Chapman JP, Kwapil TR, Eckblad M, Zinser MC. Putatively psychosis-prone subjects 10 years later. J Abnorm Psychol. 1994;103:171–183. [DOI] [PubMed] [Google Scholar]
- 35. Chapman LJ, Chapman JP, Raulin ML. Scales for physical and social anhedonia. J Abnorm Psychol. 1976;85:374–382. [DOI] [PubMed] [Google Scholar]
- 36. Barrantes-Vidal N, Grant P, Kwapil TR. The role of schizotypy in the study of the etiology of schizophrenia spectrum disorders. Schizophr Bull. 2015;41 (suppl 2):S408–S416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Barrantes-Vidal N, Gross GM, Sheinbaum T, Mitjavila M, Ballespí S, Kwapil TR. Positive and negative schizotypy are associated with prodromal and schizophrenia-spectrum symptoms. Schizophr Res. 2013;145:50–55. [DOI] [PubMed] [Google Scholar]
- 38. Cicero DC, Martin EA, Becker TM, Docherty AR, Kerns JG. Correspondence between psychometric and clinical high risk for psychosis in an undergraduate population. Psychol Assess. 2014;26:901–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Flückiger R, Ruhrmann S, Debbané M, et al. Psychosis-predictive value of self-reported schizotypy in a clinical high-risk sample. J Abnorm Psychol. 2016;125:923–932. [DOI] [PubMed] [Google Scholar]
- 40. Bedwell JS, Donnelly RS. Schizotypal personality disorder or prodromal symptoms of schizophrenia? Schizophr Res. 2005;80:263–269. [DOI] [PubMed] [Google Scholar]
- 41. Miller TJ, McGlashan TH, Rosen JL, et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull. 2003;29:703–715. [DOI] [PubMed] [Google Scholar]
- 42. Livesley W, Jackson D.. Manual for the Dimensional Assessment of Personality Pathology—Basic Questionnaire. Port Huron, MI: Sigma; 2009. [Google Scholar]
- 43. Clark LA. Schedule for Nonadaptive and Adaptive Personality—Second edition (SNAP-2). 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Krueger RF, Derringer J, Markon KE, Watson D, Skodol AE. Initial construction of a maladaptive personality trait model and inventory for DSM-5. Psychol Med. 2012;42:1879–1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Harkness AR, McNulty JL, Ben-Porath YS. The personality psychopathology five (PSY-5): constructs and MMPI-2 scales. Psychol Assess. 1995;7(1):104. [Google Scholar]
- 46. Torgersen S. Relationship of schizotypal personality disorder to schizophrenia: genetics. Schizophr Bull. 1985;11:554–563. [DOI] [PubMed] [Google Scholar]
- 47. Kendler KS, Gruenberg AM, Strauss JS. An independent analysis of the Copenhagen sample of the Danish adoption study of schizophrenia. II. The relationship between schizotypal personality disorder and schizophrenia. Arch Gen Psychiatry. 1981;38:982–984. [DOI] [PubMed] [Google Scholar]
- 48. Kwapil TR, Barrantes-Vidal N, Silvia PJ. The dimensional structure of the Wisconsin Schizotypy Scales: factor identification and construct validity. Schizophr Bull. 2008;34:444–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Vollema MG, van den Bosch RJ. The multidimensionality of schizotypy. Schizophr Bull. 1995;21:19–31. [DOI] [PubMed] [Google Scholar]
- 50. Venables PH, Rector NA. The content and structure of schizotypy: a study using confirmatory factor analysis. Schizophr Bull. 2000;26:587–602. [DOI] [PubMed] [Google Scholar]
- 51. Raine A, Reynolds C, Lencz T, Scerbo A, Triphon N, Kim D. Cognitive-perceptual, interpersonal, and disorganized features of schizotypal personality. Schizophr Bull. 1994;20:191–201. [DOI] [PubMed] [Google Scholar]
- 52. Stefanis NC, Smyrnis N, Avramopoulos D, Evdokimidis I, Ntzoufras I, Stefanis CN. Factorial composition of self-rated schizotypal traits among young males undergoing military training. Schizophr Bull. 2004;30:335–350. [DOI] [PubMed] [Google Scholar]
- 53. Cicero DC, Kerns JG. Multidimensional factor structure of positive schizotypy. J Pers Disord. 2010;24:327–343. [DOI] [PubMed] [Google Scholar]
- 54. Chmielewski M, Watson D. The heterogeneous structure of schizotypal personality disorder: item-level factors of the Schizotypal Personality Questionnaire and their associations with obsessive-compulsive disorder symptoms, dissociative tendencies, and normal personality. J Abnorm Psychol. 2008;117:364–376. [DOI] [PubMed] [Google Scholar]
