Abstract
Depression among Black transgender women (BTW) in the USA is an often understudied mental health concern with far-reaching consequences for overall physical and mental health at both the individual and community levels. Intimate partner violence (IPV) among BTW is also a frequently understudied and important social determinant of health in need of further exploration. This study sought to address the gap in research on the relationship between IPV and depression among BTW using a time- and location-based community sample of BTW from six US cities. In addition, it sought to explore the potential protective or suppressive effect of perceived social support on this relationship. Generalized structural equation models were used to assess conditional direct and indirect effects of IPV on depression via the suppression effect of perceived social support. Evidence was found of a statistically significant conditional direct effect of IPV on depression as well as a statistically significant suppression effect for perceived social support. Specifically, there was a 20% lower likelihood of increased depressive symptomatology for every 1-unit increase in perceived social support reported by participants. These findings indicated that perceived social support may be an important intervention point for helping to improve the mental health and well-being of BTW.
Keywords: Depression, Black, “African American” transgender, Intimate partner violence, Social support
Background
In the USA, transgender women report higher levels of depression than the general population [1–4]. For example, while the CDC estimates that 8.1% of adults in the USA have had depression over a given 2-week period [5], yet one Internet-based study of transgender women found that 44.1% of the sample reported depression symptomology consistent with clinical depression [2]. Prevalence of depression is even higher among Black transgender women (BTW) with one recent study indicating 49.3% of BTW reported past week depression symptomology [6]. Because depression is a risk factor for other negative downhill health outcomes such as suicidal thoughts and attempts [7], as well as HIV incidence [8–10], efforts to address depression in this population are needed.
Exploring how other health outcomes are associated with or predictive of depression among BTW could elucidate ways in which to improve or prevent depression. One potential predictor of depression in this population in need of exploration is intimate partner violence (IPV). While several other potential predictors of depression have been explored (e.g., physical and verbal violence, sex work, and gender identity) [2, 11–14], IPV has received less attention. There is a growing amount of evidence suggesting that IPV is directly associated with depression and other negative mental health outcomes [15, 16]. However, most of this research has been conducted among non-transgender (i.e., cisgender) populations [17, 18]. This is concerning given the high prevalence of IPV reported by transgender individuals. Nationally, rates of IPV among sexual and gender minority individuals are similar to or greater than the rest of the population [19]. In a recent survey study, 72% of transgender/gender non-conforming respondents reported at least one form of IPV [20]. Moreover, research related to IPV among BTW is scarcer still with few studies exploring prevalence and predictors of IPV [21] and no studies exploring IPV as a predictor of other physical and mental health outcomes [22–24].
Another factor associated with depression in the general population and among sexual and gender minorities but underexplored among BTW is social support [13, 25]. Studies within cisgender communities have explored the role of different types of social support on the relationship between IPV and depressive symptomatology [26]. These studies have shown social support may behave as either a moderator [27, 28] or a mediator [29] of said relationship. In qualitative research, transgender women have indicated that social support plays a significant role in relation to other aspects of their health such as HIV testing and care [30]. Therefore, it is important to explore whether social support could potentially mediate the relationship between IPV and depression. Such an exploration could uncover possible public health intervention points that could be used to address depression, and its deleterious sequelae, among BTW.
We sought to fill these research gaps by analyzing survey data collected from a community-based sample of BTW across six different US cities. The objectives of this research were as follows: first, to assess whether there was an association between IPV and depressive symptomatology among BTW, and second, to determine the potential suppressive or protective effect of perceived social support on this relationship.
Methods
Participants
Data for this study comes from the Promoting Our Worth, Equality, and Resilience (POWER) study [6, 31, 32]. Participants were recruited from 2014 to 2017 at Black Pride events in six cities: Atlanta, GA; Detroit, MI; Houston, TX; Memphis, TN; Philadelphia, PA; and Washington, DC. Individuals were eligible to participate in POWER if they (1) were assigned male sex at birth, (2) reported having a male sexual partner in their lifetime, (3) were 18 years or older, and (4) were able to give informed consent in English. This study only includes those who (1) identified as “Black” or “African American” and (2) identified as female, transgender, or reported having transitioned from male to female gender [33].
Data Collection Procedures
POWER employed time location sampling to recruit participants [34]. In each city, POWER randomly selected events in 2-h recruitment time blocks from all official Black Pride events. At each selected event, individuals were approached and invited to participate in the study. Once screened for eligibility via electronic tablet, participants completed an anonymous self-administered, behavioral health questionnaire on the same electronic tablet. The questionnaire was designed to take approximately 20 min to complete. To prevent duplication of participants, a unique identifier code [35] was created for each participant (for further information regarding data collection procedures, see references [1–4]). All study procedures were approved by the Institutional Review Board at [blinded for review].
Measures
Demographics
Participants were asked about their age, level of education, employment status, and relationship status and were filed by city of participation and year of study involvement. Age was measured in years. Four levels were used to measure education: less than high school, high school diploma, some college, and college diploma or more. Six categories assessed employment status: full-time, part-time, full-time student, retired, unemployed, and other. Five categories were used to measure relationship status: married (legally recognized), married (not legally recognized), partnered, single, other. Dummy variables were created for all categorical demographic variables prior to model inclusion.
IPV
IPV was assessed with the following yes/no item: “In the past year, have you been in a relationship with a partner who has ever hit, kicked, slapped, beaten or in any other way physically assaulted you?” Participants who endorsed a response of “yes” were given an item score of 1, while participants who endorsed a response of “no” were given an item score of 0.
Depression
The Center for Epidemiologic Studies Depression 10 (CES-D 10) measured past week depressive symptomatology [36]. Items were scored using a four-point Likert-type scale ranging from 0 to 3, with higher scores indicating increased depressive symptomatology. Items were then summed to create a composite score for depressive symptoms ranging from 0 to 30.
