This study describes a novel concept relating to the tripod theory with extrapolation to the upper nasal third as it pertains to cosmetic rhinoplasty.
Key Points
Question
Can we describe a concept related to the well-known tripod theory with extrapolation to the upper nasal third as it pertains to cosmetic rhinoplasty?
Findings
In this study of 10 lay individuals and 10 rhinoplasty-trained individuals who evaluated manipulated photographs of 3 women who had not had surgery, lay individuals were more likely to choose an ideal nasal profile based on surrounding facial architecture, while individuals with rhinoplasty training tended to separate the ideal nose from the surrounding face (statistically significant). Projection was recognized as being altered by both rhinoplasty-trained and lay individuals (although not statistically significant), whereas subjective changes in rotation were significantly more elusive to the lay individual (statistically significant).
Meaning
Simple alteration of the upper nasal third can result in an improved nasal profile without specific alteration of tip architecture.
Abstract
Importance
The tripod theory of the upper nasal third parallels the concept of the well-known nasal tip tripod. We are evaluating the idea that one can simply alter the upper nasal angles reliably without the complex physics associated with the nasal tip to achieve a pleasing cosmetic result.
Objective
To describe a concept related to the well-known tripod theory with extrapolation to the upper nasal third as it pertains to cosmetic rhinoplasty.
Design, Setting, and Participants
This is a prospective study in which lateral photographs of 3 women who had not undergone surgery (age range, 20-50 years) were selected for digital manipulation of the nasal radix with subsequent alteration of the nasofrontal and nasofacial angles via imaging software. The altered images were analyzed by 20 blinded individuals between July 2009 and June 2017 to assess how changes in the height of the nasal dorsum and radix alone affect nasal appearance and the perception of ideal nasal angles. The study took place at a tertiary center, and the patients chosen for evaluation had nasal architecture that only required subtle changes rather than structure that demonstrated glaringly obvious overprojection or underprojection and rotation or a large dorsal bony hump. Analysis began June 2018.
Main Outcomes and Measures
Overall trend in recognition of objective and subjective alterations in projection and rotation for the rhinoplasty- and non–rhinoplasty-trained evaluators.
Results
Ten medically trained and 10 lay individuals (13 women [65%]; mean [SD] age, 38 [8.6] years) analyzed digitally manipulated photographs of 3 women (age range, 20-50 years) who had not undergone surgery. Lay individuals were more likely to choose an ideal nasal profile based on surrounding facial architecture (28 of 30 [93%]), while individuals with rhinoplasty training tended to separate the ideal nose from the surrounding face (18 of 30 [60%]) (P < .001). Projection was consistently and accurately recognized as being altered by both rhinoplasty-trained and lay individuals (95% CI, −0.18 to 0.38; P = .60 and 95% CI, −0.26 to 0.33; P > .99 for most and least projected), whereas subjective changes in rotation were significantly more elusive to the lay individual (95% CI, −0.04 to 0.52; P = .12 and 95% CI, 0.11 to 0.65; P = .01 for most and least rotated).
Conclusions and Relevance
Predictable and consistent aesthetic results are the primary aim in rhinoplasty. Alterations in the upper nasal tripod are more reliable with extrapolated healing than with the tripod of the nasal tip. Ultimately, simple alteration of the upper nasal third can result in an improved nasal profile without specific alteration of tip architecture.
Level of Evidence
NA.
Introduction
Rhinoplasty is a complex procedure that has proven a formidable challenge in achieving predictable and consistent aesthetic results. An extensive understanding of anatomy, physics, and physiology is required to predict the perceptible changes that will occur with subtle surgical alteration. During the past 4 decades, several anatomic and physical models have been proposed to allow surgeons a better understanding of nasal anatomy and how it defines surgical technique.
In 1969, Jack R. Anderson, MD, first described the tripod concept (tri- meaning 3 and -pod meaning support), which defines the nasal tip as having 3 supporting limbs with the combined medial crura as 1 leg and each lateral crura as the other 2 legs.1 Alteration of any one of these limbs will lead to an anticipated 3-dimensional change in nasal tip structure. The tripod concept, which has truly stood the test of time throughout rhinoplasty surgery, has evolved into what is commonly referred to as the tripod theory. This theory has offered a conceptual window through which physicians of recent decades have been able to apply their surgical observations leading to modification of the original model. Certain assumptions must be made to apply the theory uniformly to all patients, which include (1) the length and relative strength of each leg should be equivalent; (2) the platform or base of each leg should be solid and equally supportive; (3) the tripod itself is a freestanding unit without any external forces acting on it; and (4) gravity affects each leg equally. However, these postulations in vivo are generally not practical and virtually impossible.