- 55. Kendler KS, Ochs AL, Gorman AM, Hewitt JK, Ross DE, Mirsky AF. The structure of schizotypy: a pilot multitrait twin study. Psychiatry Res. 1991;36:19–36. [DOI] [PubMed] [Google Scholar]
- 56. Fonseca-Pedrero E, Ortuño-Sierra J, Lucas-Molina B, et al. Brief assessment of schizotypal traits: a multinational study. Schizophr Res. 2018;197:182–191. [DOI] [PubMed] [Google Scholar]
- 57. Krueger RF, Eaton NR, Derringer J, Markon KE, Watson D, Skodol AE. Personality in DSM-5: helping delineate personality disorder content and framing the metastructure. J Pers Assess. 2011;93:325–331. [DOI] [PubMed] [Google Scholar]
- 58. Lynam DR, Widiger TA. Using the five-factor model to represent the DSM-IV personality disorders: an expert consensus approach. J Abnorm Psychol. 2001;110:401–412. [DOI] [PubMed] [Google Scholar]
- 59. Widiger TA, Trull TJ, Clarkin JF, Sanderson CJ, Costa PTJ. A description of the DSM-IV personality disorders with the five-factor model of personality. In: Costa PT Jr, Widiger TA, eds. Personality Disorders and the Five-factor Model of Personality. 2nd ed. Washington, DC: American Psychological Association; 2002:89–99. [Google Scholar]
- 60. Bergman AJ, Harvey PD, Mitropoulou V, et al. The factor structure of schizotypal symptoms in a clinical population. Schizophr Bull. 1996;22:501–509. [DOI] [PubMed] [Google Scholar]
- 61. Fogelson DL, Nuechterlein KH, Asarnow RF, Payne DL, Subotnik KL, Giannini CA. The factor structure of schizophrenia spectrum personality disorders: signs and symptoms in relatives of psychotic patients from the UCLA family members study. Psychiatry Res. 1999;87:137–146. [DOI] [PubMed] [Google Scholar]
- 62. Peters ER, Joseph SA, Garety PA. Measurement of delusional ideation in the normal population: introducing the PDI (Peters et al. Delusions Inventory). Schizophr Bull. 1999;25:553–576. [DOI] [PubMed] [Google Scholar]
- 63. Fonseca-Pedrero E, Ortuño J, Debbané M, et al. The network structure of schizotypal personality traits. Schizophr Bull. 2018;44(suppl 2):S468–S479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. John OP, Naumann LP, Soto CJ. Paradign shift to the integrative big five trait taxonomy. In: John OP, Robins RW, Pervin LA, eds. Handbook of Personality: Theory and Research. New York, NY: Guilford Press; 2008:114–158. [Google Scholar]
- 65. Chmielewski M, Bagby RM, Markon K, Ring AJ, Ryder AG. Openness to experience, intellect, schizotypal personality disorder, and psychoticism: resolving the controversy. J Pers Disord. 2014;28:483–499. [DOI] [PubMed] [Google Scholar]
- 66. Samuel DB, Widiger TA. A meta-analytic review of the relationships between the five-factor model and DSM-IV-TR personality disorders: a facet level analysis. Clin Psychol Rev. 2008;28:1326–1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. O’Connor BP. A search for consensus on the dimensional structure of personality disorders. J Clin Psychol. 2005;61(3):323–345. [DOI] [PubMed] [Google Scholar]
- 68. Saulsman LM, Page AC. The five-factor model and personality disorder empirical literature: a meta-analytic review. Clin Psychol Rev. 2004;23:1055–1085. [DOI] [PubMed] [Google Scholar]
- 69. Grazioplene RG, Chavez RS, Rustichini A, DeYoung CG. White matter correlates of psychosis-linked traits support continuity between personality and psychopathology. J Abnorm Psychol. 2016;125:1135–1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Reynolds SK, Clark LA. Predicting dimensions of personality disorder from domains and facets of the Five-Factor Model. J Pers. 2001;69:199–222. [DOI] [PubMed] [Google Scholar]
- 71. Ross SR, Lutz CJ, Bailley SE. Positive and negative symptoms of schizotypy and the Five-factor model: a domain and facet level analysis. J Pers Assess. 2002;79:53–72. [DOI] [PubMed] [Google Scholar]
- 72. Krueger RF, Markon KE. A dimensional-spectrum model of psychopathology: progress and opportunities. Arch Gen Psychiatry. 2011;68:10–11. [DOI] [PubMed] [Google Scholar]