Perceived Social Support
Perceived social support was measured using a summed composite score derived from six questions that asked: “To what degree to you feel you receive support from your/the (1) family; (2) friends; (3) church; (4) work environment; (5) gay community; (6) Black community?” Each item was assessed using a Likert-type scale with response options of: (1) none; (2) a little; (3) somewhat; and (4) a lot. Scores ranged from 0 to 24 with a mean in our sample of 8.97. Given its creation for this study, further factor and reliability analyses were performed prior to model inclusion (please see “Results” section for further details).
Homelessness
Past year homelessness was assessed with one yes/no item: “In the past 12 months, have you been homeless at any time? By homeless, I mean you were living on the street, in a shelter, in a Single Room Occupancy hotel (SRO), or in a car.” Participants who responded “yes” to this question were given a score of 1, while participants who responded “no” were given a score of 0.
Health Insurance Coverage
The presence of health insurance coverage was assessed with the following yes/no item: “Do you currently have health insurance or health care coverage?” Respondents who answered “yes” were given an item score of 1, while respondents who answered “no” were given an item score of 0.
Data Analysis
In order to explore the possible suppression effect [37] of perceived social support on depressive symptoms among BTW who have experienced IPV, we initially explored demographic characteristics, as well as the bivariate relations between these demographic characteristics and depression using t tests and ANOVAs. The perceived social support scale was created specifically for this study, so an exploratory factor analysis and reliability analysis were performed on the scale, which was then assessed for its relation with depression.
Following these initial analyses, generalized structural equation models (GSEMs) using a negative binomial link function, in order to account for the distribution of the Likert-type scales of depression and perceived social support, were constructed. The first model assessed for the conditional direct path between past year IPV and depression, while controlling for statistically significant demographic characteristics, the city in which participants were assessed, and their year of study participation. For all categorical demographic covariates the referent groups were chosen based on the groups less likely to show depressive symptomatology (e.g., those who were employed full-time, had higher educational obtainment, and/or were in legally recognized marriages). Subsequently, an indirect effect or suppression model was constructed, introducing a path between IPV and perceived social support, as well as perceived social support and depression. This model also controlled for the same demographic characteristics, the city in which participants were surveyed, and the year of study participation.
Generalized structural equation models were used for these analyses in order to account for measurement error among our variables, as well as to model all three pathways among the independent, suppressing, and dependent variables simultaneously, all while controlling for possible covariates/ confounders [38, 39]. Listwise deletion was used for missing data found within the suppression and dependent variables (i.e., perceived social support and depression), resulting in n = 476 for the conditional direct effect model and n = 478 for the conditional indirect effect model. Given the relatively recent addition of GSEM as a technique used to assess for mediation, bias-corrected bootstrapped confidence intervals using 1000 bootstrapped samples were constructed to assess for the significance of each path. In addition, given the large size of our sample, a traditional Wald test and 95% confidence interval were used to assess the significance of the indirect effect (Little, et al., 2007). All demographic, bivariate, and GSEM analyses were performed using SPSS 24© (IBM Corp, Armonk, NY) and STATA 15© (Stata Corp, College Station, TX), while the Wald test and the 95% confidence intervals for the indirect effect were computed manually.
Results
Over the course of the 4 years of sampling, data were collected from 493 BTW. Of those sampled, 58.5% (n = 283) reported a high school level of education or less, 42.9% (n = 208) were employed full-time, 66.9% (n = 325) were single, and 41.8% (n = 202) reported experiencing homelessness in the year prior to assessment. The mean age of BTW sampled was 30.9 years old, with 44.7% (n = 220) reporting that they had experienced IPV in the 12 months prior to study involvement. Further sociodemographic information can be found in Table 1.
Table 1.
Demographic overview of Black transgender women in POWER
| n = 493% (n) | |
|---|---|
| Education | |
| Less than high school | 27.2 (132) |
| High school degree | 31.3 (151) |
| Some college | 21.7 (105) |
| College degree or more | 20.0 (97) |
| Employment | |
| Full-time | 42.9 (208) |
| Part-time | 13.8 (67) |
| Full-time student | 5.6 (27) |
| Retired | 4.3(21) |
| Unemployed | 29.3 (142) |
| Other | 4.1 (20) |
| Relationship status | |
| Married, legally recognized | 10.1 (49) |
| Married, not legally recognizes | 6.8 (33) |
| Partnered | 12.1 (59) |
| Single | 66.9 (325) |
| Other | 4.1 (20) |
| Age (mean (SD)) | 30.9 (10.9) |
| City | |
| Atlanta, GA | 20.9 (103) |
| Detroit, MI | 29.4 (145) |
| Houston, TX | 23.7 (117) |
| Memphis, TN | 1.2 (6) |
| Philadelphia, PA | 9.7 (48) |
| Washington, DC | 15.0 (74) |
| Year | |
| 2014 | 28.2 (139) |
| 2015 | 30.2 (149) |
| 2016 | 27.0 (133) |
| 2017 | 14.6 (72) |
| Homeless, past year | 41.8 (202) |
| Presence of healthcare coverage | 79.1 (390) |
| Intimate partner violence | 44.7 (220) |
| Depression (mean (SD)) | 9.5 (5.1) |
| Family support (mean (SD)) | 1.5 (1.1) |
| Friend support (mean (SD)) | 1.6 (1.2) |
| Church support (mean (SD)) | 1.3 (1.1) |
| Work support (mean (SD)) | 1.4 (1.1) |
| Gay community support (mean (SD)) | 1.6 (1.2) |
| Black community support (mean (SD)) | 1.5 (1.1) |
For our sample the Cronbach’s alpha for the CES-D 10 was equal to 0.70. A bivariate exploration of the potential covariates of depression within our sample showed that education (p = 0.01), employment status (p < 0.001), relationship status (p = 0.05), past year homelessness (p < 0.001), and experiencing IPV (p < 0.001) were all statistically significantly related to differential rates of depressive symptoms among BTW. Given its lack of statistical significance in relation to depression, health insurance coverage was not included in our GSEM models. Further bivariate relations can be found in Table 2.
