Abstract
Although hearing loss is known to be associated with many adverse health outcomes in older adults, current hearing healthcare remains expensive and inaccessible to most ethnic minorities in the US. We aim to adapt an affordable, community-based hearing intervention to older Korean Americans (KAs), describe the cultural adaption process, and report pilot trial outcomes. We undertook the first four stages of Barrera & Castro’s cultural adaptation framework: information gathering, preliminary adaptation design, adaptation test, and adaptation refinement in 15 older KAs with hearing loss and 15 of their communication partners. We developed a culturally adapted intervention consisting of provision of an affordable listening device and aural rehabilitative training. Six weeks post-intervention, participants’ mean hearing handicap score (range: 0-40) reduced from 15.7 to 6.4. Communication partners demonstrated improved social-emotional function. Post-intervention focus group revealed increased hearing benefit, confidence in hearing health navigation, and awareness in hearing health among study participants. The adapted intervention was well-accepted and feasible among older KAs. This study is the first to report the cultural adaptation process of a hearing care model into older KAs and its methodology may be applied to other minority groups.
Keywords: Hearing loss, Korean Americans, Cultural Adaptation, Hearing Healthcare, Disparities
Introduction
Hearing loss affects nearly 70% of adults greater than 70 years of age in the United States (US) (Lin, Thorpe, Gordon-Salant, & Ferrucci, 2011) and is independently associated with social isolation, depression, accelerated decline in physical functioning, and risk of incident dementia (Chen et al., 2015; Lin & Albert, 2014; Lin, Metter, et al., 2011; Livingston et al., 2017; Mener, Betz, Genther, Chen, & Lin, 2013; Mick, Kawachi, & Lin, 2014). Despite its prevalence and burden on society, hearing loss is largely underdiagnosed and undertreated (Centers for Disease Control, 1997; Lin, Niparko, & Ferrucci, 2011; Lin, Thorpe, et al., 2011). Recent initiatives from the National Academies of Science, Engineering, and Medicine (The National Academies of Sciences Engineering and Medicine, 2016) and the White House President’s Council of Advisors on Science and Technology (President’s Council of Advisors on Science and Technology, 2015) established hearing loss as a critical public health issue and resulted in the passage of the Over-the-Counter Hearing Aid legislation in August 2017.
The current model of clinic-based hearing healthcare in the US remains complex, time-intensive, and highly expensive for most older adults, requiring 3-5 visits to hearing care professionals and out-of-pocket costs averaging $4,700 a pair (Nieman & Lin, 2017; Strom, 2014). The established model of hearing healthcare is additionally challenging for racial and ethnic minorities in the US, where cultural and language barriers increase the difficulty of navigating the hearing healthcare system. Previous studies have demonstrated significantly lower rates of hearing aid use among minorities (10-17.1%) compared to White older adults (28.6-35.4%) (Bainbridge & Ramachandran, 2014; Knudsen, Öberg, Nielsen, Naylor, & Kramer, 2010; Mamo, Nieman, & Lin, 2016; Meyer, Hickson, Lovelock, Lampert, & Khan, 2014); this magnitude of disparity is likely conservative given that immigrant, minority older adults with language barriers, such as Korean Americans, may be underrepresented in these studies.
Korean Americans (KAs) are one of the fastest-growing Asian sub-populations in the US with homogeneous race/ethnicity, language, and culture (Shahid, 2012). Older KAs are predominantly monolingual first-generation immigrants who typically maintain their cultural beliefs and attitudes while in the US. In South Korea, the rates of hearing aid use among older adults is estimated to be 8-11%, lower than rates found in other countries (Korea Centers for Disease Control and Prevention, 2010; National Evidence-Based Healthcare Collaborating Agency, 2011). A focus group study on a sample of older KAs with hearing loss identified high costs, navigational difficulties, language barrier, and stigma toward hearing loss as barriers for hearing aid use (Choi et al., 2018). Despite a pressing need for more accessible and affordable hearing intervention programs for minority older adults, no such programs have been implemented in KAs. In an effort to deliver a culturally competent hearing intervention that can address KAs’ unique barriers, our study team adapted a low-cost, community-delivered hearing intervention called HEARS (Hearing Equality through Accessible Research and Solutions) to older KAs following a validated model of cultural adaptation (Barrera, Castro, Strycker, & Toobert, 2013). HEARS is a theory-driven intervention originally developed to promote hearing health among English-speaking older adults in urban, low-income housing (Nieman et al., 2017).
Cultural adaptation of hearing healthcare interventions that could reach racial/ethnic minority groups of older adults is critical to improving accessibility of effective intervention programs and reducing hearing disparities (Barrera et al., 2013; The American Geriatrics Society Ethnogeriatrics Committee, 2016). While there have been many successful models of culturally-adapted health interventions for other chronic conditions including cardiovascular disease and diabetes (Brown, Garcia, Kouzekanani, & Hanis, 2002; Osuna et al., 2011), there have been few prior efforts reported in the literature to reach and provide care to minority older adults with hearing loss. This paper describes the stages of cultural adaptation of HEARS program, and the feasibility, acceptability, and preliminary efficacy of the culturally-adapted hearing intervention, called K-HEARS, targeting a population of older KAs. We hypothesized that K-HEARS would be well-accepted and feasible with a potential to reduce hearing handicap among older KAs with hearing loss.
Materials and Methods
Study Participants
We recruited community-dwelling older KAs in partnership with a suburban Korean church in Maryland between December 2014 and March 2015. An ethnic church was chosen as our intervention venue since greater than 80% of KAs report going to church regularly (Islam et al., 2013). Study announcements were made by the church pastor and in the church newsletter 2-3 weeks prior to a hearing screening session at the church. Flyers were then distributed at church on the day of hearing screening to invite potential participants to the screening session. Hearing screening was conducted using a portable audiometer (Tremetrics RA 300, CT, USA) in a quiet room at the church. Upon completion of hearing screening, bilingual study staff contacted those who met the eligibility criteria to participate in the pilot study. The study was approved by the [blinded] Institutional Review Board.
Eligibility criteria for participation in the pilot study included 1) age ≥ 55 years, 2) self-identified as Korean American, 3) self-reported ability to read and speak Korean, 4) screening audiometry pure-tone-average (PTA) 1,2,4kHz ≥ 25dB HL in worse hearing ear (i.e., hearing loss), 5) report not currently using a hearing aid, and 6) has a communication partner who was able to participate in the study. Communication partners (CPs) were individuals 1) who were aged ≥ 18 years, 2) spoke Korean, and 3) communicated with the participants on a daily basis.
Twenty-five individuals participated in the hearing screening, and twenty-two individuals were eligible to participate in the study. Of twenty-two eligible participants, four could not be reached after screening and three had scheduling conflicts. The remaining fifteen individuals with hearing loss and fifteen of their CPs participated in the pilot study. Written consent in Korean was obtained from all study participants.
Cultural Adaptation Procedures
The original program HEARS was a community-delivered, low-cost hearing intervention developed for English-speaking, low-income older adults (Nieman et al., 2017). The intervention, developed based on Bandura’s Social Cognitive Theory with specific emphasis on self-efficacy (Bandura, 1977) and a human factors approach to design for older adults (Fisk, Rogers, Charness, Czaja, & Sharit, 2009), was a one-time session that included selection of an over-the counter personal sound amplification product (PSAP), fitting and orientation to the device, and education on hearing loss and communication strategies. Greater details of the intervention design and development of the program are described elsewhere (Nieman et al., 2017). The program was shown to be effective at improving hearing handicap, communication function, and depressive symptoms among study participants. The K-HEARS intervention was adapted from the original HEARS program to serve older KAs based on the framework of the following the first four cultural adaptation stages proposed by Barrera and Castro (Table 1) (Barrera et al., 2013; Castro, Barrera, & Holleran Steiker, 2010). The final stage of the cultural adaptation trial is to be completed in the future and will be reported separately
Table 1.
