Abstract
Objective
To review the literature on the clinical application of radiolabeled somatostatin receptor scintigraphy (SRS) by SPECT and PET in adults with chronic inflammatory diseases.
Research design
Systematic review of published observational studies between 1993 and 2017.
Data collection and analysis
The Cochrane Central Register of Controlled Trials, MedLine, EMBASE, PubMed, Google Scholar, OVID, EBSCO, Scopus, and Web of Science were used to search for studies on the use of SRS in adults with chronic inflammatory diseases. A team of reviewers independently screened for eligible studies. Quality of evidence was assessed by QUADAS approach.
Results
Eligible papers included 38 studies. Studied populations were heterogeneous, and patients were classified according to the diagnosed disease: endothelial inflammation, rheumatoid arthritis, cardiac allograft rejection, granulomatous diseases, small vessel vasculitis, idiopathic pulmonary fibrosis, sarcoidosis, and thyroid exophthalmopathy. Because of many quality differences between studies, it was not possible to pool data, and a narrative synthesis is reported.
Conclusion
Results highlight the value of SRS to detect active inflammation in several chronic inflammatory conditions, despite the bias related to the index test, showing lack of standardization of the scintigraphic technique and high variability of methods used to clinically evaluate inflammatory condition.
Keywords: Somatostatin receptor imaging, SPECT, PET, Inflammatory diseases
Introduction
Chronic inflammatory diseases are characterized by long-standing mononuclear cell infiltration of the target organ, leading to hypofunction and requiring life-long treatment [1]. In the past years, several different radiopharmaceuticals have been synthetized for molecular nuclear medicine that may contribute to the diagnosis and prognosis of these diseases [2]. In particular, several peptides, receptor ligands, and monoclonal antibodies have been radiolabeled, allowing the in vivo visualization of the inflammatory process at cellular and molecular level [3].
As far as radiolabeled peptides are concerned, it is important to emphasize the increasing use of somatostatin (SST) analogues targeting somatostatin receptors (SSTR) in inflammatory diseases, particularly in rheumatoid arthritis (RA), Sjögren syndrome (SS), and autoimmune thyroid diseases. Because the broader spectrum of interaction with SSTR in other different pathological conditions than neuroendocrine tumors, such as chronic inflammation, and because the known presence of SSTR over-expression by inflammatory cells, immunological cells in different tissues, blood vessels among others, it has been possible to use different radiolabeled somatostatin analogues with diverse affinity for these receptors, for diagnostic purposes in different oncological and inflammatory scenarios [4]. Different SST analogues have been proposed in clinical practice. Among all synthetic compounds pentetreotide (Octreotide®), labeled with 111In, was the most widely used for imaging purposes, because of its high affinity for SSTR 2 and 5. New radiopharmaceuticals for somatostatin receptor scintigraphy (SRS), showing a different and/or wider affinity to the receptors, are now available and labeling has been obtained both with gamma and positron emitters for diagnostic purposes, with SPECT or PET, respectively, such as 68Ga-DOTA-TATE and 64Cu-DOTA-TATE(affinity to type 2 receptors), 68Ga-DOTA-TOC (more selective to 2 and 5 type receptors), 68Ga-DOTA-NOC (affinity to 2,3 and 5 type receptors), and 99mTc-EDDA/HYNIC-TOC (affinity to 2 and 5 type receptors) [5].
The labeling of octreotide and other analogues has been carried out by conjugation of the peptide with a bi-functional chelator, DTPA, DOTA, or NOTA [6], and subsequent addition of a radionuclide such as 123I, 111In (pentreotide), 99mTc (depreotide-EDDA/HYNIC-TOC) or 68Ga, 18F, and 64Cu (DOTATATE) [7].
SST was first isolated from ovine hypothalamic extracts and was characterized as a tetradecapetide. It was identified as part of the releasing hormone family for its property to inhibit the secretion of growth hormone from pituitary cells by Brazeau and colleagues in 1973 [8]. SST-producing cells are typically neurons or endocrine-like cells and are found in high density in the central and peripheral nervous systems and in the endocrine pancreas and in the gut and in small numbers in the thyroid, adrenals, submandibular glands, kidneys, prostate, placenta blood vessel walls, and immune cells [9]. It is a cyclic hormone that regulates several physiological cell processes via specific receptors (SSTR) which are expressed by nerve cells, many neuroendocrine cells and inflammatory cells such as lymphocytes, monocytes, monocytes/macrophages, peripheral blood mononuclear cells and thymocytes [10]. Five SSTR subtypes have been cloned which have been found in cells involved in inflammatory responses with high density expression observed on neoangiogenic and peritumoral vessels, epithelioid cells, proliferating synovial vessels, and activated lymphocytes and monocytes [11]. In the peripheral blood mononuclear cells and in the spleen, mainly SSTR subtypes 2 and 3 are found; in the thymus, mainly SSTR subtypes 1, 2, and 3; in the macrophages and in dendritic cells, mainly SSTR subtype 2; in B lymphocytes, mainly SSTR subtype 3; and in T lymphocytes, SSTR subtypes 1 to 5 [4]. For diagnostic purposes, radiolabeled SST analogues have been used in SPECT and PET with clinically relevant results in different chronic inflammatory diseases, particularly for the evaluation of disease activity, prognosis, and therapy follow-up [12, 13]. Although 18F-fluorodeoxyglucose (18F-FDG) PET/CT has recently gained a role also in infective and inflammatory disease, because logistically it is easier and quicker to perform, this radiopharmaceutical is not specific and therefore it is not able to discriminate an infection from an inflammation [14].
In this review, we systematically analyze all papers on SRS (with either SPECT or PET) in the setting of various chronic inflammatory diseases: endothelial inflammation, rheumatoid arthritis, cardiac allograft rejection, small vessel vasculitis, idiopathic pulmonary fibrosis, sarcoidosis and granulomatous diseases, and Graves’ ophthalmopathy.
Why it is important to do this review
It important to do this review because the literature has shown the potential utility of radiolabeled somatostatin analogues not only in the diagnostic setting but as prognostic factor and as part of treatment control in some chronic inflammatory diseases, it is important to assess and collect the best evidence published up today regarding to this topic.
Methods
Criteria for considering studies for this review
Types of studies
Observational cohort studies, systematic reviews, reports of more than three cases.
Types of participants
Adult patients with any diagnosed inflammatory chronic disease such as rheumatoid arthritis, sarcoidosis, cardiac allograft, atherosclerotic plaques, Sjögren disease, idiopathic pulmonary fibrosis, Graves’ exophthalmopathy who had a radiolabeled somatostatin receptor analogue scintigraphy for diagnostic purpose.
Types of intervention
Somatostatin receptor analogues radiolabeled with Spect tracers: 111In octreotide, 99mTc:99Tc-EDDA/HYNIC-TOC, 99mTc P829 and with PET tracers: 68GaDOTA-NOC, 68Ga DOTA-TOC, 68Ga DOTA-TATE, and 64CuDOTATATE.
Types of study outcome
The final diagnostic for the entire population was related to chronic inflammatory diseases such as: rheumatoid arthritis, Sjögren disease, Graves’ exophthalmopathy, atherosclerotic plaques, idiopathic pulmonary fibrosis, sarcoidosis, and other inflammatory conditions.
Search method for identifying the eligible studies
The selection of appropriate publications was based on the PRISMA guidelines [15]. We searched in Cochrane Central Register of Controlled Trials (CENTRAL) published in the Cochrane Library, MedLine (1993–2017), EMBASE (1993–2017), PubMed (1993–2017), Google Scholar (1993–2017), OVID (1993–2017), EBSCO (1993–2017), and Scopus and Web of Science (1993–2017). All relevant studies published in English, Italian, and Spanish language were identified by using the following search strategy: (“receptors, somatostatin”[MeSH Terms] OR “receptors”[All Fields] AND “somatostatin”[All Fields]) OR (“somatostatin receptors”[All Fields] OR (“somatostatin”[All Fields] AND “receptor”[All Fields]) OR “somatostatin receptor”[All Fields]) AND (“Bildgebung”[Journal] OR “imaging”[All Fields]) AND (“adult”[MeSH Terms] OR “adult”[All Fields] OR “adults”[All Fields]) NOT (“neoplasms”[MeSH Terms] OR “neoplasms”[All Fields] OR “neoplasm”[All Fields]) NOT (“tumors”[All Fields] OR “neoplasms”[MeSH Terms] OR “neoplasms”[All Fields] OR “tumors”[All Fields]) somatostatin receptor imaging AND adults.
Inclusion criteria
Studies or reports in which compounds were labeled with 68Ga, 99mTc, 68Ga, and 64Cu for applications other than in oncology-related indications were included. Every effort was made to include both the earliest and the most recent publications relating to a particular application, as well as any study with a significant new contribution. The decision to include or exclude an article was made by consensus.
Exclusion criteria
Publications in which the focus was on SRS in oncology-related applications or in which the emphasis was on aspects related to generators, radiochemistry, animal models, experimental reports, or physics were excluded.
Literature search was broadened to all reference lists of all retrieved articles, including observational studies, systematic reviews, conference proceedings, and poster presentations. Studies or reports with more than three cases in which SRS was used in patients with inflammatory diseases were also included. Case reports allusive to just one patient where not taken in consideration because the results of the observations could not be compared between patients in order to highlight differences or similarities.
Selection of studies data extraction and management
The decision to include or exclude an article was made by consensus between LKF, AWJMG, AS, and AM. We used the search strategies described to obtain titles and abstracts of studies of potential relevance to the review.
Two authors, one with expertise in the topic (LKAF), the second with expertise in the statistical methodology (SM), undertook the search. LKF, SM, and AM screened independently titles, abstracts, conferences proceedings, posters, and full texts for eligibility. We ensured the avoidance of multiple studies reporting on the same patient population by controlling the duplicate records in a peer review way, including the entire databases results; we also used standardized, pilot-tested forms, together with detailed instructions. Reviewers resolved disagreement through discussion or, if required, by adjudication by a third reviewer (SM).
Assessment of risk bias in included studies
The included studies were assessed by using the Cochrane Collaboration’s tool [16] and Quadas-2 [17] for potential source of bias and variation: patient selection bias (study design, patient recruitment, prospective data collection, consecutive patient enrollment), patient variation (demographic features, disease prevalence, disease severity, prior testing), index test bias (test review bias, threshold selection), index test variation (observer variation, availability of clinical information, test technology, test execution), reference standard bias (inappropriate reference standard, diagnostic review bias, incorporation bias), reference standard variation (definition of target condition), flow and timing bias (disease progression bias, treatment paradox, partial verification bias, differential verification bias, withdrawals, uninterpretable test results, sample size).
Data synthesis
Because of differences between studies, it was not possible to pool data, and so a narrative synthesis was prepared. Study population was very heterogeneous, for this reason we classified patients according to the diagnosed disease: endothelial inflammation and atherosclerosis, rheumatoid arthritis, idiopathic pulmonary fibrosis, Graves’ ophthalmopathy, sarcoidosis, and other chronic inflammatory diseases.
