Innovative strategies are needed to reduce the hypertension epidemic among African Americans. Reach Out was a faith-collaborative, mobile health, randomized, pilot, intervention trial of four mobile health components to reduce high blood pressure (BP) compared to usual care. It was designed and tested within a community-based participatory research framework among African Americans recruited and randomized from churches in Flint, Michigan. The purpose of this pilot study was to assess the feasibility of the Reach Out processes. Feasibility was assessed by: willingness to consent (acceptance of randomization), proportion of weeks participants texted their BP readings (intervention use), number lost to follow-up (retention), and responses to post-intervention surveys and focus groups (acceptance of intervention). Of the 425 church members who underwent BP screening, 94 enrolled in the study, and 73 (78%) completed the 6 month outcome assessment. Median age was 58 years and 79% were women. Participants responded with their BPs on average to 13.7 (sd=10.7) weeks out of 26 weeks that the BP prompts were sent. All participants reported satisfaction with the intervention. Reach Out, a faith-collaborative, mobile health intervention was feasible. Further study of the efficacy of the intervention and additional mobile health strategies should be considered.
Hypertension is the most important modifiable cardiovascular risk factor (Turnbull & Blood Pressure Lowering Treatment Trialists, 2003). Currently, the US faces a hypertension epidemic as about 80 million adults, 30% of the adult population, have hypertension.(“Hypertension among adults aged 20 and over,”) Hypertension disproportionally affects African Americans; 43% of African American have hypertension compared to 28% of non-Hispanic whites.(“Hypertension among adults aged 20 and over,”) African Americans are also less likely to have their blood pressure (BP) controlled, and for a given BP, African Americans are at a higher risk of stroke than non-Hispanic whites(Howard G & et al., 2013).
Racial disparities are also evident among midlife Americans. Midlife African Americans have a higher prevalence of hypertension than midlife whites (“Racial/Ethnic disparities in the awareness, treatment, and control of hypertension - United States, 2003–2010,” 2013). Overall, midlife Americans are less likely to have their hypertension controlled and are more likely to have poor medication adherence and more missed appointments than their older counterparts (Barron, 1980; Morris et al., 2006; Nwankwo, Yoon, Burt, & Gu, 2013). Competing demands, such as work, young families and/or the need to provide care in multigenerational families may contribute to the ability of midlife Americans to keep medical appointments and jeopardizes the feasibility of frequent face-to-face contact, which is often a large component of healthy lifestyle interventions.
Innovative, timely, and convenient approaches to reach people, particularly midlife African Americans, with high BP are needed. One promising approach is to extend the reach of medicine into the community. Text messaging is an appealing strategy given its low cost, ease of adoption, scalability, and current popularity especially in minority populations (Bennett, 2012). Mobile health interventions that address obesity and physical activity have shown promise in African American communities (Lin et al., 2015; Wilson et al., 2015). Initially lagging behind these other conditions, text messaging interventions for hypertensive patients are increasing.(Hall, Cole-Lewis, & Bernhardt, 2015) A recent American Heart Association scientific statement on the use of mobile health for cardiovascular disease prevention found 13 trials of which three (all performed outside of the US) used primarily text messaging to promote BP control (Burke et al., 2015). Two of the three trials showed a reduction in BP, but results were limited by low subject retention and absence of intention-to-treat analysis (Kiselev, Gridnev, Shvartz, Posnenkova, & Dovgalevsky, 2012; Logan et al., 2012). Furthermore while some studies have focused on hypertensive African Americans, these studies were limited to medical settings (Buis, Artinian, Schwiebert, Yarandi, & Levy, 2015). Overall studies demonstrate the potential of text messaging interventions to reduce high BP, however multiple questions remain about the feasibility of these interventions within the community setting (Burke et al., 2015).
A community-based participatory research (CBPR) framework, which emphasizes equal partnership of expertise, decision making, and ownership in research between community members and academic researchers, may be an important approach to exploring community mobile health interventions. In this framework, we developed and tested Reach Out, a health behavior theory-based, faith-collaborative, mobile health, behavioral intervention to reduce high BP among African Americans in Flint, Michigan. The purpose of this pilot study was to assess the feasibility of Reach Out processes (Thabane et al., 2010). Feasibility was defined by acceptance of randomization, proportion of participants active in the intervention, retention, and acceptance of the intervention (Bowen et al., 2009). Difference in the pre-and post-intervention BP between the intervention and control group was an exploratory outcome. We also discuss the development of Reach Out.
Methods
Reach Out was conducted in Flint, Michigan, USA. About 100,00 people live in the predominately African American (60%) city and over 40% of the population live below the poverty level (“United States Census Bureau,”). In alignment with CBPR principles, community and academic partners shared responsibility for identifying areas of interest and need within the community, developing and testing the intervention, and disseminating results (Israel, Eng, Schulz, & Parker, 2012; Wallerstein & Duran, 2010). Our partnership is composed of academic partners from the University of Michigan Stroke Program, the Eastern Michigan University Health Education Program and community partners from the Bridges into the Future, a faith-based organization dedicated to improving the health of the Flint community. The partnership was established in 2009 as part of a CDC grant award, which facilitated community-academic development and partnership. In addition to stroke prevention, the partnership also works to increase stroke preparedness (Lesli E Skolarus et al., 2016; Lesli E. Skolarus et al., 2011). The academic partners, led by Dr. Skolarus, and the community partners, led by Elder Bailey, have weekly communication surrounding the projects and meet with the larger partnership as needed. The partnership conducted community focus groups with 38 African American adults between November 2011 and March 2012 (Lesli E. Skolarus et al., 2013). The results of the focus groups confirmed an existing community awareness of high BP, an interest in healthy lifestyle strategies, and a call for stroke prevention strategies. In response to these findings and at the specific request of church leaders, the academic and community partners decided to address high BP among members of local faith-based organizations. Reach Out was a collaborative program given it was both faith placed, with the church involved in recruiting and delivering the intervention and faith based initiative, with church health team involvement (Campbell et al., 2007; DeHaven, 2004). Furthermore, the continued church involvement in the dissemination of the findings and future projects is also emblematic of collaborative programs (DeHaven, 2004).
