Abstract
After New York State mandated that hospitals follow protocols to treat sepsis in 2014, performance of the protocol increased and mortality declined. Whether these encouraging trends have equitably benefited racial and ethnic minority populations is unknown. Although there were no significant racial/ethnic differences in rates of protocol completion at the onset of New York’s Sepsis Initiative, over time white patients experienced a greater increase in protocol completion compared to black patients. The emergence of this disparity was due to lower performance improvements among hospitals with higher proportions of black patients, though white and black patients made similar improvements when treated within the same hospital. Our study suggests an urgent need to understand why improvements in sepsis care lagged in minority-serving institutions in New York. Policymakers should anticipate and monitor the effects of quality improvement initiatives on disparities to ensure that all racial and ethnic groups realize their benefits equitably.
Introduction
Sepsis is a life-threatening infection that afflicts over 1.5 million Americans, results in 250,000 deaths, and accounts for $24 billion in health care spending each year.1,2 The World Health Organization has recognized sepsis as a global public health priority.3 In an effort to improve the treatment and outcomes of sepsis, international guidelines4 and the Centers for Medicare and Medicaid Services (CMS) National Early Management Bundle for Severe Sepsis and Septic Shock (SEP-1) core measure5 call for the prompt diagnosis and early administration of antibiotics and intravenous fluids to septic patients.
In 2013 the New York State (NYS) Department of Health, in collaboration with the NYS Executive Office, launched the New York State Sepsis Initiative. The initiative requires all NYS acute-care hospitals to implement an evidence-based protocol with pre-specified performance measures to identify and manage patients with sepsis. This Initiative, known as “Rory’s Regulations,” honors Rory Staunton, a previously healthy boy who tragically died following delayed treatment of septic shock. Rory’s Regulations represent an unprecedented use of state regulation to improve the quality of care for critically ill hospitalized patients.6
Early analyses suggest that adherence rates to the protocol increased and risk-adjusted mortality declined following the implementation of the NYS Sepsis Initiative.7,8,9 Yet it remains uncertain whether these encouraging trends have equitably benefited racial and ethnic minority populations, who suffer from a higher incidence of sepsis and worse outcomes.10,11
By improving the consistency of care delivery, broadly targeted quality improvement initiatives have the potential to narrow racial and ethnic disparities in medical care. For example, the monitoring and reporting of clinical performance measures in hemodialysis facilities,12 Medicare managed care plans,13 and acute care hospitals14 were accompanied by reduced racial and ethnic gaps in the quality of care. Alternatively, quality improvement efforts may exacerbate disparities given evidence that racial and ethnic minorities disproportionately receive care in settings with fewer resources, a worse quality of care, and less developed infrastructure for quality improvement.15 Performance improvements in minority-serving institutions may therefore lag other settings and lead to increased racial and ethnic disparities.16
We studied changes in the completion of the NYS Sepsis Initiative’s 3-hour protocol from April 1, 2014 to June 30, 2016 for non-Hispanic white, non-Hispanic black, Hispanic, and Asian patients hospitalized with severe sepsis and septic shock. Then we examined the extent to which disparities in care were explained by disproportionate representation of minority patients in lower-performing hospitals versus differences in care between white and minority patients who were treated within the same hospital.
Methods
Data Sources and Study Sample
We acquired data from the NYS Sepsis Initiative from April 1, 2014 to June 30, 2016, the initiative’s first 9 quarters. As described previously,8 all 185 of New York’s non-federal hospitals were required to report on in-hospital mortality and their initiation and implementation of 3-hour and 6-hour protocols for early detection and treatment of patients with sepsis and septic shock. The 3-hour resuscitation protocol consisted of measurement of a blood lactate, collection of blood cultures prior to antibiotics, and administration of broad-spectrum antibiotics and applied to all septic patients. The 6-hour protocol included: administering 30 ml/kg of intravenous fluids to patients with hypotension (systolic blood pressure <90 mmHg) or a serum lactate ≥ 4 mmol/l, initiating vasopressors if patients had refractory hypotension following IV fluids, and remeasurement of a lactic acid, and applied to only patients with septic shock (Appendix exhibit A1)17. Participants who failed to complete the 3-hour protocol were considered to have failed the 6-hour protocol as well. This study was approved by the Internal Review Board for the NYS Department of Health with a waiver of informed consent.