- 73. Markon KE, Krueger RF, Watson D. Delineating the structure of normal and abnormal personality: an integrative hierarchical approach. J Pers Soc Psychol. 2005;88:139–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Harkness AR, McNulty JL, Finn JA, Reynolds SM, Shields SM, Arbisi P. The MMPI-2-RF Personality Psychopathology Five (PSY-5-RF) scales: development and validity research. J Pers Assess. 2014;96:140–150. [DOI] [PubMed] [Google Scholar]
- 75. Krueger RF, Markon KE. The role of the DSM-5 personality trait model in moving toward a quantitative and empirically based approach to classifying personality and psychopathology. Annu Rev Clin Psychol. 2014;10:477–501. [DOI] [PubMed] [Google Scholar]
- 76. Ohi K, Shimada T, Nitta Y, et al. The Five-Factor Model personality traits in schizophrenia: a meta-analysis. Psychiatry Res. 2016;240:34–41. [DOI] [PubMed] [Google Scholar]
- 77. Camisa KM, Bockbrader MA, Lysaker P, Rae LL, Brenner CA, O’Donnell BF. Personality traits in schizophrenia and related personality disorders. Psychiatry Res. 2005;133:23–33. [DOI] [PubMed] [Google Scholar]
- 78. Kentros M, Smith TE, Hull J, McKee M, Terkelsen K, Capalbo C. Stability of personality traits in schizophrenia and schizoaffective disorder: a pilot project. J Nerv Ment Dis. 1997;185:549–555. [DOI] [PubMed] [Google Scholar]
- 79. Herrán A, Sierra-Biddle D, Cuesta MJ, Sandoya M, Vázquez-Barquero JL. Can personality traits help us explain disability in chronic schizophrenia? Psychiatry Clin Neurosci. 2006;60:538–545. [DOI] [PubMed] [Google Scholar]
- 80. Boyette LL, Korver-Nieberg N, Verweij K, et al. ; GROUP. Associations between the Five-Factor Model personality traits and psychotic experiences in patients with psychotic disorders, their siblings and controls. Psychiatry Res. 2013;210:491–497. [DOI] [PubMed] [Google Scholar]
- 81. Compton MT, Bakeman R, Alolayan Y, et al. Personality domains, duration of untreated psychosis, functioning, and symptom severity in first-episode psychosis. Schizophr Res. 2015;168:113–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Horan WP, Blanchard JJ, Clark LA, Green MF. Affective traits in schizophrenia and schizotypy. Schizophr Bull. 2008;34:856–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Beauchamp MC, Lecomte T, Lecomte C, Leclerc C, Corbière M. Personality traits in early psychosis: relationship with symptom and coping treatment outcomes. Early Interv Psychiatry. 2011;5:33–40. [DOI] [PubMed] [Google Scholar]
- 84. Bromet EJ, Schwartz JE, Fennig S, et al. The epidemiology of psychosis: the Suffolk County Mental Health Project. Schizophr Bull. 1992;18:243–255. [DOI] [PubMed] [Google Scholar]
- 85. Bromet EJ, Kotov R, Fochtmann LJ, et al. Diagnostic shifts during the decade following first admission for psychosis. Am J Psychiatry. 2011;168:1186–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Kotov R, Fochtmann LJ, Li K, et al. Declining clinical course of psychotic disorders during two decades after first hospitalization: evidence from the Suffolk County Mental Health Project. Am J Psychiatry . 2017;174:1064–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Velthorst E, Fett A-KJ, Reichenberg A, Perlman G, van Os J, Bromet EJ, Kotov R. The 20-year longitudinal trajectories of social functioning in individuals with psychotic disorders. Am J Psychiatry. 2017;174:1075–1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Hollingshead AB. Four factor index of social status. Unpublished manuscript1975. [Google Scholar]
- 89. John OP, Srivastava S. The Big Five trait taxonomy: history, measurement, and theoretical perspectives. In: Pervin LA, John OP, eds. Handbook of Personality: Theory and Research. 2nd ed. New York, NY: Guilford Press; 1999:102–138. [Google Scholar]
- 90. Watson D, Clark LA, Chmielewski M. Structures of personality and their relevance to psychopathology: II. Further articulation of a comprehensive unified trait structure. J Pers. 2008;76:1545–1586. [DOI] [PubMed] [Google Scholar]
