Abstract
Cognitive-behavioral therapy (CBT) can improve anxiety and depression in autistic adults, but few autistic adults receive this treatment. We examined factors that may influence clinicians’ use of CBT with autistic adults. One hundred clinicians completed an online survey. Clinicians reported stronger intentions (p = .001), more favorable attitudes (p < .001), greater normative pressure (p < .001), and higher self-efficacy (p < .001) to start CBT with non-autistic adults than with autistic adults. The only significant predictor of intentions to begin CBT with clients with anxiety or depression was clinicians’ attitudes (p < .001), with more favorable attitudes predicting stronger intentions. These findings are valuable for designing effective, tailored implementation strategies to increase clinicians’ adoption of CBT for autistic adults.
Keywords: adults, autism spectrum disorder, cognitive-behavioral therapy, community mental health, implementation science, theory of planned behavior
Autistic adults have high rates of anxiety and depression (Buck et al., 2014; Croen et al., 2015), and often do not receive quality mental health care for these or other co-occurring conditions (Maddox et al., 2019; Roux, Shattuck, Rast, Rava, & Anderson, 2015; Shattuck, Wagner, Narendorf, Sterzing, & Hensley, 2011). Developing strategies to address co-occurring psychiatric conditions is a high research priority for stakeholders in the autistic community (Frazier et al., 2018; Pellicano, Dinsmore, & Charman, 2014). Recent research suggests that cognitive-behavioral therapy (CBT) is effective at treating anxiety and depression in autistic adults (Spain, Sin, Chalder, Murphy, & Happé, 2015), but many autistic adults do not receive CBT (Roux et al., 2015). This study examined factors that may influence community mental health clinicians’ use of CBT with autistic adults with co-occurring anxiety or depression. Identifying factors that influence clinicians’ use of CBT is crucial for developing mental health services and clinician training programs for autistic adults. The current study focuses on CBT because 1) CBT is a well-established evidence-based treatment for anxiety and depression among adults in the general population, making it the “current gold standard of psychotherapy” (David, Cristea, & Hofmann, 2018, p. 1), and 2) CBT is the most studied and supported psychosocial treatment for anxiety and depression in autistic adults (Weiss & Lunsky, 2010; White et al., 2018).
Few studies have examined reasons why mental health clinicians who work with – or could work with – autistic adults may or may not use CBT with this population. Cooper, Loades, and Russell (2018) surveyed 50 therapists in the UK about their experiences adapting CBT for autistic clients (of any age) and their confidence working with this population. An important study limitation is that the survey respondents were recruited through a training workshop about adapting CBT for autistic people. In this self-selected sample, 64% of therapists had not received prior training on working with autistic clients. On average, they reported feeling moderately confident about using their core therapeutic skills with autistic people (i.e., being empathetic, developing a therapeutic relationship, and gathering information from an autistic client to understand his or her difficulties), and reported less confidence in using other key skills, such as identifying effective therapeutic approaches for autistic clients and using their knowledge of mental health treatments to help autistic clients. However, this study did not test which factors influence the therapists’ intention to use CBT or actual use of CBT with their autistic clients.
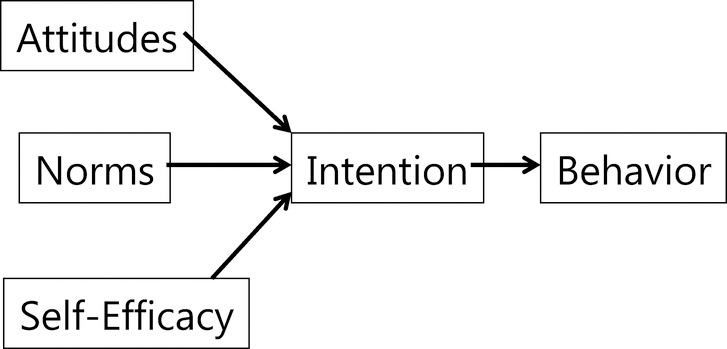
How can we increase clinicians’ use of CBT with autistic adult clients who present with anxiety or depression? To explore this question, we applied the theory of planned behavior (TPB; Ajzen, 1991), a leading causal model of behavior change. The TPB posits that an individual’s attitudes, perceived norms, and/or self-efficacy influence intentions to perform a behavior, and that intentions predict behavior, under circumstances that permit the individual to act (Figure 1). While the TPB has been used to predict and understand many health-related behaviors (Armitage & Conner, 2001), it has only recently been applied to the implementation of evidence-based practices for autistic children in community settings (Fishman, Beidas, Reisinger, & Mandell, 2018; Fishman et al., 2019; Ingersoll, Straiton, Casagrande, & Pickard, 2018). For example, Fishman and colleagues (2018) found that autism support classroom teachers’ intentions to use visual schedules with their students strongly predicted their subsequent use of this evidence-based practice. These findings highlight the value of measuring intentions to use specific practices.