Table 2.
One-way analysis of variance of depression symptomology
| Depression Score Mean (SD) | p | |
|---|---|---|
| Education | ||
| Less than high school | 10.6 (5.0) | 0.01 |
| High school degree | 8.6 (5.2) | |
| Some college | 9.2 (5.1) | |
| College degree or more | 9.9 (4.9) | |
| Employment | ||
| Full-time | 8.7(5.1) | < 0.001 |
| Part-time | 10.7 (4.1) | |
| Full-time student | 7.0 (5.3) | |
| Retired | 9.6 (4.7) | |
| Unemployed | 10.7 (5.2) | |
| Other | 9.3 (5.5) | |
| Relationship status | ||
| Married, legally recognized | 8.1 (4.0) | 0.05 |
| Married, not legally recognizes | 11.3 (4.2) | |
| Partnered | 9.2 (5.5) | |
| Single | 9.7 (5.2) | |
| Other | 8.1 (5.0) | |
| Year | ||
| 2014 | 9.1 (5.0) | 0.43 |
| 2015 | 10.0 (5.2) | |
| 2016 | 9.3 (5.0) | |
| 2017 | 9.9 (5.6) | |
| Homeless, past year | 11.0 (5.2) | < 0.001 |
| Presence of healthcare coverage | 9.5 (5.1) | 0.88 |
| Intimate partner violence | 11.3 (4.5) | < 0.001 |
| Family support | ||
| None | 9.2 (4.9) | < 0.001 |
| A little | 10.9 (4.2) | |
| Somewhat | 11.1 (5.2) | |
| A lot | 7.4 (5.4) | |
| Friend support | ||
| None | 8.9 (4.5) | < 0.001 |
| A little | 11.6 (4.2) | |
| Somewhat | 10.7 (4.4) | |
| A lot | 8.0 (5.8) | |
| Church support | ||
| None | 9.2 (4.8) | < 0.001 |
| A little | 10.6(4.5) | |
| Somewhat | 10.3(4.8) | |
| A lot | 7.8 (6.0) | |
| Work support | ||
| None | 9.4 (4.6) | < 0.001 |
| A little | 10.9 (4.4) | |
| Somewhat | 10.5 (5.7) | |
| A lot | 7.3 (5.3) | |
| Gay community support | ||
| None | 9.4 (4.6) | < 0.001 |
| A little | 11.1 (4.3) | |
| Somewhat | 11.2 (5.3) | |
| A lot | 7.3 (5.2) | |
| Black community support | ||
| None | 9.6 (4.8) | < 0.001 |
| A little | 10.7 (4.5) | |
| Somewhat | 10.5 (5.2) | |
| A lot | 7.6 (5.5) | |
The exploratory factor analysis of the perceived social support scale supported a single-factor structure, accounting for 65% of the total variance observed, with an eigenvalue of 3.91. Factor loadings for this single factor ranged from 0.73 (for support from church community) to 0.83 (for support from work colleagues). A reliability analysis found that the Cronbach’s alpha for the total scale was equal to 0.89, showing strong reliability for the scale overall. An exploration of the relationship between social support and depression within our sample found a statistically significant negative relationship (r = − 0.17, p < 0.01.)
In order to assess the potential relationship between IPV and depression among BTW in our sample, as well as the potential suppression effect of social support on the relationship between IPV and depression, GSEMs were run using a negative binomial link function. An initial GSEM assessing the relationship between IPV and depression, while controlling for participants’ age, education, employment status, experiences of homelessness, relationship status, year sampled, and city of sampling, showed a statistically significant positive relationship. Specifically, an incidence rate ratio (IRR) of 1.36 was found with a bias-corrected bootstrapped 95% confidence interval (CI) of 1.23 to 1.50, indicating a 36% increased likelihood of reporting higher depressive symptoms among those who reported past year experiences of IPV within our sample (please see Table 3 and Fig. 1).
Table 3.
Generalized structural equation model (GSEM) results for conditional direct effect of intimate partner violence on depression (Path C Model, Fig. 1)
| Incidence Rate Ratio (IRR) | Bootstrapped Standard Error | BCBa 95% CI |
|
|---|---|---|---|
| Intimate partner violence, past year | 1.36 | 0.70 | 1.23, 1.50 |
| Age | 1.00 | 0.002 | 1.00, 1.01 |
| Less than high school degreeb | 0.98 | 0.06 | 0.86, 1.11 |
| High school degreeb | 0.84 | 0.06 | 0.72, 0.96 |
| Some collegeb | 1.02 | 0.08 | 0.88, 1.20 |
| Employed part-timec | 1.27 | 0.08 | 1.12, 1.45 |
| Full-time studentc | 0.83 | 0.12 | 0.58, 1.06 |
| Retiredc | 1.03 | 0.10 | 0.84, 1.24 |
| Unemployedc | 1.17 | 0.08 | 1.03, 1.33 |
| Other form of employmentc | 1.09 | 0.18 | 0.75, 1.44 |
| Married, not legally recognized | 1.29 | 0.13 | 1.06, 1.60 |
| Partnered | 1.20 | 0.13 | 0.98, 1.50 |
| Single | 1.32 | 0.11 | 1.14,1.58 |
| Other relationship status | 1.01 | 0.16 | 0.72, 1.36 |
| Homelessness, past year | 1.12 | 0.06 | 1.00,1.26 |
| Philadelphiad | 0.93 | 0.09 | 0.77,1.14 |
| Houstond | 0.89 | 0.06 | 0.78,1.02 |
| Washington DCd | 0.86 | 0.07 | 0.73,1.01 |
| Detroitd | 1.02 | 0.07 | 0.88,1.17 |
| Memphisd | 0.69 | 0.08 | 0.53, 0.85 |
| Survey year 2 | 1.06 | 0.07 | 0.93,1.20 |
| Survey year 3 | 0.99 | 0.07 | 0.86, 1.12 |
| Survey year 4 | 1.03 | 0.09 | 0.86, 1.20 |
GSEM model used a negative binomial link function
aBias-corrected bootstrapped 95% confidence interval (1000 bootstrapped samples)
bReferent was having a college degree or higher level of education
cReferent was being employed full-time
dReferent city of participation was Atlanta
Fig. 1.
