Abstract
Background
Learning disabilities (LD) and attention-deficit hyperactivity disorder (ADHD) are often accompanied by significant socio-emotional impairments and mental health challenges. However, there is a lack of controlled, quantitative research on potential interventions to address this issue. The current study evaluated the impact of a near-peer mentoring program for youth with LD/ADHD designed to promote socio-emotional well-being.
Methods
Youth with LD/ADHD who participated in the mentoring program (Mentored; n=99) were compared to non-mentored youth with LD/ADHD (Control-NM; n=51) and typically-developing youth without LD/ADHD (Control-TD; n=81) pre-mentoring in the fall, and post-mentoring in the spring. Participants were assessed on self-report measures of anxiety, depression, interpersonal relations, and self-esteem.
Results
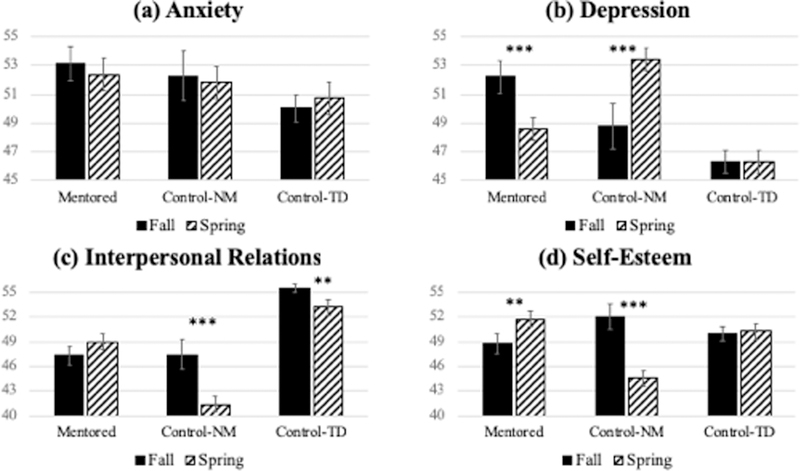
Youth with LD/ADHD showed significantly higher scores of depression and significantly lower scores of interpersonal relations compared to the Control-TD group at fall baseline. The depression and self-esteem scores of the Mentored group significantly decreased and increased respectively after mentoring. These changes were associated with mentee-perceived mentorship quality. The Control-NM group showed significant decreases in both self-esteem and interpersonal relations, as well as increases in depression over time, while the Control-TD group remained stable across all measures.
Conclusions
Results suggest that mentoring shows promise as a potential intervention for youth with LD/ADHD and co-occurring socio-emotional and mental health difficulties. The study is the first, to our knowledge, to quantify the effect of a near-peer mentoring program on youth with LD/ADHD in a design with two control groups. Implications for research and practice involving LD, ADHD, and mental health disorders are discussed.
Introduction
Learning disabilities (LD) and attention-deficit hyperactivity disorder (ADHD) are two high-incidence neurodevelopmental disorders, each occurring in approximately 5% of the population (American Psychiatric Association, 2013). LD and ADHD are typically diagnosed in childhood, are neurobiological in origin, and often co-occur (Hendren, Haft, Black, White, & Hoeft, 2018). The defining feature of LDs are impairments in reading, math, and/or writing that are unexpected given an individual’s instructional background and intelligence (American Psychiatric Association, 2013). ADHD involves a pattern of symptoms in the areas of inattention and/or hyperactivity-impulsivity, often with deficits in executive function (American Psychiatric Association, 2013). Both LDs and ADHD (hereafter LD/ADHD to refer to children with LD, ADHD, or both) pose significant barriers in academics, and if left untreated, can result in reduced occupational opportunities and quality of life in adulthood (Klassen, Tze, & Hannok, 2013).
In addition to academic challenges, youth with LD/ADHD are at risk for socio-emotional maladjustment. These youth often feel less connected to their peers (Bryan, Burstein, & Ergul, 2004), and are more likely than their classmates to experience feelings of loneliness (Margalit & Al-Yagon, 2002). These and other experiences commonly associated with the disorders, such as academic setbacks and stigma, may lead to negative perceptions about the self. Research has found that individuals with LD/ADHD have lower self-esteem than their peers (Burden, 2008; Harpin, Mazzone, Raynaud, Kahle, & Hodgkins, 2016; Mugnaini, Lassi, La Malfa, & Albertini, 2009; Singer, 2005, but see Terras, Thompson, & Minnis, 2009). This impaired self-esteem may in turn become a risk factor for developing additional mental health disorders (Burden, 2008; Elbaum & Vaughn, 2001; Terras et al., 2009). Indeed, youth with LD/ADHD have higher rates of both anxiety (Becker, Luebbe, Stoppelbein, Greening, & Fite, 2012; Mugnaini et al., 2009; Nelson & Harwood, 2011) and depression (Becker et al., 2012; Maag & Reid, 2006) compared to their counterparts without a diagnosis.
The socio-emotional and mental health risks associated with LD/ADHD bring serious consequences. Socio-emotional maladjustment may exacerbate problems with executive function and inattention in this population, setting in motion a vicious cycle between cognitive and emotional difficulties (Habib & Naz, 2015; Lima, Azoni, & Ciasca, 2011). Additionally, research has suggested that youth with LD/ADHD may be at increased risk for suicidal thoughts and attempts (McBride & Siegel, 1997; Giupponi et al., 2018; James, Lai, & Dahl, 2004; Svetaz, Ireland, & Blum, 2000).
Given the far-reaching impacts of LD/ADHD, there has been increasing interest in interventions that build socio-emotional resources and protect mental health in this population (e.g. Firth, Frydenberg, Steeg, & Bond, 2013; Haydicky, Wiener, Badali, Milligan, & Ducharme, 2012; Kotzer & Margalit, 2007). One promising type of intervention observed in youth without LD/ADHD is mentoring programs. Several meta-analyses have found improvements in behavioral and socio-emotional outcomes in youth who participate in mentoring programs compared to non-mentored youth (DuBois, Portillo, Rhodes, Silverthorn, & Valentine, 2011; Eby, Allen, Evans, Ng, & DuBois, 2008; Tolan, Henry, Schoeny, Lovegrove, & Nichols, 2014). Peer mentoring has also shown success in youth with medical or clinical conditions, such as diabetes, physical disabilities (Rabiee, Knowles, & Priestley, 2001), and cancer (Rini et al., 2007). Theorists propose that mentoring influences these outcomes by providing positive interpersonal relationships for social support and modelling adaptive strategies for emotion regulation (Rhodes, Spencer, Keller, Liang, & Noam, 2006). Programs are found to be most effective when mentors are formally trained (Allen, Eby, & Lentz, 2006), mentoring is regular and frequent (Eby, 2012), and mentors and mentees are matched based on a shared interest (DuBois et al., 20l1).
