Abstract
Bronchopulmonary lophomoniasis is rare but immunocompromised individual is susceptible to this infection. We reported a case of bronchopulmonary lophomoniasis in a Malaysian female with systemic lupus erythromatosus. She presented with productive cough, shortness of breath and high-grade fever for 2 weeks. Physical examination revealed bronchial sound and crackles over the left lung with, reduced expansion and dull percussion in lower left lobe. Chest radiography showed consolidation of the left lung. Routine laboratory tests revealed general low cell count. Blood and sputum culture were negative. Bronchoalveolar lavage stain and culture for bacterial and fungal were negative. Bronchoalveolar lavage for Lophomonas blattarum was positive. Patient was treated with antiprotozoal drug, metronidazole. All her clinical problems resolved and she was discharged 14 days after admission.
Keywords: Lophomonas, Respiratory, Pulmonary infection, Emerging parasite
1. Introduction
Lophomonas blattarum (LB) is being reported as the latest emerging parasite that reveal can cause infection of human respiratory system. There are some who questioned whether this parasite does exist and can cause disease in human [1]. However, there are increasing number of reports on LB infection from China [[2], [3], [4]], some are from Turkey [5], Spain [6], Peru [7], India [8,9] and Iran [10,11].
To this date, more than 250 cases have been reported worldwide. LB is a multiflagellated protozoon belonging to the supergroup Excavata and class Parabasalia [12]. It is the endocommensal in the hindgut of certain arthropods such as cockroaches, termites and mites [11], which usually found in the human domestic environment. Human can be infected by the organism through inhalation of aerosol containing LB cyst when they were excreted into the environment by cockroaches [12] or when human ingest the cyst contaminated food [3].
In view of the increase number of human population and reduce number of spaces especially in urban areas, human is living closely with the cockroaches. This leads to higher exposure to the infection and thus this parasite arguably have/can infect more people and cause severe disease in human in the nearer future. It is imperative that clinicians are aware this parasitic infection is one of the differential diagnosis in pulmonary infection, especially when patient is not responding to antibiotics [12].
2. Case presentation
A 29-year-old housewife with underlying systemic lupus erythromatosus (SLE) was admitted to hospital because of severe productive cough, shortness of breath and high-grade fever for 14 days prior to admission. The sputum was purulent. There was no history of night sweats, haemoptysis, loss of weight, loss of appetite. She was diagnosed to have SLE at the age of 25 years old after the birth of her first child, with the classic manifestation of the triad of fever, joint pain and butterfly malar rash. She has been on short courses of low dose prednisolone during flares and uses nonsteroidal anti-inflammatory drugs on and off especially when she had joint pain. Her most recent prednisolone administration was two months prior to admission. She did not use any other medication and her family history of chronic diseases was unremarkable.
She is a housewife with two children. Her husband usually bought food from hawker's centre nearby. They lived in an old terrace house in urban area and there is an ongoing problem with cockroaches' infestation. Otherwise, there is no termite infestation at the house.
2.1. Physical examination
On admission, the patient was conscious, orientated and feverish (39.9 °C). Her blood pressure was stable (105/70 mmHg) and slightly tachycardic with 125 beats per minute. Her respiratory rate was 35 breaths per minute. Bronchial sounds over lower left lung and pan-inspiratory crackles were noted upon auscultations. On percussion, there were dullness in lower lobe and reduced expansion on left side during inspiration. Other systemic examination was otherwise unremarkable.
2.2. Investigations
Blood investigations showed that she had anaemia with haemoglobin 9.6 g/dL, thrombocytopenia (75 × 109/L) and leukopenia (3.2 × 109/L). The liver function test was normal. C-reactive protein was 37.5 mg/L and erythrocyte sedimentation rate was 25 mm/hr. Urine test was normal and microscopy showed no protein, blood or white cells seen. Cultures of blood and sputum were negative. Gram stain sputum was also negative. Chest radiograph revealed ground glass appearance and patchy consolidation in left lower lobe.
Bronchoscopy was done on Day 8 of admission over the left lower lobe basal segment. The bronchoalveolar lavage (BAL) fluids were collected and send for culture, gram stain and detection of parasite. BAL culture and stain for bacterial and fungal were negative.
