Abstract
Background
A belief has existed for many years that severe myopia is a direct indication for cesarean section or an instrumental vaginal delivery, although many academic papers negated this opinion. The aim of this study was to analyze the mode of delivery of myopic patients in the years 1990, 2000, and 2010.
Material/Methods
Medical records of 3027 women in labor from the 1st Department of Obstetrics and Gynecology, Medical University of Warsaw were analyzed in 3 time periods: year 1990 – group 1 (G1), year 2000 – group 2 (G2), and 2010 – group 3 (G3). Maternal age, severity and proportion of myopia, ophthalmological consultations, and mode of delivery were assessed.
Results
In G1 there were 992 patients, in G2 there were 1010 patients, and in G3 there were 1025 patients. Myopic women in labor accounted for 20% of G1, 12% of G2, and 20% of G3. The mean maternal age was ±29.4 years in G1, ±30 years in G2, and ±31.5 years in G3. Myopia was divided into 3 levels of severity depending on the degree of refractive error: low myopia <−3.0 diopters sphere (DS), moderate myopia from −3 DS to −6 DS, and high myopia >−6 DS. The number of ophthalmological examinations needed in myopic patients to decide on the mode of delivery showed an increasing tendency over the evaluated years, but the rates of referrals for cesarean section/assisted delivery decreased.
Conclusions
The proportion of myopic women in labor receiving ophthalmological consultations showed an increasing trend over time. Despite publication of the Ophthalmology-Obstetrics Consensus of the Polish Society of Ophthalmology guidelines, myopia still remains an indication for cesarean section (cesarian section), but not to shorten the second stage of delivery.
MeSH Keywords: Delivery, Obstetric; Myopia; Myopia, Degenerative; Pregnancy
Background
For a long time, gynecologists, obstetricians, and ophthalmologists shared the opinion that myopia (especially high myopia) is a contraindication for spontaneous vaginal delivery out of concern for rhegmatogenous retinal detachment [1]. The decision to perform an instrumental delivery (vacuum extraction, forceps delivery) or cesarean section in an attempt to shorten the second stage of labor was based mainly on the absolute value of refractive error in a given pregnant woman, irrespective of any additional retinal abnormalities [2]. The available literature contains no reports describing retinal detachment in myopic women during spontaneous vaginal delivery. The rise in intraocular pressure during the second stage of labor results in the vitreous body being pressed against the retina, which reduces the risk of retinal tears and retinal detachment [3]. Despite this fact, Socha et al. reported myopia was the predominant (57% of woman in labor) ocular indication for cesarean section among cases analyzed from 2000 to 2008 [4]. In 2014, the Polish Ophthalmological Society published ocular guidelines for spontaneous vaginal delivery (the Ophthalmology-Obstetrics Consensus), which state that in the case of myopic women, cesarean section is indicated in the presence of macular choroidal neovascularization [5]. The aim of this study was to analyze the modes of delivery in myopic patients in the years 1990, 2000, and 2010.
Material and Methods
This study involved a retrospective analysis of the available medical records of pregnant women admitted for delivery at the Obstetrics and Gynecology Teaching Hospital of the Medical University of Warsaw in 1990 – group 1 (G1), in 2000 – group 2 (G2), and in 2010 – group 3 (G3). The parameters assessed included delivery rate, maternal age, and the proportion and severity of myopia. Based on the enclosed ophthalmological consultations, we reviewed ocular indications for cesarean section and indications for assisted (forceps delivery or vacuum extraction) shortening of the second stage of labor.
The statistical analysis was performed with the use of the Statistica v. 9.12 program. The qualitative variables are reported as absolute and relative frequencies (percentages,%). The analysis of the linear relationships/trends between the 3 groups was performed using the Mantel-Haenszel (M-H) chi-square test. The concordance correlation coefficient analysis comparing 2 groups was calculated with the use of the Pearson’s chi-square test with Yates’s correction for continuity or with the Fisher exact test. The quantitative variables are reported as means and standard deviation (SD). The differences in the mean values (of the quantitative variables analyzed) between the 3 groups were evaluated with univariate analysis of variances (ANOVA) and Tukey’s post hoc test. The results with the probability (p) of an error less than 0.05 (p<0.05) was deemed statistically significant.
The study was approved by a local ethics committee.
