Abstract
Women Veterans who experience homelessness are at high risk of unintended pregnancy and adverse outcomes. Contraception could mitigate risks, yet access barriers exist across the Veterans Health Administration (VHA). We identified all US women Veterans, age 18–44y with evidence of homelessness in VHA administrative data between fiscal years 2002–2015, in order to document the geographic distribution of ever-homeless women Veterans in relation to VA Medical Centers (VAMCs) and assess geographic associations between long acting reversible contraceptives (LARC) or permanent contraception (PC) use. We calculated VAMC travel distance from last known ZIP Code. We used multivariate logistic regression models to explore contraceptive method associations. We included 41,722 ever-homeless women Veterans; 9.2% had LARC exposure and 7.5% PC. We found 29% of ever-homeless women Veterans resided >40miles from the nearest VAMC and increasing drive distance was negatively correlated with contraceptive exposure, especially for Veterans residing >100miles from a VAMC. Increasing distance to the nearest VAMC results in a geographic barrier to the most effective contraceptive options for women Veterans. The VHA is uniquely positioned to leverage its rural and homeless healthcare expertise to address geographic barriers and integrate comprehensive contraceptive services into established programs for high-risk Veterans.
Keywords: Homelessness, Veterans, reproductive health, travel distance, contraception
Introduction
Women Veterans are the fastest growing population of Veterans Health Administration (VHA) eligible users, nearly doubling in the past decade and numbering more than 2 million in fiscal year 2015.1,2 Of women who use the VHA, 43% are of reproductive age (18–44 years)1 and meeting their comprehensive reproductive healthcare needs is a high priority. Despite this prioritization, 42% of women Veterans belong to a racial or ethnic minority and an increasing number reside in a rural area; characteristics associated with increased risk of reproductive health care disparities and access barriers.1,3–5 Additionally, VHA users have a high prevalence of medical and mental health comorbidities6, history of military sexual trauma (MST)6, and experience a 4-fold increased risk of homelessness compared to women without a military service history7. All of these characteristics increase the risks of adverse reproductive outcomes and need for pregnancy planning and preconception care. Women Veterans experiencing homelessness have increased access barriers to services and are less likely to have other insurance options to seek care from non-VHA providers, thus increasing reliance on VHA care. VHA reproductive services are critical for this high risk population, as homeless women are more likely to experience sexual trauma, unintended pregnancy, and adverse outcomes, such as preterm birth.8 Factors associated with homelessness in women Veterans, such as poor overall physical and mental health, are also associated with adverse pregnancy outcomes, which could be mitigated through contraceptive care.9
Contraception has an immense public health importance through prevention of unintended pregnancies, especially in the setting of high-risk health or socioeconomic conditions. Comprehensive contraceptive options include both long acting reversible contraceptives (LARC), such as intrauterine devices (IUDs) and contraceptive implants, and permanent sterilization. LARC and sterilization are not only the most effective contraceptive options, but also the safest in women with many health conditions, such as cardiac conditions or autoimmune diseases.10,11 Unfortunately, contraceptive method provision barriers exist in the VHA due to provider experience and clinic type or location.12,13 Currently, comprehensive Women’s Clinics with experienced women’s health providers are primarily in high-volume, relatively urban VA Medical Centers (VAMCs), presenting access barriers to those with housing instability and increased logistical challenges.14 VHA access barriers are experienced by many women Veterans and include distance to the nearest VHA facility, especially for those in rural settings, and increasing disability.15 Even if a VHA women’s health provider is located in a more accessible community-based outpatient clinic (CBOC), not all are trained to offer LARC methods and refer Veterans to VAMCs where gynecologists are located.16 Veterans in rural areas are often referred to local non-VHA surgeons who may only provide sterilization or hysterectomy and not offer LARC as an alternative, resulting in a geographic disparity of care options.17 Women Veterans are more likely to have a hysterectomy at a younger age than civilians and although LARC exposure is higher in ever-homeless women Veterans than in housed, disparities in subpopulations persist.6,17
Addressing the barriers experienced by homeless women Veterans in accessing contraception can decrease risk of unintended pregnancy and subsequent adverse pregnancy outcomes.18 Understanding geographic variation in contraceptive services could also lead to targeted provider education or service expansion in underserved locations with high-risk women Veteran populations. Thus, we leveraged VHA administrative data and geospatial informatics methods to document the geographic distribution of ever-homeless women Veterans in relation to VAMCs and assess whether geographic barriers were associated with variation in exposure to long acting or permanent contraceptive methods.
Materials and Methods
Study Ethics.
This study received approval from the University of Utah Institutional Review Board and the Research and Development Committee at the Veterans Administration Salt Lake City Health Care System.
Participants.
