Abstract
Objective:
To evaluate the association Hurricane Harvey landfall with maternal and neonatal morbidity.
Methods:
Using an institutional perinatal database from two hospitals in Houston, Texas, women with non-anomalous singletons delivering after 24 weeks of gestation between August 2011 and June 2018 were included. To evaluate the possible association of hurricane landfall with pregnancy outcomes, Gravid women delivering within 280 days (40 weeks) on or after August 25th, 2017 (the day of hurricane landfall) were categorized as exposed, and women delivered prior to August 25th, 2017, were the reference group. Composite maternal morbidity included any of the following: hypertensive disorders of pregnancy, chorioamnionitis, endometritis, blood transfusion, peripartum hysterectomy, maternal critical care admission, pulmonary edema or maternal death. Composite neonatal morbidity included any of the following: 5-minute Apgar score ≤ 3, respiratory distress syndrome, use of ventilator or continuous positive airway pressure, suspected newborn sepsis, seizure, stillbirth, or neonatal death. Adjusted odds ratios (aOR) were calculated after correcting for possible confounders identified on univariate analysis. Disruption in outcome trends were measured in time series analyses.
Results:
Of 40,502 deliveries in our database, 29,179 (72%) met the inclusion criteria, with 3,842 (13.2%) delivering within 280 days of Hurricane Harvey landfall. Women delivering after Hurricane Harvey were on average less likely to be obese and more likely to be older, Caucasian, married, have a household income over $75,000, a high school education, and private insurance. However, compared to the cohort of gravid patients who delivered prior to Hurricane Harvey, composite maternal morbidity increased by 27% (11.5% compared to 14.7%, aOR 1.27 95% CI 1.14–1.42) after the storm. Composite neonatal morbidity increased by 50% (7.8% compared to 11.9%, aOR 1.52 95% CI 1.34–1.71). In time series analyses, we observed a significant shift in composite maternal morbidity specific to women of low socioeconomic status (estimate 2.87, p=0.028).
Conclusion:
Despite having fewer at-risk baseline characteristics, gravid patients delivering after landfall by Hurricane Harvey had a significantly higher likelihood of adverse outcomes as did their neonates.
Précis
Despite fewer at-risk baseline characteristics, women delivering after Hurricane Harvey made landfall were significantly more likely to experience increased morbidity as were their neonates.
INTRODUCTION
On August 25th, 2017, Hurricane Harvey made landfall along the Texas Coast. As the storm intensified it became a Category 3 hurricane – with winds ranging from 111 to 130 mph. Upon staling over Southeast Texas for 7 days as a tropical storm, the measured rainfall of 51.88 inches in Houston led to its designation as a major natural weather disaster1. As a result of this unprecedented rainfall, Hurricane Harvey led to the greatest disaster response in the history of the state of Texas. Harris County, which encompasses the city of Houston, reported over 30,000 people displaced, 300,000 to 500,000 vehicles destroyed, and 113,136 homes significant damaged2,3.
Natural disasters, including hurricanes and floods, are recognized risk factors for adverse perinatal outcomes among pregnant women4. It is suggested that gravid patients are more vulnerable during disasters due to disruption of health services, lack of social support, or further limitation of already scarce resources5–8.
Most reports focusing on perinatal outcomes after natural weather disasters, however, have a limited sample size (n = 67 to 301), suffer from selection bias, review a limited number of birth outcomes, or lack the ability to compare the affected population to historical trends within the same population4–7. Given the limitations of current evidence, we evaluated the association of Hurricane Harvey with peripartum outcomes. We also compared outcomes based on patients’ response to a question added to our database after the storm made landfall asking they were “affected” by the natural disaster.
METHODS
We used an IRB-approved perinatal database (PeriBank), which is maintained by trained research personnel at Baylor College of Medicine in Houston, Texas9. All gravid patients who deliver at our public (Ben Taub Hospital) and our private (Texas Children’s Pavilion for Women) hospitals are approached and offered participation in the perinatal database. Over 400 different variables relating to the mother –newborn dyad are collected. This database and biorepository involve active approach and enrollment, and does not rely on volunteers to self-identify nor enter data. The rate of enrollment into the perinatal database among qualified patients did not change significantly throughout the study period, consent rates ranged from 86% in 2012 to 92% in 2016. Regular quarterly audits are done to ensure data accuracy. Data collection forms were available for both Spanish and English-speaking patients, and all subjects are directly queried in their native language. Starting in fall of 2017, after receiving IRB approval, a questionnaire related to experiences and effects of Hurricane Harvey was added; these data were collected on every gravida enrolling in PeriBank. The questions were designed to gather information on perception of the storm’s effects on health and family life, including a yes-no question assessing whether the respondent felt directly affected by Hurricane Harvey.
All women with a singleton pregnancy that delivered between August 2011 and June 2018 were included in this analysis. Only women with a documented delivery at or greater than 24 weeks of gestation were included. Women with two or more deliveries within this timeframe had one delivery randomly chosen for inclusion for the overall analysis. However, in a separate paired analysis, women with one delivery prior and one delivery post Hurricane Harvey were analyzed (n=810); these findings are reported only in the results text as the matched pair analysis. Pregnancies with known fetal anomalies were excluded.
For this analysis, enrolled pregnant women were categorized into one of two groups defined by the day the Hurricane Harvey made landfall on the Texas coast. All women delivering on or after August 25, 2017, were categorized as “exposed” to the natural disaster. To evaluate the effects of the natural disaster as the exposure of interest on outcomes in pregnancy, only women delivering within 280 days (40 weeks) of Hurricane landfall were included in this cohort. As a reference group, we included all women enrolled in our perinatal database prior to August 25th, 2017. This reference group was chosen to allow for a more comprehensive view of the baseline study population and to illustrate an estimate in the change in rates of certain outcomes over time, treating Hurricane Harvey as the exposure of interest. Although the Gulf Coast of Texas is constantly at risk of tropical storms and disturbances, no major hurricane (category 3 or higher) affected the area from 2011 to 201710. In order to directly assess for individual patients affected by Hurricane Harvey (i.e., avoid generalized estimations based on the regional population at-large) starting in October, 2017, all consented subjects in our database were asked a series of scripted questions in their native language pertaining to the perceived effects of the storm on themselves and their possessions. Subgroup analysis was undertaken on women specifically delivering after the storm’s landfall, whereby women self-identified as “affected” versus “unaffected” were compared.