Figure 1.
The proximal determinants of intention and behavior, as defined by the theory of planned behavior (Ajzen, 1991).
The present study is the first to assess TPB constructs in the context of community mental health clinicians providing CBT to autistic adults with co-occurring anxiety or depression. Specifically, we measured community mental health clinicians’ intention, or motivation, to start CBT with their autistic adult clients with co-occurring anxiety or depression, and four potential determinants of this intention (described below): attitudes, descriptive norms, injunctive norms, and self-efficacy towards starting CBT with autistic adults with co-occurring anxiety or depression. To determine whether these associations were specific to working with autistic adults, we also asked about clinicians’ intentions and potential determinants of intentions to start CBT with non-autistic adult clients with anxiety or depression. For the current study, intention to start CBT is a more appropriate outcome than the actual use of CBT with autistic adults because many community mental health clinicians have few to no autistic clients on their caseload and lack training in autism (Maddox et al., 2019). In the TPB, intentions are the most proximal determinant of behavior (Fishbein & Ajzen, 2010). Thus, understanding clinicians’ intentions to use a specific evidence-based practice can directly inform future efforts to change clinician behavior and address barriers to treatment access (Fishman et al., 2018; Moullin, Ehrhart, & Aarons, 2018).
In this study, attitudes refer to the clinicians’ perceptions of the advantages and disadvantages of starting CBT with their adult clients with co-occurring anxiety or depression. Normative pressure refers to the clinicians’ perceptions of what others like them do (descriptive norms) and what others expect them to do (injunctive norms) when offering anxiety or depression treatment with an adult client. Self-efficacy (also called perceived behavioral control) refers to the clinicians’ sense of agency to start CBT with an adult client. One advantage of considering these factors is that they are malleable and could be targeted with tailored implementation strategies to improve implementation of evidence-based practice (Fishman et al., 2019). However, it is important to note that these factors are only a small subset of possible barriers to clinicians delivering CBT to autistic adults. For example, we do not examine financial or funding issues, agency leadership engagement, implementation climate, organizational policies, or characteristics of the clients (Damschroder et al., 2009). The current study represents a first step in better understanding the research-to-practice gap related to mental health services for autistic adults.
Methods
Procedures
The University of Pennsylvania’s Institutional Review Board approved the study procedures. Participants completed a confidential online survey, which took approximately 15 minutes. We described the purpose of the study as learning about clinicians’ opinions about outpatient therapy methods. We did not mention autism in the study description, in hopes that clinicians with little to no experience with autistic clients would participate. We recruited clinicians who work with adults through an email message sent from two professional membership organizations that collectively represent more than 70 independent community mental health agencies in Southeastern Pennsylvania. These agencies serve a large proportion of Medicaid recipients and often treat clinically complex clients, meaning individuals who present with serious mental illness (e.g., psychosis), chronic mental health problems, and multiple co-occurring conditions (Community Behavioral Health, 2017). Many of these agencies have participated in Philadelphia’s behavioral health transformation effort, which includes a number of system-wide CBT initiatives (Powell et al., 2016). These initiatives include ongoing training, consultation, and technical assistance for clinicians to deliver CBT. However, these CBT initiatives have not focused on ASD or included any training about working with autistic clients.
All participants accessed the survey through a secure web link. Participants indicated consent prior to beginning the survey at the bottom of the first page, which included details about participating in the study. Participants received a $20 gift card upon completion of the survey. We collected survey responses from March to June 2018.
