Abstract
Aim:
Palliation of symptoms of patients with advanced carcinoma gallbladder (GB).
Materials and Methods:
Sixty-two newly diagnosed patients of unresectable advanced and metastatic GB cancers were enrolled, and following clinicoradiological assessment patients were considered for palliative symptom management.
Results:
The most common presenting symptom was pain in 57 (92%) patients. Obstructive jaundice was observed in 29 (46.7%) patients. Patients were considered for percutaneous biliary drainage/internal stenting, therapeutic ascitic tapping, and pain control. Patients with good performance status were considered for palliative chemotherapy.
Conclusion:
Patients with advanced carcinoma GB were managed with various palliative procedures with the aim to improve the quality of life of patients because of jaundice, loss of appetite, nausea, pain, etc. Symptoms are distressing for patients.
Keywords: Advanced gallbladder cancer, obstructive jaundice, palliation
INTRODUCTION
Gallbladder cancers (GBC) are cancers that arise from the GB mucosa. GBC is the fifth-most common malignancy of the gastrointestinal tract. The incidence of GBC correlates with the prevalence of cholelithiasis. Gallstones are found in >75% of all patients with GBC.[1] Patients who have gallstones for longer than 40 years have a significantly higher incidence of GBC than those who have had gallstones for a shorter time. GBC affects women three to four times more often than men. The incidence of GBC increases with age. Established risk factors include gallstone disease, bile composition, calcification of the GB wall, congenital biliary cysts or ductal anatomy, some infections, environmental carcinogens, and drugs. GBC can spread early by direct extension into the liver and other adjacent organs. Hematogenous metastasis tends to be from invasion into small veins that extend directly from the GB into the portal venous system, leading to hepatic metastases in segments IV and V of the liver. Patients with GBC are often asymptomatic. When symptoms occur, they may be similar to biliary colic or chronic cholecystitis and are nonspecific. Laboratory findings lack specificity and are not diagnostic. Patients may have increased alkaline phosphatase and bilirubin levels as a result of ductal obstruction in advanced cases. Serum CEA or CA19-9 may be elevated, but these tumor markers are not diagnostic. Abdominal computed tomography scans or magnetic resonance imaging can identify intraluminal polyps, GB wall thickening, mass lesions, hepatic involvement, nodal enlargement, or other distant spread. Positron emission tomography scanning may identify a disease that has not been radiologically apparent. Survival of patients with GBC is related to stage and histologic type of cancer.[2] Surgery is the only potentially curative option for GBCs. Absolute contraindications to surgery include distant metastases, vascular involvement, or nodal spread beyond the hepatoduodenal ligament. GBC has a high risk of systemic spread and local-regional failure and adjuvant chemotherapy and radiotherapy are recommended. Advanced GBC has a 1-year survival rate of <5%. Although the resection of gross disease may provide palliation and in some instances, a chance for cure, it may not always be possible. Goals of palliative treatment are to prevent biliary and bowel obstruction and to relieve pain. Palliative procedures include percutaneous biliary drainage (PTBD) to relieve biliary obstruction, pain management, chemotherapy, or radiation.[3] Aggressive nature and dismal prognosis of advanced unresectable cancer should be considered when deciding on palliative management. Patients at our institute come in advanced stages of GBC and so most are eligible for palliative treatment. The present study was carried out at a tertiary care center in Uttarakhand, which has a very high incidence of GBC and patients present at very advanced stages when only palliation of symptoms is required. In this study, we have managed patients with advanced GB malignancy by palliative procedures.
MATERIALS AND METHODS
In this study, 62 newly diagnosed patients of unresectable advanced and metastatic GBC, presenting in the Department of Surgery and Radiation Oncology were enrolled from December 2017 to December 2018. This study was performed in accordance with ethical guidelines and was approved by the Institutional Ethics Committee. The parameters such as gender, age, the presence of cholelithiasis, lymph node involvement, metastases, jaundice, and stage (according to the 8th Edition AJCC) were assessed. Personal habits of smoking or alcohol intake were also recorded.
RESULTS
Age ranged from 26 to 80 years (median = 53). Fifty-three females: 9 males (5.8:1). Cholelithiasis was present in 33 (53.2%) patients. The most common presenting symptom was pain in 57 (92%) patients.
