Abstract
Posttraumatic stress disorder (PTSD) is a highly prevalent, debilitating disorder found to develop after exposure to a potentially traumatic event (PTE). Individuals with PTSD often report sleep disturbances, specifically nightmares and insomnia, which are listed within the criteria for PTSD. This research examined prevalence of insomnia and nightmares within a national sample of 2,647 adults (data weighted by age and sex to correct for differences in sample distribution) who had been exposed to one or more PTEs. Prevalence of self-reported sleep disturbance, sleep disturbances by PTE type, and gender differences were examined. All participants completed a self-administered, structured online interview that assessed exposure to stressful events and PTSD symptoms. Among individuals who met DSM-5 criteria for PTSD, a large majority (more than 92%) reported at least one sleep disturbance. Insomnia was relatively more prevalent than PTE-related nightmares among individuals with PTSD and among all PTE-exposed individuals. A higher number of PTEs experienced significantly increased the likelihood of both trauma-related nightmares and insomnia, McFadden’s pseudo R2 = .07, p < .001. Women exposed to PTEs were more likely to endorse experience of insomnia, χ2(1, N = 2,647) = 99.13, p < .001, φ = .194, and nightmares compared to men, χ2(1, N = 2,648) = 82.98, p < .001, φ = .177, but this gender difference was not significant among individuals with PTSD, ps = .130 and .050, respectively. Differences in sleep disturbance prevalence by PTE type were also examined. Implications for treatment and intervention and future directions are discussed.
Researchers have found that among individuals with posttraumatic stress disorder (PTSD), there is a high prevalence of comorbidity with other psychological disorders (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995; Orsillo, Heimberg, Juster, & Garrett, 1996). Further, there is a higher prevalence of health problems in survivors of potentially traumatic events (PTEs) with PTSD than in PTE survivors without PTSD (Schnurr & Green, 2004). One specific area of high prevalence and comorbidity in individuals with PTSD is sleep disturbances, such as insomnia, trauma-related nightmares, nocturnal panic attacks, and other problematic nocturnal motor behaviors (Freed, Craske, & Greher, 1999; Germain, 2013; Germain, Hall, Krakow, Shear, & Buysse, 2005). The association between sleep disturbances and PTSD is complex, and a growing body of literature indicates it is potentially reciprocal, as prospective studies have shown sleep disturbances are not only a symptom of PTSD but likely a risk factor for the development of PTSD following a PTE (for detailed review, see Babson & Feldman, 2010, and Germain, 2013).
Recent research has found that treatment of sleep problems reduces other PTSD symptoms even when an individual is not directly treating the PTSD. For example, Margolies, Rybarczyk, Vrana, Leszczyszyn, and Lynch (2013) implemented treatments for insomnia and nightmares in a randomized controlled trial with 40 veterans and found the treatment not only reduced sleep complaints but also symptoms of PTSD and depression, compared to participants in a waitlist control group. Additionally, Gehrman (2015) found that using cognitive behavioral therapy for insomnia (CBT-I) with 126 veterans resulted in not only improved sleep and decreased insomnia but also improvement in PTSD symptoms. Some researchers have even posited that CBT-I should be used as a preparatory therapy for individuals with PTSD if they are resistant to exposure treatment or therapy engagement in general and cited a case study with 90-day follow up continued remission of PTSD symptoms (Baddeley & Gros, 2013).This is important because sleep disturbances in individuals with PTSD have been shown to be associated with severe physical and mental health problems, such as suicidal thoughts and depression (Clum, Nishith, & Resick, 2001; Nishith, Resick, & Mueser, 2001). Two types of sleep disturbances, nightmares and insomnia, are listed specifically within the criteria for PTSD (Criterion B, “intrusions” and Criterion E, “alterations in arousal,” respectively; American Psychiatric Association [APA], 2013; pp. 271–272) and were the focus of this study.
Insomnia disorder, which is defined as difficulty falling asleep or staying asleep at least three nights per week for at least 3 months and resulting in clinically significant distress or impairment (APA, 2013), is highly prevalent among individuals with PTSD. For instance, in two large samples (civilian and veteran), Miller and colleagues (2012) reported that 93% of civilian participants who met criteria for PTSD also reported insomnia symptoms at some point in their lifetime, which they directly attributed to a PTE. Treatment-seeking veterans showed a similar pattern, as 81% of the sample reported insomnia symptoms attributed to a PTE.
Previous research has found differences in presentation of PTSD symptomatology, such as emotion regulation, based on trauma type (Ehring & Quack, 2010; Kelley, Weathers, McDevitt-Murphy, Eakin, & Flood, 2009); recent research has applied this to sleep-related symptoms by examining this association between PTE type and insomnia risk. Hall Brown, Akeeb, and Mellman (2015) collected self-report measures from 554 nonclinical, urban, young adult African Americans and found that sexual trauma, physical assault, accidents, natural disasters, and sudden violent death predicted insomnia, although this association was mediated by PTSD severity. Fire and/or explosions and life-threatening illness or injury were not associated with insomnia symptoms. Using similar self-report methodology in a sample of 1,599 undergraduates, Lind and colleagues (2017) reported similar findings. Specifically, having experienced interpersonal PTEs (e.g., physical or sexual assault) predicted worse sleep quality, but having experienced accidental PTEs (e.g., motor vehicle accidents) did not. Consistent with Hall Brown and colleagues, Lind and colleagues found that the presence of probable PTSD mediated the association between interpersonal trauma and sleep quality. Both of these studies added valuable information to the research on the association between PTE type, PTSD symptoms, and sleep. However, both were limited to primarily healthy, young adults and therefore these results may not be generalizable to the larger public.
