Among infants <30 weeks’ gestation, in-hospital adverse outcomes among minority infants have improved, but several were still elevated by the end of the study period.
Abstract
OBJECTIVES:
To examine changes in care practices over time by race and ethnicity and whether the decrease in hospital mortality and severe morbidities has benefited infants of minority over infants of white mothers.
METHODS:
Infants 22 to 29 weeks’ gestation born between January 2006 and December 2017 at a Vermont Oxford Network center in the United States were studied. We examined mortality and morbidity rate differences and 95% confidence intervals for African American and Hispanic versus white infants by birth year. We tested temporal differences in mortality and morbidity rates between white and African American or Hispanic infants using a likelihood ratio test on nested binomial regression models.
RESULTS:
Disparities for certain care practices such as antenatal corticosteroids and for some in-hospital outcomes have narrowed over time for minority infants. Compared with white infants, African American infants had a faster decline for mortality, hypothermia, necrotizing enterocolitis, and late-onset sepsis, whereas Hispanic infants had a faster decline for mortality, respiratory distress syndrome, and pneumothorax. Other morbidities showed a constant rate difference between African American and Hispanic versus white infants over time. Despite the improvements, outcomes including hypothermia, mortality, necrotizing enterocolitis, late-onset sepsis, and severe intraventricular hemorrhage remained elevated by the end of the study period, especially among African American infants.
CONCLUSIONS:
Racial and ethnic disparities in vital care practices and certain outcomes have decreased. That the quality deficit among minority infants occurred for several care practice measures and potentially modifiable outcomes suggests a critical role for quality improvement initiatives tailored for minority-serving hospitals.
What’s Known on This Subject:
Mortality and several major in-hospital morbidities have decreased among extremely preterm infants over the past 2 decades. However, researchers have not examined whether the recent changes in hospital outcomes have benefited racial and ethnic groups similarly.
What This Study Adds:
Compared with white infants <30 weeks’ gestation, African American infants had a faster decline for mortality, hypothermia, necrotizing enterocolitis, and late-onset sepsis, whereas Hispanic infants had a faster decline for mortality, respiratory distress syndrome, and pneumothorax.
Being born extremely preterm is a major contributor to infant mortality and severe morbidities that incur a substantial cost burden to the health care system.1–3 Fortunately, rates of in-hospital mortality and several major morbidities among these preterm infants have been declining.4–6 Changes in perinatal and postnatal care practices are cited as potential causes for these decreases.4–7 However, little is known on how such changes in care practices and decreases in adverse newborn outcome rates relate to race and/or ethnicity. Such knowledge is critical to understanding whether the racial and/or ethnic disparity gap in care and outcomes of newborn infants is narrowing, especially because African American infants bear the disproportionate burden, being ∼3 times more likely to be born extremely preterm than white infants.8 Additionally, preterm-related causes contribute to more than half (55%) of the disparity in the African American–white infant mortality rate.9
In previous studies, researchers have mainly reported on trends in racial and/or ethnic disparities in infant mortality given the availability of this outcome in the US National Vital Statistics database.10–15 However, data on newborn care practices and important in-hospital morbidities are unavailable in public databases. Using data from >215 000 infants born between 22 and 29 weeks’ gestation at US centers participating in the Vermont Oxford Network (VON) between 2006 and 2017, we examined changes in newborn care practices by maternal race and/or ethnicity and whether the decrease in newborn mortality and several morbidities has benefited infants of minority over infants of white mothers.
Methods
Study Population
We conducted a retrospective study on infants born between 22 and 29 weeks’ gestation at 1 of the 789 NICUs located in the United States or Puerto Rico and participating in the VON Very Low Birth Weight Database between January 1, 2006, and December 31, 2017. We restricted our study sample to inborn, singleton infants without congenital malformations. The University of Vermont’s committee for human research approved the use of VON’s deidentified research repository for this analysis.
Study Variables
Self-reported maternal race and/or ethnicity was collected by personal interview with the mother; if unavailable, the information was obtained through birth certificate or medical record review. We combined race and ethnicity resulting in the following: non-Hispanic African American (hereafter labeled African American), non-Hispanic white (labeled white), Hispanic, Asian American, American Indian, and other race.
We examined changes over time in maternal morbidities, care practices, and newborn mortality and morbidities. Maternal morbidities included chorioamnionitis and hypertension (chronic or pregnancy induced). We divided care practices into obstetric practices (antenatal corticosteroids [ANSs], cesarean delivery), delivery room (DR) practices (tracheal intubation, epinephrine, cardiac compressions, face mask ventilation, surfactant), and NICU practices (steroids for chronic lung disease [CLD], surfactant therapy at any time, which also includes surfactants if received in the DR, conventional ventilation, ventilation after continuous positive airway pressure [CPAP], high-frequency ventilation, nasal ventilation, CPAP before ventilation, nasal CPAP, high-flow nasal cannula, inhaled nitric oxide, postnatal life support [surfactant therapy at any time, endotracheal tube ventilation, ventilator support at any time, epinephrine, or cardiac compressions]). All the above variables were available for the entire period (2006–2017) except for chorioamnionitis, hypertension, and inhaled nitric oxide, which were added in 2008.
