Abstract
We report a case of invasive mucormycosis in 52 year-old woman. CT-scan and magnetic resonance imaging found a partial right sinus thrombosis associated with homolateral ethmoidal and maxillary sinusitis with submucosal inflammation. Histopathological examination of excised tissue was positive for mucormycosis. Our patient was treated by surgical debridement and a combination of amphotericin B and caspofungin, with a good outcome.
Keywords: Mucormycosis, Amphotericin B, Caspofungin, Combine therapy
1. Introduction
The incidence of fungal infection has increased considerably over recent decades [1]. The most common pathogens remain Candida spp, Aspergillius spp and Cryptococcus. Mucormycosis is a rare, invasive and rapidly progressive infection caused by fungi in the order mucorales [2,3]. It generally occurs in immunocompromised hosts such as neutropenic patients, but also in patients with uncontrolled diabetes mellitus [[2], [3], [4]]. Mucormycosis is classified according to the site of infection. Most cases are rhinocerebral mucormycosis, but cutaneos, pulmonary, gastrointestinal and disseminated infection have been observed [5,6]. The diagnosis relies on the histology and culture is used to identify the specific species [7]. The standard therapy for invasive mucormycosis consists of surgical debridement and aggressive antifungal medication. Amphotericin B (AmB) deoxycholate and liposomal AmB remain the most antifungal agent approved for the therapy of these invasive infections [[2], [3], [4],7]. Unfortunately, the overall rate of mortality from mucoromycosis remains high [2]. New strategies for the treatment of zygomycosis are urgently needed.
We present a case of rhinocerebral mucormycosis treated successfully with AmB and caspofungin in addition to surgical debridement. Regression of the patient's clinical and radiological condition was observed with the addition of caspofungin.
2. Case
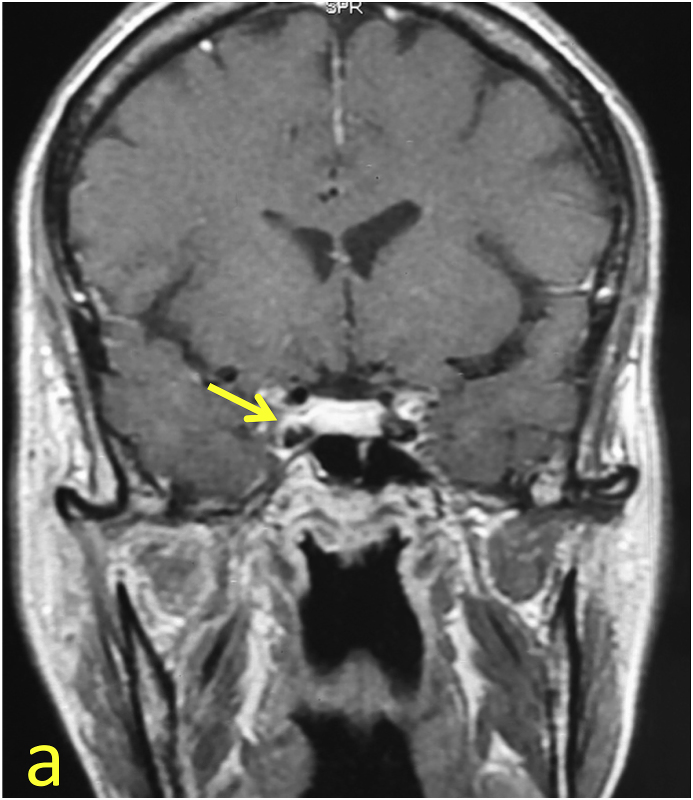
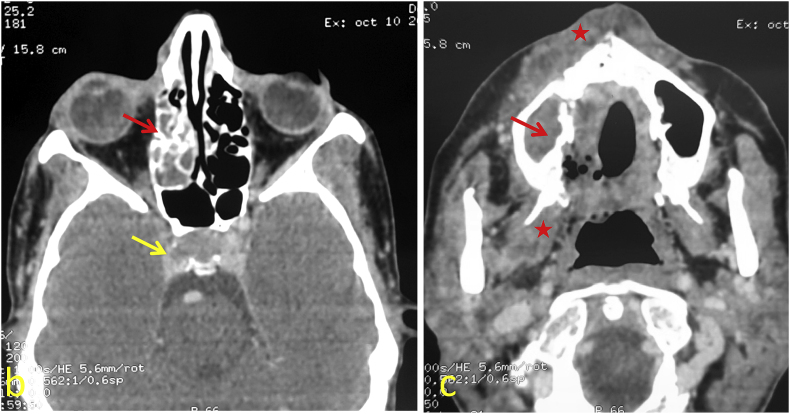
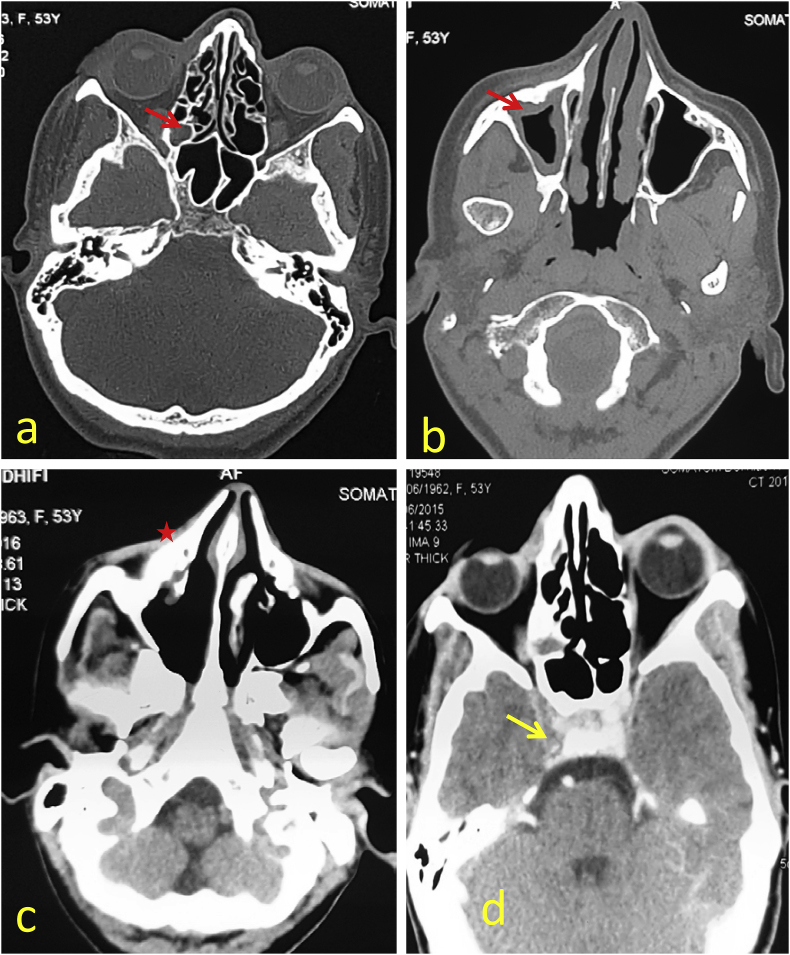
A 52 year-old diabetic female patient presented to the department of neurology with left facial paralysis, diplopia and blurred vision on September 2014 (day 0). There was “a partial right cavernous sinus thrombosis associated with homolateral ethmoidal and maxillary sinusitis with an inflammatory aspect of subcutaneous tissue “on cranial magnetic resonance (MRI) and Ct scan images (day +1) (Fig. 1, Fig. 2, Fig. 3).
Fig. 1.
MRI Coronal T1 after gadolinium injection (a): Endoluminal defect of the right cavernous sinus.
Fig. 2.