Results
We assessed a total of 3027 maternity patients in the years 1990, 2000, and 2010. In 1990, 202 out of 992 maternity patients (G1) were myopic; in 2000, 119 out of 1100 were myopic; and in 2010, 213 out of 1025 were myopic. A lower proportion of myopic patients was observed in 2000 in comparison than in 1990 and 2010 (p<0.0001). These data are presented in Table 1.
Table 1.
The number of myopic patients out of all maternity patients evaluated in the given years.
| Year | Maternity patients | Myopic maternity patients | p (1990 vs. 2000) | p (2000 vs. 2010) | p (M-H)* |
|---|---|---|---|---|---|
| 1990 | 992 | 202 (20.4%) | <0.0001 | – | 0.76 |
| 2000 | 1,010 | 119 (11.8%) | <0.0001 | ||
| 2010 | 1,025 | 213 (20.8%) | – |
Mantel-Haenszel (M-H) Chi-Square test.
Due to incomplete data, 200, 118, and 211 myopic maternity patients from the years 1990, 2000, and 2010, respectively, were included in the analysis. The mean age of the maternity patients was 29.4±5.1 years (p<0.0001) in 1990 (G1) and 29.4±4.5 years (p<0.0001) in 2000 (G2), but was significantly older in 2010 (31.5±3.8 years). We analyzed both the number of ophthalmological examinations in myopic pregnant women and the findings of those examinations.
In 1990, 10 out of 200 pregnant patients with myopia underwent an ophthalmological examination. Refractive error assessments in this subgroup revealed 2 patients with low myopia, 2 patients with moderate myopia, and 6 patients with high myopia. As a result, 9 out of 10 of these patients were assigned to undergo an instrumental vaginal delivery for ophthalmological reasons. Only 1 patient delivered naturally. In 2000, 15 out of 118 myopic patients underwent an ophthalmological examination. Examinations revealed 9 cases of moderate and 6 cases of high myopia. Six patients (3 with moderate and 3 with high myopia) were found to have indications for a cesarean section. In 2010, 42 out of 211 myopic patients were referred for ophthalmological examination. As a result, 14, 12, and 16 patients were found to have low, moderate, and high myopia, respectively. In 22 cases, a cesarean section was recommended for ophthalmological reasons. Our data show no significant relationship between the severity of myopia and referrals for cesarian section/assisted delivery in the 3 periods evaluated: in 1990 (p=0.4000), in 2000 (p=0.6224), and in 2010 (p=0.2823). The results are presented in Table 2.
Table 2.
Ophthalmological consultations, referrals for assisted delivery and C-section, and the degree of myopia in the evaluated population.
| Years | p (M-H*) | p (Chi2 Pearson’s)** | |||||
|---|---|---|---|---|---|---|---|
| 1990 | 2000 | 2010 | 1990 vs. 2000 vs. 2010 | 1990 vs. 2000 | 1990 vs. 2010 | 2000 vs. 2010 | |
| Maternity patients | 992 | 1010 | 1025 | ||||
| Myopic maternity patients | 202 (20.4%) | 119 (11.8%) | 213 (20.8%) | 0.762 | <0.0001 | 0.871 | <0.0001 |
| Myopic maternity patients (full data) | 200 | 118 | 211 | ||||
| Mean age of myopic patients (years) | 29.4±5.1 | 29.4±4.5 | 31.5±3.8 | <0.0001 | 0.998 | <0.0001 | <0.0001 |
| Number of ophthalmological consultations | 10 (5%) | 15 (12.7%) | 42 (19.9%) | <0.0001 | 0.0136 | <0.0001 | 0.098 |
| Number of referrals for assisted delivery | 9 (90%) | 6 (40%) | 22 (52%) | 0.1238; 0.0401 | 0.0177 | 0.0361 | 0.410 |
| Degree of myopia | |||||||
| Low | 1/2 | 0/0 | 8/14 | 1.00 | – | 1.00 | – |
| Moderate | 2/2 | 3/9 | 4/12 | 0.2419 | 0.1818 | 0.1648 | 1.00 |
| High | 6/6 | 3/6 | 10/16 | 0.1500 | 0.1818 | 0.1328 | 0.6550 |
| p | 0.400 | 0.6224 | 0.2823 | ||||
Mantel-Haenszel chi square test;
Pearson’s chi square test.