Reach Out Intervention Theory, Development and Implementation
Self-determination theory (SDT) provided the behavioral framework for Reach Out (Deci & Ryan, 2000; Ryan & Deci, 2000). SDT proposes that an individual’s belief that he/she can perform the behavior (competence), his/her perceived control over the behavior (autonomy), and his/her connection with others (relatedness) contribute to intrinsic motivation and sustained behavior change. SDT guided the development of the targeted and generic text messages, which stressed competence in the participants’ ability to change their behavior, autonomy to make healthy choices, and relatedness to others by encouraging participants to include family and friends in their efforts at healthy behavior change.
Reach Out consisted of four components: prompted BP self-monitoring, tailored text messages related to these BP results, targeted healthy behavior text messages, and generic healthy behavior text messages. Tailoring and targeting are both health behavior strategies to increase the personal relevance and therefore the efficacy of behavioral interventions (Kreuter, Lukwago, Bucholtz, Clark, & Sanders-Thompson, 2003). Targeting refers to the creation of materials focused on shared characteristics of a group of people. In contrast, tailoring refers to materials focused on characteristics of individuals. Additionally, generic messages were culturally relevant to African Americans and provided geographically relevant options for physical activity. After the messages were finalized, a text messaging road map was created.
During the trial, all text messages were delivered automatically through a text messaging platform developed by Mosio (“Mosio,”). Participants were instructed not to send text messages to the research team other than weekly prompted BP recordings. If other messages were sent, participants received the automated response “Remember: this is an automated messaging system, and texts other than your BP are not read. If you have questions, ask your Dr. If this is an emergency call 911.”
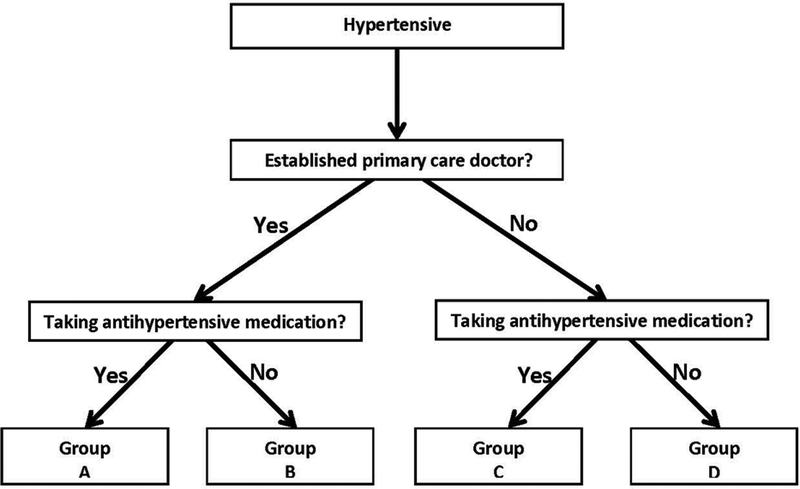
To facilitate prompted BP self-monitoring, participants randomized to the intervention were given an automated home BP monitor. Each Wednesday, participants were sent a text messages prompting them to measure their BP and text it back to the research. Up to 3 prompted messages were sent, until a BP was texted back. After texting BP recordings to the team, participants received tailored text messages that compared their current BP to their enrollment BP. Participants who reported a BP > 180/110 mm Hg were sent an automated emergency message instructing them to contact a doctor within the next 1 to 2 days. Reach Out did not contact participants or health providers in follow up. While all participants received prompted BP self-monitoring messages and tailored text messages one day per week, participants were able to select the frequency of targeted and generic text messages (twice daily, daily, or every other day) which resulted in a range from 1 targeted and 2 generic healthy behavior text messages weekly to 2 targeted and 10 generic healthy behavior text messages weekly. Targeted healthy behavior text messages were based on whether participants had a primary care provider and/or took antihypertensive medications at the time of enrollment, as shown in Figure 1. Generic health behavior text messages addressed BP goals and important lifestyle modifications to reduce BP including decreased sodium intake, increased fruit and vegetable intake, and increased physical activity.
Figure 1:
Targeted Healthy Behavior Text Messaging Road Map
Participant Recruitment, Eligibility, and Outcome Assessment
Participants were recruited from three African American churches during dedicated recruitment events following church services. Approximately two weeks before the recruitment day, Reach Out fliers were placed in the church and announcements were printed in the church bulletin. On the day of recruitment, announcements regarding Reach Out recruitment were made during church services by the pastor or other members of the church. Church service attendees were offered BP screenings. Adults, 18 years or older, with a BP≥140/90 mm Hg and mobile phones with text messaging capabilities were considered eligible and offered participation. Those who provided written informed consent were randomized to usual care group or intervention group. By design, we used broad inclusion criteria and did not exclude based on church membership. Blocked randomization was performed using blocks of 8 to allocate individuals to intervention or control in a 1:1 ratio.
