Abstract
Rationale and Objective.
Compared to others, Black and low-income patients receiving dialysis are less likely to receive kidney transplant (KT) education within dialysis centers. We examined the efficacy of two supplementary KT education approaches delivered directly to patients.
Study Design.
Prospective, 3-arm parallel-group, randomized controlled trial.
Settings and Participants.
Adult, Black and White low-income patients receiving dialysis in Missouri.
Intervention.
Patients were randomized to 1 of 3 educational conditions: 1) Standard-of-Care, usual KT education provided in dialysis centers (control); 2) Explore Transplant @ Home Patient-Guided, 4 modules of KT education sent directly to patients using print, video, and text messages; 3) Explore Transplant @ Home Educator-Guided, the patient-guided intervention plus four telephonic discussions with an educator.
Outcomes.
Primary: patient knowledge of living and deceased donor kidney transplant (LDKT, DDKT). Secondary: informed decision-making, change in attitudes in favor of LDKT and DDKTc, and change in the number of new steps taken toward KT.
Results.
In intent-to-treat analyses, patients randomized to educator- and patient-guided interventions had greater knowledge gains (1.4 point increase) than control patients (0.8 point increase, p=0.02 and 0.01, respectively). Compared to control patients, more patients randomized to educator- and patient-guided interventions were able to make informed decisions about starting KT evaluation (82% vs. 91% and 95%, p=0.003); pursuing DDKT (70% vs. 84% and 84%, p=0.003); and pursuing LDKT (73% vs. 91% and 92%, p<0.001).
Limitations.
Potential contamination because of patient-level randomization; no assessment of clinical endpoints.
Conclusions.
Education presented directly to dialysis patients, with or without coaching by telephone, increased dialysis patients’ KT knowledge and informed decision-making without increasing educational burden on providers.
Trial Registration:
Registered at ClinicalTrials.gov with study number
Keywords: kidney transplantation, patient education, dialysis, socioeconomic disparities, racial disparities, end-stage renal disease (ESRD), socioeconomic status (SES), low income, poverty, randomized controlled trial (RCT)
INTRODUCTION
In the United States, more than 678,000 patients have kidney failure, with nearly 100,000 diagnosed annually.1 Kidney transplant (KT) can help patients live longer with an improved quality of life, compared to ongoing dialysis.2 Per the Centers for Medicare and Medicaid Services, every maintenance dialysis patient must be informed of their KT options, including whether to continue dialysis or pursue either a deceased or living donor transplant (DDKT, LDKT, respectively).3 Despite available KT education, over 70% of kidney failure patients remain on dialysis.1
In addition, lack of access to KT affects some patients disproportionately. In the U.S., Black patients are 3.1 times more likely than White patients to develop kidney failure but are less likely to receive transplants,1 especially LDKTs,4 due to poorer KT knowledge,5 greater fears of KT in general and LDKT specifically,6–8 higher medical mistrust,7–10 and greater socioeconomic burdens.9 Independent of race, patients with low socioeconomic status (SES) are up to 75% less likely to receive LDKTs.11–14 The challenges of these additional barriers to KT for low SES, Black patients add complexity to learning about DDKT and LDKT.
The American Society of Transplantation (AST) recommends providing culturally tailored, community-based LDKT education to patients earlier in the transplant referral process, in modules, with transplant liaisons in dialysis clinics.15 Supplementary education provided directly to dialysis patients over a longer timeframe may enhance current KT education in dialysis centers. Text-messaging interventions,16, 17 could be utilized, since these have shown to promote behavior change.17 For patients with complex medical situations and low SES, the use of telephonic case managers18–20 has helped provide individualized support and education remotely. These educational strategies and delivery approaches have not yet been studied in combination for patients learning about DDKT and LDKT. Thus, we conducted a randomized controlled trial (RCT) testing whether an eight-month Explore Transplant @ Home education program, with or without telephonic support from an educator, could help improve transplant knowledge, informed decision-making, pro-transplant attitudes, and steps toward KT compared to traditional dialysis center KT education for low-income Black and White patients.
