Abstract
This Research Letter examines the distribution of US internal medicine specialists who are able to provide diabetes care.
For the first time, antihyperglycemic therapies are available to modify cardiovascular disease courses in type 2 diabetes . Two therapeutic classes (sodium-glucose cotransporter inhibitors and glucagon-like peptide-1 receptor agonists) are now recognized to be associated with multisystem health and reductions in cardiovascular and kidney outcomes. Despite the ongoing expansion of the evidentiary base supporting their use and the broadening of regulatory labels of select sodium-glucose cotransporter inhibitors and glucagon-like peptide-1 receptor agonists, their prescription has been largely restricted to primary care physicians and endocrinologists.1,2 Primary care physicians treat approximately 90% of individuals with type 2 diabetes nationally.3 However, high-risk patients with type 2 diabetes commonly encounter various internal medicine specialists because of high rates of comorbidities and clinical events.4 We therefore characterized the distribution of internal medicine specialists in the United States who may be able to provide care for the growing population with diabetes.
Methods
We queried state-specific diabetes prevalence and incidence among adults in 2016 using the US Centers for Disease Control and Prevention US Diabetes Surveillance System.5 We determined the number of practicing endocrinologists, cardiologists, and nephrologists in each US state using 2016 Centers for Medicare and Medicaid Services physician and other supplier public files.6 We then estimated the relative density of incident diabetes cases per specialist in each state. This study evaluating publicly available, deidentified data was exempt from institutional review board approval and consent was waived.
Results
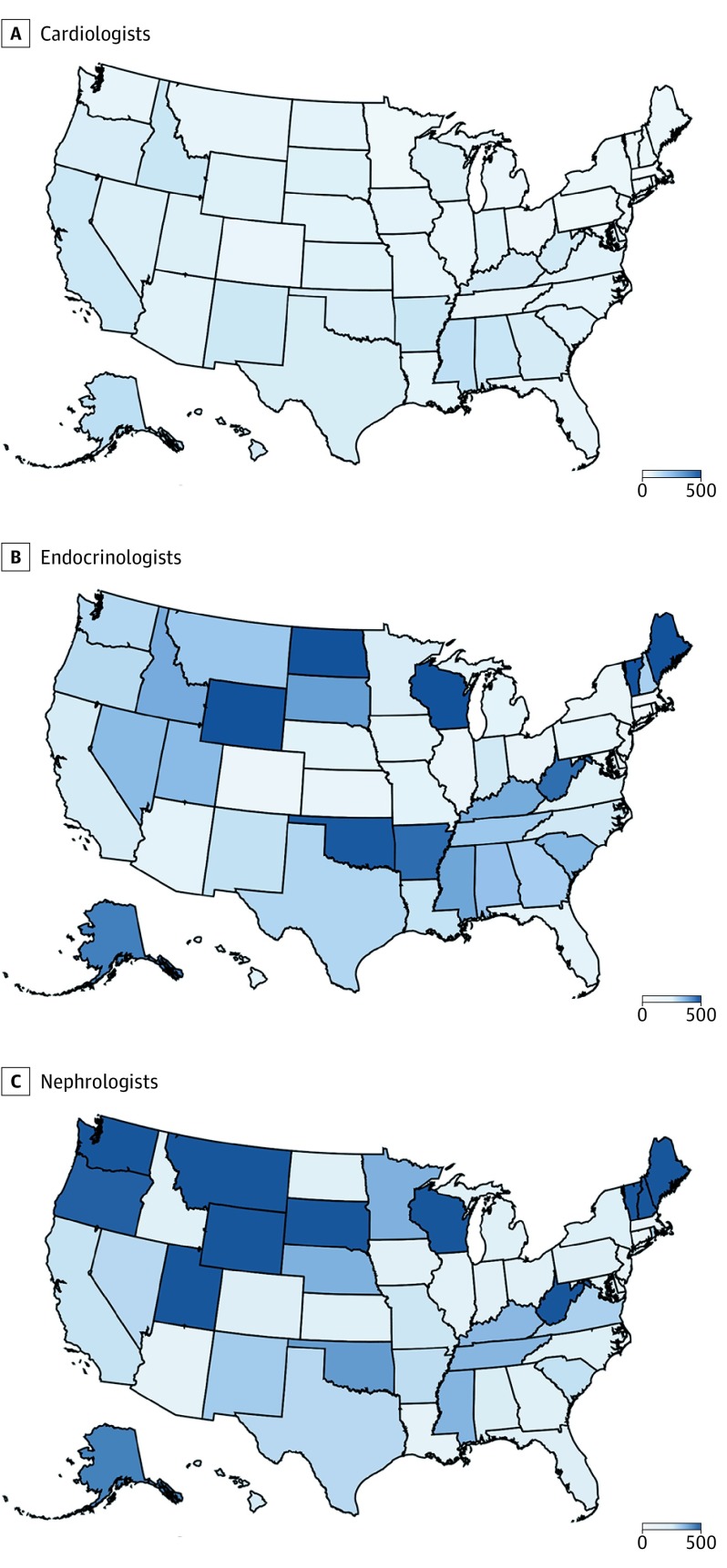
In 2016, cardiologists were the highest represented specialists (n = 22 848), followed by endocrinologists (n = 7793), and nephrologists (n = 7504). In 2016, 1.9 million US adults received a new diabetes diagnosis and the age-adjusted prevalence of diabetes ranged from 6.2% (Colorado) to 13.7% (Puerto Rico). Across the United States, we estimate that there were 81 incident diabetes cases per cardiologist, ranging from 30:1 (Washington, DC) to 154:1 (Alaska). By contrast, we observed a larger per-specialist case volume and wider distribution for endocrinologists (overall, 238:1; range, 37:1 [Washington, DC] to 667:1 [Wyoming]) and nephrologists (overall, 248:1; range, 46:1 [Washington, DC. to 2000:1 [Vermont]; Figure).
