Abstract
Background
Virtual reality (VR)-based rehabilitation is considered a beneficial therapeutic option for stroke rehabilitation. This pilot study assessed the clinical feasibility of a newly developed VR-based planar motion exercise apparatus (Rapael Smart Board™ [SB]; Neofect Inc., Yong-in, Korea) for the upper extremities as an intervention and assessment tool.
Methods
This single-blinded, randomized, controlled trial included 26 stroke survivors. Patients were randomized to the intervention group (SB group) or control (CON) group. During one session, patients in the SB group completed 30 min of intervention using the SB and an additional 30 min of standard occupational therapy; however, those in the CON group completed the same amount of conventional occupational therapy. The primary outcome was the change in the Fugl–Meyer assessment (FMA) score, and the secondary outcomes were changes in the Wolf motor function test (WMFT) score, active range of motion (AROM) of the proximal upper extremities, modified Barthel index (MBI), and Stroke Impact Scale (SIS) score. A within-group analysis was performed using the Wilcoxon signed-rank test, and a between-group analysis was performed using a repeated measures analysis of covariance. Additionally, correlations between SB assessment data and clinical scale scores were analyzed by repeated measures correlation. Assessments were performed three times (baseline, immediately after intervention, and 1 month after intervention).
Results
All functional outcome measures (FMA, WMFT, and MBI) showed significant improvements (p < 0.05) in the SB and CON groups. AROM showed greater improvements in the SB group, especially regarding shoulder abduction and internal rotation. There was a significant effect of time × group interactions for the SIS overall score (p = 0.038). Some parameters of the SB assessment, such as the explored area ratio, mean reaching distance, and smoothness, were significantly associated with clinical upper limb functional measurements with moderate correlation coefficients.
Conclusions
The SB was available for improving upper limb function and health-related quality of life and useful for assessing upper limb ability in stroke survivors.
Trial registration
The study was registered with the clinical research information service (CRIS) (KCT0003783, registered 15 April 2019; retrospectively registered).
Keywords: Virtual reality, Upper extremity, Range of motion, Quality of life, Rehabilitation, Stroke
Background
Virtual reality (VR)-based rehabilitation is being increasingly used for post-stroke rehabilitation [1]. A recent systematic review mentioned that VR is an emerging treatment option for upper limb rehabilitation among stroke patients [2]. The benefits of VR include real-time feedback, easy adaptability, and the provision of safe environments that mimic the real world [3, 4]. The gaming property of VR allows patients to experience fun, active participation, positive emotions, and engagement [5, 6]. Therefore, rehabilitation with VR enables more intense and repetitive training, which is important for rehabilitation and the promotion of neural plasticity [7].
VR systems commonly used in the entertainment industry, such as Wii and Kinect, could be used for rehabilitation. However, these game-like systems are only applicable to patients with muscle strength above a certain value, thus limiting their use by more affected patients. Therefore, adjunct therapies, such as functional electrical stimulation and robotics, have been combined with these systems [8–11]. However, those adjunct therapies are costly and require continuous monitoring by healthcare professionals because of safety concerns [12, 13]. Therefore, their use is restricted to clinical settings, and they are not actively used for telerehabilitation or home-based rehabilitation. A non-motorized or non-assisted device is required for more active use of VR for rehabilitation.
We developed the Rapael Smart Board™ (SB; Neofect Inc., Yong-in, Korea), which is a VR-based rehabilitation device incorporating planar motion exercise that does not require additional gravity compensation. This two-dimensional planar movement with full gravitational support, which lessens the need for antigravity muscle facilitation, allows for much easier participation than three-dimensional movement under gravity. Additionally, it is known to be safe and easy to learn, and it has been shown to improve motor ability with less aggravation of shoulder pain and spasticity; therefore, it is useful to patients with reduced motor ability [14]. Planar motion exercises provoke less maladaptive compensatory movements. Additionally, the nearly zero friction of the linear guides enable a wide range of repetitive active range of motion (AROM) exercises. Furthermore, the SB adopted Rapael Clinic software that was originally developed for patients with disabilities and has proven efficacy for stroke rehabilitation [9, 15]. Therefore, the SB, which has multiple advantages because of its hardware and software, might be beneficial for the functional improvement of the upper extremities. Moreover, the SB could have a role as an assessment tool because VR has been reported to be useful for objective kinematic measurements of the upper extremities [16].
The present pilot study aimed to assess the availability of this newly developed VR-based rehabilitation device incorporating planar exercises for the upper extremities as an intervention and assessment tool among stroke patients in the chronic phase of recovery. To assess the availability in terms of clinical effectiveness, we compared the effects of an intervention involving the SB and that involving dose-matched occupational therapy (OT) on upper extremity function and health-related quality of life (HRQoL). We also investigated the correlations between kinematic data from the SB and data from clinical scales regarding upper extremity function.
Methods
Study design
This study was a multicenter, single-blinded, randomized, controlled trial that included 26 stroke patients from one rehabilitation hospital and one tertiary university hospital. It was conducted between May 2017 and May 2018. Patients were randomly allocated to the SB intervention (SB) group or conventional intervention (CON) group in a 1:1 ratio using a computer-generated randomization sequence. The assigned group was determined by the consecutive opening of sealed opaque envelopes that contained the name of the group; these envelopes were placed in a plastic container. Randomization was performed centrally, and group allocation was sequentially communicated to the sites via text message.
All patients participated in 20 sets of sessions, 5 days per week, over the course of 4 weeks, which is the usual amount and frequency of treatment at the site where this study was performed. During one session, patients in the SB group completed 30 min of intervention using the SB, whereas patients in the CON group completed the same amount of conventional OT in a research intervention room. During the entire intervention session, occupational therapists were present to assist patients in groups with verbal or physical instructions if necessary. Patients from both groups received an additional 30 min of regular OT in a clinical intervention room.
Outcome measures were performed by experienced occupational therapists (more than 5 years of experience performing stroke rehabilitation including measures and interventions) who were blinded to group allocation. Evaluations were conducted three times (before intervention [T0], immediately after intervention [T1], and 1 month after intervention [T2]).
Participants
The inclusion criteria were as follows: diagnosis of hemispheric stroke resulting in unilateral upper extremity deficits at least 3 months previously; first-ever ischemic or hemorrhagic stroke; ability to understand instructions, which was confirmed by a score ≥ 25 on the Korean version of the Mini-Mental State Examination; a Medical Research Council (MRC) scale score of 2 or 3 for the strength of the affected upper extremity; and a Modified Ashworth Scale (MAS) score < 2 for spasticity.
The exclusion criteria were as follows: multiple or bilateral brain lesions; age younger than 19 years; any neurological or psychological disorder other than stroke; any severe medical condition; and predisposed to severe pain in the upper extremities that could impede participation in the intervention. A researcher screened inpatient medical records and enrolled participants who were fit for the indication. All participants provided written consent before enrollment in this study, and the study was approved by the institutional review boards of both intervention sites before initiation. The study was registered at the clinical research information service (CRIS; KCT0003783).