METHODS
Randomized Controlled Trial Design
This study was a prospective, parallel-arm RCT among 561 Black and White dialysis patients in Missouri. Patients were recruited from Missouri Kidney Program’s (MoKP) client roster or from public advertisements in dialysis centers. MoKP is a state-funded organization providing financial assistance to low-income Missouri residents with kidney failure. Patients were randomized to receive one of three educational conditions over eight months: standard transplant education provided in dialysis centers only (standard-of-care); the patient-guided Explore Transplant @ Home program without access to a telephonic educator; or the educator-guided Explore Transplant @ Home program facilitated by a telephone educator. The published protocol21 was registered at ClinicalTrials.gov (#) and approved by the University of California, Los Angeles’s Institutional Review Board (#14–000802) and the University of Missouri, Columbia Institutional Review Board (#00048966).
Setting and Participants
Participants came from 122 unique dialysis centers representing multiple dialysis organizations. Patient inclusion criteria were: 1) between 18–74 years of age, 2) self-identify as Black or White, 3) currently on dialysis, 4) household income at or below 250% of the federal poverty level, and 5) speak and read English. Patients were excluded if they: 1) had a visual and/or hearing impairment that would preclude watching and reading education, 2) had a previous KT, and/or 3) had previously been told that they were not a candidate for transplant. MoKP patients received flyers within prescription medication packets mailed to their homes, and flyers were disseminated in nearly 100 Missouri dialysis facilities. Interested patients contacted the study team directly to assess eligibility and provide verbal informed consent to participate.
Explore Transplant @ Home Patient-Guided Education Condition (Intervention 1)
Patients randomized to the patient-guided intervention received standard-of-care plus an eight-month educational program, including four video and print modules mailed every two months containing brochures, fact sheets, and an Explore Transplant DVD video, averaging 20 minutes in length, to watch at home with family or friends. If patients did not have a DVD player, one was provided for them at no charge. Additionally, 12 postcards were mailed, one every two weeks, with educational highlights from each module. Finally, patients could opt to receive text messages repeating content and asking multiple-choice and true/false questions to facilitate learning each week.
Explore Transplant @ Home Educator-Guided Education Condition (Intervention 2)
Patients randomized to the educator-guided intervention received standard-of-care and the complete patient-guided intervention over eight months. In addition, they received calls with an educator who reviewed key educational concepts from each module, probed to determine if the patient had any questions, and strategized with the patient about overcoming barriers they might face in making decisions about transplant. Calls lasted approximately 20 minutes.
standard-of-care Dialysis Center Education Condition (Control)
Patients randomized to the standard-of-care received only transplant education provided as part of usual care within their dialysis centers. Based on the results of our survey of Missouri dialysis providers, this education varied substantially. Though 57% said there was a formal education program in their center, the most common education practices included oral recommendations that patients get evaluated for transplant (93%) or learn more about transplant (89%), and dissemination of print KT materials (74%). Only 15% showed educational videos, 20% offered opportunities to talk about transplant with a kidney recipient, and 24% provided education to share with potential living donors (Table 1).
Table 1.
Standard-of-Care of Educational Practices Used by Dialysis Providers
| Description of Educational practice | Affirmative Response or Confirmed use of practice |
|---|---|
| General Approaches to Transplant Education | |
| Transplant information provided at least once to all transplant candidates, whether they have expressed interest in transplant or not | 97% |
| There is a formal transplant-education program at this center | 57% |
| There is a designated transplant educator or team of educators at this facility | 41% |
| Transplant information is provided every year to all transplant candidates, whether they have expressed interest in transplant or not | 4% |
| Transplant Education Practices | |
| Recommend to get evaluated for transplant | 93% |
| Recommend to learn more about transplant | 89% |
| Provide a list of transplant centers’ phone numbers | 89% |
| Provide handouts/brochures about transplant | 74% |
| Display transplant posters in the dialysis facility waiting room | 61% |
| Refer to an education program at a transplant center/kidney organization | 61% |
| Have detailed discussions about the risks/benefits of deceased donor transplant | 35% |
| Have detailed discussions about the risks/benefits of living donor transplant | 33% |
| Provide list of transplant websites | 28% |
| Provide patients with transplant education to share with potential living donors | 24% |
| Offer an opportunity to talk to a previous transplant recipient | 20% |
| Show transplant video(s) or DVD(s) | 15% |
| There is not good communication between nearby transplant centers and this dialysis facility | 28% |
| There is not enough time to educate patients about transplant | 28% |
| Do not have a DVD player to watch educational videos | 23% |
| The transplant centers are too far away from this facility | 22% |
| My dialysis facility administration does not value transplant education as a priority | 9% |
(n=46). Results of survey of dialysis staff representatives of 46 dialysis centers where patients in this study received care. We asked what general approaches to transplant education were used in the dialysis center and whether they used any of 12 transplant education practices. We also asked the dialysis staff about the barriers they faced to providing transplant education in their center.