- 91. Clark LA. Manual for the Schedule for Nonadaptive and Adaptive Personality (SNAP). Minneapolis: University of Minnesota Press; 1993. [Google Scholar]
- 92. Chmielewski M. The structure of common and severe psychopathology: Analyses of syndromes and symptoms. 2012; Unpublished Dissertation. [Google Scholar]
- 93. Clark LA, Simms LJ, Wu KD, Casillas A.. Schedule for Nonadaptive and Adaptive Personality. 2nd ed. Notre Dame: University of Notre Dame; 2014. [Google Scholar]
- 94. Morey LC, Warner MB, Shea MT, et al. The representation of four personality disorders by the schedule for nonadaptive and adaptive personality dimensional model of personality. Psychol Assess. 2003;15:326–332. [DOI] [PubMed] [Google Scholar]
- 95. Andreasen NC. Scale for the Assessment of Negative Symptoms. Iowa City: University of Iowa College of Medicine; 1984. [Google Scholar]
- 96. Strauss GP, Horan WP, Kirkpatrick B, et al. Deconstructing negative symptoms of schizophrenia: avolition-apathy and diminished expression clusters predict clinical presentation and functional outcome. J Psychiatr Res. 2013;47:783–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Messinger JW, Trémeau F, Antonius D, et al. Avolition and expressive deficits capture negative symptom phenomenology: implications for DSM-5 and schizophrenia research. Clin Psychol Rev. 2011;31:161–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Vrieze SI. Model selection and psychological theory: a discussion of the differences between the Akaike information criterion (AIC) and the Bayesian information criterion (BIC). Psychol Methods. 2012;17:228–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Arlot S, Celisse A. A survey of cross-validation procedures for model selection. Atatist Surv 2010;4:40–79. [Google Scholar]
- 100. Hu LT, Bentler PM. Fit indices in covariance structure modeling: sensitivity to underparameterized model misspecification. Psychol Methods. 1998;3:424–453. [Google Scholar]
- 101. Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Eq Model 1999;6(1):1–55. [Google Scholar]
- 102. Marsh HW, Hau K-T, Wen Z. In search of golden rules: comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing hu and bentler’s (1999) Findings. Struct Eq Model 2004;11(3):320–341. [Google Scholar]
- 103. Muthen LK, Muthen BO.. Mplus User’s Guide. 7th ed. Los Angeles, CA: Muthen & Muthen; 1998–2018. [Google Scholar]
- 104. Little TD, Rhemtulla M, Gibson K, Schoemann AM. Why the items versus parcels controversy needn’t be one. Psychol Methods. 2013;18:285–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Chen FF. What happens if we compare chopsticks with forks? The impact of making inappropriate comparisons in cross-cultural research. J Pers Soc Psychol. 2008;95:1005–1018. [DOI] [PubMed] [Google Scholar]
- 106. Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Eq Model. 2002;9(2):233–255. [Google Scholar]
- 107. Meade AW, Johnson EC, Braddy PW. Power and sensitivity of alternative fit indices in tests of measurement invariance. J Appl Psychol. 2008;93:568–592. [DOI] [PubMed] [Google Scholar]
- 108. Mcdonald RP. An index of goodness-of-fit based on noncentrality. J Classif. 1989;6:97–103. [Google Scholar]
- 109. Levant RF, Hall RJ, Rankin TJ. Male Role Norms Inventory-Short Form (MRNI-SF): development, confirmatory factor analytic investigation of structure, and measurement invariance across gender. J Couns Psychol. 2013;60:228–238. [DOI] [PubMed] [Google Scholar]
- 110. Kass RE, Raftery AE. Bayes factors. J Am Stat Assoc. 1995;90(430):773–795. [Google Scholar]
- 111. Horan WP, Reise SP, Subotnik KL, Ventura J, Nuechterlein KH. The validity of psychosis proneness scales as vulnerability indicators in recent-onset schizophrenia patients. Schizophr Res. 2008;100:224–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Kwapil TR, Gross GM, Silvia PJ, Barrantes-Vidal N. Prediction of psychopathology and functional impairment by positive and negative schizotypy in the Chapmans’ ten-year longitudinal study. J Abnorm Psychol. 2013;122:807–815. [DOI] [PubMed] [Google Scholar]