All participants’ received written materials developed by the American Heart Association about the importance of hypertension management among African Americans. (“High Blood Pressure and African Americans,”) Participants randomized to the intervention received a validated, automated, oscillometric BP monitor (Omron BP760)(“Sphygmomanometers for Self-measurement of Blood Pressure (SBPM),”) and were taught to measure, record and text back their BPs during the recruitment event. Participants also selected their preferred frequency of text messages for the duration of the intervention during the recruitment event. Participants randomized to usual care received the written American Heart Association materials at enrollment and text messages regarding outcome assessments. They received no additional intervention as part of the trial. At the conclusion of the trial, BP cuffs were made available via church health teams.
Assessments were conducted at study enrollment and at church-based conclusion events approximately 6 months post enrollment. Reminder text messages were sent to participants to notify them of the time and location of the conclusion event. If a participant did not attend one of the church-based conclusion events, the research team telephoned the participant and determined a mutually convenient meeting place and time to complete the assessment. Participants received $10 at the completion of baseline data collection and $20 at completion of the outcome assessment.
Outcomes
The main outcomes of this pilot trial assessed the feasibility of the Reach Out processes. Feasibility was assessed by: willingness to consent (acceptance of randomization), proportion of weeks participants texted their BP readings (intervention use), number lost to follow-up (retention), and responses to post-intervention surveys and focus groups (acceptance of the intervention). A post-intervention survey was administered to participants randomized to the intervention. The survey assessed overall satisfaction with the intervention (very satisfied and satisfied vs. neither satisfied nor dissatisfied, dissatisfied, very dissatisfied), as well as satisfaction with the intervention components. The survey also queried variables that may be important for future tailoring of text messages, such as determining the BP-related complication that was most worrisome to participants (stroke, heart attack, peripheral vascular disease, kidney failure, vision problems, other) and the preferred frequency of text messages.
Clinical outcomes were also assessed. Members of the research and church health team who were blinded to the treatment assignment assessed each participant’s systolic and diastolic BP at enrollment and at six months. All BPs were measured using the validated, automated, oscillometric BP monitor (Omron BP 760).(“Sphygmomanometers for Self-measurement of Blood Pressure (SBPM),”) Using a standard protocol, (Pickering et al., 2005) one BP measurement was taken during the church based enrollment and final outcome assessment. Medication adherence was assessed with a single item “Do you sometimes forget to take your BP medications?” (Morisky, Green, & Levine, 1986). Participant characteristics included health literacy, measured by the question “How confident are you filling out medical forms by yourself?”(Chew et al., 2008). Participants who responded as somewhat or less confident were determined to have low health literacy. Food insecurity was assessed with two questions that queried over the last 12 months whether ‘the food that I bought just didn’t last, and I didn’t have money to get more’ or ‘I couldn’t afford to eat balanced meals’. (“Food Security in the U.S.,”) Finally cost-related medication non-adherence was assessed with, “During the past 12 months, have you ever taken less of any medications prescribed by your doctor because of the cost?”(Levine et al., 2013).
Focus groups
Focus groups were conducted at one of the churches after the completion of Reach Out to learn about participant perceptions of the intervention. Both low frequency responders (i.e. participants who rarely or never responded to prompted BP self-monitoring text messages) and high frequency responders (i.e. participants who responded weekly to prompted BP self-monitoring text messages) were invited to participate in separate focus groups. Focus groups were moderated by a community partner, who previously worked as a social worker and has undergone specific training in qualitative interviewing. Academic partners provided assistance and note-taking. The focus group guide included questions about overall and specific experiences throughout Reach Out (see appendix). Focus group participants received $20 after completion of the approximately 60 minute session.
CBPR Process
Academic and community partners collaborated in each phase of the process. The phases included: focus groups to identify hypertension as an important community health issue (November 2011 and March 2012), conceptualization and intervention development (February 2013 to January 2014), intervention (February 2014 to April 2015), post-intervention focus groups and dissemination of findings (May to August 2015). After identifying hypertension as a key community priority, we then focused on the design of the intervention. Our strong commitment to ease of implementation combined with the ubiquity of mobile phones in the community resulted in selection of a mobile health intervention as the foundation for Reach Out. The text messages were then drafted by a physician (LS) and health behavior and health education professionals (MD, JC) guided by SDT. Messages were then reviewed by a community partner (SB) who added local context and community appropriateness. The community partners then reviewed the messages with a group of local individuals who served as advisors to Bridges into the Future. These individuals represented the race, sex, and age distribution of the trial population. These interviews were conducted in small groups and individual interviews at locations throughout the community. Community and academic partners reviewed American Heart Association materials on hypertension and selected hypertension materials focused on African Americans (“High Blood Pressure and African Americans,”). We also selected local churches based on church interest and church location; we were committed to diverse geographic locations throughout the city. Community and academic partners, church health teams and church leadership, including pastors and elders, were present for the recruitment events. Church health team members assisted in BP screening. Additionally, church leadership was very supportive making church announcements and participating in screening. Upon completion of the trial, results were disseminated to church leadership both verbally and through letters. Participants were given the results of the study through the churches and during the focus groups for those who choose to participate. At the completion of the study, BP cuffs were given to the church health teams to disseminate to interested usual care participants.