Outcome Measures
All patients were administered pre-randomization and post-intervention surveys. The primary outcome was patients’ knowledge of LDKT and DDKT. The transplant knowledge scale had 15 questions, 10 true/false and 5 multiple choice, scored so that correct responses contributed 1 point and incorrect or “don’t know” responses contributed 0 points. The total correct responses were summed to create a 0–15 scale, with higher scores indicating higher transplant knowledge.
Secondary outcomes included informed decision-making, LDKT and DDKT attitudes, and new steps toward transplant. The post-intervention survey included four questions asking whether the patient had all the facts they needed to make an informed decision about whether to remain on dialysis, start KT evaluation, and try to get a DDKT and/or LDKT. To each, patients rated their agreement on a 4-point scale from “Completely Agree” to “Completely Disagree,” and the proportion of patients responding that they agreed was assessed.
LDKT and DDKT attitudes were measured pre- and post-intervention with Pros, Cons, and Self-Efficacy scales (6 scales total).22, 23 The LDKT and DDKT Pros and Cons scales each had 6 items prompted with, “How important is this statement to your decision about transplant?” rated on a 5-point scale from [1] “Not important” to [5] “Extremely important” and summed to create scales ranging from 6–30 with higher scores indicating higher Pros or Cons. The LDKT and DDKT Self-Efficacy scales had 6 and 8 items, respectively, asking about potential barriers that may arise to pursuing transplant and prompted with, “If you wanted a transplant and you encountered any of the following situations along the way, how confident are you that you could continue pursuing transplant” that were rated on a 5-point scale from [1] “Not at all confident” to [5] “Completely confident.” Responses were summed creating scores from 6–30 (LDKT Self-Efficacy) and 8–40 (DDKT Self-Efficacy); higher scores indicated higher self-efficacy.
Finally, patients were asked whether they had “Already done,” “Plan to do,” or “Don’t plan to do” 11 small steps related to taking transplant actions (e.g., “Do you plan to call the transplant center to begin evaluation?”). Patients who said they had not “Already done” the action on the pre-intervention survey but reported having done so on the post-intervention survey were counted as having newly taken the step.
Other Measures
Demographic and clinical characteristics measured pre-intervention included: race, sex, age, education, health insurance type, sources of income, financial stability, dialysis type, date dialysis started, preferred communication mode, and health-related quality of life.24 We asked each patient whether they had previously read transplant brochures (yes/no) or watched transplant videos (yes/no). Health literacy was examined by asking how often patients required help reading hospital materials. Finally, we assessed the quality of social support a patient had (discrepancy between self-reported amount of social support needed and received), and medical mistrust (mean of 7 items of Medical Mistrust Index).25
Statistical Analyses
Details of the power analysis have previously been provided.21 We used a Bonferroni correction to adjust the alpha for multiple comparisons (0.05/3 = 0.017) between the 3 conditions. We calculated that 150 patients per condition would achieve 80% power to detect a 1-point difference in change in transplant knowledge between educational conditions. For continuous outcomes, to aid in interpretation of differences, standardized effect sizes were calculated as the mean difference in changes from pre- to post-survey divided by the change score standard deviation (Cohen’s d). For categorical or count outcomes, odds or incident rate ratios were used as effect size estimates. P-values presented in the results should be compared to the Bonferroni-corrected alpha value (0.017).