Figure. Density of Newly Diagnosed Cases of Diabetes per Specialist in 2016 Across US States.
A, Cardiologists. The estimates vary from 30:1 to 154:1 across states. B, Endocrinologists. The estimates vary from 37:1 to 667:1 across states. C, Nephrologists. The estimates vary from 46:1 to 2000:1 across states. Density maps of the number of incident diabetes cases per specialist were created using Microsoft Excel with Bing software (GeoNames, HERE, MSFT).
Discussion
Cardiologists appear well positioned to participate in diabetes care given their numbers and distribution relative to diabetes cases. The burden of diabetes nationally appears to be outpacing access to endocrinologists in the United States, especially in certain states. Thus, broader multispecialty engagement in diabetes care may improve overall access, increase opportunities to optimize care, and potentially lessen disparities in care provision.
Beyond their density, cardiologists often encounter high-risk patients with diabetes who may benefit most from care optimization. The ratio of cardiologist-to-endocrinologist outpatient encounters among patients with diabetes at a tertiary care center was approximately 3:1 and was even higher (approximately 5:1) for those with comorbid cardiovascular disease,4 suggesting that cardiology visits may serve as an important node of care. Additionally, the care setting may differ by specialist. Hospitalization for acute cardiovascular care may represent a teachable moment for counseling, screening, risk factor modification, and treatment initiation. Finally, diabetes therapeutic goals are shifting from glucocentric views to global risk-reduction approaches. In a recent renal outcomes trial (NCT02065791), canagliflozin delayed renal progression and markedly reduced cardiovascular outcomes in diabetic kidney disease. Nephrologists may thus serve as another critical access point for optimal diabetes care delivery.
We must begin to develop practical multidisciplinary pathways to advance evidence-based diabetes care. Currently, barriers to cardiology involvement include concerns regarding adverse effects, added time to clinical care, and the potential of overstepping interdisciplinary boundaries. National innovative models have been launched to address these issues, including cardiometabolic centers of excellence, cross-disciplinary training pathways, and population health management approaches that integrate broader care teams. Given the overall density of cardiologists, frequency of cardiovascular encounters, and shifting therapeutic paradigms, cardiovascular specialists should be equipped with the necessary practical knowledge to screen for diabetes, participate in risk factor modification, and introduce evidence-based antihyperglycemic therapies. We believe cardiologists should be integral members of the multidisciplinary care team to promote equitable access for this growing at-risk population.
References
- 1.Vaduganathan M, Patel RB, Singh A, et al. Prescription of glucagon-like peptide-1 receptor agonists by cardiologists. J Am Coll Cardiol. 2019;73(12):1596-1598. doi: 10.1016/j.jacc.2019.01.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vaduganathan M, Sathiyakumar V, Singh A, et al. Prescriber patterns of SGLT2i after expansions of U.S. Food and Drug Administration labeling. J Am Coll Cardiol. 2018;72(25):3370-3372. doi: 10.1016/j.jacc.2018.08.2202 [DOI] [PubMed] [Google Scholar]
- 3.Davidson JA. The increasing role of primary care physicians in caring for patients with type 2 diabetes mellitus. Mayo Clin Proc. 2010;85(12)(suppl):S3-S4. doi: 10.4065/mcp.2010.0466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gunawan F, Partridge C, Kosiborod M, et al. Cardiologist vs. endocrinologist encounters in patients with T2D and CVD: potential implications for glucose-lowering therapy use and education. Paper presented at: Endocrine Society Annual Meeting; March 23-26, 2019; New Orleans, LA. https://academic.oup.com/jes/article/3/Supplement_1/SUN-149/5483577. Accessed May 1, 2019. [Google Scholar]
- 5.Centers for Disease Control and Prevention US Diabetes Surveillance System. http://www.cdc.gov/diabetes/data. Accessed April 21, 2019.
- 6.Centers for Medicare & Medicaid Services Medicare provider utilization and payment data: physician and other supplier. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/Physician-and-Other-Supplier.html. Accessed February 2, 2019.