Abstract
Urban tree cover can provide several ecological and public health benefits. Secondary datasets for Tampa, FL, including sociodemographic variables (e.g., race/ethnicity), health data, and interpolated values for features of tree cover (e.g., percent canopy and leaf area index) were analyzed using correlation and regression. Percent canopy cover and leaf area index were inversely correlated to respiratory and cardiovascular outcomes, yet only leaf area index displayed a significant association with respiratory conditions in the logistic regression model. Percent racial/ethnic minority residents at the block group level was significantly negatively correlated with median income and tree density. Leaf area index was also significantly lower in block groups with more African-American residents. The percentage of African Americans (p = 0.101) and Hispanics (p < 0.001) were positively associated with respiratory outcomes while population density (p < 0.001), percent canopy (p < 0.01), and leaf area index (p < 0.01) were negatively associated. In multivariate models, higher tree density, leaf area index, and median income were significantly negatively associated with respiratory cases. Block groups with a higher proportion of African Americans had a higher odds of displaying respiratory admissions above the median rate. Tree density and median income were also negatively associated with cardiovascular cases. Home ownership and tree condition were significantly positively associated with cardiovascular cases.
Keywords: Green space, Health, Urban, Nature
Introduction
Urbanization coupled with loss of canopy cover has resulted in numerous ecological and public health implications that are not fully understood. Assessing the role of urban green space on the health of city residents is a grand environmental challenge that warrants further study [1, 2]. Hence, the importance of land cover, such as urban tree cover, is receiving more attention in the public health realm. For example, the World Health Organization regards green space (i.e., vegetated areas such as parks, forests, gardens) as a vital indicator of sustainable cities [3]. Scholars assert that the next chapter of research on sustainable cities should integrate insight from fields such as urban ecology with an area’s sociopolitical [4, 5] and public health contexts [1, 6–10]. By definition, ecosystem services pertain to the health and well-being benefits that humans receive from the natural environment [11]. Since vegetation plays a foundational role in characterizing ecosystems, a growing body of literature has analyzed the connection between urban vegetation and different aspects of health. Likewise, public health ecology is a framework that connects aspects of the natural environment (e.g., landscape structure and ecosystem functionality) with human health outcomes such as respiratory and cardiovascular concerns [12]. As Tampa adopted a 2040 comprehensive plan focused on “people, places, and natural spaces,” an improved understanding on the role of urban tree cover and health can support strategies to enhance quality of life. In this paper, we assess the relationship between urban tree canopy cover and human health. Specifically, we analyze the incidence of respiratory and cardiovascular conditions in Tampa, FL, and hypothesize that incidences of these conditions are inversely related to structural features of tree cover.
Urban green spaces provide ecosystem services that can be beneficial to various aspects of human health and well-being [7, 13–19]. These benefits were noted in studies that observed an inverse association between green spaces and health concerns such as physical inactivity [20] and depression [21] as well as cardiovascular and respiratory conditions [22, 23]. For example, counties across fifteen US states showed an increase in mortality from cardiovascular and lower-respiratory-tract conditions in correlation with loss of tree cover resulting from pest infestations [24]. On the contrary, Richardson et al. [25] did not detect a significant effect from green space upon mortality rates in some of the largest US cities. Further, the results indicated that urban sprawl and the automobile-dependent lifestyle of many American cities may eclipse the potential benefits from green spaces. Thus, numerous factors can affect the relationship between green space and health.
The spatial arrangement of urban green spaces can also interact with other factors within the built environment that support a broad vision of health [6, 26]. Several pathways can mediate the potential health benefits that humans receive through contact with green spaces. For example, improved immune function is considered a key pathway through which exposure to green space can enhance human health [27]. In addition, health benefits related to social cohesion [6, 14, 19], stress alleviation [28], and mitigation of the heat island effect (i.e., the capture and release of solar energy by impervious surfaces which lead to higher temperatures in urban areas) [29] have also emerged in the literature. The task of understanding the role of green space on health is important to strategically designed urban environments that promote positive health outcomes [1].
Canopy cover is a distinctive part of the urban landscape that is particularly important to a city’s physical and socioeconomic environment [30]. Characteristics of urban tree cover (e.g., amount and condition) can vary across the landscape [31, 32] and affect the delivery of ecosystem services [32]. For instance, leaf area index (LAI), being the total one-side area of leaves of plants per unit of ground [33], may be considered an indicator for removing air pollutants [34]. However, different stressors (e.g., urbanization and changes to land cover) can reduce the ability of ecosystems to function at an optimal state [35]. For example, trees in poor condition have a limited ability to support the growth of leaves which provide ecosystem services such as shade and the interception of rainfall. Also, damaged trees have a limited ability to withstand disturbances (e.g., storms) and pressures (e.g., soil compaction from an urban setting). Hence, degraded vegetative cover can minimize ecosystem services and potentially lead to gaps in health by socioeconomic status [7, 36] as well as race and ethnicity [7]. Numerous studies have explored how urban tree cover may relate to concerns in environmental injustice. Scholars describe how inequitable access to urban tree cover maybe linked to health disparities [7, 37] and reduced ecosystem services [32] among diverse populations. Many have analyzed this topic in the context of race/ethnicity and income. For example, previous studies found an inverse association between tree cover and the proportion of racial/ethnic minorities [32, 38–40]. Similar observations were made for the level of income [38, 39]. Despite research that has observed such inequities, the results for tree cover, inequitable access, and/or health outcomes can vary [41]. Also, few studies have captured the structural features of tree cover (e.g., leaf area index, tree density, and condition) in their analysis. For this reason, there is a need to analyze the relationship between structural qualities of canopy cover and the health of diverse populations [42].
It is also important to note, however, that all green spaces may not render the same health benefits and they may provide disservices to consider [41, 43]. Some vegetation release biogenic volatile organic compounds (BVOCs) that serve as precursor for ozone formation [44] yet some report that increasing vegetation’s LAI may significantly reduce oxygenated volatile organic compounds (oVOC) [45].
Few studies have considered the importance of the quality of green space in health studies [14, 23, 46] and the collective role of individual trees in health outcomes is rarely analyzed [1], and others encourage analysis at a finer geographic scale to enhance future studies [22]. We explore the association between tree canopy cover and rates of respiratory and cardiovascular outcomes using hospital admissions data from the City of Tampa for 2007.
Methods
Study Site
Our study area is the City of Tampa which is located at approximately 28° N latitude and 82° W longitude on the mid-western coast of the Florida peninsula. It is the third largest city in Florida, with an estimated population of 335,327 during the 2006–2010 estimate which consisted of roughly 65% Whites, 26% African Americans, and 23% who identify themselves as either Hispanic or Latino American [47]. Summers have a mean high temperature of 32 °C and winters have mean low temperature of 12 °C and most precipitation occurs in the summer at an annual average of 117 cm [48]. The City of Tampa performed an Urban Ecological Assessment which provides a comprehensive inventory of the ecological and economic benefits from its forests in 2007. Insight on the association between tree cover and human health can provide information to stakeholders and decision makers to manage natural resources that can be beneficial to all citizens.