Intervention
Smart board intervention
The SB was developed for patients with impaired upper extremity function. It is focused on proximal upper extremity rehabilitation, including AROM and coordination exercises across multiple joints. It consists of a 104.3-cm × 63.0-cm board with a two-dimensional moving forearm-supported controller, android PC, and display. Three linear guides with an H-shape configuration enable two-dimensional planar motion of the handlebar, which is attached to the horizontal linear guide (Fig. 1). The linear guides have nearly zero friction; therefore, the handlebar moves freely with high precision. Infrared sensors that detect the position of the handlebar continuously are located under the linear guides. Detachable stoppers can be used to limit the maximum moving range of the handlebar and allow one-dimensional movement training. An ergonomically designed armrest allows participants to easily use the SB. A participant is required to hold and move the handle according to the directions provided by Rapael Clinic software. Upper limb movement is visualized as real-time feedback on the system monitor that is linked to the software. Additionally, a printable progress report is presented with training history when the training session is completed. All data are registered in the system individually and are utilized for personalized intervention. The SB assigns a specific gamified intervention among 17 training programs and adjusts the difficulty level to promote active participation in the intervention. The difficulty level of the SB intervention is determined based on the initial assessment before training on the day of participation and the medical history; the specific algorithm for adjusting the level of difficulty has been described previously [15, 17].
Fig. 1.
Hardware of the Smart Board. The board and forearm-supported controller. Three linear guides with an H-shape configuration enable two-dimensional planar motion of the handlebar, which is attached to the horizontal linear guide
Smart board assessment program
The SB has the following three different kinematic assessment programs: free exploration, point-to-point reaching, and circle-drawing (Fig. 2). During the free exploration task, the participant is required to fill a large half-circle as suggested on the system screen by sweeping over the area as much as possible on the board within a given time, thus reflecting upper extremity AROM and visuomotor mapping ability. During the point-to-point reaching task, a participant is required to move the handle from a centrally located target to 10 targets with five different angles at two different distances, reflecting the ability to perform forward reaching to a given target point. During the circle-drawing task, the participant is required to draw a circle (once clockwise and once counterclockwise), thus reflecting motor coordination. Each assessment program has a time limit of 60 s, and it is automatically terminated even if the task is not completed within that time. Each assessment program has three types of SB kinematic data that are referred to as SB parameters (Table 1).
Fig. 2.
The three different kinematic assessment programs of the Smart Board. The images show the tasks of a free exploration, b point-to-point reaching, and c circle-drawing. The round cursor indicates the movement of the forearm-supported controller
Table 1.
Descriptions of Smart Board evaluation tasks and parameters
| Task | Parameter | Description |
|---|---|---|
| Free exploration | Explored area ratio (%) | The ratio of (a) the area the participant covers to (b) the area required to be filled |
| Reaching distance (cm) | The mean reaching distance in all directions | |
| Completion time (s) | The time required to finish the test | |
| Point-to-point reaching | Target error (cm) | The linear deviation between (a) the target and (b) the point where the speed drops to below 5% of the maximum speed |
| Movement time (s) | The mean time to reach the target | |
| Smoothness | The normalized jerk by integrating the absolute jerk value over all routes | |
| Circle drawing | Shape closeness | The measure of closeness between (a) the target shape (circle) and (b) the shape drawn by the participant |
| Roundness | The measure of how closely the shape drawn by the participant approaches that of a mathematically perfect circle | |
| Completion time (s) | The time required to draw the circle |
Conventional intervention
The CON intervention focused on the restoration of AROM and coordination of the upper extremities such as AROM exercises for the affected upper extremity, a graded range of motion arc, figure-of-eight tracing using a hand skate, and cone stacking. The CON intervention differs with SB intervention in that this includes some activities embedding vertical plane motion requiring anti-gravity muscle activation instead of planar motion-based activities only. Functional exercise was not incorporated in the CON intervention. Trained occupational therapists modified the type and difficulty level of the intervention according to the participant’s current status. Feedback was provided verbally by the therapists, and physical assistance was provided according to the participant’s status. The SB intervention and CON intervention were conducted in a separate research room for only one participant at a time.
Outcome measures
We assessed baseline characteristics, including age, sex, dominant hand, stroke type, stroke duration, affected body side, MRC scale scores for the shoulder flexor/extensor and elbow flexor/extensor muscle strength, and upper extremity Fugl–Meyer Assessment (FMA-UE), which is a stroke-specific, performance-based motor impairment scale.
Primary outcome
The primary outcome was the change in the FMA-UE score; a higher score indicated lower motor impairment [18]. We used the following three FMA-UE subscales that were relevant to our intervention: FMA-total (33 items; score range, 0–66); FMA-proximal (shoulder, elbow, and forearm; 18 items; score range, 0–36); and FMA-coordination (five repetitions of the finger-to-nose test in rapid succession; three items; score range, 0–6).
Secondary outcomes
The secondary outcomes were changes in the Wolf motor function test (WMFT) score, shoulder AROM, Stroke Impact Scale (SIS) score, and modified Barthel index (MBI). The WMFT, which is a quantifiable measurement of upper extremity activity and participation with timed and functional tasks, consists of 17 items, including 15 functional tasks and 2 strength tasks [19]. We used the sum of the functional ability scale scores for items rated using a 6-point scale (WMFT-FAS; higher scores indicate better motor function) and the total amount of time for each item (WMFT-time; shorter time indicates better performance). The AROM of the shoulder joint, including flexion, abduction, adduction, internal rotation, and external rotation, was measured using a goniometer.
The SIS is a stroke-specificself-reported assessment tool for measuring HRQoL. We used the Korean version of the SIS (version 3.0), which contains eight domains scored using a five-point Likert scale (score range, 0–100); higher scores indicate better patient-perspective health status [20, 21]. The SIS was designed to assess multi-dimensional stroke outcomes, including strength, hand function, mobility, activities of daily living (ADLs)/instrumental activities of daily living (IADLs), memory and thinking, communication, emotion, and social participation. Additionally, there is an extra question about stroke recovery that asks participants to indicate how much they feel that they have recovered from stroke (score range, 0–100). The total SIS score was calculated and marked as the overall score. The MBI, which contains 10 items and has a score range from 0 to 100, was used to assess activity and participation [22].
Statistical analysis
The Mann–Whitney U test and Fisher’s exact test were used for baseline comparisons of continuous and categorical variables, respectively, of the study groups. The outcome measures were analyzed using two different approaches. First, within-group changes in the outcome measures were analyzed using the Wilcoxon signed rank test. Second, analyses of the main effects of group (SB and CON), time (T0, T1, and T2), and time × group interactions were conducted by a repeated measures analysis of covariance (ANCOVA) after setting the covariates as stroke duration and baseline FMA score, which affects recovery after stroke. The Greenhouse–Geisser procedure was applied when the sphericity assumption was violated. Statistical analyses of the intervention were performed using SPSS software (version 20.0; IBM Corp., Armonk, NY).
Correlations between repeatedly measured SB parameters and clinical scales, such as FMA-UE, WMFT, and shoulder AROM, were analyzed with repeated measures correlation (rmcorr) using R 3.5.1 (http://www.r-project.org) and R package rmcorr to determine the common linear relationship for paired repeated measures data [23]; p < 0.05 was considered statistically significant.