Since patients were clustered within dialysis centers, multilevel random effects models were used, modeling the dialysis center with a random intercept. The modified intent-to-treat (ITT) analysis set included all patients who completed the study, regardless of participation in the education activities. A supplemental analysis included only patients participating in the education process according to the condition-specific protocol plan. Specifically, this included patients in the patient-guided condition who reported reading the print material and watching the videos, and patients in the educator-guided condition who both read and watched the ETH program and attended all four telephone sessions.
Baseline characteristics were compared across educational conditions with Rao-Scott χ2 tests and multilevel, random effects linear regression models. For analysis of the primary outcome, transplant knowledge, a multilevel random effects regression model, with a random intercept for dialysis center, was used to estimate the difference in change in knowledge between educational conditions via a difference-in-differences approach. In the presence of missing data, this maximum likelihood-based modeling strategy produces unbiased estimates under an assumption that the missing data are missing at random, conditional on the observed data. Causal interpretation of the results rests on a stricter assumption of missing completely at random. A similar modeling strategy was applied for the secondary outcomes of DDKT and LKDT attitudes (Pros, Cons, and Self-Efficacy). Differences between the educational conditions in the count of new steps was analyzed with a multilevel random effects Poisson model. Finally, since Informed Decision-Making was assessed only post-intervention, proportional differences between educational conditions were examined with Rao-Scott χ2 tests to account for clustering within dialysis centers.
Exploratory analyses were conducted to evaluate possible heterogeneity of effect of the interventions, compared to control, by educational background, potential transplant derailers, or baseline outcome. Since this study was not powered to detect interaction effects, this work was exploratory, and p-values were not calculated.
RESULTS
Participants
In response to advertisements, 836 patients called for eligibility assessment. Of the 673 eligible patients, 83% (n=561) completed a baseline survey and were randomized with 189 allocated to the educator-guided Explore Transplant @ Home condition, 185 to the patient-guided Explore Transplant @ Home condition, and 187 to standard-of-care control group (Figure 1). After omitting patients who withdrew, died, or were lost to follow-up, 456 patients remained with 144 (76%) in the educator-guided condition, 152 (82%) in the patient-guided condition, and 160 (86%) in the control group. This represents the modified intent-to-treat (ITT) sample.
Figure 1.
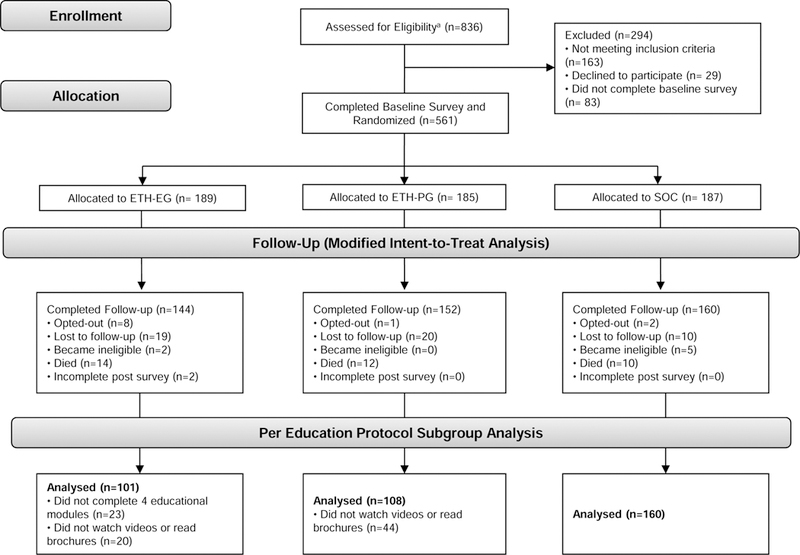
Study Flow Chart for Patient Selection
For the supplemental analyses in the per education protocol subgroup, 43 educator-guided intervention patients were omitted for not completing all four telephone education modules (n=23) and not reading the brochures or watching the videos (n=20); 44 patient-guided intervention patients were omitted for not reading the brochures or watching the videos. This analysis sample consisted of 369 patients (101 educator-guided intervention, 108 patient-guided intervention, and 160 control group).