Data
In this study, we utilized a combination of secondary datasets to analyze the interactions between structural features of tree cover and sociodemographic variables, as well as respiratory and cardiovascular-related hospital admissions.
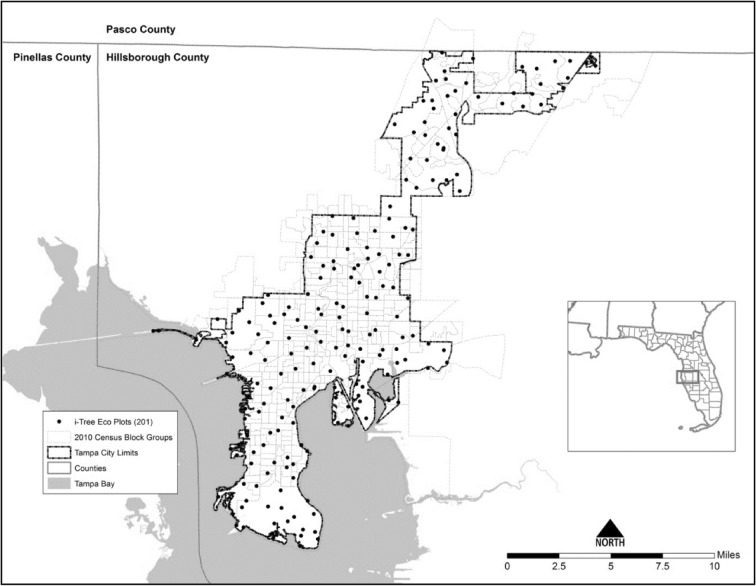
Tree Cover
Tree cover was our primary exposure variable of interest. Two datasets were used to characterize tree cover across our study site: i-Tree Eco plots [49, 50] and satellite imagery. Two hundred and one plots (circular plot area of 400 m2) were distributed across the city using random sampling with a hexagon grid and inventoried between February and July 2007 [51]. Following the sampling protocols for the i-Tree model, plots were assessed for structural features such as tree condition and leaf area index. Tree condition was measured for each woody stem with a trunk diameter of greater than 2.5 cm at a breast height of 1.5 m. Specifically, categories for tree condition were based on the percent dead tree tips in the crown of a tree (i.e., crown dieback). We also calculated the basal area (i.e., cross section of a tree stem at breast height) and tree density. Figure 1 is a map of i-Tree sample plots and census block groups within the Tampa city limits.
Fig. 1.
Map of i-Tree sample plots across census block groups in Tampa, FL
Structural characteristics were obtained or calculated for each tree and averaged at the plot level. Percent canopy cover was estimated at the census block group level using 2006 IKONOS satellite imagery data [52]. Block groups were then categorized into quartiles based on the percent canopy cover. Outputs for tree condition were converted into numerical values which included the following: excellent = 5, good = 4, fair = 3, poor = 2, critical/dying = 1, and dead = 0. Similar to other studies on tree cover [32, 53, 54], we utilized ordinary kriging as an interpolation technique to determine values and calculate the statistical probability of occurrences across a surface where values are unknown [55]. For example, structural attributes of tree cover such as tree density and LAI for all block groups within the city limits of Tampa, FL, were calculated. There was a total of 201 sample plots including plots containing values of zero to account for locations without trees. Comparatively, there were 372 block groups within the City of Tampa and 128 contained at least one sample plot. As the estimates obtained from kriging can be more accurate than averaging values at the community level [56], it provides an overall estimate of variables across the city which can be informative to this study. For example, due to the large area and sample size, kriging can provide a more accurate prediction of variables per census block group. Kriging takes into account the distance and values of surrounding variables to estimate locations and values across the entire sample surface area. Similar to other studies on vegetation [57–59] and ecosystem services [60], we used the spatial analyst technique of zonal statistics to generate predicted values within each census block group [56].
Health Data
Our primary outcomes of interest were respiratory and cardiovascular-related hospital admissions in Tampa, FL, during 2007. Health data was obtained from the Florida Agency for Health Care Administration (AHCA) for 2007 and filtered by the principal diagnosis as designated under the Ninth International Classification of Diseases Codes (ICD-9) [61]. Health records were obtained from three AHCA datasets (i.e., emergency visits, inpatient discharges, and ambulatory/outpatient) and included patient’s zip code of residence as well as the ICD-9 code. We used the following ICD-9 codes to indicate respiratory conditions: asthma (493.00–493.22; 493.8–493.82; 493.9–493.92), wheezing (786.07), bronchitis (490.0–491.9), emphysema (492.8; 491.20), along with chronic obstructive pulmonary disease (COPD) and related diagnosis (496; 495.X; 493.2X; 494.X, 491.2X, 492.X; 491.21). Cardiovascular outcomes included heart rhythm disorders (426.00–427.99), heart failure (428.00–428.99), cerebrovascular disease (430.00–438.99), ischemic heart disease (410.0–414.99; 429.00–429.99), and peripheral vascular disease (440.00–448.99). Using Geographic Information Systems, a ratio of the block group to respective zip code areas was created throughout the City of Tampa, FL. This ratio was multiplied by the number of zip code health cases to generate a proxy of health cases at the block group level. A sum of proxies was calculated for block groups located in multiple zip codes. The proxy was then multiplied by one thousand to render the number of people per 1000 that were medically diagnosed with one of these health concerns. Both respiratory and cardiovascular outcomes were dichotomized into two categories based on their respective sample median and used as the main study outcome variables. Census block groups with an incidence rate below the median were categorized as “low” while those above the median were considered “high.”
Census Data
Demographic characteristics from patients’ home locations (based on zip code) were used as control variables. The following demographic variables were obtained from the Census Bureau’s American Community Survey 5-year estimate for 2006–2010: race (e.g., non-Hispanic white and non-Hispanic African American), ethnicity (e.g., Hispanic or Latino), median household income, population density, and housing tenure (e.g., owner and renter-occupied housing) at the block group level. Specifically, a 2010 5-year estimate of sociodemographic variables were obtained from the US Census Bureau [62, 63]. Dominant race or ethnicity for a block group was determined by the group that occupied at least 50% of the block group (see Flocks et al., 2011). A label of “no dominant race” was used to identify block groups that were not occupied by at least 50% of a racial/ethnic group. Two block groups (i.e., 120579801001 and 120579806001) are located on unique land uses which do not contain census data; thus, they were omitted from the analysis related to socioeconomic variables.
While race and ethnicity are often the focus of health disparities research in the USA [64–66], other countries emphasize the role of income in such endeavors as well [67–69]. In addition, Landry and Charkrborty [38] note the importance of disentangling race and income in equity studies, especially in Tampa. Hence, our quartiles of median household income included the following: group one (income < $29,726.50), two ($29,726.50 < income < $42250), three ($42,250 < income < $63,107.50), and four ($63,107.50 > income).