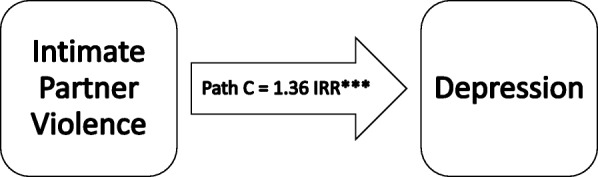
Generalized structural equation model (GSEM) for conditional direct effect of intimate partner violence on depression (path C model, incidence rate ratio (IRR), n = 476, see Table 3)
When assessing for the potential suppression effect of perceived social support on the relationship between IPV and depression, a GSEM using the negative binomial link function and controlling for the same participant characteristics/experiences above found a statistically significant conditional suppression effect. Specifically, the conditional indirect effect for the ab path was equal to the IRR path between IPV and social support (IRR = 0.81, bias-corrected bootstrapped 95% CI 0.69–0.92) multiplied by the IRR path between social support and depression (IRR = 0.98, bias-corrected bootstrapped 95% CI 0.97–0.99), resulting in a conditional IRR indirect effect of 0.80 [38, 39]. Given our large sample size, a Wald test using the non-exponentiated path coefficients and the bias-corrected bootstrapped standard errors was computed, equaling 2.09. When compared to a standard normal distribution, this statistic indicated that the indirect path was statistically significant at the p < 0.05 level, with a 95% CI for the conditional IRR indirect effect of 0.68 to 0.91. Due to the inconsistent suppression effect (i.e., the difference in the positive and negative effects between the direct and indirect paths in this model) an overall mediation ratio (PM) was not computed [40]. Interpretatively, the 0.80 conditional IRR indirect effect implies that among the BTW sampled, while holding all other covariates constant and specifically for those who endorsed past year experiences of IPV, there was a 20% lower likelihood of increased depressive symptomatology for every 1-unit increase in perceived social support reported by participants (please see Table 4 and Fig. 2).
Table 4.
Generalized structural equation model (GSEM) results for conditional indirect effect of intimate partner violence on depression (Path A-BC’ Model, Fig. 2).
| Variable | Incidence Rate Ratio (IRR) | Bootstrapped Standard Error | BCBa 95% CI |
|---|---|---|---|
| Path A (Perceived Social Support) | |||
| Intimate partner violence, past year | 0.81 | 0.06 | 0.69, 0.92 |
| Age | 1.00 | 0.003 | 1.00, 1.01 |
| Less than high school degreeb | 0.78 | 0.08 | 0.64, 0.94 |
| High school degreeb | 0.94 | 0.09 | 0.79, 1.14 |
| Some collegeb | 0.92 | 0.08 | 0.78, 1.11 |
| Employed part-timec | 1.10 | 0.09 | 0.92, 1.27 |
| Full-time studentc | 0.96 | 0.14 | 0.69, 1.25 |
| Retiredc | 1.10 | 0.15 | 0.79, 1.37 |
| Unemployedc | 0.99 | 0.08 | 0.83, 1.12 |
| Other form of employmentc | 0.79 | 0.13 | 0.55, 1.04 |
| Married, not legally recognized | 1.14 | 0.21 | 0.79, 1.67 |
| Partnered | 1.44 | 0.23 | 1.07, 1.97 |
| Single | 1.38 | 0.21 | 1.04, 1.87 |
| Other relationship status | 1.11 | 0.32 | 0.60, 1.84 |
| Homelessness, past year | 0.87 | 0.06 | 0.76, 1.02 |
| Philadelphiad | 1.07 | 0.13 | 0.84, 1.35 |
| Houstond | 0.97 | 0.09 | 0.82, 1.16 |
| Washington DCd | 0.85 | 0.10 | 0.67, 1.06 |
| Detroitd | 0.98 | 0.08 | 0.82, 1.17 |
| Memphisd | 1.67 | 0.50 | 0.73, 2.59 |
| Survey year 2 | 0.92 | 0.07 | 0.78, 1.07 |
| Survey year 3 | 1.11 | 0.09 | 0.94, 1.31 |
| Survey year 4 | 0.95 | 0.10 | 0.78, 1.16 |
| Paths BC’ (Depression)ara> | |||
| Intimate partner violence, past year | 1.34 | 0.07 | 1.21, 1.48 |
| Perceived social support | 0.98 | 0.005 | 0.97, 0.99 |
| Age | 1.00 | 0.002 | 1.00, 1.01 |
| Less than high school degreeb | 0.97 | 0.07 | 0.85, 1.11 |
| High school degreeb | 0.85 | 0.06 | 0.74, 0.97 |
| Some collegeb | 1.04 | 0.08 | 0.89, 1.20 |
| Employed part-timec | 1.28 | 0.09 | 1.11, 1.48 |
| Full-time studentc | 0.82 | 0.11 | 0.62, 1.06 |
| Retiredc | 1.05 | 0.11 | 0.81, 1.25 |
| Unemployedc | 1.15 | 0.07 | 1.01, 1.29 |
| Other form of employmentc | 1.05 | 0.17 | 0.76, 1.41 |
| Married, not legally recognized | 1.30 | 0.14 | 1.06, 1.62 |
| Partnered | 1.24 | 0.14 | 1.02, 1.61 |
| Single | 1.35 | 0.13 | 1.15, 1.65 |
| Other relationship status | 1.02 | 0.16 | 0.74, 1.38 |
| Homelessness, past year | 1.11 | 0.06 | 0.99, 1.23 |
| Philadelphiad | 0.95 | 0.09 | 0.79, 1.15 |
| Houstond | 0.90 | 0.07 | 0.79, 1.04 |
| Washington DCd | 0.85 | 0.07 | 0.73, 1.02 |
| Detroitd | 1.03 | 0.08 | 0.90, 1.19 |
| Memphisd | 0.76 | 0.10 | 0.58, 0.97 |
| Survey year 2 | 1.03 | 0.06 | 0.91, 1.16 |
| Survey year 3 | 1.00 | 0.06 | 0.88, 1.13 |
| Survey year 4 | 1.03 | 0.09 | 0.88, 1.23 |
GSEM model used a negative binomial link function
aBias-corrected bootstrapped 95% confidence interval (1000 bootstrapped samples)
bReferent was having a college degree or higher level of education
cReferent was being employed full-time
dReferent city of participation was Atlanta
Fig. 2.