While Anderson’s tripod theory highlights nasal tip support given by the strength and durability of the lower lateral cartilages alone with little emphasis given to other support contributions,1 both Westreich et al2,3 via the cantilever theory and Janeke and Wright4 demonstrate that multiple major and minor support mechanisms contribute to variable effects on nasal tip structure. The M-arch model first described by Adamson et al5 is another modification of the tripod theory, which highlights a graduated integral approach to modifying the lower lateral cartilages at multiple points throughout their entire length to achieve desired nasal rotation, projection, and refinement. Overall, the sum effect of all maneuvers must be considered over the isolated effect of any single action.
The assessment of nasal architecture by the trained and untrained eye relies on the interaction of facial angles and measurements. While rhinoplasty involves approaches of physical change resulting in anatomic modification that is both palpable and visible, it also uses methods that create the illusion of anatomic alteration that is simply visual without an anatomic or tactile foundation. For instance, alteration to the depth of the radix will modify the perception of nasal projection and rotation without specifically changing nasal tip anatomy.
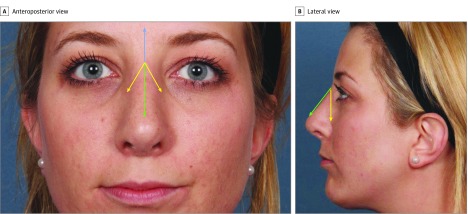
This article describes an upper nasal tripod with the radix as the main fulcrum and the lines of the nasofrontal and nasofacial angles as limbs. In both the anteroposterior and lateral view, the superior and inferior limbs of the tripod correlate to the frontonasal angle lines, and the medial and lateral limbs are the lines of the nasofacial angle (Figure 1). Thus, the inferior limb of the nasofrontal angle and the medial limb of the nasofacial angle are identical, hence a tripod (Figure 2).
Figure 1. Anteroposterior and Lateral Photograph of Tripod Components.
An anteroposterior (A) and lateral (B) photograph demonstrating the limbs and nasal angles that make up the upper nasal tripod. The superior and inferior limbs of the tripod correlate to the frontonasal angle lines (blue and green, respectively), while the medial and lateral limbs are the lines of the nasofacial angle (green and yellow, respectively). The medial leg of the nasofacial angle and inferior leg of the nasofrontal angle are identical (green).
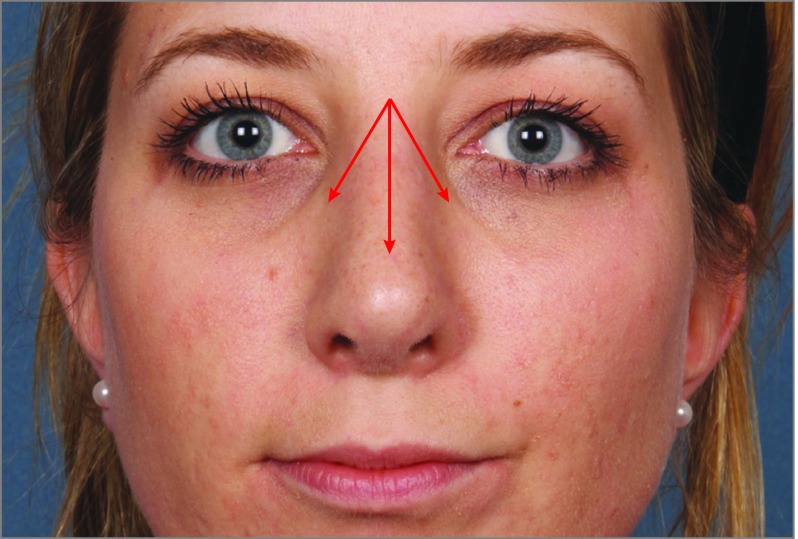
Figure 2. Anteroposterior Photograph of Tripod.
The same anteroposterior photograph as Figure 1 showing the proposed tripod of the upper nasal third using the combined inferior limb of the nasofrontal angle and the medial limb of the nasofacial angle as the medial crura correlate and the lateral limbs of the nasofacial angle as the lateral crura correlate.