There were no baseline differences between the randomized education conditions (Table 2). The largest proportion of patients were Black (70%-72%), had a high school diploma or less (48%-57%), used Medicare for health insurance (84%-90%), relied on income from disability benefits due to kidney disease (59%-68%), could live in their current situation for less than one month if income were lost (37%-46%), and were on hemodialysis (92%-94%). Most participants had read transplant brochures before joining the study (72%-76%), but few had watched videos about transplant (23%-31%). Characteristics of the per-education protocol subset of patients are in Table S1.
Table 2.
Dialysis Patient Participant Characteristics in the Modified ITT Sample
| Intervention | Standard of Care (n=187) |
p-value | ||
|---|---|---|---|---|
| Educator-Guided (n=189) |
Patient-Guided (n=185) |
|||
| Black race | 70% | 72% | 71% | 0.9 |
| Female sex | 51% | 48% | 48% | 0.7 |
| Age, y | 54 +/− 12 | 54 +/− 10 | 53 +/− 10 | 0.6 |
| PKD as etiology of kidney failure | 8% | 7% | 6% | 0.8 |
| Education level | 0.2 | |||
| High school diploma or less | 57% | 48% | 54% | |
| Some college | 31% | 37% | 29% | |
| College graduate or higher | 12% | 15% | 17% | |
| Health insurance | 0.3 | |||
| Medicare (National medical card) | 88% | 90% | 84% | |
| Medicaid (State medical card) | 8% | 6% | 10% | |
| Private insurance (HMO or PPO) | 1% | 2% | 4% | |
| Other insurance | 3% | 2% | 2% | |
| Source of incomeb | ||||
| Full-time employment | 2% | 1% | 1% | 0.9 |
| Retirement savings/pension | 4% | 4% | 6% | 0.8 |
| Social Security (Retirement) | 34% | 27% | 25% | 0.09 |
| Disability due to kidney disease | 59% | 59% | 68% | 0.1 |
| Disability due to other causes | 20% | 27% | 24% | 0.3 |
| If family lost current income, how long could you live in your current situation? | 0.3 | |||
| <1 month | 45% | 46% | 37% | |
| 1–6 months | 33% | 26% | 39% | |
| >7 months | 22% | 27% | 24% | |
| Hemodialysis as Dialysis Modality | 94% | 92% | 93% | 0.8 |
| Dialysis vintage, y | 4 [1–8] | 5 [2–7] | 3 [1–8] | 0.8 |
| Preferred mode of communication | 0.2 | |||
| Phone | 98% | 93% | 94% | |
| 0% | 2% | 1% | ||
| 1% | 2% | 2% | ||
| Text message | 1% | 3% | 3% | |
| Previously read transplant brochures | 72% | 75% | 76% | 0.6 |
| Watched transplant videos | 23% | 31% | 30% | 0.1 |
| How often requires help reading hospital materials | 0.2 | |||
| Never | 54% | 58% | 52% | |
| Any time | 46% | 42% | 48% | |
| Has needed social support | 73% | 78% | 78% | 0.4 |
| Medical mistrust c | 2.8 (0.6) | 2.8 (0.7) | 2.9 (0.6) | 0.2 |
| General health score d | 3.3 (1.0) | 3.4 (0.9) | 3.5 (1.0) | 0.1 |
(n=561). Values for continuous variables given as mean +/− standard devision or median [interquartile range].
Patients could check all appropriate options, so percentages down columns do not sum to 100%.
Score ranges from 1–4, with higher scores reflecting higher medical mistrust.