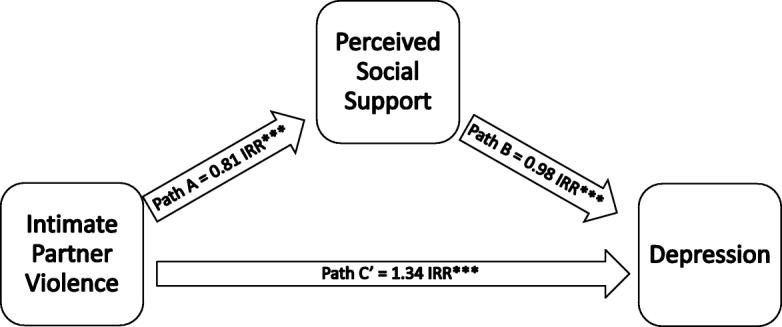
Generalized structural equation model (GSEM) for conditional direct effect of intimate partner violence on depression (path A-BC’ model, incidence rate ratio (IRR), n = 478, see Table 4)
Discussion
BTW face an epidemic of IPV. In our sample, 44.7% of BTW reported experiencing past year IPV. Our results showed that IPV is associated with negative downstream health outcomes as BTW in our sample who reported past year IPV experienced a 36% increased likelihood of reporting higher depressive symptomology. Because perceived social support lowered the likelihood of increased depressive symptomology among BTW in our sample, our results also suggest social support may be a way to mitigate the relationship between IPV and depression.
Because of the high prevalence of IPV among BTW in our sample, as well as its association with depression, we recommend future interventions among BTW should focus on thwarting instances of IPV before they happen. Increasing economic opportunities for BTW could help reduce experiences of IPV in this population. Transgender individuals face discrimination and stigma that lead to limited economic opportunity. This is illustrated in the prevalence of homelessness (12.9%), unemployment (23.0%), job discrimination (35.3%), and social service discrimination (40.6%) reported by transgender women [41]. Because BTW experience racial discrimination in addition to gender-based discrimination due to their intersecting identities [21, 42], they could be at even more of an economic disadvantage than transgender women generally [43]. This in turn could leave them vulnerable to economic dependency on an intimate partner. As economic hardship and economic dependency on an intimate partner are risk factors for IPV in other populations [44], programs aimed at increasing economic standing among BTW may help prevent IPV. Such programs could focus on housing BTW and/or assisting BTW with securing positions offering more than a sustenance wage. Additionally, future research should explore what factors are associated with IPV among BTW as such research could help inform intervention development aimed at thwarting occurrences of IPV among BTW.
While ideally interventions would be able to eliminate all instances of IPV, this is highly unlikely. Because of this, interventions should also focus on increasing social support for BTW who have experienced IPV. Perceived social support lowered the likelihood of increased depressive symptomology among BTW in our sample. Interventions should build upon existing structures to provide BTW with accessible opportunities for social support; one opportunity may be formalizing structures already in place. For example, transgender women have indicated they establish their social networks through clinics and services where they meet other transgender individuals with similar or shared experiences [45, 46]. Therefore, a clinic providing transgender-specific health care could be an ideal place to screen for IPV, and offer formal social support in the form of a peer navigator or support groups. In addition to the clinical setting, interventions aimed at increasing social support should be developed and implemented in non-clinical settings as not all BTW have access to medical care. Because numerous community-based organizations supporting BTW exist outside of healthcare environments in many places, this could be potential location in which to increase social support. Interventions could aim to connect BTW to these organizations, and local state and municipal governments and foundations could increase financial support of these organizations in order to improve their ability to provide support for BTW.
Limitations
A major limitation of our analyses is the lack of longitudinal data regarding the intra-individual change in depressive symptomatology among participants, especially as it relates to IPV and perceived social support. Despite the theoretical support for the directionality of the proposed relations in these analyses, the lack of longitudinal data makes it impossible to make causal claims in our findings [38]. Notwithstanding this limitation, this is the largest analysis of the associations between IPV, perceived social support, and depression among BTW in the USA. It is our hope that this initial exploration will help guide future longitudinal research in this area to better understand the distinct mechanisms of suppression that perceived social support may have on the relationship between IPV and depression among BTW, as well as help guide future public health and mental health-based intervention work with BTW.