Existing studies on youth with LD/ADHD specifically suggest positive influences of mentoring on self-esteem (Ahrens, DuBois, Lozano, & Richardson, 2010; Buckner, 1993; Shevitz, Weinfeld, Jeweler, & Barnes-Robinson, 2003), and interpersonal relationships (Muscott & O’Brien, 1999; Noll, 1997; Welkowitz & Fox, 2000). However, this research is sparser and has methodological limitations including small sample sizes (typically <30), lack of pre-test data, lack of standardized and quantitative measurements, and absence of a non-mentored LD/ADHD control group as well as non-mentored control group without LD/ADHD. One exception to these limitations is a study by (Ahrens et al., 2010), which evaluated the impact of naturally acquired mentoring relationships in a large sample of youth with LD (N=1,714) compared to non-mentored controls. In this study, youth were considered mentored when they answered “yes” to a question about having an adult in his or her life who made a significant positive difference. Authors found that mentored youth reported greater self-esteem and were more likely to graduate from college than non-mentored controls. However, the study did not investigate or control for characteristics of mentorship, such as content of mentoring, quality or formal vs. informal mentorships, nor did it include youth with LD with comorbid disorders such as ADHD. Although this research suggests mentoring is a promising intervention for youth with LD/ADHD, given the self-report nature of Ahrens et al.’s assessment of mentorship, the authors cautioned that “we cannot draw firm conclusions in terms of causality.”
In summary, programs such as mentoring are needed to address the detrimental socio-emotional consequences of LD/ADHD, and there is a gap in the literature on controlled, quantitative studies examining such programs. The aim of the present study is to address this gap by evaluating the impact of a mentoring program on socio-emotional and mental health outcomes of youth with LD/ADHD. We specifically examine interpersonal relationships, self-esteem, anxiety, and depression, since these variables have been shown to be associated with mentoring or with the experience of LD/ADHD. We compare the outcomes of three groups pre- and post- mentoring from similar communities: mentored youth with LD/ADHD (“Mentored”), non-mentored youth with LD/ADHD (“Control-NM”), and non-mentored youth without LD/ADHD (“Control-TD”). First, we examined differences in measures between youth with and without LD/ADHD at baseline. We hypothesized that youth with LD/ADHD might show lower scores on self-esteem and interpersonal relationships and higher scores on anxiety and depression compared to their non-LD/ADHD counterparts, in line with previous literature. Next, we examined the impact of the mentoring program on collected outcomes by comparing the three groups at two timepoints pre- and post- mentoring. We expected the largest positive changes to occur in the mentored group in the domains of self-esteem and interpersonal relationships, as previous studies have found. Finally, we investigated associations between significant changes and mentee-rated mentorship quality.
Methods
Intervention
The mentoring program being evaluated was Eye to Eye, a national organization that pairs elementary and middle school youth with LD/ADHD with mentors in high school or college who also have LD/ADHD (“near-peer” mentoring; eyetoeyenational.org).
Selection of schools
The Eye to Eye program is implemented in chosen schools, termed “mentee schools.” These mentee schools are chosen based on the number of students reported to have individualized education plans (IEPs) or enrollment in special education because of a diagnosis of LD/ADHD. Eye to Eye researches these school statistics online using data available at the district/state level. The program is then discussed with a school administrator (typically the principal). If the school administrator is interested in the program, Eye to Eye then finds a “mentor school” by contacting special education teachers or disability service offices at local high school or colleges.
Selection and diagnosis of mentees
Once mentee schools are selected, the special education staff at that school generate a list of students who fit the requirements of having a diagnosis of LD, ADHD, or comorbid LD/ADHD, using school documentation of 504 plans, IEPs, and associated neuropsychological reports. Special education staff then reach out to the parents of this list of students about the Eye to Eye program, and distribute a sign-up for the program as well as answer questions. If parents choose to enroll their student in the program, they are required to self-report their child’s LD/ADHD, as well as have documentation on file with the school confirming a diagnosis of LD, ADHD, or comorbid LD/ADHD. Once this confirmation of diagnosis is received and reviewed by Eye to Eye program coordinators and school staff, the mentee student is accepted into the program.
Selection and training of mentors
Once mentor schools are selected, the special education staff or disability service office at the school generate a list of students who fit the requirements of having a diagnosis of LD, ADHD, or comorbid LD/ADHD, using school documentation of 504 plans and IEPs. This list of students then receives information about the Eye to Eye mentoring program and a link to an application form to be a mentor for Eye to Eye. Mentors are required to: (a) have a diagnosed LD/ADHD, confirmed by school documentation, (b) pass a criminal history background check, (c) complete the mentor application form and mentor agreement, (d) be between the ages of 16–32 years old, and (e) complete mentor training with a member of Eye to Eye’s national staff. Mentors are trained in-person by program coordinators from Eye to Eye. The training is several hours and performed on-site at mentor schools, with information pertaining to the Eye to Eye curriculum, program objectives and art projects, conversations about LD/ADHD, and characteristics of an effective mentor. Moreover, each group of mentors has a designated student leader that runs and facilitates the program at the mentor school. These students are selected from an interview process with Eye to Eye, and are required to attend an intensive 5-day training on the campus of Brown University. This training provides structured educational and community building activities, reviews in-depth each program objective and associated activity, and strengthens understanding of LD/ADHD.
Program curriculum
The mentoring program mirrors the academic school year, with the first session occurring in fall and the last session concluding in spring, with a total of 18 sessions. Each week, a group of mentees at schools with Eye to Eye meets with the group of mentors in an after-school program. During this time, the mentors use art projects and activities with specific socio-emotional objectives to discuss strengths and challenges associated with LD/ADHD and develop relationships with mentees. This curriculum and socio-emotional objectives were initially developed by a team of educators with LD/ADHD, a focus group of young adults with LD/ADHD, and faculty, staff, and graduate and post-doctoral students at Brown, Harvard, and Columbia Universities. Objectives were also determined from research on a seminal longitudinal study that identified success attributes of individuals with LD/ADHD (Raskind, Goldberg, Higgins, & Herman, 1999). The curriculum revolves around using art projects to reinforce these discrete socio-emotional objectives, since art projects do not require reading, writing, or calculating, which can induce frustration in LD/ADHD students. One example of an art project is for mentees to use art materials to create a box of their “ideal learning environment,” and discuss the contexts in which they become distracted or learn best. Other project examples include: a superhero project designed to surface and celebrate individual strengths, a utility belt project to identify and promote accommodations, a self-advocacy tower project to practice the building blocks of self-advocacy, a parachute project to develop growth mindset and promote positive self-concept, and more. For more information on the Eye to Eye curriculum, email Mentoring@eyetoeyenational.org.
Participants and Procedure
This study analyzed data from a total of 234 children and adolescents (56.4% male; mean age=11.79 years, range=8–16 years). Of these, 99 were youth with LD/ADHD in the mentored group (“Mentored”) participating in the program Eye to Eye, described in the “Intervention” section below. There were 51 participants with LD/ADHD not in the mentoring program (“Control-NM”), and 84 typically-developing (“Control-TD”) participants without any LD/ADHD diagnosis. Participant characteristics are summarized in Table 1.
Table 1.