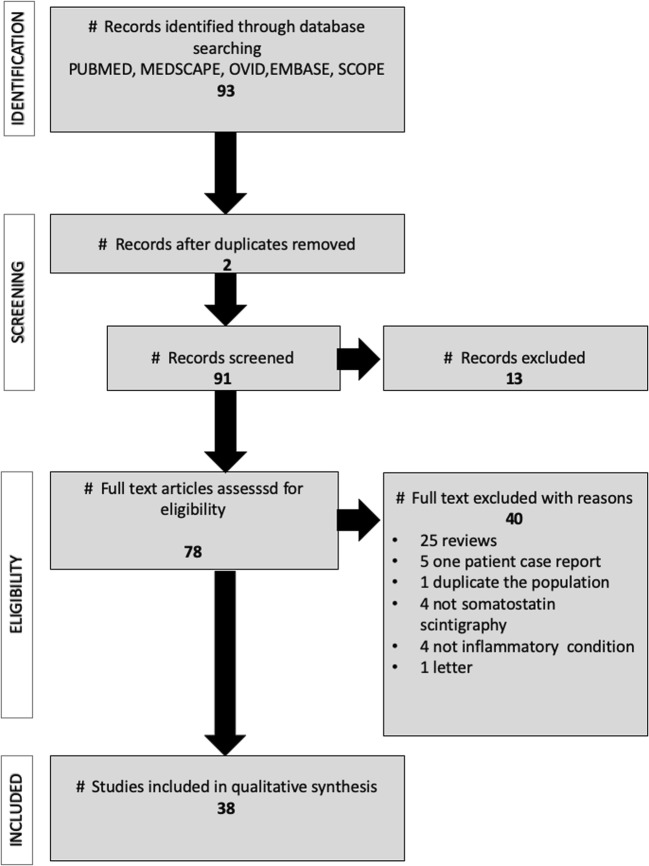
We found 93 potential studies evaluating radiolabeled SST analogues in chronic inflammatory diseases. After checking for duplicates, 13 papers were immediately excluded; after reading the full-text records, 40 were excluded because they did not fulfill the inclusion criteria. We, therefore, analyzed 38 publications, as shown in Fig. 1. Results are summarized in Table 1.
Fig. 1.
Prismal flowchart of article selection
Table 1.
Summary of analyzed papers
| Author | Type of study | Patients | Radiotracer | Risk of bias | Comments |
|---|---|---|---|---|---|
| Endothelial inflammation | |||||
| Tarkin 200118 | Prospective | 42 | 18F-FDG and 68Ga-DOTA-TATE | We did not identify source of bias | SRS identifies culprit coronary and carotid arteries in individuals with acute coronary syndrome, TIA and stroke |
| Malmberg 2015 19 | Observational prospective | 60 | 64Cu-DOTA-TATE | Reference test: they did not use reference test | SUVmax of inflamed plaques correlates with some Framingham risk factors |
| Wan 2017 21 | Prospective cohort | 20 | 68Ga-DOTA-TATE | Flow and timing: Heterogeneity of time between carotid event, PET scan and endarterectomy | No significantly different uptake in carotid plaques and contralateral carotids and no inflammatory cells at histology of excised plaques |
| Pedersen 2015 22 | Prospective cohort | 10 | 64Cu-DOTA-TATE | None | Uptake was significantly higher in symptomatic plaque versus the contralateral carotid artery and correlates with CD163 staining of plaques |
| Xian Li 2012 23 | Descriptive retrospective series of cases | 16 | 18F-FDG and 68Ga-DOTA-TATE | Reference standard and index test: unprecise reference test and lack of standard method for index test analysis. | Correlation between mean uptake of 18F-FDG or 68Ga-DOTA-TATE and patients’ score of risk factors |
| Mojtahedi 2014 24 | Retrospective series of cases | 44 | 68Ga-DOTA-TATE | Reference standard: Inaccurate method | 68Ga-DOTA-TATE detects more areas with increased uptake in patients with high cardiovascular risk |
| Rominger 2010 25 | Descriptive, retrospective | 70 | 68Ga-DOTA-TATE | Reference standard: Inaccurate method. | 68Ga-DOTA-TATE detects more areas with increased focal uptake in patients with high cardiovascular risk and with calcified plaques |
| Rheumatoid arthritis | |||||
| Anzola 2016 30 | Pilot study | 18 | 99mTc-Hynic-TOC |
Index test: Lack of standard method for index test analysis. |
By 99mTc-Hynic-TOC all patients showed uptake in joints and in 60% of salivary glands. Patients who were evaluated after Infliximab therapy showed significant reduction of joint uptake. |
| Van Hagen 1994 31 | Prospective | 18 | 111In-Octreotide | Index test and reference standard: just 2 patients were confirmed with histopathology and lack of standard method for index test analysis. | 76% of swollen RA joints were visualized. The degree of pain and swelling correlated well with positive scintigraphy findings in joints |
| Cardiac allograft rejection | |||||
| Aparici 2000 61 | Prospective | 10 | 111In-octreotide | Index test: lack of standard method for index test analysis. | Preliminary results indicate the feasibility of targeting activated lymphocytes with SRS in the detection of cardiac allograft rejection. |
| Small vessel vasculitis | |||||
| Neumann 2004 62 | Pilot study | 36 | 111In-octreotide | Reference standard: lack of immunohistochemical analysis to confirm presence of SSTR2 and SSTR3 in the whole population. | 111In-octreotide for pulmonary disease showed a sensitivity of 86%, specificity of 96% and 97% of positive predictive value for active disease. For ear nose and throat disease 68% and 100% |
| Idiopathic pulmonary fibrosis | |||||
| Ambrosini 2010 34 | Prospective | 14 | 68Ga-DOTA-NOC | Reference standard index test: it was not possible to confirm the presence of SSTR2 and SSTR3 in the affected areas. Lack of standard method for index test analysis. | 68Ga-DOTA-NOC uptake corresponded to areas of HRCT abnormalities in IPF patients, supporting the hypothesis that SSTR is over- expressed in lungs of IPF patients. |
| Lebtahi 2006 35 | Prospective | 11 | 111In-octreotide | Index test and reference standard: Lack of standard method for index test analysis. Inaccurate reference test. | Increased uptake of 111In-Octreotide in (mainly idiopathic) pulmonary fibrosis. Lung uptake correlates with alterations in lung function and with intensity of alveolitis and seems to be related to severity of lung fibrosis. |
| Win Thida 2012 36 | Prospective | 26 | 18F-FDG and 68Ga-DOTA-TATE | Patient selection, index test, reference standard: Patient heterogeneity of the population, few biopsies just in some of the patients; no threshold defined to interpret the index test. | All patients demonstrated increased pulmonary PET signal with 68Ga-DOTA-TATE and 18−F-FDG. 68Ga-DOTA-TATE might be useful to identify SSTR overexpression in this patient subgroup, and might be used for selecting patients who might benefit from somatostatin analog treatment. |
| Sarcoidosis and granulomatous diseases | |||||
| Lapa 2016 51 | Prospective | 15 | 68Ga-DOTA-TOC | No source of bias. | Extent of 68 Ga DOTATOC PET positive myocardial areas might provide the same prognostic information as shown for 18F-FDG-PET/CT in myocardial sarcoidosis. Inflammatory cells. |
| Kwekkeboom 1998 52 | Cross-sectional | 46 | 111In-octreotide | Reference test and index test: not all patients had histological proof of granuloma. Lack of standard method for index test analysis. | 111In-Octreotide somatostatin receptor imaging can demonstrate active granulomatous disease in patients with sarcoidosis. |
| Lebtahi 2001 53 | Prospective | 18 | 111In-octreotide and 67 gallium | Reference test and index test lack of in vitro analysis of somatostatin receptor presence in lesions. Lack of standard method for index test analysis. Some patients were receiving steroids previous to the scan. | 111In-octreotide SSTRs seems to be a promising alternative for evaluating the extent of sarcoidosis, detects significantly more sites of sarcoidosis involvement, especially for lung and mediastinal involvement. |
| Kamphuis 2015 54 | Retrospective | 175 | 111In-Octreotide | Reference standard and index test: lack of in vitro analysis of somatostatin receptor expression in the lesions. Lack of standard method for index test analysis. | 111In-Octreotide SRS is additional in the diagnostic workup and more sensitive than conventional imaging in sarcoidosis patients. |
| Gormsen 2016 55 | Pilot study | 19 | 68Ga-DOTA-NOC | Patient selection, reference standard, index test: 3 out of 19 patients had confirmed cardiac sarcoidosis; lack of a real reference test to diagnose the cardiac sarcoidosis; variation observer during the analysis of the index test. | 68Ga-DOTA-NOC can be used as an adjunct imaging modality in patients with suspected cardiac sarcoidosis; preferably as an imaging substitute for the obsolete 67Ga-citrate scintigraphy. |
| Nobashi 2016 56 | Retrospective | 20 | 68Ga-DOTA-TOC 67 Ga | Reference standard: lack of in vitro analysis of SSTR in the lesions. | 68Ga-DOTA-TOC was superior than 67Ga-citrate identifying lymph nodes and in visualizing lesions in the uvea and muscle as well as in the lymph nodes. |
| Piotrowoski 2012 57 | Observational | 32 | 99m Tc-HYNIC-TOC | Reference test and index test: reference test with limitations to detect extrapulmonary disease. Lack of standard method for index test analysis. | Although 99mTc-Hynic-TOC could discriminate between positive and negative studies further studies are needed to find the utility of those results. |
| Weinmmann 2000 58 | Pilot study | 13 | 111In-Octreotide | Reference test and index test: not all patients went o biopsy to confirm the activated SSTRs; Lack of standard method for index test analysis. | 111In-Penteotride identified abnormal uptake in lungs, bone, but not in the skin nor in the liver and central nervous system in patients with granulomatous disease. |
| Oztürk 1994 59 | Descriptive analysis | 3 | 111In-octreotide | Descriptive study on three cases. | Descriptive study showed increased uptake of 111In-penteotride in granulomatous lesions. |
| Vanhagen 1994 60 | Prospective | 20 | 111In-octreotide | Index test: Lack of standard method for index test analysis. | Descriptive study showed increased uptake of 111In-Penteotride in granulomatous lesions |
| Thyroid exophthalmopathy | |||||
| Aguirre Balsalobre 2007 37 | Series of cases | 18 | 111In-Octreotide | Index test: Lack of standard method for index test analysis. | 111In-Octreotide identified active thyroid orbitopathy. Patients identified as positive, treated with lanreotide showed improvement clinically and scintigraphically. |
| Colao 1998 38 | Series of cases | 10 | 111In-Octreotide |
Index test: Lack of standard method for index test analysis. |
They showed that in a semiquantitative analysis with 111In-pentreteotide for patients with higher scores in the orbital uptake, it is possible to predict the therapeutical outcome in these patients. |
| Burggasser 2003 47 | Observational prospective | 44 | 99mTcP829 |
Index test: Lack of standard method for index test analysis. |
Orbital uptake ratios were significantly different between patients with active and non-active orbitopathy. A statistically significant correlation was found between the CAS of the orbital disease and 99mTcP829 tracer uptake. |
| Gerdin 1999 39 | Prospective observational | 22 | 111In-Octreotide |
Index test: Lack of standard method for index test analysis. |
Quantitative measurement of orbital 111Octreotide uptake might be of use in predicting the outcome of immunosuppressive and radiotherapy treatment of patients with Graves ophthalmopathy. |
| Huan Sun 2007 48 | Prospective observational | 14 | 99mTc-Hynic-TOC |
Index test: Lack of standard method for index test analysis. |
Orbital 99mTc-Hynic-TOC can be useful for the estimation of disease activity and prediction of the response to radiotherapy in Graves’ ophthalmopathy patients |
| Kahaly 1998 40 | Prospective observational | 20 | 111In-octreotide | Index test: lack of standard method for index test analysis. | 111In-octreotide was a sensitive technique with a high positive predictive value to select those patients who might benefit from treatment with immunosuppressive agents. |
| Kahaly 1995 41 | Prospective observational | 44 | 111In-Octreotide |
Index test: Lack of standard method for index test analysis. |
Graves’ ophthalmopathy patients showed markedly orbital accumulation of 111In-pentetreotide in contrast to controls. |
| Krassas 1999 42 | Prospective | 14 | 111In-Octreotide |
Index test: Lack of standard method for index test analysis. |