Another limitation of this study is the conceptualization of IPV solely along the lines of physical assault. Specifically, IPV is a complex manifestation of controlling, aggressive, and coercive behaviors that may exist within a romantic pairing, including both mental and sexual abuse/coercion. As such, the ability to generalize these findings to the IPV experiences within the realms of psychological and/or sexual abuse/coercion within our sample and among BTW in general does not exist [38]. Despite this limited definition of IPV, given the high rates of physically based IPV reported by the participants in this study, it will be important to further explore in future research the ways in which mental and sexual coercion may overlap with physically based IPV, how these experiences may be related to depression among BTW, and the distinct ways in which perceived social support may attenuate these relations.
A further limitation of this study is the use of time location sampling within urban areas at Black Pride events. The limited geographic and time-based sampling methods of this study make it difficult to generalize our findings to the experiences of BTW outside of major urban areas within the USA, or to the experiences of BTW outside of the USA. Despite this lack of generalizability, these findings support the need for further exploration into the unique interplay of racial and gender-minority status as they relate to issues of IPV, perceived social support, and depression. This is especially true given the deleterious psychological, social, occupational, financial, and physical sequelae associated with experiences of both IPV and depression within the general population overall and within Black and transgender communities specifically.
Similarly, it is important to note that the study from which the data were derived was primarily focused on recruiting and elucidating the experiences of Black gay, bisexual, and other men who have sex with men (MSM). As such, the BTW recruited as part of this study may not be fully representative of BTW overall, especially those who may not interact with Black gay male communities or frequent Black gay pride events in the USA. Nevertheless, it is of note that the number of BTW recruited for this study represented roughly 10% of our overall study sample [6, 32], providing a unique perspective into the lives of BTW who do frequent Black gay pride events and are socially connected to their local Black gay male communities.
Conclusions
These analyses build on a growing body of literature exploring the experiences of BTW in the USA. To date, very little attention has been paid to the unique experiences that BTW face regarding IPV, perceived social support, and depression in the USA. The results of this study as well as previous studies suggest that it is vital to continue exploring the unique experiences of BTW, both positive and negative, in order to better work with BTW and their communities to improve overall health and well-being in this population. Such research will need to focus on the unique manifestations of IPV, social support, and depression experienced by BTW. In addition, intervention work focused on assisting BTW should make use of strength-based approaches to intervention development in order to help bring about a more just, healthy, and thriving world in which BTW may live up to their fullest potentials as vital parts of their local and global communities. As such, it is our hope that these analyses may help to continue the essential dialogs required to push such research, intervention work, and vital collaborations forward in the years to come, so as to help improve the lives and day-to-day experiences of BTW overall.
Acknowledgements
We thank the Center for Black Equity and local Black Pride organizations for partnering with us to implement POWER, the community-based organization who performed onsite HIV testing on the study’s behalf, the thousands of study participants who volunteered their time to contribute to this research, and members of the POWER Study Team who made data collection possible.
The local Black Pride organizations are as follows: D.C. Black Pride, Detroit’s Hotter than July, Houston Splash, In the Life Atlanta, Memphis Black Pride, and Philadelphia Black Pride.
The community-based organizations who performed onsite HIV testing are as follows: Atlanta: AID Atlanta, AIDS Health Care Foundation, NAESM; Detroit: Community Health Awareness Group, Horizons Project, Unified; Houston: Avenue 360, Houston AIDS Foundation, Positive Efforts; Memphis: Friends for Life; Philadelphia: Access Matters, Philadelphia FIGHT; Washington, DC: Us Helping Us.
The members of POWER study team are as follows: Center for Black Equity: Earl D. Fowlkes, Jr., Michael S. Hinson, Jr.; Columbia University: Patrick A. Wilson; University of Connecticut: Lisa A. Eaton; Rutgers University: Henry Fisher-Raymond; University of Pittsburgh: Leigh A. Bukowski, Cristian J. Chandler, Derrick D. Matthews, Steven P. Meanley, Jordan M. Sang, and Ronald D. Stall.
This study was partially supported by the National Institute for Nursing Research (R01NR013865) and by the National Institute for Mental Health (5T32MH094174–08).
Disclosures
This original, unpublished manuscript has not been submitted for review to any other journal, and has been read and approved by all co-authors.
Compliance with Ethical Standards
All study procedures were approved by the Institutional Review Board at [University of Pittsburgh].
Footnotes
Leigh A. Bukowski and Melvin C. Hampton are co-first authors
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Leigh A. Bukowski, Phone: +1-814-323-0689, Email: lab108@pitt.edu
Melvin C. Hampton, Email: mch353@nyu.edu
References
- 1.Clements-Nolle K, Marx R, Guzman R, Katz M. HIV prevalence, risk behaviors, health care use, and mental health status of transgender persons: implications for public health intervention. Am J Public Health. 2001;91(6):915–921. doi: 10.2105/ajph.91.6.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bockting WO, Miner MH, Swinburne Romine RE, Hamilton A, Coleman E. Stigma, mental health, and resilience in an online sample of the US transgender population. Am J Public Health. 2013;103(5):943–951. doi: 10.2105/AJPH.2013.301241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nuttbrock L, Bockting W, Rosenblum A, Hwahng S, Mason M, Macri M, Becker J. Gender abuse, depressive symptoms, and HIV and other sexually transmitted infections among male-to-female transgender persons: a three-year prospective study. Am J Public Health. 2013;103(2):300–307. doi: 10.2105/AJPH.2011.300568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Witcomb GL, Bouman WP, Claes L, Brewin N, Crawford JR, Arcelus J. Levels of depression in transgender people and its predictors: results of a large matched control study with transgender people accessing clinical services. J Affec Disord. 2018;235:308–315. doi: 10.1016/j.jad.2018.02.051. [DOI] [PubMed] [Google Scholar]
- 5.Brody DJ, Pratt LA, Hughes JP. Prevalence of depression among adults aged 20 and over: United States, 2013–2016 Hyattsville, MD: National Center for Health Statistics. 2011.: National Center for Health Statistics 2018.