Nightmares related to a PTE are another prevalent symptom of PTSD. In the study by Miller and colleagues (2012) described earlier, nightmares were endorsed by 66% of the civilian sample and 78% of the veteran sample, and nightmares that follow a PTE have been shown to be more significantly associated with poor sleep quality than nightmares that began prior to a PTE (Davis, Pruiksma, Rhudy, & Byrd, 2011). To our knowledge, no studies to date have examined the association between type of PTE and prevalence of nightmares.
In the current study, we investigated insomnia symptoms (henceforth “insomnia”) and nightmares as distinct entities, given these symptoms are assessed separately, contained within different symptom clusters within PTSD diagnostic criteria, and have different prevalence rates and markedly different empirically supported treatment strategies, such as exposure, relaxation, and rescripting therapy for nightmares (ERRT; Pruiksma, Cranston, Rhudy, Micol, & Davis, 2018) and CBT-I for insomnia (Trauer, Qian, Doyle, Rajaratnam,& Cunnington, 2015). It is therefore important to examine them separately to inform PTSD work from prevention to intervention. As such, the presence of each type of sleep disturbance likely results in different patterns of association with PTEs. Given that the majority of previous research examining sleep problems in PTSD has focused on nightmares and the fact that such a large percentage of individuals with PTSD report insomnia (Miller et al., 2012), unpacking the association between insomnia and PTEs and/or PTSD will significantly impact the field’s understanding and could have significant implications for treatment. Additionally, in order to better understand how sleep disturbances may differ depending upon demographic characteristics or PTE history, we examined whether other variables, such as gender or PTE type (Breslau, 2002; Haskell et al., 2010), affect rates of PTE-related sleep disturbances. Our aim was for these findings to provide new, novel information to inform research as well as clinical practice and treatment to help better understand areas for prevention and intervention. The current research was the first, to our knowledge, to examine the prevalence of insomnia and nightmares in a sample of individuals who met diagnostic criteria for PTSD according to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; APA, 2013) compared to PTE-exposed individuals without PTSD. As symptoms changed from the fourth edition of the DSM (DSM-IV) to the DSM-5, this data provides the most current view of PTSD to truly better understand how sleep disturbances are associated with PTEs and PTSD. We sought to extend previous research by examining prevalence of self-reported sleep disturbance within individuals with PTSD and investigating the interface of sleep problems, PTE type, and PTSD within a nationally representative PTE-exposed sample.
Method
Participants and Procedure
Prior to beginning the study, all procedures were approved by the Medical University of South Carolina institutional review board. Participants were recruited through the National Stressful Events Survey (NSES; Kilpatrick, Resnick, Baber, Guille, & Gros, 2011), an anonymous web survey created and commissioned by the DSM-5 Trauma & Stressor-Related Disorders Sub-Workgroup to assess the impact of proposed DSM-5 PTSD changes. The web survey was described as a national survey of exposure to extremely stressful events and/or experiences and how they affect people. Potential participants provided consent prior to engaging in the study and were encouraged to participate regardless of whether or not they had experienced stressors or had problems. Of the 3,756 people who accessed the website, 3,457 (92.0%) agreed to participate and 2,953 completed the survey, which represents 85.4% of respondents who agreed to participate and 78.6% of the total number who accessed the site. Given the anonymity of the survey, it was not possible to question the reason for dropout in individuals who did not complete the survey. Participants represented a vast age range: 10.6% were 18–24 years of age, 18.2% were 25–34, 7.4% were 35–44, 21.2% were 45–54, 23.0% were 55–64, and 19.5% were 65 and older. The majority of participants were White (75%). Sample data were weighted by age and sex to correct for differences in sample distribution on these variables from population parameters. More details on this assessment, data collection, and detailed demographic information (e.g., age, race, ethnicity, and sex) can be found in an earlier publication that reported on the same sample described in this paper (see Kilpatrick et al., 2013).
All participants completed a self-administered, structured online interview, which assessed for exposure to PTEs as well as PTSD symptoms, including insomnia (restless sleep or trouble getting to sleep or staying asleep) and PTE-related nightmares. Participants indicated to which PTE or PTEs (endorsed earlier in the survey) they attributed their PTSD symptoms. Of the 2,953 participants who completed the survey, 2,647 (89.6%) reported exposure to at least one DSM-5-defined Criterion A PTE (APA, 2013). Most participants were between 45 and 54 years of age (19.4% of sample), female (52.0%), White (63.1%), and had at least a high school degree (94.8%).
Measures
Assessment of exposure to stressful events.
Exposure was measured with 25 closed-ended questions that assesses exposure to DSM-5 Criterion A events. For the purposes of our analyses, we derived 10 categories from this broader set of exposure items: natural or manmade disaster, fire/accident, exposure to hazardous chemicals, war zone/combat exposure, physical/sexual assault, witnessing physical/sexual assault, witnessing dead bodies, family or friend experiencing a life threat or injury, violent death of a family or friend, and PTE exposure secondary to work (e.g., in the case of paramedics or other first responders). Participants were also given the opportunity to provide narrative descriptions of other events that produced physical injuries, fear of being seriously injured or hurt, or any potential other event that was not included. Participants who indicated that they had experienced one or more of the events listed were then asked a series of follow-up questions to determine how many times they experienced PTEs, which event they experienced first, and, if they had experienced multiple events, which they considered to be the worst. Descriptive information about the first PTE and the worst PTE was collected. We also assessed for Criterion A2 (i.e., whether the participant thought they might be seriously injured or killed, experienced a panic attack during or shortly after the event, and/or experienced emotions of fear, anger, sadness, horror, violation of trust, or embarrassment/shame during the event). Of note, the strategy used to assess for exposure to PTEs, as well as whether participants met other diagnostic criteria, was more comprehensive than is typical of epidemiological studies. More details on the assessment of PTEs can be found elsewhere (see Kilpatrick et al., 2013).