Statistical Analyses
Statistical analyses were conducted using SPSS Version 22.0 [70]. We calculated descriptive statistics (Table 1) and bivariate analysis and a comparison of means using Spearman correlation and chi-square, respectively. In addition, adjusted logistic regression models were used to assess the relationship between urban tree canopy cover and rates of respiratory and cardiovascular-related hospital admissions. The two logistic regression models included respiratory and cardiovascular outcomes as the dependent variable. The unit of analysis was the census block group. Adjusted regression models also included the following independent variables: percent home owner, median income, categories of dominant race, tree density, percent canopy cover, categories of dominant race, leaf area index, population density, and tree condition.
Table 1.
Descriptive statistics for variables within census block groups in Tampa, FL
| Variables | N | Minimum | Maximum | Mean | Median | Std. error | Standard deviation |
|---|---|---|---|---|---|---|---|
| Income (scaled to $10,000) | 369 | 0 | 25.0 | 5.2 | 4.4 | 0.1 | 3.6 |
| Percent owner | 370 | 0 | 100 | 57.7 | 63.0 | 1.4 | 27.3 |
| Population density per 1000 (sq. km) | 370 | 0.1 | 62.9 | 12.1 | 11.4 | 0.4 | 7.7 |
| Percent canopy cover | 370 | 1.7 | 83.4 | 27.7 | 26.6 | 0.6 | 13.2 |
| Leaf area index | 370 | 0.9 | 3.1 | 1.9 | 1.8 | 0.0 | 0.3 |
| Tree condition | 370 | 1.4 | 4.3 | 2.9 | 2.9 | 0.0 | 0.5 |
| Tree density | 370 | 21.9 | 1726.5 | 194.0 | 89.2 | 12.7 | 245.5 |
| Respiratory incidence rate per 1000 | 370 | 0 | 85.7 | 7.6 | 4.8 | 0.5 | 9.7 |
| Cardiovascular incidence rate per 1000 | 370 | 0 | 143.8 | 14.6 | 11.0 | 0.8 | 16.2 |
Multivariate Regression
A numerical characterization for dominant race/ethnicity (1 = White, 2 = African American, 3 = Hispanic/Latino, 4 = no dominant race) was also included in the model. For the statistical model building, first, a crude logistic regression models examining the relationship between each of the two health outcomes (respiratory and cardiovascular conditions) and each of the sociodemographic variables and tree coverage-related variables were fitted. In the final model, an adjusted logistic regression model was fitted by including all the sociodemographic and tree coverage-related variables in one model for both respiratory and cardiovascular conditions (Table 2). Results were analyzed at a confidence interval of 95% which is equivalent to p value of 0.05.
Table 2.
Multivariate association between respiratory and cardiovascular rates and with sociodemographic variables and other covariates
| Variable | Adjusted model for respiratory rates per 1000 | Adjusted model for cardiovascular rates per 1000 | ||
|---|---|---|---|---|
| Odds ratio | 95% CI | Odds ratio | 95% CI | |
| Percent owner | 0.99 | 0.98–1.01 | 1.01 | 0.99–1.02 |
| Dominant race | ||||
| White | Ref | Ref | Ref | Ref |
| African American | 2.84 | 1.28–6.29 | 0.22 | 0.10–0.47 |
| Hispanic | 1.19 | 0.54–2.64 | 0.54 | 0.24–1.23 |
| No dominant race | 1.22 | 0.16–9.04 | 1.04 | 0.12–8.79 |
| Income | 0.86 | 0.78–0.95 | 0.89 | 0.80–0.98 |
| Tree density | 0.99 | 0.99–0.99 | 0.99 | 0.99–0.99 |
| Percent canopy cover | 1.00 | 0.98–1.02 | 0.98 | 0.97–1.01 |
| Leaf area index | 0.16 | 0.06–0.42 | 2.28 | 0.91–5.74 |
| Population density | 0.79 | 0.75–0.84 | 0.77 | 0.73–0.82 |
| Tree condition | 2.13 | 1.17–3.85 | 1.68 | 0.93–3.02 |
Results
On average, the block groups in this study included a median income of about $52, 908, 57% owner occupied housing, 24% African Americans, 68% Whites, 22% Hispanics, and population density of 12,167 km2. The mean canopy coverage was about 27% of the census block group. For the overall block groups included in this study, approximately 66% (n = 243) are dominated by Whites, 19% (n = 71) by African Americans, and 13% (n = 48) Hispanic/Latino. Also, about 2% of the blockgroups (n = 8) were not designated a dominant race/ethnicity due to the similar proportions. The majority (i.e., 66%) of block groups dominated by African Americans were located in the lowest quartile for median income. Regarding the other quartiles of median income, the percentage of block groups dominated by African Americans in quartiles 2, 3, and 4 were roughly 27%, 5%, and 1% respectively. About 25% of the Hispanic/Latino population were located in block groups within the first quartile for median income, while the percentage for quartiles two through four were about 52%, 21%, and 2% respectively. Within the block groups dominated by Whites, about 12% were located in the lowest quartile for median income. However, the frequency for quartiles two through four for median income were 18%, 32%, and 37% respectively. One block group dominated by Whites did not contain data on income. Thus, these distributions imply that quartiles with the lowest levels of median income overlap block groups dominated by racial/ethnic minorities.
Figure 2 presents a dual axes for incidences of respiratory and cardiovascular conditions in relation to quartiles of percent canopy cover.
Fig. 2.
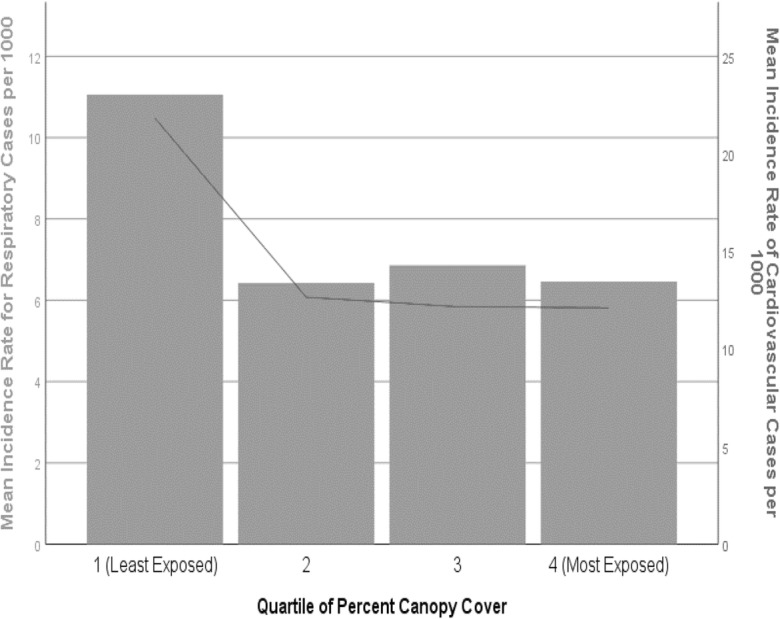
Incidence rate of respiratory and cardiovascular outcomes compared to quartiles of percent canopy cover. Quartile 1 is the lowest canopy cover and quartile 4 is the highest (bar graph represents respiratory rate per 1000; line represents cardiovascular rate per 1000)
Spearman correlation was performed between multiple variables included in this study. We observed that tree density was negatively associated with rates of both respiratory (r = − .31) and cardiovascular conditions (r = − .19), at a statistically significant level. Tree condition showed a significant positive correlation to leaf area index (r = .33) yet it was negatively correlated with tree density (r = − .13). Overall, the incidence rate of respiratory outcomes is negatively correlated with characteristics of tree cover such as leaf area index (r = − .28) and tree density (r = − .31), at a statistically significant level. However, tree density was the structural variable that showed a significant inverse association (r = − .19) with cardiovascular conditions.