Results
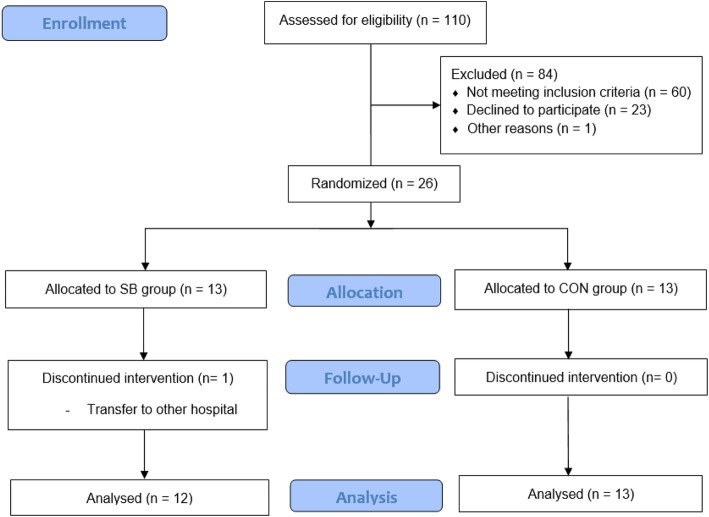
Of the 26 patients enrolled in the present study, 13 were allocated to the SB group and 13 were allocated to the CON group (Fig. 3). One patient was transferred to another hospital and dropped out of the SB group; therefore, this patient was excluded from the dataset. A total of 25 patients (12 in the SB group and 13 in the CON group) completed the 4-week intervention and were included in the final analysis. No adverse events were observed in either group during the study, which confirmed the safety of the SB intervention. There were no significant differences in baseline characteristics between the two groups (Table 2).
Fig. 3.
Study flowchart of participants
Table 2.
Demographic and clinical characteristics of the participants
| Characteristics | SB group (n = 12) | CON group (n = 13) | P-value |
|---|---|---|---|
| Demographic characteristics | |||
| Age, years | 53.5 ± 13.0 | 51.5 ± 16.7 | 0.397 a |
| Sex, male | 7 (53.8) | 8 (61.5) | 0.888 b |
| Dominant hand, right | 13 (100) | 10 (76.9) | 0.220 b |
| Stroke characteristics | |||
| Ischemia | 5 (38.5) | 8 (61.5) | 0.813 b |
| Time from stroke, days | 982.3 ± 1473.3 | 533.5 ± 635.3 | 0.331 a |
| Clinical characteristics | |||
| MRC scale shoulder flexor | 2.0 ± 0.0 | 2.2 ± 0.6 | 0.511 a |
| MRC scale shoulder extensor | 2.5 ± 0.5 | 2.6 ± 0.9 | 0.287 a |
| MRC scale elbow flexor | 1.8 ± 0.4 | 2.2 ± 0.8 | 0.920 a |
| MRC scale elbow extensor | 2.0 ± 0.7 | 2.2 ± 0.9 | 0.579 a |
| FMA-total score | 16.8 ± 7.3 | 19.9 ± 9.9 | 0.448 a |
Data are presented as mean ± standard deviation or number (%)
SB Smart Board intervention, CON Conventional intervention, MRC Medical Research Council, FMA Fugl–Meyer assessment
a Mann–Whitney U test, b Fisher’s exact test
Primary outcomes
Changes in the FMA-UE scores of the SB and CON groups are presented in Table 3. At the end of the intervention, both groups showed statistically significant improvements in the FMA-total and proximal scores at both T1 and T2, but not the FMA-coordination scores. Repeated measures ANCOVA showed no significant time × group interactions for all FMA-UE subscales. For stroke patients, the minimal clinical detectable change (MCID) was 9 or 10 for FMA-upper extremity [24, 25]. No FMA scores exceeded the MCID in both groups.
Table 3.
Changes in FMA, WMFT, AROM, and MBI scores and repeated measures ANCOVA outcomes
| SB group (n = 12) | CON group (n = 13) | RM ANCOVA | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T0 | T1 | Change (T1-T0) | p -value | T2 | Change (T2-T0) | p-value | T0 | T1 | Change (T1-T0) | p-value | T2 | Change (T2-T0) | p-value | F | p-value | |
| FMA-total | 17.1 ± 7.5 | 19.0 ± 7.5 | 1.9 ± 2.8 | 0.036 | 19.6 ± 7.5 | 2.5 ± 3.7 | 0.014 | 19.9 ± 9.9 | 22.0 ± 10.3 | 2.1 ± 2.7 | 0.018 | 25.50 ± 11.8 | 5.6 ± 8.6 | 0.012 | 0.971 | 0.387 |
| FMA-prox | 13.8 ± 3.7 | 14.9 ± 3.2 | 1.2 ± 1.8 | 0.041 | 15.0 ± 3.0 | 1.3 ± 2.1 | 0.041 | 16.9 ± 6.5 | 18.4 ± 6.6 | 1.5 ± 1.8 | 0.018 | 19.9 ± 7.1 | 3.0 ± 4.6 | 0.035 | 1.194 | 0.301 |
| FMA-dist | 2.3 ± 3.5 | 2.9 ± 3.6 | 0.6 ± 0.9 | 0.034 | 3.4 ± 3.7 | 1.1 ± 1.8 | 0.024 | 1.8 ± 2.8 | 2.2 ± 3.1 | 0.4 ± 0.9 | 0.102 | 4.0 ± 4.2 | 2.2 ± 3.6 | 0.018 | 0.787 | 0.462 |
| FMA-coor | 1.0 ± 1.8 | 1.3 ± 2.0 | 0.3 ± 0.9 | 0.180 | 1.3 ± 2.1 | 0.3 ± 0.9 | 0.180 | 1.4 ± 1.8 | 1.5 ± 1.9 | 0.1 ± 0.6 | 0.655 | 1.7 ± 1.9 | 0.3 ± 1.2 | 0.414 | 0.649 | 0.528 |
| WMFT-FAS | 15.0 ± 10.4 | 19.3 ± 11.1 | 4.3 ± 5.9 | 0.012 | 20.3 ± 11.0 | 5.3 ± 6.6 | 0.008 | 19.6 ± 14.0 | 24.4 ± 12.9 | 4.8 ± 5.9 | 0.003 | 29.7 ± 15.1 | 10.1 ± 10.1 | 0.001 | 1.451 | 0.246 |
| WMFT-time (log) | 3.1 ± 0.1 | 3.01 ± 0.1 | −0.1 ± 0.1 | 0.002 | 3.0 ± 0.1 | −0.1 ± 0.1 | 0.026 | 3.0 ± 0.2 | 3.0 ± 0.2 | −0.0 ± 0.1 | 0.016 | 2.9 ± 0.2 | −0.1 ± 0.1 | 0.023 | 0.425 | 0.577 |
| AROM-Sf | 68.8 ± 39.9 | 88.3 ± 45.7 | 19.6 ± 11.4 | 0.004 | 90.0 ± 44.5 | 21.3 ± 17.1 | 0.011 | 85.8 ± 45.4 | 95.8 ± 44.9 | 10.0 ± 10.8 | 0.016 | 107.3 ± 49.4 | 21.5 ± 27.9 | 0.011 | 0.928 | 0.373 |
| AROM-Sab | 60.8 ± 41.2 | 75.0 ± 43.8 | 14.2 ± 16.9 | 0.007 | 82.1 ± 53.8 | 21.3 ± 23.4 | 0.007 | 70.8 ± 42.3 | 77.3 ± 39.9 | 6.5 ± 8.0 | 0.026 | 80.0 ± 39.6 | 9.2 ± 14.4 | 0.041 | 1.516 | 0.231 |
| AROM-Sad | 29.2 ± 10.8 | 32.9 ± 11.8 | 3.8 ± 5.7 | 0.059 | 33.0 ± 11.8 | 10.4 ± 12.9 | 0.059 | 28.5 ± 14.6 | 32.3 ± 13.0 | 3.9 ± 6.5 | 0.059 | 33.9 ± 13.3 | 5.4 ± 6.6 | 0.020 | 0.198 | 0.722 |
| AROM-Sint | 35.5 ± 26.0 | 42.9 ± 22.2 | 10.4 ± 12.9 | 0.026 | 46.3 ± 19.2 | 13.8 ± 13.0 | 0.010 | 36.9 ± 25.2 | 41.9 ± 24.1 | 5.0 ± 10.4 | 0.109 | 42.7 ± 24.2 | 5.8 ± 11.2 | 0.109 | 2.221 | 0.137 |
| AROM-Sext | 30.0 ± 37.7 | 33.8 ± 36.4 | 3.8 ± 5.7 | 0.059 | 37.1 ± 34.3 | 7.1 ± 8.1 | 0.026 | 24.2 ± 29.9 | 30.4 ± 26.7 | 6.2 ± 10.4 | 0.066 | 36.2 ± 29.8 | 11.9 ± 14.1 | 0.026 | 0.335 | 0.717 |