- 113. Cannon TD, Cadenhead K, Cornblatt B, et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008;65:28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Fusar-Poli P, Borgwardt S, Bechdolf A, et al. The psychosis high-risk state: a comprehensive state-of-the-art review. JAMA Psychiatry. 2013;70:107–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Hanssen M, Krabbendam L, Vollema M, Delespaul P, Van Os J. Evidence for instrument and family-specific variation of subclinical psychosis dimensions in the general population. J Abnorm Psychol. 2006;115:5–14. [DOI] [PubMed] [Google Scholar]
- 116. Ettinger U, Meyhöfer I, Steffens M, Wagner M, Koutsouleris N. Genetics, cognition, and neurobiology of schizotypal personality: a review of the overlap with schizophrenia. Front Psychiatry. 2014;5:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Tarbox SI, Pogue-Geile MF. A multivariate perspective on schizotypy and familial association with schizophrenia: a review. Clin Psychol Rev. 2011;31:1169–1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Berenbaum H, Valera EM, Kerns JG. Psychological trauma and schizotypal symptoms. Schizophr Bull. 2003;29:143–152. [DOI] [PubMed] [Google Scholar]
- 119. Raine A, Sheard C, Reynolds GP, Lencz T. Pre-frontal structural and functional deficits associated with individual differences in schizotypal personality. Schizophr Res. 1992;7:237–247. [DOI] [PubMed] [Google Scholar]
- 120. Giakoumaki SG. Cognitive and prepulse inhibition deficits in psychometrically high schizotypal subjects in the general population: relevance to schizophrenia research. J Int Neuropsychol Soc. 2012;18:643–656. [DOI] [PubMed] [Google Scholar]
- 121. Marjoram D, Miller P, McIntosh AM, Cunningham Owens DG, Johnstone EC, Lawrie S. A neuropsychological investigation into ‘Theory of Mind’ and enhanced risk of schizophrenia. Psychiatry Res. 2006;144:29–37. [DOI] [PubMed] [Google Scholar]
- 122. Rojas SL, Widiger TA. Convergent and discriminant validity of the Five Factor Form. Assessment. 2014;21:143–157. [DOI] [PubMed] [Google Scholar]
- 123. Strauss GP, Gold JM. A Psychometric comparison of the clinical assessment interview for negative symptoms and the brief negative symptom scale. Schizophr Bull. 2016;42:1384–1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Fortunati R, Ossola P, Camerlengo A, et al. Anhedonia in schizophrenia: the role of subjective experiences. Compr Psychiatry. 2015;62:152–160. [DOI] [PubMed] [Google Scholar]
- 125. Campellone TR, Elis O, Mote J, Sanchez AH, Kring AM. Negative symptoms in psychometrically defined schizotypy: the role of depressive symptoms. Psychiatry Res. 2016;240:181–186. [DOI] [PubMed] [Google Scholar]
- 126. Thomas EH, Rossell SL, Tan EJ, et al. Do schizotypy dimensions reflect the symptoms of schizophrenia? Aust N Z J Psychiatry. 2018:4867418769746. [DOI] [PubMed] [Google Scholar]
- 127. Gooding DC, Tallent KA, Matts CW. Clinical status of at-risk individuals 5 years later: further validation of the psychometric high-risk strategy. J Abnorm Psychol. 2005;114:170–175. [DOI] [PubMed] [Google Scholar]
- 128. Tarbox SI, Addington J, Cadenhead KS, et al. Premorbid functional development and conversion to psychosis in clinical high-risk youths. Dev Psychopathol. 2013;25:1171–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Healey KM, Penn DL, Perkins D, Woods SW, Keefe RSE, Addington J. Latent profile analysis and conversion to psychosis: characterizing subgroups to enhance risk prediction. Schizophr Bull. 2018;44:286–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Docherty AR, Sponheim SR. Anhedonia as an indicator of genetic vulnerability to schizophrenia. In: Ritsner MS, ed. Anhedonia: A Comprehensive Handbook Volume II: Neuropsychiatric And Physical Disorders. Dordrecht: Springer Netherlands; 2014:105–123. [Google Scholar]
- 131. Kendler KS, Thacker L, Walsh D. Self-report measures of schizotypy as indices of familial vulnerability to schizophrenia. Schizophr Bull. 1996;22:511–520. [DOI] [PubMed] [Google Scholar]