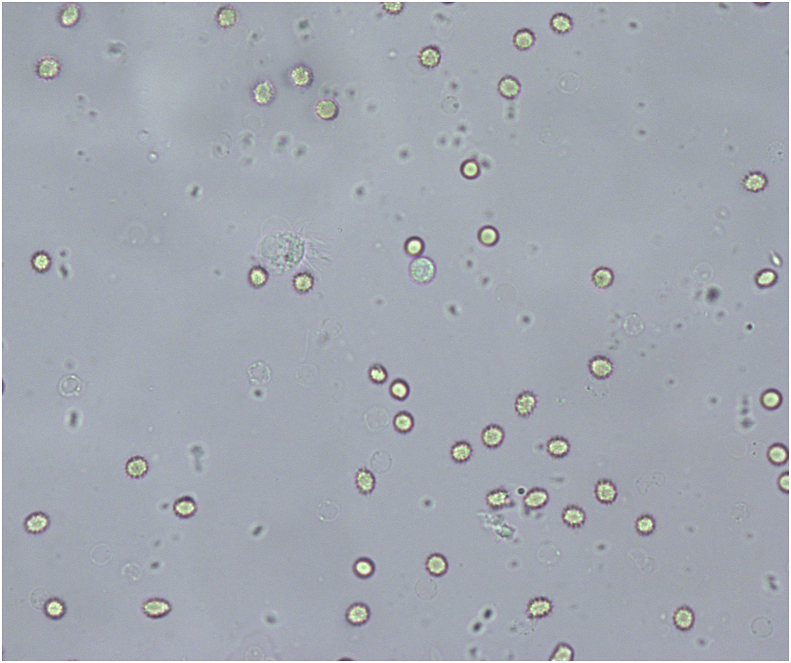
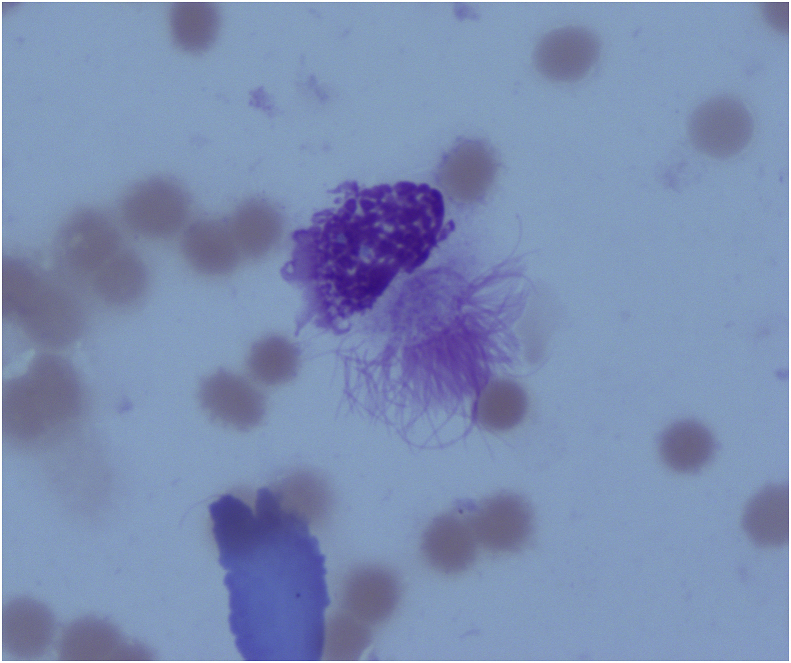
Parasitological microscopic examination of BAL showed many independent mobile trophozoites moving freely in jerky circular motion using its numerous flagella. The trophozoites had round and oval-shaped body with more than 50 flagella (Fig. 1). Their body size was around 25–40 μm. The flagella were very fine, of different length (10–15 μm) and were arranged in tufts at one end of cytoplasm. The longest flagella located in the centre of the tuft while shorter ones were found at the periphery. There was a large nucleus situated at the base of the tuft itself and many coarse, granulated vacuoles concentrated on the opposite site stained dark purple in Giemsa (Fig. 2). A diagnosis of Lophomonas blattarum infection and a flare up of systemic lupus erythematous was made.
Fig. 1.
Direct smear of BAL in saline. Mobile flagellated trophozoite found under light microscope with x400 magnification.
Fig. 2.
A multiflagellated protozoa in Giemsa stain, under light microscope with x1000 magnification.
2.3. Treatment
She was initially diagnosed as pneumonia and was treated with combination of two intravenous broad-spectrum antibiotics (beta-lactam meropenem and aminoglycosides) for three days and continued parenteral for four days. However, there was no improvement of her symptoms. After confirming Lophomonas blattarum infection, she was treated with a loading dose of 15mg/kg of metronidazole intravenously and then continued with oral metronidazole 500mg three doses per day for 10 days. She responded well, and all symptoms resolved and blood tests were back to normal. She was then prescribed with 10mg Prednisolone for 7 days with tapering dose when she was discharged after 14 days of admission.
2.4. Outcome and follow-up
Follow-up was done 3 months later and the patient was free from any respiratory problems. Her physical examination and laboratory tests were unremarkable. Lung x-ray was normal.