Comparison of participant groups on demographic measures, extracurricular activities, and counseling services.
| Mentored (n=99) | Control-NM (n=51) | Control-TD (n=84) | Test of group differences | |
|---|---|---|---|---|
| Age in years (M, SD) | 11.97 (1.25) | 12.06 (1.86) | 11.52 (1.87) | p=.099 |
| Biological sex (% male) | 59.6% | 54.9% | 53.6% | p=.694 |
| Race (% nonwhite) | 52.5 % | 35.3% | 39.3% | p=.073 |
| Family Affluence Scale (0–8) | 6.12 (1.81) | 5.86 (1.61) | 7.52 (0.81) | p<.005 |
| # of Extracurricular Activities (M, SD) | 2.08 (1.22) | 1.84 (1.42) | 1.88 (0.92) | p=.380 |
| Counseling Services (% receiving) | 10.1% | 17.6% | 6.0% | p=.094 |
At the time of this study, the mentoring program was implemented in approximately 109 schools. We then determined that to have adequate power and maintain our research budget, we would choose 18 of these schools to participate in the present research. We chose these schools to specifically represent a range of socioeconomic status, geographic regions, and school type (private, public, or charter). The Mentored group was recruited from the pool of families who had signed up to participate in Eye to Eye in these schools, before the mentoring program had started. School counselors sent these families flyers advertising our study in the summer before the academic school year – families then indicated their interest, and were consented to participate in the study as part of the Mentored group.
Due to ethical concerns in withholding mentoring from certain LD/ADHD students, randomization was not used to assign individuals to a mentored or non-mentored group. Instead, the Control-NM and Control-TD groups were recruited through advertisements distributed in schools and organizations in communities similar to those of the Mentored group. Specifically, we reached out to schools who did not have the implemented mentoring program, but were within the same district or geographic region of a school with the mentoring program. We asked school teachers and administrators to distribute flyers advertising our study to families, and parents contacted us if they were interested in participating. Inclusion criteria included any age between 8 and 16, ability to read and understand English, and no self-reported or diagnosis of a neurodevelopmental or major psychiatric disorder (besides LD/ADHD for the Mentored and Control-NM groups). Diagnoses of LD/ADHD were verified for the Control-NM group by both school documentation of an IEP or 504 plan, by parental report that students had received a diagnosis, and by students themselves. Participants were excluded from the Control-NM and Control-TD groups if they indicated any participation in a formal mentorship program. All participants provided informed consent for all aspects of the study.
Participants were assessed on measures through self-report questionnaires administered online. There was an audio option available for questions to be read to the participant from a recording. The survey was administered once at the beginning of the academic school year, and again at the end of the school year (pre- and post- mentoring for the Mentored group). The average time between survey administrations was 7.64 months (range: 6.93–8.27 months). The order of questions was randomized for each participant. Demographic information was collected from participants on the online questionnaire and verified from surveys given to parents of participants.
Outcome Measures
All outcome measures collected (anxiety, depression, interpersonal relations, and self-esteem) were self-report scales from the Behavior Assessment System for Child Second Edition (BASC-2; Reynolds & Kamphaus, 2004). BASC-2 is widely used to assess behavioral and emotional issues in children. Test-retest reliability for all scales was between .70–.80. The BASC-2 has shown construct, convergent, and discriminant validity – scales were correlated with similar self-report measures such as the Revised Children’s Manifest Anxiety Scale, Brief Symptom Inventory, Beck Depression Inventory-II, and Minnesota Multiphasic Personality Inventory.
The anxiety scale asks participants questions about how frequently they have worrisome thoughts or feelings of fear. This scale has excellent reliability for both children and adolescents (coefficient alpha = .86).
The depression scale assesses typical symptoms of depression, such as sadness and feelings of hopelessness, loneliness, or loss of enjoyment. Coefficient alpha of this scale for children and adolescents is .84 and .88 respectively, indicating excellent reliability.
The interpersonal relations scale asks the participant to report on how successful they feel regarding relating to others and how much they enjoy these interactions. This scale has good reliability for both children and adolescents (coefficient alpha = .81 and .79 respectively).
The self-esteem scale is a measure of global self-worth and measures whether a participants’ sense of their identity is more positive or negative. This scale has good reliability as indicated by coefficient alphas of .77 and .83 respectively for children and adolescents.
Covariates and Demographics
Family affluence was measured from the Family Affluence Scale II (FAS-II; Boudreau & Poulin, 2009), which measures the degree of material resources available to the family by asking about vacations, and car and computer ownership. Previous studies have found that the FAS-II reduces the rate of nonresponse, and has convergent validity with other measures of socioeconomic status, such as maternal education (Boudreau & Poulin, 2009). We modified the original scale by removing a question about number of bedrooms, given that some studies have indicated this item is the least indicative of the FAS-II items (e.g. Kehoe & O’Hare, 2010). Higher scores on the FAS-II indicate higher family affluence, a metric of socioeconomic status.
Mentorship quality was measured from a modified version of the Quality of Mentoring Relationship Engagement Scale (Q-MRES). This measure asks mentees to rate how true certain positive statements are of their mentors (e.g. asking for opinions, sharing interests). Questions which were not relevant to the present study and its mentorship program were removed (e.g. “my mentor calls me on the telephone often.”). The Q-MRES has shown good reliability in previous studies (coefficient alpha = .88) as well as convergent validity with another mentoring relationship scale (Ferro, Wells, Speechley, Lipman, & DeWit, 2014). This measure was only collected with the Mentored group.
Demographic and diagnosis information such as age, gender, and type of LD/ADHD diagnosis was collected through questionnaires given to both participants and their parents. This questionnaire also asked about the number of extracurricular activities as a potential covariate.
Analytic Approach
Differences between groups on demographics and diagnoses were investigated using χ2 tests and one-way analysis of variance (ANOVA). To investigate baseline differences between participants with and without LD/ADHD, the scores from the Mentored and Control-NM groups were combined and compared to the Control-TD group in an analysis of covariance (ANCOVA). We controlled for family affluence given group differences in this measure. To examine the impact of the mentoring program, two-way mixed ANCOVAs were conducted to determine if there was an interaction between group (Mentored, Control-NM, and Control-TD) and time (pre- and post) on outcome variables, controlling for family affluence. Significant interactions were probed with follow-up ANCOVAs and repeated measure ANOVAs to test for simple main effects. A reliable change index (RCI) was computed as an indicator of change over time for variables with significant changes over time for the Mentored group. The RCI involves dividing the discrepancy between scores at two timepoints by the standard error of the difference (Duff, 2012). Associations between the RCI and mentorship quality were investigated through linear regression.
Missing data was determined to be missing at random. Due to clicking the next button in rapid succession, some pages of question blocks were accidentally skipped by a few participants (as determined by observing the time spent on each page). The percentage of data that is missing for key outcome variables in the overall sample is small: 1.9% of anxiety scores, 2.1% of depression scores, 1.7% of interpersonal relations scores, and 1.9% of self-esteem scores. No group had more than 3% of data missing for any variable. To address missing data, listwise deletion was used.
Results
Participant Characteristics
Participant characteristics and group differences are summarized in Table 1. There were no significant differences between groups in terms of age, gender, race, or number of extracurricular activities (all ps>.05). There was a significant group difference in family affluence (F(2,234)=28.285, p<.005), with the Control-TD group reporting higher family affluence than both the Mentored (p<.005) and Control-NM (p<.005) groups. There was no difference in family affluence between the Mentored and Control-NM groups. The type of diagnoses of the ADHD/LD participants is displayed in Table 2. There were no group differences in composition of diagnoses when categorized as ADHD only, LD only, or comorbid LD/ADHD.
Table 2.