There were 113,380 episodes of sepsis submitted to the New York State Department of Health during the study period. Patients were included in the analysis if they were diagnosed with severe sepsis or septic shock as defined by the Sepsis 2 International Consensus definitions.18 Information about data collection and audits is provided in the Appendix exhibit A2.17 We excluded patients who were transferred from another hospital, and those with clinical contraindications to the protocol, with advance directives limiting care, who declined interventions, who were under age 18, who were excluded by the hospital, and who participated in a clinical trial, yielding 91,357 cases. We then further excluded 17,064 cases in which the protocol was not initiated (consistent with NYS’ reporting processes), 15,819 in which the protocol was initiated outside the emergency department, and 8,445 where the patient was not identified as non-Hispanic white, non-Hispanic black, Hispanic or Asian, yielding our final study sample of 50,029 (Appendix exhibit A3).17 Following the approach of Seymour et al.,8 we limited our study population to patients who presented to the emergency department with sepsis and excluded the 21.3% of sepsis cases that developed after admission to the hospital or in the intensive care unit. Sensitivity analyses that include the cases in which the protocol was initiated outside the emergency department, that examine quarterly trends in the fraction of cases in which the protocol was initiated, and that include patients who were not non-Hispanic white, non-Hispanic black, Hispanic or Asian are presented in the online supplement.17 The unit of analysis was the sepsis encounter.
Measures
The primary endpoint was a dichotomous outcome indicating timely completion of all the 3-hour protocol elements. Secondary outcomes were 6-hour protocol completion and in-hospital mortality. The primary independent variable was patient race or ethnic group (white, black, Hispanic or Asian). In a secondary analysis of within- and between-hospital racial disparities (described below), we constructed a hospital-level variable denoting the fraction of black patients with sepsis during the study period. Race/ethnicity was collected by the hospital. Patient-level covariates and modeling previously described by Phillips et al.19 include: site of infection, admission source, lower respiratory infection, mechanical ventilation required prior to protocol initiation, the interaction between lower respiratory infection and mechanical ventilation, diagnosis of severe sepsis vs. septic shock, thrombocytopenia (<150,000 cell/mm3) metastatic cancer, lymphoma/leukemia/multiple myeloma, patient age (continuous), square root of the comorbidity count, the interaction between, age and square root of comorbidity count, serum lactate entered as a quadratic expression, and the interaction between linear serum lactate and the square root of the comorbidity count. Hospital-level covariates were geographic region (New York City (NYC), non- NYC metropolitan, or rural location), teaching or non-teaching status, the number of beds (continuous), the number of sepsis cases (continuous), and the proportion of sepsis cases with Medicaid coverage or who were designated as self-pay. We selected these patient and hospital covariates to account for confounders or mediators of the relationship between race/ethnicity and study outcomes.
Statistical Analysis
First we performed binary analysis of completion of the 3- and 6-hour sepsis protocols and patient mortality over time by race/ethnicity. We assessed the magnitude of racial and ethnic disparity, defined as the absolute difference between the performance rate for white and racial/ethnic minority patients.
For our primary analysis examining rates of 3- and 6-hour protocol completion we used logistic regression with a robust standard error based on clustering patient observations within hospitals. A robust standard error accounts for the possibility that observations within a given hospital may be similar in nature. Consistent with NYS reporting, the patient-level clinical and demographic covariates were not included in protocol completion, since timely completion of the protocol represents a process-of-care that should be performed for all eligible patients. A similar logistic model was used to generate mortality rates; however, this model included the patient-level covariates described above.8,19 After running each model, linear combinations of the coefficients were used to generate the specific rates of interest along with 95% confidence intervals (CI) and p-values. We performed sensitivity analyses of the 3- and 6- hour protocols by randomly selecting one observation for patients who had multiple admissions for sepsis and of hospital mortality by using the last observation for each patient in the database. To determine the extent to which payer-mix mediated racial disparities, an additional sensitivity analysis adjusted for each hospital’s proportion of sepsis cases with Medicaid coverage or self-pay status.
For the secondary analysis to examine white-black racial disparity within and between hospitals, we constructed a mixed-effects logistic regression where the outcome was 3-hour protocol completion and the primary independent variables were a 3-way interaction between categorical race/ethnicity, all three 2-way interactions, a hospital level percentage of black septic patients (continuous), and continuous time (quarter 2, 2014 through quarter 2, 2016). This model was adjusted for the following hospital characteristics: teaching facility (dichotomized), non-profit status (dichotomized), region (NYC metro vs. non-NYC metro vs. rural), hospital observations (continuous), and the number of certified hospital beds (continuous). The difference in completion between the last and the first quarter for whites and for blacks were generated using combinations of the model coefficients. This analysis produced estimates of trends in adjusted outcomes for white and black patients according to the fraction of the patients in their treating hospital who were black. To determine whether this analysis was robust to exclusion of outlier hospitals with high proportions of black patients, a sensitivity analysis estimated this model after excluding 5 hospitals with 70% or more black patients. We also estimated this model after excluding hospital characteristics. All statistical analyses were performed with Stata/MP (version 14.2, StataCorp LLC, College Station, Texas).