Unlike the concept described in the inferior nasal third, the upper nasal tripod is more easily applied to a universal model in regard to the previously mentioned postulations of a tripod. These include (1) all limbs are solid and equally supported as the foundation is osseous; (2) the strength of each limb is equivalent; (3) the upper nasal tripod may be freestanding without any external forces acting on it; and (4) gravity is inconsequential as the support of all limbs is bony and firm with the radix being the point of rotation.
Methods
This study was approved by the institutional review board at Louisiana State University Health Sciences Center in New Orleans. All patients provided written informed consent. Data were collected between July 2009 and June 2019, and analyses began June 2018.
Computer Imaging Analysis
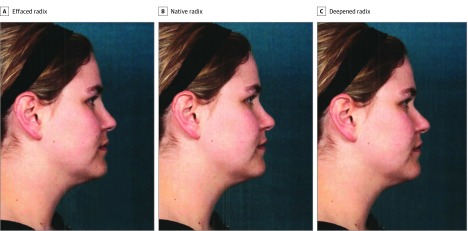
Lateral photographs of 3 individuals who had not undergone operation were selected for digital manipulation of the nasal radix with subsequent alteration of the nasofrontal and nasofacial angles via imaging software. The altered images were analyzed by 20 blinded evaluators (10 otolaryngologists with rhinoplasty training, 10 lay individuals with no medical training). Each image underwent digital morphing to first deepen and then efface the radix. This resulted in 3 images to be analyzed for each patient: (1) native radix, (2) deepened radix, and (3) effaced radix (Figure 3). All photographic alterations were performed by computer imaging software (IntelliStudio SB T2i; Canfield Imaging Systems). Angle measurement variability was not significant when measured on 3 separate occasions. Photographs were selected randomly without attention to facial or nasal analysis. The study consisted of an all-female population; sex was not pertinent for analysis and outcome measurements. Alterations were not standardized numerically and instead were made to allow for a balanced appearance to the nose with the angles measured subsequently. Analysis was performed using the χ2 and contingency table models. A 2-sided P value was considered statistically significant at less than .05.
Figure 3. Digitally Manipulated Photographs.
One of the 3 sets of lateral photographs of a nonoperated individual selected for digital manipulation of the nasal radix with subsequent alteration of the nasofrontal and nasofacial angles via imaging software.
Survey
The survey was designed to first ask evaluators to determine the “best-appearing nose” after viewing a single series of 3 images (ie, effaced radix, deepened radix, native radix). Examiners were then asked whether or not the best-appearing nose was also the nose that fit best with overall facial harmony. The remainder of the questions asked evaluators to examine tip morphology regarding projection and rotation. For the lay evaluator, the terms projection and rotation were defined in a rudimentary fashion (Box 1 and Box 2).
Box 1. Survey for Lay Individuals.
-
Which image do you believe has the best-appearing nose?
Patient 1
Patient 2
Patient 3
-
Which image do you believe has the best nasal appearance with regard to facial harmony?
Patient 1
Patient 2
Patient 3
-
In which image does the nose “stick out” the most? The least?
Most:
Patient 1
Patient 2
Patient 3
Least:
Patient 1
Patient 2
Patient 3
-
In which image does the tip of the nose look the most “rotated upward”? Least?
Most:
Patient 1
Patient 2
Patient 3
Least:
Patient 1
Patient 2
Patient 3
Box 2. Survey for Rhinoplasty-Trained Individuals.
-
Which image do you believe has the best-appearing nose?
Patient 1
Patient 2
Patient 3
-
Which image do you believe has the best nasal appearance with regard to facial harmony?
Patient 1
Patient 2
Patient 3
-
Which image has the most projected appearing nose? The least projected?
Most:
Patient 1
Patient 2
Patient 3
Least:
Patient 1
Patient 2
Patient 3
-
Which image has the most rotation? Least?
Most:
Patient 1
Patient 2
Patient 3
Least:
Patient 1
Patient 2
Patient 3
Nasal Angle Measurements and Analysis
Nasofacial and nasofrontal angles were measured on lateral views before and after all radix alterations using imaging software. The nasofrontal angle is defined as the angle formed by the intersection of the line from glabella to nasion with the line from nasion to nasal tip; a normal angle is between 115° to 130°. The nasofacial angle is defined as the angle formed by the intersection of the line from glabella to pogonion with the line from nasion to nasal tip; a normal angle is between 30° to 40°.