Count and frequency of diagnoses for Mentored and Control-NM groups (all youth with LD/ADHD).
| Mentored (n=99) | Control-NM (n=51) | Test of group differences | |
|---|---|---|---|
| ADHD only | 21 (21.2%) | 9 (17.6%) | p=.605 |
| LD only | 39 (39.4%) | 25 (49.0%) | p=.259 |
| RD | 29 | 15 | |
| MD | 1 | 0 | |
| WD | 0 | 1 | |
| Multiple LD | 9 | 9 | |
| ADHD + LD | 29 (29.3%) | 12 (23.5%) | p=.453 |
| ADHD+ RD | 19 | 8 | |
| ADHD + MD | 0 | 0 | |
| ADHD + WD | 0 | 0 | |
| ADHD + Multiple LD | 10 | 4 | |
| Prefer Not to Disclose | 10 (10.1%) | 5 (9.8%) | p=.954 |
Note. RD=reading disorder, MD=mathematics disorder, WD=writing disorder
We also investigated differences in the number of individuals receiving counseling services in each group. By “counseling services,” we refer to personal therapy that is not related to academics, speech, or language (e.g. school, community, or private practice psychological services or mental health treatment). There were 10 individuals in the Mentored group (10.1%), 9 individuals in the Control-NM group (17.6%), and 5 individuals in the Control-TD group (6.0%) receiving counseling services – not a significant difference by group (p=.094).
Baseline Differences Based on LD/ADHD Diagnosis
Differences in baseline scores controlling for family affluence between youth with and without LD/ADHD are displayed in Table 3. Scores reported are unadjusted means and standard deviations. For anxiety and depression, scores are interpreted as within normal limits (<60), at-risk (60–69), or clinically significant (≥ 70) – for all groups, mean scores were within normal limits. There were no significant baseline differences between the two groups in either anxiety or self-esteem. There was a significant group difference in depression with participants with LD/ADHD reporting higher depression scores than the Control-TD group (F(1,288)=5.372, p=.029), although this difference was not significant at an alpha level corrected for multiple comparisons (α=.013). The score of participants with LD/ADHD on interpersonal relations at baseline was significantly lower than that of the Control-TD group at an alpha-corrected level (F(1,228)=18.873, p<.005). When separated out by diagnosis (ADHD only, LD only, comorbid ADHD+LD), there were no significant group differences on anxiety, depression, interpersonal relations, self-esteem, or demographic information by diagnostic group (all ps >.05; Supplementary Table 1).
Table 3.
Baseline comparison of scores based on LD/ADHD diagnosis, with tests of group differences controlling for family affluence.
| LD/ADHD (Mentored + Control-NM) | Non-LD/ADHD (Control-TD) | Test of group differences | |
|---|---|---|---|
| Anxiety | 53 (11.76) | 50 (8.52) | p=.226 |
| Depression | 51 (11.08) | 46 (7.12) | p=.029 |
| Interpersonal Relations | 47 (11.34) | 56 (4.87) | p<.005 |
| Self-Esteem | 50 (11.47) | 50 (8.30) | p=.856 |
Impact of Mentoring on Outcome Variables
The mean scores of outcome variables for each group at each timepoint are displayed in Figure 1. Significance is evaluated at an alpha level corrected for multiple comparisons (α=.013). For ease of interpretation, we also computed effect size (d) of the mentoring intervention for the Mentored group compared to the Control-NM and Control-TD groups separately, displayed in Table 4.
Figure 1.
Scores of mentored youth with LD/ADHD (Mentored), non-mentored youth with LD/ADHD (control-NM), and their typically-developed (control-TD) peers on outcome measures of (a) anxiety, (b) depression, (c) interpersonal relations, and (d) self-esteem in fall (pre-mentoring) and spring (post-mentoring).**=p<.01, ***=p<.005
Table 4.
Effect size (d) of the mentoring intervention on changes in outcomes of interest (anxiety, depression, interpersonal relations, self-esteem) for the Mentored group, compared separately to the Control-NM and Control-TD groups. Effect size is calculated as mean pre-post change in the Mentored group minus the mean pre-post change in the control group, divided by the pooled pretest standard deviation (Morris, 2008).
| Effect Size Compared to Control-NM Group (d) | Effect Size Compared to Control-TD Group (d) |
|
|---|---|---|
| Anxiety | .02 | −.14 |
| Depression | −.75*** | −.38** |
| Interpersonal Relations | 44** | .32 |
| Self-Esteem | 87*** | .25 |
=p<01
=p<.005
There was a statistically significant group by time interaction on depression with family affluence as a covariate (Figure 1b; F(2,221)=15.221, p<.005, partial η2=12). There was a significant main effect of group in fall (F(2,221)=5.108, p=.007, partial η2=04), with the Control-TD group reporting lower scores of depression than the Mentored group (p=.013). Depression scores of the Control-NM group were not significantly different from either the Control-TD or Mentored groups. In spring, there was also a significant main effect of group (F(2,221)=6.649, p=.002, partial η2=06), with the Control-NM group scoring significantly higher on depression than both the Mentored (p=.007) and Control-TD (p=.002) groups. There was no significant difference between the Mentored and Control-TD group in spring. There was a significant main effect of time for the Mentored group (F(1,95)=19.326, p<.005, partial η2=17), with depression scores decreasing significantly from Fall to Spring. There was also a significant main effect of time for the Control-NM group in the opposite direction (F(1,48)=8.665, p=.005, partial η2=15), with depression scores significantly increasing from fall to spring. There was no effect of time for the Control-TD group. Overall, the results showed that the Mentored group significantly increased while the Control-NM group significantly decreased in depression over time, while the Control-TD group remained the same. There was a group difference in depression scores between the Mentored and Control-TD group in Fall, but not in Spring.
There was a statistically significant group by time interaction on interpersonal relations with family affluence as a covariate (Figure 1c; F(2,223)=10.841, p<.005, partial η2=09). In Fall, there was a significant main effect of group (F(2,223)=9.690, p<.005, partial η2=08), with the Control-TD group scoring significantly higher on interpersonal relations than both the Mentored (p<.005) and Control-NM (p=.004) groups. There was no significant difference in Fall between the interpersonal relations scores of the Mentored and Control-NM groups. There was also a significant main effect of group in Spring (F(2,223)=18.670, p<.005, partial η2=14), with the Control-NM group scoring significantly lower on interpersonal relations than both the Control-TD and Mentored groups (both ps<.005). There was a trend-level significant difference between the Mentored and Control-TD groups on interpersonal relations in spring (p=.032). There was no main effect of time on interpersonal relations scores for the Mentored group (F(1,95)=2.904, p=.092, partial η2=03). There was a significant main effect of time for both the Control-NM (F(1,47)=8.488, p=.005, partial η2=15) and Control-TD (F(1,82)=10.600, p=.002, partial η2=11) groups, with interpersonal relations scores of both groups significantly decreasing from Fall to Spring. Overall, results showed a decrease in interpersonal relations scores of both the Control-NM and Control-TD groups, but no change in the Mentored group, with the Control-NM group scoring significantly lower than the Control-TD group in both Fall and Spring.
There was no statistically significant interaction between group and time on anxiety with family affluence as a covariate (Figure 1a; F(2,221)=0.509, p=.602, partial η2=01).