| AROM-total | 221.3 ± 136.2 | 272.9 ± 134.8 | 51.7 ± 37.1 | 0.002 | 288.3 ± 138.9 | 67.1 ± 44.3 | 0.003 | 246.2 ± 136.8 | 277.7 ± 123.3 | 31.5 ± 30.4 | 0.005 | 294.4 ± 131.1 | 53.9 ± 56.5 | 0.003 | 0.729 | 0.454 |
| MBI | 69.8 ± 16.4 | 74.9 ± 16.8 | 5.1 ± 6.8 | 0.018 | 78.4 ± 13.2 | 8.6 ± 13.1 | 0.036 | 70.7 ± 17.9 | 76.5 ± 15.5 | 5.9 ± 7.4 | 0.018 | 78.9 ± 14.4 | 8.6 ± 10.2 | 0.005 | 0.101 | 0.848 |
Data are presented as mean ± standard deviation. The RM ANCOVA covariates were the time from stroke and FMA baseline data
ANCOVA Analysis of covariance, SB Smart Board intervention, CON Conventional intervention, FMA Fugl–Meyer assessment (FMA-total, FMA-proximal, FMA-distal, FMA-coordination), WMFT Wolf motor function test (WMFT-total, WMFT-functional ability scale, WMFT-time), WMFT-time presented as a log value, AROM Active range of motion (Sf Shoulder flexion, Sab Shoulder abduction, Sad Shoulder adduction, Sint Shoulder internal rotation, Sext Shoulder external rotation), MBI Modified Barthel index
Secondary outcomes
Table 3 presents the changes in secondary outcomes. The WMFT (WMFT-FAS and WMFT-time), MBI, and shoulder AROM of flexion and abduction significantly improved in both groups. Shoulder AROM of internal rotation significantly improved only in the SB group. Additionally, total shoulder AROM and shoulder AROM of flexion, abduction, and internal rotation showed similar or better improvements in the SB group than in the CON group at T1, and these findings continued at T2; however, there was no statistical significance. Repeated measures ANCOVA showed no significant time × group interactions for WMFT, MBI, and shoulder AROM. However, by applying the MCID as which 0.2 to 0.4 for WMFT-FAS, the changes in WMFT-FAS (T1-T0 and T2-T0) showed higher scores than the MCID in both SB and CON groups [26].
Regarding the SIS evaluation, one patient did not complete the assessment due to refusal to participate in the final SIS evaluation. Therefore, the SIS data analysis was performed for 24 patients (12 patients in each of the two groups). Table 4 summarizes the SIS data and their changes during the intervention for the SB and CON groups. The recovery and overall scores showed significant differences between T0 and T1 only in the SB group. The emotion and communication scores showed improvements in the SB group and deterioration in the CON group. Repeated measures ANCOVA showed statistically significant time × group interactions for memory and thinking and the overall SIS score, with larger differences observed in the SB group.
Table 4.
Changes in SIS scores in the SB and CON groups and repeated measures ANCOVA outcomes
| SB group (n = 12) | CON group (n = 12) | RM ANCOVA | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T0 | T1 | Change (T1-T0) | p-value | T2 | Change (T2-T0) | p-value | T0 | T1 | Change (T1-T0) | p-value | T2 | Change (T2-T0) | p-value | F | p-value | |
| Strength | 22.3 ± 14.0 | 29.4 ± 18.0 | 7.2 ± 10.0 | 0.034 | 27.3 ± 20.0 | 5.1 ± 12.2 | 0.153 | 19.7 ± 11.4 | 28.3 ± 13.1 | 8.58 ± 10.7 | 0.027 | 27.0 ± 14.3 | 7.3 ± 12.5 | 0.065 | 0.327 | 0.723 |
| Hand function | 0.8 ± 1.9 | 2.9 ± 5.8 | 2.1 ± 5.8 | 0.180 | 2.9 ± 6.2 | 2.1 ± 6.6 | 0.285 | 5.4 ± 8.6 | 6.3 ± 12.1 | 0.8 ± 8.5 | 0.891 | 8.3 ± 13.7 | 2.9 ± 12.1 | 0.357 | 0.086 | 0.858 |
| Mobility | 50.7 ± 26.0 | 53.6 ± 20.0 | 2.9 ± 15.9 | 0.386 | 58.5 ± 18.1 | 7.8 ± 16.5 | 0.103 | 69.9 ± 28.9 | 68.0 ± 30.3 | − 1.9 ± 7.9 | 0.675 | 73.7 ± 29.1 | 3.8 ± 7.0 | 0.046 | 1.844 | 0.171 |
| ADLs/IADLs | 59.2 ± 15.6 | 61.7 ± 14.7 | 2.5 ± 13.6 | 0.789 | 62.9 ± 12.6 | 3.8 ± 12.5 | 0.307 | 64.5 ± 15.5 | 62.5 ± 15.1 | − 2.0 ± 6.1 | 0.259 | 70.8 ± 16.3 | 2.5 ± 6.1 | 0.085 | 0.667 | 0.519 |
| Memory and thinking | 70.2 ± 20.8 | 80.1 ± 15.4 | 9.9 ± 16.1 | 0.052 | 76.7 ± 16.9 | 6.5 ± 16.9 | 0.258 | 86.3 ± 10.0 | 85.5 ± 13.5 | − 0.8 ± 7.3 | 0.865 | 88.8 ± 11.2 | 6.3 ± 10.1 | 0.172 | 4.484 | 0.017 |
| Communication | 83.8 ± 20.1 | 90.4 ± 16.8 | 6.6 ± 18.8 | 0.123 | 89.9 ± 19.1 | 6.1 ± 18.9 | 0.123 | 95.2 ± 5.5 | 90.7 ± 10.4 | −4.5 ± 6.2 | 0.034 | 92.8 ± 9.5 | −2.3 ± 5.4 | 0.167 | 4.009 | 0.051 |
| Emotion | 65.1 ± 17.9 | 70.8 ± 15.1 | 5.7 ± 15.5 | 0.182 | 70.8 ± 18.6 | 5.7 ± 12.5 | 0.212 | 80.5 ± 13.7 | 79.0 ± 15.8 | −1.5 ± 5.5 | 0.475 | 80.1 ± 15.3 | − 0.4 ± 8.9 | 0.959 | 1.901 | 0.163 |
| Social participation | 36.2 ± 20.6 | 42.8 ± 23.2 | 6.6 ± 10.1 | 0.050 | 41.3 ± 22.5 | 5.2 ± 9.9 | 0.096 | 39.3 ± 12.3 | 41.5 ± 15.7 | 2.2 ± 14.5 | 0.574 | 41.7 ± 11.1 | 2.3 ± 9.5 | 0.444 | 0.144 | 0.867 |
| Recovery | 31.7 ± 13.5 | 43.3 ± 13.9 | 11.7 ± 13.2 | 0.004 | 45.0 ± 13.7 | 13.3 ± 13.9 | 0.004 | 47.5 ± 17.1 | 49.6 ± 15.3 | 2.1 ± 8.1 | 0.493 | 57.5 ± 17.0 | 10.0 ± 10.2 | 0.011 | 2.673 | 0.081 |