Mortality was defined as death before hospital discharge. Hypothermia was defined as the infant’s body temperature <36.5°C measured within the first hour of NICU admission.16 Respiratory distress syndrome (RDS) was defined as room air Pao2 <50 mm Hg, room air with central cyanosis, supplemental oxygen to maintain Pao2 >50 mm Hg, or supplemental oxygen to maintain a pulse oximeter saturation >85% and a chest radiograph consistent with RDS within the first 24 hours of life.16 Necrotizing enterocolitis (NEC) was diagnosed at surgery or postmortem or required ≥1 clinical sign (eg, bilious gastric aspirate, abdominal distension, occult blood in stool) and ≥1 radiographic finding (eg, pneumatosis intestinalis, hepatobiliary gas, or pneumoperitoneum).16 Focal intestinal perforation, separate from NEC, was defined as a single focal perforation with the remainder of the bowel appearing normal, diagnosed at surgery time or postmortem examination.16 NEC and focal intestinal perforation were combined into 1 outcome labeled NEC. Early-onset sepsis (EOS; on or before day 3 of life) was defined as bacterial pathogen recovered from blood or cerebrospinal fluid.16 Late-onset sepsis (LOS; after day 3 of life) was defined as bacterial pathogen or coagulase-negative Staphylococcus recovered from blood or cerebrospinal fluid or fungus recovered from blood culture.16 Coagulase-negative Staphylococcus infection also required ≥1 sign of generalized infection and treatment with ≥5 days of intravenous antibiotics.16 Severe intraventricular hemorrhage (sIVH) was defined as grades 3 or 4 using Papile’s classification within 28 days of birth.17 Severe retinopathy of prematurity (sROP) was defined as stages 3 to 5 based on a retinal examination before hospital discharge.18 CLD was defined as any supplemental oxygen use at 36 weeks’ postmenstrual age or on oxygen at discharge at 34 to 35 weeks if transferred or discharged <36 weeks’ gestation.16 We also examined survival to discharge without a major neonatal morbidity defined as ≥1 of early or late bacterial or fungal infection, NEC/focal intestinal perforation, CLD, sIVH, cystic periventricular leukomalacia (multiple small periventricular cysts on a cranial ultrasound, computed tomography, or MRI), or sROP. Reporting hospitals tracked mortality before hospital discharge and after transfer until ultimate disposition.
Statistical Analysis
We computed summary statistics of maternal and neonatal characteristics and care practices by maternal race and/or ethnicity. We subsequently calculated the following:
incidence rates of maternal morbidities, obstetric practices, DR practices, NICU practices, and other practices by race and/or ethnicity and birth year along with 95% confidence intervals (CIs);
incidence rates of infant mortality and morbidity by race and/or ethnicity and birth year along with 95% CIs; and
differences between rates for African American and Hispanic versus white infants by birth year, along with 95% CIs.
We tested differences in trends over time between white and African American or Hispanic infants for mortality and morbidity rates using likelihood ratio tests (LRTs) on nested binomial regression models. The null model included main effects for race and/or ethnicity and a third-degree polynomial on birth year. The alternative model included the same main effects as well as an interaction between them. No adjustments were made for other variables related to medical care to prevent masking of temporal effects.
Similar analyses were conducted separately to compare white and Asian American infants, provided as Supplemental Information. Statistical significance was set at 5%. Analyses were performed by using R19 (version 3.2.2.) and SAS software (version 9.4; SAS Institute, Inc, Cary, NC).
Sensitivity Analysis
We assessed the sensitivity of the results when restricting the study sample to centers participating in VON throughout the entire 12-year period. The restricted sample had 414 centers and 75.5% (n = 165 432) of the infants.
Results
Study Sample
Of 226 283 singleton infants born at VON centers, we excluded infants with unknown sex (n = 37), missing race and/or ethnicity (n = 935), and missing (n = 126) or implausible birth weight (n = 912). Implausible birth weights were defined as values below or above gestational age–specific cutoffs, determined by using a method based on data sparsity.20,21 Overall, 1986 infants were excluded, resulting in 224 297 infants. Given the limited sample size, we further excluded infants of American Indian (n = 1628) or other (n = 3535) race. This resulted in 219 134 infants for our main analyses; 40.6% white, 34.8% African American, 20.4% Hispanic, and 4.2% Asian American. Table 1 shows maternal and newborn characteristics and care practices by race and/or ethnicity. African American mothers had the highest rates of hypertension and chorioamnionitis. African American and Hispanic mothers had the lowest rates of ANSs.
TABLE 1.