The pain was because of stretching of liver capsule, compression by retroperitoneal nodes, GB lump or distension of abdomen due to the presence of ascites and omental nodules. Obstructive jaundice was observed in 29 (46.7%) patients due to compression by nodes at the porta hepatis, at the level of common bile duct or liver metastases. Fever was present in 23 (37%) patients because of cholangitis or disease process, 40 (64.5%) patients had loss of appetite, 45 (72.5%) had the loss of weight. Forty (64.5%) patients also experienced fatigue [Figure 1]. Others symptoms were pruritus, nausea, vomiting, and constipation.
Figure 1.
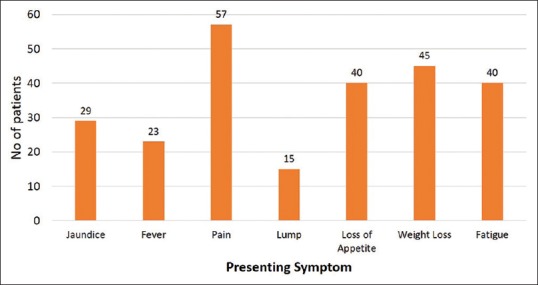
Symptoms of the patients of gall bladder cancer
None of the patients had a positive family history. Six patients had smoking and 2 had alcohol intake history. On clinical examination, the most common finding was abdominal distension with tenderness 24 (38.7%), 18 (29%) had GB mass with hepatomegaly, 14 (22.5%) had only GB lump palpable, 4 (6.4%) had gross ascites, and 2 (3.2%) left supraclavicular lymphadenopathy [Figure 2]. Hemoglobin levels varied from 5.5 to 13.8 mg/dl. Twenty-nine patients had obstructive jaundice (4.63–38.8 mg/dl). Patients were staged according to the AJCC 8th Edition and were 5 (8%) IIIA, 7 (11.2%) IIIB, 2 (3.2%) IVA, and 48 (77.4%) IVB.
Figure 2.
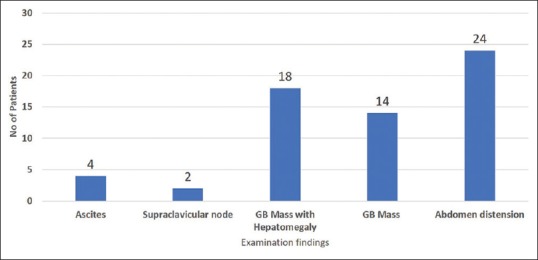
Clinical presentation of patients of gall bladder cancer
Symptom management
Patients were evaluated for their disease status, and it was found stage IV B was because of the liver or omental metastases in 24 patients and nodal involvement in 38. Fifteen patients had Hb below 10 g/dl, which lead to fatigue. Hence, blood transfusion was done in these patients. Therapeutic ascitic tapping was done in four patients as it was leading to respiratory distress. Patients with biliary obstruction were managed by percutaneous biliary drainage (PTBD) in 24 and internal stenting in five patients to relieve the biliary obstruction. Patients with internal stenting had a better quality of life as tube care was cumbersome. In patients with PTBD and internal stenting 10 had normalization of bilirubin levels and were considered for palliative chemotherapy. Pain control was required in 57 patients and the WHO analgesic ladder pattern was followed. Four patients were considered for the celiac block as the pain was not controlled on oral, intravenous, or transdermal patch and two were considered for palliative Radiotherapy for bone metastases. Three patients were considered for palliative gastrojejunostomy in view of duodenal obstruction due to the mass lesion [Figure 3].
Figure 3.
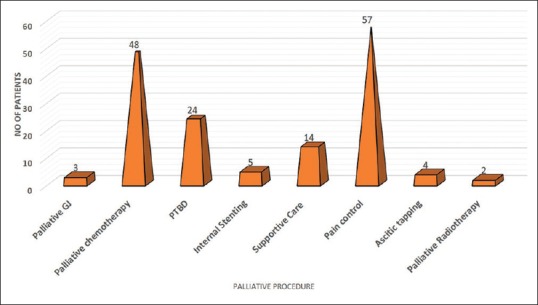
Palliative procedures performed in patients of gall bladder cancer
At compilation of the study, 5 (8%) died, 20 (32.2%) lost to follow-up, and 15 (24%) received palliative chemotherapy had radiological response after three cycles, but at the end of six cycles, stable/progression of disease and 22 (35.4%) were on supportive care. Patients who are receiving supportive care come for symptomatic management, for example, ascitic tapping, pain, constipation, feeding access, and any other problem or issue. At each visit, attendants were empowered for home care and counseled on a regular basis.