The number of ophthalmological examinations in myopic patients performed to decide on the method of delivery had a tendency to increase over time.
In comparison with the relevant data from 1990, we observed a decrease in referral rates for cesarean delivery in pregnant women evaluated in 2000 (p=0.0177) and in 2010 (p=0.0361); the respective proportions were 90.0% in 1990, 40.0% in 2000, and 52.0% in 2010 (Mantel-Haenszel chi-square test, p=0.1238).
The numerical data and proportion of instrumental deliveries and cesarian sections recommended due to ophthalmological indications are presented in Table 2, Figure 1.
Figure 1.
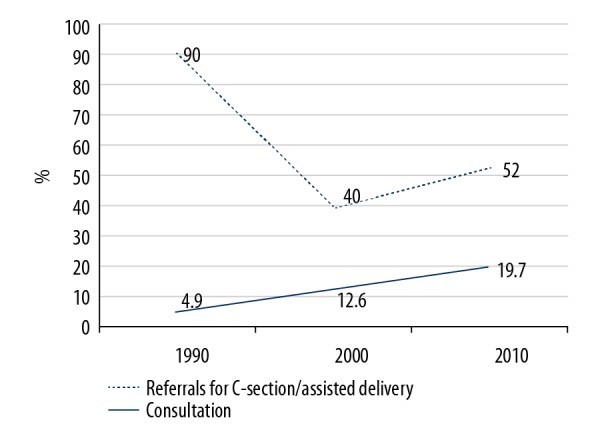
The proportion of ophthalmological consultations and referrals for cesarean section or assisted delivery in myopic patients. There was a significant increase in ophthalmological consultations among myopic patients, from 5% in 1990 to 12.7% in 2000 and 19.9% in 2010 (p<0.0001, Mantel-Haenszel test). Referrals for cesarean section or instrumental delivery decreased significantly from 1990 to 2000 and from 1990 to 2010, but did not change significantly from 2000 to 2010.
Our analysis of the indications for assisted delivery or cesarian section in myopic patients showed a tendency towards more detailed ophthalmological examinations. Throughout the analyzed period, the predominant ophthalmological indications for a cesarian section or assisted delivery in myopic parturients were peripheral retinal degenerative lesions (some already treated with laser photocoagulation) and retinal thinning: 9 of 10 patients in 1990, 6 of 15 patients in 2000, and 16 of 22 patients in 2010. In 2010, the more detailed ophthalmological examination resulted in finding other indications for assisted/cesarean delivery: retinal tear treated with laser photocoagulation (1 case), optic nerve atrophy (1 case), glaucoma (2 cases), cavernous hemangioma of the optic disc (1 case), diabetic retinopathy (1 case), and 2 cases of decreased corneal thickness following refractive surgery (LASIK).
In the analyzed years, we compared the number of cesarian sections and assisted deliveries performed in myopic patients (including those who did not undergo ophthalmological examination prior to delivery) and in patients with no vision impairment. We observed a significant increase in the number of cesarian sections in both of these groups (Figure 2).
Figure 2.
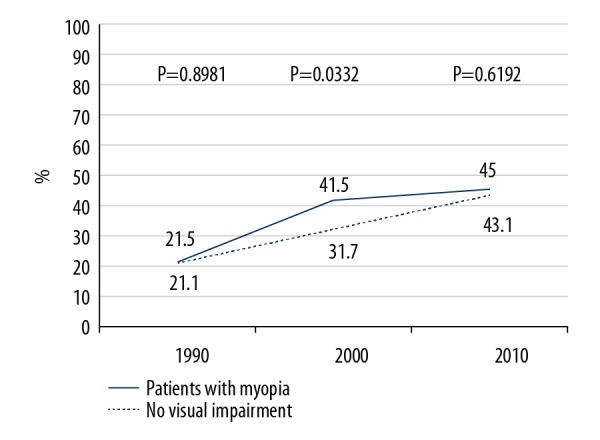
The proportion of cesarean section or assisted delivery in myopic patients and patients without visual impairment stratified by year. The comparison of non-spontaneous vaginal delivery in parturients with myopia and without visual impairment (non-myopic) shows significant increases in both groups.