Maternal and Newborn Characteristics and Care Practices by Race and Ethnicity
| Characteristics and Care Practices | White, N = 88 884 | African American, N = 76 256 | Hispanic, N = 44 774 | Asian American, N = 9220 |
|---|---|---|---|---|
| Maternal | ||||
| Prenatal care | 85 811 of 88 732 (96.7) | 71 358 of 75 968 (93.9) | 42 206 of 44 586 (94.7) | 8942 of 9203 (97.2) |
| Hypertensiona | 21 671 of 74 295 (29.2) | 20 190 of 64 418 (31.3) | 9290 of 37 811 (24.6) | 1919 of 8004 (24.0) |
| Chorioamnionitis | 13 144 of 74 211 (17.7) | 13 472 of 64 269 (21.0) | 6764 of 37 763 (17.9) | 1302 of 7988 (16.3) |
| ANSsb | 75 493 of 88 717 (85.1) | 61 668 of 76 076 (81.1) | 36 055 of 44 653 (80.7) | 7634 of 9201 (83.0) |
| Cesarean delivery | 58 415 of 88 873 (65.7) | 47 148 of 76 249 (61.8) | 27 923 of 44 772 (62.4) | 5563 of 9220 (60.3) |
| Newborn | ||||
| Male | 47 645 of 88 884 (53.6) | 38 946 of 76 256 (51.1) | 24 088 of 44 774 (53.8) | 5065 of 9220 (54.9) |
| Birth wt, g, mean (SD) | 947 (301) | 876 (282) | 934 (299) | 934 (296) |
| Gestational age, wk | ||||
| 22 | 2440 (2.8) | 3102 (4.1) | 1762 (3.9) | 327 (3.6) |
| 23 | 5376 (6.0) | 6401 (8.4) | 3497 (7.8) | 602 (6.5) |
| 24 | 8920 (10.0) | 9343 (12.2) | 5066 (11.3) | 944 (10.2) |
| 25 | 10 441 (11.8) | 9980 (13.1) | 5397 (12.1) | 1074 (11.6) |
| 26 | 12 030 (13.5) | 10 509 (13.8) | 6119 (13.7) | 1228 (13.3) |
| 27 | 14 113 (15.9) | 11 594 (15.2) | 6815 (15.2) | 1453 (15.8) |
| 28 | 16 572 (18.6) | 12 441 (16.3) | 7682 (17.2) | 1670 (18.1) |
| 29 | 18 992 (21.4) | 12 886 (16.9) | 8436 (18.8) | 1922 (20.9) |
| Apgar score at 5 min ≤3 | 9458 of 87 940 (10.8) | 9956 of 75 111 (13.3) | 5352 of 44 111 (12.1) | 1056 of 9122 (11.6) |
| Postnatal life supportc | 85 294 of 88 878 (96.0) | 72 559 of 76 244 (95.2) | 42 346 of 44 772 (94.6) | 8667 of 9220 (94.0) |
| DR intubation | 56 353 of 88 858 (63.4) | 51 033 of 76 213 (67.0) | 27 500 of 44 758 (61.4) | 5032 of 9215 (54.6) |
| Surfactant therapy anytime | 68 940 of 88 863 (77.6) | 57 004 of 76 229 (74.8) | 32 472 of 44 761 (72.6) | 6181 of 9217 (67.1) |
| Conventional ventilation | 63 575 of 84 953 (74.8) | 55 410 of 72 296 (76.6) | 30 785 of 42 175 (73.0) | 6014 of 8660 (69.5) |
| Postnatal steroids | 11 735 of 84 824 (13.8) | 10 243 of 72 197 (14.2) | 4522 of 42 087 (10.7) | 880 of 8642 (10.2) |
| Admission temperatured, °C | ||||
| 36.5–37.5 | 42 880 of 82 673 (51.9) | 32 820 of 70 045 (46.9) | 21 698 of 41 057 (52.9) | 4593 of 8457 (54.3) |
| <36.5 | 33 715 of 82 673 (40.8) | 33 246 of 70 045 (47.5) | 16 478 of 41 057 (40.1) | 3271 of 8457 (38.7) |
| >37.5 | 6078 of 82 673 (7.4) | 3979 of 70 045 (5.7) | 2881 of 41 057 (7.0) | 593 of 8457 (7.0) |
| Enteral feeding at discharge | ||||
| None | 13 386 of 84 826 (15.8) | 12 718 of 72 120 (17.6) | 7421 of 42 115 (17.6) | 1336 of 8641 (15.5) |
| Any human milk | 36 468 of 84 826 (43.0) | 18 833 of 72 120 (26.1) | 17 572 of 42 115 (41.7) | 4906 of 8641 (56.8) |
| Formula only | 34 972 of 84 826 (41.2) | 40 569 of 72 120 (56.3) | 17 122 of 42 115 (40.7) | 2399 of 8641 (27.8) |
| Total length of stay median (IQR), d | 70 (49–96) | 69 (46–98) | 70 (48–96) | 71 (49–98) |
Numbers are n (%) unless otherwise indicated. Hypertension and chorioamnionitis variables were added in 2008; postnatal steroids and admission temperature variables were only recorded for infants admitted to the NICU. Data missing for prenatal care 0.29%, hypertension 0.24%, chorioamnionitis 0.40%, ANSs 0.22%, cesarean 0.01%, Apgar at 5-min 1.30%, postnatal life support 0.01%, DR intubation 0.04%, surfactant therapy anytime 0.03%, postnatal steroids 0.17%, admission temperature 2.8%, enteral feeding at discharge 5.22%, total length of stay 0.68%. IQR, interquartile range.
Maternal hypertension defined as chronic or pregnancy induced, with or without edema and proteinuria, or as maternal blood pressure above 140 systolic or 90 diastolic before or during the present pregnancy.
Exposure to ANSs defined as steroids administered IM or IV to the mother during pregnancy at any time before delivery.
Postnatal life support includes any of the following: surfactant therapy at any time, endotracheal tube ventilation, ventilator support at any time (including nasal CPAP, nasal ventilation, face mask ventilation, or mechanical ventilation), epinephrine, or cardiac compressions.
Infant’s body temperature (measured by taking a rectal, esophageal, tympanic, or axillary temperature) was recorded within the first h after admission to the NICU.
Maternal Morbidities
Chorioamnionitis rate slightly increased over time with African American mothers having the highest rate. The rate of maternal hypertension showed an increasing trend over time for all groups but was highest for African American mothers and lowest for Hispanic mothers (Supplemental Fig 4).
Obstetric Practices
Use of ANSs increased over time for all groups, and although the increase was more prominent for African American and Hispanic than white mothers (% change 2006–2017 white: 13.0%, African American: 18.7%, Hispanic: 21.2%), the rate remained highest for white mothers. Cesarean delivery rate increased over time for all groups but remained highest for white mothers (Supplemental Fig 5).