Stages in the Cultural Adaptation of the Hearing Intervention and Adaptation Activities
| Stage | Adaptation Activities | Findings & Cultural Adaptation Components |
|---|---|---|
| Information gathering | Literature review |
Findings from literature review:
|
| Focus groups |
Findings from focus groups (n=2, 11 participants):
|
|
| Preliminary adaptation design | Preliminary changes to the intervention |
|
| Intervention materials translation |
|
|
| Preserve core elements of original intervention |
|
|
| Preliminary adaptation tests | Delivery of a preliminary version |
|
| Assessment of implementation difficulties, content/activities, and satisfaction |
Findings from the case studies:
|
|
| Adaptation refinement | Revision of intervention based on the feedback |
|
| Cultural adaptation trial | Pilot trial of the revised intervention |
|
| In-depth interviews of participants |
|
|
| Final trial (to be completed) |
|
1). Information gathering:
The bilingual/bicultural study team conducted a literature review to search for evidence of subcultural group differences in hearing healthcare among KAs and previous applications of evidence-based interventions. Next, we conducted two focus groups including older KAs (age ≥55 years) with hearing loss and their CPs (n=11). Findings on the perceptions towards hearing loss and unique barriers to hearing healthcare use among KAs were previous reported (Choi et al., 2018). In this stage, we further explored the acceptability and feasibility of core components of the original HEARS intervention among older KAs and their CPs. Participants responded positively to a proposed hearing program to be delivered in their community, if the program was delivered by a bilingual interventionist who is fluent in Korean and familiar with Korean culture. Among a choice of devices, the over-the-counter listening device with a design resembling a Bluetooth headset instead of a standard hearing aid was highly acceptable to participants.
2). Preliminary Intervention Design:
We made preliminary changes to the intervention as informed by the Information Gathering stage. Changes were made in intervention staffing, recruitment, demographic and outcome measures, and intervention form and content while preserving the core elements of the original intervention. Specific changes made to the original HEARS intervention are highlighted in Table 1.
3). Preliminary Adaptation Test:
A bilingual interventionist (J.C.) delivered the preliminary version of the adaptation. Case studies were conducted where the interventionist delivered the preliminary version to 2 native/bilingual healthcare professionals and 2 community representatives (one older KA with hearing loss and his CP). We received feedback to assess implementation difficulties and satisfaction with the program content and activities.
4). Adaptation Refinement:
In response to the feedback from the Preliminary Adaptation Test stage, we made changes to further tailor the intervention. Changes included: enhancing cultural values during role play of communication strategies by incorporating short scripts relatable to family/social settings of KA family and adding a visual guide to explain participant’s level of hearing loss (e.g. speech banana audiogram with the participant’s hearing screening result). Final 1-hour education session of K-HEARS consisted of orientation to the listening device followed by communication education and counseling. Follow-up included a phone call from an interventionist within 5 days of intervention and a group troubleshooting session after 2 weeks of intervention. Details of the characteristics of the final intervention are described in Table 2.
Table 2.
Characteristics of the Intervention delivered as the Final Stage of the Cultural Adaptation
| Intervention Content | |
|---|---|
| 30-min Screening a(P) |
|
| 1-hour Education (P and CP) a |
Device Provision & Orientation
|
Communication Education & Counseling
| |
| Follow-up (P) |
|
P: Participants with hearing loss, CP: Communication Partners
Screening session was followed by the education session in one-sitting
Participants selected from two devices: the Sound World Solutions CS-50® (Park Ridge, IL; approximate retail price $350) or the Williams Sound Pocketalker Ultra Duo Pack® (Eden Prairie, MN; approximate retail price $120). The devices were selected by the medical and audiological team based on the quality of output, features, and price point. Devices were provided free-of-charge as part of the study.
5). Cultural Adaptation Trial:
A pilot study of the K-HEARS intervention was conducted using older KAs with hearing loss (n=15) and their CPs (n=15) as an initial step towards the final trial to be completed in the future. We conducted post-intervention focus groups with pilot study participants (n=2, 11 participants) to gather suggestions for future modifications and to determine whether the intervention had a potential to reduce hearing handicap. Details of the pilot trial are summarized in Table 2.
Focus Groups
As part of the cultural adaptation process, we conducted focus groups pre-intervention (n=2, 11 participants) and post-intervention (n=2, 11 participants). The moderator’s guide questions were developed in English based on previous literature and the study team’s experiences in working with individuals with hearing loss and the KA community. Bilingual study staff translated the questions and their accuracy was confirmed by a certified translator. After informed consent, short demographic data were collected using questionnaires. Two bilingual moderators familiar with Korean culture facilitated each focus group and a separate note-taker was present to audiotape the discussion and record notes. Moderators and a note-taker reviewed the discussion notes after each focus group and audiotapes were transcribed verbatim.
The focus group interview data was analyzed using qualitative content analysis with an inductive coding approach (Hsieh & Shannon, 2005; Knudsen et al., 2012; Thomas, 2006). Two coders independently reviewed the transcripts and field notes multiple times to understand each focus group and documented initial coding to identify themes and subthemes of the group responses. Then, the research team discussed the discrepancy of the themes and subthemes until a consensus was reached in iterative fashion. After a series of team discussions, final categories of themes and subthemes were determined. Only final results of themes, subthemes, and supporting quotes were translated to English (Barnes, 1996; Suh, Kagan, & Strumpf, 2009).
Measures
Assessments of the participants were obtained at baseline and 6 weeks after receiving the intervention. Baseline measures included questions on demographics, acculturation, and potential covariates including hearing history. The primary outcome was self-reported communication difficulties assessed by using the validated, Korean version of the Hearing Handicap Inventory for the Elderly (HHIE-S) (Y. Kim et al., 2001; Park et al., 2011; Ventry & Weinstein, 1983). Scores range from 0 to 40 with higher scores indicating higher levels of hearing handicap. An HHIE-S score ≥8 is considered indicative of a significant hearing handicap (Lichtenstein, Bess, & Logan, 1988). Participants were also assessed on social-emotional function using Korean language versions of the UCLA Loneliness Scale (O. S. Kim, 1997) and the Patient Health Questionnaire (PHQ-9) (C. Han et al., 2008), and health-related quality of life using Short-Form General Health Survey (SF-12) (Nam et al., 2007). Psychosocial factors associated with listening device use were assessed by using the Attitudes towards Loss of Hearing Questionnaire (ALHQ) among participants with hearing loss (Saunders & Cienkowski, 1996). Components of the ALHQ include denial of hearing loss, negative associations with listening device, negative coping strategies, self-reported difficulties with manual dexterity and vision, and hearing-related self-esteem. Third-party disability was assessed among CPs by using the Significant Other Scale for Hearing Disability (SOS-HEAR) (Scarinci, Worrall, & Hickson, 2009). Overall program, device use, and satisfaction were measured with the International Outcome Inventory-Alternative Interventions (IOI-AI) (Chu et al., 2012) and self-reported willingness to pay (Yueh et al., 2001). Validated Korean versions were used for all available questionnaires. SOS-HEAR questionnaire was not available in a validated Korean version. As such, the questions were translated to Korean by a native speaker with an expertise in hearing loss to ensure that the questionnaire addressed the needs of the target population. The translations were further verified by a certified translator (Hall et al., 2018).