- 132. Pflum MJ, Gooding DC. Context matters: social cognition task performance in psychometric schizotypes. Psychiatry Res. 2018;264:398–403. [DOI] [PubMed] [Google Scholar]
- 133. Cohen AS, Callaway DA, Najolia GM, Larsen JT, Strauss GP. On “risk” and reward: investigating state anhedonia in psychometrically defined schizotypy and schizophrenia. J Abnorm Psychol. 2012;121:407–415. [DOI] [PubMed] [Google Scholar]
- 134. Yee CM, Mathis KI, Sun JC, et al. Integrity of emotional and motivational states during the prodromal, first-episode, and chronic phases of schizophrenia. J Abnorm Psychol. 2010;119:71–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Waltz JA, Demro C, Schiffman J, et al. Reinforcement learning performance and risk for psychosis in youth. J Nerv Ment Dis. 2015;203:919–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Kirschner M, Hager OM, Muff L, et al. Ventral striatal dysfunction and symptom expression in individuals with schizotypal personality traits and early psychosis. Schizophr Bull. 2018;44:147–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Wotruba D, Heekeren K, Michels L, et al. Symptom dimensions are associated with reward processing in unmedicated persons at risk for psychosis. Front Behav Neurosci. 2014;8:382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Kerns JG, Becker TM. Communication disturbances, working memory, and emotion in people with elevated disorganized schizotypy. Schizophr Res. 2008;100:172–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Kerns JG. Schizotypy facets, cognitive control, and emotion. J Abnorm Psychol. 2006;115:418–427. [DOI] [PubMed] [Google Scholar]
- 140. Blanchard JJ, Horan WP, Collins LM. Examining the latent structure of negative symptoms: is there a distinct subtype of negative symptom schizophrenia? Schizophr Res. 2005;77:151–165. [DOI] [PubMed] [Google Scholar]
- 141. Linscott RJ. The latent structure and coincidence of hypohedonia and schizotypy and their validity as indices of psychometric risk for schizophrenia. J Pers Disord. 2007;21:225–242. [DOI] [PubMed] [Google Scholar]
- 142. Ahmed AO, Strauss GP, Buchanan RW, Kirkpatrick B, Carpenter WT. Are negative symptoms dimensional or categorical? detection and validation of deficit schizophrenia with taxometric and latent variable mixture models. Schizophr Bull. 2015;41:879–891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Kendler KS. The structure of self-reported schizotypy in twins. J Personal Disord. 1992;6(1):1–17. [Google Scholar]
- 144. Compton MT, Goulding SM, Bakeman R, McClure-Tone EB. Confirmation of a four-factor structure of the Schizotypal Personality Questionnaire among undergraduate students. Schizophr Res. 2009;111:46–52. [DOI] [PubMed] [Google Scholar]
- 145. Gross GM, Mellin J, Silvia PJ, Barrantes-Vidal N, Kwapil TR. Comparing the factor structure of the Wisconsin schizotypy scales and the schizotypal personality questionnaire. Personal Disord. 2014;5:397–405. [DOI] [PubMed] [Google Scholar]
- 146. Freeman D, Pugh K, Vorontsova N, Antley A, Slater M. Testing the continuum of delusional beliefs: an experimental study using virtual reality. J Abnorm Psychol. 2010;119:83–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Elahi A, Perez Algorta G, Varese F, McIntyre JC, Bentall RP. Do paranoid delusions exist on a continuum with subclinical paranoia? A multi-method taxometric study. Schizophr Res. 2017;190:77–81. [DOI] [PubMed] [Google Scholar]
- 148. Marsh HW, Lüdtke O, Nagengast B, Morin AJ, Von Davier M. Why item parcels are (almost) never appropriate: two wrongs do not make a right–camouflaging misspecification with item parcels in CFA models. Psychol Methods. 2013;18:257–284. [DOI] [PubMed] [Google Scholar]
- 149. Meade AW, Kroustalis CM. Problems with item parceling for confirmatory factor analytic tests of measurement invariance. Org Res Methods. 2006;9(3):369–403. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.