- 6.Bukowski LA, Chandler CJ, Creasy SL, Matthews DD, Friedman MR, Stall RD. Characterizing the HIV care continuum and identifying barriers and facilitators to HIV diagnosis and viral suppression among black transgender women in the United States. JAIDS. 2018;79(4):413–420. doi: 10.1097/QAI.0000000000001831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clements-Nolle K, Marx R, Katz M. Attempted suicide among transgender persons: the influence of gender-based discrimination and victimization. J Homosex. 2006;51(3):53–69. doi: 10.1300/J082v51n03_04. [DOI] [PubMed] [Google Scholar]
- 8.Stall R, Mills T, Williamson J, Hart T, Greenwood G, Paul J, et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93(6):939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brennan J, Kuhns LM, Johnson AK, Belzer M, Wilson EC, Garofalo R, the Adolescent Medicine Trials Network for HIV/AIDS Interventions Syndemic theory and HIV-related risk among young transgender women: the role of multiple, co-occurring health problems and social marginalization. Am J Public Health. 2012;102(9):1751–1757. doi: 10.2105/AJPH.2011.300433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Merkel J. Access to healthcare and lack thereof for transgender people. Theory in Action. 2017;10(4):41–47. [Google Scholar]
- 11.Bith-Melander P, Sheoran B, Sheth L, Bermudez C, Drone J, Wood W, Schroeder K. Understanding sociocultural and psychological factors affecting transgender people of color in San Francisco. J Assoc Nurses AIDS Care. 2010;21(3):207–220. doi: 10.1016/j.jana.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 12.Wilson EC, Garofalo R, Harris RD, Herrick A, Martinez M, Martinez J, Belzer M, Transgender Advisory Committee and the Adolescent Medicine Trials Network for HIV/AIDS Interventions Transgender female youth and sex work: HIV risk and a comparison of life factors related to engagement in sex work. AIDS Behav. 2009;13(5):902–913. doi: 10.1007/s10461-008-9508-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Budge SL, Adelson JL, Howard KAS. Anxiety and depression in transgender individuals: the roles of transition status, loss, social support, and coping. Journal Consult Clin Psychol. 2013;81(3):545–557. doi: 10.1037/a0031774. [DOI] [PubMed] [Google Scholar]
- 14.Sánchez FJ, Vilain E. Collective self-esteem as a coping resource for male-to-female transsexuals. J Couns Psychol. 2009;56(1):202–209. doi: 10.1037/a0014573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Faisal-Cury A, Menezes PR, d’Oliveira AFPL, Schraiber LB, Lopes CS. Temporal relationship between intimate partner violence and postpartum depression in a sample of low income women. Matern Child Health J. 2013;17(7):1297–1303. doi: 10.1007/s10995-012-1127-3. [DOI] [PubMed] [Google Scholar]
- 16.Sabri B, Bolyard R, McFadgion AL, Stockman JK, Lucea MB, Callwood GB, et al. Intimate partner violence, depression, PTSD, and use of mental health resources among ethnically diverse black women. Soc Work in Health Care. 2013;52(4):351–369. doi: 10.1080/00981389.2012.745461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Godoy-Ruiz P, Toner B, Mason R, Vidal C, McKenzie K. Intimate partner violence and depression among Latin American women in Toronto. J Immigr Minor Health. 2015;17(6):1771–1780. doi: 10.1007/s10903-014-0145-1. [DOI] [PubMed] [Google Scholar]
- 18.Ouellet-Morin I, Fisher HL, York-Smith M, Fincham-Campbell S, Moffitt TE, Arseneault L. Intimate partner violence and new-onset depression: a longitudinal study of women's childhood and adult histories of abuse. Depress Anxiety. 2015;32(5):316–324. doi: 10.1002/da.22347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen P-H, Rovi S, Vega ML, Barrett T, Pan K-Y, Johnson MS. Birth outcomes in relation to intimate partner violence. J Natl Med Assoc. 2017;109(4):238–245. doi: 10.1016/j.jnma.2017.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Henry RS, Perrin PB, Coston BM, Calton JM. Intimate partner violence and mental health among transgender/gender nonconforming adults. J Interpers Violence. 2018: Publish Ahead of Print; 10.1177/0886260518775148. [DOI] [PMC free article] [PubMed]
- 21.Garthe RC, Hidalgo MA, Hereth J, Garofalo R, Reisner SL, Mimiaga MJ, Kuhns L. Prevalence and risk correlates of intimate partner violence among a multisite cohort of young transgender women. LGBT Health. 2018;5(6):333–340. doi: 10.1089/lgbt.2018.0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guadalupe-Diaz XL, Anthony AK. Discrediting identity work: understandings of intimate partner violence by transgender survivors. Deviant Behav. 2017;38(1):1–16. [Google Scholar]
- 23.Valentine SE, Peitzmeier SM, King DS, O'Cleirigh C, Marquez SM, Presley C, et al. Disparities in exposure to intimate partner violence among transgender/gender nonconforming and sexual minority primary care patients. LGBT Health. 2017;4(4):26–267. doi: 10.1089/lgbt.2016.0113. [DOI] [PubMed] [Google Scholar]
- 24.West CM. Partner abuse in ethnic minority and gay, lesbian, bisexual, and transgender populations. Partner Abuse. 2012;3(3):336–357. [Google Scholar]