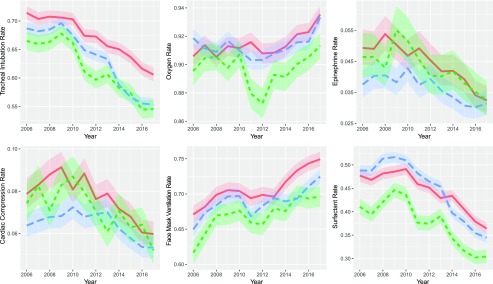
DR Practices
DR tracheal intubation, epinephrine, cardiac compression, and surfactant therapy rates decreased, whereas face mask ventilation rate increased over time for all groups (Fig 1). Tracheal intubation rate was higher for African American than Hispanic and white infants, whereas DR surfactant rate was lowest among Hispanic infants. Supplemental oxygen use remained relatively constant over time with similar rates for all groups.
FIGURE 1.
Rates of DR practices among white, African American, and Hispanic infants by birth year. The blue line represents white infants, the red line represents African American infants, and the green line represents Hispanic infants; borders represent 95% CIs.
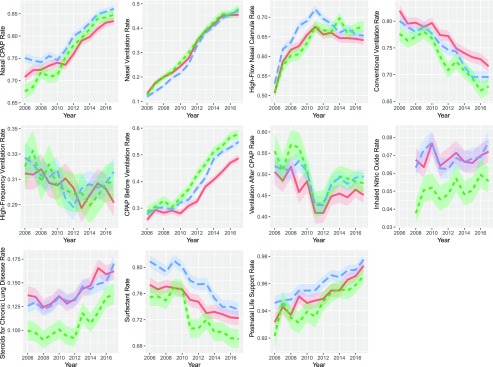
NICU Practices
Nasal CPAP use revealed positive trends over time with slightly lower rates among African American infants (Fig 2). Nasal ventilation and high-flow nasal cannula use also increased over time with relatively similar rates for all groups. Conventional ventilation decreased over time for all groups of infants, but rates were higher among African American (2017 rate: 71.6%) than white (69.6%) and Hispanic (67.8%) infants. High-frequency ventilation rate was relatively constant over time with similar rates among all groups. CPAP before assisted ventilation increased over time but revealed lower rates for African American (2017 rate: 48.7%) than Hispanic (57.6%) and white (54.9%) infants. Ventilation after CPAP revealed a negative trend followed by a positive trend with slightly lower rates among African American infants. Inhaled nitric oxide use was relatively constant over time with lower rates among Hispanic infants. Although the rate of steroids for CLD increased over time for all infants, it remained lowest for Hispanic (2017 rate: 13.8%) infants (white: 17.0%, African American: 16.2%). Surfactants decreased for all infants, with the lowest rates observed for Hispanic (2017 rate: 69.1%) infants (white: 73.5%, African American: 72.2%). Postnatal life support rates increased for all groups.
FIGURE 2.
Rates of NICU practices among white, African American, and Hispanic infants by birth year. The blue line represents white infants, the red line represents African American infants, and the green line represents Hispanic infants; borders represent 95% CIs.
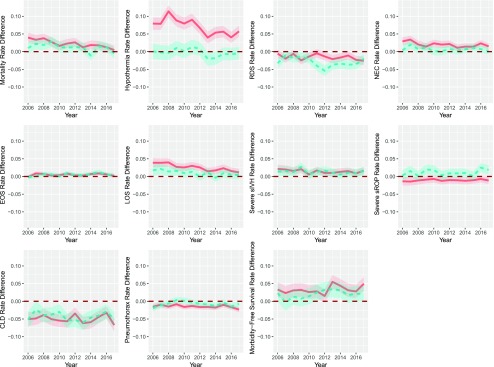
Mortality and Morbidities
Supplemental Table 2 shows the overall rates of outcomes by race and/or ethnicity. Mortality and morbidity rates across the years are shown in Supplemental Fig 6, separately for each group. Rate differences between African American and Hispanic versus white infants during the study period are shown in Fig 3.
FIGURE 3.
Rate differences in mortality and morbidity outcomes among African American and Hispanic versus white infants by birth year. The red line represents the rate difference among African American versus white infants, and the blue line represents the rate difference among Hispanic versus white infants; borders represent 95% CIs.
For African American versus white infants, RDS, EOS, sIVH, sROP, CLD, pneumothorax, and morbidity-free survival revealed a constant rate difference over time. EOS rates revealed occasionally slightly higher rates for African American infants, whereas sIVH was higher among African American than white infants for most of the years. RDS and sROP were lower among African American infants for some but not all years. Hypothermia was higher, whereas CLD and pneumothorax were lower among African American infants throughout the study period. Morbidity-free survival was higher among African American infants for all years except one. The rate difference for mortality, hypothermia, NEC, and LOS remained higher for African American infants throughout the study period. However, the rates for these outcomes decreased faster over time for African American than white infants with a significant year-race interaction (LRT P < .0001, mortality; P < .0001, hypothermia; P = .028, NEC; P < .0001, LOS).
For Hispanic versus white infants, hypothermia, NEC, EOS, LOS, sIVH, sROP, CLD, and morbidity-free survival revealed a constant rate difference over time. NEC, EOS, and morbidity-free survival revealed occasionally slightly higher rates for Hispanic than white infants. Mortality, LOS, sIVH, and sROP revealed higher rates among Hispanic infants for some but not all years. RDS and pneumothorax were lower among Hispanic infants for some but not all years. CLD rate was lower among Hispanic infants for the whole study period. The rates for mortality, RDS, and pneumothorax decreased faster over time for Hispanic than white infants, with a significant year-race interaction (LRT P = .032, mortality; P < .0001, RDS; P = .0016, pneumothorax).