Block groups with a higher percentage of canopy cover showed a significant positive correlation with median income (r = 0.21), percent owner (r = 0.29), percent White residents (r = 0.11), and leaf area index (r = 0.15). Block groups with a high percentage of Whites were also positively correlated with median income (r = 0.59), percent owner (r = 0.37), leaf area index (r = 0.25), and tree density (r = 0.11) in a significant fashion. As the percentage of African Americans increased, a significant decrease in median income (r = − 0.62), percent owner (r = − 0.36) and tree density (r = − .17) were observed. These observations align with similar findings in Tampa and other articles in the environmental justice literature [37, 38]. Block groups with a greater proportion of African-American residents were positively correlated with respiratory outcomes (r = 0.19) and population density (r = 0.12) yet negatively correlated to cardiovascular conditions (r = − .12) and leaf area index (r = − 0.27), both at a significant level. Similar to block groups with a high percentage of African Americans, areas with more Hispanic/Latino persons were also negatively correlated with median income (r = − .19) and tree density (r = − 0.11) at a significant level.
Adjusted regression estimates are shown in Table 2. Higher tree density and income showed a significant negative association with respiratory cases. Interestingly, factors such as percent canopy cover and the proportion of owner housing were not significantly associated with respiratory cases in the adjusted model. Block groups with a higher proportion of African Americans have higher odds for having above-median rate of respiratory-related hospital admissions (OR 2.84, 95% CI 1.28–6.29). Leaf area index (OR 0.16, 95% CI 0.06–0.42) and tree density (odds ratio estimate = 0.99, 95% CI 0.99–0.99) were significantly negatively associated with respiratory cases. Tree condition was positively associated with rate of respiratory admissions (OR 2.13, 95% CI 1.17–3.85).
Conversely, percent African-American residents (odds ratio estimate = 0.22, 95% CI 0.10–0.47) at the block group level was negatively associated with cardiovascular admission rates. Areas with greater leaf area index were 2.2 times more likely to have an above-median rate of cardiovascular cases. Tree density (odds ratio estimate = 0.99, 95% CI 0.99, 0.99) was significantly associated with a lower odds of cardiovascular cases. Tree condition was positively associated with rate of cardiovascular outcomes, in some cases to a great degree (OR 1.68, 95% CI 0.93, 3.02); however, some negative associations were also present and this observation was not statistically significant. Income was found to be negatively associated with above-median rate of cardiovascular admissions (OR 0.89, 95% CI 0.73–0.82).
As some suggest that the evidence on green space and physical activity has been mixed [14], one speculation for this unexpected result could be that trees in better condition or higher leaf area index can provide shade which may encourage people to have sedentary behavior instead of being physically active. Since trees on private property often produce more benefits and require less maintenance in comparison to trees on public spaces [71], perhaps well-maintained yard trees do not encourage the same level of physical activity as publicly owned green spaces. Also, as trees on private property can dominate urban forests [72], some suggest that planting trees along roads maybe particularly beneficial to health measures such as cardio-metabolic conditions [1]. Previous studies have observed a lower risk of cardiovascular concerns in some black populations in comparison to Whites [73]. For example, another Florida study observed that initial disparities for stroke mortality diminished in regression modeling after adjusting for factors such as gender and insurance status [74].
Discussion
This project extends prior studies by integrating structural factors of tree cover and exploring their relationship to respiratory and cardiovascular health outcomes across sociodemographic groups. We hypothesized that areas with less tree cover would have a higher incidence of selected health conditions. Although our results for canopy cover were not significant in the regression analysis, other structural variables of tree cover were associated in some cases. For example, tree density was significantly negatively associated with both respiratory and cardiovascular outcomes. Our observations on an inverse association between tree density and health outcomes align with another study in Toronto [1]. Also, previous ecological literature describes how tree condition supports leaf area index [75]. This article makes a number of key contributions to the literature: it accounts for the structural characteristics (e.g., tree density, tree condition, and leaf area index) of canopy cover at a small geographic scale and it explores public health implications across variations in income and race/ethnicity. In the bivariate analysis, leaf area index was negatively associated with racial/ethnic minorities and African Americans tended to reside in block groups with less tree density. Higher tree density was correlated with fewer cases of respiratory and cardiovascular admissions. By assessing the amount and quality of tree cover, we can gain additional insight on a population’s intensity of response to canopy cover with respect to health outcomes [76]. Also, compared to prior studies on green space and health, it does not utilize subjective measures of health that may be limited by personal bias and perception [1]. Similar to other research on tree cover and environmental justice, two factors can be positively related in bivariate analysis yet regression results can be negatively linked [77].
The tradeoffs between the benefits and disservices of tree cover should be kept in mind as we interpret such research findings. This may provide some insight as it relates to tree condition. The same trees that support aesthetic surroundings that encourage physical activity [10, 78] may be related to allergic sensitivities to tree pollen [42] which exacerbate respiratory concerns. It is also important to acknowledge that canopy cover is not the sole way to alleviate air pollution concerns in urban areas. Since the role that tree cover plays in reducing ambient pollutants may increase over time [79], this can affect our results and conclusions on tree cover and respiratory conditions that were analyzed for a static point in time. Multivariate regression results imply that tree density was statistically significant with lower admissions of both cardiovascular and respiratory conditions. This observation aligns with another study which found tree density to be linked with improved perceptions of health [1]. However, future research with a larger sample size of census block groups may also enhance statistical power and other study implications. As potential access to health insurance and preventive care can differ among various demographic groups, differences between the incidence and mortality of a health outcome may have also affected the sociodemographic findings in this study. Some note differences in the extent of healthcare coverage and Medicaid eligibility due to income level and race/ethnicity [80]. Although data limitations could not capture the racial/ethnic subsets in 2007, later estimates note that about 17% of Whites, 22% of African Americans, and 29% of Hispanic/Latino persons were uninsured for health coverage in 2009 [81]. Restrictions related to income and health care coverage can affect the willingness to seek medical attention. Thus, the full extent of cardiovascular and respiratory cases may not be fully captured in low-income persons. Also, the occurrence of health cases can also be related to the type of the health outcome and the individual’s perception of risk for the outcome. For example, the proxy for respiratory ailments included a mixture of acute and chronic health concerns (e.g., wheezing, bronchitis, and asthma). On the other hand, the severity of cardiovascular concerns can increase the urgency for residents to seek medical attention for these ailments in comparison to respiratory concerns.