For the overall estimates of the association of Hurricane Harvey as the exposure of interest, comparisons were made between those gravid patients delivering within 280 days after August 25, 2017 referent to equivalent prior. Specifically, we evaluated the historical trend of the adverse outcomes by comparing gravid patients delivering within the same time frame during all previous years to this referent exposure cohort. Additionally, a time trend analysis was conducted to further evaluate the potential seasonal variation among certain adverse outcomes and to evaluate whether we were observing a disruption due to Hurricane Harvey exposure, or rather a generalized trend coincident with Hurricane Harvey. For this analysis, we employed autoregressive integrated moving average (ARIMA) modeling. Specifically, we used the OUTLIER statement to detect changes in the dynamics of the outcomes being modeled11. Model fit was assessed by AIC values and the presence of white noise. The data was summarized by quarterly period within each year as a moving window analysis (January-March, April-June, July-September, and October-December).
Given the potential for confounding by socioeconomic status (specifically, the potential for at-risk women to leave the area before or after the Hurricane) we examined the influence of both change in socioeconomic status of the population over the study years (2011–2018) and the effects of socioeconomic status on pre and post composite morbidity. Specifically, based on our initial findings, analysis for composite maternal morbidity was stratified by combining marital status and education with a separate time series performed for gravid patients who were married and had a >= high school education (defined as high socio-economic status) and a second time series analysis on gravid patients not meeting the previous criteria (defined as low socio-economic status)12. Hence, our conducted time series analysis allowed us to detect the presence of both additive changes and observable sustained shifts throughout the study period, allowing us to attribute a shift as occurring as a result of Hurricane Harvey exposure rather than a generalized trend in the overall interval. In the final model and in the presence of a shift which was observed starting in in September, 2017 (the month after Hurricane Harvey), we controlled for any changes (additive or permanent) which may have been potential confounders prior to that time point.
In addition to our time series analysis, we assessed for a generalized trend of worsening outcomes at a per-subject level, by conducting a matched pair analysis among those gravid patients in our database which had multiple deliveries recorded, specifying that one had to occur prior to Hurricane Harvey and one had to occur after Hurricane Harvey. This resulted in a paired analysis of n=810 subjects, with resultant trend-wise rates for both maternal and neonatal composite indices.
Baseline maternal characteristics and demographics as well as adverse perinatal outcomes were analyzed on all eligible participants. Composite maternal morbidity included any of the following: hypertensive disorders of pregnancy, chorioamnionitis, endometritis, blood transfusion, peripartum hysterectomy, maternal critical care admission, pulmonary edema or maternal death. Composite neonatal morbidity included any of the following: 5-minute Apgar score ≤ 3, respiratory distress syndrome (RDS), use of ventilator or continuous positive airway pressure device, suspected newborn sepsis, seizure, stillbirth, or neonatal death. Small (<10th percentile for GA) and large (at least 90th percentile for GA) for gestational age newborns were cataloged according to their birth weight use population-based curves13.
The sample size for this analysis was determined by the number of participants in the database. This study was approved by the Institutional Review Board of Baylor College of Medicine (H-26364 and H-43879). Descriptive statistics were used to report all variables of interest. Analysis was corrected for possible confounders identified on univariate analysis. Adjusted odds ratio (OR) and 95% confidence intervals (CI) were calculated. A p value <0.05 or a confidence interval excluding 1.0 were considered significant. A final logistic regression analysis was performed using the propensity score as a covariate. Propensity score was estimated by using all covariates significantly different between the two study groups from univariate analysis14. This score was then used as a covariate (and hence adjusted for) in the logistic regression model when examining the association between each outcome and exposure of interest. All analyses were performed in STATA v15 (College Station, Texas) and SAS statistical software version 9.4 (SAS Institute, Cary, NC). The STROBE guidelines for reporting observational studies were followed15.
RESULTS
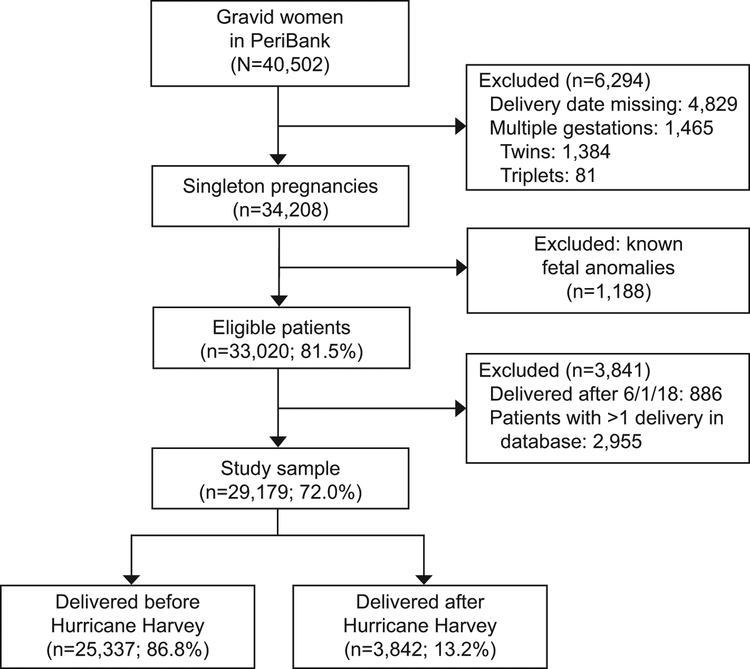
A total of 40,502 women have been enrolled in the perinatal database since its inception. After excluding multiple gestations, 34,208 (84.5%) singleton pregnancies remained. A final study sample of 29,179 (72.0%) women was identified after excluding non-eligible patients; of these, 3,842 (13.2%) delivered during the 280 days after Hurricane Harvey made landfall (Figure 1).