PTSD symptoms and functional impairment.
Symptoms of PTSD were measured using questions designed for this study that assessed for each DSM-5 PTSD symptom. Functional impairment was measured by asking participants to rate, on a 5-point scale (1= not at all to 5 = extremely), how distressing it was when they had PTSD symptoms and whether PTSD symptoms had resulted in problems with employment, daily living, relationships, or in school. If participants endorsed a 4 (quite a bit distressing) or 5 (extremely distressing), on any of these distress items or indicated that PTSD symptoms had produced significant problems with employment, daily living, relationships, or school, they were coded positive for functional impairment. We used collective information about PTE exposure, PTSD symptoms, and functional impairment to determine whether participants met criteria for a lifetime PTSD diagnosis (i.e, whether the participant endorsed a traumatic event along with the right configuration of symptoms for diagnosis and whether the participant noted his or her symptoms were functionally impairing). The PTSD assessment used in the current report did not require specification of an index PTE; therefore, participants’ responses may reflect symptom experience that resulted from multiple PTEs. Specifically, this report used a composite PTSD score as defined in Kilpatrick et. al. (2013) in which all symptom criteria thresholds must be met, but they could be met in response to any combination of Criterion A PTEs. However, it is important to note that all participants who endorsed any PTSD symptom were either asked if the symptom was directly related to the PTE (i.e., nightmare content) or asked follow-up questions as to whether the symptom began or worsened after the PTE (i.e., insomnia). All analyses conducted that included the nightmare symptom had to do with trauma-related nightmares, and all analyses that examined insomnia were run both with the full sample as well as with the 72% of participants who endorsed symptom onset and/or worsening that was directly related to the PTE; the results did not significantly differ when we excluded the 28% of participants who did not directly attribute their insomnia to the PTE, as is outlined in the Results and Discussion sections. Therefore, we proceeded on the notion that the reported symptoms were, in fact, related to the PTE and not just daily life stressors.
Sleep problems.
Lifetime experience of insomnia symptoms was assessed with one dichotomous item: “Have you ever had a period of time of more than a few days when you had restless sleep or trouble getting to sleep or staying asleep?” Similarly, lifetime experience of nightmares was assessed with one dichotomous item: “Have you ever had repeated distressing dreams or nightmares about a stressful experience from the past or distressing dreams that were closely related to the stressful experience?” As described earlier, participants were then queried as to whether the symptom began or worsened following the PTE.
Data Analysis
Data were collected by the original authors for a larger study (see Kilpatrick, Resnick, Milanak et al., 2013. Analyses were conducted using IBM SPSS (Version 21) and R 3.4.1 (R Core Team, 2017). Missing data were minimal (less than 1.0% of data missing on all study variables) and were handled using pairwise deletion. We used McNemar’s test to investigate differences in the endorsement of insomnia and nightmares in our sample. We then ran chi-square tests to compare group-level differences (i.e., gender and lifetime PTSD diagnostic status) in insomnia and nightmares. We also conducted several logistic regression analyses to examine the odds of experiencing lifetime sleep disturbances (i.e., insomnia and nightmares) based on endorsement of 10 types of PTEs and the association between total number of PTEs and presence of sleep disturbances.
Results
Prevalence of PTEs and Lifetime PTSD
Of the 2,953 participants who completed the survey, 2,647 (89.6%) endorsed experience of at least one lifetime DSM-5-defined PTE, with experience of physical/sexual assault and violent death of family/friend as the most prevalent event types endorsed by PTE-exposed participants. Of these participants, 277 (10.5%) met full lifetime DSM-5 criteria for PTSD. Descriptive information that details the prevalence of PTE-related insomnia and nightmares as well as various PTE types within the sample is reported in Table 1.
Table 1.
Descriptive Statistics on Study Variables by Trauma Exposure and Posttraumatic Stress Disorder (PTSD) Diagnosis
| Variable | Trauma Exposed (n = 2, 647) |
PTSD Diagnosis (n = 277) |
|||
|---|---|---|---|---|---|
| Sleep Disturbance | n | % | n | % | |
| Insomnia only | 444 | 16.8 | 69 | 24.9 | |
| Nightmares only | 360 | 13.6 | 31 | 11.3 | |
| Both insomnia and nightmares | 366 | 13.8 | 157 | 56.7 | |
| Neither sleep problem | 1,477 | 55.8 | 19 | 6.9 | |
| Traumatic event typea | |||||
| Natural or manmade Disaster | 1,491 | 56.3 | 126 | 54.5 | |
| Accident or fire | 1,427 | 53.9 | 167 | 60.5 | |
| Hazardous chemicals | 493 | 18.6 | 74 | 26.6 | |
| War zone/combat | 231 | 8.7 | 24 | 8.8 | |
| Physical/sexual assault | 1,568 | 59.2 | 240 | 86.7 | |
| Witness physical/sexual assault | 982 | 37.1 | 163 | 58.7 | |
| Witness dead bodies | 667 | 25.2 | 106 | 38.3 | |
| Family/friend life threat/injury | 956 | 36.1 | 160 | 57.7 | |
| Family/friend violent death | 1,529 | 57.8 | 206 | 74.6 | |
| Secondary work Exposure | 340 | 12.9 | 60 | 21.7 | |
Participants were able to endorse experience of multiple event types; thus, cumulative percentages for endorsement of traumatic events will exceed 100%.