Nasal projection and rotation were also objectively evaluated using the imaging software. Rotation was measured using the nasolabial angle, which is defined as the angle formed by the intersection of the labial surface of the upper lip at the midline and the inferior border of the nose.
The Goode method, Crumley’s triangle, and Simons method were used to evaluate nasal projection. The Goode method measures nasal projection by drawing a right triangle. The first side is a line from nasion to alar crease, the second side is a perpendicular line from alar crease to tip-defining point, and the third side is a line along the nasal dorsum. The ratio of the line from the alar crease to nasal tip and from the nasion to nasal tip should be 0.55 to 0.60; a greater ratio signifies an overprojected nose, while a lesser ratio demonstrates underprojection of the nose. Crumley’s triangle describes the nasal profile as a right triangle as well with vertices at the nasion, nasal tip, and alar crease. The sides of the triangle have a 3:4:5 ratio. Both methods infer a resultant nasofacial angle of 36°. Simons used the upper lip length to calculate nasal projection by proposing that the nasal basal length should equal the length of the upper lip.
Results
Alterations of the radix demonstrated a change in nasal projection on nasal analysis. Deepening of the radix changed the native nasofrontal angle by an average of −6.7° and the nasofacial angle an average of 2.9°. Effacement of the radix altered the nasofrontal angle by an average of 4.1° and the nasofacial angle by an average of −4.2°. With the Goode method, nasal projection increased with deepening of the radix and lessened with effacement of the nasofrontal angle. The Goode ratio in morphed photographs was modified by a mean (SD) of 0.6° (0.036°). Crumley’s triangle method showed a change in the nasofacial angle by a mean (SD) of 32.2% (3.5%). Simons ratio was unaffected as it does not take upper nasal anatomy or position into account. True nasal rotation via the nasolabial angle was not changed though the perception of alteration was created.
Lay evaluators were more inclined to select the “best-appearing nose” to also be the nose that best fits with overall facial harmony. Essentially, most lay evaluators answered survey questions 1 and 2 identically 93% (28 of 30) of the time. This was not true of the rhinoplasty-trained otolaryngologists. The best-appearing nose was often taken out of context from the rest of the face, and the question of nasofacial harmony resulted in another nasal morphology as being ideal 60% (18 of 30) of the time. This difference was noted to be statistically significant (95% CI, 0.30-0.76; P < .001).
While projection was both subjectively and objectively altered with changing the radix as were the nasofrontal and nasofacial angles, there was no statistical significance between groups in answering question 3 (most and least) in both surveys (Box 1 and Box 2) regarding projection (95% CI, −0.18 to 0.38; P = .60 and 95% CI, −0.26 to 0.33; P > .99, respectively). The groups were overall congruent in their evaluations regarding perceived projection. Alteration in projection was similarly noted by both groups as 62% (37 of 60) of evaluators agreed that deepening the radix increases projection and 58% (35 of 60) agreed that effacement decreases projection.
Rotation, as detailed in question 4 (most and least) in both surveys (Box 1 and Box 2), was not quantitatively altered with modification of the radix per the nasolabial angle. Rhinoplasty-trained evaluators noted the relative alteration in rotation by deepening and effacing the radix compared with nonmedical examiners. This was not statistically significant for most rotated but was significant for least rotated (95% CI, −0.04 to 0.52; P = .12 and 95% CI, 0.11 to 0.65; P = .01, respectively).
Discussion
The nasal tip is regarded as the most dynamic area within nasal surgery, and its refinement is often described as an art form. The effects of wound healing and readherence of the soft tissue envelope to the underlying structure after rhinoplasty can negatively modify the results of even the most sophisticated surgeons. Anderson’s tripod theory has allowed surgeons an improved understanding of nasal tip dynamics and has opened the door for multidimensional applications to surgical technique.
The tripod theory of the upper nasal third embarks on the idea that one can simply alter the upper nasal angles reliably without the complex physics associated with the nasal base as described in Anderson’s tripod theory1 and Westrich’s cantilever theory.2,3 The nasal tip rests on a semirigid and elastic base, while the upper nose has a firm, bony foundation. Extrapolations from the idea of a tripod are more easily applied to the firm, bony base of the upper nasal third, making modifications more consistent.
The goal of radix surgery is to modify the position of the nasion and sometimes its width to balance different parts of the nose. Determination of the ideal position of the nasion, located at the midpoint of the nasofrontal suture, is critical. The radix is positioned at the nasion and is defined as the root or starting point of the nasal dorsum as it leaves the glabella. The radix is measured from the anterior corneal plate with a normal height ranging from 9 mm to 14 mm and should be at the approximate level of the upper tarsal crease. By altering the radix, one changes the main angles of the upper nasal third as well as the nasofrontal and nasofacial angles.