Limitations
Our study has limitations. First, the observational study design cannot establish a causal relationship between the NYS Sepsis Initiative and increased racial and ethnic disparities. Secondly, though we found no significant differences in mortality trends between white and black patients, the point estimates indicate that mortality declined by 4.5 percentage points among white patients and 2.2 percentage points among black patients. This suggests that we may have been underpowered to detect meaningful racial differences in mortality trends, though we note significant reductions in mortality for the entire cohort. Nevertheless, the emergence of a disparity in protocol completion is concerning, given the evidence of an association between timely protocol completion and a lower rate of mortality.8,9 Third, it is possible that facility-level factors such as staffing, ED crowding, and quality improvement infrastructure may have mediated the observed disparities between hospitals with higher and lower fractions of black patients, but information on these factors were not available in our data. Fourth, our study focused on the measures targeted by the NYS Sepsis Initiative and did not assess changes in other key performance domains, including indicators of safety, efficiency, and patient-centeredness. Fifth, we lacked data on compliance with the 3- and 6-hour protocol for patients that did not have the protocol initiated. However, racial and ethnic differences in the rates of protocol initiation did not appear to change over time. Finally, our study sample had relatively small fractions of Hispanic (11.0%) and Asian patients (5.1%) limiting our ability to characterize trends for these groups. Further studies that focus on sepsis care and outcomes for these populations are needed.
Results
Patient Characteristics
Our study sample included 50,029 emergency department encounters for severe sepsis and septic shock, consisting of white (66.6%), black (17.3%), Hispanic (11.0%) and Asian (5.1%) patients. Compared to white patients, black and Hispanic patients were younger, and had a greater number of comorbid conditions (Exhibit 1). Both black and Hispanic patients were more likely than white patients to receive care at larger hospitals, teaching hospitals, and hospitals that treated a greater number of sepsis cases. Additionally, black and Hispanic patients were more likely to live within New York City.
Exhibit 1.
Characteristics of Patients Hospitalized for Sepsis in New York State from 2014 to 2016, According to Racial or Ethnic Group
| Characteristics | White | Black | Hispanic | Asian |
|---|---|---|---|---|
| Patient Variable | ||||
| N (% of total sample) | 33,338 (66.6) | 8,663 (17.3) | 5,489 (11.0) | 2,539 (5.1) |
| Mean Age, y | 72.7 | 66.1 | 65.1 | 70.4 |
| Female, % | 48.5 | 49.5 | 51.1 | 56.5 |
| Coexisting condition, % | ||||
| Diabetes mellitus | 32.9 | 42.6 | 43.7 | 43.5 |
| Congestive heart failure | 21.9 | 20.3 | 17.9 | 16.0 |
| Chronic respiratory disease | 11.4 | 13.5 | 10.7 | 12.3 |
| End-stage renal disease | 9.2 | 17.8 | 11.1 | 10.5 |
| Metastatic cancer | 8.9 | 9.8 | 9.1 | 11.9 |
| Chronic liver disease | 5.0 | 7.5 | 9.8 | 7.6 |
| Lymphoma/leukemia/multiple myeloma | 4.5 | 4.2 | 4.0 | 4.7 |
| Organ transplant | 1.4 | 1.8 | 2.2 | 2.8 |
| HIV/AIDS | 0.9 | 7.5 | 4.8 | 0.7 |
| Site of infection, % | ||||
| Respiratory | 39.6 | 38.7 | 38.9 | 40.6 |
| Urinary | 28.0 | 25.1 | 26.8 | 25.9 |
| Gastrointestinal | 10.4 | 8.1 | 11.0 | 12.7 |
| Skin | 7.1 | 8.4 | 6.5 | 3.7 |
| Other | 7.7 | 9.8 | 8.9 | 9.2 |
| Unknown | 7.1 | 9.9 | 7.8 | 7.9 |
| Positive blood cultures, % | 27.6 | 30.8 | 28.4 | 28.1 |
| Serum lactate (mmol/liter), median | 2.6 | 2.8 | 2.8 | 2.9 |
| Septic shock, % | 45.4 | 42.8 | 43.4 | 45.8 |
| In-hospital mortality, % | 23.5 | 24.8 | 20.2 | 24.5 |
| Hospital Variable | ||||
| Teaching hospital, % | 75.8 | 93.6 | 94.0 | 95.9 |
| Tax status, not-for-profit % | 90.3 | 73.6 | 79.6 | 84.8 |
| Medicaid or uninsured/self-pay, median | 9.7 | 31.7 | 26.0 | 14.4 |
| Geographic location, % | ||||
| New York City | 23.3 | 62.1 | 73.3 | 73.7 |
| Non-NYC metro | 71.8 | 37.7 | 26.5 | 26.1 |
| Rural | 4.9 | 0.2 | 0.2 | † |
| Number of sepsis cases, median | 580 | 557 | 737 | 789 |
| Number of certified beds, median ( | 375 | 457 | 495 | 535 |
Source: Authors’ analysis of data provided from the New York Sepsis Initiative. Notes: P-values for all comparisons between racial and ethnic groups were <0.001 with the exception of presence of lymphoma/leukemia/multiple myeloma (P=0.20). All percentages are based on the total N except for the percent of each race, which is based on the total study population of 50,029.