We identified all women Veterans (regardless of their combat era) with administrative evidence of homelessness at any time (“ever-homeless”) who accessed the VHA between fiscal years (FY) 2002–2015 using a national VHA research database of administrative and clinical data managed by the Veteran’s Informatics and Computing Infrastructure (VINCI).19 Homelessness was identified through previously validated classification system, which included International Classification of Diseases, Ninth Revision (ICD-9) codes, Homeless Care stop codes (which are administrative codes for specific clinic locations) for specialized VHA homeless care programs such as Department of Housing and Urban Development VA Shared Housing, or treatment specialty codes (e.g. administrative codes for receipt of homeless services for hospitalized Veterans).20 We chose the study timeframe of federal fiscal years (FY) 2002 to 2015 based upon a previous cohort developed after validation of the homeless classification system.20,21 We included only women Veterans age 18–44y in birth cohorts for each FY and censored them in subsequent cohorts if they aged beyond inclusion criteria. We chose the age cutoff of 44 years to be in-line with the designation of “reproductive age Veterans” in other VA publications, which use the age categories of 18–44, 45–64, and 65+ years to identify Veteran characteristics, utilization and disparities.1 Finally, we utilized a previously established, matched cohort of 46,381 housed reproductive age women Veterans6 to explore whether the effect of geographic barriers on contraception use was unique to ever-homeless women Veterans or a barrier for all women Veterans, regardless of housing status.
Measures and Analyses.
Demographic variables included birth year, marital status, race, ethnicity, and religious affiliation, as these variables may impact contraceptive use.22–24 Military characteristics included Service branch, receipt of combat exposure pay (as a proxy for exposure for combat), and MST screening results (positive or negative). While MST status was not routinely screened for or reliably captured in structured data until 2004, Veterans who accessed care prior to 2004 were screened at follow-up encounters and those responses analyzed.25 We captured ICD-9 and Current Procedural Terminology (CPT®) codes for sterilization, hysterectomy, and IUD or implant insertion, surveillance, removal or exchange. We also extracted service dates and each woman Veteran’s age at the time of the procedure. We chose a dichotomous outcome for LARC as “exposure”, rather than limiting to “insertion”. This outcome captures any LARC use, even if a visit is for removal, as devices can be maintained for three to twelve years and Veterans may receive them during active duty or in other healthcare settings. The date of hysterectomy or sterilization was captured for any women with procedure documentation. We included hysterectomy in our analyses, as this procedure ends any future risk of unintended pregnancy, even though the surgical indication for a hysterectomy is not for sterilization alone. If a woman Veteran had more than one code for LARC, sterilization or hysterectomy, only the code associated with the first date of service was used to define method use. For example, a Veteran would be included in the sterilization cohort if she had a tubal sterilization prior to IUD placement for bleeding control.
We defined the ever-homeless women Veteran’s geographic “residence” as last known ZIP Code reported at the time of homelessness designation. For women with only post office box (PO Box) numbers, we assumed PO boxes were in close proximity to where they were staying and assigned the associated ZIP Code as their “residence”. The population density of homeless women Veterans per ZIP Code was plotted on a map of the U.S. using population-weighted ZIP Code centroid points along with geocoded VAMC locations. We represented ever-homeless women Veterans counts using proportional, graduated points such that relatively larger, darker points represented a larger count of as compared to less populated locations (represented with relatively smaller, lighter points). All mapping was completed using ESRI’s ArcMAP GIS software (version 10.4.1, Redlands, CA).
We performed all drive distance calculations using the nearest facility function (shortest distance) in the Network Analyst extension for ArcMAP software and used Veterans Integrated Service Network (VISN) boundaries in effect prior to a 2016 VISN boundary realignment. Veterans are typically assigned to the nearest VHA clinic site within their VISN, regardless of whether they may live geographically closer to another VHA site outside VISN boundaries. To compare travel burdens based upon VISN boundaries, we calculated a second closest facility measurement that ignored the VISN boundary restrictions. We also plotted all FY2015 reproductive age women Veterans using data from the National Center for Veterans Analysis and Statistics (obtained through the GIS vendor, ESRI) to define median travel distances to the nearest VAMC for comparison to our findings for ever-homeless women Veterans. Finally, to illustrate the effect of high mileage distances between home locations and VAMCs on ever-homeless women Veterans (who have additional logistics to travel compared to Veterans with more resources), we created nested driving distance bands from the VAMCs in VISN 19 and then plotted the approximate geographic “home” for those in this area. We chose VISN 19 (including the majority of Montana, Wyoming, Utah, and Colorado, with smaller swaths of Nevada, Idaho, Nebraska, and Kansas) due to the high proportion of rural and frontier land compared to other VISNs.