Cerebro-facial CT scan: Parenchymal window Axial sections (b and c): Endoluminal defect of the right cavernous sinus (yellow arrow). Complete filling of the right and subtotal ethmoid cells of the ipsilateral maxillary sinus (red arrows). Collections of straight nasolabial soft tissues and at the level of homolateral pterygoid muscles (red stars) (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
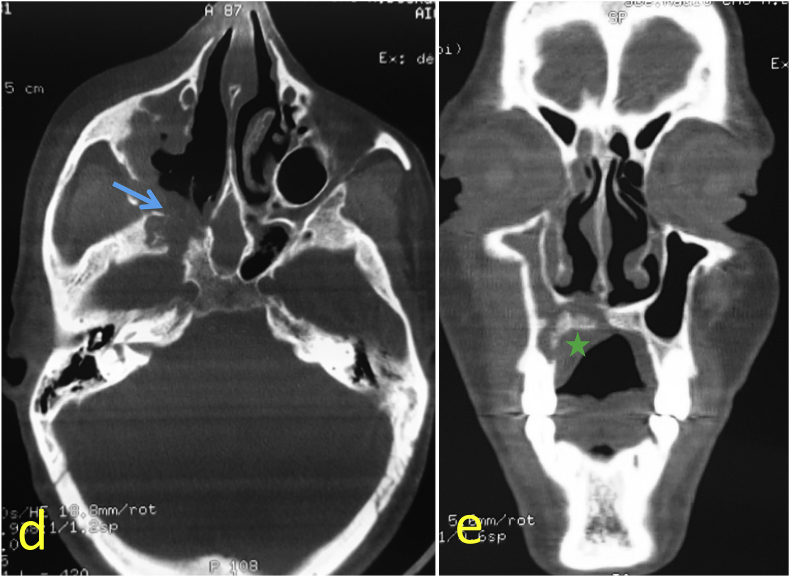
Fig. 3.
Destruction of the bony palate with detachment of a bone sequestrum (green star) as well as posterior and medial walls of the right maxillary sinus. Enlargement of the ipsilateral sphenopalatine foramen and extension to the inferior orbital fissure (blue arrow). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
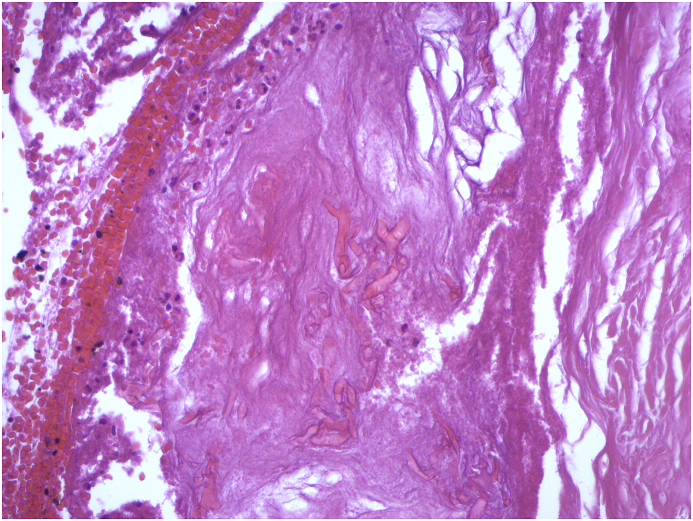
Endoscopic examination of the right nasal cavity revealed necrotic tissues in the inferior nasal turbinate (day +5). She underwent a right ethmoidectomy and middle meatectomy with a resection of the middle right canal. Histopathological examination of the sample demonstrated the presence of fungal cells which was consistent with mucormycosis (Fig. 4, Fig. 5).