Survey Measures
TPB constructs
We measured clinicians’ intentions to start CBT with adult clients who present for anxiety or depression treatment. We also measured their attitudes, norms, and self-efficacy about starting CBT with adult clients who present for anxiety or depression treatment. Survey participants first answered these questions about adult clients in general, and then the questions were repeated asking participants to think about autistic clients who present for anxiety or depression treatment. The questions about non-autistic clients appeared first, as to not bias respondents toward thinking about autistic clients. The example questions below show the general question format (i.e., without specifying autistic clients).
We followed standardized procedures from social psychology for measuring intentions, attitudes, norms, and self-efficacy and adapted them for our specific research question about starting CBT for anxiety or depression (Fishbein & Ajzen, 2010). This standardized approach encourages a fairly specific definition of the behavior of interest, which is why we selected “start CBT,” rather than more general language such as “use CBT” or “provide CBT.” For each construct, we relied on item stems that are designed for modification to any target behavior. Other studies have adapted these stems and shown adequate to excellent psychometric properties (Fishbein & Ajzen, 2010; Fishman et al., 2019).
Intentions were measured by asking clinicians: “How likely is it that you will start CBT with each of your adult clients who present for anxiety or depression treatment?” The response options used a seven-point scale ranging from “extremely unlikely” to “extremely likely,” with higher scores representing stronger intentions.
Attitudes towards starting CBT with adult clients who present for anxiety or depression treatment were measured with standard semantic differential scales (Fishbein & Ajzen, 2010), which use opposite adjective pairs (e.g., bad-good) to anchor the evaluative dimensions. Respondents rated the unfavorable-favorableness of starting CBT with adult clients who present for anxiety or depression treatment using six dimensions (rated 0–10), such as those ranging from “unpleasant” to “pleasant” and from “useless” to “effective.” In the current sample, the scale had high internal consistency for the questions about clients with and without autism (α = .97 and .96, respectively). The total scale score was computed by averaging all items, where the higher the score, the more favorable the attitude.
Norms were measured using standard item stems about two types of normative pressure: the clinicians’ perceptions that other people like them start CBT with adult clients who present for anxiety or depression treatment (descriptive norm), and that other people important to them will approve of them starting CBT with adult clients who present for anxiety or depression treatment (injunctive norm). One item reflecting descriptive norms asked respondents to rate the degree to which they agreed or disagreed with the statement that “most clinicians like me will start CBT with adult clients who present for anxiety or depression treatment.” Respondents used a five-point scale ranging from “strongly disagree” to “strongly agree.” There were three statements used to measure injunctive norms, reflecting the perceived approval of other clinicians, the respondent’s supervisor, and the respondent’s adult clients with anxiety or depression. Respondents were asked: “How much would each of these groups disapprove or approve if you start CBT with your adults clients who present for anxiety or depression treatment?” For each of the three groups (other clinicians, supervisor, and adult clients with anxiety or depression), respondents used a five-point scale ranging from “strongly disapprove” to “strongly approve.” The total injunctive norms score was computed by averaging all three items. In the current sample, the scale had adequate internal consistency for the questions about clients with and without autism (α = .79 and .80, respectively). For both descriptive and injunctive norms, higher scores indicate greater normative pressure.
Self-efficacy was measured through responses to two statements on a five-point scale measuring clinicians’ perceptions of themselves as having the ability to start CBT with adult clients who present for anxiety or depression treatment. For example, respondents used a scale ranging from “strongly disagree” to “strongly agree” to rate their agreement with the statement: “I have the skills needed to start CBT with my adult clients who present for anxiety or depression treatment.” The total scale score was computed by averaging both items, with higher scores reflecting higher self-efficacy. In the current sample, the scale had acceptable internal consistency for the questions about clients with and without autism (α = .63 and .52, respectively).
Clinician Background
The survey ended with a brief section on clinicians’ background. Respondents reported demographic characteristics, including age, race/ethnicity, and gender, as well as professional characteristics, such as educational background, years passed since earning highest degree, staff/trainee status, and primary theoretical orientation. They also indicated the number of autistic adult clients on their caseload, both currently and previously, whether they had ever received formal training about working with autistic adults, and how likely they would be to attend a specific training in mental health interventions for autistic adults if offered through their agency. We adapted these autism background questions from a survey for community mental health clinicians serving autistic children (Brookman-Frazee, Drahota, Stadnick, & Palinkas, 2012).