Similar results were obtained after restricting the analysis to VON centers that participated for all 12 years, although the results were strengthened for the year-race interaction among African American infants for NEC (P = .0049) and among Hispanic infants for mortality (P = .020) (Supplemental Fig 7).
Supplementary Analyses
For Asian American infants, maternal morbidities, obstetric, DR, and NICU, are reported in Supplemental Figs 8–11, respectively. Briefly, trends for Asian American infants were as those reported for white infants. Maternal hypertension and cesarean delivery were higher for white mothers. Asian American infants had lower rates of DR tracheal intubation and surfactants. For NICU practices, Asian American infants had lower rates of conventional ventilation, steroids for CLD, and surfactants and higher rates of CPAP use before ventilation.
Mortality and morbidity rates for Asian American and white infants during the study period are shown in Supplemental Fig 12. Rate differences between Asian American versus white infants are shown in Supplemental Fig 13. Few to no significant rate differences across the study period among Asian American versus white infants were observed for mortality, hypothermia, NEC, EOS, LOS, and sIVH. For some but not all years, Asian infants had higher rates for sROP and morbidity-free survival and lower rates for RDS, CLD, and pneumothorax. Only RDS revealed a significant race-year interaction in both the main and the sensitivity analysis restricted to VON centers participating for the whole study period (P = .013, main analysis; P = .028, sensitivity analysis).
Discussion
In a study of >215 000 infants born at 22 to 29 weeks’ gestation between 2006 and 2017 in the United States, we report that the disparity for certain care practices and outcomes have narrowed over time for African American and Hispanic infants. Compared with white infants, African American infants had a faster decline for mortality, hypothermia, NEC, and LOS, whereas Hispanic infants had a faster decline for mortality, RDS, and pneumothorax. However, by 2017, mortality and several morbidities remained elevated, especially for African American infants.
Disparate patterns in the site of delivery by race and/or ethnicity might contribute to the observed disparities in newborn care practices and outcomes. Several studies in the adult literature report that minority racial and/or ethnic patients disproportionately receive care at the lowest quality hospitals and care providers.22–26 Recent studies also reveal that this is applicable to the perinatal health field. In New York City, the quality of the birth hospital explained 40% of the African American–white disparity and 30% of the Hispanic-white disparity in hospital adverse outcomes of very preterm births, but there was no evidence of within-hospital disparities.27 In California NICUs, there was evidence of racial and/or ethnic disparities in quality of care between and within NICUs.28 A national study from VON showed that African American, Hispanic, and Asian American preterm infants were segregated across NICUs, with large differences in NICU quality between geographic regions.29 Compared with white infants, Asian American and Hispanic infants were concentrated at higher quality NICUs, whereas African American infants received care at lower quality NICUs.29 Accounting for region of residence explained the association for Hispanic but not for Asian American or African American infants.29
Despite the racial and/or ethnic disparities in which minority (especially African American infants) might receive care, our study suggests a positive outlook. The narrowing of the gap in the rate of evidence-based care practices such as ANSs and the decrease in rates of mortality and several morbidities such as hypothermia and LOS among minority infants suggests that care among these infants has been improving. In a recent study, Horbar et al6 examined the change in the performance of 756 VON NICUs admitting very low birth weight infants between 2005 and 2014 and reported that rates of in-hospital death and severe morbidities declined. By 2014, >98% of all NICUs achieved the risk-adjusted mortality rate of the best 10% of units in 2005, and 75% of all NICUs achieved performance rates equivalent to the best quartile of the 2005 benchmark for all severe morbidities (NEC, LOS, sIVH, sROP) except CLD.6 The application of evidence-based care practices through quality improvement (QI) methods has been cited as a potential explanation for this progress.6 Indeed, QI initiatives have been successful in improving care and reducing adverse newborn outcomes.30–36 LOS has been a major focus of several of these initiatives, with evidence suggesting that infection rates in NICUs can be reduced.37–41 The VON has been a pioneer in QI collaboratives with >550 NICUs participating in such collaboratives since 1995.6 Given that minority-serving NICUs have lower quality of care than non–minority-serving NICUs,27,29,42,43 one would hypothesize on the basis of the above study6 and our findings that the improvement in performance has also occurred among minority-serving NICUs.