Cell suppressed due to small sample size.
Racial and Ethnic Performance Rates for Protocol Completion and Mortality
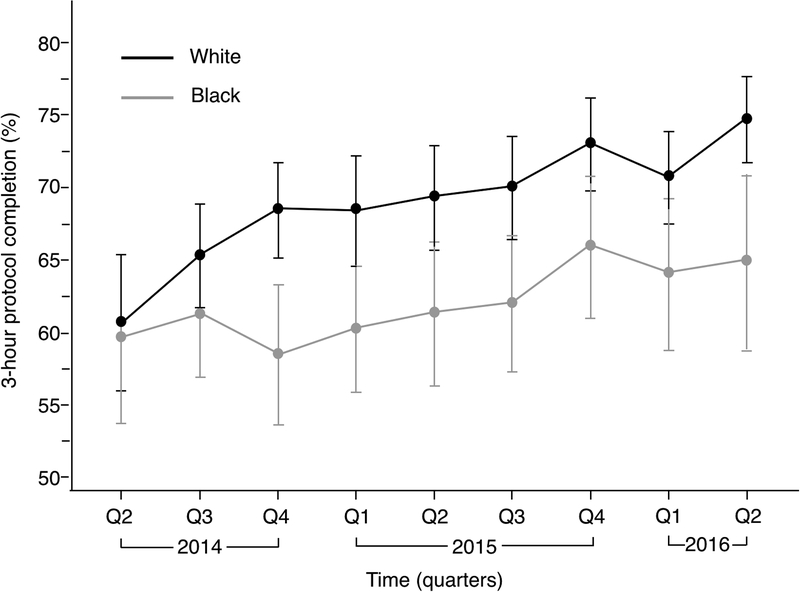
In the first quarter of the study, there were no statistically significant differences in rates of unadjusted 3-hour completion between white (60.8% [95% CI 56.1–65.5]), black (59.7% [95% CI 53.9 to 65.5]), Hispanic (62.6% [95% CI 55.9 to 69.2]), and Asian (58.8% [95% CI 49.0 to 68.7]) patients (Exhibit 2). Over the 2.25-year study period, white patients experienced a greater increase in the adjusted rate of the 3-hour protocol completion (14.0 percentage points [95% CI 9.2 to 18.9]) compared to black patients (5.3 percentage points [95% CI −2.1 to 12.7]; P=0.025 for comparison of improvement between white and black patients; Exhibit 3). Rates of improvement in 3-hour protocol completion were 6.7 percentage points [95% CI −1.0 to 14.5] for Hispanic patients and 8.4 percentage points [95% CI 1.3 to 15.6] for Asian patients. The magnitudes of improvement observed among Hispanic and Asian patients were not statistically different when compared to whites (Exhibit 2 and Appendix exhibit A4).17
Exhibit 2.
Change in 3- and 6-Hour Protocol Completion and Risk-Adjusted Hospital Mortality for Patients Presenting to the Emergency Department with Sepsis, by Race/Ethnicity.