Figure 1.
Flow diagram of sample size utilized.
Compared to gravid patients that delivered prior to Hurricane Harvey, gravid patients delivering after the storm were significantly older and more likely to be Caucasian, less likely to have a pre-pregnancy BMI over 30 kg/m2 and more likely to be married. They were also more likely to have a household income over $75,000, more likely to have insurance enabling care outside of pregnancy and the postpartum interval, and more likely to have completed at least a high school education (Table 1).
Table 1.
Baseline characteristics
| Delivered prior to Hurricane Harvey (N = 25,337) | Delivered after Hurricane Harvey (N = 3,842) | P value | |
|---|---|---|---|
| Age – Mean (SD) | 29.7 (6.1) | 30.2 (5.9) | <0.01 |
| Nulliparous - N (%) | 6,796 (26.8) | 1,192 (31.0) | 0.01 |
| Race – N (%) | |||
| BMI at delivery (kg/m2) – Mean (SD) | 32.0 (6.3) | 32.0 (6.5) | 0.96 |
| Marital Status Married – N (%) | 16,033 (65.0) | 2,940 (77.1) | <0.01 |
| Average household income - N (%) | |||
| Insurance type | |||
| High school education – N (%) | 14,063 (64.5) | 2,998 (78.8) | <0.01 |
| Seizure - N (%) | 22 (0.9) | 36 (0.9) | 0.71 |
| Chronic Hypertension – N (%) | 1,274(5.1) | 202 (5.3) | 0.60 |
| Hyperthyroidism – N (%) | 83 (0.3) | 16 (0.4) | 0.9 |
| Type 1 Diabetes - N (%) | 156 (0.6) | 15 (0.4) | 0.08 |
| Type 2 Diabetes - N (%) | 558 (2.2) | 83 (2.2) | 0.83 |
| Gestational Diabetes - N (%) | 2,419 (9.6) | 347 (9.1) | 0.28 |
BMI – body mass index, SD – standard deviation. Bolded if significantly different.
Women delivering after Hurricane Harvey were less likely to be diagnosed with premature rupture of membranes, more likely to be delivered by cesarean, to be diagnosed with an infection during their labor admission, be colonized by group B Streptococcus and more likely to suffer from composite maternal morbidity (11.5% compared to 14.7%, aOR 1.27 95% CI 1.14–1.42). Hypertensive disorders of pregnancy were 60% more likely to occur among gravid patients delivering after Hurricane Harvey (Table 2).
Table 2.
Maternal outcomes
| Variable | Delivered prior to Hurricane Harvey (N = 25,337) | Delivered after Hurricane Harvey (N = 3,842) | Crude OR (95% CI) | aOR (95% CI) | OR adjusted with propensity score (95% CI) |
|---|---|---|---|---|---|
| Premature rupture of membranes – N (%) | 98 (0.4) | 28 (0.7) | 1.89 (1.24 – 2.88) | ||
| Delivery by cesarean section – N (%) | 7,38 (28.9) | 1,37 (34.8) | 1.31 (1.22 – 1.41) | 1.18 (1.09 – 1.28) | |
| Composite Maternal Morbidity – N (%) | 2,900 (11.5) | 564 (14.7) | 1.33 (1.20 – 1.46) | 1.27 (1.14 – 1.42) | 1.22 (1.09 – 1.37) |
| Hypertensive disorders of pregnancy – N (%) | 1,124 (4.4) | 285 (7.4) | 1.72 (1.51 – 1.97) | 1.60(1.37 – 1.86) | 1.52 (1.30 – 1.77) |
| Chorioamnionitis – N (%) | 1,363 (5.4) | 210 (5.5) | 1.01 (0.87 – 1.18) | 0.99 (0.84 – 1.18) | 1.04 (0.87 – 1.22) |
| Endometritis – N (%) | 128 (0.5) | 16 (0.4) | 0.82 (0.49 – 1.39) | ||
| Blood transfusion during labor – N (%) | 141 (0.6) | 24 (0.6) | 1.12 (0.73 – 1.73) | ||
| Blood transfusion postpartum – N (%) | 291 (1.2) | 63 (1.6) | 1.43 (1.09 – 1.89) | ||
| Peripartum hysterectomy – N (%) | 63 (0.3) | 14 (0.4) | 1.33 (0.75 – 2.38) | ||
| Peripartum ICU admission – N (%) | 33 (0.1) | 9 (0.2) | 1.79 (0.86 – 3.75) | ||
| Peripartum Pulmonary edema – N (%) | 53 (0.2) | 19 (0.5) | 2.37 (1.40 – 4.01) | ||
| Maternal Death – N (%) | 0 | 0 | - | - | |
| Infections antepartum – N (%) | 262 (1.0) | 45 (1.2) | 1.13 (0.83 – 1.56) | ||
| Infections during labor admission – N (%) | 6,225 (24.6) | 1,213 (31.6) | 1.41 (1.32 – 1.53) | 1.41 (1.31 – 1.54) | 1.47 (1.35 – 1.60) |
| GBS colonization antepartum – N (%) | 4,345 (17.2) | 862 (22.4) | 1.40 (1.28 – 1.52) | 1.28 (1.17 – 1.40) | 1.33 (1.21 – 1.47) |
| Infections postpartum – N (%) | 484 (1.9) | 93 (2.4) | 1.27 (1.02 – 1.60) | 0.97 (0.76–1.26) | 0.99 (0.76 – 1.29) |
| Wound infection – N (%) | 39 (0.2) | 3 (0.1) | 0.51 (0.16 – 1.64) | ||
| Abscess formation postpartum – N (%) | 5 (0.02) | 1 (0.03) | 1.32 (0.15 – 11.3) |
Multivariate logistic regression adjusted for maternal age, race, BMI at delivery, nulliparity, education level, insurance type, household income and marital status. aOR were only reported if the outcome of interested had a minimum number of events reported (80) thus allowing 8 adjustors to be used.