Statistical Analyses
Descriptive statistics were used to characterize the cohort and to summarize outcome measures before and after the intervention. Mean and standard deviation were used to summarize continuous variables and frequency was used for categorical variables. The primary outcome was change in HHIE-S scores from baseline to 6 weeks post-treatment. Hypothesis tests were not conducted given the study was a feasibility pilot study with a small sample size. All analyses were conducted using Stata 11.1 (StataCorp, College Station, Texas).
Results
Our study cohort included 15 dyads comprised of 15 older adults with hearing loss and their 15 CP counterparts (Table 3). The mean age of participants with hearing loss was 67.9 years (range: 57-82 years) and 62.9 years for CPs (range: 30-75 years). Most participants with hearing loss had an annual household income less than $25,000 (73%) and an education level of high school or less (60%). Period of residency in the US varied among participants from 9 to 40 years, and all participants with hearing loss moved to the US when they were 22 years or older (Table 3). Most participants with hearing loss and their CPs reported speaking only Korean at home (83%). Seven participants had mild hearing loss (PTA 1,2,4kHz 25-39dB HL in worse hearing ear), 7 had moderate hearing loss (PTA 1,2,4kHz40-59dB HL), and 1 participant had normal hearing in one ear and severe hearing loss in the other ear (PTA 1,2,4kHz; ≥60 dB HL). Ten CPs were spouses of the participants with hearing loss (67%), and 5 CPs were either a child, sibling, or fellow parishioner.
Table 3.
Participants characteristics of the pilot trial (n=30)
| Characteristics | Participants with HL (n=15) |
Communication Partners (n=15) |
|---|---|---|
| Age, years (S.D.) | 67.9 (8.1) | 62.9 (11.6) |
| [Range] | [57-82] | [30-75] |
| Sex (%) | ||
| Female | 5 (33%) | 13 (87%) |
| Education (%) | ||
| Some college | 6 (40%) | 4 (36%) |
| Annual income, US Dollar (%) | ||
| <$25,000 | 11 (73%) | 8 (53%) |
| Insurance (%) | ||
| Medicare/Medicaid | 8 (53.3%) | 9 (60.0%) |
| Other insurance | 7 (46.7%) | 6 (40.0%) |
| Period of residency in the US, years (S.D.) | 27.1 (9.7) | 27.1 (8.9) |
| [Range] | [9-40] | [9-40] |
| Age when first came to the US, years (S.D.) | 41.5 (12.2) | 36 (13.8) |
| [Range] | [22-64] | [3-61] |
| Language use at homea (%) | ||
| Only Korean | 13 (87%) | 12 (80%) |
| More Korean than English | 1 (7%) | 3 (20%) |
| Both equally | 1 (7%) | 0 (0%) |
| Assessment of HL using speech-frequency pure-tone audiometerb (%) | ||
| No hearing lossc | 1 (6.7%) | - |
| Mild | 7 (46.7%) | - |
| Moderate | 7 (46.7%) | - |
| Self-reported trouble hearingd | ||
| Good | 2 (13%) | - |
| A little trouble | 5 (33%) | - |
| Moderate | 4 (27%) | - |
| A lot of trouble | 4 (27%) | - |
| Ever received hearing exam (%) | 9 (60%) | - |
| Ever hearing aid user (%) | 3 (20%) | - |
| Current hearing aid user (%) | 0 (0%) | - |
| Relationship with participant with HL (%) | ||
| Spouse | - | 10 (67%) |
| Child/sibling | - | 3 (20%) |
| Parishioner | - | 2 (13%) |
HL=Hearing Loss
Participants were asked, “what language(s) do you usually speak at home? Only Korean, more Korean than English, both equally, more English than Korean, or only English?”
Audiometry-measured hearing status is defined by a speech-frequency pure tone average of hearing thresholds at 1, 2, and 4 kHz in the better-hearing ear (normal PTA <25dB, mild hearing loss 25-39dB, moderate or greater ≥ 40dB).
One older adult with unilateral severe hearing loss included in the study
Participants were asked, “Which statement best describes your hearing (without a hearing aid)? Would you say your hearing is excellent, good, that you have a little trouble, moderate trouble, a lot of trouble, or are you deaf?”
Pre- versus Post-Intervention Changes in Outcome Measures
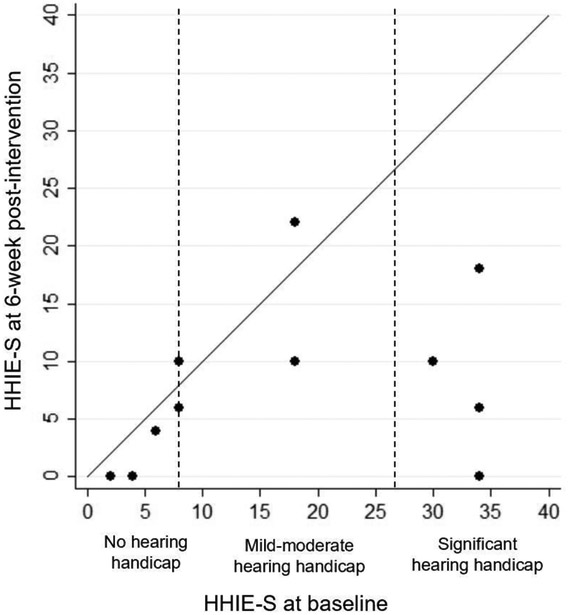
At baseline, the participants with hearing loss reported relatively high levels of communication difficulties with mean HHIE-S scores of 15.7 (SD: 13.1, range: 2-34). After intervention, the HHIE-S scores decreased to 6.4 (SD: 6.9, range 0-22) (Table 4). For psychosocial factors associated with listening device use, mean scores in 4 out of 5 components of ALHQ (score range 0-5) improved after intervention: reduced negative associations with listening device use (2.5 to 1.8), reduced negative coping strategies (2.6 to 2.2), reduced difficulties with manual dexterity and vision (2.5 to 2.1), and improved hearing-related esteem (3.3 to 3.8). Among participants with hearing loss, there were minimal changes in mean scores of social-emotional function measured by UCLA Loneliness Scale (31.8 to 32.7) and PHQ9 (7.9 to 7.6). For quality of life, there was a slight improvement in mental component SF-12 scores after intervention (45.4 to 49.6) while change in physical component scores was minimal (40.5 to 40.0).
Table 4.