There was a statistically significant group by time interaction on self-esteem with family affluence as a covariate (Figure 1d; F(2,222)=21.273, p<.005, partial η2=16). There was no main effect of group in Fall (F(2,222)=1.581, p=.208). In Spring, there was a significant main effect of group (F(2,222)=8.845, p<.005), where the Control-NM group scored significantly lower on self-esteem than the Mentored group (p<.005), and marginally lower than the Control-TD group (p=.017). There was no significant difference in self-esteem scores between the Mentored and Control-TD group in Spring. There was a main effect of time on self-esteem scores for the Mentored group (F(1,97)=9.970, p=.002, partial η2=09) where self-esteem scores significantly increased over time, and for the Control-NM group (F(1,46)=38.089, p<.005, partial η2=45) where self-esteem scores significantly decreased over time. There was no effect of time on self-esteem scores for the Control-TD group. Overall, the results showed that the Mentored group significantly increased while the Control-NM group significantly decreased in self-esteem over time, and the Control-TD group remained the same. There Mentored group reported significantly lower self-esteem than the Control-TD group in the Spring, but not in Fall.
Association of Changes with Perceived Mentorship Quality
Visual inspection of plots indicated a linear relationship between variables. Mentee-perceived mentorship quality significantly predicted change in depression (F(1,95)=3.989, p=.049), and change in self-esteem (F(1,97)=6.994, p=.010). Although these associations were significant, the proportion of variance in depression and self-esteem explained was low – 4.2% and 7.1% respectively.
Discussion
This study examined differences in depression, interpersonal relations, anxiety, and self-esteem among youth with and without LD/ADHD, as well as the impact of mentoring on these variables. Most of the hypotheses were supported by the findings. The study is the first to our knowledge to quantify the effect of a near-peer mentoring program on socio-emotional and mental health outcomes of youth with LD/ADHD in a controlled design. Results suggest baseline socio-emotional differences between youth with and without LD/ADHD, but show that mentoring can positively impact depression, self-esteem, and interpersonal relations.
In line with our hypothesis, youth with LD/ADHD reported significantly higher depression scores than the Control-TD group at Fall baseline. Previous studies have also found higher symptoms of depression in youth with LD/ADHD compared to their peers without LD/ADHD (Mammarella et al., 2016; Mugnaini et al., 2009; Willcutt & Pennington, 2000). Although some research has shown a modest genetic contribution to this comorbidity (Willcutt, 2014), the majority of studies highlight the role of environmental factors. Depression in youth with LD/ADHD has been hypothesized to result from experiences associated with LD/ADHD, such as academic failure (Willcutt & Pennington, 2000), peer victimization (Baumeister, Storch, & Geffken, 2008), or as a byproduct of low self-esteem (Sitthimongkol & Apinuntavech, 2012). If left unaddressed, depressive symptoms in youth with LD/ADHD can continue into adulthood (Klassen et al., 2013).
Youth with LD/ADHD also had significantly lower scores on interpersonal relations than their Control-TD counterparts. This is in line with previous studies showing associations between LD/ADHD and poor peer relationships (Al-Yagon, 2016; Hoza et al., 2005; Parhiala et al., 2015; Pearl & Donahue, 2004). These social difficulties may arise as a result of deficits in encoding and processing social information observed in some children with LD/ADHD (Al-Yagon & Margalit, 2013; Parhiala et al., 2015). Internalizing and externalizing problems that frequently co-occur with LD/ADHD may also make social relationships difficult to maintain. Indeed, stigmatization (Lebowitz, 2016; Lisle & Wade, 2013) and bullying from peers (Baumeister et al., 2008; Rose, Espelage, Monda-Amaya, Shogren, & Aragon, 2015; Roy, Hartman, Veenstra, & Oldehinkel, 2015) have been shown to accompany LD/ADHD. Regardless of whether peer stigmatization is actually present, youth with LD/ADHD may be self-conscious of the stigma associated with their diagnosis (May & Stone, 2010; Shifrer, 2013), and so may be less likely to seek out friendships.
Contrary to our hypothesis, youth with LD/ADHD did not show significantly higher anxiety scores than the Control-TD group. This is in contrast to some previous studies showing higher anxiety in this population relative to controls (Nelson & Harwood, 2011). Because the LD/ADHD population in our sample was identified through school settings rather than clinics or hospitals, the severity of LD/ADHD – and therefore level of anxiety – may have been less than in other studies. Another possibility is that anxiety in youth with LD/ADHD is more domain-specific, which was not measured by our anxiety assessment. For example, children with math LD have been shown to have a specific negative affective response to math (mathematics anxiety; Rubinsten & Tannock, 2010), which is related to, but distinct from, general anxiety (Suarez-Pellicioni, Nunez-Pena, & Colome, 2016). Of note, we assessed anxiety on a dimensional rather than categorical approach. Our results may have been different if we conducted a clinical, dichotomous assessment of anxiety and compared the two groups.
Youth with LD/ADHD in our sample also did not show significantly lower self-esteem scores than their Control-TD peers at baseline. There are mixed findings in the literature on self-esteem in this population, with some studies finding lower self-esteem in youth with LD/ADHD (e.g. Burden, 2008; Harpin, Mazzone, Raynaud, Kahle, & Hodgkins, 2016), and some research showing no deficit (e.g. Terras et al., 2009). One explanation for this in our sample may be that the experience of academic failure leads to low self-esteem in this group. Therefore, at Fall baseline before the start of school, given presence of non-academic activities in summer, the self-esteem of youth with LD/ADHD remains intact. This finding may also be due to positive illusory bias, where individuals hold overly positive appraisals of themselves and their abilities which are discrepant with actual competencies (Owens & Hoza, 2003). The positive illusory bias is commonly reported in individuals with ADHD (Owens, Goldfine, Evangelista, Hoza, & Kaiser, 2007), and may lead to higher-than-expected reports of self-esteem. There are mixed opinions on whether positive illusions are maladaptive or are instead an adaptive self-protective mechanism (Heath & Glen, 2005).
Our findings showed that depression for the Mentored group decreased significantly post-mentoring so that there were no longer any group differences between the Mentored and Control-TD group in spring. By contrast, the Control-NM group reported significantly more depressive symptoms in Spring than in Fall, which were then significantly higher than both the Mentored and Control-TD groups. This same pattern was observed for self-esteem – the Mentored group significantly increased over time, whereas the Control-NM group significantly decreased. In both depression and self-esteem scores, the Control-TD group remained stable over time. These results suggest overall that the near-peer mentoring had a positive impact in reducing depressive symptoms and boosting self-esteem for youth with LD/ADHD. The increase in self-esteem has been observed in other studies as a consequence of mentoring for youth with LD/ADHD (Ahrens et al., 2010; Buckner, 1993; Shevitz et al., 2003). Although research on mechanisms of this impact is limited, mentoring may impact self-esteem by providing social support through challenges and correcting negative views youth may hold about themselves (Erdem, DuBois, Larose, De Wit, & Lipman, 2016; Rhodes et al., 2006). Further, this increase in self-esteem may be related to the observed decreases in depressive symptoms reported in the Mentored group post-mentoring. Mediational models in youth without LD/ADHD have shown that mentoring decreases levels of depression and other emotional issues via increasing youth confidence and self-esteem (Erdem et al., 2016; Hurd, Albright, Wittrup, Negrete, & Billingsley, 2018). We could not investigate mediating models of mentoring with two time-points in the present study, but recognize this as an area of future research for youth with LD/ADHD.