Discussion
During pregnancy, the eye undergoes a number of physiological, hormone-induced, hemodynamic changes. An increase in circulating blood volume and water retention cause corneal thickening, which changes corneal curvature, thus inducing temporary myopia (inducing or exacerbating visual impairment by –1 DS) and an associated distance vision impairment. This phenomenon is most commonly observed during the third trimester of pregnancy and resolves after childbirth [5–7]. Before the 1990s, myopia was the predominant contraindication for spontaneous vaginal delivery [2,8]. This was dictated by the widespread fear of rhegmatogenous retinal detachment during the second stage of labor. The reasoning behind this belief was that the fluctuations in intraocular and orbital pressures (induced by the Valsalva manoeuvre) would lead to a displacement or even partial detachment of the vitreous body, which would facilitate rhegmatogenous retinal detachment in cases with pre-existing retinal degenerations [9].
For this reason, the absolute value of refractive error alone, often with no retinal examination, determined whether the obstetrician shorten the second stage of labor via instrumental assisted delivery or cesarean section. In the previous century, such recommendations were part of the obstetric protocol. Consequently, in most cases, the obstetrician’s decision as to mode of delivery was based solely on the refractive error in a given patient.
This is consistent with the findings of our analysis for the year 1990, where 90% of patients had their second stage of labor shortened for ocular reasons, with a very low number of consultations (5%). This decision-making paradigm was not observed in earlier studies [10].
There are no available reports illustrating the relationship between natural delivery on one hand and retinal detachment and refraction error on the other. Kuba et al. maintained that an increase in intraocular pressure during the second stage of labor pushed the vitreous body against the retina, eliminating the risk of retinal tears or detachment [3]. This is consistent with studies by Neri et al. and Prost, which examined parturients prior to and after delivery. No patients showed new degenerative lesions in the retina, retinal tears, or rhegmatogenous detachment [10–12].
Our analysis for the years 2000 and 2010 confirmed a shift in the earlier belief towards the view that it is not the degree of refractive error that should determine the mode of delivery in myopic patients. The years 2000 and 2010 showed a dramatic increase in the number of pre-delivery ophthalmological consultations that focused on assessing the condition of the retina, and a subsequent decrease in the proportion of cesarean deliveries (to 53% and 45%, respectively). Our findings are consistent with those of Socha et al., who reported that 57% of myopic patients underwent cesarean delivery in the period 2000–2008 [4]. Discrepancies of opinion as to the recommended mode of delivery in myopic parturients resulted in establishing the 2014 Ophthalmology-Obstetrics Consensus regarding the mode of delivery in patients with ocular lesions, under the auspices of the Polish Ophthalmological Society [5]. Consequently, cesarean section is recommended in myopic patients only when there is concomitant choroidal neovascularization in a macular region (which in some cases accompanies high myopia) due to the associated risk of retinal hemorrhage during the second stage of labor and the ensuing sudden deterioration of visual acuity [13].
Our findings demonstrate that the view regarding the degree of refraction error as the sole basis for choosing the mode of delivery has undergone a radical shift. Nonetheless, despite a number of unequivocal reports, ophthalmologists still often have reservations about a natural delivery in light of the condition of the retina in their myopic patients [8,14,15]. Moreover, the demanding attitude of those women who, for various reasons, are afraid of natural delivery also undoubtedly plays a role in decision-making.
The advisability of prophylactic laser retinal photocoagulation before a spontaneous vaginal delivery is somewhat controversial. Based on their observations in 10 women with ocular lesions predisposing to rhegmatogenous retinal detachment, Landau et al. did not recommend prophylactic retinal photocoagulation in asymptomatic cases [16]. Conversely, Millazzo et al. and other researchers did recommend prophylactic laser photocoagulation prior to spontaneous vaginal delivery in patients with degenerative retinal lesions and/or holes predisposing to retinal detachment [7,11,12,14,17].
Conclusions
It is widely accepted that myopia itself, as a refractive error, is not a contraindication for spontaneous vaginal delivery. If the physician has doubts, the ophthalmic indications for non-spontaneous vaginal delivery in myopic women should be justified by a detailed eye examination. including macula and peripheral retina. for any anomalies (e.g., choroid neovascularization) to assess the risk of ocular complications during spontaneous vaginal delivery [11,13–15]. Concomitant macular neovascularization is an indication for cesarian section. This topic is the subject of current research, and we look forward to obtaining data from 2020.