We explored differences in contraceptive exposure by VA region with boundaries defined prior to the 2016 changes, which were accessible in VINCI.19 (Figure 1) Finally, the census tract-based Rural-Urban Commuting Area Codes (RUCA) that were also adopted by the VA for rural designation26 were used to understand the effect of rurality on access to contraceptive methods. These codes were developed from the 2010 work commuting data from the U.S. Census Bureau and classify census tracts using measures of population density. We used the following VHA definitions in this analysis: urban, rural, and highly-rural.26,27
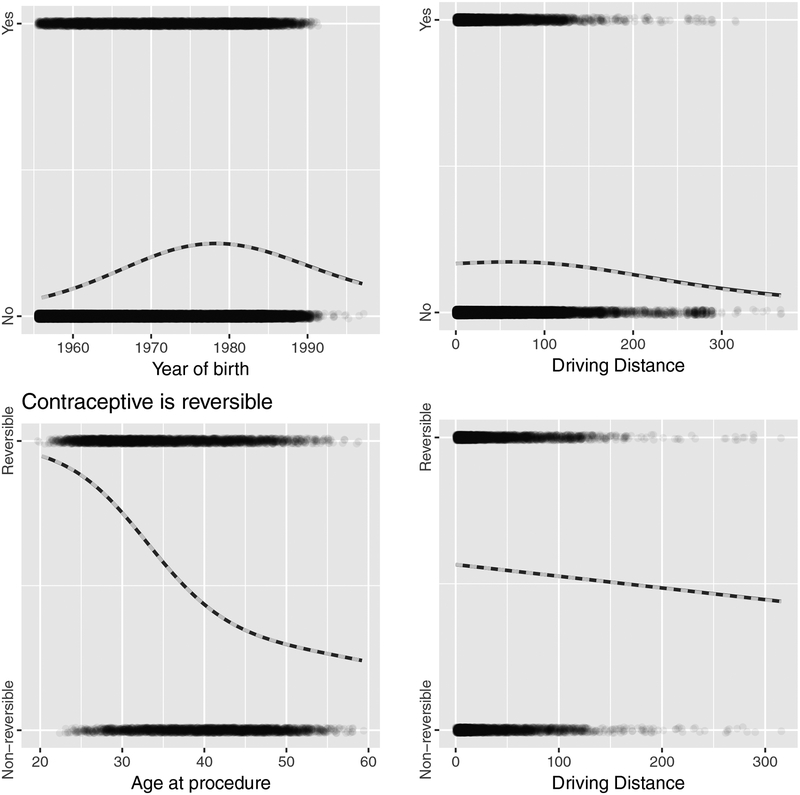
Figure 1:
Estimated effect curves for age and driving distance variables on use of any highly effective contraceptive and whether the method is reversible in homeless women Veterans who accessed the Veterans Health Administration between Fiscal Years 2002–2015
We calculated descriptive statistics for demographic, military and geographic characteristics on all reproductive age women with a homelessness designation in the study timeframe via Chi square analyses. For the models, we excluded women Veterans with the following characteristics: conflicting LARC billing codes, reported ZIP Codes not matched to US postal service records or outside of the contiguous US, and multiple entries for demographic or military characteristics. We utilized a multivariate logistic regression model to explore the associations between descriptive variables on contraceptive exposure. We fit four hierarchical models at progressing granularity levels for contraceptive exposure. The first modeled the likelihood of ever-homeless women Veterans to have any contraceptive exposure. The second distinguished those with LARC from those with permanent contraceptives. The final models separated those with IUDs from those with implants among those with LARC, and those with hysterectomies from those with tubal sterilizations among those with permanent methods.
We fit all models with the same set of variables with one exception: In the first model, we used year of birth for the age variable rather than age at procedure. We fit continuous age and driving distance variables with linear and quadratic terms to test curvature in the effect of said variables. Model analyses were performed in R Version 3.4.0.
Results
We identified a total of 41,722 women Veterans with a homelessness designation and VHA utilization between FY2002–2015. A total of 3,825 (9.2%) had documented LARC exposure and 3,126 (7.5%) had permanent contraception. Comparative statistics on the total cohort identified statistically significant (p<0.05) differences between those with and without contraceptive methods in all variables except religion. Trends that emerged included finding LARC method use more common in ever-homeless women Veterans who were single, white, served in the Navy, had combat exposure, and the shortest drive distances to a VAMC (<40mi). Permanent sterilization or hysterectomy appeared more common in the older age group, divorced/separated or widowed relationship status, black, served in the Army, and reported a history of MST. (Table 1)
Table 1:
Characteristics associated with long-acting reversible (LARC) and permanent contraception use in ever-homeless women Veterans who accessed care in the Veterans Health Administration between Fiscal Years 2002–2015
| Variable N=41722 |
LARC n=3825 (100%) |
Permanent n=3126 (100%) |
None n=34771 (100%) |
|---|---|---|---|
| Year of Birth | |||
| Marital Status | |||
| Race | |||
| Ethnicity | |||
| Religion | |||
| Military Branch of Service | |||
| Combat Experience | |||
| Military Sexual Trauma History1 | |||
| Drive distance to nearest VAMC2 | |||
| Rurality Designation3 | |||
| VA Region4 |
VAMC= Veterans Association Medical Center;
Indicated data excluded from multivariate logistic regression models
Data from Veterans Association Military Sexual Trauma screen responses
Calculated in miles by last ZIP Code reported at the time of homelessness designation to the nearest VAMC
Based upon Rural-Urban Commuting Area codes
Based upon VA Regions prior to 2016 boundary changes
Following application of exclusion criteria, we included 39,684 ever-homeless women Veterans in multivariate logistic regression models. Compared to single women, married women and those divorced/separated or widowed are more likely to have any contraceptive method, including both LARC (married aOR 1.44; 95%CI 1.33–1.55) and permanent sterilization. Race only remained marginally significant with a trend toward decreased LARC use in black women (aOR 0.86; 95%CI 0.76–0.98). Ever-homeless women Veterans who served in the Army trended towards less use of any contraceptive (aOR 0.90; 95%CI 0.83–0.97) and in those who did have a highly effective method, it was less likely to be a LARC method compared to permanent use (aOR 0.77; 95%CI 0.65–0.90). (Table 2)