111In-Octreoscan correlates well with the clinical activity of the thyroid exophthalmopathy and orbital accumulation of radioactivity was diminished after treatment with somatostatin analogues. |
| Krassas 1995 43 | Prospective | 20 | 111In-Octreotide |
Index test: Lack of standard method for index test analysis. |
111In-Octreoscan could predict those patients with Graves’ thyroid eye disease who might benefit from treatment. |
| Lincke 2009 50 | Prospective | 73 | 111In-pentetreotide and 68Ga-DOTA-TOC | Index test, reference standard: lack of standard method for index test analysis; there was not immunohistochemical confirmation of activated SSTRs in the thyroid nodules. | Normal thyroid tissue shows detectable 111In-Pentetreotide and 68Ga-DOTA-TOC which could indicate a basal SSTR expression in normal tissue. Hot nodules showed increased uptake of both tracers also for active Hashimoto and Graves. |
| Moncayo 1999 44 | Prospective | 51 | 111In-octreotide | Index test: lack of standard method for index test analysis. | Positive 111In-Octreotide in patients Images provide useful information on the efficacy of immunosuppressive therapy. |
| Nocaudi 1999 45 | Prospective | 17 | 111In-Octreotide | Index test: lack of standard method for index test analysis. | 111In-pentreteotide scintigraphy may be a good indicator of the likelihood of evolution in thyroid-associated ophthalmopathies. |
| Postema 1994 46 | Cross sectional | 58 | 111In-Octreotide | Patient selection, index test: lack of standard method for index test analysis. | Thyroidal and orbital Graves’ disease can be visualized by 111In-Octreotide reflecting disease activity. |
| Rong Zhao 2012 49 | Prospective | 46 | 99mTc-Hynic-TOC | Index test: lack of standard method for index test analysis. | Orbital 99mTc-TOC fusion imaging is able to determine the pathological phase of Graves’ disease, giving a high positive scan in the active early phase and a low positive or negative scan in the stable end phase of the disease. |
Endothelial inflammation and atherosclerosis
In total, we analyzed 9 studies and excluded 2 for the analysis because they did not complete the inclusion criteria; 7 studies with the use of SRS for endothelial inflammation were included, with a total of 262 patients (Table 1). In details, Tarkin et al. [18], in a descriptive study, compared PET with 18F-fluorodeoxyglucose (FDG) and 68Ga-DOTA-TATE to detect culprit coronary and carotid arteries with acute coronary syndrome, transient ischemic attacks and stroke, and demonstrated best results with 68Ga-DOTA-TATE in the diagnostic accuracy to detect stable and unstable inflamed coronary lesions and vascular inflammation in neighboring coronary and aortic vasculature. When age, total cholesterol, and BMI were evaluated with other relevant clinical factors using multi- variate linear regression, they remained significant predictors of 68Ga-DOTATATE mTBRmax. In patients with TIA or stroke, increased 68Ga-DOTATATE inflammatory signals were reliably differentiated between culprit carotid plaques and contralateral nonculprit carotid arteries. Ex vivo 68Ga-DOTATATE carotid autoradiography showed high levels of specific ligand binding to SSTR2 receptors. SSTR2 and CD68 mRNA levels were highly correlated within carotid plaque. Carotid SSTR2 and CD68 mRNA levels also showed strong correlation with in vivo 68Ga-DOTATATE TBRmax values measured at the corresponding level in clinical PET images. These data provided both histological and molecular validation of 68Ga-DOTATATE as specific marker of atherosclerotic inflammation. Under QUADAS analysis, we did not find any significant source of risk bias in this report. Malmberg et al. [19] in an observational study in 60 consecutive patients described the differences between 68Ga-DOTA-TOC and 64Cu-DOTA-TATE in detecting atherosclerotic plaques in different vessels, showing better performance of 64Cu-DOTA-TATE explained by the longer half-life which allows for early as well as late PET scanning, even the day after injection. 64Cu has also a substantially shorter positron range than 68Ga, 1 versus 4 mm, rendering it a much better spatial resolution, but a lower positron abundance [20] Uptake of 64Cu-DOTATATE was significantly higher than 68Ga-DOTATOC in the vascular regions both when calculated as maximum and mean uptake. In a multivariate analysis, there was a significant association between Framingham risk score and the overall maximum uptake of 64Cu-DOTATATE using SUV as well as target-to-background ratio, whereas no association was found with 68Ga-DOTATOC. The association of risk factors and maximum SUV of 64Cu-DOTATATE was found driven by body mass index, smoking, diabetes, and coronary calcium score suggesting the potential use of this radiotracer as noninvasive biomarker of cardiovascular risk. According to QUADAS 2 analysis, we considered the reference test as the main source of risk of bias because it did not use the anatomopathological evidence to validate the results on 68Ga-DOTATOC but the calcium score on CT. Simon Wan et al. [21] conducted a descriptive study with 20 patients with recent stenotic carotid events and described the findings of 68Ga-DOTA-TATE in carotid plaques versus histology. Surprisingly, they did not find any significant uptake of 68GaDOTATOC in the plaques neither activated macrophages expressing SSTR2; and they could not support the use of 68GaDOTATOC for evaluating the inflamed plaque; the source of bias in this report, (misclassification explained by heterogeneity of time between carotid event, research PET, and endarterectomy) could maybe explain the results. In QUADAS 2 analysis, this source of bias corresponds to flow and timing. Pedersen et al. [22], in a population of 10 patients with clinical symptoms of stroke or transient ischemic attack, described the findings of 64Cu-DOTA-TATE uptake in atherosclerotic plaques. 64Cu-DOTA-TATE uptake was significantly higher in symptomatic plaques and correlated with CD163 expression by activated macrophages at histology. We did not find any important source of risk of bias in this report according to QUADAS analysis. Xian Li et al. [23] in a retrospective series of 16 patients, analyzed simultaneously 18F-FDG and 68Ga-DOTA-TATE PET/CT and showed significantly increased uptake in the fibrotic and vulnerable atherosclerotic plaques compared with normal coronary arteries, suggesting a potential role of this tracer for molecular assessment of coronary artery disease. They found higher values of focal uptake with 68GaDOTATATE in patients with high cardiovascular risk and significant correlation between the mean uptake of both tracers and the patient’s score of risk factor. We found that the reference test and the index test were source of risk of bias in QUADAS 2 analysis. Mojtahedi et al. [24] generated a preliminary data by using 68Ga-DOTATATE PET/CT, with in vulnerable or fibrotic atherosclerotic plaques in the coronary arteries. In a population of 44 patients with neuroendocrine tumors (NET) who underwent 68Ga-DOTATATE PET/CT, they found that the mean TBR value in the normal group was 1.345 ± 0.58 while the mean TBR value in the fibrotic plaque group was 1.752 ± 1.50 (p 0.0043) and in atherosclerotic plaques group was 2.043 ± 1.76, p < 0.0001). There was a significant correlation (p = 0.0026) between 68Ga-DOTATATE uptake and the progression to formation of atherosclerotic plaques, based on coronary CT calcium score, HU. Those findings suggested the potential of 68Ga-DOTATATE PET/C for molecular assessment of coronary artery disease. According to QUADAS 2 analysis, we considered as potential source of risk bias the reference standard they used for validate the 68Ga-DOTATATE PET results. Rominger et al. [25] in a descriptive analysis of 70 consecutive patients correlated 68Ga-DOTATATE uptake in the left anterior descending coronary artery with the presence of calcified plaques and cardiovascular risk factors. Higher uptake lead distinguishes between patients with and without coronary calcifications. As in the abovementioned reports, the main source of bias of this series in QUADAS 2 analysis was related to the reference standard they used to validate the 68Ga-DOTATATE results.
It is well known that monocytes and macrophages, being the first inflammatory cells associated with vascular inflammation, play an important role in the pathogenesis of atherosclerosis, contributing to necrotic core formation, fibrous cap thinning, and plaque vulnerability [26]. These cells express SSTR-2 on the cell surface in cultures [27] and therefore 68Ga-DOTA-TATE uptake was thought to have the potential to be a surrogate marker of inflammation to study plaque biology [28]. Taking together all published data, it is likely that there are complex relationships between the stage of plaque evolution (chronic vs acute), macrophage density and activity, SSTR subtype expression, and 18F-FDG and 68Ga-DOTA-TATE uptake. Evidences, so far, show a tendency to confirm the utility of SRS with 68Ga-DOTA-TOC to detect high-risk, vulnerable, atherosclerotic plaques and an interesting correlation with risk factors. Added value of TOC (specific for inflammatory cells only provides an in vivo information on the vulnerability of plaques) vs FDG (global inflammatory burden but non-specific and does not provide a relevant histopathological information) and 18F-Na and calcium score [29].
Rheumatoid arthritis
In total, 11 publications were analyzed, but just 2 clinical studies were included within 36 patients (Table 1), since most were reviews, case reports or in vitro or animal studies. Anzola et al. [30] conducted a pilot study to evaluate the uptake pattern of 99mTc-EDDA/HYNIC-TOC in the joints of 18 patients with rheumatoid arthritis refractory to treatment. They showed high uptake of the molecule in all evaluated joints and also in the salivary glands of some patients as possible evidence of Sjogren syndrome. There was a statistically significant reduction in uptake after treatment with anti-TNFα antibodies in all patients. The authors concluded that this scan can be useful to select and monitor RA patients for therapy with anti-TNFα antibodies. In QUADAS 2 analysis, we found as potential source of risk of bias the index test because the lack of standardized method to evaluate the results. Vanhagen et al. [31] reported the results of 14 patients with RA and 4 with osteoarthritis using 111In-octreotide. They reported sensitivity (uptake of the tracer in swollen and painful joints) of 76% in RA patients and of 20% in osteoarthritis. As in the abovementioned series, we found lack of a standardized method to evaluate the results and weakness in the reference test used to compare the results (QUADAS 2, reference and index test source of bias).