By CDC HRQOL-4; score ranges from 0–5, with higher scores reflecting higher health-related quality of life. ITT: intent-to-treat; PKD: polycystic kidney disease; HRQOL: health-related quality of life
Primary Outcome: Transplant Knowledge
At baseline, the mean transplant knowledge score was 7.2 (SD, 2.3; range, 0–14), indicating that patients responded correctly to less than 50% of the 15 questions. In comparison to the control group, significant increases in transplant knowledge were observed for the educator-guided and patient-guided conditions (Figure 2). The difference-in-differences analysis yielded the following estimated differences in knowledge increases between conditions: 0.6 (d = 0.26) for educator-guided intervention vs. control (p = 0.02), 0.7 (d = 0.30) for patient-guided intervention vs. control (p = 0.01) (Table 3). There was no heterogeneity of intervention effects on knowledge for any of the factors examined. The supplemental analysis produced similar results (Table S2).
Figure 2.
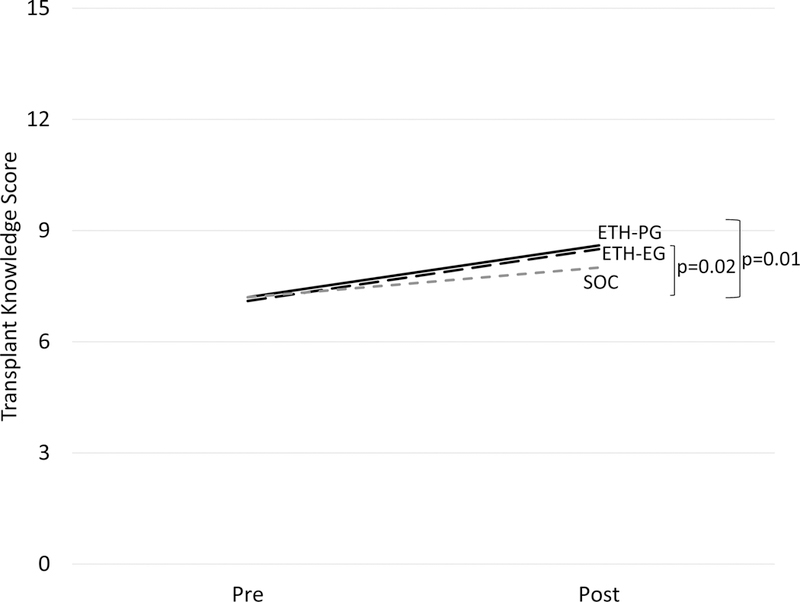
Pre- to Post Change in Transplant Knowledge Educational Condition – modified ITT sample
ETH-EG = Explore Transplant Educator-Guided Condition; ETH-PG = Explore Transplant Patient-Guided Condition; SOC = Standard of Care education Condition
ETH-EG vs. SOC p=0.02; ETH-PG vs. SOC p=0.01.
Table 3.
Difference-in-Differences Analysis of Pre- to Post-Change between Educational Conditions in Transplant Knowledge, LDKT Attitudes, and DDKT Attitudes in the Modified Intent-to-Treat Analysis (n=456)
| Intervention | Standard-of-Care (n=160) |
Difference-in-Differences (vs Standard-of-Care)a | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Educator-Guided (n=144) |
Patient-guided (n=152) |
||||||||||
| Pre | Post | Diff | Pre | Post | Diff | Pre | Post | Diff | Educator-Guided | Patient-Guided | |
| Transplant Knowledge | 7.1 | 8.5 | +1.4 | 7.2 | 8.6 | +1.4 | 7.2 | 8.0 | +0.8 | 0.6 (0.3), p=0.02 | 0.7 (0.3), p=0.01 |
| LDKT Pros | 24.3 | 25.1 | +0.8 | 25.4 | 25.4 | 0 | 25.5 | 25.0 | −0.5 | 1.3 (0.6), p=0.03 | 0.4 (0.6), p=0.5 |
| LDKT Cons | 20.5 | 19.8 | −0.7 | 19.4 | 19.6 | +0.2 | 19.7 | 19.8 | +0.1 | −0.7 (0.9), p=0.4 | 0.1 (0.9), p=0.9 |
| LDKT Self-Efficacy | 21.3 | 21.2 | −0.1 | 23.0 | 22.4 | −0.6 | 22.5 | 20.9 | −1.6 | 1.5 (0.9), p=0.1 | 1.0 (0.9), p=0.3 |
| DDKT Pros | 25.9 | 26.8 | 0.8 | 26.5 | 26.6 | 0.1 | 27.0 | 26.8 | −0.2 | 1.0 (0.5), p=0.04 | 0.3 (0.5), p=0.6 |
| DDKT Cons | 21.5 | 19.4 | −2.2 | 20.6 | 19.8 | −0.8 | 21.4 | 20.8 | −0.6 | −1.5 (0.7), p=0.03 | −0.2 (0.7), p=0.8 |
| DDKT Self-Efficacy | 30.8 | 31.5 | 0.7 | 33.2 | 32.2 | −1.0 | 33.4 | 32.2 | −1.2 | 1.9 (0.9), p=0.03 | 0.2 (0.9), p=0.8 |
Difference-in-differences b estimate (standard error)
LDKT: living donor kidney transplant; DDKT: deceased donor kidney transplant;
Secondary Outcomes: LDKT and DDKT Attitudes (Pros, Cons, and Self-Efficacy)