Table 2:
Sample multivariate logistic regression models assessing probability of any long-acting reversible (LARC)1 or permanent contraception2 use and method type in ever-homeless women Veterans who accessed care in the Veterans Health Administration between Fiscal Years 2002–2015
| Variables* | Any LARC or permanent contraceptive1 (OR, 95% CI) |
LARC use compared to permanent method2 (OR, 95% CI) |
Hysterectomy compared to sterilization (OR, 95% CI) |
IUD compared to implant (OR, 95% CI) |
|---|---|---|---|---|
| Marital Status | ||||
| Race | ||||
| Hispanic ethnicity | ||||
| Religion | ||||
| Military Service Branch | ||||
| Combat Experience | ||||
| MST History | ||||
| Rurality Designation | ||||
| VA Region |
OR: odds ratio; CI: confidence interval; MST: Military Sexual Trauma; VA: Veterans Administration
Continuous variables of age at procedure and driving distance were included in the models and represented in Figure 1
LARC includes intrauterine devices and contraceptive implants
Permanent contraception includes all types of permanent female sterilization and hysterectomy
We represented the continuous variables of age and driving distance in Figure 1, which shows the estimated effect curves for the age (first column) and driving distance (second column) variables for the contraceptive presence model (first row) and the reversible contraceptive model (second row). The lines in Figure 1 represent the estimate of effect from the raw data and the estimate from the model. The close proximity of the lines indicates that the shown variables are modeled adequately for the given data. When controlling for other variables, age at procedure remained highly significant with increasing age less likely to receive LARC and more likely to have a hysterectomy than sterilization (p<0.001). From Figure 1, panel 1 we can see the effect of year of birth on contraceptive use with those showing highest usage being born between approximately 1975 and 1980, with decreasing usage farther away from the center. Increasing driving distance to the nearest VAMC decreased the likelihood that a woman would receive any type of LARC or permanent sterilization (p<0.001) and those who did were more likely to receive a permanent method than LARC (p<0.03). From the second row in Figure 1, we see that increased age has a negative effect on the chance the contraceptive method is reversible. For driving distance, only the linear term is statistically significant, however the negative linear trend is highly significant for the contraceptive model, indicating that distance to a facility is highly predictive of failing to find evidence of LARC use. In women with any highly effective contraceptive use (LARC or permanent contraception), driving distance is negatively correlated with LARC (Figure 1).
Compared to urban Veterans, rural designation decreased the likelihood of LARC exposure (aOR 0.78; 95%CI 0.66–0.92) and increased the odds of having a hysterectomy compared to tubal sterilization (aOR 1.44; 95%CI 1.13–1.84). The small numbers in the model for highly rural designation led to wide confidence intervals without significance. National geographic variation by VA region was evident in contraceptive exposure. Compared to the West Region 1, the Midwest Region 2 had increased exposure to any highly effective method (aOR 1.41; 95%CI 1.15–1.82) and increased LARC exposure over permanent methods (aOR 3.68; 95%CI 2.42–5.70). Similarly, women in the New England Region 4 were more likely to receive a LARC method (aOR 1.92; 95%CI 1.29–2.89) compared to West Region 1. (Table 2)
We then explored the effect of housing status in the same models with both the ever-homeless and previously established matched cohort of housed women (sociodemographic comparisons are published elsewhere, but did not consider geographic variables6). We found the effect of distance equally decreased use of contraceptive methods, regardless of housing status. When controlling for driving distance, rurality, and VHA region, in addition to the sociodemographic and military characteristics, we found ever-homeless women were more likely than housed controls to use either LARC or permanent contraception (aOR 1.27; 95%CI 1.19–1.35), but the method was less likely to be reversible (aOR 0.81; 95%CI 0.72–0.92). (Models for housed cohort not shown)
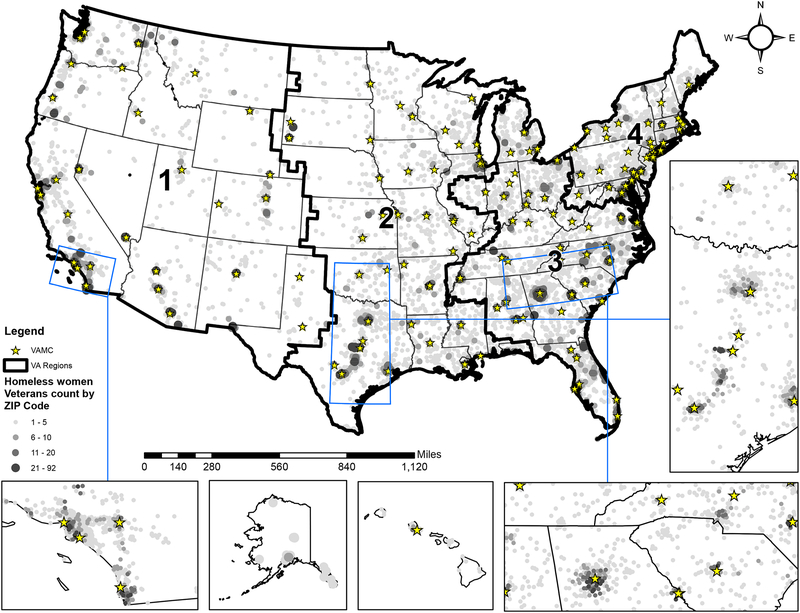
Our analysis resulted in two maps (Figure 2 and Figure 3). The map in Figure 2 shows the geographic distribution of ever homeless women Veterans, with darker areas represent concentrations of homeless women Veterans and stars represent VAMCs. The inset maps shows populated areas in the greater Los Angeles area, in eastern Texas, and across northern Georgia and South Carolina.