Analysis:
Sociodemographics, co-morbidities, health literacy,(Chew et al., 2008) food insecurity(“Food Security in the U.S.,”) and cost-related medication non-adherence(Levine et al., 2013) were compared using descriptive statistics. For the 6 month intervention, we determined the number of BP text messages sent to the research team in response to the BP prompts. Subject satisfaction was summarized using univariate statistics. As an exploratory analysis, the pre-and post-intervention change in BP in the intervention group was compared to BP change in the usual care group using the two-sample t-test. Medication adherence was assessed using the Wilcoxon signed rank test. We did not adjust for multiple comparisons, because these exploratory analyses serve only for hypothesis generation. Qualitative content analysis was used to analyze the focus group data (Hsieh & Shannon, 2005). Quantitative analyses were conducted in Stata 11 and SAS. This study was approved by the University of Michigan Institutional Review Board and was registered on clinicaltrials.gov ().
Results
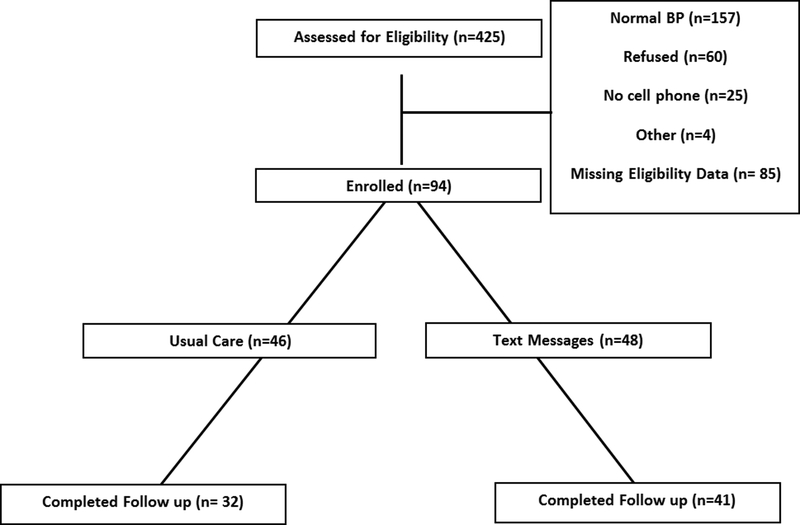
Of the 425 church members who underwent BP screening, 94 enrolled in the trial. Among the recorded intervention exclusions, normal BP was the most frequent (Figure 2). Absence of text messaging capability accounted for about 8% of recorded exclusions. While 18% of the exclusions were due to enrollment refusals, there were no exclusions due to refusals to be randomized. Of the 94 (46 usual care, 48 intervention) participants, 73 (32 usual care, 41 intervention) participants completed the outcome assessment.
Figure 2:
Reach Out Eligibility and Outcome Assessment
Nearly all participants were African American (97%) and 79% were women (Table 1). The mean age was 58 (sd=9.8) years. A total of 85% of participants reported a known history of hypertension, 85% reported taking an antihypertensive medication, and 16% reported having been hospitalized for hypertension in the past. Additionally, 85% of participants were under the care of a primary care provider. Nearly 20% of participants had low health literacy and 30% reported cost-related medication non-adherence. Food insecurity in the last year was high among participants. Approximately 45% of respondents could not afford enough food, and 38% reported they could not afford to eat balanced meals. Stroke and heart attack were identified as the most worrisome consequences of hypertension (32% each), followed by kidney failure (12%). Participants were nearly evenly divided between preference for receiving messages once per day (41%) and every other day (46%). Few participants preferred two messages per day (13%).
Table 1:
Sociodemographics, comorbidity, and other baseline characteristics.
| Total Participants % or mean (SD) |
Usual Care N=46 % or mean (SD) |
Intervention N=48 % or mean (SD) |
p | |
|---|---|---|---|---|
| Age years, (n=92) |
58 (9.8) |
58.7 (11.2) |
57.8 (8.5) |
0.65 |
| Women (n=90) |
79 | 77 | 80 | 0.71 |
| African American (n=92) |
97 | 98 | 96 | 0.63 |
| Takes hypertension
medications (n=91) |
85 | 80 | 89 | 0.20 |
| Prior hypertension
hospitalization (n=94) |
16 | 20 | 13 | 0.35 |
| History of hypertension (n=94) |
85 | 83 | 88 | 0.51 |
| Current smoker (n=94) |
12 | 9 | 15 | 0.38 |
| Under the care of a primary care
provider (n=92) |
85 | 85 | 85 | 0.93 |
| Insurance status (N=92) |
0.55 | |||
| Private | 47 | 46 | 48 | |
| Medicare | 16 | 17 | 15 | |
| Medicaid | 22 | 20 | 24 | |
| Other | 20 | 20 | 20 | |
| Uninsured | 7 | 9 | 4 | |
| Low health literacy⃰ (n=94) |
19 | 15 | 23 | 0.53 |
| Cost-related medication non-adherence∞ (n=71) |
30 | 21 | 40 | 0.71 |
| Cannot afford enough food~ (n=86) |
||||
| Often true | 12 | |||
| Sometimes true | 34 | |||
| Never true | 50 | |||
| Don’t Know | 5 | |||
| Cannot afford to eat balanced meals~ (n=89) |
||||
| Often true | 10 | |||
| Sometimes true | 28 | |||
| Never true | 61 | |||
| Don’t Know | 1 |
*“How confident are you filling out medical forms by yourself?”(Chew et al., 2008) Those who responded with somewhat or less confident were determined to have low health literacy.