Although we depict in our study several encouraging findings, further progress is warranted. Human milk at discharge based on VON data remains suboptimal among African American infants,44 potentially contributing to disparities in NEC and LOS rates.45–49 Collaborative QI initiatives in California and 4 Southern US states have been successful in demonstrating a significant and sustained increase in breast milk feeding rates, which can decrease racial inequities.49,50 Similarly, targeted interventions can reduce hypothermia rates,51,52 which were highest among African American infants by the end of the study period. Further improvements in ANS rates among African American and Hispanic infants can also contribute to decreasing sIVH.53
We are uncertain how racial and/or ethnic differences in response to life-saving treatments54 and usage of more invasive approaches to respiratory support might have contributed to outcomes such as sIVH and CLD. Our findings suggest that African American infants have higher rates of DR intubation and lower rates of CPAP use before ventilation than white infants. Previous studies have revealed that avoidance of DR intubation when possible and decreasing the number of intubation attempts can reduce sIVH.53,55 For CLD, potentially better practices include avoiding intubation by using early CPAP, by using surfactants selectively, and minimizing duration of mechanical ventilation.56 However, QI initiatives have not been as successful in reducing CLD rates contrary to the declines observed for other morbidities.4,6 We show in our study, similar to previous studies, that African American compared with white infants have lower CLD and pneumothorax rates.28,57 However, despite their lower CLD rates, African American infants develop worse longer-term respiratory outcomes than white infants.58
Strengths of our study include a large sample size with data on care practices and outcomes of >215 000 infants over a 12-year period. These data represent 88% of all US births at 22 to 29 weeks’ gestation. Limitations of our study include lack of data on causes of death to probe whether deaths related to RDS, NEC, and LOS also decreased over time. We also realize that race and/or ethnicity are complex social constructs,59 with substantial heterogeneity in health outcomes within Hispanic and Asian American subgroups.12,15,60
Conclusions
Between 2006 and 2017, the disparity gap for care practices and certain outcomes narrowed between minority and white infants. However, by 2017, disparities in care practices and several outcomes remained, especially for African American infants. That the quality deficit among minority infants occurred for several care practice measures and potentially modifiable6 outcomes suggests a critical role for QI initiatives tailored for minority-serving hospitals. In the absence of effective preterm birth prevention strategies, it is imperative that researchers of future studies continue to assess care and outcome trends to ensure that infants of all racial and ethnic backgrounds benefit equally from medical developments.
Acknowledgments
We thank our colleagues who submit data to the Vermont Oxford Network on behalf of infants and their families. Participating centers are listed in Supplemental Table 3.
Glossary
- ANS
antenatal corticosteroid
- CI
confidence interval
- CLD
chronic lung disease
- CPAP
continuous positive airway pressure
- DR
delivery room
- EOS
early-onset sepsis
- LOS
late-onset sepsis
- LRT
likelihood ratio test
- NEC
necrotizing enterocolitis
- QI
quality improvement
- RDS
respiratory distress syndrome
- sIVH
severe intraventricular hemorrhage
- sROP
severe retinopathy of prematurity
- VON
Vermont Oxford Network
Footnotes
Dr Boghossian participated in the conception and design of the study, including the analysis plan and in the interpretation of the data, obtained funding, and wrote all drafts of the manuscript; Dr Geraci participated in designing the analysis plan, was responsible for the data management and data analysis, participated in the interpretation of the data, and contributed to writing sections of the manuscript; Drs Lorch, Phibbs, and Edwards participated in the conception of the study and the interpretation of the data; Dr Horbar participated in the conception of the study, is the Chief Executive and Scientific Officer of the Vermont Oxford Network, from which the data were drawn, and participated in the interpretation of the data; and all authors helped to revise the manuscript critically for important intellectual content, approved the final manuscript as submitted, and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: Dr Horbar is an employee of Vermont Oxford Network and Dr Edwards receives salary support from Vermont Oxford Network; the other authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under award R03HD097305. Drs Edwards and Horbar receive support from the Eunice Kennedy Shriver National Institute of Child Health & Human Development, National Institutes of Health, award R01HD083368. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2019-2002.
References
- 1.Korvenranta E, Lehtonen L, Rautava L, et al. ; PERFECT Preterm Infant Study Group . Impact of very preterm birth on health care costs at five years of age. Pediatrics. 2010;125(5). Available at: www.pediatrics.org/cgi/content/full/125/5/e1109 [DOI] [PubMed] [Google Scholar]
- 2.Phibbs CS, Schmitt SK, Cooper M, et al. . Birth hospitalization costs and days of care for mothers and neonates in California, 2009-2011. J Pediatr. 2019;204:118–125.e14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel RM. Short- and long-term outcomes for extremely preterm infants. Am J Perinatol. 2016;33(3):318–328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stoll BJ, Hansen NI, Bell EF, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network . Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA. 2015;314(10):1039–1051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Horbar JD, Carpenter JH, Badger GJ, et al. . Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Pediatrics. 2012;129(6):1019–1026 [DOI] [PubMed] [Google Scholar]