The interpersonal relations scores of the Mentored group increased over time, but this increase was not significant. However, the Control-NM group ratings of interpersonal relations significantly decreased over time. These results suggest that mentoring might have a protective effect on interpersonal relations, preventing a decrease in interpersonal relations that might otherwise occur in youth with LD/ADHD. Indeed, the significant decrease that occurred in the Control-NM group in interpersonal relations and self-esteem, and the significant increase in depression are striking. As previously mentioned, youth with LD/ADHD have been shown to have impairments in self-esteem (Burden, 2008), interpersonal relations (Bryan et al., 2004), and depressive symptoms (Maag & Reid, 2006) in prior literature. Our results raise the question of whether this maladjustment is exacerbated by negative environmental experiences in school (e.g. academic failure, peer rejection).
The finding that changes in self-esteem and depression were significantly predicted by mentee-perceived mentorship quality further supports the idea that mentoring played a role in these positive changes. These findings suggest that the perceived quality of the mentoring relationship – and not just the mentoring content – is important in the mentoring impact. However, although significant, the total variance in depression and self-esteem predicted by mentorship quality is relatively low – 4.2% and 7.1% respectively. This suggests that there are a number of other factors related or unrelated to mentoring that may be influencing these changes, and future studies should include more detailed measurements of these factors (e.g. observations of conversation quality, mentor-perceived quality, number of hours spent with mentor, number of other significant relationships, etc.).
Several limitations of this study should be acknowledged. First, youth with LD/ADHD were not randomized into a mentoring or non-mentoring group due to ethical concerns. Instead, efforts were made to recruit the Control-NM group from neighboring schools without implemented Eye to Eye mentoring programs to minimize intergroup differences. Still, we acknowledge that there may be a form of selection bias where participants in the mentoring program were more impaired than the comparison group in socio-emotional variables at baseline. We did not observe this pattern in our data, but recognize that differences may have occurred in domains that we did not assess. Second, we relied on self-report data to collect information on socio-emotional and mental health outcomes. Because we were interested in the perceptions of the individuals, this was an appropriate choice for our purposes. However, we acknowledge that accuracy of self-report scales may be hindered by a “social desirability response bias,” where participants underreport negative symptoms to present themselves more favorably (Van de Mortel, 2008). If true, this means that we may be underestimating impairment in the youth with LD/ADHD at baseline. Future studies might consider implementing other tools to index socio-emotional variables, such as emotion tasks, psychophysiology, or teacher- or parent- reports. Third, the aim of the present study is to provide information on the impact of mentoring, but not provide mechanistic accounts. Because our data consists of two timepoints, we are restricted in our ability to test mediational models between variables. A future direction for this line of research might be to collect data at multiple timepoints and further characterize the mentoring relationship to inform models of mentoring mechanisms. Additionally, future studies might consider investigating the impact of mentoring in a wider age range, or deploying an “active” control group (e.g. individuals that participate in the curriculum but without the presence of mentors). Finally, we did not separately verify diagnoses of LD/ADHD through neuropsychological testing or scale ratings. The diagnoses of all participants in the Mentored or Control-NM were confirmed through 3 sources: school documentation, parent report, and student report. Still, we recognize that there is a chance of misdiagnosis in these participants and their current symptom severity cannot be confirmed.
In summary, the present study echoes prior research in highlighting the socio-emotional and mental health challenges faced by youth with LD/ADHD. In our sample, youth with LD/ADHD showed significantly higher depression and lower perceptions of interpersonal relations than their peers without LD/ADHD at baseline. Moreover, without the support of mentoring, youth with LD/ADHD exhibited significantly more impairments in self-esteem, interpersonal relations, and depression at the end of the academic year. Our study contributes new knowledge in quantifying the impact of a potential intervention to address this maladjustment: near-peer mentoring. The youth with LD/ADHD who participated in mentoring significantly increased in self-esteem and decreased in depression after participating in the program, and were protected from declines in interpersonal relations that occurred in their non-mentored LD/ADHD peers. Effect sizes of mentoring for the Mentored group compared to the Control-NM group were large for self-esteem and depression (d=.87 and .75 respectively), and medium (d=.44) for interpersonal relations. These effect sizes are larger than for other youth mentoring programs (both with and without LD/ADHD), which are generally reported to be small to medium for self-esteem and psychological outcomes (Ahrens et al., 2010; Eby et al., 2008). The changes in self-esteem and depression were related to mentee-perceived mentorship quality, and appeared to be significant regardless of gender, age, family affluence, and relationship with parents. The present study has implications for educators, parents, and clinicians in considering the emotional sequelae of youth with LD, ADHD, and other related neurodevelopmental disorders. Given the observed consequences such as suicide, mental health disorders, or poor functioning in adulthood if left unaddressed, interventions to address the socio-emotional side of LD/ADHD should be a focus of research and practice. Our results suggest near-peer mentoring is one promising intervention to address this need, and that socio-emotional variables are malleable to positive change in socially supportive contexts for youth with LD/ADHD.
Supplementary Material
Key Practitioner Message.
LD and ADHD are associated with increased anxiety, depression, and impaired self-esteem and interpersonal relationships.
There is a lack of research on interventions that could address the mental health problems and socio-emotional difficulties that co-occur with learning disabilities and ADHD.
Near-peer mentoring is a promising intervention that can improve socio-emotional well-being and mental health in youth with learning disabilities and ADHD, and highlights the importance of strong interpersonal relationships as a protective factor.
Acknowledgements
This work was funded by Oak Foundation ORIO-16–012. Author FH was additionally funded by NICHD R01HD086168, R01HD096261, R01HD078351, P50HD052120 (PI: R. Wagner), National Science Foundation NSF-1540854, University of California Office of the President Multicampus Research Programs and Initiatives Award MRP-17–454925, UCSF Dyslexia Center, Ray & Lori dePole, Dyslexia Training Institute, The Potter Family, ALTA, San Mateo County of Education, IMBES, SfN, Hyde Park Day School, and University of Chicago Laboratory Schools. The authors would like to acknowledge Eye to Eye National for their continued partnership, support and facilitation of this research. FH and SH conceived of and designed the study. FH supervised all study procedures and manuscript writeup. SH conducted data analysis and drafted the manuscript. TC, CL, and FT participated in cleaning the data and organizing it for analysis, as well as offered comments on the manuscript. All authors read and approved the final manuscript. The authors have declared that they have no competing or potential conflicts of interest.