Figure 2:
Distribution of homeless women Veterans in the United States who accessed the Veterans Health Administration between Fiscal Years 2002–2015 by Veterans Health Administration (VHA) Region and their proximity to Veterans Health Administration Medical Centers (VAMC)
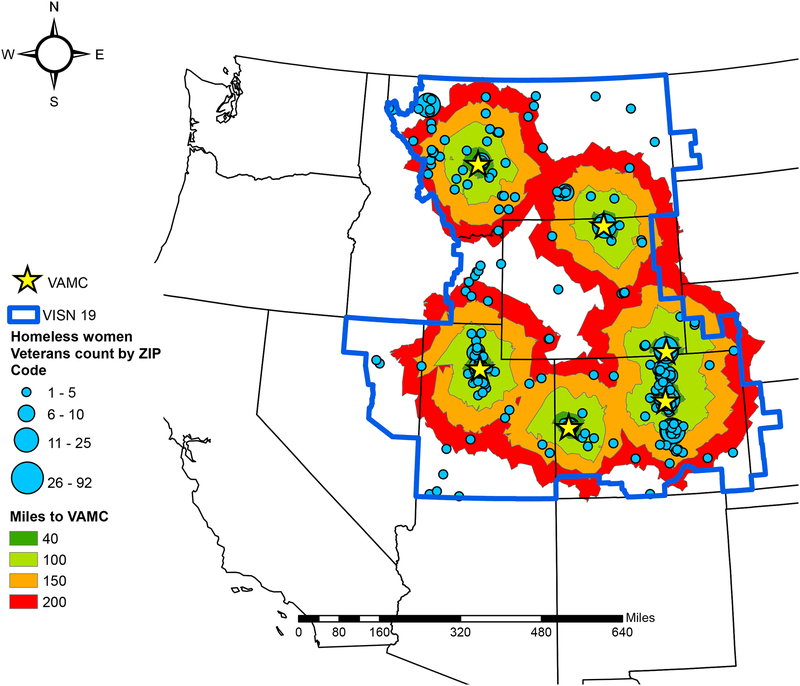
Figure 3:
Driving distance bands from Veterans Health Administration Medical Centers (VAMC) in Veterans Integrated Service Network (VISN) 19 and distribution of homeless women Veterans who accessed the Veterans Health Administration between Fiscal Years 2002–2015
Figure 3 represents drive distances for the 946 ever-homeless women Veterans who we could map in VISN 19 (roughly, Colorado, Montana, Utah, Wyoming, and eastern Idaho), where large areas of rural and frontier land designations exist and contribute to the interpretation of the VA Region 1 West data. We found that 52.3% (n=495, represented by the dark green area) of these lived less than 40 miles to a VAMC; 28.2% resided between 40–100 miles (n=267, light green band), 9.7% resided 101–150 miles (n=92, orange band), and 6.8% resided 151–200 miles (n=64, red band) driving miles from the closest VAMC. We counted 3% (n=28) of these Veterans living farther than 200 miles driving miles from the closest VAMC.
We compared drive distances to the nearest VAMC by housing status to assess differences in those living beyond 40 and 100 miles. Using the test of two proportions, we found ever-homeless women Veterans were more likely to live <40 miles from a VAMC (n=28,867, 69.2%) than housed reproductive age women Veterans (n=29,324, 63.2%: p<0.0001). Ever-homeless women Veterans were less likely to live >40 miles from a VAMC compared to the housed population, in which 24.5% (n=11,345) resided 40–100 miles (p<0.0001) and 8.9% (n=4,157) resided >100 miles from a VAMC (p<0.04).