Prevalence of Sleep Disturbances by PTE Exposure and PTSD Diagnostic Category
Among participants who reported exposure to at least one lifetime PTE, results from an exact McNemar’s test showed that more individuals reported experience of insomnia than experience of nightmares, p < .001. However, as shown in Table 1, the majority of individuals (55.8%) reported experiencing neither sleep disturbance. Among participants who met criteria for lifetime PTSD, the results from an exact McNemar’s test also demonstrated that more individuals reported experience of insomnia than reported experience of nightmares, p < .001.
In contrast to PTE-exposed participants who did not meet criteria for PTSD, far more participants with PTSD endorsed experience of sleep disturbances, with 56.7% of this group endorsing experience of both PTE-related insomnia and nightmares, and 93.0% of participants endorsing some type of sleep disturbance (i.e., insomnia only, nightmares only, or both). The full breakdown of sleep disturbance prevalence is found in Table 1. We performed chi-squared tests to compare endorsement of insomnia and nightmares among PTE-exposed individuals with and without PTSD diagnoses. Note that comparisons of these symptoms included individuals who endorsed experience of both types of sleep disturbance. Results of these tests revealed a significant association between insomnia and PTSD diagnosis, χ2(1, N = 2,646) = 381.36, p < .001, such that individuals with PTSD were more likely to endorse insomnia (n = 226, 81.9% vs. n = 584, 24.6% for those without PTSD). Similar results were observed for the association between nightmares and PTSD, in that individuals with PTSD were more likely to endorse experience of nightmares over the lifetime, χ2(1, N = 2,647) = 256.28, p < .001. Specifically, only 22.7% (n = 538) of PTE-exposed participants endorsed experiencing nightmares, compared to 68.1% (n = 226) of those with PTSD.
Differences in Experience of Sleep Disturbances, by Gender
Among all adults exposed to PTEs, women were significantly more likely to meet lifetime PTSD diagnostic criteria compared to men (n = 197, 14.3% vs. n = 80, 6.3%), χ (1, N = 2,647) = 45.39, p < .001. Additionally, compared to men, women reported higher prevalence of PTE-related insomnia (n = 539, 39.2% vs. n = 271, 21.3%), χ2(1, N = 2,647) = 99.13, p < .001; as well as PTE-related nightmares (n = 482, 35.0% vs. n = 244, 19.2%) χ2(1, N = 2,648) = 82.98, p < .001. When analyses were restricted to only the participants who met lifetime DSM-5 PTSD diagnostic criteria, women and men did not differ in their endorsement of PTE-related insomnia (n = 157, 79.7% vs. n = 70, 86.4%), χ2(1, N = 277) = 1.73, p = .130; or on endorsement of PTE-related nightmares (n = 140, 71.1% vs. n = 48, 60.0%) χ2(1, N = 277) = 3.20, p = .050, although the latter difference was marginal.
We considered the possibility that some of our questions about the prevalence of sleep problems in people with and without PTSD could be confounded by the fact that sleep problems are two of the symptoms of PTSD. Note that in our sample, 83.5% of the people who met criteria for PTSD as defined in the DSM-5 would still meet the criteria if their sleep symptoms were ignored. When our prevalence analyses were re-conducted using these groups, all findings remained the same, except for one: When sleep is removed from PTSD diagnosis, the results showed that among people with PTSD, women experience more nightmares than men.
Sleep Disturbances Based on Type of PTE
To examine the role that different trauma types play in lifetime sleep disturbance, a series of four nested multinomial logistic regression models were estimated. The outcome variable had four categories: no sleep difficulties, nightmares only, insomnia only, and both insomnia and nightmares. This variable was created by combining the two questions about nightmares and insomnia, described earlier in the Measures section. For all models, the no sleep difficulties group was treated as the reference group. In order of parameter parsimony, the null model included only an intercept term and was treated as the baseline comparison model; the gender-only model included and intercept and a gender term (male = 1, female = 0); the PTE count model included an intercept term, gender, and a variable representing the count of how many different types of PTEs (e.g., fire, combat, witnessing death) a participant had experienced, ranging from 1 to 10; and finally, the full PTE types model included and intercept and gender, but also an individual term for each of the 10 PTE types, instead of a single count term. Because it is relevant for subsequent testing, the reader is reminded that the PTE Count model is technically nested within the full PTE Types. That is, the PTE Count is a special case of the PTE Types model, in which every unique PTE term has the same b-coefficient.