Although structural features of tree cover (e.g., percent canopy, leaf area index, tree density) were negatively associated with cardiovascular outcomes, some variables (e.g., leaf area index) did not show a statistically significant correlation. This observation can be attributed to various possibilities. The presence of tree cover does not necessarily ensure the level of physical activity that promotes cardiovascular health. For instance, during a study of neighborhood parks in Tampa, Floyd et al. [82] observed that the majority of park users were involved in sedentary behavior, especially across demographic groups. Even though parks can provide the setting to promote physical activity, personal preferences to relax in these spaces may limit the degree of physical activity actually taking place. On the other hand, they also noted that areas predominated by high-income Hispanics and low-income Whites displayed the highest level of energy expenditure in parks [82]. Similar to Floyd et al. [82], we observed that many Tampa block groups with over 50% Hispanics also contained a high proportion of white residents. This overlap of the White and Hispanic population can make it challenging to delineate health disparities by race and ethnicity. Nonetheless, there is room to promote physically active park use in Tampa, especially in predominantly African-American neighborhoods [82].
There are also other factors to consider in the implications of these study results. The layout and maintenance of canopy cover can be affected by housing tenure which pertains to ownership or renter status of a property. Since renters do not own or manage the activities on their property, they generally do not contribute to the long-term maintenance that trees require [32]. Therefore, programs to increase tree planting programs might consider targeting the managers of rental properties along with the actual residents in outreach. However, considering sociodemographic factors in tree planting may inform existing efforts to minimize environmental inequities [79, 83, 84]. For instance, other scholars recently articulated the importance of not only increasing tree planting programs in low-income and racially/ethnically diverse communities, but also providing support for tree maintenance and community engagement [85].
On the other hand, some benefits from urban green spaces can be derived merely through their presence. Similar studies in Tampa reinforce the need for amenities, park infrastructure, and configuration to be considered in efforts to integrate nature-based health promotion [82]. Since urban growth models foresee continued development in Tampa into 2025, particularly the eastern parts of the city and its watershed [86], it is critical to evaluate how current development activities affect present and future layout of tree cover in urban areas [85]. Future studies can account for such factors.
One potential method to enhance the quality of tree cover across socioeconomic boundaries is to improve public education on tree maintenance. This is particularly important as simply planting trees may not be a suitable strategy to achieve sustainability and environmental justice goals unless factors such as the extent of coverage and quality of trees are also considered [32]. Our observations imply the majority of trees are in fair condition. Although urban landscaping preferences can vary with factors such as income, ethnicity, preferences of neighbors, and home ownership [87], this study did not include a qualitative component to assess the preference of residents. However, observations from other studies in Tampa can inform our findings. For example, another study noted that some low-income residents of East Tampa were not in favor of former tree planting programs in the vicinity of their property due to concerns related to storm damage [38]. Likewise, our Spearman analyses indicate that leaf area index is inversely related to block groups dominated by African-Americans and Hispanic/Latino groups. A number of factors can lead to this relationship such as historic inequities, inadequate planning, and sociodemographic disparities. Although environmental indicators (e.g., trees) can be applied to various ecosystems, some indicators are unique to a locations socioeconomic characteristics, spatial design, and policy needs [88]. Since Tampa is a coastal city whose location may play a role in the flux and deposition of atmospheric pollutants, future research could apply this study to a comparable inland location. Along with atmospheric conditions, the unique climatic, cultural, geographic, and population features of Tampa could encourage replication of this work in other areas.
Limitations
There are a number of limitations to note in this study. For example, the proxy for health data assumed that the human population is evenly distributed throughout the block group. While the complexities of cumulative assessment can complicate the task of establishing causal links in health research [89], people can interact with green space through multiple pathways [25]. Ultimately, studies that attempt to capture various socioeconomic factors cannot account for the full range of spatial, temporal, cultural, and personal factors that collectively play a role in human health [90]. Similar to other studies, we were unable to capture how long individuals resided in their respective block groups with the associated canopy cover before they were diagnosed with the respective health concern [68]. For example, we did not account for the use of residential pesticides and the presence of indoor mold which can also influence the onset of respiratory symptoms is outside the scope of this project. Also, age is another variable to consider in research on health disparities in heart disease [91] yet it was not explored in this study. Due to limited data, confounding factors related to personal lifestyle (e.g., physical activity, smoking, or diet), and local pollution sources were not considered. For instance, between 2008 and 2010, estimates for criteria air pollutants found that the Tampa-St. Petersburg-Clearwater area averaged 343 days with good to moderate air quality [92]. However, another project in Tampa mentioned that the city’s monitoring infrastructure does not adequately capture the ambient pollution that burdens minority communities since Tampa’s minority populations live closer to pollution sources and farther from air pollution monitors [93]. In addition, private physician visits were not captured in the health database. The extent of healthcare coverage may also be associated with the extent of cases that are reported and diagnosed by a medical professional. For example, census estimates indicate that 21% of the population in Hillsborough County was uninsured in 2007 [94]. Also, since another tree equity study in Tampa primarily focused on residential block groups [38], other studies that include all block groups (e.g., residential and non-residential) within the city boundary may affect the relationships between tree cover and human health outcomes.
Conclusions
By understanding the spatial variation involved in human-environmental systems, we are positioned to identify areas of vulnerability and adaptability in support of broader strategies in sustainable development [95]. The results of this study analyze the interaction between multiple human-environment interactions (e.g., structural features of tree cover, demographics, and health outcomes) and contribute to the literature and support previous research that urban tree cover is a factor in human health outcomes and equity. Others propose that integrating multiple aspects of vegetation such as the type, density, and degree of coverage can be included in an index to assess different characteristics of vegetation [96]. Future research efforts can explore the collective role of such characteristics of green space. As urban municipalities continue to explore and develop strategies to address inequalities in tree cover [38], such efforts may support health promotion in numerous ways.
Acknowledgments
The authors would like to acknowledge the City of Tampa who funded the study to collect land cover data as well as the vegetation inventory and analysis. Additional thanks are extended to Wayne Zipperer, Shawn Landry, Francisco Escobedo, Melissa Friedman, Michael Andreu, Michael Bowker, Cassandra Johnson Gaither, Stan Zarnoch, D. Wafula, and Seock-Ho Kim, and Francis Annor for their guidance and feedback.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kardan O, Gozdyra P, Misic B, Moola F, Palmer LJ, Paus T, et al. Neighborhood greenspace and health in a large urban center. Sci Rep. 2015;5, 11610:1–14. [DOI] [PMC free article] [PubMed]
- 2.Shanahan D, Lin B, Bush R, et al. Toward improved public health outcomes from urban nature. Am J Public Health. 2015;105(3):470–477. doi: 10.2105/AJPH.2014.302324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO. Measuring health gains from sustainable development 2012; Health in the green economy. http://www.who.int/hia/green_economy/sustainable_development_summary2.pdf?ua=1. Accessed 7 May 2014.