DISCUSSION
Overall prognosis in patients with advanced GBC is miserably poor, with a median survival of <6 months and 5-year survival of 5%–10%. The reason is because most patients, when symptomatic and diagnosed, have an advanced stage of the disease. Symptoms of GBC are problematic to distinguish from those of gallstone disease. Majority of patients with advanced GBC have unresectable disease. These patients but require need palliation of stressful symptoms of pain, jaundice, cholangitis, pruritus, and vomiting. The approach toward obstructive jaundice in patients with advanced unresectable GBC has now been changed and these patients are now offered endoscopic palliation.[4] In inoperable malignancies causing biliary obstruction, endoscopic retrograde cholangiopancreatography with the placement of plastic endoprosthesis or PTBD with metallic stenting remains minimally invasive options.[5,6] Choice of the procedure depends on the level of obstruction, interventionists expertise, and level of postprocedural care provided to the patient. If hepatic confluence is blocked and segmental ducts are also involved due to disease process, percutaneous intervention (percutaneous transhepatic biliary drainage and stenting) is offered for biliary drainage.[7] Thus, relieving jaundice improves quality of life of patients. Patients with advanced GBC may have mechanical gastric outlet obstruction due to duodenal compression/infiltration producing symptoms of early satiety, postprandial fullness, nausea, and vomiting.[8] Gastrojejunostomy helps in relieving symptoms in such patients. Palliative chemotherapy in advanced GBC is considered in patients with good performance status and standard of care in patients with advanced GBC is regarded to be gemcitabine in combination with cisplatin. In the present study, patients were managed according to the performance status and wishes of the patient and their families. All the symptoms were assessed and managed accordingly.
CONCLUSION
In the present study, patients with advanced carcinoma GB were managed with various palliative procedures according to their needs and performance status. The main aim was to improve the quality of life of patients because jaundice, loss of appetite, nausea, pain, etc., symptoms are distressing for patients. As this region is high incidence region for carcinoma GB and due to advanced stages at presentation more and more palliative procedures need to be individualized according to requirements of GBC patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Batra Y, Pal S, Dutta U, Desai P, Garg PK, Macharia G, et al. Gallbladder cancer in India: A dismal picture. J Gastroenterol Hepatol. 2005;20:309–14. doi: 10.1111/j.1440-1746.2005.03576.x. [DOI] [PubMed] [Google Scholar]
- 2.Pradeep R, Kaushik SP, Sikora SS, Bhattacharya BN, Pandey CM, Kapoor VK, et al. Predictors of survival in patients with carcinoma of the gallbladder. Cancer. 1995;76:1145–9. doi: 10.1002/1097-0142(19951001)76:7<1145::aid-cncr2820760708>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 3.Saxena R, Sikora SS, Kaushik SP. A triple bypass procedure for advanced carcinoma of the neck of gallbladder. Br J Surg. 1995;82:394–5. doi: 10.1002/bjs.1800820337. [DOI] [PubMed] [Google Scholar]
- 4.Vij JC, Govil A, Chaudhary A, Gulati R, Mehta S, Ganguli S, et al. Endoscopic biliary endoprosthesis for palliation of gallbladder carcinoma. Gastrointest Endosc. 1996;43:121–3. doi: 10.1016/s0016-5107(06)80112-4. [DOI] [PubMed] [Google Scholar]
- 5.Chaudhary A, Dhar P, Sachdev A, Agarwal A. Gastric outlet obstruction in carcinoma gall bladder. Indian J Gastroenterol. 1999;18:101–3. [PubMed] [Google Scholar]
- 6.Kapoor VK, Pradeep R, Haribhakti SP, Sikora SS, Saxena R, Kaushik SP. Intrahepatic segment III cholangio-jejunostomy as a palliative procedure in carcinoma of the gall bladder. Br J Surg. 1996;83:1709–11. doi: 10.1002/bjs.1800831215. [DOI] [PubMed] [Google Scholar]
- 7.Singh B, Kapoor VK, Sikora SS, Kalawat TC, Das BK, Kaushik SP, et al. Malignant gastroparesis and outlet obstruction in carcinoma gall bladder. Trop Gastroenterol. 1998;19:37–9. [PubMed] [Google Scholar]
- 8.Chandrashekhara SH, Gamanagatti S, Singh A, Bhatnagar S. Current status of percutaneous transhepatic biliary drainage in palliation of malignant obstructive jaundice: A review. Indian J Palliat Care. 2016;22:378–87. doi: 10.4103/0973-1075.191746. [DOI] [PMC free article] [PubMed] [Google Scholar]