Synovia of patients with active rheumatoid arthritis expresses a high density SSTR [32]. The experience published in these two clinical papers, shows the potential of SRS to localize and identify sites of active inflammation in joints, both symptomatic and asymptomatic, and extra-articular involvement as in salivary glands. The information provided by SRS is different from other imaging modalities and provides in vivo histopathological information on the activity of cell-mediated inflammation. This information has an important impact for therapy decision-making and therapy follow-up as also appears in other studies [33].
Idiopathic pulmonary fibrosis
In total, 7 studies were analyzed, but only 3 studies could be included within 51 patients (Table 1). Ambrossini et al. [34] in an observational study evaluated the potential role of 68Ga-DOTANOC PET/CT in patients with idiopathic pulmonary fibrosis (IPF) and non-specific interstitial pulmonary pneumonia (NSIP). 68Ga-DOTANOC PET/CT findings were compared with HRCT results. In IPF patients, 68Ga-DOTA-NOC uptake appeared as a typical subpleural and peripheral distribution involving both lung fields predominantly at the bases. Areas of 68Ga-DOTA-NOC uptake directly corresponded to pathologic areas on HRCT. In contrast, 68Ga-DOTANOC uptake was faint in NSIP patients and undetectable in healthy control subjects. No significant association was documented in NSIP cases. According to QUADAS 2 analysis, we found as source of potential risk of bias the index test because they did not use a previous standardized method to evaluate the results and they did not confirm the findings under histopathogical analysis.
Lebtahi et al. [35] investigated the expression in vivo of SSTR in the lungs of 11 patients with IPF, and 6 patients with pulmonary fibrosis associated with systemic sclerosis by using 111In-octreotide scintigraphy and compared the results with 19 control patients. They reported higher uptake in all 11 IPF patients and in 4 of 6 systemic sclerosis patients related to normal control population. Increased uptake correlated significantly with different lung function and cytological tests. As in the abovementioned series, according to QUADAS 2 analysis, we found as potential source of risk of bias the index test and the reference test explained by the same conditions argued before.
Win Thida et al. [36] analyzed in an observational study 26 patients with diffuse parenchymal lung disease (10 patients with idiopathic pulmonary fibrosis, 12 with nonspecific interstitial pneumonia and 4 with other forms of interstitial lung disease), by using 68Ga-DOTA-TATE and 18F-FDG by combined PET and HRCT. All patients demonstrated increased pulmonary signal with both 68Ga-DOTA-TATE and 18−F-FDG.
The experience reported in this review shows the potential utility of the SSTR scintigraphy to localize and to detect the active inflammation mediated by an immunological response in idiopathic pulmonary fibrosis. In QUADAS 2 analysis, we found as source of risk of bias the reference test and index test explained by the same reasons argued above.
Graves’ ophthalmopathy
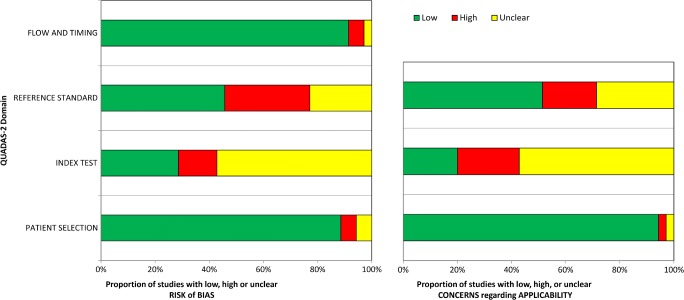
In total, 33 papers were reviewed, 14 studies with in total 451 patients were included (Table 1). Aguirre-Balsalobre et al. [37] in a series of 18 patients affected by thyroid orbitopathy with Graves’ diseases by using a semiquantitative analysis of the images with 111In-pentreotide, demonstrated how patients with higher scores had better response to corticosteroid therapy; according to QUADAS 2, analyzing the source of bias of this experience was related to the index test because lack of standardized method. Colao et al. [38], Gerdin et al. [39], Kahaly et al. [40], Kahaly et al. [41], Krassas et al. [42], Krassas et al. [43], Moncayo et al. [44], Nocaudie et al. [45], Postema et al. [46], in similar study designs by using 111In octreotide, described how patients with active orbitopathy in Graves’ disease had higher uptake of the tracer in the orbits, and how this finding was helpful to discriminate active disease Vs non-active disease and how it helped to choose better the candidates to immunotherapy, radiotherapy or somatostatin analogues therapy. In those series, it was possible to observe how patients with higher uptake in orbits responded well to the installed treatment. The common source of bias for the abovementioned authors according to QUADAS 2 analysis was related to the index test, and although none of the authors used a standardized method to analyze the images, the results were not only similar but also promissory; moreover, in Postema’s report, it was seen with a high frequency of source of risk bias related to patient selection. In Postema’s series, it also found the patient selection as source of risk of bias (Fig. 2).
Fig. 2.
Graphical representation of frequencies of biases in analyzed papers by QUADAS 2
Burggasser et al. [47] in a series of 44 consecutive patients, by using 99mTcP-829, demonstrated statistically the differences in the orbital uptake between control and disease patients and between active and inactive orbitopathy, in Graves’ disease patients with orbitopathy. Even though they used two different methods to analyze the images, we considered the index test as source of bias according to QUADAS 2 analysis. Huang Sung et al. [48], by using 99mTc HYNIC-TOC, reported similar results of the above authors with the same previous described source of bias.
Rong Zhao et al. in a prospective study [49] by using SPECT/CT system as novel technique, investigated the predictive role of the orbital somatostatin receptor scintigraphy with 99mTc-EDDA/HYNIC-TOC (99mTc-TOC) to detect clinical stage of Graves’ ophthalmopathy (GO) and the response to corticosteroid therapy in a sample of 46 patients with GO and four volunteers without eye disease. The treatment effect was evaluated both by the orbital 99mTc-TOC uptake and NOSPECS. Orbital images were quantified by region of interest (ROI) analysis. Semi-quantitative evaluation of retrobulbar uptake was performed with irregular ROIs which were placed over the orbits (O) and the reference area over the occipital area (OC). This prospective study demonstrated marked orbital accumulation of 99m Tc-TOC in 22 GO patients, showing higher activity score and clinical improvement; they demonstrated good correlation of orbital 99m Tc-TOC scintigraphy with CAS. The value of this study was to identify the anatomical structures depicted with 99m Tc-TOC in patients with GO by means of SPECT and CT image fusion analysis. Thus, in the absence of histology, because of a favorable target-to-background ratio and fusion imaging of SPECT/CT in this study, orbital 99mTc-TOC fusion imaging was able to determine the pathological phase of Graves’ disease, giving a high positive scan in the active early phase and a low positive or negative scan in the stable end phase of the disease. We consider that the analysis of the images under hybrid images diminishes the risk of bias related in index test (QUADAS 2).
Lincke et al. [50] is the only report so far that used PET study in thyroid-related pathologies. He compared the characteristics of uptake between 111In-pentreotide and 68Ga-DOTA-TOC in normal and pathologically altered thyroid glands and found that both tracers showed higher uptake in active Hashimoto and Graves’ disease most likely caused by SSTR expressing lymphocytes in the thyroid tissue; however, the physiologic or pathophysiologic relevance of the increased In-111 pentetreotide and Ga-68 DOTATOC uptake in normal thyroid glands, hot and cold nodules, and goiters and nodular thyroids remain to be determined. According to QUADAS 2 analysis in this report, the index test and the reference test were considered as unclear sources of bias.
During the last 20 years, it demonstrated the utility of SSTRs scintigraphy identifying active orbitopathy in Graves’ exophthalmopathy. No matter as a common source of bias in those series it was found to be lacking of validated method to evaluate the SSTR scintigraphies, all the authors reported similar results showing scintigraphic patterns consistently with high uptake of the molecule in the periorbitary zone as evidence of active disease with prognostic implications.
Sarcoidosis and other chronic inflammatory diseases
As far as sarcoidosis is concerned, were reviewed 18 publications, of which 6 were excluded (Table 1). Lapa et al. [51] in an observational study conducted a pilot prospective study in 6 patients with active peri−/myocarditis and 6 with sub-acute myocardial infarction, who underwent SSTR-PET/CT, 68Ga DOTA-TOC and cardiac MRI within 3–10 days after onset of symptoms. They compared the results under semiquantitative analysis with 12 oncologic patients with no history of coronary artery disease. In patients with clinical evidence of myocarditis, PET/CT returned 26 positive segments and MRI 13 segments, respectively. In patients with myocardial infarction, there were 29 68Ga-DOTA-TOC positive segments and 31 abnormal segments in MRI. On a head-to-head comparison, SSTR-PET and MRI were concordantly positive in 36 segments (76.6%). Nineteen segments were SSTR-PET positive and MRI-negative (9.3%; 19/204), and 11 SSTR-PET negative and MRI-positive (5.4%; 11/204). Both modalities returned negative results in 138 segments, thus leading to an overall concordance of 85.3%. Agreement of the modalities was higher in patients with myocardial infarctions. SUV mean and SUV max were significantly higher in the infarcted/ inflamed myocardium as compared with remote myocardium or the left ventricular (LV) cavity. We did not find any relevant risk of bias according to QUADAS 2 analysis (Fig. 3). The overall concordance of the 2 modalities was 96.1%. Kwekkeboom et al. [52] in a cross sectional study in 46 patients with known mediastinal, hilar, and interstitial sarcoidosis, by using SRS with 111In-pentetreotide showed positive results in 36 out of 37 patients with known pathology, and in 7 with normal X-rays. In 13 patients who had no evidence of extrapulmonary disease involvement with physical examination and conventional imaging, somatostatin receptor imaging revealed abnormal uptake of radioactivity outside the chest. Neither the degree of radioactive accumulation nor a specific pattern of pathological uptake was correlated with disease severity or clinical course. They repeated the scintigraphy on 13 patients, 5 of 6 patients who showed X-rays improvement, the SSTRs also improved. Two of 5 patients whose X-rays did not improve, lung function and SSTRs improved. They could not conclude that pentetreotide scintigraphy has a role in predicting prognosis or clinical course in patients with sarcoidosis. According to QUADAS 2 analysis, the source of risk of bias in this series was related to the lack of a standardized method to evaluate the results in the index test, and also we found a low concern related to the reference test used in some situations. Lebtahi et al. [53] in an observational study demonstrated the superiority of 111In pentetreotide compared with 67Ga scintigraphy in the evaluation of pulmonary and extrapulmonary involvement in 18 patients with proven sarcoidosis especially in the hilar or mediastinal area. Nine were or recently had been receiving steroid therapy at the time of the examination. Gallium scintigraphy found abnormalities in 89% of patients and detected 65% of the clinically involved sites. SRS found abnormalities in 100% of patients and detected 83% of clinically involved sites. Of the 9 treated patients, gallium scintigraphy found abnormalities in 78%, detecting 59% of the clinically involved sites whereas SRS found abnormalities in 100%, detecting 82% of the clinically involved sites. SRS images were consistently better than gallium images, with well-delineated lesions, especially in the hilar or mediastinal area, on either planar or SPECT images. They concluded that SSTRs seems to be a promising alternative to gallium scintigraphy for evaluating the extent of sarcoidosis, detects significantly more sites of sarcoidosis involvement with lesion contrast significantly higher than with gallium scintigraphy, especially for lung and mediastinal involvement. Despite the good results reported, we found as potential source of bias in QUADAS 2 analysis the lack of standardized method to evaluate the images on 111In pentetreotide and also the lack of a well-defined reference test. Kamphuis et al. [54] in a retrospective study evaluated the additive value of SRS scintigraphy with 111In pentetreotide in the clinical evaluation of sarcoidosis and compared the results with chest X-ray and CT. In both histologically proven and unproven sarcoidosis, in all but one SSTR uptake was demonstrated. In the thoracic region SRS increased the yield with 36% and 32% in comparison with X-ray and CT, respectively. In the histologically proven group, there were no negative SRS results, and the SRS increased the yield for thoracic localization in 30% and 14% of the patients in comparison with X-ray and CT, respectively. As in the abovementioned series, although the results reported were encouraging, we found in QUADAS 2 analysis that the lack of a standardized method for evaluating the SRS scintigraphy with 111In pentetreotide was a source of potential bias as well as the reference test was source of potential risk of bias. Gormsen et al. [55]in a pilot study in 19 patients with suspected cardiac sarcoidosis compared the diagnostic accuracy and inter-observer variability of 68Ga-DOTANOC vs 18F-FDG PET/CT. Cardiac sarcoidosis (CS) was diagnosed in 3/19 patients. By consensus, 11/19 18F-FDG scans were rated as inconclusive, resulting in low agreement among reviewers (Fleiss combined kappa 0.27) and correspondingly poor diagnostic accuracy; for 68Ga-DOTANOC, no scan was rated as inconclusive but it was reported as a poor interobserver agreement (Fleiss combined kappa 0.46). The sensitivity of 18F-FDG PET for diagnosing CS was 33%, specificity was 88%, PPV was 33%, NPV was 88%, with 79% of diagnostic accuracy; in contrast to 68Ga-DOTANOC, and accuracy was 100%. 68Ga-DOTANOC PET/CT looks very promising as an alternative CS PET tracer. When we analyzed under QUADAS 2 protocol, we found in the index test and reference test the potential source of risk of bias.