Participants
One hundred twenty clinicians started the survey and 100 completed it. Because the demographic questions appeared at the end of the survey, we could not compare people with and without missing data on demographic variables. Table 1 provides demographic information about the final sample (n = 100). The majority of clinicians had their Master’s degree in social work or counseling. Participants shared similar demographics with community mental health clinicians from previous research in Philadelphia (e.g., Beidas et al., 2015). Participant demographics also broadly match national demographics of mental health clinicians, with regard to gender and race/ethnicity (Salsberg et al., 2017).
Table 1.
Clinician Characteristics (n = 100)
| Clinician frequency % or mean (SD) | |
|---|---|
| Sex | |
| Female | 82% |
| Male | 18% |
| Agea | 35.58 (12.51) |
| Hispanic/Latino | 7% |
| Race/ethnicity | |
| Alaska Native | 1% |
| American Indian | 2% |
| Asian | 5% |
| Black/African American | 9% |
| Middle Eastern | 1% |
| White | 79% |
| Multiracial | 3% |
| Educational background | |
| Bachelor’s degree | 6% |
| Master’s degree | 83% |
| Doctoral degree | 11% |
| Years since highest degree | 6.32 (9.42) |
| Licensed | 37% |
| Fee-for-service provider | 37% |
| Trainee | 30% |
| Theoretical orientationb | |
| Cognitive-behavioral | 62% |
| Eclectic | 31% |
| Humanistic | 22% |
| Family systems | 20% |
| Psychodynamic | 19% |
| Other | 6% |
| Currently treating an autistic adult | 30% |
| Has ever treated an autistic adult | 60% |
| Received formal training on autistic adults | 24% |
| Desire training in treating autistic adults | 96% |
One participant did not report age.
Participants could select more than one response.
Analyses
Data were analyzed with IBM SPSS Statistics Version 24. First, we calculated descriptive statistics for participant characteristics, intentions, attitudes, norms, and self-efficacy. Based on our interest in “strong” versus “weak” intentions to start CBT, we also dichotomized the intentions variables to report the percentage of strong intenders. Second, we used paired sample t-tests to compare clinicians’ mean ratings for clients with and without autism. Third, we used two separate regression models to test whether attitudes, descriptive norms, injunctive norms, and self-efficacy predicted intentions to start CBT with 1) non-autistic clients who present for anxiety or depression treatment and 2) autistic clients who present for anxiety or depression treatment. We included socio-demographic variables in the regression models as covariates. Covariates for each model were chosen by identifying socio-demographic variables correlated with the dependent variable, intentions, at p < 0.2. For the general (i.e., not autism specific) model, gender, age, licensure status, staff/contractor status, and trainee status showed associations with intentions to start CBT at p < .2 and were therefore included as covariates. For the autism model, age and staff/contractor status were associated with intentions to start CBT at p < .2 and were included as covariates.
Results
Table 1 provides information about the clinicians who completed the survey. Most respondents (70%) indicated that they had no autistic adults currently on their caseload, and most (76%) had not received any formal training (e.g., CE workshop, graduate school coursework) in working with autistic adults.
Table 2 summarizes the range and average ratings for intentions, attitudes, norms, and self-efficacy. For each of these constructs, clinicians reported higher ratings for starting CBT with clients without autism, compared to autistic clients. For intentions, more than half (52%) of the participants indicated they were “quite likely” or “extremely likely” to start CBT with clients without autism, whereas only 20% responded the same for clients on the spectrum. Clinicians reported stronger intentions (p = .001, d = .34), more favorable attitudes (p < .001, d = .69), greater descriptive normative pressure (p < .001, d = .39), greater injunctive normative pressure (p < .001, d = .66), and higher self-efficacy (p < .001, d = .81) to start CBT with non-autistic adults than with autistic adults.
Table 2.
