Abstract
Gout is the most common inflammatory arthritis which initially presents as a monoarthritis that usually favours peripheral joints namely the 1st MTP. It was reported in the literature to rarely involve the axial joint, such as the sacroiliac joint, and often mimics seronegative spondyloarthritis (SpA). Gout is a male disease and after menopause the risk in females is equal to males. Previous reports describe male patients developing gout involving the SI joint. We report a lady with a history of gout presenting with acute onset lower back pain. MRI of the sacroiliac joints revealed unilateral sacroilitis. With the help of Dual-Energy Computed Tomography (DECT) which is a newer imaging technique, a diagnosis of gout involving the sacroiliac joint was established. Gout involving the sacroiliac joints is rare, however it should be considered in the differential diagnosis in patients with unilateral sacroilitis given the similarity in presentation to SpA. Utilization of newer imaging modalities including DECT can highly guide in establishing a diagnosis and providing the correct treatment.
Keywords: Gout, sacroiliac joint, dual energy CT scan
Introduction
Gout is a common form of inflammatory arthritis frequently involving the appendicular skeleton. Rarely, it involves the axial skeleton or sacroiliac (SI) joints, mimicking spondyloarthritis (SpA), infectious arthritis, or osteoarthritis. We report on the challenging case of a post-menopausal female presenting with acute-onset low back pain with asymmetrical sacroiliitis, as assessed based on scans obtained via magnetic resonance imaging (MRI). With the help of dual-energy computed tomography (DECT), she was confirmed to have gout affecting the SI joints and excellent response to treatment. Our case highlights the usefulness of DECT in establishing the diagnosis of gout at uncommon sites, where joint aspiration may not be feasible.
Case Presentation
A 62-year-old female with a past history of morbid obesity, type 2 diabetes mellitus, hypertension, mild chronic kidney disease, and asymptomatic hyperuricemia with acute-onset low back pain for two weeks was transferred to our institution from an external facility. Prior to admission, she reported to have experienced sudden onset severe low back and left buttock pain to a degree that she was unable to ambulate. She had no associated neurological symptoms. She did not report any other joint symptoms, skin rash, or fever. There was no prior history of trauma.
Musculoskeletal exam showed paraspinal tenderness in the lumbosacral region, which was more intense in the left gluteal region. Peripheral joint exam was normal, and there were no palpable tophi.
Laboratory test results showed a normal complete blood count; liver function test showed normal results. Serum creatinine level of 90 (reference range of 35–88 micromol/L) and uric acid level of 567 (normal range of 143–339 micromol/L) with elevated acute-phase reactants, including an erythrocyte sedimentation rate of 72 (reference range of <20 mm/hr) and a C-reactive protein level of 38.2 (reference range of <5.00 mg/L), were noted. Serological laboratory test results for tuberculosis, Lyme, Brucella, and serial blood cultures were negative. Autoimmune test results for HLA-B27, antinuclear antibody, rheumatoid factor, and anti-cyclic citrullinated peptide were negative.