Fig. 3.

Graphical representation of biases in each analyzed papers by QUADAS 2
Nobashi et al. [56] in a descriptive study compared the utility of 68Ga-DOTA-TOC with conventional 67Ga-citrate in the visualization of active sarcoidosis and correlated quantitative parameters on 68Ga-DOTA-TOC PET/CT with clinical data. Twenty patients with sarcoidosis underwent both studies. The diagnosis was confirmed in 12 patients histologically and in the other 8 on clinical and paraclinical data. Active lesions were identified by visual interpretation when focal increases in radioactivity were higher than the normal biodistribution of tracers. Quantitative analysis on 68Ga-DOTATOC was made by using SUVmax values. DOTATOC-PET/CT showed abnormal findings in 19 patients, whereas 67Ga showed abnormal findings in 17. DOTATOC was superior than 67Ga identifying lymph nodes (p < 0.046). SUVmax in each organ did not show statistical difference between involved organs; however, the average SUVmax of lymph nodes was highest among the involved organs. It was not seen as statistically different in SUVmax between patients with and without symptoms. Active lesion volume calculated by DOTATOC-PET moderately correlated with serum ACE concentrations. 68 GaDOTATOC-PET was superior to 67Ga in visualizing lesions in the uvea and muscle as well in the lymph nodes. As a source of bias, there was partial verification bias because the lack of in vitro analysis of somatostatin receptor in the lesions and because not all patients were diagnosed by the same reference standard. There is patient variation bias in some patients who were receiving treatment for the clinical condition in the same time when there were acquired studies. According to QUADAS 2 analysis, the potential source of bias in this series relied on the index test and reference standard explained by the same arguments in the above references.
Piotrowoski et al. [57], in an observational study, evaluated 32 patients with sarcoidosis and used 99mTc-HYNIC-TOC scintigraphy as a reference method to evaluate the clinical usefulness of traditional markers, such as angiotensin-converting enzyme (SACE), C-reactive protein (CRP), serum calcium (S-Ca2+ level, and 24-h Urinary-Ca2+ los, bronchoalveolar lavage fluid (BALF lymphocytes) as well as of a novel marker of lipid peroxidation-8-IP in exhaled breath condensate (EBC 8-IP). They divided the patients according to the 99mTc-HYNIC-TOC results in two groups: grade 1 (20 patients) when the scintigraphy was positive for an abnormal uptake in thorax and grade 0 (12 patients) when the scan was negative. The only significant difference between scintigraphic negative vs positive results was found in the level of EBC 8-IP; unfortunately, this marker is not specific for sarcoidosis. Furthermore, it observed a trend towards higher levels of SACE in the group with positive radiotracer uptake. Although the tendency was noticed towards higher percentage in patients with positive scintigraphy results, the statistical significance was not reached. It was not possible to demonstrate the capacity of any laboratory test to estimate the intensity of the inflammatory process. The SSRTs could discriminate between positive and negative studies but further studies are needed to find the utility of those results. The reference standard was the most frequent source of bias and applicability concern in QUADAS analysis.
SRS has been proposed also for studying other chronic inflammatory conditions, in particular in histiocytosis, tuberculosis, cardiac allograft rejection, and small vessel vasculitis. Weinmann et al. [58] evaluated 13 patients with histiocytosis. Lung uptake of 111In-pentreotride visually and semiquantitative analyzed was statistically significantly higher in patients compared with controls. This report showed concern as potential source of bias in the reference and index test. Oztürk et al. [59] described three similar cases: 2 patients with pulmonary sarcoidosis and one with tuberculosis by 111In-pentreotide scintigraphy; this report generated in QUADAS 2 analysis concern about the source of risk of bias in the three items contained in the evaluation: patient selection, index test, and reference standard. Vanhagen et al. [60] reported in a consecutive series of 20 patients the utility of 111In-octreotide localizing sites of granuloma infiltration in patients with sarcoidosis and tuberculosis. In vitro autoradiography of fresh tissue biopsies showed bonding of the molecule at sites that were microscopically identified as granulomatous disease. The major contribution of this study was that this scintigraphy procedure demonstrated the expression of somatostatin receptor in such kind of granulomas. Under QUADAS 2 analysis, we found index test as a potential risk of bias because of the lack of a standardized method to evaluate the results.
Aparici et al. [61] conducted a prospective study in 13 patients with suspected cardiac allograft rejection to assess the feasibility of SRS with 111In-pentreotide to target activated lymphocytes in transplanted heart as a possible early marker of rejection. A high cardiac uptake was observed in 8 patients: 3 had an acute rejection and 5 had mild or no rejection. However, in 4 of the 5 patients with no rejection at time of study, a biopsy, performed 1 week later, demonstrated a significant rejection requiring treatment. These preliminary results indicate the feasibility of targeting activated lymphocytes for the detection of cardiac allograft rejection and suggest a possible predictive role of SRS. These preliminary results indicate the feasibility of targeting activated lymphocytes with somatostatin receptor imaging in the detection of cardiac allograft rejection.
Index test generated in QUADAS analysis the high concern as source of bias and eligibility concern. The method used to evaluate the pattern uptake was not validated previously.
Neumann et al. [62], by using 111 In-pentreotide, analyzed 32 consecutive patients with ANCA-associated small vessel disease (AASV). Disease activity was evaluated with the Birmingham Vasculitis Activity Score (BVAS). For pulmonary AASV, SRS showed a sensitivity of 86% and a specificity of 96% with a positive predictive value of 97% for active disease. False negative scans were seen in patients under immunosuppressive therapy. In patients with ear/nose/throat involvement, SRS showed a sensitivity of 68% and a specificity of 100% with a positive predictive value of 100%. In patients who responded to therapy and went into full remission, repeat SSTR scintigraphy demonstrated the absence of previously present tracer accumulation; patients with aggressive disease who responded poorly to immunosuppressive therapy remained positive at repeat scintigraphy. Immunohistochemical analysis for SSTR2 and SSTR3 was performed on three open lung biopsies in active disease obtained from two patients with Wegener’s granulomatosis (WG) and one patient with microscopic polyangiitis as well as on nasal and lung tissue of one autopsy case with WG. All specimens demonstrated STR2 y and STR3 expression on monocytes-macrophages and giant cells surrounding granulomas and occasionally in the center of the granulomatous reactions. The reference standard generated in QUADAS analysis high concern as source of bias and applicability concern, because the immunohistochemical analysis was obtained just in three patients.
Reported evidence so far shows the utility of 68Ga-DOTA-TOC for detecting sarcoidosis lesions, especially for lymph nodes, uvea, and muscles, as well as for vasculitis and other chronic inflammatory diseases. In particular, the results obtained for monitoring cardiac allografts open a new important clinical application of SRS to early detect lymphocytic infiltration in transplanted tissues and to monitor the effect of therapies in preventing rejection.
Discussion
This is the first systematic review performed about the usefulness of SRS (both SPECT and PET) to diagnose chronic inflammatory diseases. The role of somatostatin as mediator in inflammatory processes and how different immunological cells express SSTRs is well known. The possibility to specifically target the SSTRs by molecular imaging gave us the opportunity to visualize active inflammation in a variety of inflammatory disorders.
In general, based on the results of this systematic review, we found that SRS has a large potential to be used as diagnostic tool in patients suspected to have chronic inflammatory diseases. The evidence reported until now is supported mainly by observational studies that were designed to investigate different groups of chronic inflammatory conditions: we found a wide heterogeneity in used protocols, in studied conditions, and in the studied population. Furthermore, we observed that in almost every study a validated and standard method to analyze the images was lacking, a condition that became the most important source of bias.
The most frequent pathology evaluated by PET was the endothelial inflammation and vulnerable plaques, where promising correlations between quantitative uptake and histopathology were found, emphasizing the role of SRS for this inflammatory condition. Monocytes and macrophages were the first inflammatory cells to be associated with atherosclerosis. They are believed to play important roles in its pathogenesis, contributing to necrotic core formation and fibrous cap thinning in advanced atherosclerosis, features thought to confer vulnerability [26] It is known that human macrophages express sst2 on their cell surface in cell culture [27]. 68Ga-DOTATATE, a specific sst2 receptor agonist, therefore was thought to have the potential to be a surrogate marker of inflammation to study plaque biology [28]. Taken together, it is likely that there are complex relationships between stage of plaque evolution (chronic vs. acute), macrophage density and activity, somatostatin receptor subtype expression, 18F-FDG, and somatostatin receptor PET signal. The today evidence shows a high tendency to confirm the utility of the SSTRs 68GaDOTATOC to detect the high risk atherosclerotic plaque and its interesting correlation with risk factors. Studies are needed to confirm those finding with better designs which enables to choose better the study population, to calculate a good sample size and to validate the findings with good references tests.
