Dear Editor,
Hepatic hemangiomas (HHs) are the most common benign tumors of the liver. Most of the HHs are asymptomatic, usually detected incidentally, and can be managed through observation (1). Surgery is rarely indicated, especially for large giant HH (>40 mm) lesions causing complications such as nausea, vomiting, portal hypertension, venous outflow obstruction, obstructive jaundice, and rupture and compression of the adjacent organ (1–3). We describe the case of a patient with a symptomatic giant HH who was treated with surgical resection.
A 43-year-old woman presented to our institute with complaints of postprandial nausea and vomiting, epigastric pain for several weeks, and recent weight loss of about 10 kg. Physical examination revealed a palpable mass in the epigastrium. On biochemical analysis, her complete blood count as well as kidney and liver function test results were found to be normal, except slightly elevated total and direct bilirubin levels (2.08 mg/dL and 0.61 mg/dL, respectively). Upper gastrointestinal endoscopy revealed external compression of the corpus of the stomach. Abdominal ultrasonography showed a giant hemangioma-like lesion about 140×120 mm in diameter in the left lobe of the liver. Contrast-enhanced multidetector computed tomography imaging with different planes showed a large lesion with lobulated contours about 130×100×100 mm in diameter, constituting a great proportion of the left lobe of the liver and extending postero-inferiorly; the lesion was hypodense in contrast-free sections and showed peripheral intermittent nodular contrast enhancement and centripetal filling in postcontrast sections, leading to a diagnosis of giant HH (Figure 1). Surgery was undertaken due to the symptoms of stomach compression. An upper midline incision was made, and a giant hemangioma completely filling the left lobe lateral segment and compressing the stomach was seen. After cholecystectomy, left hepatic vein and hepatic hilar dissections were made. Then, hepatic parenchyma was dissected using the liver hanging maneuver just to the left of the falciform ligament, and finally, the left lobe lateral segment was resected (Figure 2). Intraoperative cholangiography showed that remaining bile ducts were normal. Operation time was approximately 3 h, and intraoperative blood loss was about 150 mL. No complications developed in the postoperative period. Patient’s postprandial nausea and vomiting resolved, and she was discharged on the postoperative day 7.
Figure 1.
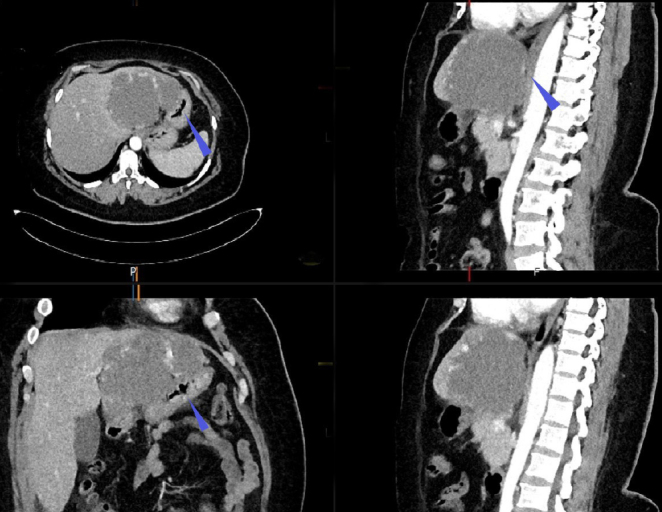
Preoperative multidetector computed tomography images of different planes revealed a lesion about 130×100×100 mm in diameter located in the left lobe lateral segment of the liver.
Figure 2.
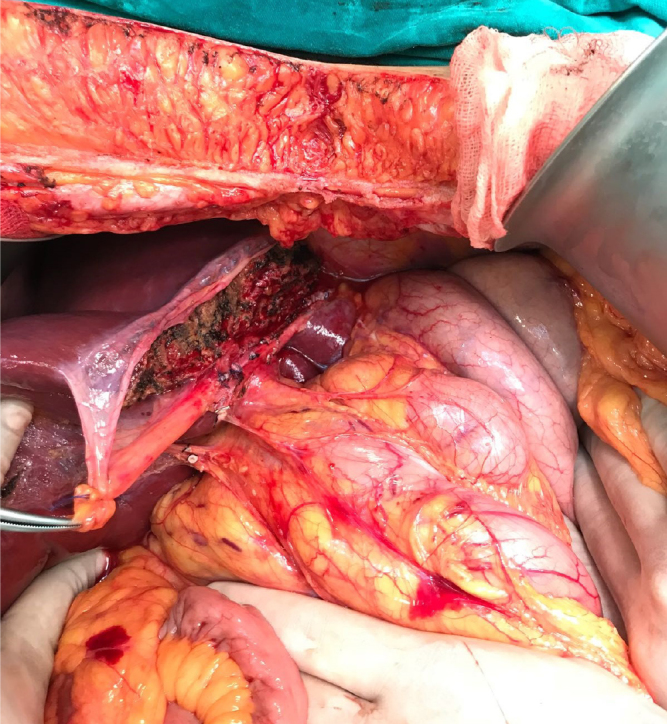
Intraoperative view following left lobe lateral segment resection.