| Outcome | N | Initial Rate Q2 2014 | Final Rate Q2 2016 | Absolute change in percentage from Q2 2104 to Q2 2016 |
|---|---|---|---|---|
| % (95% CI) | % (95% CI) | Percentage points | ||
| 3-hour protocol completion | 49,939 | |||
| White | 33,284 | 60.8 | 74.8 | 14.0 (referent) |
| Black | 8,642 | 59.7 | 65.0 | 5.3** |
| Hispanic | 5,480 | 62.6 | 69.3 | 6.7* |
| Asian | 2,533 | 58.8) | 67.2 | 8.4 |
| 6-hour protocol completion | 49,707 | |||
| White | 33,121 | 34.1 | 48.8 | 14.7 (referent) |
| Black | 8,600 | 35.1 | 41.9 | 6.8** |
| Hispanic | 5,458 | 35.3 | 48.3 | 13.0 |
| Asian | 2,528 | 30.6 | 45.5 | 14.9 |
| Risk-adjusted hospital mortality | 50,029 | |||
| White | 33,338 | 25.8 | 21.3 | −4.5 (referent) |
| Black | 8,663 | 25.4 | 23.1 | −2.2 |
| Hispanic | 5,489 | 24.6 | 17.1 | −7.5 |
| Asian | 2,539 | 21.9 | 23.5 | 1.7* |
Source: Authors’ analysis of data provided from the New York Sepsis Initiative. Notes: 3-hour and 6-hour protocol completion un-adjusted; however, a robust standard error was used based on clustering on the 175 hospitals. Mortality adjusted for: site of infection, admission source, lower respiratory infection, mechanical ventilation required prior to protocol initiation, the interaction between lower respiratory infection and mechanical ventilation, diagnosis of severe sepsis vs. septic shock, thrombocytopenia (<150,000 cell/mm3) metastatic cancer, lymphoma/leukemia/multiple myeloma, patient age (continuous), square root of the comorbidity count, the interaction between, age and square root of comorbidity count, serum lactate entered as a quadratic expression, and the interaction between linear serum lactate and the square root of the comorbidity count. Ninety patients have missing data for 3-hour protocol completion and 322 patients for 6-hour protocol completion. P-values refer to comparison of absolute change relative to white patients.
Significance:
p < 0.10,
p<0.05
Exhibit 3. Figure. Three-hour protocol completion for white and black patients with sepsis presenting to the emergency department.
Authors’ analysis of data provided from the New York Sepsis Initiative. Notes: 3-hour protocol completion is un-adjusted for patient level variables. The 95% confidence interval uses a robust standard error based on clustering on the 175 hospitals. The Y-axis runs from 50 to 80%. White patient encounters = 33,284; black patient encounters = 8,642.
White patients made a greater improvement in 6-hour protocol completion (14.7 percentage points [95% CI 9.6 to 19.8]) compared to black patients (6.8 percentage points [95% CI −0.9 to 14.4]; P=0.04 for comparison of change between white and black patients; Exhibit 2 and Appendix exhibit A5).17 An analysis of all patients (emergency department, intensive care unit, and wards) showed that white patients made a greater improvement in 3-hour protocol completion (13.7 percentage points [95% CI 8.9 to 18.4]) over the study period compared to black patients (5.7 percentage points [95% CI −1.5 to 13.0]; P=0.037 for comparison of improvement between white and black patients; Appendix exhibit A6 and A7).17 Results for the 3- and 6-hour protocol completion remained significant following sensitivity analyses that randomly selected one observation among patients with multiple episodes of sepsis (Appendix exhibit A8)17 and that adjusted for each hospital’s fraction of cases with Medicaid or self-pay status (Appendix exhibit A9).17 Compared with white, black patients had lower rates of protocol initiation and Asian patients had higher rates, but these differences remained stable over the study period. (Appendix exhibit A10).17
In the first quarter of the study, risk-adjusted mortality rates were statistically similar for white (25.8% [95% CI 24.0 to 27.6]), black (25.4% [95% CI 22.3 to 28.5]), Hispanic (24.6% [95% CI 20.7 to 28.5]), and Asian patients (21.9% [95% CI 18.0 to 25.7]). Risk-adjusted rates of mortality decreased 4.5 percentage points [95% CI −6.7 to −2.2] for white patients, 2.2 percentage points [95% CI −7.4 to 2.9] for black patients, 7.5 percentage points [95% CI −11.7 to −3.3] for Hispanic patients, and increased 1.7 percentage points [95% CI −4.1 to 7.4] for Asian patients. The difference in the magnitudes of change between white and minority patients did not reach statistical significance (Exhibit 2, Appendix exhibit A8).17
Within- and Between-Hospital Racial and Ethnic Differences in 3-hour Protocol Completion and Mortality
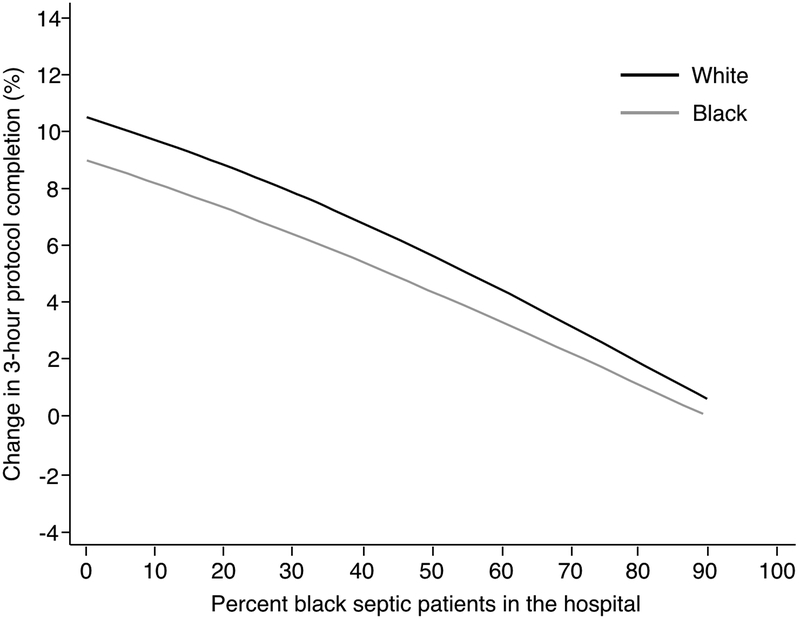