Composite maternal morbidity includes: hypertensive disorders of pregnancy, chorioamnionitis, endometritis, blood transfusion intrapartum or postpartum, peripartum hysterectomy, maternal ICU admission, pulmonary edema or maternal death. Bolded if significantly different.
Adverse neonatal outcomes were also more common among gravid patients delivering after Hurricane Harvey made landfall. Composite neonatal morbidity increased by 50% (7.8% compared to 11.9%, aOR 1.52 95% CI 1.34–1.71). The rates for both respiratory distress syndrome and suspected or proven neonatal sepsis were increased among women delivering after the storm made landfall (Table 3). Overall, with propensity score analysis, there was no change in the magnitude or the direction of the odds ratios (Tables 2 and 3).
Table 3.
Neonatal outcomes
| Variable | Delivered prior to Hurricane Harvey (N = 25,337) | Delivered after Hurricane Harvey (N = 3,842) | P value/ Crude OR (95% CI) | aOR (95% CI) | OR adjusted with propensity score (95% CI) |
|---|---|---|---|---|---|
| Gestational age at delivery – Median (IQ range) | 38.8 (2.1) | 38.8 (2.2) | 0.40 | - | |
| Birth weight (grams) – Mean (SD) | 3279.9 (570.9) | 3250.8 (579.2) | 0.05 | - | |
| Head circumference del (cm) – Mean (SD) | 34.0 (2.35) | 34.0 (2.30) | 0.70 | - | |
| Female neonate – N (%) | 12,376 (48.9) | 1,913 (49.8) | 0.29 | - | |
| Small for gestational age – N (%) | 2,608 (10.3) | 420 (10.9) | 1.06 (0.96 – 1.19) | 1.09 (0.96 – 1.23) | |
| Large for gestational age – N (%) | 1,850 (7.3) | 255 (6.6) | 0.90 (0.79 – 1.04) | 0.89 (0.77 – 1.04) | |
| Arterial cord pH <7.1 – N (%) | 104 (0.4) | 38 (1.0) | 2.42 (1.67 – 3.52) | ||
| Meconium at birth – N (%) | 3,377 (13.5) | 448 (11.7) | 0.85 (0.77 – 0.95) | 0.95 (0.84 – 1.08) | |
| Transient tachypnea of newborn – N (%) | 366 (1.5) | 105 (2.7) | 1.91 (1.53 – 2.38) | 1.81 (1.43 – 2.30) | 1.76 (1.36 – 2.24) |
| Retinopathy of prematurity – N (%) | 75 (0.3) | 23 (0.6) | 2.01 (1.26 – 3.22) | ||
| Composite Neonatal Morbidity – N (%) | 1,965 (7.8) | 456 (11.9) | 1.60 (1.43–1.78) | 1.52 (1.34 – 1.71) | 1.48 (1.30 – 1.67) |
| Apgar at 5 min ≤3 – N (%) | 68 (0.3) | 7 (0.2) | 0.68 (0.31 – 1.48) | ||
| Respiratory distress syndrome – N (%) | 709 (2.8) | 173 (4.5) | 1.63 (1.38 – 1.94) | 1.75 (1.44 – 2.13) | 1.66 (1.34 – 2.05) |
| Use of ventilator support/CPAP – N (%) | 94 (0.4) | 2 (0.1) | 0.13 (0.03 – 0.57) | ||
| Suspected/proven newborn sepsis – N (%) | 1,270 (5.0) | 337 (8.8) | 1.81 (1.60 – 2.06) | 1.54 (1.34 – 1.77) | 1.50 (1.30 – 1.73) |
| Confirmed neonatal seizures – N (%) | 25 (0.1) | 3 (0.1) | 0.79 (0.24 – 2.61) | ||
| IUFD/Stillbirth – N (%) | 17 (0.1) | 4 (0.1) | 1.55 (0.52 – 4.62) | ||
| Neonatal Death – N (%) | 40 (0.1) | 6 (0.2) | 0.9 (0.42 – 2.33) |
Multivariate logistic regression adjusted for maternal age, race, body mass index at delivery, nulliparity, education level, insurance type, household income and marital status. aOR were only reported if the outcome of interested had a minimum number of events reported (80) thus allowing 8 adjustors to be used. Bolded if significantly different.
Composite neonatal morbidity includes: 5-minute Apgar score ≤ 3, respiratory distress syndrome (RDS), use of ventilator/CPAP, suspected newborn sepsis, seizure, stillbirth, or neonatal death.
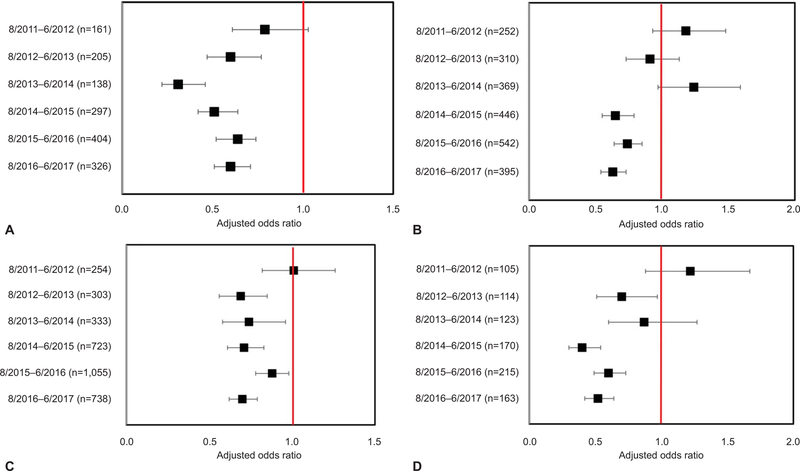
Composite neonatal morbidity was increased among the offspring of women delivering after Hurricane Harvey when compared to all but one historical cohort (Figure 2). This same trend was noted when evaluating antepartum group B Streptococcus colonization. Composite maternal morbidity among women delivering after Hurricane Harvey was increased when compared to the three most recent historical cohorts indicating the natural weather disaster was associated with a reversal in the downward trend in composite maternal morbidity that was experienced within our population.