3. Discussion
This is the first case report on bronchopulmonary lophomoniasis in a Malaysian patient. She presented with common respiratory symptoms of mild pneumonia. It is challenging to diagnose parasitic lung infection solely based on clinical presentations. This is because the symptoms of parasitic lung infection are similar to other respiratory pathology [12]. The physician in this case have diagnosed this patient with bacterial pneumonia and treated her as such, even though the sputum and blood culture were negative for bacterial infections. Risk factors for this infection have been discussed in previous case reports [4,5,[11], [12], [13]] and these includes: immunocompromised status and prolonged use of steroids, contact with cockroaches’ and poor food hygiene practice.
In our case, the patient is immunocompromised, on low dose steroid for the past 4 years and the family usually eating food prepared by hawker (which may have been contaminated with cysts of the protozoa). Another important factor is the cockroaches’ infestation in the house which is an old terrace house in urban areas especially in central Kuala Lumpur. This finding seems to be consistent with other case reports of LB infection which found the lophomoniasis commonly reported in cases of immunocompromised patient [4,5,14,15]. Previous study by He et al. [4] reported two cases of transplant recipients had contact with cockroaches prior to symptoms diagnosed with late onset of pulmonary L. blattarum infection. In addition, Woerden et al. [15] comparing steroid-medicated asthmatic patients had more prevalent presence of flagellated protozoa in sputum than comparable healthy control. Even though so, these protozoa may infect immunocompetent individual as previous case reported by Tyagi et al. [9]; a case of L. blattarum infection in a healthy young male presented with pulmonary pathology symptoms revealed presence of L. blattarum in his BAL specimen.
Many similar case reports eosinophilia as the predominant results in blood tests [2,3,9,10,12]. Our patient's blood test results were reflective of her SLE conditions during flare up in which almost all her cell counts were reduced. Due to her immunosuppressive conditions, there is no increase of eosinophil. There is a delay in the diagnosis of this case. The sputum was not sent for parasitic investigations even though several cases have reported LB were seen in sputum [10,13,15] and the bronchoalveolar specimen were only taken on day 8 of admission after the antibiotic treatment failed.
Detection of at least one LB organism on a smear under microscopic examination is sufficient in establishing the diagnosis of LB infection in the context of related clinical manifestations. However, LB organism confirmation requires skilled parasitologist observation [12]. This is because it is difficult to distinguish between the LB and ciliated bronchial epithelial cells in the untrained eyes [16] and unsuitable staining method. The morphological features of LB are best demonstrated with Giemsa staining (as shown in our case). Other staining methods have been used such as Trichrome, Wheatley, Papanicolaou, Wright stain [5,12,13,17,18] with less clear morphology.
The pathognomonic morphological characteristics of ciliated epithelial fragments were round-oval nucleus at the basal end of the cell (if a nucleus was present) and a marked terminal bar at the apical end of the cell with regular, unidirectional cilia inserted into the terminal bar [13]. The parasites seen in our case has different lengths of flagella which are arrange irregularly and able to moves freely as individual flagellum. There were also cyst forms seen in the specimen.
Our patient's clinical problems only resolved after she was treated with metronidazole. It has been debated that this drug is also effective to treat broad range of respiratory anaerobic infections [19] thus is possible that there are other causes of her clinical manifestations. However, since repeated routine laboratory tests were negative for bacterial, fungal and other parasitic infections it is most likely that her rapid clinical improvement supported the diagnosis of bronchopulmonary lophomoniasis. Metronidazole have been reported in all other cases as the most effective treatment for this infection worldwide [2,5,8,9,20].
Declaration of competing interest
There are no conflict of interest.