- 4.Grimm NB, Faeth SH, Golubiewski NE, Redman CL, Wu J, Bai X, Briggs JM. Global change and the ecology of cities. Science. 2008;319(5864):756–760. doi: 10.1126/science.1150195. [DOI] [PubMed] [Google Scholar]
- 5.Jennings V, Yun J, Larson L. Finding common ground: environmental ethics, social justice, and a sustainable path for nature-based health promotion. Healthcare. 2016;4(3):61. doi: 10.3390/healthcare4030061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jennings V, Larson L, Yun J. Advancing sustainability through urban green space: cultural ecosystem services, equity, and social determinants of health. Int J Environ Res Public Health. 2016;13(2):196. doi: 10.3390/ijerph13020196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jennings V, Johnson Gaither C. Approaching environmental health disparities and green spaces: an ecosystem services perspective. Int J Environ Res Public Health. 2015;12(2):1952–1968. doi: 10.3390/ijerph120201952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kondo M, Fluehr J, McKeon T, Branas C. Urban green space and its impact on human health. Int J Environ Res Public Health. 2018;15(3):445. doi: 10.3390/ijerph15030445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Silva RA, Rogers K, Buckley TJ. Advancing Environmental Epidemiology to Assess the Beneficial Influence of the Natural Environment on Human Health and Well-Being. ACS Publications; 2018;52(17), 9545–9555. [DOI] [PMC free article] [PubMed]
- 10.Browning M, Rigolon A. Do income, race and ethnicity, and sprawl influence the greenspace-human health link in city-level analyses? Findings from 496 cities in the United States. Int J Environ Res Public Health. 2018;15(7):1541. doi: 10.3390/ijerph15071541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coutts C, Hahn M. Green infrastructure, ecosystem services, and human health. Int J Environ Res Public Health. 2015;12(8):9768–9798. doi: 10.3390/ijerph120809768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coutts C. Public Health Ecology, J Environ Health. 2010;72(6):53–5. [PubMed]
- 13.Kondo MC, South EC, Branas CC. Nature-based strategies for improving urban health and safety. J Urban Health. 2015;92(5):1–15. [DOI] [PMC free article] [PubMed]
- 14.Hartig T, Mitchell R, de Vries S, Frumkin H. Nature and health. Annu Rev Public Health. 2014;35(1):207–228. doi: 10.1146/annurev-publhealth-032013-182443. [DOI] [PubMed] [Google Scholar]
- 15.Wolf KL, Robbins AS. Metro nature, environmental health, and economic value. Environ Health Perspect. 2015;123(5):390–398. doi: 10.1289/ehp.1408216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jackson L, Daniel J, McCorkle B, Sears A, Bush K. Linking ecosystem services and human health: the eco-health relationship browser. Int J Public Health. 2013;58(5):747–755. doi: 10.1007/s00038-013-0482-1. [DOI] [PubMed] [Google Scholar]
- 17.Larson L, Jennings V, Cloutier SA. Public parks and wellbeing in urban areas of the United States. PLoS One. 2016;11(4):e0153211. doi: 10.1371/journal.pone.0153211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tsai W-L, Floyd MF, Leung Y-F, McHale MR, Reich BJ. Urban Vegetative Cover Fragmentation in the U.S: Associations with physical activity and BMi. Am J Prev Med. 2015;50(4):509–517. [DOI] [PubMed]
- 19.Jennings V, Bamkole O. The relationship between social cohesion and urban green space: an avenue for health promotion. Int J Environ Res Public Health. 2019;16(3):452. doi: 10.3390/ijerph16030452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McCormack GR, Shiell A, Doyle-Baker PK, Friedenreich CM, Sandalack BA. Subpopulation differences in the association between neighborhood urban form and neighborhood-based physical activity. Health Place. 2014;28(0):109–115. doi: 10.1016/j.healthplace.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 21.Miles R, Coutts C, Mohamadi A. Neighborhood urban form, social environment, and depression. J Urban Health. 2012;89(1):1–18. doi: 10.1007/s11524-011-9621-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coutts C, Horner M, Chapin T. Using geographical information system to model the effects of green space accessibility on mortality in Florida. Geocarto Int. 2010;25(6):471–484. [Google Scholar]
- 23.Shen Y-S, Lung S-CC. Mediation pathways and effects of green structures on respiratory mortality via reducing air pollution. Sci Rep. 2017;7, 42854:1–9. [DOI] [PMC free article] [PubMed]
- 24.Donovan GH, Butry DT, Michael YL, Prestemon JP, Liebhold AM, Gatziolis D, Mao MY. The relationship between trees and human health: evidence from the spread of the emerald ash borer. Am J Prev Med. 2013;44(2):139–145. doi: 10.1016/j.amepre.2012.09.066. [DOI] [PubMed] [Google Scholar]
- 25.Richardson EA, Mitchell R, Hartig T, de Vries S, Astell-Burt T, Frumkin H. Green cities and health: a question of scale? J Epidemiol Community Health. 2012;66:160–165. doi: 10.1136/jech.2011.137240. [DOI] [PubMed] [Google Scholar]
- 26.Kondo MC, Low SC, Henning J, Branas CC. The impact of green stormwater infrastructure installation on surrounding health and safety. Am J Public Health. 2015;105(3):e114–e121. doi: 10.2105/AJPH.2014.302314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuo M. How might contact with nature promote human health? Promising mechanisms and a possible central path–way. Front Psychol. 2015;6, 1093. [DOI] [PMC free article] [PubMed]
- 28.Ward Thompson C, Roe J, Aspinall P, Mitchell R, Clow A, Miller D. More green space is linked to less stress in deprived communities: evidence from salivary cortisol patterns. Landsc Urban Plan. 2012;105:221–229. [Google Scholar]
- 29.EPA US. Reducing urban heat islands: compendium of strategies-trees and vegetation. Retrieved from http://www.epa.gov/heatisland/resources/pdf/TreesandVegCompendium.pdf. District of Columbia; 2011.