Descriptive Statistics and Within-Group Comparisons of Intentions, Attitudes, Norms, and Self-Efficacy Related to Starting Cognitive-Behavioral Therapy with Adult Clients (with and without Autism) who Present for Anxiety or Depression Treatment
| Clients without autism | Autistic clients | |
|---|---|---|
| Variable | Mean (SD), range | Mean (SD), range |
| Intentions** | 4.92 (1.92), 1–7 | 4.22 (1.35), 2–7 |
| Attitudes*** | 7.27 (2.15), .5–10 | 5.90 (2.08), 0–10 |
| Descriptive norms*** | 3.45 (.86), 1–5 | 3.04 (.72), 1–5 |
| Injunctive norms*** | 3.86 (.73), 1.33–5 | 3.37 (.64), 1.33–5 |
| Self-efficacy*** | 3.88 (.62), 2–5 | 3.28 (.75), 1–5 |
Note. **p < .01, ***p < .001 for paired sample t-test analyses. Higher scores indicate stronger intentions, more favorable attitudes, greater normative pressure, and higher self-efficacy.
Table 3 provides the results of the two regression models predicting intentions to start CBT with 1) non-autistic clients who present for anxiety or depression treatment and 2) autistic clients who present for anxiety or depression treatment. The only significant predictor in both models was clinicians’ attitudes towards starting CBT (p < .001), with more favorable attitudes predicting stronger intentions.
Table 3.
Regression Models Predicting Intentions to Start Cognitive-Behavioral Therapy with Adult Clients who Present for Anxiety or Depression Treatment
| Clients without autism | Autistic clients | |||
|---|---|---|---|---|
| Variable | B | p | B | P |
| Attitudes | .40 | < .001 | .61 | < .001 |
| Descriptive norms | .07 | .59 | .17 | .07 |
| Injunctive norms | .16 | .30 | −.06 | .60 |
| Self-efficacy | .07 | .47 | .07 | .49 |
| Clinician age (years) | −.11 | .25 | −.15 | .06 |
| Clinician gender (0 = male, 1 = female) | .04 | .64 | N/A | N/A |
| Licensure status (0 = not licensed, 1 = licensed) | −.12 | .21 | N/A | N/A |
| Staff/contractor status (0 = staff, 1 = contractor) | −.01 | .93 | −.04 | .64 |
| Trainee status (0 = not a trainee; 1 = trainee) | −.16 | .15 | N/A | N/A |
Note. Adjusted R2 = .36 for general model (not autism specific). Adjusted R2 = .51 for autism model. Statistically significant findings at p < .001 are in bold.
Discussion
This study is one of the first to examine which factors may influence the use of CBT among community mental health clinicians when treating autistic adults with anxiety or depression. To better understand why clinicians may or may not start CBT with an autistic adult client who presents for anxiety or depression treatment, we examined intentions, attitudes, norms, and self-efficacy. Clinicians reported stronger intentions, more favorable attitudes, greater descriptive normative pressure, greater injunctive normative pressure, and higher self-efficacy for starting CBT with non-autistic clients who present for anxiety or depression treatment, than for autistic clients. These differences are not surprising given clinicians’ limited autism training and limited direct experience treating autistic adults, which could lead to misconceptions about autistic adults. These underlying beliefs about how autism presents in adults likely contribute to the clinicians’ reported intentions, attitudes, norms, and self-efficacy. For example, in our qualitative study, several community mental health clinicians spoke about all autistic adults having intellectual disability or aggressive behaviors, and therefore doubted whether they could use CBT with autistic adults (Maddox et al., 2019). Although CBT is certainly not an appropriate treatment option for all adults on the autism spectrum, it could be an effective treatment for many autistic adults who seek outpatient psychotherapy for anxiety or depression (Spain et al., 2015).
An unexpected finding is that clinicians’ intentions to start CBT for anxiety or depression with their clients without autism were not strong, with an average rating between “not sure” and “slightly likely,” despite a solid evidence base for this treatment modality (e.g., Beacon & Abramowitz, 2004; Cuijpers et al., 2013; DiMauro, Domingues, Fernandez, & Tolin, 2013). Most participants endorsed “cognitive-behavioral” for their theoretical orientation, although we do not know how much training they have received in CBT. It also is possible that high endorsement of a cognitive-behavioral orientation could reflect a social desirability bias, but if so, it is unclear why respondents would report relatively low intentions to start using it. Future research could investigate whether training clinicians to deliver CBT to autistic adults has any positive carryover effects, meaning that clinicians also increase their intention to use and frequency of use of CBT in sessions with adults without autism who present for anxiety or depression treatment.