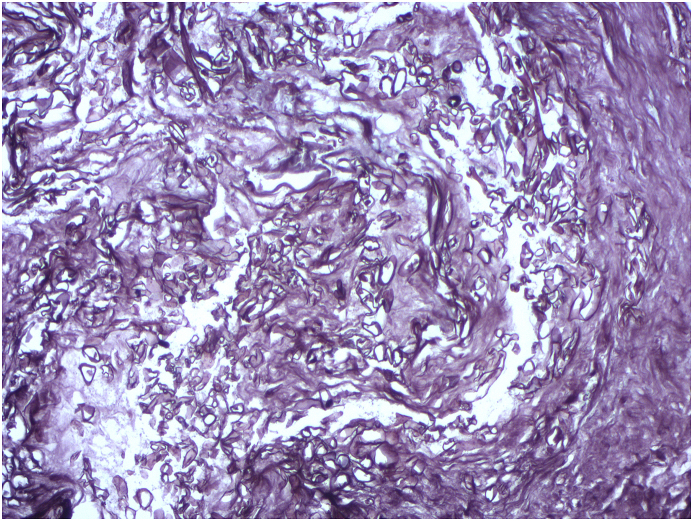
Fig. 4.
Histopathological examination of the operation material: Wide pleomorphic branching hyphae in a necrotic background (HE x 200).
Fig. 5.
Histopathological examination of the operation material: Methenamine-silver stain reveals numerous wide hyphae without septations (x 200).
Intravenous AmB was initiated, on day+30, at the dose of 50 mg (1mg/Kg/day) and the patient was transferred to our department of infectious diseases (day +31). Fourteen days after hospitalization, a cranial angioscan demonstrated “persistent thrombosis of cavernous sinus, the filling of the maxillary sinus and collections of straight nasolabial soft tissues and at the level of homolateral pterygoid muscles”.
A sinus biopsy was done on day +50. The biopsy specimen shows mucorales filaments. Molecular identification to the species isolates Rhizopus arrhizus.
The identification of Rhizopus was based on specific morphological characteristics.
Macroscopically, colonies are fast-growing and resemble white-to-gray cotton candy, darkening with time. The reverse is light-colored to white.
Microscopically, mycelia are marked by numerous stolons connecting groups of long sporangiophores.
Sporangiophores are usually unbranched, long, and terminate in a columella and a dark round sporangium containing oval colorless to brown spores. Stolons bear large rhizoids which are found immediately adjacent to the sporangiophore in the nodal position. Columella and sporangium collapse easily after discharging spores.
Sequencing of mucor species is only done when there are difficulties in species diagnosis, especially, since our country lacks the means to include molecular biology as systematic tools for mucormycosis diagnosis.
Our patient complained of fever and headache in the 73rd day of hospitalization. A biological control demonstrated an inflammatory syndrome. Targocid (2*400mg IV the first day then 400mg), cefaxone (2g IM) and Flagyl (3*500 mg IV) were added to her treatment.
Persistent thrombosis of right cavernous sinus associated to partial filling of maxillary and ethmoidal sinus was observed on the cranial scan on day +80. Caspofungin were added to her treatment (70 mg on the first day followed by 50 mg daily) on day +90. The antibiotics were suspended on day +120. Clinical symptoms resolved rapidly: regression of the facial paralysis and ocular involvement. Cranial scan on day +140 after first presentation demonstrated complete regression of ethmoid cell filling and persistence of thickening in the right maxillary sinus, disappearance of all previously described collections but the persistence of cavernous sinus thrombosis (Fig. 6). The combination antifungal therapy was continued for 4 weeks (stopped on day +171). No recurrence of the disease has been noted in more than 4 years follow-up.
Fig. 6.
Control CT scan after treatment with caspofungin: Axial cuts in bone window (a and b) and parenchymal (c and d): Virtually complete regression of ethmoid cell filling and persistence of thickening in the right maxillary sinus (red arrows). Disappearance of all previously described collections (red star). Persistence of right cavernous sinus thrombus (yellow arrow). . (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
3. Discussion
Treatment options for invasive mucormycosis are limited [3]. There have been no prospective randomized trials to define the optimal antifungal therapy for zygomycosis. For more than three decades treatment has been limited to amphotericin B deoxycholate with or without Flucytosine [2]. The past 10 years have witnessed a major expansion in the antifungal armamentarium through the introduction of less toxic formulations of AmB, the development of improved antifungal triazoles, and the advent of echinocandins lipopeptides. The echinocandins are a new class of antifungal agents that, although it had no activity against mucorales, it was shown that R. arrhizus expressed the target enzyme for Caspofungin 1,3β glucan synthase [4].