The sum of our study’s survey answers demonstrates an overall trend in recognition of both objective and subjective alterations in tip architecture including projection and rotation for both the rhinoplasty-trained and lay evaluators. The answers to questions 3 and 4 in Box 1 support deepening the radix to increase projection and rotation. Conversely, questions 3 and 4 in Box 2 confirm that effacing the radix will decrease projection and rotation. The evaluators agreed on their assessment of projection but differed significantly in their perception of rotation. This finding is supported as projection is objectively altered via the Goode or Crumley method, while rotation is only subjectively altered. Subjective changes are perhaps more obvious to those trained in the art of rhinoplasty. The untrained evaluators also appeared to take the entire facial structure into account when evaluating the nose, which may explain the oversight of subtle radix modifications that impart relative changes of rotation.
While predictable and consistent aesthetic results are difficult to achieve during rhinoplasty, the nasofrontal and nasofacial angles can be reliably altered to render subtle and subjective refinement to the nasal profile. The patient population chosen for evaluation purposefully included nasal architecture that only required subtle changes rather than those that demonstrated glaringly obvious overprojection or underprojection and rotation or large dorsal bony hump. This allowed for frank comparison of the lay vs medically trained eye in perceiving elegant subtle changes of the nasal structure. It is unlikely that alteration of the upper nasal third would be the only intervention, and as such, it is the sum of multiple subtle maneuvers that renders the overall effect. Ultimately, modification of the upper nasal third may simply be more reliable and stable.
Limitations
To our knowledge, this is the first study describing a theoretical concept related to the well-known tripod theory with extrapolation to the upper nasal third as it pertains to cosmetic rhinoplasty. While it brings insight into the clinical evolution of rhinoplasty, the study’s findings should be interpreted within the context of its limitations. An inherent limitation is that it is a prospective study with a small sample size and not a randomized clinical trial. However, as this is an innovative concept, study participants played significant role in such a limited study pool. Another limitation is that multiple comparisons were performed; thus, there is an appreciable risk that these findings constitute type I error. More importantly, selection of patients was based on nasal architecture that only required subtle alterations allowing for frank comparison of the lay vs medically trained eye in perceiving refined changes of the nasal structure.
Conclusions
Predictable and consistent aesthetic results are the ultimate aim during rhinoplasty. The impact of modifications to an individual’s nasal contour can be better predicted with a thorough understanding of objective and subjective or perceived alterations in rotation and projection. Alterations in the upper nasal tripod are more reliable with extrapolated healing than with the tripod of the nasal tip in regards to the postulates as described by Anderson.1 Ultimately, simple alteration of the upper nasal third can result in an improved nasal profile without specific alteration of tip architecture, and the subtle subjective or perceived changes of nasal rotation are not always obvious to the lay individual.
References
- 1.Anderson JR. The dynamics of rhinoplasty, in Proceedings of the Ninth International Congress of Otolaryngology. Excerpta Medica International Congress Series, No. 206. Amsterdam, Netherlands: Excerpta Medica. 1969:708-710. [Google Scholar]
- 2.Westreich RW, Lawson W. The tripod theory of nasal tip support revisited: the cantilevered spring model. Arch Facial Plast Surg. 2008;10(3):170-179. doi: 10.1001/archfaci.10.3.170 [DOI] [PubMed] [Google Scholar]
- 3.Westreich RW, Courtland HW, Nasser P, Jepsen K, Lawson W. Defining nasal cartilage elasticity: biomechanical testing of the tripod theory based on a cantilevered model. Arch Facial Plast Surg. 2007;9(4):264-270. doi: 10.1001/archfaci.9.4.264 [DOI] [PubMed] [Google Scholar]
- 4.Janeke JB, Wright WK. Studies on the support of the nasal tip. Arch Otolaryngol. 1971;93(5):458-464. doi: 10.1001/archotol.1971.00770060704004 [DOI] [PubMed] [Google Scholar]
- 5.Adamson PA, Litner JA, Dahiya R. The M-Arch model: a new concept of nasal tip dynamics. Arch Facial Plast Surg. 2006;8(1):16-25. doi: 10.1001/archfaci.8.1.16 [DOI] [PubMed] [Google Scholar]