- 6.Horbar JD, Edwards EM, Greenberg LT, et al. . Variation in performance of neonatal intensive care units in the United States. JAMA Pediatr. 2017;171(3):e164396. [DOI] [PubMed] [Google Scholar]
- 7.Boghossian NS, Geraci M, Edwards EM, Horbar JD. Sex differences in mortality and morbidity of infants born at less than 30 weeks’ gestation. Pediatrics. 2018;142(6):e20182352. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention Natality information: live births. Available at: http://wonder.cdc.gov/natality.html. Accessed October 25, 2017
- 9.MacDorman MF, Mathews TJ. Understanding racial and ethnic disparities in U.S. infant mortality rates. NCHS Data Brief. 2011;(74):1–8 [PubMed] [Google Scholar]
- 10.Alexander GR, Wingate MS, Bader D, Kogan MD. The increasing racial disparity in infant mortality rates: composition and contributors to recent US trends. Am J Obstet Gynecol. 2008;198(1):51.e1–51.e9 [DOI] [PubMed] [Google Scholar]
- 11.Mathews TJ, Driscoll AK. Trends in infant mortality in the United States, 2005-2014. NCHS Data Brief. 2017;(279):1–8 [PubMed] [Google Scholar]
- 12.Matthews TJ, MacDorman MF, Thoma ME. Infant mortality statistics from the 2013 period linked birth/infant death data set. Natl Vital Stat Rep. 2015;64(9):1–30 [PubMed] [Google Scholar]
- 13.Reddy UM, Bettegowda VR, Dias T, Yamada-Kushnir T, Ko CW, Willinger M. Term pregnancy: a period of heterogeneous risk for infant mortality. Obstet Gynecol. 2011;117(6):1279–1287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Riddell CA, Harper S, Kaufman JS. Trends in differences in US mortality rates between black and white infants. JAMA Pediatr. 2017;171(9):911–913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rossen LM, Schoendorf KC. Trends in racial and ethnic disparities in infant mortality rates in the United States, 1989-2006. Am J Public Health. 2014;104(8):1549–1556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vermont Oxford Network Manuals and forms. Available at: https://public.vtoxford.org/manualsforms/. Accessed May 17, 2017
- 17.Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92(4):529–534 [DOI] [PubMed] [Google Scholar]
- 18.International Committee for the Classification of Retinopathy of Prematurity The international classification of retinopathy of prematurity revisited. Arch Ophthalmol. 2005;123(7):991–999 [DOI] [PubMed] [Google Scholar]
- 19.R Core Team A Language and Environment for Statistical Computing. Vienne, Austria: R Foundation for Statistical Computing; Available at: https://www.R-project.org/. Accessed July 12, 2019 [Google Scholar]
- 20.Boghossian NS, Geraci M, Edwards EM, Morrow KA, Horbar JD. Anthropometric charts for infants born between 22 and 29 weeks’ gestation. Pediatrics. 2016;138(6):e20161641. [DOI] [PubMed] [Google Scholar]
- 21.Rich C, Geraci M, Griffiths L, Sera F, Dezateux C, Cortina-Borja M. Quality control methods in accelerometer data processing: identifying extreme counts. PLoS One. 2014;9(1):e85134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351(6):575–584 [DOI] [PubMed] [Google Scholar]
- 23.Hasnain-Wynia R, Baker DW, Nerenz D, et al. . Disparities in health care are driven by where minority patients seek care: examination of the hospital quality alliance measures. Arch Intern Med. 2007;167(12):1233–1239 [DOI] [PubMed] [Google Scholar]
- 24.Jha AK, Orav EJ, Li Z, Epstein AM. Concentration and quality of hospitals that care for elderly black patients. Arch Intern Med. 2007;167(11):1177–1182 [DOI] [PubMed] [Google Scholar]
- 25.Liu JH, Zingmond DS, McGory ML, et al. . Disparities in the utilization of high-volume hospitals for complex surgery. JAMA. 2006;296(16):1973–1980 [DOI] [PubMed] [Google Scholar]
- 26.Skinner J, Chandra A, Staiger D, Lee J, McClellan M. Mortality after acute myocardial infarction in hospitals that disproportionately treat black patients. Circulation. 2005;112(17):2634–2641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Howell EA, Janevic T, Hebert PL, Egorova NN, Balbierz A, Zeitlin J. Differences in morbidity and mortality rates in black, white, and Hispanic very preterm infants among New York city hospitals. JAMA Pediatr. 2018;172(3):269–277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Profit J, Gould JB, Bennett M, et al. . Racial/ethnic disparity in NICU quality of care delivery. Pediatrics. 2017;140(3):e20170918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Horbar JD, Edwards EM, Greenberg LT, et al. . Racial segregation and inequality in the neonatal intensive care unit for very low-birth weight and very preterm infants [published online ahead of print March 25, 2019]. JAMA Pediatr. 10.1001/jamapediatrics.2019.0241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ellsbury DL, Clark RH, Ursprung R, Handler DL, Dodd ED, Spitzer AR. A multifaceted approach to improving outcomes in the NICU: the pediatrix 100 000 babies campaign. Pediatrics. 2016;137(4):e20150389. [DOI] [PubMed] [Google Scholar]
- 31.Lee HC, Lyndon A, Blumenfeld YJ, Dudley RA, Gould JB. Antenatal steroid administration for premature neonates in California. Obstet Gynecol. 2011;117(3):603–609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee HC, Powers RJ, Bennett MV, et al. . Implementation methods for delivery room management: a quality improvement comparison study. Pediatrics. 2014;134(5). Available at: www.pediatrics.org/cgi/content/full/134/5/e1378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee SK, Aziz K, Singhal N, et al. . Improving the quality of care for infants: a cluster randomized controlled trial. CMAJ. 2009;181(8):469–476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pai VV, Lee HC, Profit J. Improving Uptake of Key Perinatal Interventions Using Statewide Quality Collaboratives . Improving uptake of key perinatal interventions using statewide quality collaboratives. Clin Perinatol. 2018;45(2):165–180 [DOI] [PubMed] [Google Scholar]