Caspofungin and Amphotericin B combination therapies were shown to have a synergistic effect in diabetic ketoacidosis mice with mycormycosis [3,4,[8], [9], [10], [11]]. In the literature, there are several case reports of favorable outcome in patients, with mucormycosis, treated with combination polyene–echinocandins. Ojeda-Uride proposed this synergic therapy and the hypothesis accounting for this synergistic effect was the degradation of cell wall beta-glucan cross linking by Caspofungin which strengthens polyene entry into cells [9]. The study of Kazak reported the regression of the patient's clinical and radiological condition with the addition of caspofungin in a rhino-cerebral mycormycosis initially treated with AmB [8]. Vaquez reported a successful treatment of rhinocerebral zygomycosis with a combination of caspofungin and liposomal AmB [10]. In a retrospective study, combination liposomal AmB–caspofungin therapy was associated with significantly improved outcomes for rhino-orbital-cerebral mucormycosis among patients with diabetes, compared with polyene monotherapy [12] (Table 1).
Table 1.
Revue of literature of outcome of combine therapy compared to AmB monotherapy in the treatment of mucormycosis.
| Series | Country of study | Year of study | Number of cases | Type of study | Pathological history | Age at Diagnosis (years) | Cause of Combine therapy | Combine Therapy and duration (days) | Outcome of Combine therapy |
|---|---|---|---|---|---|---|---|---|---|
| Kocoglu [14] | Turkey | 2017 | 1 | Humain | Diabetes | 51/F | Progression of the disease | Liposomal AmphotericinB + Caspofungin | Clinical success |
| Sheybani [2] | Iran | 2015 | 2 | Humain | Diabetes | 64/F 43/H |
Adverse reaction to AMB | Posaconazol + Caspofungin (30 days/42 days) | Clinical success |
| Abidi [15] | USA | 2014 | 101 | Humain | •Oncologic Malignancy •Organ or stem cell transplantation |
52/M | Severe cases | Liposomal AmphotericinB+ Caspofungin And/or posaconazole |
combination anti-fungal therapy has not improved survival |
| Kazak [9] | Turkey | 2013 | 1 | Humain | Diabetes | 41/F | Progression of the disease | Liposomal AmphotericinB+ Caspofungin (62 days) |
Regression of clinical and radiological condition |
| Lanterier [16] | France | 2012 | 101 | Humain | •Hematological malignancies (50%) •diabetes (23%) •trauma (18%) |
50/H | patients with hematological malignancies |
Liposomal AmphotericinB+ Posaconazole Or Liposomal AmphotericinB+ Caspofungin Or Liposomal AmphotericinB+ Caspofungin+ Posaconazole |
combination anti-fungal therapy has not improved survival |
| Ibrahim [17] | USA | 2012 | Murin | Diabetes neutropenia | Liposomal AmphotericinB+ Posaconazole |
• Benefit of combination therapy during intranasal or inhalational zygomycosis. •The study do not support combination polyene-posaconazole therapy for disseminated zygomycosis. |
|||
| Ojeda [10] | Paris | 2010 | 1 | Humain | •acute myeloid leukaemia •Diabetes |
55/F | Neutropenic Patientsduring The Induction of chemotherapy |
Liposomal AmphotericinB+ Caspofungin (56 days) |
Clinical success |
| Reed [13] | LA, USA | 2008 | 41 | Humain | •Diabetes (83%) •cancer (34%) •corticosteroid therapy (46%) •neutropenia (12%) •transplantation (10%) |
51/24 M (4–83) | Liposomal AmphotericinB+ Caspofungin |
•Therapeutic success •survival benefit most pronounced with patients with cerebral involvement |
|
| Vaquez [11] | Spain | 2005 | 1 | Humain | acute myelogenous leukaemia |
63/M | Progression of the disease | Liposomal AmphotericinB+ Caspofungin (45 days) |
Clinical success |
| Spellberg [18] | LA, USA | 2004 | Murine | Liposomal AmphotericinB+ Caspofungin (4 days) |
•Survival benefit •Prophylactic combine therapy was not more effective than prophylactic ABLC alone |
||||
| Our study | Tunisia | 2018 | 1 | Humain | Diabetes | 52/F | Progression of the disease | AmphotericinB+ Caspofungin (32 days) |
Regression of clinical and radiological condition |
The major limitations of our study are the only use of conventional amB as liposomal amB is unavailable in our country and the difficulties to make conclusions from a single case.