| Overall | 388.2 ± 93.4 | 431.6 ± 58.4 | 43.4 ± 56.1 | 0.033 | 430.3 ± 70.8 | 42.2 ± 60.5 | 0.041 | 460.8 ± 72.0 | 461.7 ± 85.3 | 0.8 ± 24.3 | 0.824 | 483.3 ± 89.4 | 22.4 ± 30.2 | 0.018 | 3.559 | 0.038 |
Data are presented as mean ± standard deviation. The RM ANCOVA covariates were the time from stroke and FMA baseline data
SIS Stroke impact scale, ANCOVA Analysis of covariance, SB Smart Board intervention, CON Conventional intervention, ADLs/IADLs Activities of daily living/instrumental activities of daily living
SB assessment
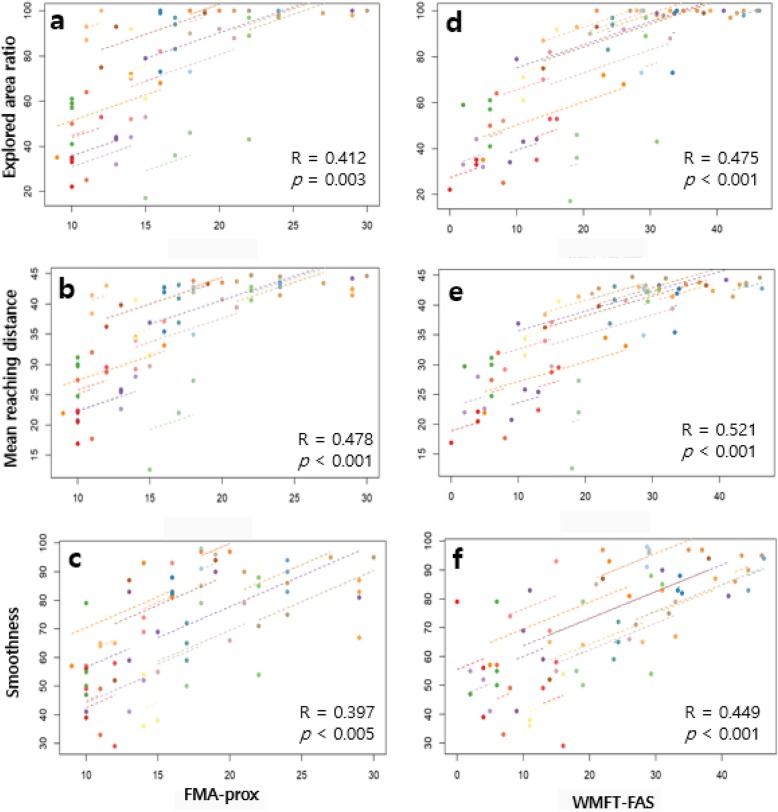
A repeated measures correlation analysis showed that changes in the three SB assessment aspects (explored area ratio [EAR], mean reaching distance [MRD], and smoothness [Sm]) were significantly correlated with changes in clinical scale scores such as FMA-total, FMA-prox, WMFT-FAS, WMFT-time, and shoulder AROM. In particular, AROM total score and MRD showed the highest correlation coefficients (R = 0.592; p < 0.001). Figure 4 demonstrates the FMA-prox and WMFT-FAS graphs that showed high correlation with the three aforementioned parameters (EAR, MRD, and Sm). However, parameters such as target error (TE) and roundness (Ro) showed no significant correlation with any clinical parameters we examined. Generally, the SB parameters showed higher correlation coefficients with WMFT scales than with FMA scales. The FMA-coordination scale was not correlated with any SB parameter (Table 5).
Fig. 4.
Repeated correlation graphs. Correlations between repeatedly measured clinical scales (a-c FMA-prox; d-f WMFT-FAS) and Smart Board parameters (a and d explored area ratio; b and e mean reaching distance; c and f smoothness) were analyzed by repeated measures correlation (rmcorr). R indicates the correlation coefficient. FMA, Fugl–Meyer assessment; WMFT, Wolf motor function test
Table 5.
Correlation analysis of SB parameters and clinical scales
| Task | Free exploration | Point-to-point reaching | Circle drawing | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Parameter | EAR | MRD | ECT | TE | MT | Sm | SC | Ro | CCT |
| FMA-total | 0.360* | 0.414** | −0.210 | − 0.063 | − 0.112 | 0.342* | 0.185 | 0.089 | −0.232 |
| FMA-prox | 0.412** | 0.478** | −0.146 | −0.069 | − 0.152 | 0.397** | 0.228 | 0.107 | −0.240 |
| FMA-dist | 0.311* | 0.348* | −0.267 | −0.055 | − 0.060 | 0.267 | 0.109 | 0.036 | −0.223 |
| FMA-coor | 0.172 | 0.138 | −0.134 | −0.006 | − 0.028 | 0.069 | 0.120 | 0.019 | −0.083 |
| WMFT-FAS | 0.475** | 0.521** | −0.297* | −0.245 | − 0.228 | 0.449** | 0.219 | 0.045 | −0.287* |
| WMFT-time | −0.400** | −0.441** | 0.139 | 0.277 | 0.363* | −0.344* | −0.261 | − 0.041 | 0.303* |
| AROM-Sf | 0.577** | 0.635** | −0.240 | −0.203 | − 0.252 | 0.424** | 0.376** | −0.009 | − 0.084 |
| AROM-Se | −0.081 | − 0.025 | −0.133 | − 0.226 | −0.223 | 0.045 | 0.090 | −0.046 | 0.109 |
| AROM-Sab | 0.337* | 0.389** | −0.380** | −0.052 | − 0.157 | 0.213 | 0.261 | −0.009 | − 0.183 |
| AROM-Sad | 0.465** | 0.470** | < −0.001 | −0.041 | − 0.395** | 0.378** | 0.270 | 0.007 | 0.001 |
| AROM-Sint | 0.505** | 0.503** | −0.199 | −0.015 | − 0.441** | 0.324* | 0.238 | 0.063 | − 0.309* |
| AROM-Sext | 0.441** | 0.497** | −0.299* | −0.173 | − 0.050 | 0.072 | 0.141 | 0.098 | −0.178 |
| AROM-total | 0.529** | 0.592** | −0.337* | −0.186 | − 0.344* | 0.364* | 0.353* | 0.009 | −0.155 |
EAR Explored area ratio (%), MRD Mean reaching distance (cm), ECT Exploration completion time (s), TE Target error (cm), MT Movement time (s), Sm Smoothness, SC Shape closeness, Ro Roundness, CCT Circle completion time (s), FMA Fugl–Meyer assessment (FMA-total, FMA-proximal, FMA-distal, FMA-coordination), WMFT Wolf motor function test (WMFT-total, WMFT-functional ability scale, WMFT-time), AROM Active range of motion (Sf Shoulder flexion, Sab Shoulder abduction, Sad Shoulder adduction, Sint Shoulder internal rotation, Sext Shoulder external rotation)
The number means correlation coefficient (R) and P-values are presented as *p < 0.05, **p < 0.01
Discussion
The SB, which is a newly developed VR-based planar exercise apparatus, was available for stroke rehabilitation in terms of clinical effectiveness. We found that the SB intervention with conventional OT improved upper extremity function, and that the effects on the SB group were not different from those on the CON group, without any adverse events. Notably, greater improvement was observed in shoulder AROM in the SB group than in the CON group, although there was a lack of statistical significance. This was meaningful because upper limb AROM is closely related to upper extremity function among stroke survivors, and shoulder AROM was found to explain 65% of the variance in upper extremity function [27, 28]. The largest difference between the SB and CON groups was noted for shoulder abduction, which is known to be closely related to upper limb functional recovery [29].