During the past 12 months, have you ever taken less of any medications prescribed by your doctor because of the cost?
Food insecurity was assessed with two questions that queried over the last 12 months whether ‘the food that I bought just didn’t last, and I didn’t have money to get more’ or ‘I couldn’t afford to eat balanced meals’.
Feasibility Outcomes
In total, participants texted back their BP readings to the research team on 587 (47%) of the available 1248 person-weeks on which they received prompts. Participants responded on average to 13.7 (sd=10.7) weeks out of 26 weeks the BP prompts were sent. A total of 7 participants (17%) did not respond to any weeks of BP text message prompts, while 11 (26%) participants responded with their BP every week. There was no difference in age or baseline BP between participants who responded to any BP prompts and those who did not respond to these prompts. Four participants received one emergency BP message, one participant received two emergency BP messages, and one participant received three emergency BP messages.
Of those intervention participants who responded (n=37), 100% reported satisfaction with the intervention. Over 90% found that the language used in the intervention was consistent with language that they use, 84% found the BP monitor easy to use, and 95% felt that the messages provided helpful tips to manage BP. Furthermore, 84% would have chosen to continue to receive text messages if they could. Few (8%) respondents reported technical problems with the text messages. At the conclusion of the study, respondents were mixed in their stated preferences for the frequency of text messages (grouped irrespective of their actual frequency of provided text messages during the intervention): 30% preferred weekly texts, 30% preferred every other day texts, and 21% preferred twice daily texts. Concerning the overall length of the intervention, 81% of participants thought the duration of Reach Out was “just right.”
Clinical Outcomes
There were no between group differences in the change from pre- to post-intervention systolic or diastolic BP (Table 2). The within intervention group change in systolic BP was −11.3 mmHg (sd=22.9 mmHg) and within the control group was −14.4 mmHg (sd=26.4 mmHg); this between group difference was not significant (−3.1, 95% CI −14.4, 8.3, p=0.60). Similarly, the within intervention group change in diastolic BP was −8.6 (sd=15.9) and within the control group was −9.5 mmHg (sd=12.9 mmHg); this between group difference was not significant (−0.9, 95%CI −7.7, 5.9, p=0.79). Within the intervention group, there was no change in medication adherence (p=0.69).
Table 2:
Change in Blood Pressure
| Baseline | 6 months | Reduction from
Baseline Mean (SD) |
P value for between groups difference in blood pressure | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||
| Systolic Blood Pressure, mmHg | ||||
| Control | 162.2 (20.5) | 146.7 (20.5) | 14.4 (26.4) | |
| ntervention | 160.7 (23.6) |
147.2 (21.8) | 11.3 (22.9) | 0.60 |
| Diastolic Blood Pressure, mmHg | ||||
| Control | 99.2 (17.8) | 88.5 (11.5) | 9.5 (12.9) | |
| Intervention | 99.0 (11.8) |
89.4 (13.9) | 8.6 (15.9) | 0.79 |
Focus groups following completion of the intervention
The “low frequency BP responder” focus group included 4 participants (1 man and 3 women) and the “high frequency BP responder” focus group also included 4 participants (2 men and 2 women). The majority of the low frequency responders reported technical problems with responding to the text. Feedback included responses such as “I had a problem texting back, sometimes it wouldn’t accept it. I would wonder what I was doing wrong.” However, many reported that they continued to take their BP each week. The feedback about the targeted and generic healthy behavior text messaging was overwhelmingly positive from both focus groups. Multiple subjects queried, ‘Where are my texts? Can I have them back?’ A participant noted “Everyday [text messages] would be fine for me, it reminded me to take my BP medication.” Tailored text messages received unanimous positive responses. Participants reported using their texts to keep a record of their BPs to take to their primary care providers. In some cases, multiple family members used the BP monitor. Overwhelmingly, participants did not want text messages supplemented with phone calls, workshops, cooking demonstrations, or internet modules. Additionally, participants did not want religious content included in their text messages.
Discussion
Reach Out, a pilot trial of a faith-collaborative, mobile health intervention to decrease high BP in an economically disadvantaged, urban, predominately African American community, supports the feasibility of the study design within the community. We found ease of recruitment of hypertensive participants from a faith-based setting, pervasiveness of mobile phones in the community, acceptance of randomization and adequate study retention. Additionally, participants were highly engaged in the intervention as evident by their willingness to self-monitor their BP and text their weekly BP to the study team. Furthermore, quantitative and qualitative data support high acceptability of the Reach Out program. Our results provide critical insights into the design of future trials of mobile health interventions for this underserved population, which is otherwise challenging to reach.
One advantage of faith-collaborative, mobile health interventions like Reach Out is its ability to target a high-risk population that may be difficult to reach through more traditional medical clinic-based efforts. A significant proportion of our participants had financial barriers to medical care, as evidenced by the higher proportion of patients with lower health literacy, financially-based medication nonadherence, and food insecurity. Like other faith-placed interventions,(Lancaster, Carter-Edwards, Grilo, Shen, & Schoenthaler, 2014; Resnicow et al., 2004) Reach Out predominately enrolled midlife African American women, a group with the highest prevalence of high BP of any racial/ethnic group in the U.S (Mozaffarian et al., 2015). Elevated midlife BP increases the risk of stroke for up to the next 30 years and is associated with later-life cognitive decline,(Gottesman, Schneider, Albert, & et al., 2014) which highlights the need for interventions to improve BP control in populations at such high risk. In addition, Reach Out, like other faith-placed interventions, was able to reach people who do not seek routine preventive medical care. In our study, we found that 15% of participants were not taking any antihypertensive medications and 15% of participants did not have a primary care provider.