Model-level statistics are given in Table 2, which shows that both the PTE count and PTE types models are consistently superior to the null and gender-only models, consistent with what would be expected based on the literature above that shows sleep is affected by trauma. However, when the models were directly compared to one another, results were more ambiguous as to whether the PTE count or PTE types model was superior. Specifically, the PTE types model has a significantly improved chi-square value as well as the associated improvement in Akaike information criterion (AIC) and pseudo R2 over the PTE count model. This suggests that some trauma types may have more powerful (and different) effects on different types of sleep difficulties than others. However, the degree to which they do so is likely quite small (i.e., leading to only a 2% increase in pseudo R2). Moreover, the Bayesian information criterion (BIC) clearly favored the simpler PTE count model. This suggests that, if model complexity is incorporated into model selection, of all the models we estimated , the PTE count model provided the best tradeoff between explanatory power and parsimony.
Table 2.
Model Statistics for Nested Multinomial Logistic Regressions.
| Modela | df | Deviance | AIC | BIC | McFadden’s pseudo R2 | χ2 Diff. | χ2 Diff. p |
|---|---|---|---|---|---|---|---|
| Null | 3 | 6,618.46 | 6,624.46 | 6,642.17 | |||
| Gender only | 6 | 6,486.36 | 6,498.36 | 6,533.73 | .02 | 132.10 | < .001 |
| PTE count | 9 | 6,149.63 | 6,167.63 | 6,220.69 | .07 | 336.73 | < .001 |
| Unique PTE types | 36 | 6,095.80 | 6,167.80 | 6,380.02 | .08 | 53.84 | .002 |
AIC = Akaike information criterion; BIC = Bayesian information criterion; diff. = difference; PTE = potentially traumatic event.
The null model includes only an intercept. The gender-only model includes an intercept and gender. The PTE count model includes an intercept, gender, and the count of PTE types a participant reported. The unique PTE types model includes an intercept, gender, and a dichotomous variable for each PTE type separately (1 = experienced and 0 = not experienced).
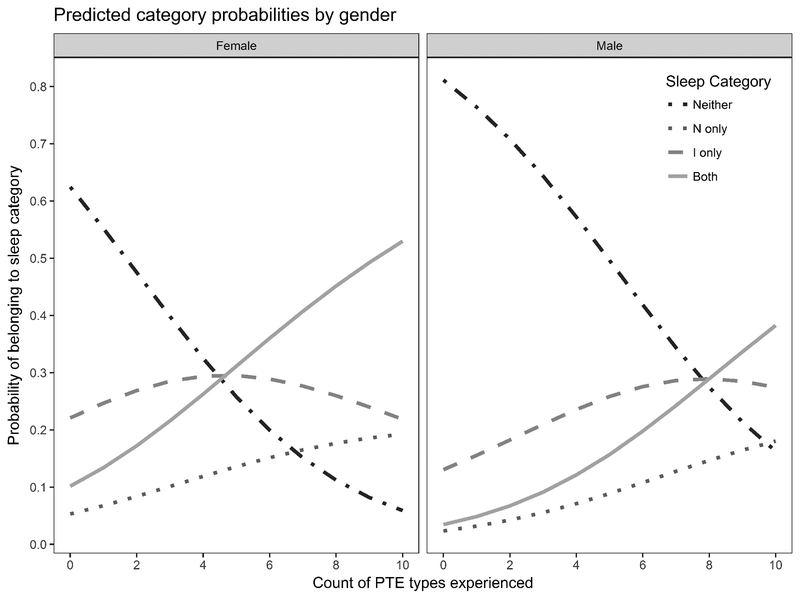
Given these somewhat equivocal results, we present parameter estimates for both models in Tables 3 and 4. We clarify that additional samples will need to be studied before any questions about the unique effect of any particular traumatic event can be confirmed. However, the current results did provide strong support for the impact of exposure to any PTE on both nightmares and insomnia as well as strong support for the assumption that greater exposure to a diverse set of traumas is associated with a higher risk of both nightmares and insomnia for both men and women. This finding is most easily seen in Figure 1, which shows the predicted probabilities of different lifetime sleep difficulties according the PTE count model. As the figure shows, the more different types of PTEs a person reports (i.e., his or her PTE count), the more likely he or she is to experience lifetime sleep difficulty, especially both nightmares and insomnia.
Table 3.