- 30.Nowak DJ, Greenfield EJ. Tree and impervious cover in the United States. Landsc Urban Plan. 2012;107(1):21–30. [Google Scholar]
- 31.Wheeler BW, Lovell R, Higgins SL, White MP, Alcock I, Osborne NJ, Husk K, Sabel CE, Depledge MH. Beyond greenspace: an ecological study of population general health and indicators of natural environment type and quality. Int J Health Geogr. 2015;14(1):17. doi: 10.1186/s12942-015-0009-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Flocks J, Escobedo F, Wade J, Varela S, Wald C. Environmental justice implications of urban tree cover in Miami-Dade County, Florida. Environ Justice. 2011;4(2):125–134. [Google Scholar]
- 33.Escobedo FJ, Nowak DJ. Spatial heterogeneity and air pollution removal by an urban forest. Landsc Urban Plan. 2009;90(3–4):102–110. [Google Scholar]
- 34.de Groot RS, Alkemade R, Braat L, Hein L, Willemen L. Challenges in integrating the concept of ecosystem services and values in landscape planning, management and decision making. Ecol Complex. 2010;7(3):260–272. [Google Scholar]
- 35.Brown ME, Grace K, Shively G, Johnson KB, Carroll M. Using satellite remote sensing and household survey data to assess human health and nutrition response to environmental change. Popul Environ. 2014;36(1):48–72. doi: 10.1007/s11111-013-0201-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Myers S, Gaffikin L, Golden C, et al. Human health impacts of ecosystem alteration. Proc Natl Acad Sci U S A. 2013;110(47):18753–18760. doi: 10.1073/pnas.1218656110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jennings V, Johnson Gaither C, Gragg R. Promoting environmental justice through urban green space access: a synopsis. Environ Justice. 2012;5(1):1–7. [Google Scholar]
- 38.Landry SM, Chakraborty J. Street trees and equity: evaluating the spatial distribution of an urban amenity. Environ Plan A. 2009;41(11):2651–2670. [Google Scholar]
- 39.Heynen N, Perkins HA, Roy P. The political ecology of uneven urban green space. Urban Aff Rev. 2006;42(1):3–25. [Google Scholar]
- 40.Zhou X, Kim J. Social disparities in tree canopy and park accessibility: a case study of six cities in Illinois using GIS and remote sensing. Urban For Urban Green. 2013;12(1):88–97. [Google Scholar]
- 41.Jennings V, Floyd MF, Shanahan D, Coutts C, Sinykin A. Emerging issues in urban ecology: implications for research, social justice, human health, and well-being. Popul Environ. 2017;39(1):69–86.
- 42.Lovasi GS, O'Neil-Dunne J, Lu JWT, et al. Urban tree canopy and asthma, wheeze, rhinitis, and allergic sensitization to tree pollen in a New York City birth cohort. Environ Health Perspect. 2013;121(4):494–500. doi: 10.1289/ehp.1205513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pataki DE, Carreiro MM, Cherrier J, Grulke NE, Jennings V, Pincetl S, Pouyat RV, Whitlow TH, Zipperer WC. Coupling biogeochemical cycles in urban environments: ecosystem services, green solutions, and misconceptions. Front Ecol Environ. 2011;9(1):27–36. [Google Scholar]
- 44.Benjamin MT, Winer AM. Estimating the ozone-forming potential of urban trees and shrubs. Atmos Environ. 1998;32(1):53–68. [Google Scholar]
- 45.Karl T, Harley P, Emmons L, Thornton B, Guenther A, Basu C, Turnipseed A, Jardine K. Efficient atmospheric cleansing of oxidized organic trace gases by vegetation. Science. 2010;330(6005):816–819. doi: 10.1126/science.1192534. [DOI] [PubMed] [Google Scholar]
- 46.van den Berg M, Wendel-Vos W, van Poppel M, Kemper H, van Mechelen W, Maas J. Health benefits of green spaces in the living environment: a systematic review of epidemiological studies. Urban For Urban Green. 2015;14(4):806–816.
- 47.Bureau UC. Census 2010 summary file 1 100 percent data 2010. http://factfinder2.census.gov/faces/nav/jsf/pages/searchresults.xhtml?ref=top&refresh=t. Accessed 14 August 2012.
- 48.University FS. Climate Summaries for Florida 2012. https://climatecenter.fsu.edu/products-services/summaries. Accessed 26 Sept 2016.
- 49.Nowak D, Crane D, Stevens C, Ibarra M. Brooklyn’s urban forest. USDA Forest Service General Technical Report 290. US Department of Agriculture Forest Service Northern Research Station, Newtown Square, PA. 2002.
- 50.Tools I-T. 2017. http://www.itreetools.org/resources/archives.php. Accessed 2 June 2017.
- 51.Andreu MG, Friedman MH, Landry SM, Northrop RJ. City of Tampa Urban Ecological Analysis 2006-2007. Final Report to the City of Tampa, April 24, 2008. City of Tampa, Florida; 2008.
- 52.Landry SM, Andreu MG, Friedman MH, Northrop R. A report on the City of Tampa’s existing and possible urban tree canopy: final report to the City of Tampa. Tampa, Florida; 2009.
- 53.Runfola DM, Polsky C, Nicolson C, Giner NM, Pontius RG, Jr, Krahe J, Decatur A. A growing concern? Examining the influence of lawn size on residential water use in suburban Boston, MA, USA. Landsc Urban Plan. 2013;119:113–123. [Google Scholar]
- 54.Hernández-Stefanoni JL, Dupuy J. Mapping species density of trees, shrubs and vines in a tropical forest, using field measurements, satellite multiespectral imagery and spatial interpolation. Biodivers Conserv. 2007;16(13):3817–3833. [Google Scholar]
- 55.Kevin J, Hoef J, Krivoruchko K, Lucas N. Geostatistical analyst. Redlands, California; 2003.
- 56.Jerrett M, Burnett RT, Renjun M, et al. Spatial analysis of air pollution and mortality in Los Angeles. J Epidemiol. 2005;16(6):727–736. doi: 10.1097/01.ede.0000181630.15826.7d. [DOI] [PubMed] [Google Scholar]
- 57.Duque JC, Patino JE, Ruiz LA, Pardo-Pascual JE. Measuring intra-urban poverty using land cover and texture metrics derived from remote sensing data. Landsc Urban Plan. 2015;135:11–21. [Google Scholar]
- 58.Voepel H, Ruddell B, Schumer R, Troch PA, Brooks PD, Neal A, et al. Quantifying the role of climate and landscape characteristics on hydrologic partitioning and vegetation response. Water Resour Res. 2011;47(10):1–13.
- 59.Colson V, Garcia S, Rondeux J, Lejeune P. Map and determinants of woodlands visiting in Wallonia. Urban For Urban Gree. 2010;9(2):83–91. [Google Scholar]
- 60.Chen B, Adimo OA, Bao Z. Assessment of aesthetic quality and multiple functions of urban green space from the users' perspective: the case of Hangzhou Flower Garden, China. Landsc Urban Plan. 2009;93(1):76–82. [Google Scholar]
- 61.Corporation PMI. International Classification of Diseases, Nineth Edition (ICD-9-CM). Millennium Edition ed. Los Angeles, California; 2002.
- 62.Bureau USC. Data Ferrett 2017. https://dataferrett.census.gov/. Accessed 1 June 2015.
- 63.U.S Census Bureau SE. American Community Survey 2006-2010 Summary File: Technical Documentation. https://www.socialexplorer.com/data/ACS2010_5yr/documentation/.