Figure 2.
Adjusted ORs of adverse outcomes compared to same timeframe during previous years. Composite neonatal morbidity (A), composite maternal morbidity (B), group B streptococcus colonization (C), and hypertensive disorders of pregnancy (D). Adjusted OR reported for historical comparisons. All previous years were compared to reference of 8/24/2017 to 6/1/2018 (period after Harvey). The red vertical line represents the referent, period after Hurricane Harvey. The n value represents the number of events in comparison group.
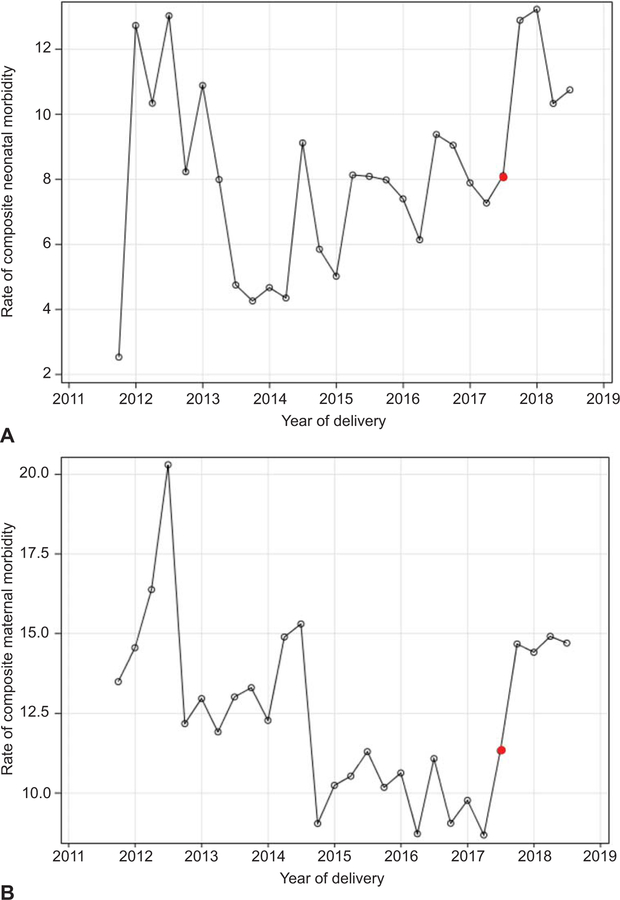
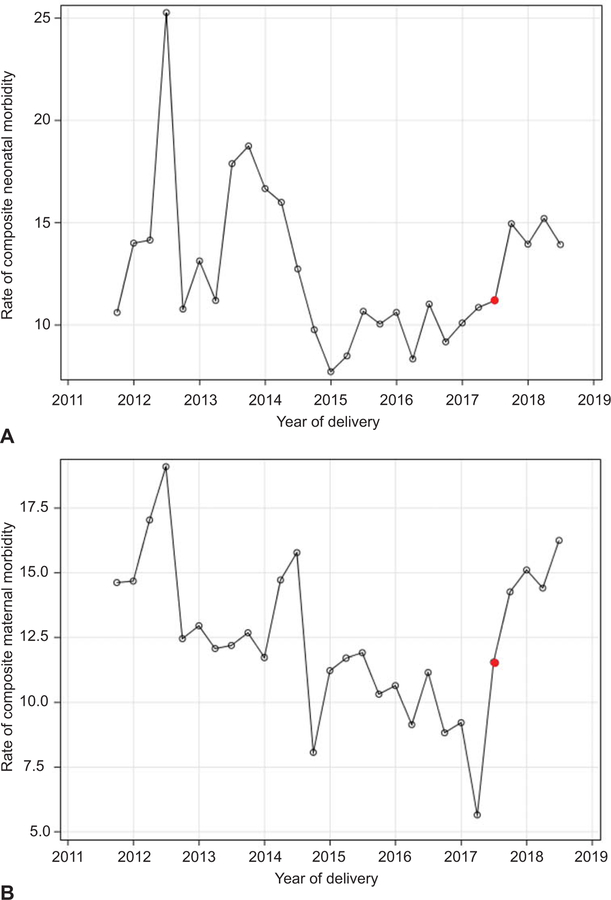
There was a significant shift in the direction of increase in composite maternal morbidity beginning in September, 2017 (estimate 2.49, p=0.018, Figure 3). However, this shift was not observed for composite neonatal morbidity suggesting specificity for maternal morbidity. Among the high socioeconomic group (married and having achieved at least a high school education) no significant shift in composite maternal morbidity was observed between 2011 and 2018. However, among women of lower socioeconomic status, we again observed a significant shift with an increase in composite maternal morbidity specific to the events on or after September 2017 (estimate 2.87, p=0.028) (Figure 4).
Figure 3.
Time series analysis for composite neonatal morbidity (A) and composite maternal morbidity (B). The exposure group (delivery after Hurricane Harvey) is represented from the third quarter of 2017 (red dot) and beyond.
Figure 4.
Time series analysis for composite maternal morbidity stratified by socioeconomic status. High socioeconomic status (A) and low socioeconomic status (B). The exposure group (delivery after Hurricane Harvey) is represented from the third quarter of 2017 (red dot) and beyond.