Nevertheless, our encouraging findings underscore the need for other studies to define the efficacy of combination AmB and caspofungin for the treatment of mucormycosis. Until such data are available, it may be reasonable to consider this combination given the unacceptably poor outcomes with amB monotherapy and the well-established safety profile of the echinocandins.
In our case, mycormycosis progressed clinically and radiologically despite AmB treatment associated to surgical debridement. A response occurred and radiological findings were markedly reduced with the addition of caspofungin.
4. Conclusion
Rhinocerebral mucormycosis remains a difficult to treat disease with high mortality rate. Presently, the triad of clinicians’ awareness, appropriate antifungal therapy and timely surgical intervention represent the main methods against the disease. Combination therapy with AmB and caspofungin could be more effective than amB monotherapy.
Continued research into the pathology of mycormycosis and large scale evaluation of arising treatment options are mandatory future directions in the area of rhino cerebral mucormycosis.
Conflict of interest
We have no conflicts of interest to disclose.
Ethical form
This investigation is in accordance with the Code of Ethics of the World. We have obtained written informed consent from the participant. Our patient's anonymity is preserved.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
References
- 1.Ibrahim A.B.J., Avanessian V., Brown K., Spellberg B., Edwards J. Caspofungin inhibits Rhizopus oryzae 1,3--D-glucan synthase, lowers burden in brain measured by quantitative PCR, and improves survival at a low but not a high dose during murine disseminated zygomycosis. Am. Soc. Microbiol. 2005;49(2):721–727. doi: 10.1128/AAC.49.2.721-727.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sheybani F.N.H., Sarvghad M., Ghabouli M., Arian M. How should we manage a patient with invasive mucoromycosis who develops life threatening reaction to amphotericin B? Report of two cases and literature review. Med. Mycol. Case Rep. 2015;8:29–31. doi: 10.1016/j.mmcr.2015.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reed C.B.R., Ibrahim A., Edwards J., Filler S., Robert Goldberg R. Combination polyene-caspofungin treatment of rhino-orbital-cerebral mucormycosis. Clin. Infect. Dis. 2008;47(3):364–371. doi: 10.1086/589857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mallis A.M.S., Naxakis S.S., Papadas A.T. Rhinocerebral mucormycosis: an update. Eur. Rev. Med. Pharmacol. Sci. 2010;14:987–992. [PubMed] [Google Scholar]
- 5.Ogawa T.T.K., Tojima I., Shibayama M., Kouzaki H., Ishida M. Successful treatment of rhino-orbital mucormycosis by a new combination therapy with liposomal amphotericin B and micafungin. Auris Nasus Larynx. 2012;39:224–228. doi: 10.1016/j.anl.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 6.Skiada A.L.F., Groll A., Pagano L., Zimmerli S., Herbrecht R. Diagnosis and treatment of mucormycosis in patients with hematological malignancies: guidelines from the 3rd European Conference on Infections in Leukemia (ECIL 3) Decis. Mak. Probl. Solving. 2013;98(4):492–504. doi: 10.3324/haematol.2012.065110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Izquierdo A.C.M., Cuesta I., Zaragoza O., Monzón A., Mellado E. In vitro activity of antifungals against Zygomycetes. Clin. Microbiol. Infect. 2009;15(5):71_6. doi: 10.1111/j.1469-0691.2009.02984.x. [DOI] [PubMed] [Google Scholar]