Footnotes
Source of support: Departmental sources
Conflict of interests
None.
References
- 1.Atassi A. Intraocular pressure variations during delivery. Geburtshilfe Frauenheilkd. 1972;32:832–34. [PubMed] [Google Scholar]
- 2.Iancu G, Coviltir V, Iancu R, Corbu C. Particularities of myopia in pregnancy. Gineco Eu. 2013;9:196–99. [Google Scholar]
- 3.Kuba GB, Kroll P. [Labor monitoring and indications for abortion and cesarean section in eye diseases – an overview]. Klin Monatsbl Augenheilkd. 1997;211:349–53. doi: 10.1055/s-2008-1035146. [In Grerman] [DOI] [PubMed] [Google Scholar]
- 4.Socha M, Piotrowiak I, Jagielska I, et al. [Retrospective analysis of ocular disorders and frequency of cesarean sections for ocular indications in 2000–2008 – our own experience]. Ginekol Pol. 2010;81:188–91. [in Polish] [PubMed] [Google Scholar]
- 5.Ophthalmology-Obstetrics Consensus of Polish Society of Ophthalmology. 2014;10:06. [Google Scholar]
- 6.Ciszewska J, Moneta-Wielgos J, Brydak-Godowska J, Turczynska M. [Pregnancy and the eye – selected aspects]. Okulistyka. 2011;14(1–2):27–29. [in Polish] [Google Scholar]
- 7.Pilas-Pomykalska M, Czajkowski J, Oszukowski P. [Ocular changes during pregnancy]. Ginekol Pol. 2005;68:8. [in Polish] [PubMed] [Google Scholar]
- 8.Mohammadi SF, Letafad Nejdan M, Ashrafi E, et al. A survey of ophthalmologist and gynecologist regarding termination of pregnancy and choice of delivery mode in the presence of eye diseases. J Curr Ophthalmol. 2017;29:126–32. doi: 10.1016/j.joco.2016.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Juenemann AM, Nowomiejska K, Oleszczuk A, et al. [Mode of delivery and eye diseases]. Ginekol Pol. 2012;83:613–17. [in Polish] [PubMed] [Google Scholar]
- 10.Neri A, Grausbord R, Kremer I, et al. The management of labor in high myopic patients. Eur J Obstet Gynecol Reprod Biol. 1985;19:277–79. doi: 10.1016/0028-2243(85)90041-3. [DOI] [PubMed] [Google Scholar]
- 11.Prost M. [Severe myopia and delivery]. Klin Oczna. 1996;2:129–30. [In Polish] [PubMed] [Google Scholar]
- 12.Ciszewska J, Dróbecka-Brydak E. [Ocular disorders during pregnancy]. Terapia. 2000;11:18–19. [In Polish] [Google Scholar]
- 13.Karska-Basta I, Tarasiewicz M, Kubicka-Trzaska A, et al. [Cesarean section and eye disorders]. Ginekol Pol. 2016;87:217–21. doi: 10.17772/gp/61752. [In Polish] [DOI] [PubMed] [Google Scholar]
- 14.Moneta-Wielgos J, Brydak Godowska J, Golebiewska J, et al. The assessment of retina in pregnant women with myopia. Neuro Endocrinol Lett. 2018;(4):321–24. [PubMed] [Google Scholar]
- 15.Ciszewska J, Brydak-Godowska J, Moneta-Wielgos J, et al. [Delivery in myopic women – facts and myths]. Okulistyka. 2011;14(1–2):41–42. [Google Scholar]
- 16.Landau D, Seelenfreund MH, Tadmor O, et al. The effect of normal childbirth on eyes with abnormalities predisposing to rhegmatogenous retinal detachment. Graefes Arch Clin Exp Ophthalmol. 1995;233(9):598–600. doi: 10.1007/BF00404712. [DOI] [PubMed] [Google Scholar]
- 17.Millazo S, Mikou R, Berthout A, Bremond-Gignac D. Understanding refraction disorders and oculomotor problems during pregnancy. J Fr Ophthalmol. 2010;33:368–71. doi: 10.1016/j.jfo.2010.03.001. [in French] [DOI] [PubMed] [Google Scholar]