Outcomes at Baseline and 6-week follow-up
| Measures (score range) | Participants with HL (n=15) | Communication Partners (n=15) | ||||
|---|---|---|---|---|---|---|
| Baseline Mean (SD) |
6-week follow-up Mean (SD |
Mean Change |
Baseline | 6-week follow-up |
Mean Change |
|
| Communication Function | ||||||
| HHIE-S (0-40) | 15.7 (13.1) | 6.4 (7.0) | −9.3 | - | - | - |
| Attitudes towards Loss of Hearing (ALHQ) | ||||||
| Denial of Hearing Loss (0-5) | 3 (0.7) | 3.1 (0.5) | 0.1 | - | - | - |
| Negative Associations (0-5) | 2.5 (0.8) | 1.8 (0.8) | −0.7 | - | - | - |
| Negative Coping Strategies (0-5) | 2.6 (0.8) | 2.2 (0.6) | −0.4 | - | - | - |
| Manual Dexterity and Vision (0-5) | 2.5 (1.0) | 2.1 (0.8) | −0.4 | - | - | - |
| Hearing-related Esteem (0-5) | 3.3 (0.7) | 3.8 (0.8) | 0.5 * | - | - | - |
| Third-party Disability (SOS-HEAR) | ||||||
| SOS-HEAR Total Score (0-5) | - | - | - | 2.0 (1.5) | 1.7 (1.2) | −0.3 |
| Social-Emotional Function | ||||||
| UCLA Loneliness Scale (20-80) | 31.8 (12.7) | 32.7 (13.5) | 0.9 | 31.6 (9.5) | 28.6 (8.3) | −3.0 |
| PHQ9 (0-30) | 7.9 (6.5) | 7.6 (7.8) | −0.3 | 4.7 (3.4) | 3.0 (3.5) | −1.7 |
| Quality of Life | ||||||
| SF-12 Physical Component (0-100) | 40.5 (10.6) | 40.0 (11.8) | −0.5 * | 43.1 (11.7) | 42.3 (11.4) | −0.8 * |
| SF-12 Mental Component (0-100) | 45.4 (12.2) | 49.6 (11.1) | 4.2 * | 47.5 (10.2) | 51.8 (8.4) | 3.8 * |
Measures with high scores representing better function
Among CPs, the mean scores in SOS-HEAR questionnaires assessing their third-party disability (score ranges 1-5) decreased from 2.0 at baseline to 1.7 after intervention. Reductions in mean scores of UCLA Loneliness scale (31.6 to 28.6) and PHQ9 (4.7 to 3.0) were relatively more substantial than the mean score changes among their partners with hearing loss. Similar to the changes observed among participants with hearing loss, mental component of SF-12 scores slightly improved (47.5 to 51.8) and there was minimal change in physical component scores (43.1 to 42.3).
Intervention Feasibility and Acceptability
All participants completed the study without adverse events. Most participants reported using the listening device and communication strategies regularly (Supplement A). The majority of the participants, both older KAs with hearing loss and CPs, reported moderate or greater benefit from the program, slight to no limitation in residual activity, high satisfaction, and slight or higher improvement in quality of life (Supplement A). All participants reported slight or significant benefit from the K-HEARS program and that they would recommend the listening device and the K-HEARS program to others. Eighty seven percent of participants with hearing loss and 93% of CPs felt more connected with others. Ninety three percent of participants with hearing loss and 87% of CPs felt less lonely. Ninety tree percent of participants with hearing loss and 100% of CPs found having a CP to go through the program with to be helpful. Seventy eight percent of participants with hearing loss who attended the follow-up group session reported great benefit from the session. The mean amount for the K-HEARS program that the participants were willing to pay were $139 (range $0-$500) and $115 (range $30-$500) for the older KAs with hearing loss and CPs, respectively.
Post-intervention Focus Groups
Focus groups were conducted after the 6-week follow-up session with the intervention participants (n=2, 11 participants) to explore their experiences with the program, the intervention impact, and further modifications needed for future programs. Qualitative content analysis revealed four themes 1) Intervention impact on participants, 2) Facilitators for program participation, 3) Barriers to listening device use, and 4) Plans for future studies (Table 5).
Table 5.
Post-intervention Focus Group Themes, Subthemes, and Supporting Quotes
| Subthemes | Sample Quotes |
|---|---|
| Theme 1: Intervention Impact on Participants | |
| Hearing Benefit | [Before the program] I couldn't hear well at work when the customers say their phone numbers. Now I try to wear this device at work as much as possible. PHL 001 |
| One time during sermon, I experimented taking off the amplification device to see the difference. It's definitely better to keep the device on. I am very satisfied. I used to not to be able to hear the sermon very well. PHL 002 | |
| [Before participating in the program] I only guessed and thought to myself that [my partner] had hearing problems. Now I clearly know how severe his hearing loss is, so I try to enunciate, speak more clearly and slowly, and make sure that he understands… I've become more considerate. I used to grumble over thinking to myself, 'wow why can't he understand this' but now I don't feel that way anymore. CP 001 | |
| Confidence in hearing health navigation | I've earned this basic knowledge in listening device [from the program]. Since I've used it once, I have confidence. … I can ask appropriate questions if I were to buy another one. The experience gave me confidence. PHL 002 |
| I don't worry much about [future] problems [with follow-up care or the device], I can always come back here [to the K-HEARS program for those problems]. PHL 002 | |
| Increased awareness of listening device and hearing health | None of us knew that this thing called an amplification device existed. We only knew about hearing aids. [Through the K-HEARS program], we learned about the device, how to use the device, and actually have been using the device. I'm glad that I didn't miss this opportunity to know about this useful device. CP 004 |
| Many of my friends do have hearing difficulties but they live on as if nothing's wrong. … Now those friends want me to contact the program staff so they can enroll in the program. CP 002 | |
| Theme 2: Facilitators for Program Participation | |
| Price | I knew that my hearing was bad enough to have to use hearing aids. But I didn't have [money] to purchase hearing aids that were thousands of dollars. I came here [to participate in the program] for a listening device. PHL 001 |
| Since my partner got older, he has been saying that he can't hear well. We were going to get him tested anyways and I heard that there was a free hearing screening. We thought why not as it's free. CP 004 | |
| Accessibility | I liked that [the education sessions] were done at church. I didn't have to make any extra trips as they were scheduled before or after mass on Sundays. PHL 001 |
| I wouldn’t know who to trust if I were to buy an amplification device from the market myself. I'm sure there are many types of amplification devices and I can't try and wear every single one out there. I could use this amplification device because I got it from the program. I would be afraid if I had to choose one from the market myself. PHL 002 | |
| Face-to-face interaction | I don't know how I feel about [learning how to use the amplification device] myself. But [the interventionist] explained and set up everything for us in-person [in this program] … I feel more comfortable [about using the device]. PHL 002 |
| In fact, it is a lot easier for us to listen and see [how to use an amplification device] than trying to read a book. CP 003 | |
| Group Session | Only when you're starving do you understand others' hunger. Similarly, unless you are hard of hearing, you won't understand the pain of someone that is hard of hearing. When I first met everyone [at the group session] and even now, I feel that [we understand each other]. PHL 001 |
| [During the group session], I could listen to other people's stories and see everybody's different circumstances. Since some people had worse hearing than others, I learned what it would be like to be in their situation and what I need to do if my hearing ever got that bad. The group session was helpful because I could plan out what to do in the future and learn from others. PHL | |
| Theme 3: | Barriers to Listening Device Use |
| Shame | During mass or conversations, I need to say 'This is a listening device,' because they're going to think 'Why is that person wearing that?' I actually feel more intimidated and shrink away when I'm wearing this device, since I need to tell people that my hearing has gotten so bad that I need to wear this now. PHL 001 |
| Discomfort | Most people don't acknowledge that I've gotten older, but when I'm wearing this device they comment, 'You're already wearing that? PHL 003 I can't wear this all day. I don't know if it's the shape of my ears, but it's very uncomfortable to wear it and I've only worn it up to 7 hours. PHL 001 |
| If the device is tightly on, it's okay. But if something touches it, like when I'm driving and the window is close to the device, there's all these noises. So I take it off. PHL 004 | |
| Forgetfulness | When I'm working, this device can fall out. So I don't wear it at work. Since I shouldn't lose it, I sometimes just leave it at home or put it in my bag and only wear it when I need to. PHL 007 |
| Theme 4: | Plans for Future Studies |
| Raise program awareness | You need to be able to advertise. If you include a pamphlet in the Sunday bulletin [at the church] about what an amplification device is, everybody can see it. Then, you can put information about when you will be doing this program and who to contact. Having a pamphlet would be the best. PHL 002 |
| Everything in this project costs money, right? Even [the amplification device] is expensive. So even though it was explained that this program was for research, I was wondering if this was a ploy by the amplification device company to sell their product. I'm sure many people had the same thought and didn't participate in this even if they wanted to.” CP 002 | |