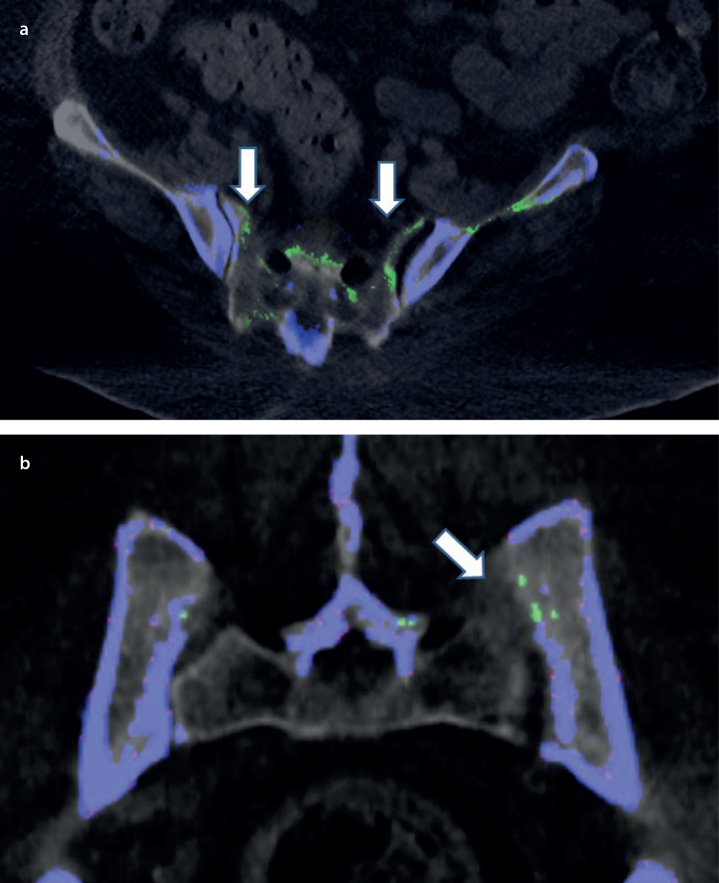
Prior to transfer to our facility, she underwent imaging studies including X-ray of SI joints and computed tomography (CT) of the pelvis and hips, which showed asymmetric widening of the left sacroiliac joint. MRI of the pelvis revealed bilateral asymmetrical sacroiliitis, with more intense inflammation involving the left SI joint. Additionally, there was mild left paraspinal muscle edema and inflammation (Figure 1). Lumbar spine MRI showed multilevel mild degenerative disc changes with no significant spinal canal or neural foraminal stenosis. Dual-energy computed tomography (DECT) scan revealed widespread green color-coded deposits involving the sacrum, transverse processes of the visualized lower lumbar spine, and bilateral iliac wings. Green color-coded deposits were seen to line up along the margins of both SI joints but were noted to be more extensively to the left. These findings were consistent with those of extensive monosodium urate (MSU) deposition in the pelvis (Figure 2).
Figure 1. a, b.
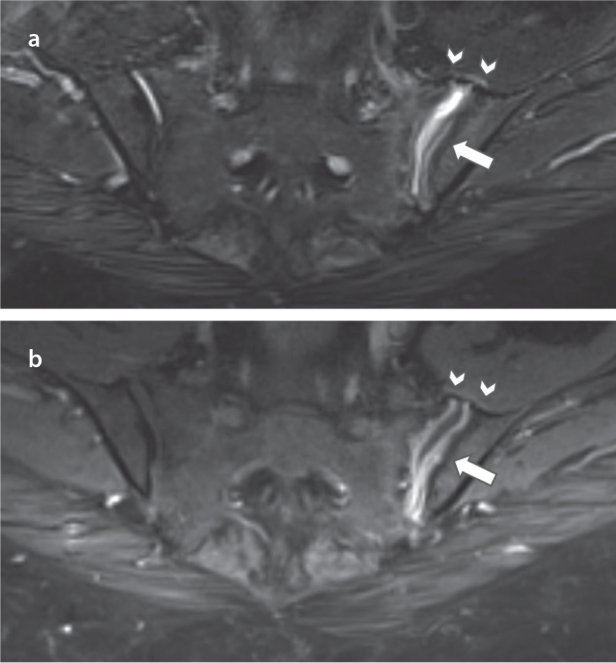
Axial T2–weighted MRI shows left SI joint widening and fluid (arrow) with muscular edema along its anterior border (arrowheads) (a). Corresponding axial post contrast T1–weighted MRI reveals thick synovial and mild periarticular contrast enhancement reflecting synovitis and reactive myositis (b).
Figure 2. a, b.
Axial (A) and Coronal (B) DECT of the pelvis showing extensive green color-coded MSU deposits (arrows) (a). Axial (A) and Coronal (B) DECT of the pelvis showing extensive green color-coded MSU deposits (arrows) (b).
The patient was initially treated with intravenous methylprednisolone and then switched to a reducing dose of oral prednisone along with colchicine. Within a week, the patient reported almost complete resolution of her symptoms. Subsequently, she was treated with a gradually up-titrating dose of allopurinol. Prednisone and colchicine were discontinued after 2 months of treatment. On subsequent follow-up visits over the next 6 months, she has remained pain free, and with allopurinol 300 mg daily, the serum uric acid levels have been within the target range of <350 micromol/L.