The peripheral nervous system and its neuropeptidergic pathways may play an important role in the pathogenesis and development of rheumatoid arthritis. Somatostatin via its receptors has shown to be implicated in inflammatory diseases and particularly it is known how the synovium in active rheumatoid arthritis express a high density of somatostatin receptors [32]. The experience published in these papers although lacks of a rigorous methodology, shows the potential of radiolabeled somatostatin receptors to localize and identify sites of active inflammation in joints and extra articular involvement and to identify the patients who could benefit of the therapy. In this setting it will be necessary to conduct rigorous prospective studies to validate the methodology to make an accurate approach in arthritis patients.
Different radiotracers were used in patients with Idiopathic Pulmonary Fibrosis (IPF). Ambrosini reported results with 68Ga-DOTANOC, which presents the broader SSTR-subtype affinity [63], a favorable dosimetry, and no uptake in the intact lung [64]; recent preclinical evidence demonstrated SSTR expression on fibroblasts of both murine models of IPF and human tissue samples from IPF patients [65]. Although 68Ga-DOTANOC binding sites within the lungs cannot be precisely localized without direct sampling, the evidence that tracer uptake was observed in IPF cases allows one to speculate that PET with 68Ga-DOTANOC might be useful to identify SSTR overexpression in this patient subgroup. In Ambrosini’s report areas of 68Ga-DOTANOC uptake directly corresponded to pathologic areas on HRCT and the preliminary data supported the hypothesis that SSTR is over expressed in the lungs of IPF patients. Lebtahi showed an interesting correlation between STRR scintigraphy findings with 111In-Octreotide in IPF patients and functional pulmonary tests. Win Thida reported results with 68Ga-DOTATATE and 18F-FDG with similar pattern of distribution with both tracers. The experience above mentioned, although has methodological deficiencies showed clearly the potential utility of STRRs imaging detecting active disease in pulmonary fibrosis and opening the possibility to include this technique not only for controlling the response to the therapy, but selecting those who might benefit from somatostatin analog treatment or combined approaches in which 68Ga-DOTANOC may function as a carrier for specific antifibrotic drugs or cytotoxic isotopes.
The evidence that 111In-DTPA octreotide is highly concentrated in the orbits of patients with Graves’ ophthalmopathy indicated new frontiers in the diagnostic work-up of the disease [46]. Somatostatin receptors, especially SSTR-2 and SSTR-5 subtypes, with high affinity for octreotide [66] are found in retro-ocular muscles and retrobulbar fat of Graves’ ophthalmopathy. During the active phase of disease, activated lymphocytes also express somatostatin receptors. Several studies [39, 41] have already shown that scintigraphy with indium-111 pentetreotide can reveal massive orbital uptake of this analogue of somatostatin in cases of thyroid-associated ophthalmopathy, in contrast to other non-thyroid causes of exophthalmia. Because of the kinetics of the radiotracer and because of the increased blood flow occurring in active thyroid-associated ophthalmopathy, the early pentetreotide accumulation is high and, according to Kahaly et al. [41], could be a sensitive criterion of active disease. Thyroid-associated ophthalmopathy (TAO) is one of the most difficult autoimmune disorders to investigate. The clinical definition of the activity of the ophthalmopathy at the initial presentation is crucial to the identification of the correct therapeutic approach [67]. The treatment of TAO is based on immunosuppressive therapy, such as the use of corticosteroids or radiation, or surgical therapy [68]. Immunosuppression is considered beneficial only in the early active stage, whereas surgery represents the treatment for the end stage of the disease. On the basis of this evidence, a new approach, using labeled somatostatin analogues intended to highlight the presence of activated T lymphocytes in orbital tissue, was attempted in order to identify the early stage of TAO, which should be particularly sensitive to immunosuppressive treatment [69]. Although the evidence to date is characterized by series with lack of standardized methods for evaluating the scintigraphic findings, there is a common trend to demonstrate a potentially relevant role for SRS in the pretreatment evaluation of TAO [70], showing for instance a positive correlation between clinical activity score and 111In-octreotide uptake in patients with TAO [40, 46]. Similarly, others [39] reported that visual semi-quantitative analysis of 4 h/24 h planar images during SRS was correlated with the ophthalmologic progression. As the presence of activated lymphocytes in the orbit represents the first requisite for the effectiveness of corticosteroid therapy and as it can be revealed by SRS, recently, this approach was attempted in patients with TAO. The results of orbital 111In-octreotide uptake predicted the response to corticosteroid therapy in these patients [38]. Nocaudie et al. [45] found that all patients with severe thyroid ophthalmopathy with positive 111In-DTPA Octreotide results showed clinical improvement at 6 months, whereas patients with negative SRS results had not improved. Although a larger group of patients should be investigated before definitive conclusions can be drawn, SRS seems to be a useful method for predicting the clinical response to immunosuppressive treatment in patients with TAO. This might avoid the use of corticosteroid therapy in patients for whom it would have only adverse effects, and might delay surgical treatment for those patients who could benefit from other kinds of medical therapy. Furthermore, some authors [41, 44] demonstrated how 111In-octreotide uptake in both orbits was significantly lower after corticosteroid and irradiation treatment [41] and after immunosuppressive therapy [43].
The experience reported in sarcoidosis has the biggest sample of patients (275). In cardiac sarcoidosis, SSTRs might allow for direct assessment of disease activity, especially in the course of treatment. While the current gold standard MRI depicts structural changes like cardiac damage and scarring and edema with the highest spatial resolution, 68Ga-DOTATOC uptake may directly reflect the underlying immunological cell activity. In the future, given the complementary nature of PET and MRI signals, the combination of the two may be the optimal diagnostic approach, preferably by integrated MRI/PET. Additionally, whereas a recent study [56] comparing 68Ga-DOTANOC and 18F-FDG PET/CT has demonstrated encouraging diagnostic accuracy for SSTR-directed PET, the prognostic value of 68Ga-DOTATOC PET/CT, especially in comparison to 18F-FDG has to be clarified in future trials. Sarcoidosis is a multisystem granulomatous disorder, most frequently involving the lungs, skin, or eyes. Somatostatin receptor scintigraphy (SRS) can visualize sarcoid granulomas through binding of a radionuclide-coupled somatostatin analog to somatostatin receptors that are expressed in sarcoidosis. Somatostatin receptor subtype 2 (SST2) is highly expressed in sarcoid granulomas and used as a substrate for somatostatin receptor scintigraphy (SRS) with 111 In-DTPA octreotide and the pendant in PET imaging with 68Gallium-labeled somatostatin analogs [71, 72]. The use of SSTR-targeted radiotracers to assess sarcoidosis disease activity is not a novel idea. Giant cells, epithelioid cells, and lymphocytes constitute the bulk of active inflammatory cells in sarcoid granulomas and express SSTRs abundantly [56]. 68Ga-DOTANOC PET/CT detected significantly more sites than 67Gallium scintigraphy (P 0.00 l), especially for thoracic and central nervous system involvement, and appeared more accurate for evaluation of disease activity. 68GaDOTATOC-PET was also used and was superior to 67Ga in visualizing lesions in the uvea and muscle as well in the lymph nodes in patients with proven sarcoidosis. Three reports [52–54] demonstrated the utility of 111In-pentreotide detecting extrapulmonary disease involvement in sarcoidosis and its superiority related to 67Gallium nevertheless neither the degree of radioactive accumulation nor a specific pattern of pathological uptake was correlated with disease severity or clinical course, and the SSTRs augmented the yield for thoracic localization in 30% and 14% of the patients for X-rays and CT respectively. There is one report [57] that used 99mTcHYNIC-TOC in sarcoidosis patients and compared the results with laboratory tests, and although the SSTRs clearly could discriminate between positive and negative studies, further studies are needed to find the utility of those results. The evidence about the utility of radiolabeled somatostatin receptor in granulomatous diseases is weak, and although in references found the authors have reported increase uptake of the tracer in the inflammatory focus and visualization of granuloma sites with 111In-pentetreotide, the use of radiolabeled somatostatin receptor in patients with granulomatous disease, such as sarcoidosis, tuberculosis, and Wegener’s granulomatosis [73] has also been previously reported; further studies would be important to validate the technique tested with good reference tests and with new radiolabeled somatostatin receptors as with 68Ga tracers. The characteristics of 67Gallium, as far as lower lesion contrast, the physiological uptake, and the photon energy, are overcome by the characteristics of SSTRs, making it a promising alternative to scintigraphy for evaluating the extend of sarcoidosis [53].
The invasive nature of endomyocardial biopsy has led to a search for alternative diagnostic modalities for the detection of cardiac allograft rejection. The rejection process usually presents with lymphocyte infiltration with or without myocyte necrosis, which indicates the severity of cardiac allograft rejection and the necessity of treatment. Activated lymphocytes express somatostatin receptors; thus somatostatin receptor imaging could be used to target them. The published experience shows the attractive possibility to screen cardiac graft rejection. It is a series of cases with the limitation of the radioligand labeled with 111−In, with a source of bias, misclassification, explained by the technical limitations of the index test, not only because the lack of a validated method to evaluate the findings but the image characteristics of the 111In as radioligand. It would be interesting to conduct a prospective study by using 68Ga compounds.
The upper and lower respiratory tract are common targets in antineutrophil cytoplasmic antibody (ANCA)-associated small vessel diseases (AASV) such as Wegener’s granulomatosis (WG), microscopic polyangiitis (MPA), and the Churg–Strauss syndrome (CSS). Although ANCAs have been proven as an important diagnostic tool [74], it has to be emphasized that, especially in limited AASV, a negative ANCA result does not exclude the diagnosis of active WG or MPA [75]. In AASV, activated T cells are believed to play a central role in pathogenesis [76] and the prominence of T cells and monocyte–macrophages has been demonstrated in lung [77] ear, nose, and throat (ENT) [78] and kidney specimens of active AASV [79]. The promissory results of Neuman’s experience highlight the potential value of SSTR scintigraphy as a non-invasive diagnostic procedure that could detect active disease early in the course of (AASV) and register disease extent, reflecting also response to treatment.
Conclusions
The evidence summarized in this systematic review highlights the promising results of the potential value of SSTR scintigraphy to detect active disease in different inflammatory conditions mediated by activated somatostatin receptors; although the lack of standardized methods for evaluating the parameters in the index test was the most common characteristic in the majority of the series, there was a clear trend to report positive results related to activated somatostatin receptors in the different organs affected by the inflammatory conditions. In this review, the most solid results had to do with the potential in the atherosclerotic plaque field where undoubtedly the contribution of nuclear medicine by PET/CT systems provided important information about the prediction of acute cardiac events. Because of the methodological limitations in the other series, the results must be rigorously analyzed without ignoring the probity of the molecule.
As a future perspective, it is meaningful to encourage the scientific community to advocate the conduction of large and robust prospective studies with the intention of validating the technique in different scenarios; henceforth, considering the inclusion of this tool in different decision-making trees for diagnostic and prognostic purposes.
Compliance with ethical standards
Conflict of interest
The authors declare they have not conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was not obtained.