References
- Ahrens K, DuBois DL, Lozano P, & Richardson LP (2010). Naturally Acquired Mentoring Relationships and Young Adult Outcomes Among Adolescents with Learning Disabilities. Learning Disabilities Research & Practice, 25, 207–216. 10.1111/j.1540-5826.2010.00318.x [DOI] [Google Scholar]
- Allen TD, Eby LT, & Lentz E (2006). The relationship between formal mentoring program characteristics and perceived program effectiveness. Personnel Psychology, 59(1), 125–153. [Google Scholar]
- Al-Yagon M (2016). Perceived Close Relationships With Parents, Teachers, and Peers: Predictors of Social, Emotional, and Behavioral Features in Adolescents With LD or Comorbid LD and ADHD. J Learn Disabil. 10.1177/0022219415620569 [DOI] [PubMed] [Google Scholar]
- Al-Yagon M, & Margalit M (2013). Social cognition of children and adolescents with LD: Intrapersonal and interpersonal perspectives In Handbook of learning disabilities (2nd ed., pp. 278–292). New York: Guilford Press. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders, fifth edition (DSM-5) (Fifth Edition). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Baumeister AL, Storch EA, & Geffken GR (2008). Peer victimization in children with learning disabilities. Child and Adolescent Social Work Journal, 25, 11–23. [Google Scholar]
- Becker SP, Luebbe AM, Stoppelbein L, Greening L, & Fite PJ (2012). Aggression among children with ADHD, anxiety, or co-occurring symptoms: Competing exacerbation and attenuation hypotheses. Journal of Abnormal Child Psychology, 40(4), 527–542. [DOI] [PubMed] [Google Scholar]
- Boudreau B, & Poulin C (2009). An examination of the validity of the Family Affluence Scale II (FAS II) in a general adolescent population of Canada. Social Indicators Research, 94(1), 29. [Google Scholar]
- Bryan T, Burstein K, & Ergul C (2004). The social-emotional side of learning disabilities: A science-based presentation of the state of the art. Learning Disability Quarterly, 27(1), 45–51. [Google Scholar]
- Buckner AE (1993). Mediating At-Risk Factors among Seventh and Eighth Grade Students with Specific Learning Disabilities Using a Holistically Based Model.
- Burden R (2008). Is dyslexia necessarily associated with negative feelings of self-worth? A review and implications for future research. Dyslexia, 14, 188–196. [DOI] [PubMed] [Google Scholar]
- DuBois DL, Portillo N, Rhodes JE, Silverthorn N, & Valentine JC (2011). How effective are mentoring programs for youth? A systematic assessment of the evidence. Psychological Science in the Public Interest, 12(2), 57–91. [DOI] [PubMed] [Google Scholar]
- Duff K (2012). Evidence-based indicators of neuropsychological change in the individual patient: relevant concepts and methods. Archives of Clinical Neuropsychology, 27(3), 248–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eby LT (2012). Workplace mentoring: Past, present, and future perspectives. In The Oxford Handbook of Organizational Psychology, Volume 1. [Google Scholar]
- Eby LT, Allen TD, Evans SC, Ng T, & DuBois DL (2008). Does mentoring matter? A multidisciplinary meta-analysis comparing mentored and non-mentored individuals. Journal of Vocational Behavior, 72(2), 254–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbaum B, & Vaughn S (2001). School-based interventions to enhance the self-concept of students with learning disabilities: A meta-analysis. The Elementary School Journal, 101(3), 303–329. [Google Scholar]
- Erdem G, DuBois DL, Larose S, De Wit D, & Lipman EL (2016). Mentoring relationships, positive development, youth emotional and behavioral problems: Investigation of a mediational model. Journal of Community Psychology, 44(4), 464–483. [Google Scholar]
- Ferro A, Wells S, Speechley KN, Lipman E, & DeWit D (2014). The measurement properties of mentoring relationship quality scales for mentoring programs. Prevention Science, 15(5), 663–673. [DOI] [PubMed] [Google Scholar]
- Firth N, Frydenberg E, Steeg C, & Bond L (2013). Coping Successfully with Dyslexia: An Initial Study of an Inclusive School-Based Resilience Programme. Dyslexia, 19(2), 113–130. [DOI] [PubMed] [Google Scholar]
- Giupponi G, Giordano G, Maniscalco I, Erbuto D, Berardelli I, Conca A, … Pompili M (2018). Suicide risk in attention-deficit/hyperactivity disorder. Psychiatria Danubina, 30(1), 2–10. [DOI] [PubMed] [Google Scholar]
- Habib A, & Naz F (2015). Cognitive failure, teacher’s rejection and interpersonal relationship anxiety in children with dyslexia. Pakistan Journal of Medical Sciences, 31(3), 662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harpin V, Mazzone L, Raynaud JP, Kahle J, & Hodgkins P (2016). Long-term outcomes of ADHD: a systematic review of self-esteem and social function. Journal of Attention Disorders, 20(4), 295–305. [DOI] [PubMed] [Google Scholar]
- Haydicky J, Wiener J, Badali P, Milligan K, & Ducharme JM (2012). Evaluation of a mindfulness-based intervention for adolescents with learning disabilities and co-occurring ADHD and anxiety. Mindfulness, 3, 151–164. [Google Scholar]
- Heath NL, & Glen T (2005). Positive illusory bias and the self-protective hypothesis in children with learning disabilities. Journal of Clinical Child and Adolescent Psychology, 34(2), 272–281. [DOI] [PubMed] [Google Scholar]
- Hendren RL, Haft SL, Black JM, White NC, & Hoeft F (2018). Recognizing Psychiatric Comorbidity With Reading Disorders. Frontiers in Psychiatry, 9, 101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoza B, Mrug S, Gerdes AC, Hinshaw SP, Bukowski WM, Gold JA, … Arnold LE (2005). What aspects of peer relationships are impaired in children with attention-deficit/hyperactivity disorder? Journal of Consulting and Clinical Psychology, 73(3), 411. [DOI] [PubMed] [Google Scholar]
- Hurd NM, Albright J, Wittrup A, Negrete A, & Billingsley J (2018). Appraisal support from natural mentors, self-worth, and psychological distress: Examining the experiences of underrepresented students transitioning through college. Journal of Youth and Adolescence, 47(5), 1100–1112. [DOI] [PubMed] [Google Scholar]
- James A, Lai FH, & Dahl C (2004). Attention deficit hyperactivity disorder and suicide: a review of possible associations. Acta Psychiatrica Scandinavica, 110(6), 408–415. [DOI] [PubMed] [Google Scholar]
- Kehoe S, & O’Hare L (2010). The reliability and validity of the Family Affluence Scale. Effective Education, 2(2), 155–164. [Google Scholar]
- Klassen RM, Tze VM, & Hannok W (2013). Internalizing problems of adults with learning disabilities: A meta-analysis. Journal of Learning Disabilities, 46(4), 317–327. [DOI] [PubMed] [Google Scholar]
- Kotzer E, & Margalit M (2007). Perception of competence: risk and protective predictors following an e-self-advocacy intervention for adolescents with learning disabilities. European Journal of Special Needs Education, 22(4), 443–457. [Google Scholar]
- Lebowitz MS (2016). Stigmatization of ADHD: A developmental review. Journal of Attention Disorders, 20(3), 199–205. [DOI] [PubMed] [Google Scholar]
- Lima R. F. de, Azoni CAS, & Ciasca SM (2011). Attentional performance and executive functions in children with learning difficulties. Psicologia: Reflexao e Critica, 24(4), 685–691. [Google Scholar]