The beneficial effects of the SB on AROM might be associated with the hardware characteristics of the SB. Although AROM exercises have been emphasized for stroke rehabilitation, they have not been performed sufficiently because they are difficult to perform alone and the absolute amount of rehabilitation is limited. The SB attempted to overcome these limitations by using easily movable non-motorized equipment in combination with VR. Specifically, the SB was designed to be non-motorized but free from friction so that it would be suitable for repetitive movement without assisted force. Moreover, simple two-dimensional exercise could be intensively practiced using visual cues on the monitor during training. This planar movement training might be appropriate during the preliminary phase of recovery, when motor performance is not sufficient for complex movement training.
Regarding the SIS, the SB with conventional OT showed better results for improving the overall score of HRQoL when compared with the same amount of conventional OT, and it showed positive effects for many domains of the SIS. A recent Cochrane review could not conclude the role of VR with regard to quality of life because of the lack of studies [2]. However, similar to the findings of our previous studies, the present findings support the beneficial effects of VR on HRQoL after stroke rehabilitation [15, 30]. Interestingly, there was a marked difference between SIS-emotion scores of the two study groups, thus reflecting the strength of the gaming properties of the SB. Similarly, a previous study showed that VR with serious games significantly increased the Beck Depression Inventory score [31]. These emotional changes might occur gradually with positive experience, because gaming properties, including immediate and concrete feedback, reappraisal, challenging tasks, and optimal difficulty levels, can provide an enjoyable feeling and a feeling of achievement, which help motivate active participation in the rehabilitation process, thereby leading to better functional outcomes [30, 32–34]. A recent review demonstrated that VR and active video gaming have positive effects on a patient’s motivation and enjoyment [35].
The SB group showed relatively notable improvements in the SIS-ADLs/IADLs domain, despite limited differences in the MBI when compared with the findings of the CON group. Therefore, positive emotional improvements might have contributed to improved subjective perception of ADLs because the SIS reflects the perceived ability of ADLs, whereas the MBI reflects the real ability.
In addition to therapeutic effects, the SB allows for a simple, easily applicable, objective, and quantitative assessment of motor performance. VR has not been commonly used for assessments, although it is popular in the therapy field. Similarly, correlations between VR-based measurements and clinical scales for assessing upper extremity function have not been sufficiently explored. The SB as a new VR-based assessment tool could be used to evaluate upper limb function with simultaneous recordings of kinematic data using an SB-embedded sensor without the need to attach additional sensors to the participant during a short period of 3 min.
The SB parameters significantly matched the clinical scales for upper limb function and their changes. Among the nine SB parameters used, three (EAR, MRD, Sm) were moderately correlated with the FMA and WMFT, suggesting that evaluation with the SB allows for estimation of the upper extremity function across impairment and activity domains. Therefore, the SB assessment might help provide precise and reliable feedback to participants. Fundamentally, evaluation using the SB has the advantage of providing objective measurements of movement performance that could complement conventional clinical assessments.
The SB allows more immediate and frequent feedback to therapists and participants, potentially allowing more individualized rehabilitation. Although the correlation coefficients were not high enough to consider replacing clinically established scales, we obtained moderate correlations that were comparable with robotic measurements, which are more costly than our measurements [36]. Further combinations of multiple metrics could lead to a higher estimation of competence of the SB [37].
SB parameters are activity-relevant and specific. The correlation coefficients for the SB parameters (EAR, MRD, and Sm) and the WMFT were higher than the coefficients for the parameters and the FMA, indicating that the SB parameters reflect activity and participation more than impairment. Correlations with shoulder AROM were greater during the free exploration task than during the other two tasks (point-to-point reaching and circle-drawing tasks) because of the similarity between free exploration and AROM.
In contrast to the positive results of these SB parameters, the time-relevant factors of free exploration and point-to-point reaching (completion time and movement time) showed only limited significant correlations with clinical scales. This might be associated with the floor effects of those parameters because most of the participants did not finish the free exploration and point-to-point reaching tasks within 1 min; therefore, the movement time was nearly the same among the participants. In contrast, the time variables of the circle-drawing task, which most participants could finish within 1 min, showed significant correlations with the WMFT. Therefore, it is necessary to modify the approaches by adjusting the difficulty or altering the calculation method to increase diagnostic validity.
The SB originally targeted both AROM exercises and coordination at the development stage; however, the SB intervention failed to achieve significant improvements in coordination. There is still a lack of evidence indicating that coordination could be improved with rehabilitation, and most improvements occur during the acute phase of stroke because of spontaneous recovery rather than during the chronic phase [38, 39]. Similarly, the SB intervention was incapable of accomplishing notable voluntary control ability associated with coordination. Moreover, we did not find any significant coordination-correlated SB parameters because FMA-coordination, which includes only three items (tremor, dysmetria, and speed), might not be sufficient to reflect coordination compared to more specific outcome measures such as inter-joint movement analysis or sub-movement analysis [40, 41].
The present study had several limitations. First, our results should be carefully interpreted because both the SB and CON groups received 30 min of OT in addition to the primary intervention. Therefore, the effects could not be solely attributed to either intervention. Second, the sample size was small and the number of participants was not calculated with a power analysis because the present study was a preliminary study performed to assess availability, thus limiting the ability to draw a definite conclusion. Therefore, a future study with more participants for comparison of a single intervention is needed. Finally, the SB kinematic data have not been evaluated for their reliability even though the infrared sensor is able to present accurate measurements. Therefore, a reliability test might be needed to utilize the SB kinematic data as a more reliable outcome measurement.
Conclusion
VR-based rehabilitation incorporating planar motion exercises is available as an intervention and assessment tool for stroke patients. It could be a user-friendly rehabilitation approach for not only upper extremity function and AROM but also HRQoL. Additionally, easily applicable assessments, which are moderately correlated with clinical scales and associated with a short time period, could broaden and support the role of VR in rehabilitation.