Discussion
Access to contraception is a safe, actionable, and cost-effective means to decrease risk of unintended pregnancy for all women Veterans, but especially those with high-risk issues, such as homelessness. Despite VHA prioritization of women’s health care services, this study found distance to VAMCs and rurality impacted exposure to LARC and permanent contraceptive options. At a time when national legislative changes are being enacted to improve access to care and community partnerships for all Veterans, contraceptive care is unique due to legislative family planning restrictions5 and geographic barriers must be considered.
Ever-homeless women Veterans serve as an example of a highly vulnerable VHA population, but are not alone in their need for comprehensive contraceptive care or their experience of geographic barriers to health care. In order to address access issues for timely, specialized VHA services, the Veterans Access, Choice and Accountability Act of 2014 (VACAA; sometimes also referred to as the “Choice” program) was passed and follow-up 2015 legislation allowed Veterans waiting >30 days for VHA care, those >40 miles from a VHA facility, and those with “unusual and excessive burden for travel” to receive “Choice” contracted community healthcare.28 This legislation went into effect within 90 days without a feasibility review and subsequent studies show logistical and coordination challenges with civilian providers.29 When evaluating contraceptive access, state-level legislative restrictions have limited publicly-funded family planning services that homeless women Veterans would rely upon outside the VHA.5 Unfortunately, many of the same VHA regions across the US that we found in this study to have decreased LARC exposure are also those with the most restrictive Medicaid eligibility requirements which would insure poor women Veterans for civilian care.30 It is important to acknowledge the national variation by VHA region and decreased access to LARC methods in the western United States, which includes states with the greatest rural population and lack of state-level support for publicly-funded reproductive healthcare.31 This study found 29% of ever-homeless women Veterans live >40 miles from the nearest VAMC and women Veterans are increasingly residing in rural locations1. The VHA community-based outpatient clinics (CBOCs) fill basic healthcare needs, but providers have a low volume of women Veterans in these settings and often refer to VAMCs for LARC. Travel distance and rurality will continue to serve as barriers to contraception for all women Veterans regardless of housing stability, unless CBOC providers or civilian services can fill the gap.
While national policy allows for non-VHA community access to overcome travel barriers, the VHA, unlike many non-VHA providers, is uniquely qualified to provide trauma-informed care and serve as a healthcare model for disparate groups. The high MST prevalence in this study and the known co-occurrence of post-traumatic stress disorder6 may not be addressed by non-VHA providers inexperienced in Veterans’ needs. Many women Veterans prefer a “safe” environment, supportive chaperones, female providers and additional time to get through a triggering exam.32 Additionally, women Veterans with housing instability experience a high prevalence of intimate partner violence which may impact contraceptive needs.33 VHA providers receive training on these special needs and have highly developed MST and mental health services that are lacking in most non-VHA community offices. Unlike previous studies which found poor women and racial/ethnic minorities have reproductive health disparities22,34,35, this study did not find significant differences in contraceptive method exposure based upon reported race or ethnicity, but did find ever-homeless women are more likely to rely on permanent than reversible methods compared to housed women Veterans. It is beyond the scope of this study to identify the reason, but could be due to access barriers, Veteran preference or provider coercion. Access to all contraceptive options fits within the reproductive justice framework where women can chose highly effective methods—if they want them—without coercion, access barriers, or lack of acknowledgement of prior reproductive health abuses to socioeconomically disadvantaged groups.36
Potential solutions to meet vulnerable Veterans’ needs within the VHA when non-VHA services or funding are not available, include reproductive healthcare integration into established homeless services and expanded telehealth use for rural Veterans. As distance impacts contraceptive use regardless of housing status, contraceptive educational initiatives and clinical mentorship for designated women’s health providers in rural areas are essential to meet the needs of all reproductive age women Veterans in their catchment area. Some primary care providers may feel less comfortable with IUD insertions, thus focusing training on contraceptive implants may be more realistic and expand rural access to one LARC method. Improved knowledge and counseling around LARC by VHA providers, even if they do not personally perform surgical sterilizations or LARC insertions, may also increase Veteran knowledge and address disparities noted in permanent contraception.
This study has limitations due to use of structured data captured for clinical care, inability to account for Veterans who never sought care in the system, and use of a validated methodology of administrative evidence to identify homelessness.20 To minimize misclassification, we excluded conflicting codes (i.e. both an IUD and contraceptive implant insertion at the same visit) from our multivariate models. The study captured all women Veterans over a thirteen-year timeframe and we cannot control for the amount of time of each homelessness event. Thus, we refer to the cohort as “ever-homeless” since socioeconomic challenges and comorbidities likely persist beyond the homeless episode. Finally, the use of ZIP Codes at the time of homelessness designation is the best available data proxy for a geographic “home”. This may impact the drive distances calculated and misrepresent travel influence on contraceptive exposure, as well as confound associations if residential mobility occurred. Though the ‘residence’ for an individual experiencing homelessness is a difficult concept, using the last known “residence” is a structured variable that is captured in the VHA medical record and this allows us to begin to understand the distances homeless women Veterans would need to travel to access health care.