While this study demonstrates the feasibility of the intervention to the target community population, no statistically significant BP treatment effect was identified. This may be related to the small sample size of this pilot design resulting in inadequate power to detect small but potentially clinically meaningful decreases in BP. This possibility is supported by the wide confidence interval for the between group difference in BP of the intervention group compared to the control group (Bland, 2009). Obscuring a difference may also be regression to the mean as BP decreased in both groups given that an elevated BP was part of the enrollment criteria. Alternately, it may be that the intervention was not sufficiently intense. Data on the efficacy of BP self-monitoring among African Americans are mixed. Systematic reviews and meta-analyses have shown that BP self-monitoring is effective in reducing BP, particularly when paired with additional support or tele-monitoring (Bray, Holder, Mant, & McManus, 2010; Cappuccio, Kerry, Forbes, & Donald, 2004; Uhlig, Patel, Ip, Kitsios, & Balk, 2013). In contrast, BP self-monitoring trials have had no impact on BP compared to usual care when tested in urban, largely minority clinic populations (Hebert et al., 2012; Yi et al., 2015) though notably, these previous self-monitoring trials did not include text messages or tele-monitoring. Little is known about the efficacy of tailored responses to BP or of targeted or generic healthy behavior text messaging interventions in predominately African American communities. Moving forward, one possible strategy may be a clinical trial design such as multiphase optimization strategy testing (MOST), which allows testing of multiple intervention components and ‘dose’ of the intervention component to select the most promising components of a multicomponent health behavioral intervention (Collins, Murphy, Nair, & Strecher, 2005). Increasing the intensity of the intervention by adding other intervention components, such as financial assistance via transportation vouchers to provider appointments or medication assistance, could also be considered.
Our study had several strengths. First, Reach Out was created within a CBPR framework at the request of the Flint, African American, faith-based community in which the intervention was delivered. The intervention was personalized, allowing participants to select their preferred frequency of text messages and text messages were tailored to the individual participants’ own BP recordings. The study design was rigorous in that it was randomized and included a control group. We found a high penetrance of text messaging capability in the community suggesting the intervention would be readily scalable. Finally, Reach Out enrolled an underserved, racial minority population with a high need for primary and secondary cardiovascular disease prevention programs and demonstrates that there is both a capacity and a demand to engage in interventions within this population.
Our study had limitations. First, while we had an attrition rate of 22% at the 6-month follow-up, this is similar to that seen in other community-based studies in underserved minority populations in community health centers(Ogedegbe et al., 2014) and churches (Lancaster et al., 2014; Resnicow et al., 2004). Second, due to the high volume of interested participants at the time of enrollment, we were unable to perform 3 consecutive BP readings according to the suggested best practices for measuring BP. For consistency, one BP was recorded at the follow up assessments. Medication adherence was based on self-report rather than pill counts or pharmacy records. The health literacy assessment question was validated in a medical setting rather than in the community. Additionally, there were some technical difficulties that prevented some participants from responding with their BPs and thus receiving the tailored messages. This could be mitigated in the future by initial technology check-ins with participants as they begin the intervention.
In conclusion, this study has shown that a faith-collaborative, mobile health intervention addressing elevated BP is feasible with an underserved African American community-based population. Future interventions should consider study designs to assess the optimum ‘dose’ of text messages, and assess additional mobile health strategies to increase the intensity of the intervention.
Funding:
The Project was funded by the University of Michigan Cardiovascular Center Inaugural award (Skolarus). Dr. Skolarus was funded by NIH/NINDS K23 NS073685; Drs. Baek and Wheeler were funded by NIH/NINDS U10 NS086526.
Appendix: Reach Out Focus Group Guide:
How did you feel about the REACH OUT platform in an overall sense?
How could we make REACH OUT better?
Did you have any technical difficulties with the text messaging system?
How did you feel about the specific messages you received?
How did you feel about the topics addressed? Were they relevant to you, or would you have liked to have been messaged about something else?
What did you think about the frequency with which you received the text messages?
How do you feel about the blood pressure cuff you received? Did you find it useful? How often did you use it? Will you continue to use it in the future?
Would you like more or less of a particular type of message?
Are there any specific aspects of religious content that should be included in REACH OUT messages?
Are there any specific aspects of the African American culture that should be Figure 1: Targeted Healthy Behavior Text Messaging Road Map
included?