Acknowledgments
The authors would like to acknowledge the contribution from physician and patient for this study. Last but not least, assistance from staff and Head Department of Parasitology & Medical Entomology, Faculty of Medicine, Universiti Kebangsaan Malaysia, Kuala Lumpur.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rmcr.2019.100939.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Li R., Gao Z.C. Lophomonas blattarum infection or just the movement of ciliated epithelial cells? China Med. J. 2016;129(6):739–742. doi: 10.4103/0366-6999.178025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yao G., Zeng L., Zhang B., Chang Z. Bronchopulmonary Lophomonas blattarum infection: two cases report and literature review. Zhonghua nei ke za zhi. 2008;47(8):176–182. [PubMed] [Google Scholar]
- 3.Xue J., Li Y.L., Yu X.M., Li D.K., Liu M.F., Qiu J.F. Bronchopulmonary infection of Lophomonas blattarum: a case and literature review. Korean J. Parasitol. 2014;52(5):521–525. doi: 10.3347/kjp.2014.52.5.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.He Q., Chen X., Lin B., Qu L., Wu J., Chen J. Late onset pulmonary Lophomonas blattarum infection in renal transplantation: a report of two cases. Intern. Med. 2011;50(9):1039–1043. doi: 10.2169/internalmedicine.50.4672. [DOI] [PubMed] [Google Scholar]
- 5.Kilimcioglu A.A., Havlucu Y., Girginkardesler N., Celik P., Yereli K., Ozbilgin A. Putative bronchopulmonary flagellated protozoa in immunosuppressed patients. BioMed Res. Int. 2014;912346:1–5. doi: 10.1155/2014/912346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martinez-Giron R., Doganci L. Lophomonas blattarum: a bronchopulmonary pathogen. Acta Cytol. 2010;54(5 Suppl):1050–1051. [PubMed] [Google Scholar]
- 7.Zerpa R., Ore E., Patio L., Espinoza Y.A. Lophomonas sp. in respiratory tract secretions in hos- pitalized children with severe lung disease. Rev. Peru. Med. Exp. Salud Pública. 2010;27(4):575–577. doi: 10.1590/s1726-46342010000400013. [DOI] [PubMed] [Google Scholar]
- 8.Verma S., Verma G., Singh D.V., Mokta J., Negi R.S., Jhobta A. Dual infection with pulmonary tuberculosis and Lophomonas blattarum in India. Int. J. Tuberc. Lung Dis. 2015;19(3):368–369. doi: 10.5588/ijtld.14.0513. [DOI] [PubMed] [Google Scholar]
- 9.Tyagi R., Anand K.B., Teple K., Negi R.S. Lophomonas blattarum infection in immunocompetent patient. Lung India. 2016;33(6):667–668. doi: 10.4103/0970-2113.192867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berenji F., Parian M., Fata A., Bakhshaee M., Fattahi F. First case report of sinusitis with Lophomonas blattarum from Iran. Case Rep Infect Dis. 2016;2614187:1–2. doi: 10.1155/2016/2614187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghafarian N., Bakhtiari E., Berenji F., Nakhaei M., Nakhaei B., Jamali-Behnam F. The study of Lophomonas blattarum infection in children with respiratory symptoms: a descriptive clinical study in North East of Iran. Int. J. Pediatr. 2018;6(6):7797–7802. [Google Scholar]
- 12.Martinez-Giron R., Woerden H.C.V. Lophomonas blattarum and bronchopulmonary disease. J. Med. Microbiol. 2013;62(11):1641–1648. doi: 10.1099/jmm.0.059311-0. [DOI] [PubMed] [Google Scholar]
- 13.Martinez-Giron R., Woerden H.C.V. Clinical and immunological characteristics associated with the presence of protozoa in sputum smears. Diagn. Cytopathol. 2013;41(1):22–27. doi: 10.1002/dc.21752. [DOI] [PubMed] [Google Scholar]
- 14.Rao X., Liao Q., Pan T., Li S., Zhang X., Zhu S. Retrospect and prospect of Lophomonas blattarum infections and lophomoniasis reported in China. Open Access Libr. J. 2014;1(e1121):1–6. [Google Scholar]
- 15.Woerden H.C.V., Ratier-Cruz A., Aleshinloye O.B., Martinez-Giron R., Gregory C., Matthews I.P. Association between protozoa in sputum and asthma: a case-control study. Respir. Med. 2011;105(6):877–884. doi: 10.1016/j.rmed.2010.11.016. [DOI] [PubMed] [Google Scholar]
- 16.Willy D., Patricia C., Rainier O., Nestor L. Community-acquired pneumonia caused by Lophomona sp. Community Acquir. Infect. 2017;4(2):38–40. [Google Scholar]
- 17.Martinez-Giron R., Woerden H.V. Bronchopulmonary lophomoniasis: emerging disease or unsubstantiated legend? Parasites Vectors. 2014;7(1):284. doi: 10.1186/1756-3305-7-284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alam-Eldin Y.H., Abdulaziz A.M. Identification criteria of the rare multi-flagellate Lophomonas blattarum: comparison of different staining techniques. Parasitol. Res. 2015;114(9):3309–3314. doi: 10.1007/s00436-015-4554-4. [DOI] [PubMed] [Google Scholar]
- 19.Woerden H.C.V., Martinez-Giron R. Lophomonas blattarum: is it only its morphology that prevents its recognition? Chin. Med. J. 2017;130(1):117. doi: 10.4103/0366-6999.196579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berenji F., Fata A., Vakili V., Sayedi S.J., Abdollahi B., Imanfar H. Unexpected high rate of Lophomonas blattarum in resistant upper and lower respiratory infection. Int. J. Med. Res. Health Sci. 2016;5(9):74–80. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.