- 64.Hicken M, Gragg R, Hu H. How cumulative risks warrant a shift in our approach to racial health disparities: the case of lead, stress, and hypertension. Health Aff. 2011;30(10):1895–1901. doi: 10.1377/hlthaff.2010.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gee GC, Payne-Sturges D. Environmental health disparities: a framework integrating psychosocial and environmental concepts. Environ Health Perspect. 2005;113(1):A18. doi: 10.1289/ehp.7074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Payne-Sturges D, Gee GC. National environmental health measures for minority and low-income populations: tracking social disparities in environmental health. Environ Res. 2006;102(2):154–171. doi: 10.1016/j.envres.2006.05.014. [DOI] [PubMed] [Google Scholar]
- 67.Truesdale BC, Jencks C. The health effects of income inequality: averages and disparities. Annu Rev Public Health. 2016;37:413–430. doi: 10.1146/annurev-publhealth-032315-021606. [DOI] [PubMed] [Google Scholar]
- 68.Mitchell R, Popham F. Effect of exposure to natural environment on health inequalities: an observational population study. Lancet. 2008;372(9650):1655–1660. doi: 10.1016/S0140-6736(08)61689-X. [DOI] [PubMed] [Google Scholar]
- 69.Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. Socioeconomic disparities in health in the United States: what the patterns tell us. Am J Public Health. 2010;100(S1):S186–S196. doi: 10.2105/AJPH.2009.166082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Corporation I. IBM SPSS Statistics for Windows. In (Vol.Version 24). Armonk, California; 2016.
- 71.Peper PJ, McPherson EG, Simpson JR, Albers SN, Xiao Q. Central Florida community tree guide. Retrieved from https://www.itreetools.org/streets/resources/Streets_CTG/PSW_GTR230_Central_Florida_CTG.pdf. Albany, California; 2010.
- 72.Nowak DJ, Randler PB, Greenfield EJ, Comas SJ, Carr MA, Alig RJ. Sustaining America’s urban trees and forests: a Forests on the Edge report. Gen Tech Rep NRS-62 Newtown Square, PA: US Department of Agriculture, Forest Service, Northern Research Station 27 p. 2010;62.
- 73.Jensen PN, Thacker EL, Dublin S, Psaty BM, Heckbert SR. Racial differences in the incidence of and risk factors for atrial fibrillation in older adults: the cardiovascular health study. J Am Geriatr Soc. 2013;61(2):276–280. doi: 10.1111/jgs.12085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pathak EB, Sloan MA. Recent racial/ethnic disparities in stroke hospitalizations and outcomes for young adults in Florida, 2001–2006. Neuroepidemiology. 2009;32(4):302–311. doi: 10.1159/000208795. [DOI] [PubMed] [Google Scholar]
- 75.Beets PN, Bulman LS, Pearce SH. Relationships between leaf area, growth, tree health attributes, and LiDAR. 2008.
- 76.Shanahan DF, Fuller RA, Bush R, Lin BB, Gaston KJ. The health benefits of urban nature: how much do we need? Bioscience. 2015;65:476–485. [Google Scholar]
- 77.Schwarz K, Fragkias M, Boone CG, Zhou W, McHale M, Grove JM, O’Neil-Dunne J, McFadden JP, Buckley GL, Childers D, Ogden L, Pincetl S, Pataki D, Whitmer A, Cadenasso ML. Trees grow on money: urban tree canopy cover and environmental justice. PLoS One. 2015;10(4):e0122051. doi: 10.1371/journal.pone.0122051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Jennings V, Larson C, Larson L. Ecosystem services and preventive medicine: a natural connection. Am J Prev Med. 2016;50(5):642–645. doi: 10.1016/j.amepre.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 79.Shandas V, Voelkel J, Rao M, George L. Integrating high-resolution datasets to target mitigation efforts for improving air quality and public health in urban neighborhoods. Int J Environ Res Public Health. 2016;13(790) [DOI] [PMC free article] [PubMed]
- 80.Yue D, Rasmussen PW, Ponce NA. Racial/ethnic differential effects of Medicaid expansion on health care access. Health Serv Res. 2018;53(5):3640–3656. doi: 10.1111/1475-6773.12834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bureau USC. Health Insurance Coverage Status American Community Survey 1 Year Estimates. 2009.
- 82.Floyd MF, Spengler JO, Maddock JE, Gobster PH, Suau L. Environmental and social correlates of physical activity in neighborhood parks: an observational study in Tampa and Chicago. Leis Sci. 2008;30(4):360–375. [Google Scholar]
- 83.Rigolon A, Browning M, Jennings V. Inequities in the quality of urban park systems: an environmental justice investigation of cities in the United States. Landsc Urban Plan. 2018;178:156–169. [Google Scholar]
- 84.Rigolon A. A complex landscape of inequity in access to urban parks: a literature review. Landsc Urban Plan. 2016;153:160–169. [Google Scholar]
- 85.Watkins SL, Mincey SK, Vogt J, Sweeney SP. Is planting equitable? An examination of the spatial distribution of nonprofit urban tree-planting programs by canopy cover, income, race, and ethnicity. Environ Behav. 2016;49(4):1–31.
- 86.Xian G, Crane M, Steinwand D. Dynamic modeling of Tampa Bay urban development using parallel computing. Comput Geosci. 2005;31(7):920–928. [Google Scholar]
- 87.Peterson MN, Thurmond B, McHale M, Rodriguez S, Bondell HD, Cook M. Predicting native plant landscaping preferences in urban areas. Sustain Cities Soc. 2012;5:70–76. [Google Scholar]
- 88.van Oudenhoven APE, Petz K, Alkemade R, Hein L, de Groot RS. Framework for systematic indicator selection to assess effects of land management on ecosystem services. Ecol Indic. 2012;21:110–22.
- 89.Wakefield S, Baxter J. Linking health inequality and environment justice: articulating a precautionary framework for research and action. Environ Justice. 2010;3(3):95–102. [Google Scholar]
- 90.Tzoulas K, Korpela K, Venn S, Yli-Pelkonen V, Kaźmierczak A, Niemela J, James P. Promoting ecosystem and human health in urban areas using green infrastructure: a literature review. Landsc Urban Plan. 2007;81(3):167–178. [Google Scholar]
- 91.Kramer MR, Valderrama AL, Casper ML. Decomposing black-white disparities in heart disease mortality in the United States, 1973–2010: an age-period-cohort analysis. Am J Epidemiol. 2015;182(4):302–312. doi: 10.1093/aje/kwv050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.EPA US. Air Data: Air Quality Data Collected at Outdoor Monitors Across the US. 2016. https://www.epa.gov/outdoor-air-quality-data. Accessed 23 Sept 2016.
- 93.Stuart A, Mudhasakul S, Sriwatanapongse W. The social distribution of neighborhood-scale air pollution and monitoring protection. J Air Waste Manage Assoc. 2009;59(5):591–602. doi: 10.3155/1047-3289.59.5.591. [DOI] [PubMed] [Google Scholar]
- 94.Prevention USCBatCoDCa. Small area health insurance estimates. 2008.
- 95.Chapin FS, Lovecraft AL, Zavaleta ES, Nelson J, Robards MD, Kofinas GP, Trainor SF, Peterson GD, Huntington HP, Naylor RL. Policy strategies to address sustainability of Alaskan boreal forests in response to a directionally changing climate. Proc Natl Acad Sci U S A. 2006;103(45):16637–16643. doi: 10.1073/pnas.0606955103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gupta K, Kumar P, Pathan SK, Sharma KP. Urban neighborhood green index: a measure of green spaces in urban areas. Landsc Urban Plan. 2012;105(3):325–335. [Google Scholar]