Conclusion
Homeless women Veterans represent a vulnerable population at risk for adverse pregnancy outcomes. Geographic variability in comprehensive contraceptive services limits access to the safest and most effective methods. Recent legislation (such as VACAA and the Mission Act) aimed at making local healthcare an option for Veterans who live 40 or more miles from VHA facilities assumes that non-VHA community care will be available and will have the skills necessary to provide contraceptive care. While we applaud the intent as a step in the right direction, this may not work for women Veterans who find themselves living far from the VAMCs where comprehensive contraceptive care is available. As compared to the United States as a whole, western states are more rural, geographically larger, have greater travel burdens, have fewer family planning providers available in rural areas, and often have legislatures enacting relatively restrictive state funding policies for contraceptive care. The VHA can be a national model of excellence to overcome geographic barriers by integrating comprehensive contraceptive services into the current, successful rural health and homeless healthcare programs.
Acknowledgements:
This work was supported by the NIH/NICHD Grant IK12HD085816 (PI: Silver) and K24HD087436 (PI: Turok); University of Utah’s Health Equity and Inclusion Seed Grant; VA HSR&D grant #IIR 12–084 (PI: Gundlapalli) and VA Salt Lake City Center of Innovation Award #I50HX001240 from the Health Services Research and Development of the Office of Research and Development of the US Department of Veterans Affairs.
Footnotes
Disclosure Statement: The authors report no conflicts of interest. The views expressed in this article are those of the authors and do not necessarily represent the position or policy of the US Department of Veterans Affairs or the US government.
References
- 1.Department of Veterans Affairs Women’s Health Services. Longitudinal Trends in Sociodemographics, Utilization, Health Profile, and Geographic Distribution. Sourcebook: Women Veterans in the Veterans Health Administration, Volume 4 Washington, DC: Department of Veterans Affairs; 2018. [Google Scholar]
- 2.Department of Veterans Affairs. Women Veterans Population. Available: http://www1.va.gov/womenvet/docs/WomenVeteransPopulationFactSheet.pdf. Accessed: Nov 7, 2016.
- 3.Carter A, Borrero S, Wessel C, et al. Racial and Ethnic Health Care Disparities Among Women in the Veterans Affairs Healthcare System: A Systematic Review. Womens Health Issues 2016;26(4):401–409. [DOI] [PubMed] [Google Scholar]
- 4.Callegari LS, Zhao X, Schwarz EB, Rosenfeld E, Mor MK, Borrero S. Racial/ethnic differences in contraceptive preferences, beliefs, and self-efficacy among women veterans. Am J Obstet Gynecol 2017;216(5):504 e501–504 e510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gawron L, Pettey WBP, Redd A, Suo Y, Turok DK, Gundlapalli AV. The “Safety Net” of Community Care: Leveraging GIS to Identify Geographic Access Barriers to Texas Family Planning Clinics for Homeless Women Veterans. AMIA Annu Symp Proc. 2017;2017:750–759. [PMC free article] [PubMed] [Google Scholar]
- 6.Gawron LM, Redd A, Suo Y, Pettey W, Turok DK, Gundlapalli AV. Long-acting Reversible Contraception Among Homeless Women Veterans With Chronic Health Conditions: A Retrospective Cohort Study. Med Care 2017; 55 (9):S111–S120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Balshem H, Christensen V, Tuepker A, Kansagara D. Department of Veterans Affairs Health Services Research and Development A Critical Review of the Literature Regarding Homelessness Among Veterans. Washington, DC: Department of Veterans Affairs; 2011. [PubMed] [Google Scholar]
- 8.Cutts DB, Coleman S, Black MM, et al. Homelessness during pregnancy: a unique, time-dependent risk factor of birth outcomes. Matern Child Health J 2015;19(6):1276–1283. [DOI] [PubMed] [Google Scholar]
- 9.Washington DL, Yano EM, McGuire J, Hines V, Lee M, Gelberg L.Risk factors for homelessness among women veterans. J Health Care Poor Underserved 2010:21(1): 82–91. [DOI] [PubMed] [Google Scholar]
- 10.American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 121: Long-acting reversible contraception: Implants and intrauterine devices. Obstet Gynecol 2011;118(1):184–196. [DOI] [PubMed] [Google Scholar]
- 11.US Centers for Disease Control. U.S. Medically Eligibility Criteria for Contraceptive Use. Available: http://www.cdc.gov/mmwr/pdf/rr/rr5904.pdf. Accessed Nov 8, 2016.