| Expansion of the program | There are a lot of older people that are hard of hearing, but there are also a fair amount of younger people with the same problems. Even in my case, my hearing problem started from a long time ago. PHL 001 |
Firstly, participants discussed impact of the program on themselves, family members, and their community. Emergent subthemes included: hearing benefit, improved confidence in hearing care navigation, and increased awareness of available listening devices and hearing health. One participant noted,
“The most important [change] is that I can hear things that I couldn't hear before. I've felt joy and hope … that I can hear anything I want to hear. I would recommend this program to anyone in my situation [with hearing loss]” PHL 001
Participants with hearing loss reported significant hearing benefit in many situations including social and religious gatherings and at work. These were situations in which they previously could not effectively hear CPs confirmed their partners’ hearing benefit by noting reduced TV volume at home and improved ease when conversing with their partners. Furthermore, CPs noted their own change in attitudes when dealing with the residual frustrating situations due to their partner’s hearing loss. In addition to the hearing benefit, participants expressed increased confidence in dealing with potential problems with their listening device and navigating the related hearing care system. Interestingly, participants discussed that the impact of the intervention was not solely limited to the older adults who participated in the program but rather, the impact also included their family and friends. One CP stated,
“Now that this program exists [in our community], people around me who didn't have any thoughts [on hearing loss] are getting interested, talking about it, and asking me questions about it, so I get to answer their questions.” CP 002
The community-delivered intervention has increased awareness of listening devices and hearing care among the broader social network of the participants.
Facilitators for program participation were discussed in the context of study enrollment and program components. Emergent subthemes were price, accessibility, face-to-face interaction, and group session. Participants reported that the affordability and accessibility of the program aided in their enrollment in the program. One older adult with hearing loss described the K-HEARS program that was offered in the community as a gateway to the standard hearing care that had been previously inaccessible.
“[In order to get a hearing test], I have to make a trip to an ENT clinic. Here [through the K-HEARS program] I can just stop by and get my hearing tested. I will go to an ENT clinic if I find something's wrong.” CP 003
In addition to the convenient location of the program, participants also appreciated accessibility to a reliable listening device provided through the program. Many participants also appreciated the face-to-face interaction with the interventionist throughout the intervention, which allowed the participants to easily and efficiently learn how to use the new listening device. The group follow-up session was discussed as another component of the intervention that has enhanced their learning through open discussions and social support.
Given that the number of hours of listening device use varied among the participants, we extensively discussed barriers to listening device use. Emergent subthemes include shame, sound and physical discomfort, and forgetfulness. Some participants who used the listening device selectively identified shame as a barrier to device use. Participants were often self-conscious about other people noticing them wearing the device. For example, one participant noted,
“I feel like the other person often feels that I'm being disrespectful or weird because I'm wearing this device.” PHL 007
Participants were well-aware of the stigma of hearing loss in their community, and subsequently the presence of the listening device, that is associated with aging and disability. Younger participants with hearing loss tended to express more shame towards wearing a noticeable device in social situations. Discomfort in the context of long hours of device use and noise was also identified as a barrier. Participants who reported physical discomfort tried to maximize the benefit from the device by using the device only in situations where they deemed it important to hear. Device feedback and loud background noise were other contributing factors for limited device use. Participants noted that they had taken the device off in settings where device feedback arose or where background noise was overwhelming, and subsequently forgot to put the device back on later.
As for plans for future studies, participants discussed different ways to raise program awareness and expand the program. Firstly, use of resources at church such as the weekly Sunday newsletter was emphasized. Participants stated that an advertisement through different churches in KA community would be an effective and efficient way to reach out to more KA older adults with hearing loss considering high rates of church attendance among older KAs. The cost for participating in the program, source of funding, and reliable affiliation were identified as the most important information that needed to be stated clearly and explicitly on the flyer to attract more participants, provided that older KAs are typically wary of commercial flyers. Participants agreed that the program would benefit many older KAs in similar situations once the program can be advertised to older adults in the community. One older adult with hearing loss stated,
“I hope this program can expand more. Have it be done more by the community, like welfare benefit, to reach out to the older population, including the older folks that live alone. I hope this can help more people.” CP 004
Given that older KAs share similar experiences of hearing loss and barriers that could be addressed by a culturally competent intervention, the older KAs in our study group supported expansion of the program to help additional older KAs by reaching out to more churches and KA senior centers. Further suggestions included expanding the eligibility criteria (e.g. include younger adults and those without an identifiable CP).
Discussion
To our knowledge, this is the first study to describe the cultural adaptation of a community-based hearing care intervention for older KAs. The adapted intervention incorporating the first four stages of Barrera and Castro’s cultural adaptation framework was well-accepted and feasible among the community-dwelling older KAs with hearing loss and their CPs.
The findings related to change in hearing handicap in our pilot trial demonstrated the potential impact of the adapted intervention on reducing hearing handicap. The improvement in mean scores in HHIE-S after the adapted intervention was comparable to changes in mean scores achieved with the original HEARS intervention and, most importantly, after standard-of-care hearing interventions including hearing aid fitting and cochlear implantation which range from 8 to 16 (Chisolm et al., 2007; Newman, Jacobson, Hug, Weinstein, & Malinoff, 1991; Vuorialho, Karinen, & Sorri, 2006). Further testing of the K- HEARS intervention is needed, including an appropriate control group to determine efficacy. At baseline, the measures in denial of hearing loss and negative associations with listening device use were higher among the KA study participants than the average scores from the previously published normative data of the Attitudes towards Loss of Hearing Questionnaire (ALHQ) (Saunders, Cienkowski, Forsline, & Fausti, 2005). There have been no previous studies in the literature exploring changes in scores of ALHQ after hearing treatment. In the current study, study participants demonstrated improved scores in most components of ALHQ including negative associations and negative coping strategies. In terms of social-emotional function and quality of life, the impact of the intervention on short-term outcomes was inconsistent as in previous studies (Acar, Yurekli, Babademez, Karabulut, & Karasen, 2011; Hickson, Meyer, Lovelock, Lampert, & Khan, 2014; Mulrow et al., 1990).
CPs were a vital component of the intervention where they systematically enhanced social support and allowed examination of the intervention’s impact on third-party disability. Inclusion of family and friends has been an effective strategy utilized by many aural rehabilitation programs (Hawkins, 2005) and health interventions targeting older adults (Brown et al., 2002; Irene J. Kim, 2006; Whittemore, 2007). We found trends toward improved third-party disability, improved social-emotional function, and improved mental component of quality of life among CPs after the intervention. During post-intervention interviews, many CPs noted increased awareness of age-related hearing loss and the effectiveness of communication strategies at home. Increased understanding of their partner’s hearing loss from the intervention may have changed their attitudes toward hearing loss from frustration to consideration. While the absence of a CP should not inhibit older adults with hearing loss from receiving hearing care, participation of family and friends in their aural rehabilitation process should be highly encouraged in the KA community.