We identified a relationship between an increasing black patient population within hospitals and lower magnitudes of improvement in completion of the 3-hour protocol. For example, hospitals that cared for a 10% black patient population improved by 9.0 percentage points [95%CI 4.8 to 13.3], while those caring for a 50% black patient population improved 2.2 percentage points [95%CI −3.9 to 8.3], resulting in an adjusted difference of 6.8 percentage points [95%CI 12.9 to 0.08] (P=0.027), (Appendix exhibit A11).17 Exhibit 4 illustrates the results of a mixed effects model that partitions the variance in disparities into within and between hospital components. For both white and black patients, hospitals that cared for an increasing percentage of black patients made smaller magnitudes of improvement in completion of the 3-hour protocol. However, within each hospital, white and black patients made equal levels of improvement in the 3-hour protocol. Among black patients, approximately 20% of all encounters occurred in hospitals in which the proportion of patients who were black was 70% or greater. Exclusion of these hospitals yielded similar findings to those of our main analysis (Appendix exhibit A12).17 The distribution of white and black patients within hospitals is shown in Appendix exhibit A13 and an analysis that did not adjust for hospital characteristics produced similar results to our fully adjusted model (Appendix exhibit A14).17
Exhibit 4. Figure. Improvement in adjusted 3-hour protocol completion for all emergency department patients stratified by the percent black septic patients in the hospital.
Authors’ analysis of data provided from the New York Sepsis Initiative. Notes: Analysis based upon a mixed effects logistic regression where the hospital’s percentage black population, calendar quarter, and their interaction are entered into the model as a linear continuous term (N=49,939). The white and the black populations are shown. Model adjusted for teaching hospital (dichotomized), non-profit hospital vs. other, NYC vs. metro vs. rural location, number of cases, and the number of certified hospital beds. The unit of analysis is the hospital. There is no statistical difference between the lines representing white and black patients. A figure displaying 95% confidence intervals is provided in the online supplement (Appendix Exhibit A13)17.
Discussion
We examined racial and ethnic trends in health care and outcomes following the New York State Sepsis Initiative, a statewide mandate designed to improve the quality of care delivered to patients with sepsis. Our findings indicate that while protocol adherence improved for all racial/ethnic groups following the implementation of the Sepsis Initiative, these improvements were accompanied by the emergence of a disparity between white and black patients. Black, white, Hispanic, and Asian patients had similar initial rates of completion of the 3- and 6-hour protocols: the low performance in protocol completion among all racial and ethnic groups at the study onset suggests that the protocol was not a widely targeted goal in sepsis care prior to the NYS Initiative. In the first 2.25 years of the Sepsis Initiative, white patients experienced a greater improvement compared to black patients. An analysis that adjusted for where patients received care demonstrated that white and black patients received equivalent care when treated within the same hospital. However, hospitals that cared for higher proportions of black patients showed limited improvement in protocol completion, while those caring for predominately white patient populations improved more substantially. Finally, we did not find evidence of an increased disparity in risk-adjusted mortality between white and minority patients.
Although the National Academies of Medicine and others have established equity as a fundamental dimension of the quality of care, empirical evidence about the effects of quality improvement interventions on equity is limited.12–14 In theory, interventions that improve the consistency of care or that standardize treatment protocols may reduce unwanted racial/ethnic variations in the use of effective care. The findings of our study, however, raise concerns about the potential for broadly targeted quality improvement initiatives to exacerbate inequities in care. Our findings align with a study of New York State’s Coronary Artery Bypass (CABG) report card.20 In that study, Werner et al. demonstrated that implementation of statewide public reporting of surgical outcomes resulted in fewer black and Hispanic patients receiving cardiac surgery, potentially because providers avoided treating minority patients who they perceived to have a higher risk of mortality. In contrast to the findings of Werner et al., the increased racial gap in sepsis treatment is unlikely to be the result of hospitals’ avoidance of high-risk patients in response to public reporting. The NYS Sepsis Initiative did not publicly report performance data before 2017, and it is unlikely that hospitals can select the patients who they treat for sepsis. Instead, the emergence of a disparity in sepsis care occurred because hospitals treating higher fractions of black patients made lower gains in performance, though white and minority patients were treated similarly when cared for within the same hospital.