Parameter Estimates for Potentially Traumatic Event Types Model
| Outcome and Predictora | B | SE | Wald’s Z | p | Relative Risk Ratio |
|---|---|---|---|---|---|
| Nightmares only | |||||
| Intercept | 0.08 | 0.18 | 0.45 | .655 | 1.09 |
| Gender | 0.35 | 0.16 | 2.14 | .033 | 1.41 |
| Disaster | 1.05 | 0.15 | 6.92 | < .001 | 2.86 |
| Accident/fire | 1.52 | 0.16 | 9.68 | < .001 | 4.58 |
| Hazardous chemicals | 0.61 | 0.21 | 2.86 | .004 | 1.84 |
| Combat exposure | 1.41 | 0.26 | 5.48 | < .001 | 4.10 |
| Physical/sexual assault | 1.96 | 0.16 | 12.29 | < .001 | 7.10 |
| Witnessing assault | 2.42 | 0.17 | 13.86 | < .001 | 11.21 |
| Witnessing bodies | 1.47 | 0.18 | 8.14 | < .001 | 4.34 |
| Friend or family member in danger | 1.48 | 0.16 | 8.97 | < .001 | 4.38 |
| Friend or family member dying | 1.28 | 0.16 | 7.91 | < .001 | 3.61 |
| Work-related trauma | 1.34 | 0.21 | 6.26 | < .001 | 3.83 |
| Insomnia only | |||||
| Intercept | 0.31 | 0.12 | 2.66 | .008 | 1.37 |
| Gender | 0.51 | 0.11 | 4.87 | < .001 | 1.67 |
| Disaster | 0.97 | 0.10 | 9.44 | < .001 | 2.63 |
| Accident/fire | 0.98 | 0.10 | 9.39 | < .001 | 2.68 |
| Hazardous chemicals | 0.85 | 0.14 | 5.92 | < .001 | 2.34 |
| Combat exposure | 0.95 | 0.20 | 4.84 | < .001 | 2.59 |
| Physical/sexual assault | 1.72 | 0.10 | 16.48 | < .001 | 5.57 |
| Witnessing assault | 1.62 | 0.12 | 13.09 | < .001 | 5.03 |
| Witnessing bodies | 1.17 | 0.13 | 8.80 | < .001 | 3.23 |
| Friend or family member in danger | 1.47 | 0.11 | 12.88 | < .001 | 4.37 |
| Friend or family member dying | 1.80 | 0.11 | 16.81 | < .001 | 6.07 |
| Work-related trauma | 0.80 | 0.17 | 4.64 | < .001 | 2.23 |
| Both insomnia and nightmares | |||||
| Intercept | 0.14 | 0.14 | 0.97 | .332 | 1.15 |
| Gender | 0.31 | 0.13 | 2.42 | .016 | 1.36 |
| Disaster | 1.01 | 0.12 | 8.51 | < .001 | 2.74 |
| Accident/fire | 1.31 | 0.12 | 10.75 | < .001 | 3.69 |
| Hazardous chemicals | 1.25 | 0.15 | 8.34 | < .001 | 3.51 |
| Combat exposure | 0.91 | 0.22 | 4.09 | < .001 | 2.49 |
| Physical/sexual assault | 2.40 | 0.13 | 19.12 | < .001 | 10.98 |
| Witnessing assault | 1.87 | 0.14 | 13.56 | < .001 | 6.47 |
| Witnessing bodies | 1.26 | 0.15 | 8.64 | < .001 | 3.54 |
| Friend or family member in danger | 1.79 | 0.13 | 14.06 | < .001 | 5.98 |
| Friend or family member dying | 1.81 | 0.13 | 14.30 | < .001 | 6.12 |
| Work-related trauma | 1.01 | 0.18 | 5.60 | < .001 | 2.76 |
The reference group for all outcomes was “neither insomnia or nightmares.”
Table 4.
Parameter Estimates for Potentially Traumatic Event Count Model
| Outcome and Predictora | b | SE | Wald’s z | p | Relative Risk Ratio | |
|---|---|---|---|---|---|---|
| Nightmares only | ||||||
| Intercept | 0.09 | 0.15 | 0.55 | .579 | 1.09 | |
| Gender | 0.34 | 0.15 | 2.24 | .025 | 1.40 | |
| PTE count | 1.44 | 0.03 | 42.99 | < .001 | 4.22 | |
| Insomnia only | ||||||
| Intercept | 0.35 | 0.10 | 3.55 | < .001 | 1.42 | |
| Gender | 0.46 | 0.10 | 4.55 | < .001 | 1.58 | |
| PTE count | 1.26 | 0.02 | 52.80 | < .001 | 3.54 | |
| Both insomnia and nightmares | ||||||
| Intercept | 0.16 | 0.12 | 1.37 | .171 | 1.18 | |
| Gender | 0.26 | 0.12 | 2.18 | .030 | 1.30 | |
| PTE count | 1.49 | 0.03 | 55.31 | < .001 | 4.45 | |
PTE = potentially traumatic event.
The reference group for all outcomes is “neither insomnia or nightmares.”
Figure 1.
Predicted probabilities of experiencing different sleep problems for female and male participants, according to the potentially traumatic event (PTE) count model. The genders are separated by panel. Each line inside a panel represents a different category of sleep difficulty. The height of a line at a given PTE count represents the probability a person experiencing that many different types of PTEs will experience that category of sleep problems. For example, a female individual who endorses 10 PTEs has a 0.05 probability of having neither nightmares nor insomnia, a 0.14 probability of having only nightmares, a 0.16 probability of having only insomnia, and a 0.65 probability of having both. Because a person must always belong to one, and only one, of these groups, the sum of the predicted probabilities at each PTE level is always 1. Neither = neither nightmares or insomnia; N only = nightmares only; I only = insomnia only; Both = both nightmares and insomnia.
Discussion
Consistent with what has been reported in previous research (e.g., Germain 2013; Miller et al., 2012), PTE-related insomnia and nightmares were prevalent among participants who reported a history of PTE exposure, and we found that prevalence of these sleep disturbances increased substantially among individuals who met criteria for PTSD. Indeed, among individuals who met criteria for PTSD, the large majority (93.0%) reported at least one PTE-related sleep disturbance. Insomnia was relatively more prevalent than PTE-related nightmares among individuals with PTSD and among all PTE-exposed individuals. We also found that the number of PTEs participants experienced significantly increased the likelihood they would have both PTE-related nightmares and insomnia. Our results highlight the importance of assessing for and treating insomnia among individuals with a history of PTE exposure and, particularly, those with a concurrent PTSD diagnosis. Although many providers and researchers might view nightmares as the core sleep disturbance among individuals with a history of PTE exposure, and especially among those with PTSD, we found that insomnia may be more prevalent and represent a more critical treatment target for individuals with a history of PTE exposure. These results are especially salient, as they demonstrate the high prevalence of insomnia among a general population-based sample of individuals that was not restricted to those seeking treatment for sleep disturbances. Therefore, these findings significantly contribute to the literature by highlighting the importance of urging providers to assess for insomnia specifically and include interventions to target insomnia.