Acknowledgements
This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI) funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI15C1529). This research was supported by the MSIT (Ministry of Science and ICT), Korea, under the ITRC (Information Technology Research Center) support program (IITP-2019-2015-0-00363) supervised by the IITP (Institute for Information & Communications Technology Planning & Evaluation).
Abbreviations
- ADLs/IADLs
Activities of daily living/instrumental activities of daily living
- ANCOVA
Analysis of covariance
- AROM
Active range of motion
- CON
Control
- FMA
Fugl–Meyer assessment
- HRQoL
Health-related quality of life
- MAS
Modified Ashworth Scale
- MBI
Modified Barthel index
- MRC
Medical Research Council scale
- OT
Occupational therapy
- rmcorr
Repeated measures correlation
- SB group
SB intervention group
- SB
Rapael Smart Board™
- SIS
Stroke Impact Scale
- WMFT
Wolf motor function test
Authors’ contributions
MP conducted the data analysis and interpretation and wrote and edited the manuscript. MHK contributed to the study design and data collection. SWO contributed to data analysis and interpretation. HY, YC, and DH contributed to device develop and wrote the device description. JYL and YH performed the research and data collection. JHS contributed to the study design, prepared the research protocol, interpreted the data, and wrote and edited the manuscript. All authors have read and approved the final manuscript.
Funding
This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI) funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI15C1529).
Availability of data and materials
The dataset used in the present study is available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The study was registered at CRIS (KCT0003783) and followed the requirements of the Declaration of Helsinki. The study protocol was approved by the Ethics Committee of the National Rehabilitation Center in South Korea (NRC-2017-01-003) and Chonbuk National University Hospital (2017–03-009). All participants provided written informed consent prior to enrollment in this study.
Consent for publication
Not applicable.
Competing interests
Hyoseok Yi, Younggeun Choi, and Dokyeong Ha hold equity in and work for Neofect Inc. Joon-Ho Shin’s family member holds equity in Neofect Inc. Neofect Inc. has a direct financial interest in the results of this study. Although the Smart Board from Neofect Inc. was used in the present study, Neofect Inc. was not involved in the study conception, data collection, data analysis, or result reporting.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mina Park, Email: mmaabb@naver.com.
Myoung-Hwan Ko, Email: mhko@jbnu.ac.kr.
Sang-Wook Oh, Email: sangwook05@hanmail.net.
Ji-Yeong Lee, Email: wldud3575@hanmail.net.
Yeajin Ham, Email: aqualla@naver.com.
Hyoseok Yi, Email: hyoseok@neofect.com.
Younggeun Choi, Email: younggch@gmail.com.
Dokyeong Ha, Email: dokyeong.ha@neofect.com.
Joon-Ho Shin, Phone: +82-2-901-1884, Email: asfreelyas@gmail.com.
References
- 1.Hatem SM, Saussez G, della Faille M, Prist V, Zhang X, Dispa D, Bleyenheuft Y. Rehabilitation of motor function after stroke: a multiple systematic review focused on techniques to stimulate upper extremity recovery. Front Hum Neurosci. 2016;10:442. doi: 10.3389/fnhum.2016.00442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Laver KE, Lange B, George S, Deutsch JE, Saposnik G, Crotty M. Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev. 2017;11:CD008349. doi: 10.1002/14651858.CD008349.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sveistrup H, McComas J, Thornton M, Marshall S, Finestone H, McCormick A, Babulic K, Mayhew A. Experimental studies of virtual reality-delivered compared to conventional exercise programs for rehabilitation. Cyberpsychol Behav. 2003;6(3):245–249. doi: 10.1089/109493103322011524. [DOI] [PubMed] [Google Scholar]
- 4.Burdea GC. Virtual rehabilitation–benefits and challenges. Methods Inf Med. 2003;42(05):519–523. doi: 10.1055/s-0038-1634378. [DOI] [PubMed] [Google Scholar]
- 5.Levin MF, Weiss PL, Keshner EA. Emergence of virtual reality as a tool for upper limb rehabilitation: incorporation of motor control and motor learning principles. Phys Ther. 2015;95(3):415–425. doi: 10.2522/ptj.20130579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prange GB, Kottink AI, Buurke JH, Eckhardt MM, van Keulen-Rouweler BJ, Ribbers GM, Rietman JS. The effect of arm support combined with rehabilitation games on upper-extremity function in subacute stroke: a randomized controlled trial. Neurorehabil Neural Repair. 2015;29(2):174–182. doi: 10.1177/1545968314535985. [DOI] [PubMed] [Google Scholar]
- 7.Kleim JA, Jones TA. Principles of experience-dependent neural plasticity: implications for rehabilitation after brain damage. J Speech Lang Hear Res. 2008;51(1):S225–S239. doi: 10.1044/1092-4388(2008/018). [DOI] [PubMed] [Google Scholar]
- 8.Mirelman A, Bonato P, Deutsch JE. Effects of training with a robot-virtual reality system compared with a robot alone on the gait of individuals after stroke. Stroke. 2009;40(1):169–174. doi: 10.1161/STROKEAHA.108.516328. [DOI] [PubMed] [Google Scholar]
- 9.Lee SH, Lee J-Y, Kim M-Y, Jeon Y-J, Kim S, Shin J-H. Virtual reality rehabilitation with functional electrical stimulation improves upper extremity function in patients with chronic stroke: a pilot randomized controlled study. Arch Phys Med Rehabil. 2018;99(8):1447–1453.e1. doi: 10.1016/j.apmr.2018.01.030. [DOI] [PubMed] [Google Scholar]
- 10.Blank AA, French JA, Pehlivan AU, O’Malley MK. Current trends in robot-assisted upper-limb stroke rehabilitation: promoting patient engagement in therapy. Curr Phys Med Rehabil Rep. 2014;2(3):184–195. doi: 10.1007/s40141-014-0056-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saposnik G, Teasell R, Mamdani M, Hall J, McIlroy W, Cheung D, Thorpe KE, Cohen LG, Bayley M. Effectiveness of virtual reality using Wii gaming technology in stroke rehabilitation: a pilot randomized clinical trial and proof of principle. Stroke. 2010;41(7):1477–1484. doi: 10.1161/STROKEAHA.110.584979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Subramanian SK, Lourenço CB, Chilingaryan G, Sveistrup H, Levin MF. Arm motor recovery using a virtual reality intervention in chronic stroke: randomized control trial. Neurorehabil Neural Repair. 2013;27(1):13–23. doi: 10.1177/1545968312449695. [DOI] [PubMed] [Google Scholar]