Gravid patients answering positively to direct queries (in their native language) whether or not they were affected by Hurricane Harvey had higher rates of blood transfusions intrapartum, suspected/proven newborn sepsis and were more likely to suffer a of neonatal death (0.03% compared to 1.3%, Table 4). Similarly, separate subgroup analyses of outcomes after the Hurricane were similar across all trimesters of pregnancy. (Appendix 1, available online at http://links.lww.com/xxx). Finally, matched pair analysis conducted on gravid patients in our database with one recorded and abstracted delivery before and one after August 25, 2017 (n=810 subjects) revealed no significant changes in the rate of composite neonatal morbidity, group B Streptococcus colonization antepartum or hypertensive disorders of pregnancy. However, the rate of composite maternal morbidity was noted to be significantly higher prior to the storm, 11.7% vs. 6.9%, p<0.01; this is consistent with generalized trends when comparing primiparous and multiparous gravid patients.
Table 4.
Comparison between gravid patients who reported they were affected by Hurricane Harvey and woman not affected by the natural weather disaster
| Variable | Not Affected by Hurricane REFERENCE (N = 3,439) | Affected by Hurricane (N = 403) | Crude OR (95% CI) | aOR (95 % CI)* |
|---|---|---|---|---|
| Preterm Birth <37 weeks – N (%) | 327 (9.5) | 43 (10.7) | 1.14 (0.81 – 1.59) | 1.02 (0.70 – 1.48) |
| Premature rupture of membranes – N (%) | 26 (0.8) | 2 (0.5) | 0.65 (0.15 – 2.77) | |
| Delivery by cesarean section – N (%) | 1,191 (43.6) | 146 (36.2) | 1.07 (0.86 – 1.33) | 1.03 (0.81 – 1.31) |
| Infections during labor admission – N (%) | 1,084 (31.5) | 129 (32.0) | 1.02 (0.82 – 1.28) | 0.99 (0.78 – 1.26) |
| GBS colonization antepartum – N (%) | 761 (22.1) | 101 (25.1) | 1.17 (0.92 – 1.50) | 1.17 (0.90 – 1.52) |
| Small for gestational age – N (%) | 376 (10.9) | 44 (10.9) | 0.99 (0.72 – 1.39) | 0.97 (0.68 – 1.40) |
| Composite Maternal Morbidity – N (%) | 508 (14.8) | 56 (13.9) | 0.92 (0.69 – 1.23) | 0.85 (0.61 – 1.19) |
| Hypertensive disorders of pregnancy – N (%) | 263 (7.7) | 22 (5.5) | 0.70 (0.45 – 1.09) | 0.73 (0.45 – 1.18) |
| Blood transfusion during labor admission – N (%) | 18 (0.5) | 6 (1.5) | 2.89 (1.14 – 7.33) | |
| Blood transfusion postpartum – N (%) | 55 (1.6) | 8 (2.0) | 1.24 (0.59 – 2.64) | |
| Peripartum Pulmonary edema – N (%) | 16 (0.5) | 3 (0.8) | 1.60 (0.47 – 5.54) | |
| Arterial cord pH <7.1 – N (%) | 30 (0.9) | 8 (2.0) | 2.30 (1.05 – 5.05) | |
| Transient tachypnea of newborn – N (%) | 91 (2.7) | 14 (3.5) | 1.32 (0.74 – 2.34) | 1.31 (0.72 – 2.38) |
| Retinopathy of prematurity – N (%) | 17 (0.5) | 6 (1.5) | 3.02 (1.19 – 7.72) | |
| Composite Neonatal Morbidity – N (%) | 393 (11.4) | 63 (15.6) | 1.43 (1.08 – 1.92) | 1.42 (1.03 – 1.94) |
| Respiratory distress syndrome – N (%) | 155 (4.5) | 18 (4.5) | 0.98 (0.60 – 1.63) | 0.92 (0.53 – 1.57) |
| Suspected/proven newborn sepsis – N (%) | 288 (8.4) | 49 (12.2) | 1.51 (1.09 – 2.09) | 1.39 (0.98 – 1.98) |
| Suspected/proven newborn seizure – N (%) | 1 (0.03) | 2 (0.5) | 17.1 (1.55 – 188.8) | |
| Neonatal death – N (%) | 1 (0.03) | 5 (1.3) | 43.2 (5.03 – 370.6) |
Multivariate logistic regression adjusted for maternal age, race, body mass index at delivery, nulliparity, education level, insurance type, household income and marital status. aOR were only reported if the outcome of interested had a minimum number of events were identified (80) thus allowing 8 adjustors to be used. Bolded if significantly different.
Discussion
In this analysis, we report maternal and neonatal data from over 3800 gravid women and their offspring exposed to Hurricane Harvey landfall in reference to 25,337 (86.8%) pregnancies delivered prior to the storm. Women delivering after Hurricane Harvey, despite having fewer at-risk baseline demographic characteristics, were significantly more likely to have adverse outcomes as were their neonates compared to women delivering prior to storm’s landfall. Additionally, gravid patients stating they were affected by Hurricane Harvey were also more likely to have higher rates of adverse perinatal outcomes and their neonates were more likely to die.
In smaller cohorts, natural weather disasters have been suggested to increase the rate of occurrence several adverse perinatal outcomes. Prior publications typically evaluate gravid patients months after the full effect of the natural disaster has occurred7,16,17 and lack the ability to compare the study population to historical cohorts thus allowing for time trend fluctuations to become evident4. They also are unable to effectively eliminate the risk of falsely reporting seasonal variations as changes in rate of occurrence known to afflict certain perinatal outcomes5–7,16,18. The limited number of both maternal and neonatal outcomes that are reported in the literature also may contribute to publication bias.