References
- Barron WM (1980). Failed Appointments - Who Misses Them, Why They Are Missed, and What Can Be Done. Primary Care, 7(4), 563–574. [PubMed] [Google Scholar]
- Bennett GG (2012). Connecting eHealth with 2-1-1 to reduce health disparities. American journal of preventive medicine, 43(5), 5. [DOI] [PubMed] [Google Scholar]
- Bland JM (2009). The tyranny of power: is there a better way to calculate sample size? Bmj, 339, b3985. [DOI] [PubMed] [Google Scholar]
- Bowen DJ, Kreuter M, Spring B, Cofta-Woerpel L, Linnan L, Weiner D, … Fabrizio C (2009). How we design feasibility studies. American journal of preventive medicine, 36(5), 452–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray EP, Holder R, Mant J, & McManus RJ (2010). Does self-monitoring reduce blood pressure? Meta-analysis with meta-regression of randomized controlled trials. Annals of medicine, 42(5), 371–386. [DOI] [PubMed] [Google Scholar]
- Buis LR, Artinian NT, Schwiebert L, Yarandi H, & Levy PD (2015). Text Messaging to Improve Hypertension Medication Adherence in African Americans: BPMED Intervention Development and Study Protocol. JMIR research protocols, 4(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke LE, Ma J, Azar KM, Bennett GG, Peterson ED, Zheng Y, … Quinn CC (2015). Current Science on Consumer Use of Mobile Health for Cardiovascular Disease Prevention: A Scientific Statement From the American Heart Association. Circulation, 132(12), 1157–1213. doi: 10.1161/cir.0000000000000232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, & Baskin M (2007). Church-based health promotion interventions: evidence and lessons learned. Annu. Rev. Public Health, 28, 213–234. [DOI] [PubMed] [Google Scholar]
- Cappuccio FP, Kerry SM, Forbes L, & Donald A (2004). Blood pressure control by home monitoring: meta-analysis of randomised trials. Bmj, 329(7458), 145. doi: 10.1136/bmj.38121.684410.AE [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew L, Griffin J, Partin M, Noorbaloochi S, Grill J, Snyder A, … VanRyn (2008). Validation of Screening Questions for Limited Health Literacy in a Large VA Outpatient Population. Journal of General Internal Medicine, 23(5), 561–566. doi: 10.1007/s11606-008-0520-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins LM, Murphy SA, Nair VN, & Strecher VJ (2005). A strategy for optimizing and evaluating behavioral interventions. Annals of Behavioral Medicine, 30(1), 65–73. [DOI] [PubMed] [Google Scholar]
- Deci EL, & Ryan RM (2000). The” what” and” why” of goal pursuits: Human needs and the self-determination of behavior. Psychological inquiry, 11(4), 227–268. [Google Scholar]
- DeHaven MJ (2004). Health programs in faith-based organizations: are they effective? American journal of public health (1971), 94(6), 1030–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Food Security in the U.S. United States Department of Agriculture Economic Research Service. Retrieved from http://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us.aspx
- Gottesman RF, Schneider AC, Albert M, & et al. (2014). Midlife hypertension and 20-year cognitive change: The atherosclerosis risk in communities neurocognitive study. JAMA Neurology, 71(10), 1218–1227. doi: 10.1001/jamaneurol.2014.1646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall AK, Cole-Lewis H, & Bernhardt JM (2015). Mobile Text Messaging for Health: A Systematic Review of Reviews. Annual review of public health, 36, 393–415. doi: 10.1146/annurev-publhealth-031914-122855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebert PL, Sisk JE, Tuzzio L, Casabianca JM, Pogue VA, Wang JJ, … McLaughlin MA (2012). Nurse-led disease management for hypertension control in a diverse urban community: a randomized trial. Journal of General Internal Medicine, 27(6), 630–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- High Blood Pressure and African Americans. Retrieved from http://www.heart.org/HEARTORG/Conditions/HighBloodPressure/UnderstandYourRiskforHighBloodPressure/High-Blood-Pressure-and-African-Americans_UCM_301832_Article.jsp#.WFARR2orLRY
- Howard G, L. DT K. DO, & et al. (2013). RAcial differences in the impact of elevated systolic blood pressure on stroke risk. JAMA Internal Medicine, 173(1), 46–51. doi: 10.1001/2013.jamainternmed.857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh H-F, & Shannon SE (2005). Three Approaches to Qualitative Content Analysis. Qualitative Health Research, 15(9), 1277–1288. doi: 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- Hypertension among adults aged 20 and over. Retrieved from www.cdc.gov/nchs/data/hus/2015/054.pdf
- Israel BA, Eng E, Schulz AJ, & Parker EA (2012). Methods for Community-Based Participatory Research for Health: Wiley. [Google Scholar]
- Kiselev AR, Gridnev VI, Shvartz VA, Posnenkova OM, & Dovgalevsky PY (2012). Active ambulatory care management supported by short message services and mobile phone technology in patients with arterial hypertension. Journal of the American Society of Hypertension, 6(5), 346–355. [DOI] [PubMed] [Google Scholar]
- Kreuter MW, Lukwago SN, Bucholtz DC, Clark EM, & Sanders-Thompson V (2003). Achieving Cultural Appropriateness in Health Promotion Programs: Targeted and Tailored Approaches. Health Education & Behavior, 30(2), 133–146. doi: 10.1177/1090198102251021 [DOI] [PubMed] [Google Scholar]
- Lancaster KJ, Carter-Edwards L, Grilo S, Shen C, & Schoenthaler AM (2014). Obesity interventions in African American faith-based organizations: a systematic review. Obesity Reviews, 15, 159–176. doi: 10.1111/obr.12207 [DOI] [PubMed] [Google Scholar]