- Lisle K, & Wade TJ (2013). Does the presence of a Learning Disability elicit a stigmatization? British Journal of Education, Society & Behavioural Science, 211. [Google Scholar]
- Maag JW, & Reid R (2006). Depression among students with learning disabilities assessing the risk. J Learn Disabil, 39, 3–10. [DOI] [PubMed] [Google Scholar]
- Mammarella IC, Ghisi M, Bomba M, Bottesi G, Caviola S, Broggi F, & Nacinovich R (2016). Anxiety and depression in children with nonverbal learning disabilities, reading disabilities, or typical development. Journal of Learning Disabilities, 49(2), 130–139. [DOI] [PubMed] [Google Scholar]
- Margalit M, & Al-Yagon M (2002). The loneliness experience of children with learning disabilities. The Social Dimensions of Learning Disabilities, 53–75. [Google Scholar]
- May AL, & Stone CA (2010). Stereotypes of individuals with learning disabilities: Views of college students with and without learning disabilities. J Learn Disabil. [DOI] [PubMed] [Google Scholar]
- McBride HE, & Siegel LS (1997). Learning disabilities and adolescent suicide. Journal of Learning Disabilities, 30(6), 652–659. [DOI] [PubMed] [Google Scholar]
- Mugnaini D, Lassi S, La Malfa G, & Albertini G (2009). Internalizing correlates of dyslexia. World Journal of Pediatrics, 5(4), 255–264. [DOI] [PubMed] [Google Scholar]
- Morris SB (2008). Estimating effect sizes from pretest-posttest-control group designs. Organizational research methods, 11(2), 364–386 [Google Scholar]
- Muscott HS, & O’Brien ST (1999). Teaching character education to students with behavioral and learning disabilities through mentoring relationships. Education and Treatment of Children, 373–390. [Google Scholar]
- Nelson JM, & Harwood H (2011). Learning disabilities and anxiety: A meta-analysis. Journal of Learning Disabilities, 44(1), 3–17. [DOI] [PubMed] [Google Scholar]
- Noll V (1997). Cross-age mentoring program for social skills development. The School Counselor, 44(3), 239–242. [Google Scholar]
- Owens JS, Goldfine ME, Evangelista NM, Hoza B, & Kaiser NM (2007). A critical review of self-perceptions and the positive illusory bias in children with ADHD. Clinical Child and Family Psychology Review, 10(4), 335–351. [DOI] [PubMed] [Google Scholar]
- Owens JS, & Hoza B (2003). The role of inattention and hyperactivity/impulsivity in the positive illusory bias. Journal of Consulting and Clinical Psychology, 71(4), 680. [DOI] [PubMed] [Google Scholar]
- Parhiala P, Torppa M, Eklund K, Aro T, Poikkeus A-M, Heikkilä R, & Ahonen T (2015). Psychosocial Functioning of Children with and without Dyslexia: A Follow-up Study from Ages Four to Nine. Dyslexia, 21(3), 197–211. [DOI] [PubMed] [Google Scholar]
- Pearl R, & Donahue ML (2004). Peer relationships and learning disabilities In Learning About Learning Disabilities (Third Edition) (pp. 133–165). Elsevier. [Google Scholar]
- Rabiee P, Knowles J, & Priestley M (2001). Whatever Next!: Young Disabled People Leaving Care. First Key Limited. [Google Scholar]
- Raskind MH, Goldberg RJ, Higgins EL, & Herman KL (1999). Patterns of change and predictors of success in individuals with learning disabilities: Results from a twenty-year longitudinal study. Learning Disabilities Research & Practice, 14(1), 35–49. [Google Scholar]
- Rhodes JE, Spencer R, Keller TE, Liang B, & Noam G (2006). A model for the influence of mentoring relationships on youth development. Journal of Community Psychology, 34(6), 691–707. [Google Scholar]
- Rini C, Lawsin C, Austin J, DuHamel K, Markarian Y, Burkhalter J, … Redd WH (2007). Peer mentoring and survivors’ stories for cancer patients: positive effects and some cautionary notes. Journal of Clinical Oncology, 25(1), 163. [DOI] [PubMed] [Google Scholar]
- Rose CA, Espelage DL, Monda-Amaya LE, Shogren KA, & Aragon SR (2015). Bullying and middle school students with and without specific learning disabilities: an examination of social-ecological predictors. J Learn Disabil, 48, 239–254. 10.1177/0022219413496279 [DOI] [PubMed] [Google Scholar]
- Roy A, Hartman CA, Veenstra R, & Oldehinkel AJ (2015). Peer dislike and victimisation in pathways from ADHD symptoms to depression. European Child & Adolescent Psychiatry, 24(8), 887–895. [DOI] [PubMed] [Google Scholar]
- Rubinsten O, & Tannock R (2010). Mathematics anxiety in children with developmental dyscalculia. Behavioral and Brain Functions, 6(1), 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shevitz B, Weinfeld R, Jeweler S, & Barnes-Robinson L (2003). Mentoring empowers gifted/learning disabled students to soar! Roeper Review, 26(1), 37–40. [Google Scholar]
- Shifrer D (2013). Stigma of a label: Educational expectations for high school students labeled with learning disabilities. Journal of Health and Social Behavior, 54(4), 462–480. [DOI] [PubMed] [Google Scholar]
- Singer E (2005). The strategies adopted by Dutch children with dyslexia to maintain their self-esteem when teased at school. Journal of Learning Disabilities, 38(5), 411–423. [DOI] [PubMed] [Google Scholar]
- Suárez-Pellicioni M, Núñez-Peña MI, & Colomé À (2016). Math anxiety: A review of its cognitive consequences, psychophysiological correlates, and brain bases. Cognitive, Affective, & Behavioral Neuroscience, 16(1), 3–22. [DOI] [PubMed] [Google Scholar]
- Svetaz MV, Ireland M, & Blum R (2000). Adolescents with learning disabilities: Risk and protective factors associated with emotional well-being: Findings from the National Longitudinal Study of Adolescent Health. Journal of Adolescent Health, 27, 340–348. [DOI] [PubMed] [Google Scholar]
- Terras MM, Thompson LC, & Minnis H (2009). Dyslexia and psycho-social functioning: an exploratory study of the role of self-esteem and understanding. Dyslexia, 15(4), 304–327. [DOI] [PubMed] [Google Scholar]
- Tolan PH, Henry DB, Schoeny MS, Lovegrove P, & Nichols E (2014). Mentoring programs to affect delinquency and associated outcomes of youth at risk: A comprehensive meta-analytic review. Journal of Experimental Criminology, 10(2), 179–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van de Mortel TF (2008). Faking it: social desirability response bias in self-report research. Australian Journal of Advanced Nursing, The, 25(4), 40. [Google Scholar]
- Welkowitz J, & Fox W (2000). A model mentor/advisor program supporting secondary youth with emotional and behavioral challenges and their families within rural Vermont. Burlington: University of Vermont, Center on Disability and Community Inclusion. [Google Scholar]
- Willcutt EG (2014). Behavioral genetic approaches to understand the etiology of comorbidity In Behavior Genetics of Psychopathology (pp. 231–252). Springer. [Google Scholar]
- Willcutt EG, & Pennington BF (2000). Psychiatric comorbidity in children and adolescents with reading disability. Journal of Child Psychology and Psychiatry, 41(08), 1039–1048. [PubMed] [Google Scholar]
- Yajai Sitthimongkol RN, & Apinuntavech S (2012). Predicting Factors for Risk of Depression in Adolescents with Learning Disorders. J Med Assoc Thai, 95, 1480–1484. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.