Our findings extend prior research documenting that racial and ethnic disparities are often driven by where patients receive care.21–24 For instance, Hasnain-Wynia et al. demonstrated that controlling for the differences between treating hospitals accounted for the majority of observed racial and ethnic disparity in the quality of hospital care for acute myocardial infarction, congestive heart failure, and pneumonia.15 Further, a disproportionate number of black and Hispanic patients receive care from a small number of hospitals22,25 and physicians.26 Minority-serving institutions have been shown to operate with fewer resources, less quality improvement infrastructure, more emergency department (ED) overcrowding,27,28 and unfavorable nurse-to-patient ratios.29 These factors may explain why performance gains lagged in these facilities. Although between-hospital differences were the primary driver of disparities in sepsis care, other studies have reported that provider-level differences remain an important source of disparities for other outcomes and conditions.14,22,30 This supports the continuing need to characterize patient and provider contributions to health care disparities.
Our study has three main policy implications. First, stratified reporting of performance is essential to understand the impact of quality improvement strategies on the equity of care for vulnerable populations.15,16 This is consistent with the mission priorties of the CMS Office of Minority Health Equity Plan.31 Of note, the NYS Sepsis Initiative 3-hour protocol is identical to the CMS SEP-1 core measure,5 and CMS is considering tying the measure to hospital reimbursement as part of a value-based payment strategy. If the results of our study extend to other states, policymakers should monitor whether these incentives exacerbate racial disparities in sepsis care, and penalize hospitals that disproportionately serve black patients. Second, urgent efforts are needed to understand why performance improvements in sepsis care lagged in minority-serving institutions in New York. Third, when implementing a new quality improvement initiative, policymakers could identify minority-serving hospitals at risk of poor compliance and collect data on their quality improvement infrastructure and barriers to improving care. These efforts could determine whether these institutions have the resources to successfully implement quality improvement strategies and direct financial and technical support to hospitals that have difficulty meeting targeted performance thresholds.32
In conclusion we found that while the implementation of the NYS Sepsis Initiative was associated with improved protocol adherence for all racial and ethnic groups, these improvements were accompanied by the emergence of a widening disparity in sepsis care between white and black patients over time. This disparity primarily arose from lower performance gains in hospitals with higher proportions of black patients. Our study suggests an urgent need to understand why improvements in sepsis care lagged in minority-serving institutions in NYS. Policymakers should anticipate and monitor the effects of quality improvement initiatives on disparities to ensure that all racial and ethnic groups realize their benefits equitably.
Supplementary Material
References
- 1.Torio CM, Moore BJ. National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2013: Statistical Brief #204 Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006. [PubMed] [Google Scholar]
- 2.Gaieski DF, Edwards JM, Kallan MJ, Carr BG. Benchmarking the incidence and mortality of severe sepsis in the United States. Crit Care Med. 2013;41:1167–74. [DOI] [PubMed] [Google Scholar]
- 3.Reinhart K, Daniels R, Kissoon N, Machado FR, Schachter RD, Finfer S. Recognizing Sepsis as a Global Health Priority - A WHO Resolution. N Engl J Med. 2017;377:414–7. [DOI] [PubMed] [Google Scholar]
- 4.Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43:304–77. [DOI] [PubMed] [Google Scholar]
- 5.NQF-Endorsed Voluntary Consensus Standards for Hospital Care – Sepsis, SEP-1. Version 5.0a. Accessed on April 1, 2018 at https://www.nhfca.org/psf/resources/Updates1/SEP-1%20Measure%20Information%20Form%20(MIF).pdf [Google Scholar]
- 6.Hershey TB, Kahn JM. State Sepsis Mandates - A New Era for Regulation of Hospital Quality. N Engl J Med. 2017;376:2311–3. [DOI] [PubMed] [Google Scholar]
- 7.New York State Report on Sepsis Care Improvement Initiative: Hospital Quality Performance. Office of the Medical Director Office of Quality and Patient Safety, March 2017 Accessed on April 1, 2018 at https://www.health.ny.gov/press/reports/docs/2015_sepsis_care_improvement_initiative.pdf [Google Scholar]