In addition to highlighting the prevalence of insomnia among PTE-exposed individuals, we also investigated gender differences in endorsement of symptomatology. We found that PTE-exposed women were more likely to endorse the experience of insomnia and nightmares compared to men. Among participants with PTSD, however, this gender difference was not significant. One reason may be that the majority of individuals with PTSD were women, as is the case in the broader literature (Breslau, 2002); therefore, the gender effect may wash out when controlling for PTSD only. These findings are important for providers to be aware of to ensure that a thorough assessment for sleep disturbances is conducted, especially in women with a history of PTE exposure.
Although PTE-related insomnia and nightmares are highly prevalent in general, prevalence varied somewhat depending on the type of sleep disturbance and PTE history. Having a better understanding of differential effects of PTEs on sleep disturbances not only informs the general literature, but again has significant implications for treatment and intervention. Keeping in mind that the results of our multinomial models were ambiguous as to which specific model was best, we found that, at a minimum, the number of diverse traumas to which a person has been exposed is associated with increased risk of insomnia alone, nightmares alone, and both nightmares and insomnia together. In other words, experiencing not only multiple PTEs but multiple types of PTEs (e.g., experiencing a car accident and sexual assault) increases an individual’s risk for developing sleep disturbances. When we examined results from another model that did not assume one common slope across all trauma types, that model showed that several types of PTEs, especially physical or sexual assault, were uniquely associated with a higher likelihood of both insomnia and nightmares,. Therefore, these data provide preliminary evidence that it is not only the number of PTEs but also the types of PTEs an individual experiences that play a significant role in insomnia and/or nightmares after PTE exposure. Further research will be necessary and important to examine the more specific association between trauma type and sleep disturbance. Given the observed association between direct physical and/or sexual assault and both types of sleep disturbances, our findings provide some support to the findings of Lind and colleagues (2015), who found a robust association between interpersonal PTEs and disturbed sleep.
Strengths of this study included use of a large, population-based sample and measurement of a vast array of types of PTE. These findings add to the current literature, as we examined the prevalence of insomnia and nightmares (the two types of sleep disturbance included in a PTSD diagnosis) in a sample of individuals who met diagnostic criteria for PTSD according to the DSM-5, and analyzed the association between sleep disturbance and type of PTE in a large, PTE-exposed sample.
Limitations included the cross-sectional nature of the study; the assessment of insomnia and nightmares via a single-item, self-reported question; and lack of information about time since index PTE. Further, although 71.8% of our participants reported that their insomnia began or worsened after a trauma, some of them did not, and it is possible that some of the differences in prevalence across the various groups we compared in this study were partially affected by people who were experiencing a non-trauma-specific insomnia. However, it is important to note that when we conducted auxiliary analyses that excluded the 28% of participants who did not specifically endorse onset and/or worsening of sleep disturbances after the PTE, the results remained unchanged. In addition, our analyses addressed these associations with respect to having ever had a PTSD diagnosis, and it is important to determine if the same pattern of results would occur among individuals with PTSD during the past 6 months or current PTSD.
Future research should examine correlates and/or longitudinal predictors of different patterns of sleep disturbances (e.g., insomnia, nightmares, or both) as well as additional types of sleep disorders (e.g., narcolepsy, obstructive sleep apnea) to more fully understand prevalence and patterns of sleep disorders that may occur after, and/or be associated with, PTEs and PTSD. Furthermore, it will be important to better understand differential patterns of sleep disturbance experience based upon PTE type, particularly as they are associated with indirect or witnessed PTEs. One of the largest practical applications of this research relates to the high prevalence of sleep disturbances we observed in the current study, which clinically supports the need for mental health providers to assess for and directly treat sleep disturbances in individuals with a history of PTE exposure and particularly for those with PTSD. Additionally, given the potential for ethnic/racial differences in prevalence and symptom presentation, it will be important to examine such differences in future work. Finally, given the high prevalence of insomnia observed among participants with PTSD, our findings highlight the importance of recognizing that nightmares are not the sole, nor the most prevalent, sleep disturbance related to PTE exposure.
Acknowledgments
This research was funded by an American Psychiatric Association DSM grant to Dean Kilpatrick as well as by the U.S. Department of Veterans Affairs Mental Health Services. This work was supported in part by the South Carolina Clinical and Translational Research Institute, with an academic home at the Medical University of South Carolina (National Institute of Health: UL1 RR029882 and UL1 TR000062).