Marginally significant increases in LDKT and DDKT Pros were observed for educator-guided intervention compared to the control group. The difference-in-differences analysis yielded the following estimated differences in score changes: LDKT Pros, 1.3 (d = 0.27) for educator-guided intervention vs. control group (p = 0.03); DDKT Pros, 1.03 (d = 0.22) for educator-guided intervention vs. control (p = 0.04); DDKT Cons, −1.5 (d = 0.25) for educator-guided intervention vs. control (p = 0.03); and DDKT Self-Efficacy, 1.9 (d = 0.28) for educator-guided intervention vs. control (p = 0.03) (Table 3). No significant differences between the patient-guided intervention and control groups were observed. The supplemental analysis produced similar results (Table S3).
There were some notable differences in the effects of each educational condition within subgroups. The educator-guided intervention more effectively increased LDKT self-efficacy for patients with insufficient social support (6.6 [95% CI, 2.6 to 10.6] points) than for those with sufficient social support (0.2 [95% CI, −2.0 to 2.4] points), as well as for those with higher baseline LDKT Pros (5.3 [95% CI, 2.3 to 8.2] points) than lower LDKT Pros (−1.3 [95% CI, −3.9 to 1.2] points). The patient-guided intervention more effectively increased LDKT self-efficacy for patients with higher baseline transplant knowledge (4.3 [95% CI, 1.5 to 7.1] points) than for those with less knowledge (−1.7 [95% CI, −4.2 to 0.8] points).
Secondary Outcome: New Steps Toward Transplant
At baseline, patients reported having completed a median of 2 out of 11 steps toward transplant (IQR, 0–4). The most common steps that patients completed at baseline included calling the transplant center to begin KT evaluation (40%) and talking to transplant recipients about their experiences (34%). For all patients enrolled, the most common new steps taken between pre- and post-survey were: 1) sharing interest in LDKT with friends and family (25%); 2) talking to transplant recipients about their experiences (23%); 3) calling the transplant center to begin KT evaluation (17%); 4) making a list of potential living donors (17%); 5) talking to living donors about their experiences (16%); and 6) telling a transplant coordinator of their interest in LDKT (15%).
In a random effects Poisson model, the count of new steps taken by those in the patient-guided condition was marginally higher than that of those in the control group: incident rate ratio (IRR), 1.21 (95% CI, 1.01–1.47); p=0.04. However, there was no difference between the educator-guided and control group conditions: IRR, 1.04 (95% CI, 0.85–1.27); p=0.4 (Table 4). Only one subgroup difference was notable when examining heterogeneity of intervention effects. The educator-guided intervention more effectively increased the number of steps taken toward KT compared to control group among patients with more than a high school education (IRR, 2.20; 95% CI, 1.55–3.13), while patients with a high school education or less had a reduced number of steps taken compared to control group (IRR, 0.52; 95% CI, 0.37–0.74). The effect of patient-guided intervention was somewhat more pronounced in the supplemental analysis (Table S3).
Table 4.