Hemangiomas are benign tumors that develop due to abnormal proliferation of endothelial cells. The frequency of hemangiomas ranges between 0.4% and 20% (1). HHs are diagnosed mostly between the ages of 30 and 50 years and are 5–6 times more common in women (2).
Most of the patients are asymptomatic, but those with giant HHs may become symptomatic. The symptoms mentioned earlier are mostly associated with the site and the extent of tumor. Furthermore, such patients may develop Kasabach-Merritt syndrome, which is characterized by consumptive coagulopathy, thrombocytopenia, and microangiopathic hemolytic anemia. A rare and life-threatening complication of this tumor is the rupture of the tumor. Thus, close monitoring of asymptomatic patients is recommended (1–4). Indications for treatment are giant hemangiomas with complications, enlargement, and suspicion of malignancy.
Treatment options for HHs are systemic corticosteroid treatment, interferon treatment, transarterial embolization, ligation of hepatic artery, radiotherapy, resection, and, occasionally, transplantation (4). Of these, only hepatic resection and transplantation are successful in the long term. Regarding liver resection methods, many surgeons favor enucleation for HH. The dissection plane for this technique is just between the capsule of the hemangioma and liver tissue. Enucleation is a safe and quick technique with low blood loss and low morbidity and mortality rates. However, it might not be a suitable option for a lesion that is >100 mm in size or is centrally located because of a high risk of massive blood loss (4). But if Pringle’s maneuver is performed properly, enucleation can be successfully performed for a large and centrally located lesion. Liver resections are generally feasible for large lesions in the left lobe or right posterior section of the liver (2). For patients with multiple and bilaterally located hemangiomas, assessment of hepatic reserve is necessary. In such patients, lesions that give rise to symptoms should be resected first. Symptomatic patients with unresectable lesions involving large parts of the liver bilaterally or involving the hepatic hilum may require liver transplantation (2–4). In the present case, the stomach was compressed by a giant HH, and the patient had nausea, vomiting, and weight loss. Eventually, her symptoms were resolved postoperatively. Liver resection is a safe and effective treatment option for a symptomatic giant HH when performed at specialized centers, like our liver transplant center, where such patients are frequently treated.
Footnotes
Informed Consent: Written informed consent was obtained from the patient who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - S.A., E.O.; Design - S.A.; Supervision - S.Y.; Data Collection and/or Processing - S.A., S.Y., K.K.; Analysis and/or Interpretation - S.A., S.Y.; Literature Search - S.A., E.O. K.K.; Writing Manuscript - E.O., S.A.; Critical Review - S.Y., S.A.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Aydin C, Akbulut S, Kutluturk K, Kahraman A, Kayaalp C, Yilmaz S. Giant hepatic hemangioma presenting as gastric outlet obstruction. Int Surg. 2013;98:19–23. doi: 10.9738/CC170.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abdel Wahab M, El Nakeeb A, Ali MA, et al. Surgical Management of Giant Hepatic Hemangioma: Single Center’s Experience with 144 Patients. J Gastrointest Surg. 2018;22:849–58. doi: 10.1007/s11605-018-3696-y. [DOI] [PubMed] [Google Scholar]
- 3.Akbulut S, Yilmaz M, Kahraman A, Yilmaz S. Bilateral lower limb edema caused by compression of the retrohepatic inferior vena cava by a giant hepatic hemangioma. Int Surg. 2013;98:229–33. doi: 10.9738/INTSURG-D-13-00046.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vagefi PA, Klein I, Gelb B, et al. Emergent orthotopic liver transplantation for hemorrhage from a giant cavernous hepatic hemangioma: case report and review. J Gastrointest Surg. 2011;15:209–14. doi: 10.1007/s11605-010-1248-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xia F, Lau WY, Qian C, Wang S, Ma K, Bie P. Surgical treatment of giant liver hemangiomas: enucleation with continuous occlusion of hepatic artery proper and intermittent Pringle maneuver. World J Surg. 2010;34:2162–7. doi: 10.1007/s00268-010-0592-3. [DOI] [PubMed] [Google Scholar]