K-HEARS was developed using a theory-driven model of cultural adaptation. Cultural adaptation has emerged as a promising intervention strategy in response to diversification of the American population and the growing demand to reach subcultural groups (Castro et al., 2010). Previously introduced interventions with cultural adaptation were effective in promoting many health behaviors and improving health disparities in diverse health conditions, including diabetes (Glazier, Bajcar, Kennie, & Willson, 2006; Hawthorne, Robles, Cannings-John, & Edwards, 2010), mammography use (H. R. Han et al., 2009), and HIV/AIDS (Darbes, Crepaz, Lyles, Kennedy, & Rutherford, 2008). Adapted interventions that were built upon theoretical foundations, using both quantitative and qualitative efforts (e.g. needs assessments, focus groups, and pilot studies) to validate the cultural appropriateness and efficacy, were more effective than unadapted interventions (Darbes et al., 2008). Hearing loss and its treatments involve diverse cultural health beliefs and varying degree of stigma associated with aging and disability, particularly in older KAs (Choi et al., 2018). Systematic cultural adaptation could be an effective way to capture and address the culture-specific hearing care beliefs among ethnic minorities.
Shame, discomfort, and forgetfulness were identified as remaining barriers to device use during post-intervention focus groups. Hearing loss is an invisible disability that is rarely brought up by either patients or health providers in KA community (Choi et al., 2018). There is a need for collective efforts from both the health professionals and the KA community to support of the idea of seeking help for hearing loss and to support the use of listening devices. It is also important to understand that hearing loss is a chronic health condition requiring long-term rehabilitative process involving regular listening device use and coping strategies (Laplante-Lévesque, Hickson, & Worrall, 2010). Actively involving the older adults in intervention decision making process and enhancing the expected management may improve the intervention uptake and adherence as in many chronic conditions (Barlow, Wright, Sheasby, Turner, & Hainsworth, 2002).
There are several limitations to this study. First, our study was a preliminary pilot study with a small cohort of older adults. Inference testing or statistical comparisons were not performed. Future studies must include a larger number of participants and a control group to test the efficacy and effectiveness of the adapted intervention as part of the final trial of the cultural adaptation framework. Second, participants were recruited in partnership with a Korean church, limiting the generalizability of the results to participants recruited in other faith-based or non-faith based organizations. However, nearly 80% of KAs are estimated to attend church, and the church setting has been identified as an optimal environment facilitating participation in health-related activities among KAs (Jo, Maxwell, Yang, & Bastani, 2010; Juon, Kim, Shankar, & Han, 2004; Ma, Shive, Wang, & Tan, 2009). Study participants were required to involve CPs, which may have limited participation of the older KAs without identifiable CP, and therefore, at particular risk for experiencing negative social-emotional consequences of hearing loss. In this study, participants mostly had mild to moderate hearing loss and our results may not be representative of the results from the participants with severe or profound hearing loss. Finally, the intervention including provision of a listening device and the education sessions was delivered to all study participants at no cost as part of the research study. Program participation and satisfaction with the device may be different with varying costs for participation.
In summary, our study suggests that K-HEARS, encompassing culturally-adapted hearing counseling and an affordable listening device, is a feasible intervention for older KAs with hearing loss. This community-based hearing care model may be an effective way to address poor access to hearing care among other racial/ethnic minorities with language and cultural barriers. With the coming changes in the regulation of hearing aids and the creation of over-the-counter hearing aids, models such as HEARS and K-HEARS are of particular importance in connecting older adults with the technology they need. The next step of research will need to include the final trial of the cultural adaptation framework to examine the efficacy and effectiveness of the adapted intervention, efforts to address the remaining barriers to listening device use, and to explore the sustainability and widespread implementation of a community-based intervention.
Supplementary Material
Figure 1.
Hearing Handicap Inventory for the Elderly (HHIE-S) scores at six weeks post-intervention versus baseline (n=15)
Acknowledgement:
We thank our program participants for taking the time to share their experiences.
Funding: This manuscript was supported in part by NIH K23DC011279 (FRL), R33DC015062 (FRL), T32DC000027 (CLN), the Eleanor Schwartz Charitable Foundation (FRL), a Triological Society/American College of Surgeons Clinician Scientist Award (FRL) and the Johns Hopkins Institute for Clinical and Translational Research (ICTR) which is funded in part by NIH TL1 TR001078 (JSC) from the National Center for Advancing Translational Sciences (NCATS). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the Johns Hopkins ICTR, NCATS or NIH.
Footnotes
Disclosures: FRL reimbursed travel to meetings from Cochlear Ltd and speaker honoraria from Triton Hearing and Caption Call. FRL reports being the director of the Johns Hopkins Cochlear Center for Hearing and Public Health that is funded in part by a philanthropic gift from Cochlear Ltd to the Johns Hopkins Bloomberg School of Public Health. FRL reports being a board member of AccessHEARS and the Health Sciences Policy Board at the National Academies. SKM reports have meeting expenses paid for by the Oticon Foundation.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- Acar B, Yurekli MF, Babademez MA, Karabulut H, & Karasen RM (2011). Effects of hearing aids on cognitive functions and depressive signs in elderly people. Arch Gerontol Geriatr, 52(3), 250–252. doi: 10.1016/j.archger.2010.04.013 [DOI] [PubMed] [Google Scholar]
- Bainbridge KE, & Ramachandran V (2014). Hearing aid use among older U.S. adults; the national health and nutrition examination survey, 2005-2006 and 2009-2010. Ear Hear, 35(3), 289–294. doi: 10.1097/01.aud.0000441036.40169.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A (1977). Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev, 84(2), 191–215. [DOI] [PubMed] [Google Scholar]
- Barlow J, Wright C, Sheasby J, Turner A, & Hainsworth J (2002). Self-management approaches for people with chronic conditions: a review. Patient Educ Couns, 48(2), 177–187. [DOI] [PubMed] [Google Scholar]
- Barnes DM (1996). An Analysis of the Grounded Theory Methods and the Concept of Culture. Qual Health Res, 6, 429–441. [Google Scholar]