Footnotes
This article is part of the Topical Collection on Infection and Inflammation
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chianelli M, Parisela M, DÁlessandria C, et al. The developing role of peptide radiopharmaceuticals in the study of chronic inflammation: new techniques for novel therapeutic options. Q J Nucl Med. 2003;47:256–269. [PubMed] [Google Scholar]
- 2.Chianelli M, Mather SJ, Martin-Comin J, et al. Radiopharmaceuticals for the study of inflammatory processes. A review. Nucl Med Commun. 1997;18:437–455. doi: 10.1097/00006231-199705000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Anzola LK, Galli F. Dierck RA. SPECT radiopharmeceuticals for imaging chronic inflammatory diseases in the last decade. Q J Nucl Med Mol Imaging. 2015;59:197–213. [PubMed] [Google Scholar]
- 4.Bhanat E, Koch C, Paramr R, Garla V, Vijayakumar V. Somatostatine receptor expression in non-classical locations-clinical relevance? Reviews in Endocrine and Metabolic Disorders. 10.1007/s11154-018-9470-3. [DOI] [PubMed]
- 5.Cascini GL, Cuccurullo V, Tamburrini O, et al. Peptide imaging with somatostatin analogues: more than cancer probes. Curr Radiopharm. 2013;6:36–40. doi: 10.2174/1874471011306010006. [DOI] [PubMed] [Google Scholar]
- 6.Sosabowski J, Melendez A, Mather S. Radiolabelling of peptides for diagnosis and therapy of non-oncological disease. Q J Nucl Med. 2003;43:223–237. [PubMed] [Google Scholar]
- 7.Rambaldi PF, Cuccurullo V, Briganti V. The present and future role of 111In pentetreotide in the PET era. Q J Nucl Med Mol Imaging. 2005;49(3):225–235. [PubMed] [Google Scholar]
- 8.Brazeau P, Vale WW, Burgus R, et al. Hypothalamic polypeptide that inhibits the secretion of immunoreactive pituitary growth hormone. Science. 1973;5(179):77–79. doi: 10.1126/science.179.4068.77. [DOI] [PubMed] [Google Scholar]
- 9.Patel YC, Reichlin S. Somatostatin in hypothalamus, extrahypothalamic brain, and peripheral tissues of the rat. Endocrinology. 1978;102:523–530. doi: 10.1210/endo-102-2-523. [DOI] [PubMed] [Google Scholar]
- 10.Narayanan S, Kunz PL. Role of somatostatine analogues in the treatment of neuroendocrine tumors. J Natl Compr Cancer Netw. 2015;13:109–117. doi: 10.6004/jnccn.2015.0012. [DOI] [PubMed] [Google Scholar]
- 11.Duet M, Liote F. Somatostatine and somatostatine analog scintigraphy: any benefits for rheumatology patients? Joint Bone Spine. 2004;71:530–535. doi: 10.1016/j.jbspin.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 12.Cascini GL, Cuccurullo V, Mansi L. The non tumor uptake of 111In octreotide creates new clinical indications in benign diseases, but also in oncology. Q J Nucl Med Mol Imaging. 2010;54:24–36. [PubMed] [Google Scholar]
- 13.Wouter AP, de Blois E, Chan HS, et al. 68Ga-labeled DOTA-peptides and 68Ga-labeled radiopharmaceuticals for positron emission tomography: current status of research, clinical applications, and future perspectives. Semin Nucl Med. 2011;41:314–321. doi: 10.1053/j.semnuclmed.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 14.Signore A, Lauri C, Auletta S, Anzola K, Galli F, Casali M, Versari A, Glaudemans AWJM. Immuno-imaging to predict treatment response in infection, inflammation and oncology. J Clin Med. 2019;8:681. doi: 10.3390/jcm8050681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 16.Higgins JPTAD, Sterne JAC. Assessing risk of bias in included studies. In: Higgins JPT, Green S, eds. Cochrane handbook for systematic reviews.
- 17.Whitting PF, Rutjes AWS, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–536. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 18.Tarkin JM, Joshi FR, Evans NR, et al. Detection of atherosclerotic inflammation by 68Ga-DOTATATE PET compared to 18FFDG PET imaging. J Am Coll Cardiol. 2017;69(14):774–791. doi: 10.1016/j.jacc.2017.01.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Malmberg C, Ripa RS, Johnbeck CB, et al. 64Cu-DOTATATE for noninvasive assessment of atherosclerosis in large arteries and its correlation with risk factors: head-to-head comparison with 68Ga-DOTATOC in 60 patients. J Nucl Med. 2015;56:1895–1900. doi: 10.2967/jnumed.115.161216. [DOI] [PubMed] [Google Scholar]
- 20.Velikyan I. Prospective of 68Ga-radiopharmaceutical development. Theranostics. 2013;4:47–80. doi: 10.7150/thno.7447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wan SMY, Endozo R, Michopoulou S, et al. PET/CT imaging of unstable carotid plaque with 68 Ga-labeled somatostatin receptor ligand. J Nucl Med. 2017;58:774–780. doi: 10.2967/jnumed.116.181438. [DOI] [PubMed] [Google Scholar]
- 22.Pedersen SF, Sandholt VB, Keller SH, et al. 64Cu-DOTA-TATE PET/MRI for detection of activated macrophages in carotid atherosclerotic plaques. Arterioscler Thromb Vasc Biol. 2015;35:1696–1703. doi: 10.1161/ATVBAHA.114.305067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li X, Samnick S, Lapa C, et al. 68Ga-DOTA-TATE PET/CT for the detection of inflammation of large arteries: correlation with 18F-FDG, calcium burden and risk factors. EJNMMI Res. 2012;2:52–62. doi: 10.1186/2191-219X-2-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mojtahedi A, Alavi A, Thamake S, et al. Assessment of vulnerable atherosclerotic and fibrotic plaques in coronary arteries using 68Ga-DOTATATE PET/CT. Am J Nucl Med Mol Imaging. 2015;5(1):65–71. [PMC free article] [PubMed] [Google Scholar]
- 25.Rominger A, Saam T, Vogl E, et al. In vivo imaging of macrophage activity in the coronary arteries using 68Ga-DOTATATE PET/CT: correlation with coronary calcium burden and risk factors. J Nucl Med. 2010;51:193–197. doi: 10.2967/jnumed.109.070672. [DOI] [PubMed] [Google Scholar]
- 26.Moore KJ, Tabas I. Macrophages in the pathogenesis of atherosclerosis. Cell. 2011;145:341–355. doi: 10.1016/j.cell.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Armani C, Catalani E, Balbarini A, et al. Expression, pharmacology, and functional role of somatostatin receptor subtypes 1 and 2 in human macrophages. J Leukoc Biol. 2007;81:845–855. doi: 10.1189/jlb.0606417. [DOI] [PubMed] [Google Scholar]
- 28.Rinne P, Hellberg S, Kiugel M, et al. Comparison of somatostatin receptor 2-targeting PET tracers in the detection of mouse atherosclerotic plaques. Mol Imaging Biol. 2016;18:99–108. doi: 10.1007/s11307-015-0873-1. [DOI] [PubMed] [Google Scholar]
- 29.Signore A, Anzola LK, Auletta S, et al. Current status of molecular imaging in inflammatory and autoimmune disorders. Curr Pharm Des. 2018;24:1–11. doi: 10.2174/138161282401180322163953. [DOI] [PubMed] [Google Scholar]
- 30.Anzola LK, Chianelli M, Galli F, et al. Somatostatin receptor scintigraphy in patients with rheumatoid arthritis and secondary Sjögren’s syndrome treated with infliximab: a pilot study. EJNMMI Res. 2016;6(1):49–60. doi: 10.1186/s13550-016-0202-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vanhagen PM, Markusse MH, Lamberts SWJ, et al. Somatostatin receptor imaging the presence of somatostatin receptors in rheumatoid arthritis. Arthritis Rheum. 1994;37(10):1521–1527. doi: 10.1002/art.1780371017. [DOI] [PubMed] [Google Scholar]
- 32.Reubi JC, Waser B, Markusse HM, et al. Vascular somatostatin receptors in synovium from patients with rheumatoid arthritis. Eur J Pharmacol. 1994;271:371–378. doi: 10.1016/0014-2999(94)90796-X. [DOI] [PubMed] [Google Scholar]
- 33.Malviya G, Signore A, Lagana B, et al. Radiolabelled peptides and monoclonal antibodies for therapy decision making in inflammatory diseases. Curr Pharm Des. 2008;14:2401–2014. doi: 10.2174/138161208785777414. [DOI] [PubMed] [Google Scholar]
- 34.Ambrosini V, Zompatori M, De Lucca F, et al. Ga-DOTANOC PET/CT allows somatostatin receptor imaging in idiopathic pulmonary fibrosis: preliminary results. J Nucl Med. 2010;51:1950–1955. doi: 10.2967/jnumed.110.079962. [DOI] [PubMed] [Google Scholar]
- 35.Lebtahi R, Moreau S, Marchan-Adam S, et al. Increased uptake of 111In-octreotide in idiopathic pulmonary fibrosis. J Nucl Med. 2006;47:1281–1287. [PubMed] [Google Scholar]
- 36.Win T, Screaton NJ, Porter J, et al. Novel positron emission tomography/computed tomography of diffuse parenchymal lung disease combining a labeled somatostatin receptor analogue and 2-deoxy-2 18F Fluoro-D-glucose. Mol Imaging. 2012;11(2):91–98. doi: 10.2310/7290.2011.00030. [DOI] [PubMed] [Google Scholar]
- 37.Aguirre-Balsalobre F, Mengual-Verdu E, Muñoz-Acosta JM, et al. Octreotide scintigraphy in thyroid orbitopathy. Arch Soc Esp Oftalmol. 2007;82:133–140. doi: 10.4321/s0365-66912007000300004. [DOI] [PubMed] [Google Scholar]
- 38.Colao A, Lastoria S, Ferone D, et al. Clinical response to corticosteroid therapy in patients with graves ophthalmopathy. J Clin Endocrinol Metab. 1998;83:3790–3794. doi: 10.1210/jcem.83.11.5274. [DOI] [PubMed] [Google Scholar]
- 39.Gerdin MN, Van der Zan FM, Van Royen EA, et al. Octreotide-scintigraphy is a disease-activity parameter in graves ophthalmopathy. Clin Endocrinol. 1999;50:373–379. doi: 10.1046/j.1365-2265.1999.00681.x. [DOI] [PubMed] [Google Scholar]
- 40.Kahaly G, Rainer G, Diaz M, et al. Indium-111-pentetreotide in Graves’ disease. J Nucl Med. 1998;39:553–536. [PubMed] [Google Scholar]