According to the TPB, attitudes, norms, and self-efficacy can each predict intentions to perform a certain behavior, and the extent to which each does or does not must be empirically determined for each behavior and population of interest (Ajzen, 1991). In this study, more favorable attitudes predicted stronger intentions to start CBT, for both clients with and without autism. Knowing that clinicians’ attitudes strongly predicted intentions is valuable for designing effective, tailored implementation strategies to increase clinicians’ adoption of CBT for autistic adults. For example, an implementation strategy targeting attitudes could include message content to change beliefs about the perceived advantages and disadvantages of using CBT with autistic adults. Social psychologists have successfully developed messages that change attitudes about complex behaviors, which has strengthened intention and modified behavior (Fishbein & Ajzen, 2010). Since attitudes also explained variance in intention to start CBT with clients without autism, future research could investigate whether a message can be developed to change attitudes towards using CBT with both groups.
Limitations and Future Directions
Several study limitations should be noted. The survey was conducted in a Northeastern urban area, and findings may not be generalizable to other states or countries. In addition, the findings may not generalize to other agencies, particularly those outside a publicly funded system contracted to deliver CBT (Powell et al., 2016). Clinicians who self-selected to complete the survey may not represent the larger clinician population. Given our goal to keep the survey brief, we did not assess clinicians’ knowledge about the evidence base for CBT and other treatments, and we did not ask about their intentions to start other types of treatment with autistic adults. Because the background information section appeared at the end of the survey, we could not compare clinicians with and without missing data on demographic variables. Some constructs specified by the TPB model (i.e., intention and descriptive norms) were measured with a single item, due to concerns about participant burden. However, previous studies have successfully used one item to measure TPB constructs (e.g., Fishman et al., 2019, Ingersoll et al., 2018). Finally, we compared only two groups of clients: autistic adults and typically developing adults. Future research could investigate how clinicians’ intentions and attitudes about starting CBT may differ for clients with intellectual disability, other developmental disabilities, or multiple co-occurring psychiatric conditions to determine whether our findings are unique to autistic adults.
Longitudinal studies are needed to test whether intentions predict clinicians’ use of CBT with autistic adults who present for anxiety or depression treatment. Measuring the use of CBT was not a priority for the current study because most clinicians were not trained to and/or did not have the opportunity to deliver CBT to autistic adults, so it would be an unfair comparison between clients with and without autism. Our team is currently preparing to pilot test a clinician training program based on the findings from this study and our qualitative study (Maddox et al., 2019). One challenge is that many community mental health clinicians do not currently have an autistic adult on their caseload, which could limit the real-time practice of skills learned in a training program. It also is important to highlight that clinician training alone is likely insufficient to produce meaningful and sustainable improvement in mental healthcare for autistic adults. We need to examine other implementation strategies as well, including those aimed at the organization- or systems-level (Maddox et al., 2019). In addition, future research could explore which mental health treatment strategies are clinicians choosing to deliver to autistic adults; the current study suggests that many clinicians may not choose CBT, but we do not know what they are doing instead.
Conclusions
This study applied a validated causal model of behavior change to better understand clinicians’ intentions to start CBT with autistic adults. Most clinicians did not report strong intentions to start CBT with autistic adults who present for anxiety or depression treatment, which is concerning given that CBT can be an effective treatment for these concerns in autistic adults (Spain et al., 2015). Despite even more empirical support for using CBT to treat anxiety or depression in adults without autism, clinicians’ intentions to use this evidence-based practice were not strong overall, which likely relates to research showing that few clients who could benefit from CBT actually receive it in their community (e.g., Wolitzky-Taylor, Zimmermann, Arch, De Guzman, & Lagomasino, 2015). Given the relationship between clinicians’ attitudes and their reported intentions to start CBT with their clients, targeting attitudes may be particularly important for designing effective implementation strategies. Although social psychologists have succeeded at modifying attitudes as a means of strengthening intention and changing behavior (Fishbein & Ajzen, 2010), this approach has not yet been applied to improving the implementation of evidence-based practice for autistic adults.