- Barrera M Jr., Castro FG, Strycker LA, & Toobert DJ (2013). Cultural adaptations of behavioral health interventions: a progress report. J Consult Clin Psychol, 81(2), 196–205. doi: 10.1037/a0027085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SA, Garcia AA, Kouzekanani K, & Hanis CL (2002). Culturally competent diabetes self-management education for Mexican Americans: the Starr County border health initiative. Diabetes Care, 25(2), 259–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro FG, Barrera M Jr., & Holleran Steiker LK (2010). Issues and challenges in the design of culturally adapted evidence-based interventions. Annu Rev Clin Psychol, 6, 213–239. doi: 10.1146/annurev-clinpsy-033109-132032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control. (1997) Health People 2000 Review, 1995-96 National Center for Health statistics: Centers for Disease Control, National Center for Health Statistics. [Google Scholar]
- Chen DS, Betz J, Yaffe K, Ayonayon HN, Kritchevsky S, Martin KR, … Health, A. B. C. s. (2015). Association of hearing impairment with declines in physical functioning and the risk of disability in older adults. J Gerontol A Biol Sci Med Sci, 70(5), 654–661. doi: 10.1093/gerona/glu207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chisolm TH, Johnson CE, Danhauer JL, Portz LJ, Abrams HB, Lesner S, … Newman CW (2007). A systematic review of health-related quality of life and hearing aids: final report of the American Academy of Audiology Task Force On the Health-Related Quality of Life Benefits of Amplification in Adults. J Am Acad Audiol, 18(2), 151–183. [DOI] [PubMed] [Google Scholar]
- Choi JS, Shim KS, Kim K, Nieman CL, Mamo SK, Lin FR, & Han HR (2018). Understanding Hearing Loss and Barriers to Hearing Health Care Among Korean American Older Adults: A Focus Group Study. J Appl Gerontol, 37(11), 1344–1367. doi: 10.1177/0733464816663554 [DOI] [PubMed] [Google Scholar]
- Chu H, Cho Y-S, Park S-N, Byun JY, Shin JE, Han GC, … Jung JY (2012). Standardization for a Korean Adaptation of the International Outcome Inventory for Hearing Aids: Study of Validity and Reliability. Korean J Otorhinolaryngol-Head Neck Surg, 55, 20–25. [Google Scholar]
- Darbes L, Crepaz N, Lyles C, Kennedy G, & Rutherford G (2008). The efficacy of behavioral interventions in reducing HIV risk behaviors and incident sexually transmitted diseases in heterosexual African Americans. AIDS, 22(10), 1177–1194. doi: 10.1097/QAD.0b013e3282ff624e [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisk AD, Rogers WA, Charness N, Czaja SJ, & Sharit J (2009). Designing for older adults: Principles and creative human factors approaches: CRC press. [Google Scholar]
- Glazier RH, Bajcar J, Kennie NR, & Willson K (2006). A systematic review of interventions to improve diabetes care in socially disadvantaged populations. Diabetes Care, 29(7), 1675–1688. doi: 10.2337/dc05-1942 [DOI] [PubMed] [Google Scholar]
- Hall DA, Zaragoza Domingo S, Hamdache LZ, Manchaiah V, Thammaiah S, Evans C, … NETwork, T. I. R. (2018). A good practice guide for translating and adapting hearing-related questionnaires for different languages and cultures. Int J Audiol, 57(3), 161–175. doi: 10.1080/14992027.2017.1393565 [DOI] [PubMed] [Google Scholar]
- Han C, Ahn S. m., JH;, K., CU;, P., D.;, S., I.;, J., & MH;, P. (2008). Validation of the Patient Health Questionnaire-9 Korean version in the elderly population: the Ansan Geriatric study. Comprehensive Psychiatry, 49, 218–223. [DOI] [PubMed] [Google Scholar]
- Han HR, Lee JE, Kim J, Hedlin HK, Song H, & Kim MT (2009). A meta-analysis of interventions to promote mammography among ethnic minority women. Nurs Res, 58(4), 246–254. doi: 10.1097/NNR.0b013e3181ac0f7f [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins DB (2005). Effectiveness of counseling-based adult group aural rehabilitation programs: a systematic review of the evidence. J Am Acad Audiol, 16(7), 485–493. [DOI] [PubMed] [Google Scholar]
- Hawthorne K, Robles Y, Cannings-John R, & Edwards AG (2010). Culturally appropriate health education for Type 2 diabetes in ethnic minority groups: a systematic and narrative review of randomized controlled trials. Diabet Med, 27(6), 613–623. doi: 10.1111/j.1464-5491.2010.02954.x [DOI] [PubMed] [Google Scholar]
- Hickson L, Meyer C, Lovelock K, Lampert M, & Khan A (2014). Factors associated with success with hearing aids in older adults. Int J Audiol, 53 Suppl 1, S18–27. doi: 10.3109/14992027.2013.860488 [DOI] [PubMed] [Google Scholar]
- Hsieh HF, & Shannon SE (2005). Three approaches to qualitative content analysis. Qual Health Res, 15(9), 1277–1288. doi: 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- Irene J Kim LK, Kelly James G.. (2006). Developing cultural competence in working with Korean immigrant families. Journal of Community Psychology, 342, 149–165. [Google Scholar]
- Islam NS, Zanowiak JM, Wyatt LC, Chun K, Lee L, Kwon SC, & Trinh-Shevrin C (2013). A randomized-controlled, pilot intervention on diabetes prevention and healthy lifestyles in the New York City Korean community. J Community Health, 38(6), 1030–1041. doi: 10.1007/s10900-013-9711-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jo AM, Maxwell AE, Yang B, & Bastani R (2010). Conducting health research in Korean American churches: perspectives from church leaders. J Community Health, 35(2), 156–164. doi: 10.1007/s10900-009-9213-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juon H-S, Kim M, Shankar S, & Han W (2004). Predictors of adherence to screening mammography among Korean American women. Preventive Medicine, 393, 474–481. [DOI] [PubMed] [Google Scholar]
- Kim OS (1997). Korean Version of the Revised UCLA Lonliness Scale: Reliability and Validity Test. Journal of Korean Academy of Nursing, 871–879. [Google Scholar]
- Kim Y, Won C, Kim B, Choi H, Kim S, Kim J, & Lim J (2001). Usability of HHIE S as a screening test of hearing imairment in the Korean elderly. J Korean Acad Fam Med, 22 (6), 878–885. [Google Scholar]
- Knudsen LV, Laplante-Lévesque A, Jones L, Preminger JE, Nielsen C, Lunner T, … Kramer SE (2012). Conducting qualitative research in audiology: a tutorial. Int J Audiol, 51(2), 83–92. doi: 10.3109/14992027.2011.606283 [DOI] [PubMed] [Google Scholar]
- Knudsen LV, Öberg M, Nielsen C, Naylor G, & Kramer SE (2010). Factors influencing help seeking, hearing aid uptake, hearing aid use and satisfaction with hearing aids: a review of the literature. Trends Amplif, 14(3), 127–154. doi: 10.1177/1084713810385712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korea Centers for Disease Control and Prevention. (2010). Health Statistics 2009: Korea National Health and Nutrition Examination Survey (KNHANES IV-3). Retrieved from http://knhanes.cdc.go.kr/knahnes/index.do
- Laplante-Lévesque A, Hickson L, & Worrall L (2010). Rehabilitation of older adults with hearing impairment: a critical review. J Aging Health, 22(2), 143–153. doi: 10.1177/0898264309352731 [DOI] [PubMed] [Google Scholar]
- Lichtenstein MJ, Bess FH, & Logan SA (1988). Diagnostic performance of the hearing handicap inventory for the elderly (screening version) against differing definitions of hearing loss. Ear Hear, 9(4), 208–211. [DOI] [PubMed] [Google Scholar]