Some similarities with prior reporting on this topic are noticeable. Our analysis revealed a 5% increase in the Cesarean delivery rate among our study population. Using U.S. vital statistics, Hamilton et al6 reported a similar 6–10% increase in the Cesarean rate by affected areas during Hurricane Katrina. The rate of low birth weight infants has also been reported not be associated with the effects of Hurricanes on pregnant populations by some6, a finding similar to our own. The potential link between increased preterm birth rates and natural weather disasters reported by others is worth closer examination6–8. Our analysis did not demonstrate any change in the preterm birth rate when we compared women delivering before and after landfall by Hurricane Harvey as well as women stating there were affected by the hurricane versus those not affected. Similarly, data evaluating the effects of Hurricane Katrina on New Orleans and Baton Rouge 6–18 months later did not reveal an increase in the preterm birth rate7. However, another report did find an increase in only very preterm births when the analysis was limited to FEMA-designated counties in Alabama after the same storm6. The effect of flooding may also contribute to an increase in the rate of births prior to 37 weeks as evidenced by a report by Tong et al that reveals a nearly 9% increase in the rate after flooding from the Red River in North Dakota8. Resolving these differences and their potential underlying causes is of likely importance for both management and prevention in the setting of such natural weather disasters and warrants future investigation.
Certain biological changes associated with natural disasters could explain the increase in adverse outcomes. Prenatal stress after natural disasters increases insulin excretion19 which may lead to metabolic disorders in gravid patients. The transcriptional regulation of the placental glucocorticoid system appears to be downregulated among women affected by prenatal stress after a major flood with associated decreased fetal protection20,21. Cortisol, a hormone known to be involved in parturition22, may also be affected. Evening levels of salivary cortisol levels decrease among survivors with high depression after natural disasters23.
However, stress alone is unlikely to explain all observations noted in this report. Perinatal outcomes may be affected by increased exposure to chemical and environmental pollutants (both ambient and soil or water-based) resulting from a hurricane’s widespread flooding and wind damage. Levels of polycyclic aromatic hydrocarbons such as benzo[a]pyrene, benzo[b]fluorene and dibenz[a,h]anthracene have be found to be higher in placental tissue among preterm deliveries compared to term deliveries in woman living close to Superfund sites in Harris County, Texas24. Changes within epigenetic markers linked to fetoplacental development have been observed in placental tissue of women exposed to environmental pollutants such as polybrominated diphenyl ethers25. Exposure to air pollution has been linked to an increased risk of preterm birth among residents of Harris County26. It is of note that the associations we observed were significant in time series analysis among patients of lower socioeconomic strata. Given associations between socioeconomic status and both stress and environmental exposures, we speculate that our observations are consistent with the notion that perinatal morbidity in association with natural disasters may be another example of health disparities and is worthy of future focused study and investigations.
Although robust, our analysis does have several limitations. This is a retrospective analysis and therefore all limitations specific to such a research design are present. Given the significant difference in baseline demographics between the groups, unintentional selection bias due to migration out of the hurricane’s affected area is a possibility. However, based on our time trend analyses which demonstrated that significance was retained among gravid patients of lower socioeconomic status, it is more likely that these socioeconomic strata experience distinct susceptibility and resilience to natural disasters. Specifically, in the case of Hurricane Harvey, our data demonstrate vulnerability of women of lower socioeconomic status as they experienced a significant higher rate of composite maternal morbidity which was not observed among higher socioeconomic strata over the same comparative interval. Whether this is due to an association with a yet unidentified individual, community-based, or environmental protective or mitigating factor cannot be determined by the current analysis. As noted above, this may be partially attributable to health disparities, specifically social and environmental justice disparities. We can only infer on an association between event and outcomes and are not able to draw any conclusions on causality and our theory on biologic plausibility remain informed by the literature but speculative at this juncture. We included only patients presenting for delivery at our two institutional affiliate hospitals, and thus potentially over representing a subgroup of the entire pregnant population affected by Hurricane Harvey. Thus, the perinatal outcomes in different settings may differ from ours. With our sample size of affected women and the infrequency of certain adverse outcomes, type II error remains a potential limitation. Lastly, while influence of in-utero exposure to disaster and adverse health outcomes in children are known27–29, we did not ascertain long term data. We, therefore, cannot comment on the persistent and long-term effects, if any, of a natural disaster on the mother-child dyad.
The strengths of this analysis should also be acknowledged. The larger sample size compared to previous reports allowed for a more robust analysis. The respondents were from two different hospitals with marked ethnic and racial diversity. The number of maternal and neonatal outcomes evaluated is more comprehensive than earlier articles7,16,17. Our data allowed for historical comparisons and seasonal variation to be assessed within our study population, including rigorous time series and propensity analyses, alongside the unique use of a limited number of pair-wise comparisons. Thus, our findings are unlikely to be misattributed to generalized population nor individual trends towards worse outcomes over the study interval, since both trended towards improvement and August, 2017 was the significant disruption. Data collection done by trained multilingual research staff, as well as the regularly scheduled database audits increases the validity of the data obtained from focused interviews with subjects. Overall, the combination of a large, prospective cohort, detailed individual subject data, and time series analyses provides confidence to our interpretations and conclusions.
In summary, gravid patients delivering after Hurricane Harvey experienced worse perinatal outcomes compared to those delivering prior to the natural disaster. This was most notable in women of low socioeconomic strata. It is our sincere hope that this study may provide other colleagues and health care professionals with the initial data which are necessary for efforts aimed at prioritizing resources to susceptible individuals (including of lower socioeconomic strata) during an emergency.
Supplementary Material
Acknowledgments
This work was supported by NIEHS R21ES029462 (to Kjersti Aagaard).
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
Presented as a poster at the Society of Maternal Fetal Medicine Annual Meeting – Las Vegas, NV February 11–16 2019
REFERENCES
- 1.Historic Disaster Response to Hurricane Harvey in Texas. FEMA September 22, 2017. (Accessed Nov-9, 2018, at https://www.fema.gov/news-release/2017/09/22/historic-disaster-response-hurricane-harvey-texas.)
- 2.Service Assessment - August–September 2017 Hurricane Harvey. U.S. DEPARTMENT OF COMMERCE June 2018. (Accessed Nov-9, 2018, at https://www.weather.gov/media/publications/assessments/harvey6-18.pdf.)