Acknowledgments
The authors are grateful to our community partners and the study participants. Portions of these findings were presented at the 2019 International Society for Autism Research Annual Meeting.
Funding: This work was funded by the National Institute of Mental Health (F32MH111166; PI: Maddox) and the FAR Fund (PI: Maddox).
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
Ethical approval: All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- Ajzen I (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50, 179–211. doi: 10.1016/0749-5978(91)90020-T [DOI] [Google Scholar]
- Armitage CJ, & Conner M (2001). Efficacy of the theory of planned behaviour: A meta- analytic review. British Journal of Social Psychology, 40, 471–499. doi: 10.1348/014466601164939 [DOI] [PubMed] [Google Scholar]
- Beacon BJ, & Abramowitz JS (2004). Cognitive and behavioral treatments for anxiety disorders: A review of meta- analytic findings. Journal of Clinical Psychology, 60, 429–441. doi: 10.1002/jclp.10255 [DOI] [PubMed] [Google Scholar]
- Beidas RS, Marcus S, Aarons GA, Hoagwood KE, Schoenwald S, Evans AC, … Mandell DS (2015). Predictors of community therapists’ use of therapy techniques in a large public mental health system. JAMA Pediatrics, 169, 374–382, 2015 doi: 10.1001/jamapediatrics.2014.3736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brookman-Frazee L, Drahota A, Stadnick N, & Palinkas LA (2012). Therapist perspectives on community mental health services for children with autism spectrum disorders. Administration and Policy in Mental Health, 39, 365–373. doi: 10.1007/s10488-011-0355-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buck TR, Viskochil J, Farley M, Coon H, McMahon WM, Morgan J, & Bilder DA (2014). Psychiatric comorbidity and medication use in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 44, 3063–3071. doi: 10.1007/s10803-014-2170-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Community Behavioral Health. (2017). 2017 Annual Report: Philadelphia Behavioral HealthChoices Program. Retrieved from the Community Behavioral Health website: https://dbhids.org/wp-content/uploads/2018/10/CBH-2017-Annual-Report-1.pdf
- Cooper K, Loades ME, & Russell A (2018). Adapting psychological therapies for autism. Research in Autism Spectrum Disorders, 45, 43–50. doi: 10.1016/j.rasd.2017.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croen LA, Zerbo O, Qian Y, Massolo ML, Rich S, Sidney S, & Kripke C (2015). The health status of adults on the autism spectrum. Autism, 19, 814–823. doi: 10.1177/1362361315577517 [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Berking M, Andersson G, Quigley L, Kleiboer A, & Dobson KS (2013). A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. The Canadian Journal of Psychiatry, 58, 376–385. doi: 10.1177/070674371305800702 [DOI] [PubMed] [Google Scholar]
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, & Lowery JC (2009). Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science, 4, 50. doi: 10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- David D, Cristea I, & Hofmann SG (2018). Why cognitive behavioral therapy is the current gold standard of psychotherapy. Frontiers in Psychiatry, 9:4. doi: 10.3389/fpsyt.2018.00004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMauro J, Domingues J, Fernandez G, & Tolin DF (2013). Long-term effectiveness of CBT for anxiety disorders in an adult outpatient clinic sample: A follow-up study. Behaviour Research and Therapy, 51, 82–86. doi: 10.1016/j.brat.2012.10.003 [DOI] [PubMed] [Google Scholar]
- Fishbein M, & Ajzen I (2010). Predicting and changing behavior: The reasoned action approach. New York, NY: Psychology Press. [Google Scholar]
- Fishman J, Beidas R, Reisinger E, & Mandell DS (2018). The utility of measuring intentions to use best practices: A longitudinal study among teachers supporting students with autism. Journal of School Health, 88, 388–395. doi: 10.n11/josh.12618 [DOI] [PubMed] [Google Scholar]