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Babson KA, & Feldner MT (2010). Temporal relations between sleep problems and both traumatic event exposure and PTSD: A critical review of the empirical literature. Journal of Anxiety Disorders, 24, 1–15. 10.1016/j.janxdis.2009.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baddeley JL, & Gros DF (2013). Cognitive behavioral therapy for insomnia as a preparatory treatment for exposure therapy for posttraumatic stress disorder. American Journal of Psychotherapy, 67, 199–210. 10.1176/appi.psychotherapy.2013.67.2.203 [DOI] [PubMed] [Google Scholar]
- Breslau N (2002). Gender differences in trauma and posttraumatic stress disorder. The Journal of Gender-Specific Medicine, 5, 34–40. [PubMed] [Google Scholar]
- Clum GA, Nishith P, & Resick PA (2001). Trauma-related sleep disturbance and self-reported physical health symptoms in treatment-seeking female rape victims. The Journal of Nervous and Mental Disease, 189, 618–622. 10.1097/00005053-200109000-00008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JL, Pruiksma KE, Rhudy JL, & Byrd P (2011). A comparison of lifelong and posttrauma nightmares in a civilian trauma sample: Nightmare characteristics, psychopathology, and treatment outcome. Dreaming, 21, 70–80. 10.1037/a0022862 [DOI] [Google Scholar]
- Ehring T, & Quack D (2010). Emotion regulation difficulties in trauma survivors: The role of trauma type and PTSD symptom severity. Behavior Therapy, 41, 587–598. 10.1016/j.beth.2010.04.004 [DOI] [PubMed] [Google Scholar]
- Freed S, Craske MG, & Greher MR (1999). Nocturnal panic and trauma. Depression and Anxiety, 9, 141–145. [DOI] [PubMed] [Google Scholar]
- Gehrman P (2015). CBT for insomnia in veterans with PTSD. Sleep Medicine, 16, S9–S10. 10.1016/j.sleep.2015.02.021 [DOI] [Google Scholar]
- Germain A (2013). Sleep disturbances as the hallmark of PTSD: Where are we now? American Journal of Psychiatry, 170, 372–382. 10.1176/appi.ajp.2012.12040432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Germain A, Hall M, Krakow B, Shear MK, & Buysse DJ (2005). A brief sleep scale for posttraumatic stress disorder: Pittsburgh Sleep Quality Index Addendum for PTSD. Journal of Anxiety Disorders, 19, 233–244. 10.1016/j.janxdis.2004.02.001 [DOI] [PubMed] [Google Scholar]
- Hall Brown TS, Akeeb A, & Mellman TA (2015). The role of trauma type in the risk for insomnia. Journal of Clinical Sleep Medicine, 11, 735–739. 10.5664/jcsm.4846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haskell SG, Gordon KS, Mattocks K, Duggal M, Erdos J, Justice A, & Brandt CA (2010). Gender differences in rates of depression, PTSD, pain, obesity, and military sexual trauma among Connecticut war veterans of Iraq and Afghanistan. Journal of Women’s Health, 19, 267–271. 10.1089/jwh.2008.1262] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, & Nelson CB (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52, 1048–1060. 10.1001/archpsyc.1995.03950240066012 [DOI] [PubMed] [Google Scholar]
- Kelley LP, Weathers FW, McDevitt-Murphy ME, Eakin DE, & Flood AM (2009). A comparison of PTSD symptom patterns in three types of civilian trauma. Journal of Traumatic Stress, 22, 227–235. 10.1002/jts.20406 [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Baber B, Guille C, & Gros K (2011). The national stressful events web survey (NSES-W). Charleston, SC: Medical University of South Carolina. [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, & Friedman MJ (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress, 26, 537–547. 10.1002/jts.21848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lind MJ, Baylor A, Overstreet CM, Hawn SE, Rybarczyk BD, Kendler KS, … Amstadter AB (2017). Relationships between potentially traumatic events, sleep disturbances, and symptoms of PTSD and alcohol use disorder in a young adult sample. Sleep Medicine, 34, 141–147. 10.1016/j.sleep.2017.02.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolies SO, Rybarczyk B, Vrana SR, Leszczyszyn DJ, & Lynch J (2013). Efficacy of a cognitive-behavioral treatment for insomnia and nightmares in Afghanistan and Iraq veterans with PTSD. Journal of Clinical Psychology, 69, 1026–1042. 10.1002/jclp.21970 [DOI] [PubMed] [Google Scholar]
- Miller MW, Wolf EJ, Kilpatrick D, Resnick H, Marx BP, Holowka DW, … Friedman MJ (2013). The prevalence and latent structure of proposed DSM-5 posttraumatic stress disorder symptoms in U.S. national and veteran samples. Psychological Trauma: Theory, Research, Practice, and Policy, 5, 501–513. 10.1037/a0029730 [DOI] [Google Scholar]
- Nishith P, Resick PA, & Mueser KT (2001). Sleep difficulties and alcohol use motives in female rape victims with posttraumatic stress disorder. Journal of Traumatic Stress, 14, 469–479. 10.1023/A:1011152405048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orsillo SM, Heimberg RG, Juster HR, & Garrett J (1996). Social phobia and PTSD in Vietnam veterans. Journal of Traumatic Stress, 9, 235–252. 10.1002/jts.2490090207 [DOI] [PubMed] [Google Scholar]
- Pruiksma KE, Cranston CC, Rhudy JL, Micol RL, & Davis JL (2018). Randomized controlled trial to dismantle exposure, relaxation, and rescripting therapy (ERRT) for trauma-related nightmares. Psychological Trauma: Theory, Research, Practice, and Policy, 10, 67–78. 10.1037/tra0000238 [DOI] [PubMed] [Google Scholar]
- R Core Team. (2017). R: A language and environment for statistical computing Vienna, Austria: R Foundation for Statistical Computing; Retrieved from http://www.R-project.org/ [Google Scholar]
- Schnurr PP, & Green BL (2004). Trauma and health: Physical health consequences of exposure to extreme stress. Washington, DC: American Psychological Association. [Google Scholar]
- Trauer JM, Qian MY, Doyle JS, Rajaratnam SM, & Cunnington D (2015). Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Annals of Internal Medicine, 163, 191–204. 10.7326/M14-2841 [DOI] [PubMed] [Google Scholar]