- Lin FR, & Albert M (2014). Hearing loss and dementia - who is listening? Aging Ment Health, 18(6), 671–673. doi: 10.1080/13607863.2014.915924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin FR, Metter EJ, O'Brien RJ, Resnick SM, Zonderman AB, & Ferrucci L (2011). Hearing loss and incident dementia. Arch Neurol, 68(2), 214–220. doi: 10.1001/archneurol.2010.362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin FR, Niparko JK, & Ferrucci L (2011). Hearing loss prevalence in the United States. Arch Intern Med, 171(20), 1851–1852. doi: 10.1001/archinternmed.2011.506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin FR, Thorpe R, Gordon-Salant S, & Ferrucci L (2011). Hearing loss prevalence and risk factors among older adults in the United States. J Gerontol A Biol Sci Med Sci, 66(5), 582–590. doi: 10.1093/gerona/glr002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston G, Sommerlad A, Orgeta V, Costafreda SG, Huntley J, Ames D, … Cohen-Mansfield J (2017). Dementia prevention, intervention, and care. The Lancet, 390(10113), 2673–2734. [DOI] [PubMed] [Google Scholar]
- Ma GX, Shive SE, Wang MQ, & Tan Y (2009). Cancer screening behaviors and barriers in Asian Americans. Am J Health Behav, 33(6), 650–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamo SK, Nieman CL, & Lin FR (2016). Prevalence of Untreated Hearing Loss by Income among Older Adults in the United States. J Health Care Poor Underserved, 27(4), 1812–1818. doi: 10.1353/hpu.2016.0164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mener DJ, Betz J, Genther DJ, Chen D, & Lin FR (2013). Hearing loss and depression in older adults. J Am Geriatr Soc, 61(9), 1627–1629. doi: 10.1111/jgs.12429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer C, Hickson L, Lovelock K, Lampert M, & Khan A (2014). An investigation of factors that influence help-seeking for hearing impairment in older adults. Int J Audiol, 53 Suppl 1, S3–17. doi: 10.3109/14992027.2013.839888 [DOI] [PubMed] [Google Scholar]
- Mick P, Kawachi I, & Lin FR (2014). The association between hearing loss and social isolation in older adults. Otolaryngol Head Neck Surg, 150(3), 378–384. doi: 10.1177/0194599813518021 [DOI] [PubMed] [Google Scholar]
- Mulrow CD, Aguilar C, Endicott JE, Tuley MR, Velez R, Charlip WS, … DeNino LA (1990). Quality-of-life changes and hearing impairment. A randomized trial. Ann Intern Med, 113(3), 188–194. [DOI] [PubMed] [Google Scholar]
- Nam WH, Park KM Lim EJ, Kim YH Sin CM Lee HW, & Kim JS (2007). Correlation Analysis between SF36 and Polysomnographic Measures in Patients with OSAS. Korean J Otorhinolaryngol-Head Neck Surg, 50, 896–902. [Google Scholar]
- National Evidence-Based Healthcare Collaborating Agency. (2011). 난청환자의 국내 보청기 사용 효과성과 장애요인 분석 [Effectiveness of Hearing Aids use among Patients with Hearing Impairment and Disability Factors in Korea] Retrieved from http://www.neca.re.kr/center/researcher/report_view.jsp?boardNo=GA&seq=40&q=626f6172644e6f3d4741
- Newman CW, Jacobson GP, Hug GA, Weinstein BE, & Malinoff RL (1991). Practical method for quantifying hearing aid benefit in older adults. J Am Acad Audiol, 2(2), 70–75. [PubMed] [Google Scholar]
- Nieman CL, & Lin FR (2017). Increasing access to hearing rehabilitation for older adults. Curr Opin Otolaryngol Head Neck Surg, 25(5), 342–346. doi: 10.1097/MOO.0000000000000386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nieman CL, Marrone N, Mamo SK, Betz J, Choi JS, Contrera KJ, … Lin FR (2017). The Baltimore HEARS Pilot Study: An Affordable, Accessible, Community-Delivered Hearing Care Intervention. Gerontologist, 57(6), 1173–1186. doi: 10.1093/geront/gnw153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osuna D, Barrera M Jr., Strycker LA, Toobert DJ, Glasgow RE, Geno CR, … Doty AT (2011). Methods for the cultural adaptation of a diabetes lifestyle intervention for Latinas: an illustrative project. Health Promot Pract, 12(3), 341–348. doi: 10.1177/1524839909343279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S-N, Han GC, Cho Y-S, Byun JY, Shin JE, Chu H-S, … Choi JY (2011). Standardization for a Korean Version of Hearing Handicap Inventory for the Elderly. Korean J Otorhinolaryngol-Head Neck Surg, 54, 828–834. [Google Scholar]
- President's Council of Advisors on Science and Technology. (2015). Aging america & hearing loss: Imperative of improved hearing technologies. Retrieved from https://www.whitehouse.gov/sites/default/files/microsites/ostp/PCAST/pcast_hearing_tech_letterreport_final.pdf
- Saunders GH, & Cienkowski KM (1996). Refinement and psychometric evaluation of the Attitudes Toward Loss of Hearing Questionnaire. Ear Hear, 17(6), 505–519. [DOI] [PubMed] [Google Scholar]
- Saunders GH, Cienkowski KM, Forsline A, & Fausti S (2005). Normative data for the Attitudes towards Loss of Hearing Questionnaire. J Am Acad Audiol, 16(9), 637–652. [DOI] [PubMed] [Google Scholar]
- Scarinci N, Worrall L, & Hickson L (2009). The effect of hearing impairment in older people on the spouse: development and psychometric testing of the significant other scale for hearing disability (SOS-HEAR). Int J Audiol, 48(10), 671–683. doi: 10.1080/14992020902998409 [DOI] [PubMed] [Google Scholar]
- Shahid EMHSRMOKH (2012). The Asian Population: 2010 Retrieved from https://www.census.gov/prod/cen2010/briefs/c2010br-11.pdf
- Strom K (2014). Hearing Review 2013 dispenser survey: dispensing in the age of internet and big box retailers. Hear Rev, 21(4), 22–28. [Google Scholar]
- Suh EE, Kagan S, & Strumpf N (2009). Cultural competence in qualitative interview methods with Asian immigrants. J Transcult Nurs, 20(2), 194–201. doi: 10.1177/1043659608330059 [DOI] [PubMed] [Google Scholar]
- The American Geriatrics Society Ethnogeriatrics Committee. (2016). Achieving High-Quality Multicultural Geriatric Care. J Am Geriatr Soc, 64(2), 255–260. doi: 10.1111/jgs.13924 [DOI] [PubMed] [Google Scholar]
- The National Academies of Sciences Engineering and Medicine. (2016). Hearing Health Care for Adults: Priorities for Improving Access and Affordability. Retrieved from http://nationalacademies.org/hmd/reports/2016/Hearing-Health-Care-for-Adults.aspx [PubMed]
- Thomas DR (2006). A general inductive approach for analyzing qualitative evaluation data. American journal of evaluation, 27(2), 237–246. [Google Scholar]
- Ventry IM, & Weinstein BE (1983). Identification of elderly people with hearing problems. ASHA, 25(7), 37–42. [PubMed] [Google Scholar]
- Vuorialho A, Karinen P, & Sorri M (2006). Effect of hearing aids on hearing disability and quality of life in the elderly. Int J Audiol, 45(7), 400–405. doi: 10.1080/14992020600625007 [DOI] [PubMed] [Google Scholar]
- Whittemore R (2007). Culturally competent interventions for Hispanic adults with type 2 diabetes: a systematic review. J Transcult Nurs, 18(2), 157–166. doi: 10.1177/1043659606298615 [DOI] [PubMed] [Google Scholar]
- Yueh B, Souza PE, McDowell JA, Collins MP, Loovis CF, Hedrick SC, … Deyo RA (2001). Randomized trial of amplification strategies. Arch Otolaryngol Head Neck Surg, 127(10), 1197–1204. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.