- 41.Kahaly G, Diaz M, Hahn K, et al. Indium-111-Pentetreotide scintigraphy in Graves’ ophthalmopathy. J Nucl Med. 1995;36:550–554. [PubMed] [Google Scholar]
- 42.Krassas GE, Doumas A, Kaltsas TH, et al. Somatostatin receptor scintigraphy before and after treatment with somatostatine analogues in patients with thyroid eye disease. Thyroid. 1999;9:47–52. doi: 10.1089/thy.1999.9.47. [DOI] [PubMed] [Google Scholar]
- 43.Krassas GE, Doumas A, Pontikides N, et al. Somatostatin receptor scintigraphy and octreotide treatment in patients with thyroid eye disease. Clin Endocrinol. 1995;42:571–580. doi: 10.1111/j.1365-2265.1995.tb02682.x. [DOI] [PubMed] [Google Scholar]
- 44.Moncayo R, Balsissera I, Decristoforo C, et al. Evaluation of immunological mechanisms mediating thyroid-associated ophthalmopathy by radionuclide imaging using the somatostatine analogue 111In-octreotide. Thyroid. 1997;7:21–29. doi: 10.1089/thy.1997.7.21. [DOI] [PubMed] [Google Scholar]
- 45.Nocaudie M, Bailliez A, Itti E, et al. Somatostatine receptor scintigraphy to predict the clinical evolution and therapeutic response of thyroid-associated ophthalmopathy. Eur J Nucl Med. 1999;26:511–517. doi: 10.1007/s002590050419. [DOI] [PubMed] [Google Scholar]
- 46.Postema P, Krenning EP, Reubi JC, et al. 111In-DTPA-d-Phe1octreotide scintigraphy in thyroidal and orbital Graves’s disease: a parameter for disease activity? J Clin Endocrinol Metab. 1994;79:1845–1851. doi: 10.1210/jcem.79.6.7989493. [DOI] [PubMed] [Google Scholar]
- 47.Burggasser G, Hurtl I, Hauff W, et al. Receptor tracer 99mTc-P829 in patients with Graves’ disease. J Nucl Med. 2003;44:1547–1555. [PubMed] [Google Scholar]
- 48.Sun H, Xu-Feng J, Wang S, et al. 99mTcHYNIC-TOC scintigraphy in evaluation of active Grave’s ophthalmopathy (GO) Endocrinol. 2007;31:305–310. doi: 10.1007/s12020-007-0039-2. [DOI] [PubMed] [Google Scholar]
- 49.Zhao R, Wang J, Deng J, Yang W, Wang J. Efficacy of 99mTcEDDA/HYNIC-TOC SPECT/CT scintigraphy in Graves’ ophthalmopathy. Am J Nucl Med Mol Imaging. 2012;2(2):242–247. [PMC free article] [PubMed] [Google Scholar]
- 50.Lincke T, Singer J, Kluge R, et al. Relative quantification of indium-111 pentetreotide and gallium-68 DOTATOC uptake in the thyroid gland and association with thyroid pathologies. Thyroid. 2009;19:381–389. doi: 10.1089/thy.2008.0389. [DOI] [PubMed] [Google Scholar]
- 51.Lapa C, Reiter T, Kircher M, et al. Somatostatine receptor based PET/CT in patients with the suspicion of cardiac sarcoidosis: an initial comparison to cardiac MRI. Oncotarget. 2016;7(47):77807–77814. doi: 10.18632/oncotarget.12799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kwekkeboom DJ, Krenning EP, Siang Kho G, et al. Somatostatine receptor imaging in patients with sarcoidosis. Eur J Nucl Med. 1998;25:1284–1292. doi: 10.1007/s002590050297. [DOI] [PubMed] [Google Scholar]
- 53.Lebtahi R, Crestani B, Belmatoug N, et al. Somatostatin receptor scintigraphy and gallium scintigraphy in patients with sarcoidosis. J Nucl Med. 2001;42:21–26. [PubMed] [Google Scholar]
- 54.Kampuis LS, Kwekkeboom DJ, Missotten TO, et al. Somatostatine receptor scintigraphy patterns in patients with sarcoidosis. Clin Nucl Med. 2015;40:925–929. doi: 10.1097/RLU.0000000000000977. [DOI] [PubMed] [Google Scholar]
- 55.Gormsen LC, Haraldsen A, Kramer S, et al. A dual tracer 68-Ga-DOTANOC PET/CT and 18F-FDG PET/CT pilot study for detection of cardiac sarcoidosis. EJNMI Res. 2016;6:52–64. doi: 10.1186/s13550-016-0207-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nobashi T, Nakamoto Y, Kubo T, et al. The utility of PET/CT with 68Ga-DOTATOC in sarcoidosis: comparison with Ga-scintigraphy. Ann Nucl Med. 2016;30:544–552. doi: 10.1007/s12149-016-1095-6. [DOI] [PubMed] [Google Scholar]
- 57.Piotrowski WJ, Bienkiwicz M, Frieske I, et al. Somatostatine receptor scintigraphy in sarcoidosis: relation to selected clinical and laboratory markers. Polskie Archiwum Medycyny Wewnetrznej. 2012;122(3):98–105. doi: 10.20452/pamw.1179. [DOI] [PubMed] [Google Scholar]
- 58.Weinmann P, Crestani B, Tazi A, et al. 111In-pentreotide scintigraphy in patients with Langerhans’ cell histiocytosis. J Nucl Med. 2000;41:1808–1812. [PubMed] [Google Scholar]
- 59.Oztürk E, Günalp B, Ozgüven M, et al. The visualization of granulomatous disease with somatostatin receptor scintigraphy. Clin Nucl Med. 1994;19(2):129–132. doi: 10.1097/00003072-199402000-00010. [DOI] [PubMed] [Google Scholar]
- 60.Vanhagen PM, Krenning EP, Reubi JC, Kwekkeboom DJ, Bakker WH, Mulder AH, et al. Somatostatine analogue scintigraphy in granulomatous disease. Eur J Nucl Med. 1994;21(6):497–502. doi: 10.1007/BF00173035. [DOI] [PubMed] [Google Scholar]
- 61.Aparici CM, Narula J, Puig M, et al. Somatostatin receptor scintigraphy predicts impending cardiac allograft rejection before endomyocardial biopsy. Eur J Nucl Med. 2000;27(12):1754–1759. doi: 10.1007/s002590000347. [DOI] [PubMed] [Google Scholar]
- 62.Neumann I, Mirszaei S, Birck R, et al. Expression of somatostatin receptors in inflammatory lesions and diagnostic value of somatostatin receptor scintigraphy in patients with ANCA-associated small vessel vasculitis. Rheumatology. 2004;43:195–201. doi: 10.1093/rheumatology/keg479. [DOI] [PubMed] [Google Scholar]
- 63.Antunes P, Ginj M, Zhang H, et al. Are radiogallium-labelled DOTA-conjugated somatostatin analogues superior to those labelled with other radiometals? Eur J Nucl Med Mol Imaging. 2007;34:982–993. doi: 10.1007/s00259-006-0317-x. [DOI] [PubMed] [Google Scholar]
- 64.Pettinato C, Sarnelli A, Di Donna M, et al. 68Ga-DOTANOC: biodistribution and dosimetry in patients affected by neuroendocrine tumors. Eur J Nucl Med Mol Imaging. 2008;35:72–79. doi: 10.1007/s00259-007-0587-y. [DOI] [PubMed] [Google Scholar]
- 65.Borie R, Fabre A, Prost F, et al. Activation of somatostatin receptors attenuates pulmonary fibrosis. Thorax. 2008;63:251–258. doi: 10.1136/thx.2007.078006. [DOI] [PubMed] [Google Scholar]
- 66.Breeman WAP, Martin Van Hagen P, Kwekkeboom DJ, Visser TJ, Krenning EP. Somatostatin receptor scintigraphy using 111In-DTPA-octreotide. Eur J Nucl Med. 1998;25:182–186. doi: 10.1007/s002590050213. [DOI] [PubMed] [Google Scholar]
- 67.Pérez Moreiras J, Coloma Bockos JE, Prada Sánchez MC. Orbitopatía tiroidea (fisiopatología, diagnóstico y tratamiento) Arch Soc Esp Oftalmol. 2003;78:407–431. doi: 10.4321/S0365-66912003000800004. [DOI] [PubMed] [Google Scholar]
- 68.Jacobson DH, Gorman CA. Endocrine ophthalmopathy: current ideas concerning etiology, pathogenesis and treatment. Endocr Rev. 1984;5:200–220. doi: 10.1210/edrv-5-2-200. [DOI] [PubMed] [Google Scholar]
- 69.Colao A, Pivinello R, Lastoria S, et al. Clinical implications of somatostatin-receptor scintigraphy in ophthalmic Graves’ disease. Eur J Endocrinol. 2000;143:S35–S42. doi: 10.1530/eje.0.143s035. [DOI] [PubMed] [Google Scholar]
- 70.Postema PTE, Kwekkeboom DJ, Van Hagen PM, et al. Somatostatin-receptor scintigraphy in Graves’s orbitopathy. Eur J Nucl Med. 1996;23:615–617. doi: 10.1007/BF00834521. [DOI] [PubMed] [Google Scholar]
- 71.Dalm VA, van Hagen PM, van Koetsveld PM, et al. Expression of somatostatin, cortistatin, and somatostatin receptors in human monocytes, macrophages, and dendritic cells. Am J Physiol Endocrinol Metab. 2003;285:E344–E353. doi: 10.1152/ajpendo.00048.2003. [DOI] [PubMed] [Google Scholar]
- 72.Khan MU, Khan S, El-Refaie S, et al. Clinical indications for Gallium-68 positron emission tomography imaging. Eur J Surg Oncol. 2009;35:561–567. doi: 10.1016/j.ejso.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 73.Vanhagen PM, Krenning EP, Reubi JC, et al. Somatostatin analogue scintigraphy in granulomatous disease. Eur J Nucl Med. 1994;21(6):497–502. doi: 10.1007/BF00173035. [DOI] [PubMed] [Google Scholar]
- 74.Hagen EC, Daha MR, Hermans J, et al. Diagnostic value of standardized assays for anti-neutrophil cytoplasmic antibodies in idiopathic systemic vasculitis. Kidney Int. 1998;53:743–753. doi: 10.1046/j.1523-1755.1998.00807.x. [DOI] [PubMed] [Google Scholar]
- 75.Rao JK, Weinberger M, Oddone EZ, Allen NB, Landsman P, Feussner JR. The role of anti neutrophil cytoplasmic antibody (c-ANCA) testing in the diagnosis of Wegener granulomatosis. A literature review and meta-analysis. Ann Intern Med. 1995;123:925–932. doi: 10.7326/0003-4819-123-12-199512150-00005. [DOI] [PubMed] [Google Scholar]
- 76.Harper L, Savage CO. Pathogenesis of ANCA-associated systemic vasculitis. J Pathol. 2000;190:349–359. doi: 10.1002/(SICI)1096-9896(200002)190:3<349::AID-PATH524>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 77.Gephardt GN, Ahmad M, Tubbs RR. Pulmonary vasculitis (Wegener’s granulomatosis) immunohistochemical study of T and B cell markers. Am J Med. 1983;74:700–704. doi: 10.1016/0002-9343(83)91030-6. [DOI] [PubMed] [Google Scholar]
- 78.Rasmussen N, Petersen J. Cellular immune responses and pathogenesis in c-ANCA positive vasculitides. J Autoimmun. 1993;6:227–236. doi: 10.1006/jaut.1993.1020. [DOI] [PubMed] [Google Scholar]
- 79.Ferrario F, Rastaldi MP. Necrotizing-crescentic glomerulonephritis in ANCA-associated vasculitis: the role of monocytes. Nephrol Dial Transpl. 1999;14:1627–1631. doi: 10.1093/ndt/14.7.1627. [DOI] [PubMed] [Google Scholar]