- 8.Seymour CW, Gesten F, Prescott HC, Friedrick ME, Iwashyna TJ, Phillips GS, et al. Time to Treatment and Mortality during Mandated Emergency Care for Sepsis. N Engl J Med. 2017;376:2235–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Levy MM, Gesten FC, Phillips GS, Terry KM, Seymour CW, Prescott HC, et al. Mortality Changes Associated with Mandated Public Reporting for Sepsis. The Results of the New York State Initiative. Am J Resp Crit Care Med. 2018;198:1406–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–54. [DOI] [PubMed] [Google Scholar]
- 11.Barnato AE, Alexander SL, Linde-Zwirble WT, Angus DC. Racial variation in the incidence, care, and outcomes of severe sepsis: analysis of population, patient, and hospital characteristics. Am J Respir Crit Care Med. 2008;177:279–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sehgal AR. Impact of quality improvement efforts on race and sex disparities in hemodialysis. JAMA. 2003;289:996–1000. [DOI] [PubMed] [Google Scholar]
- 13.Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. Trends in the quality of care and racial disparities in Medicare managed care. N Engl J Med. 2005;353:692–700. [DOI] [PubMed] [Google Scholar]
- 14.Trivedi AN, Nsa W, Hausmann LR, Lee JS, Ma A, Bratzler DW, et al. Quality and equity of care in U.S. hospitals. N Engl J Med. 2014;371:2298–308. [DOI] [PubMed] [Google Scholar]
- 15.Hasnain-Wynia R, Kang R, Landrum MB, Vogeli C, Baker DW, Weissman JS. Racial and ethnic disparities within and between hospitals for inpatient quality of care: an examination of patient-level Hospital Quality Alliance measures. J Health Care Poor Underserved. 2010;21:629–48. [DOI] [PubMed] [Google Scholar]
- 16.Casalino LP, Elster A, Eisenberg A, Lewis E, Montgomery J, Ramos D. Will pay-for-performance and quality reporting affect health care disparities? Health Aff (Millwood). 2007;26:w405–14. [DOI] [PubMed] [Google Scholar]
- 17.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 18.Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003;31:1250–6. [DOI] [PubMed] [Google Scholar]
- 19.Phillips GS, Osborn TM, Terry KM, Gesten F, Levy MM, Lemeshow S. The New York Sepsis Severity Score: Development of a Risk-Adjusted Severity Model for Sepsis. Crit Care Med. 2017;46:674–83. [DOI] [PubMed] [Google Scholar]
- 20.Werner RM, Asch DA, Polsky D. Racial profiling: the unintended consequences of coronary artery bypass graft report cards. Circulation. 2005;111:1257–63. [DOI] [PubMed] [Google Scholar]
- 21.Schulman KA, Berlin JA, Harless W, Kerner JF, Sistrunk S, Gersh BJ, et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med.1999;340:618–26. [DOI] [PubMed] [Google Scholar]
- 22.Hasnain-Wynia R, Baker DW, Nerenz D, Feinglass J, Beal AC, Landrum MB, et al. Disparities in health care are driven by where minority patients seek care: examination of the hospital quality alliance measures. Arch Intern Med. 2007;167:1233–9. [DOI] [PubMed] [Google Scholar]
- 23.Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305:675–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Skinner J, Chandra A, Staiger D, Lee J, McClellan M. Mortality after acute myocardial infarction in hospitals that disproportionately treat black patients. Circulation. 2005;112:2634–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jha AK, Orav EJ, Li Z, Epstein AM. Concentration and quality of hospitals that care for elderly black patients. Arch Intern Med. 2007;167:1177–82. [DOI] [PubMed] [Google Scholar]
- 26.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351:575–84. [DOI] [PubMed] [Google Scholar]
- 27.Trzeciak S, Rivers EP. Emergency department overcrowding in the United States: an emerging threat to patient safety and public health. Emerg Med J. 2003;20:402–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sun BC, Hsia RY, Weiss RE, Zingmond D, Liang LJ, Han W, et al. Effect of emergency department crowding on outcomes of admitted patients. Ann Emerg Med. 2013;61:605–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288:1987–93. [DOI] [PubMed] [Google Scholar]
- 30.Trivedi AN, Grebla RC, Wright SM, Washington DL. Despite improved quality of care in the Veterans Affairs health system, racial disparity persists for important clinical outcomes. Health affairs. 2011;30:707–15. [DOI] [PubMed] [Google Scholar]
- 31.The CMS Equity Plan for Improving Quality in Medicare. Accessed on April 1, 2018 at https://www.cms.gov/About-CMS/Agency-Information/OMH/OMH_Dwnld-CMS_EquityPlanforMedicare_090615.pdf
- 32.Werner RM, Goldman LE, Dudley RA. Comparison of change in quality of care between safety-net and non-safety-net hospitals. Jama 2008;299:2180–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.