- 35.Shah V, Warre R, Lee SK. Quality improvement initiatives in neonatal intensive care unit networks: achievements and challenges. Acad Pediatr. 2013;13(suppl 6):S75–S83 [DOI] [PubMed] [Google Scholar]
- 36.Ellsbury DL, Clark RH. Does quality improvement work in neonatology improve clinical outcomes? Curr Opin Pediatr. 2017;29(2):129–134 [DOI] [PubMed] [Google Scholar]
- 37.Fisher D, Cochran KM, Provost LP, et al. . Reducing central line-associated bloodstream infections in North Carolina NICUs. Pediatrics. 2013;132(6). Available at: www.pediatrics.org/cgi/content/full/132/6/e1664 [DOI] [PubMed] [Google Scholar]
- 38.Wirtschafter DD, Powers RJ, Pettit JS, et al. . Nosocomial infection reduction in VLBW infants with a statewide quality-improvement model. Pediatrics. 2011;127(3):419–426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schulman J, Stricof R, Stevens TP, et al. ; New York State Regional Perinatal Care Centers . Statewide NICU central-line-associated bloodstream infection rates decline after bundles and checklists. Pediatrics. 2011;127(3):436–444 [DOI] [PubMed] [Google Scholar]
- 40.Kaplan HC, Lannon C, Walsh MC, Donovan EF; Ohio Perinatal Quality Collaborative . Ohio statewide quality-improvement collaborative to reduce late-onset sepsis in preterm infants. Pediatrics. 2011;127(3):427–435 [DOI] [PubMed] [Google Scholar]
- 41.Payne NR, Finkelstein MJ, Liu M, Kaempf JW, Sharek PJ, Olsen S. NICU practices and outcomes associated with 9 years of quality improvement collaboratives. Pediatrics. 2010;125(3):437–446 [DOI] [PubMed] [Google Scholar]
- 42.Lake ET, Staiger D, Horbar J, Kenny MJ, Patrick T, Rogowski JA. Disparities in perinatal quality outcomes for very low birth weight infants in neonatal intensive care. Health Serv Res. 2015;50(2):374–397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Morales LS, Staiger D, Horbar JD, et al. . Mortality among very low-birthweight infants in hospitals serving minority populations. Am J Public Health. 2005;95(12):2206–2212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Parker MG, Greenberg LT, Edwards EM, Ehret DEY, Belfort MB, Horbar JD. Human milk at discharge among VLBW infants: national trends and variation by maternal race/ethnicity and region. In: Presented at the Pediatric Academic Societies; May 5-8, 2018; Toronto, Canada [Google Scholar]
- 45.Gephart SM, Spitzer AR, Effken JA, Dodd E, Halpern M, McGrath JM. Discrimination of GutCheck(NEC): a clinical risk index for necrotizing enterocolitis. J Perinatol. 2014;34(6):468–475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Colaizy TT, Bartick MC, Jegier BJ, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network . Impact of optimized breastfeeding on the costs of necrotizing enterocolitis in extremely low birthweight infants. J Pediatr. 2016;175:100–105.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Quigley M, Embleton ND, McGuire W. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst Rev. 2018;6:CD002971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schanler RJ, Lau C, Hurst NM, Smith EO. Randomized trial of donor human milk versus preterm formula as substitutes for mothers’ own milk in the feeding of extremely premature infants. Pediatrics. 2005;116(2):400–406 [DOI] [PubMed] [Google Scholar]
- 49.Lee HC, Kurtin PS, Wight NE, et al. . A quality improvement project to increase breast milk use in very low birth weight infants. Pediatrics. 2012;130(6). Available at: www.pediatrics.org/cgi/content/full/130/6/e1679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Merewood A, Bugg K, Burnham L, et al. . Addressing racial inequities in breastfeeding in the southern United States. Pediatrics. 2019;143(2):e20181897. [DOI] [PubMed] [Google Scholar]
- 51.Andrews C, Whatley C, Smith M, Brayton EC, Simone S, Holmes AV. Quality-improvement effort to reduce hypothermia among high-risk infants on a mother-infant unit. Pediatrics. 2018;141(3):e20171214. [DOI] [PubMed] [Google Scholar]
- 52.Russo A, McCready M, Torres L, et al. . Reducing hypothermia in preterm infants following delivery. Pediatrics. 2014;133(4). Available at: www.pediatrics.org/cgi/content/full/133/4/e1055 [DOI] [PubMed] [Google Scholar]
- 53.Handley SC, Passarella M, Lee HC, Lorch SA. Incidence trends and risk factor variation in severe intraventricular hemorrhage across a population based cohort. J Pediatr. 2018;200:24–29.e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hamvas A, Wise PH, Yang RK, et al. . The influence of the wider use of surfactant therapy on neonatal mortality among blacks and whites. N Engl J Med. 1996;334(25):1635–1640 [DOI] [PubMed] [Google Scholar]
- 55.Sauer CW, Kong JY, Vaucher YE, et al. . Intubation attempts increase the risk for severe intraventricular hemorrhage in preterm infants-a retrospective cohort study. J Pediatr. 2016;177:108–113 [DOI] [PubMed] [Google Scholar]
- 56.Picarillo AP, Carlo W. Using quality improvement tools to reduce chronic lung disease. Clin Perinatol. 2017;44(3):701–712 [DOI] [PubMed] [Google Scholar]
- 57.Ryan RM, Feng R, Bazacliu C, et al. ; Prematurity and Respiratory Outcome Program (PROP) Investigators . Black race is associated with a lower risk of bronchopulmonary dysplasia. J Pediatr. 2019;207:130–135.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Keller RL, Feng R, DeMauro SB, et al. ; Prematurity and Respiratory Outcomes Program . Bronchopulmonary dysplasia and perinatal characteristics predict 1-year respiratory outcomes in newborns born at extremely low gestational age: a prospective cohort study. J Pediatr. 2017;187:89–97.e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kaufman JS, Cooper RS. Commentary: considerations for use of racial/ethnic classification in etiologic research. Am J Epidemiol. 2001;154(4):291–298 [DOI] [PubMed] [Google Scholar]
- 60.Baker LC, Afendulis CC, Chandra A, McConville S, Phibbs CS, Fuentes-Afflick E. Differences in neonatal mortality among whites and Asian American subgroups: evidence from California. Arch Pediatr Adolesc Med. 2007;161(1):69–76 [DOI] [PMC free article] [PubMed] [Google Scholar]