- Fishman J, Lushin V, Lawson G, Seidman M, Beidas RS, & Mandell DS (2019). A theory for implementation prediction (TIP): Applying causal models of behavior change to specific evidence-based practices. Manuscript submitted for publication. [Google Scholar]
- Frazier TW, Dawson G, Murray D, Shih A, Sachs JS, & Geiger A (2018). Brief report: A survey of autism research priorities across a diverse community of stakeholders. Journal of Autism and Developmental Disorders, 48, 3965–3971. doi: 10.1007/s10803-018-3642-6. [DOI] [PubMed] [Google Scholar]
- Ingersoll B, Straiton D, Casagrande K, & Pickard K (2018). Community providers’ intentions to use a parent-mediated intervention for children with ASD following training: An application of the theory of planned behavior. BMC Research Notes, 11, 777. doi: 10.1186/s13104-018-3879-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddox BB, Crabbe S, Beidas RS, Brookman-Frazee L, Cannuscio CC, Miller JS, Nicolaidis C, & Mandell DS (2019). “I wouldn’t know where to start”: Perspectives from clinicians, agency leaders, and autistic adults on improving community mental health services for autistic adults. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moullin JC, Ehrhart MG, & Aarons GA (2018). Development and testing of the Measure of Innovation-Specific Implementation Intentions (MISII) using Rasch measurement theory. Implementation Science, 13, 89. doi: 10.1186/s13012-018-0782-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellicano E, Dinsmore A, & Charman T (2014). What should autism research focus upon? Community views and priorities from the United Kingdom. Autism, 18, 756–770. doi: 10.1177/1362361314529627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell BJ, Beidas RS, Rubin RM, Stewart RE, Wolk CB, Matlin SL, … Mandell DS (2016). Applying the policy ecology framework to Philadelphia’s behavioral health transformation efforts. Administration and Policy in Mental Health, 43(6), 909–926. doi: 10.1007/s10488-016-0733-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roux AM, Shattuck PT, Rast JE, Rava JA, & Anderson KA (2015). National autism indicators report: Transition into young adulthood. Life Course Outcomes Research Program, A.J. Drexel Autism Institute, Drexel University: Philadelphia, PA. [Google Scholar]
- Salsberg E, Quigley L, Mehfoud N, Acquaviva K, Wyche K, & Sliwa S (2017). Profile of the social work workforce. Retrieved from the Council on Social Work Education website: https://www.cswe.org/Centers-Initiatives/Initiatives/National-Workforce-Initiative/SW-Workforce-Book-FINAL-11-08-2017.aspx
- Shattuck PT, Wagner M, Narendorf S, Sterzing P, & Hensley M (2011). Post high school service use among young adults with autism spectrum disorder. Archives of Pediatrics and Adolescent Medicine, 165, 141–146. doi: 10.1001/archpediatrics.2010.279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spain D, Sin J, Chalder T, Murphy D, & Happé F (2015). Cognitive behaviour therapy for adults with autism spectrum disorders and psychiatric co-morbidity: A review. Research in Autism Spectrum Disorders, 9, 151–162. doi: 10.1016/j.rasd.2014.10.019 [DOI] [Google Scholar]
- Weiss JA, & Lunsky Y (2010). Group cognitive behaviour therapy for adults with Asperger syndrome and anxiety or mood disorder: A case series. Clinical Psychology and Psychotherapy, 17, 438–446. doi: 10.1002/cpp.694 [DOI] [PubMed] [Google Scholar]
- White SW, Simmons GL, Gotham KO, Conner CM, Smith IC, Beck KB, & Mazefsky CA (2018). Psychosocial treatments targeting anxiety and depression in adolescents and adults on the autism spectrum: Review of the latest research and recommended future directions. Current Psychiatry Reports, 20:82. doi: 10.1007/s11920-018-0949-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolitzky-Taylor K, Zimmermann M, Arch JJ, De Guzman E, & Lagomasino I (2015). Has evidence-based psychosocial treatment for anxiety disorders permeated usual care in community mental health settings? Behaviour Research and Therapy, 72, 9–17. doi: 10.1016/j.brat.2015.06.010 [DOI] [PubMed] [Google Scholar]