- 12.Wagner C, Dichter ME, Mattocks K. Women Veterans’ Pathways to and Perspectives on Veterans Affairs Health Care. Womens Health Issues 2015;25(6):658–665. [DOI] [PubMed] [Google Scholar]
- 13.Reddy SM, Rose DE, Burgess JF, Charns MP, Yano EM. The Role of Organizational Factors in the Provision of Comprehensive Women’s Health in the Veterans Health Administration. Womens Health Issues 2016;26(6):648–655. [DOI] [PubMed] [Google Scholar]
- 14.Gabrielian S, Yuan A, Rubenstein L, Anderson RM, Gelberg L. Serving homeless veterans in the VA Desert Pacific Healthcare Network: a needs assessment to inform quality improvement endeavors. J Health Care Poor Underserved 2013;24(3):1344–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Washington DL, Farmer MM, Mor SS, Canning M, Yano EM. Assessment of the healthcare needs and barriers to VA use experienced by women veterans: findings from the national survey of women Veterans. Med Care 2015;53(Suppl 1):S23–31. [DOI] [PubMed] [Google Scholar]
- 16.Katon J, Reiber G, Rose D, Bean-Mayberry B, Zephyrin L, Washington DL, Yano EM. VA location and structural factors associated with on-site availability of reproductive health services. J Gen Intern Med 2013;28(Suppl 2):S591–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Callegari LS, Gray KE, Zephyrin LC, et al. Hysterectomy and Bilateral Salpingo-Oophorectomy: Variations by History of Military Service and Birth Cohort. Gerontologist 2016;56(Suppl 1):S67–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American College of Obstetricians and Gynecologists. Committee opinion No. 576: health care for homeless women. Obstet Gynecol 2013;122(4):936–940. [DOI] [PubMed] [Google Scholar]
- 19.US Department of Veterans Affairs. VA Informatics and Computing Infrastructure (VINCI), US Department of Veterans Affairs; Washington, D.C. 2015. [Google Scholar]
- 20.Peterson R, Gundlapalli AV, Metraux S, et al. Identifying Homelessness among Veterans Using VA Administrative Data: Opportunities to Expand Detection Criteria. PloS one 2015;10(7):e0132664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Finer LB, Jerman J, Kavanaugh ML. Changes in use of long-acting contraceptive methods in the United States, 2007–2009. Fertility Sterility 2012;98(4):893–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kavanaugh ML, Jerman J, Hubacher D, Kost K, Finer LB. Characteristics of women in the United States who use long-acting reversible contraceptive methods. Obstet Gynecol 2011;117(6):1349–1357. [DOI] [PubMed] [Google Scholar]
- 23.Rosenfeld E, Callegari LS, Sileanu FE, et al. Racial and ethnic disparities in contraceptive knowledge among women veterans in the ECUUN study. Contraception 2017;96(1):54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fehring RJ, Bouchard T, Meyers M. Influence of Contraception Use on the Reproductive Health of Adolescents and Young Adults. Linacre Q 2018;85(2):167–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brignone E, Gundlapalli AV, Blais RK, et al. Differential Risk for Homelessness Among US Male and Female Veterans With a Positive Screen for Military Sexual Trauma. JAMA Psych 2016;73(6):582–589. [DOI] [PubMed] [Google Scholar]
- 26.Rural Health Research Center. Available:http://depts.washington.edu/uwruca/ruca-uses.php. Accessed February 9, 2017. [Google Scholar]
- 27.US Department of Veterans Affairs Office of Rural Health. Rural Definition 2017; Available: https://www.ruralhealth.va.gov/aboutus/ruralvets.asp-def. Accessed Feb 8, 2018.
- 28.Shulkin D Message from VA Secretary Dr. David Shulkin (2017). VAntage Point: Official Blog of the U.S. Department of Veterans Affairs. Available: http://www.blogs.va.gov/VAntage/35253/message-from-va-secretary-david-shulkin/ Accessed: Feb 16, 2017.
- 29.Mattocks KM. Care coordination for women veterans: bridging the gap between systems of care. Med Care 2015;53(4 Suppl 1):S8–9. [DOI] [PubMed] [Google Scholar]
- 30.Hasstedt K Why We Cannot Afford to Undercut the Title X National Family Planning Program. Guttmacher Policy Review 2017;20:20–23. [Google Scholar]
- 31.Institute Guttmacher. Medicaid Family Planning Eligibility Expansions. (2017) Available: https://www.guttmacher.org/state-policy/explore/medicaid-family-planning-eligibility-expansions. Accessed: March 7, 2017.
- 32.Department of Veterans Affairs. Study of Barriers for Women Veterans to VA Health Care. (2015) Available: http://www.womenshealth.va.gov/WOMENSHEALTH/index.asp. Accessed: Dec 15, 2017.
- 33.Kimerling R, Iverson KM, Dichter ME, Rodriguez AL, Wong A, Pavao J. Prevalence of Intimate Partner Violence among Women Veterans who Utilize Veterans Health Administration Primary Care. J Gen Intern Med, 31 (8) (2016), pp. 888–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Breland JY, Chee CP, Zulman DM. Racial Differences in Chronic Conditions and Sociodemographic Characteristics Among High-Utilizing Veterans. J Racial Ethn Health Disparities 2015;2(2):167–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dehlendorf C, Park SY, Emeremni CA, Comer D, Vincett K, Borrero S. Racial/ethnic disparities in contraceptive use: variation by age and women’s reproductive experiences. Am J Obstet Gynecol 2014;210(6):526 e521–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Higgins JA. Celebration meets caution: LARC’s boons, potential busts, and the benefits of a reproductive justice approach. Contraception 2014;89(4):237–241. [DOI] [PMC free article] [PubMed] [Google Scholar]