Litreature Review
Gout is a common form of inflammatory arthritis that develops owing to the deposition of MSU crystals in joints and soft tissues. It mainly affects middle-aged men and postmenopausal women. Acute gout predominantly affects the appendicular skeleton but rarely involves the axial skeleton. Although lumbar spine involvement is more common (1–3), sacroiliac joints (SI) may be involved in rare cases closely mimicking axial spondyloarthropathies or infections (4). Based on the results of radiographic analysis, the prevalence of lumbar and SI joint involvement owing to gout has been reported to be ranging from 13% to 17% (5, 6).
Evidence of bone marrow edema along the SI joints on MRI is a nonspecific finding and can be seen in various conditions, including spondyloarthropathies, infectious arthritis, gouty sacroiliitis, and osteoarthritis. The distribution and intensity of bone marrow edema on MRI with associated findings can assist in revealing the correct etiology only to a certain extent but cannot directly identify MSU crystals. However, CT-guided needle aspiration of the affected joint remains the gold standard for diagnosing gout; arthrocentesis can be technically challenging at difficult-to-access sites, such as SI joints, and in patients with minimal joint effusion. In such cases, DECT can be a useful imaging modality because it can specifically identify MSU crystal deposition based on its chemical composition. DECT has a high sensitivity and specificity in identifying MSU crystals of size >3 mm, with an overall accuracy of 87%–94%. Moreover, it has several other advantages, including no requirement for administration of a contrast agent, shorter scan time, and higher inter-observer agreement (7).
Conclusion
In conclusion, this case demonstrates the importance of including axial gouty arthropathy in the differential diagnosis of patients presenting with low back pain when appropriate risk factors are present. It also highlights the usefulness of newer noninvasive imaging modalities, such as DECT, in establishing the diagnosis and offering appropriate treatment.
Main Points.
Sacroliliac gouty arthritis is a rare manifestation however it should be considered as part of the differential diagnosis in patients with multiple comorbidities including obesity, chronic renal disease and hypertension.
Dual-energy computed tomography is a useful imaging modality that can differentiate gouty arthritis from spondyloarthropathies and infectious arthritis.
Gout arthritis involving the axial skeleton is treated with corticosteroids, colchicine and urate lower mediations.
References
- 1.Alarcón-Segovia DA, Cetina JA, Díaz-Jouanen E. Sacroiliac joints in primary gout. Clinical and roentgenographic study of 143 patients. Am J Roentgenol Radium Ther Nucl Med. 1973;118:438–43. doi: 10.2214/ajr.118.2.438. [DOI] [PubMed] [Google Scholar]
- 2.Konatalapalli RM, Demarco PJ, Jelinek JS, Jelinek JS, Murphey M, Gibson M, et al. Gout in the axial skeleton. J Rheumatol. 2009;36:609–13. doi: 10.3899/jrheum.080374. [DOI] [PubMed] [Google Scholar]
- 3.De Mello FM, Helito PV, Bordalo-Rodrigues M, Fuller R, Halpern AS. Axial gout is frequently associated with the presence of current tophi, although not with spinal symptoms. Spine. 2014;39:E1531–6. doi: 10.1097/BRS.0000000000000633. [DOI] [PubMed] [Google Scholar]
- 4.Cardoso FN, Omoumi P, Wieers G, Malfague B, Malghem J, Lecouvet FE, et al. Spinal and sacroiliac gouty arthritis: report of a case and review of the literature. Acta Radiol Short Rep. 2014;3 doi: 10.1177/2047981614549269. 2047981614549269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Monu JU, Pope TL., Jr Gout: a clinical and radiologic review. Radiol Clin North Am. 2004;42:169–84. doi: 10.1016/S0033-8389(03)00158-1. [DOI] [PubMed] [Google Scholar]
- 6.Jajic I. Gout in the spine and sacro-iliac joints: radiological manifestations. Skeletal Radiol. 1982;8:209–12. doi: 10.1007/BF00355508. [DOI] [PubMed] [Google Scholar]
- 7.Glazebrook KN, Guimaraes LS, Murthy NS, Black DF, Bongartz T, Manek NJ, et al. Identification of intraarticular and periarticular uric acid crystals with dual-energy CT: initial evaluation. Radiology. 2011;261:516–24. doi: 10.1148/radiol.11102485. [DOI] [PubMed] [Google Scholar]