- 3.Texas Hurricane Harvey (DR-4332). FEMA September 2017. (Accessed Nov-9, 2018, at https://www.fema.gov/disaster/4332.)
- 4.Harville E, Xiong X, Buekens P. Disasters and perinatal health:a systematic review. Obstet Gynecol Surv 2010;65:713–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duff EM, Cooper ES. Neural tube defects in Jamaica following Hurricane Gilbert. Am J Public Health 1994;84:473–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hamilton BE, Sutton PD, Mathews TJ, Martin JA, Ventura SJ. The effect of Hurricane Katrina: births in the U.S. Gulf Coast region, before and after the storm. Natl Vital Stat Rep 2009;58:1–28, 32. [PubMed] [Google Scholar]
- 7.Xiong X, Harville EW, Mattison DR, Elkind-Hirsch K, Pridjian G, Buekens P. Exposure to Hurricane Katrina, post-traumatic stress disorder and birth outcomes. Am J Med Sci 2008;336:111–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tong VT, Zotti ME, Hsia J. Impact of the Red River catastrophic flood on women giving birth in North Dakota, 1994–2000. Matern Child Health J 2011;15:281–8. [DOI] [PubMed] [Google Scholar]
- 9.Antony KM, Hemarajata P, Chen J, et al. Generation and validation of a universal perinatal database and biospecimen repository: PeriBank. J Perinatol 2016;36:921–9. [DOI] [PubMed] [Google Scholar]
- 10.A STORM TO REMEMBER: FISCAL NOTES. A REVIEW OF THE TEXAS ECONOMY FROM THE OFFICE OF GLENN HEGAR, TEXAS COMPTROLLER OF PUBLIC ACCOUNTS SPECIAL EDITION HURRICANE HARVEY AND THE TEXAS ECONOMY. February, 2018. at https://comptroller.texas.gov/economy/fiscal-notes/2018/special-edition/history.php.)
- 11.Falk M, Marohn F, Michel R, et al. A First Course on Time Series Analysis : Examples with SAS2005. [Google Scholar]
- 12.Parker JD, Schoendorf KC, Kiely JL. Associations between measures of socioeconomic status and low birth weight, small for gestational age, and premature delivery in the United States. Ann Epidemiol 1994;4:271–8. [DOI] [PubMed] [Google Scholar]
- 13.Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. A United States national reference for fetal growth. Obstet Gynecol 1996;87:163–8. [DOI] [PubMed] [Google Scholar]
- 14.Propensity Score Analysis And Assessment Of Propensity Score Approaches Using SAS® Procedures Statistics and Data Analysis, 2012. (Accessed 7/1/2019, at https://pdfs.semanticscholar.org/c10a/cf956fd8fd91debda40aa16c18f707303ec7.pdf.)
- 15.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007;370:1453–7. [DOI] [PubMed] [Google Scholar]
- 16.Harville EW, Xiong X, Buekens P. Hurricane Katrina and perinatal health. Birth 2009;36:325–31. [DOI] [PubMed] [Google Scholar]
- 17.Xiong X, Harville EW, Mattison DR, Elkind-Hirsch K, Pridjian G, Buekens P. Hurricane Katrina experience and the risk of post-traumatic stress disorder and depression among pregnant women. Am J Disaster Med 2010;5:181–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Savage J, Giarratano G, Bustamante-Forest R, Pollock C, Robichaux A, Pitre S. Post-Katrina perinatal mood and the use of alternative therapies. J Holist Nurs 2010;28:123–32; quiz 33–5. [DOI] [PubMed] [Google Scholar]
- 19.Dancause KN, Veru F, Andersen RE, Laplante DP, King S. Prenatal stress due to a natural disaster predicts insulin secretion in adolescence. Early Hum Dev 2013;89:773–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.St-Pierre J, Laplante DP, Elgbeili G, et al. Natural disaster-related prenatal maternal stress is associated with alterations in placental glucocorticoid system: The QF2011 Queensland Flood Study. Psychoneuroendocrinology 2018;94:38–48. [DOI] [PubMed] [Google Scholar]
- 21.Suter MA, Abramovici AR, Griffin E, et al. In utero nicotine exposure epigenetically alters fetal chromatin structure and differentially regulates transcription of the glucocorticoid receptor in a rat model. Birth Defects Res A Clin Mol Teratol 2015;103:583–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liggins GC. The role of cortisol in preparing the fetus for birth. Reprod Fertil Dev 1994;6:141–50. [DOI] [PubMed] [Google Scholar]
- 23.Yonekura T, Takeda K, Shetty V, Yamaguchi M. Relationship between salivary cortisol and depression in adolescent survivors of a major natural disaster. J Physiol Sci 2014;64:261–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Suter MA, Aagaard KM, Coarfa C, et al. Association between elevated placental polycyclic aromatic hydrocarbons (PAHs) and PAH-DNA adducts from Superfund sites in Harris County, and increased risk of preterm birth (PTB). Biochem Biophys Res Commun 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kappil MA, Li Q, Li A, et al. In utero exposures to environmental organic pollutants disrupt epigenetic marks linked to fetoplacental development. Environ Epigenet 2016;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kahr MK, Suter MA, Ballas J, et al. Preterm birth and its associations with residence and ambient vehicular traffic exposure. Am J Obstet Gynecol 2016;215:111 e1–e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Malaspina D, Corcoran C, Kleinhaus KR, et al. Acute maternal stress in pregnancy and schizophrenia in offspring: a cohort prospective study. BMC Psychiatry 2008;8:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brand SR, Engel SM, Canfield RL, Yehuda R. The effect of maternal PTSD following in utero trauma exposure on behavior and temperament in the 9-month-old infant. Ann N Y Acad Sci 2006;1071:454–8. [DOI] [PubMed] [Google Scholar]
- 29.Kleinhaus K, Harlap S, Perrin M, et al. Prenatal stress and affective disorders in a population birth cohort. Bipolar Disord 2013;15:92–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.