- 25.Vincke J, Bolton R. Social support, depression, and self-acceptance among gay men. Hum Relat. 1994;47(9):1049–1062. [Google Scholar]
- 26.Hoffman B. An overview of depression among transgender women. Depress Res Treat. 2014;2014:1–9. doi: 10.1155/2014/394283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Coker AL, Watkins KW, Smith PH, Brandt HM. Social support reduces the impact of partner violence on health: application of structural equation models. J Prev Med. 2003;37(3):259–267. doi: 10.1016/s0091-7435(03)00122-1. [DOI] [PubMed] [Google Scholar]
- 28.Mitchell MD, Hargrove GL, Collins MH, Thompson MP, Reddick TL, Kaslow NJ. Coping variables that mediate the relation between intimate partner violence and mental health outcomes among low-income, African American women. J Clin Psychol. 2006;62(12):1503–1520. doi: 10.1002/jclp.20305. [DOI] [PubMed] [Google Scholar]
- 29.Beeble ML, Bybee D, Sullivan CM, Adams AE. Main, mediating, and moderating effects of social support on the well-being of survivors of intimate partner violence across 2 years. J Consul Clin Psychol. 2009;77(4):718–729. doi: 10.1037/a0016140. [DOI] [PubMed] [Google Scholar]
- 30.Sevelius JM, Patouhas E, Keatley JG, Johnson MO. Barriers and facilitators to engagement and retention in care among transgender women living with human immunodeficiency virus. Ann Behav Med. 2014;47(1):5–16. doi: 10.1007/s12160-013-9565-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Friedman MR, Bukowski L, Eaton LA, Matthews DD, Dyer TV, Siconolfi D, et al. Psychosocial health disparities among black bisexual men in the U.S.: effects of sexuality nondisclosure and gay community support. Arch Sex Behav. 2018: Pub Ahead of Print; 10.1007/s10508-018-1162-2. [DOI] [PMC free article] [PubMed]
- 32.Eaton LA, Matthews DD, Bukowski LA, Friedman MR, Chandler CJ, Whitfield DL, et al. Elevated HIV prevalence and correlates of PrEP use among a community Sample of black men who have sex with men. JAIDS. 2018;Publish Ahead of Print; 10.1097/QAI.0000000000001822. [DOI] [PMC free article] [PubMed]
- 33.Miller RS, Lefcourt HM. The assessment of social intimacy. J Pers Assess. 1982;46(5):514–518. doi: 10.1207/s15327752jpa4605_12. [DOI] [PubMed] [Google Scholar]
- 34.Raymond HF, McFarland W. Racial mixing and HIV risk among men who have sex with men. AIDS Behav. 2009;13(4):630–637. doi: 10.1007/s10461-009-9574-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hammer GP, Kellogg TA, McFarland WC, Wong E, Louie B, Williams I, et al. Low incidence and prevalence of hepatitis C virus infection among sexually active non-intravenous drug-using adults, San Francisco, 1997-2000. Sex Transm Dis. 2003;30(12):919–924. doi: 10.1097/01.OLQ.0000091152.31366.E6. [DOI] [PubMed] [Google Scholar]
- 36.Zhang W, O'Brien N, Forrest JI, Salters KA, Patterson TL, Montaner JS, et al. Validating a shortened depression scale (10 item CES-D) among HIV-positive people in British Columbia, Canada. PLoS One. 2012;7(7):e40793. doi: 10.1371/journal.pone.0040793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prev Sci. 2000;1(4):173–181. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Little TD, Preacher KJ, Selig JP, Card NA. New developments in latent variable panel analyses of longitudinal data. Int J Behav Dev. 2007;31(4):357–365. [Google Scholar]
- 39.Preacher KJ. Advances in mediation analysis: a survey and synthesis of new developments. Annu Rev Psychol. 2015;66(1):825–852. doi: 10.1146/annurev-psych-010814-015258. [DOI] [PubMed] [Google Scholar]
- 40.Wen Z, Fan X. Monotonicity of effect sizes: questioning kappa-squared as mediation effect size measure. Psychol Methods. 2015;20(2):193–203. doi: 10.1037/met0000029. [DOI] [PubMed] [Google Scholar]
- 41.Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N, et al. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008;12(1):1–17. doi: 10.1007/s10461-007-9299-3. [DOI] [PubMed] [Google Scholar]
- 42.Cho S, Crenshaw KW, McCall L. Toward a field of intersectionality studies: theory, applications, and praxis. Signs. 2013;38(4):785–810. [Google Scholar]
- 43.Budge SL, Thai JL, Tebbe EA, Howard KAS. The intersection of race, sexual orientation, socioeconomic status, trans identity, and mental health outcomes. Couns Psychol. 2016;44(7):1025–1049. [Google Scholar]
- 44.Golden SD, Perreira KM, Durrance CP. Troubled times, troubled relationships: how economic resources, gender beliefs, and neighborhood disadvantage influence intimate partner violence. J Interpers Violence. 2013;28(10):2134–2155. doi: 10.1177/0886260512471083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pinto RM, Melendez RM, Spector AY. Male-to-female transgender individuals building social support and capital from within a gender-focused network. J Gay Lesbian Soc Serv. 2008;20(3):203–220. doi: 10.1080/10538720802235179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bauer GR, Hammond R, Travers R, Kaay M, Hohenadel KM, Boyce M. “I don’t think this is theoretical; this is our lives”: how erasure impacts health care for transgender people. J Assoc Nurses AIDS Care. 2009;20(5):348–361. doi: 10.1016/j.jana.2009.07.004. [DOI] [PubMed] [Google Scholar]