- Levine DA, Morgenstern LB, Langa KM, Piette JD, Rogers MA, & Karve SJ (2013). Recent trends in cost‐related medication nonadherence among stroke survivors in the United States. Annals of neurology, 73(2), 180–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin M, Mahmooth Z, Dedhia N, Frutchey R, Mercado CE, Epstein DH, … Cheskin LJ (2015). Tailored, Interactive Text Messages for Enhancing Weight Loss Among African American Adults: The TRIMM Randomized Controlled Trial. The American journal of medicine, 128(8), 896–904. doi: 10.1016/j.amjmed.2015.03.013 [DOI] [PubMed] [Google Scholar]
- Logan AG, Irvine MJ, McIsaac WJ, Tisler A, Rossos PG, Easty A, … Cafazzo JA (2012). Effect of home blood pressure telemonitoring with self-care support on uncontrolled systolic hypertension in diabetics. Hypertension, 60(1), 51–57. [DOI] [PubMed] [Google Scholar]
- Morisky DE, Green LW, & Levine DM (1986). Concurrent and predictive validity of a self-reported measure of medication adherence. Medical care, 24(1), 67–74. [DOI] [PubMed] [Google Scholar]
- Morris AB, Li J, Kroenke K, Bruner-England TE, Young JM, & Murray MD (2006). Factors associated with drug adherence and blood pressure control in patients with hypertension. Pharmacotherapy, 26(4), 483–492. doi: 10.1592/phco.26.4.483 [DOI] [PubMed] [Google Scholar]
- Mosio. Retrieved from http://www.mosio.com/
- Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, … Howard VJ (2015). Heart Disease and Stroke Statistics—2015 Update A Report From the American Heart Association. Circulation, 131(4), e29–e322. [DOI] [PubMed] [Google Scholar]
- Nwankwo T, Yoon SS, Burt V, & Gu Q (2013). Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011–2012. NCHS data brief(133), 1–8. [PubMed] [Google Scholar]
- Ogedegbe G, Tobin JN, Fernandez S, Cassells A, Diaz-Gloster M, Khalida C, … Schwartz J (2014). Counseling African Americans to Control Hypertension (CAATCH): cluster randomized clinical trial main effects. Circulation, CIRCULATIONAHA. 113.006650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, … Roccella (2005). Recommendations for Blood Pressure Measurement in Humans and Experimental Animals: Part 1: Blood Pressure Measurement in Humans: A Statement for Professionals From the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension, 45(1), 142–161. doi: 10.1161/01.HYP.0000150859.47929.8e [DOI] [PubMed] [Google Scholar]
- Racial/Ethnic disparities in the awareness, treatment, and control of hypertension - United States, 2003–2010. (2013). MMWR Morb Mortal Wkly Rep, 62(18), 351–355. [PMC free article] [PubMed] [Google Scholar]
- Resnicow K, Kramish Campbell M, Carr C, McCarty F, Wang T, Periasamy S, … Stables G (2004). Body and soul: a dietary intervention conducted through African-American churches. American journal of preventive medicine, 27(2), 97–105. doi:DOI: 10.1016/j.amepre.2004.04.009 [DOI] [PubMed] [Google Scholar]
- Ryan RM, & Deci EL (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol, 55(1), 68–78. [DOI] [PubMed] [Google Scholar]
- Skolarus LE, Murphy JB, Zimmerman MA, Bailey S, Fowlkes S, Brown DL, … Morgenstern LB (2013). Individual and Community Determinants of Calling 911 for Stroke Among African Americans in an Urban Community. Circulation: Cardiovascular Quality and Outcomes, 6(3), 278–283. doi: 10.1161/circoutcomes.111.000017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skolarus LE, Zimmerman MA, Bailey S, Dome M, Murphy JB, Kobrossi C, … Morgenstern LB (2016). Stroke Ready Intervention: Community Engagement to Decrease Prehospital Delay. Journal of the American Heart Association, 5(5), e003331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skolarus LE, Zimmerman MA, Murphy J, Brown DL, Kerber KA, Bailey S, … Morgenstern LB (2011). Community-Based Participatory Research: a new approach to engaging community members to rapidly call 911 for stroke. Stroke, 42(7), 1862–1866. doi: 10.1161/strokeaha.110.609495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sphygmomanometers for Self-measurement of Blood Pressure (SBPM). Retrieved from http://www.dableducational.org/sphygmomanometers/devices_2_sbpm.html#OmronHEM7220Z
- Thabane L, Ma J, Chu R, Cheng J, Ismaila A, Rios LP, … Goldsmith (2010). A tutorial on pilot studies: the what, why and how. BMC medical research methodology, 10(1), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turnbull F, & Blood Pressure Lowering Treatment Trialists C (2003). Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet, 362(9395), 1527–1535. [DOI] [PubMed] [Google Scholar]
- Uhlig K, Patel K, Ip S, Kitsios GD, & Balk EM (2013). Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis. Ann Intern Med, 159(3), 185–194. doi: 10.7326/0003-4819-159-3-201308060-00008 [DOI] [PubMed] [Google Scholar]
- United States Census Bureau. Retrieved from http://quickfacts.census.gov/qfd/states/26/2629000.html
- Wallerstein N, & Duran B (2010). Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health, 100(S1), S40–S46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson DK, Van Horn ML, Siceloff ER, Alia KA St. George SM, Lawman HG, … Gadson B (2015). The Results of the “Positive Action for Today’s Health” (PATH) Trial for Increasing Walking and Physical Activity in Underserved African-American Communities. Annals of Behavioral Medicine, 49(3), 398–410. doi: 10.1007/s12160-014-9664-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi SS, Tabaei BP, Angell SY, Rapin A, Buck MD, Pagano WG, … Chamany (2015). Self-Blood Pressure Monitoring in an Urban, Ethnically Diverse Population: A Randomized Clinical Trial Utilizing the Electronic Health Record. Circulation: Cardiovascular Quality and Outcomes, 8(2), 138–145. doi: 10.1161/circoutcomes.114.000950 [DOI] [PMC free article] [PubMed] [Google Scholar]