- 8.De Pauw B.W.T., Donnelly P., Stevens D., Edwards J., Calandra Th. Revised definitions of invasive fungal disease from the european organization for research and treatment of cancer/invasive fungal infections cooperative group and the national institute of allergy and infectious diseases mycoses study group (EORTC/MSG) consensus group. Clin. Infect. Dis. 2009;46(12):1813–1821. doi: 10.1086/588660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kazak E.A.E., Akalin H., Saraydaroğlu O., Hakyemez B., Erisen L. A mucormycosis case treated with a combination of caspofungin and amphotericin B. J. Mycol. Med. 2013;23:179–184. doi: 10.1016/j.mycmed.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 10.Ojeda-Uribe M.H.R., Kiefer M.H., Schultz Ph, Chain J., Chenard M.P. Lessons from a case of oromandibular mucormycosis treated with surgery and a combination of amphotericin B lipid formulation plus caspofungin. Acta Haematol. 2010;124:98–102. doi: 10.1159/000315675. [DOI] [PubMed] [Google Scholar]
- 11.Vazquez L.M.J., Sanz-Rodriguez C., Perez E., Caballero D., San Miguel J.F. Successful treatment of rhinocerebral zygomycosis with a combination of caspofungin and liposomal amphotericin B. Haematologica. 2005;90(12):39. 2005. [PubMed] [Google Scholar]
- 12.Ibrahim A.G.T., Fu Y., Edwards J., Spellberg B. Combination echinocandin-polyene treatment of murine mucormycosis. Antimicrob. Agents Chemother. 2008;52(4):1556–1558. doi: 10.1128/AAC.01458-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reed C.B.R., Ibrahim A., Edwards J., Filler S., Goldberg R. Combination polyene-caspofungin treatment of rhino-orbital- cerebral mucormycosis. Clin. Infect. Dis. 2008;47(3):364–371. doi: 10.1086/589857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kocoglu H.O.Y., Yazici Z., Hursitoglu M., Harmankaya O., Pehlivan B. Successful treatment of rhinocerebral mucormycosis with combination of liposomal amphotericin B and caspofungin (LAmB-C): an anecdotal clinical experience that deserves further investigations. Eurasian J. Med. Oncol. 2017;1(3):172–174. [Google Scholar]
- 15.Abidi M.S.M., Cummins N., Wilhelm M., Wengenack N., Brumble L. Stability in the cumulative incidence, severity, and mortality of 101 cases of invasive mucormycosis in high-risk patients from 1995-2011: a comparison of eras immediately before and after the availability of voriconazole and echinocandin-amphotericin combination therapies. Mycoses. 2014;57(11):687–698. doi: 10.1111/myc.12222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lanternier F.D.E., Morizot G., Elie C., Garcia-Hermoso D., Huerre M. A global analysis of mucormycosis in France: the RetroZygo study (2005–2007) Clin. Infect. Dis. 2012;54(1):35–43. doi: 10.1093/cid/cir880. [DOI] [PubMed] [Google Scholar]
- 17.Ibrahim A.G.T., Schwartz J., Edwards J., Spellberg B. Posaconazole mono- or combination therapy for treatment of murine zygomycosis. Antimicrob. Agents Chemother. 2009;53(2):772–775. doi: 10.1128/AAC.01124-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spellberg B.F.Y., Edwards J., Ibrahim A. Combination therapy with amphotericin B lipidcomplex and caspofungin acetate of disseminated zygomycosis in diabetic ketoacidotic mice. Antimicrob. Agents Chemother. 2005;49(2):830–832. doi: 10.1128/AAC.49.2.830-832.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]