- 13.Maciejasz P, Eschweiler J, Gerlach-Hahn K, Jansen-Troy A, Leonhardt S. A survey on robotic devices for upper limb rehabilitation. J Neuroeng Rehabil. 2014;11(1):3. doi: 10.1186/1743-0003-11-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krebs HI, Ferraro M, Buerger SP, Newbery MJ, Makiyama A, Sandmann M, Lynch D, Volpe BT, Hogan N. Rehabilitation robotics: pilot trial of a spatial extension for MIT-Manus. J Neuroeng Rehabil. 2004;1(1):5. doi: 10.1186/1743-0003-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shin J-H, Kim M-Y, Lee J-Y, Jeon Y-J, Kim S, Lee S, Seo B, Choi Y. Effects of virtual reality-based rehabilitation on distal upper extremity function and health-related quality of life: a single-blinded, randomized controlled trial. J Neuroeng Rehabil. 2016;13(1):17. doi: 10.1186/s12984-016-0125-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Piron L, Cennis F, Tonins P, Dam M. Virtual Reality as an assessment tool. Medicine Meets Virtual Reality 2001. 2001;81:386. [PubMed]
- 17.Choi Y, Gordon J, Park H, Schweighofer N. Feasibility of the adaptive and automatic presentation of tasks (ADAPT) system for rehabilitation of upper extremity function post-stroke. J Neuroeng Rehabil. 2011;8(1):42. doi: 10.1186/1743-0003-8-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fugl-Meyer AR, Jääskö L, Leyman I, Olsson S, Steglind S. The post-stroke hemiplegic patient. 1. A method for evaluation of physical performance. Scand J Rehabil Med. 1975;7(1):13–31. [PubMed] [Google Scholar]
- 19.Morris DM, Uswatte G, Crago JE, Cook EW, III, Taub E. The reliability of the wolf motor function test for assessing upper extremity function after stroke. Arch Phys Med Rehabil. 2001;82(6):750–755. doi: 10.1053/apmr.2001.23183. [DOI] [PubMed] [Google Scholar]
- 20.Duncan PW, Bode RK, Lai SM, Perera S, Investigators GAiNA Rasch analysis of a new stroke-specific outcome scale: the stroke impact scale1. Arch Phys Med Rehabil. 2003;84(7):950–963. doi: 10.1016/S0003-9993(03)00035-2. [DOI] [PubMed] [Google Scholar]
- 21.Choi SU, Lee HS, Shin JH, Ho SH, Koo MJ, Park KH, Yoon JA, Kim DM, Oh JE, Yu SH. Stroke impact scale 3.0: reliability and validity evaluation of the Korean version. Ann Rehabil Med. 2017;41(3):387–393. doi: 10.5535/arm.2017.41.3.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel index for stroke rehabilitation. J Clin Epidemiol. 1989;42(8):703–709. doi: 10.1016/0895-4356(89)90065-6. [DOI] [PubMed] [Google Scholar]
- 23.Bakdash JZ, Marusich LR. Repeated measures correlation. Front Psychol. 2017;8:456. doi: 10.3389/fpsyg.2017.00456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Narayan Arya K, Verma R, Garg R. Estimating the minimal clinically important difference of an upper extremity recovery measure in subacute stroke patients. Top Stroke Rehabil. 2011;18(sup1):599–610. doi: 10.1310/tsr18s01-599. [DOI] [PubMed] [Google Scholar]
- 25.Pandian S, Arya KN. Stroke-related motor outcome measures: do they quantify the neurophysiological aspects of upper extremity recovery? J Bodyw Mov Ther. 2014;18(3):412–423. doi: 10.1016/j.jbmt.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 26.Lin KC, Hsieh YW, Wu CY, Chen CL, Jang Y, Liu JS. Minimal detectable change and clinically important difference of the Wolf Motor function test in stroke patients. Neurorehabil Neural Repair. 2009;23(5):429–434. doi: 10.1177/1545968308331144. [DOI] [PubMed] [Google Scholar]
- 27.Beebe JA, Lang CE. Active range of motion predicts upper extremity function 3 months after stroke. Stroke. 2009;40(5):1772–1779. doi: 10.1161/STROKEAHA.108.536763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lang CE, Beebe JA. Relating movement control at 9 upper extremity segments to loss of hand function in people with chronic hemiparesis. Neurorehabil Neural Repair. 2007;21(3):279–291. doi: 10.1177/1545968306296964. [DOI] [PubMed] [Google Scholar]
- 29.Nijland RH, van Wegen EE, Harmeling-van der Wel BC, Kwakkel G. Presence of finger extension and shoulder abduction within 72 hours after stroke predicts functional recovery: early prediction of functional outcome after stroke: the EPOS cohort study. Stroke. 2010;41(4):745–750. doi: 10.1161/STROKEAHA.109.572065. [DOI] [PubMed] [Google Scholar]
- 30.Shin J-H, Park SB, Jang SH. Effects of game-based virtual reality on health-related quality of life in chronic stroke patients: a randomized, controlled study. Comput Biol Med. 2015;63:92–98. doi: 10.1016/j.compbiomed.2015.03.011. [DOI] [PubMed] [Google Scholar]
- 31.Song GB, Park EC. Effect of virtual reality games on stroke patients’ balance, gait, depression, and interpersonal relationships. J Phys Ther Sci. 2015;27(7):2057–2060. doi: 10.1589/jpts.27.2057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Burke J, McNeill M, Charles D, Morrow P, Crosbie J, McDonough S. Proceedings of the 8th international conference on disability, virtual reality & associated technologies. 2010. Designing engaging, playable games for rehabilitation; pp. 195–201. [Google Scholar]
- 33.Burke JW, McNeill M, Charles DK, Morrow PJ, Crosbie JH, McDonough SM. Optimising engagement for stroke rehabilitation using serious games. Vis Comput. 2009;25(12):1085. doi: 10.1007/s00371-009-0387-4. [DOI] [Google Scholar]
- 34.Ma M, Bechkoum K. Serious games for movement therapy after stroke. In: 2008 IEEE international conference on systems, man and cybernetics, 2008 SMC. Singapore: IEEE; 2008. p. 1872–7.
- 35.Rohrbach N, Chicklis E, Levac DE. What is the impact of user affect on motor learning in virtual environments after stroke? A scoping review. J Neuroeng Rehabil. 2019;16(1):79. doi: 10.1186/s12984-019-0546-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Do Tran V, Dario P, Mazzoleni S. Kinematic measures for upper limb robot-assisted therapy following stroke and correlations with clinical outcome measures: a review. Med Eng Phys. 2018;53:13–31. doi: 10.1016/j.medengphy.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 37.Bosecker C, Dipietro L, Volpe B, Igo Krebs H. Kinematic robot-based evaluation scales and clinical counterparts to measure upper limb motor performance in patients with chronic stroke. Neurorehabil Neural Repair. 2010;24(1):62–69. doi: 10.1177/1545968309343214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jarrassé N, Proietti T, Crocher V, Robertson J, Sahbani A, Morel G, Roby-Brami A. Robotic exoskeletons: a perspective for the rehabilitation of arm coordination in stroke patients. Front Hum Neurosci. 2014;8:947. doi: 10.3389/fnhum.2014.00947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.van Kordelaar J, van Wegen EE, Nijland RH, Daffertshofer A, Kwakkel G. Understanding adaptive motor control of the paretic upper limb early poststroke: the EXPLICIT-stroke program. Neurorehabil Neural Repair. 2013;27(9):854–863. doi: 10.1177/1545968313496327. [DOI] [PubMed] [Google Scholar]
- 40.Cirstea M, Mitnitski A, Feldman A, Levin M. Interjoint coordination dynamics during reaching in stroke. Exp Brain Res. 2003;151(3):289–300. doi: 10.1007/s00221-003-1438-0. [DOI] [PubMed] [Google Scholar]
- 41.Dipietro L, Krebs HI, Fasoli SE, Volpe BT, Stein J, Bever CT, Hogan N. Changing motor synergies in chronic stroke. J Neurophysiol. 2007;98(2):757–768. doi: 10.1152/jn.01295.2006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset used in the present study is available from the corresponding author on reasonable request.