Number of New Steps Taken from Pre- to Post-Survey in the Modified Intent-to-Treat Analysis
| Intervention | Standard-of-Care | ||
|---|---|---|---|
| Patient-Guided | Educator-Guided | ||
| No. of particpants | 144 | 152 | 160 |
| No. of steps: pre | |||
| Mean | 2.9 | 2.6 | 2.7 |
| Median | 2.0 | 1.0 | 2.0 |
| No. of steps: New from pre-post | |||
| Mean | 1.9 | 1.6 | 1.6 |
| Median | 1.0 | 1.0 | 1.0 |
| IRRa (95% CI) | 1.21 (1.01–1.47) | 1.04 (0.85–1.27) | Reference |
| p-value | 0.04 | 0.4 | - |
Incident rate ratio from Poisson model
Secondary Outcome: Informed Decision-Making
Compared to control patients, significantly higher proportions of patients randomized to the educator-guided and patient-guided conditions were able to make informed decisions about starting KT evaluation (82% [120/146] vs. 91% [115/127] vs. 95% [130/137], p=0.003), getting a DDKT (70% [103/147] vs. 84% [107/128] vs. 84% [115/137], p=0.003), and getting a LDKT (73% [106/145] vs. 91% [116/127] vs. 92% [125/136], p<0.001) (Figure 3). Heterogeneity of intervention association with informed decision-making was not examined because the small number of patients reporting an inability to make informed decisions (less than 20 in several instances) limits the stability of the required logistic regression models.
Figure 3.
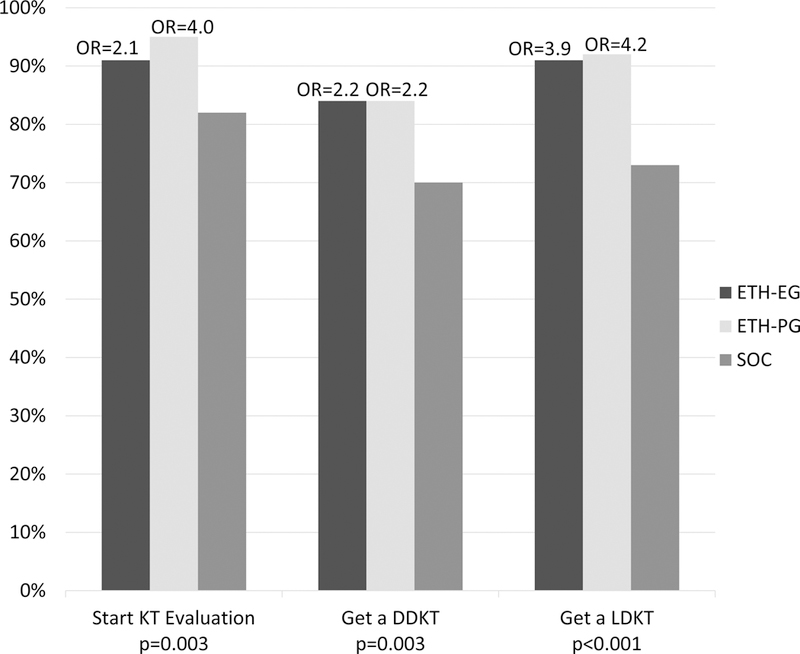
Differences in Reported Ability to Make an Informed Decision about Transplant Options at Post-Survey between Explore Transplant @ Home Conditions and Standard of Care – modified ITT Analysis
OR: Odds ratio, KT: Kidney transplant, DDKT: Deceased donor kidney transplant, LDKT: Living donor kidney transplant, ETH-EG: Explore Transplant at Home – Educator Guided, ETH-PG: Explore Transplant at Home – Patient Guided, SOC: Standard of Care. Odds ratios estimate the difference in odds of reporting being able to make an informed decision about KT evaluation, DDKT, and LDKT for each ETH condition vs. standard of care. Rao-Scott χ2 p-values are given for each overall comparison.
DISCUSSION
Research in over 6000 U.S. dialysis centers has shown that patients undergoing dialysis receive inconsistent KT education, with Black and low-income patients less likely to be educated about, referred for, and receive KTs or LDKTs.26 Applying best practices,3 this study examined the value of delivering systematic education over time and in varied delivery formats to support patients with different levels of health literacy and learning styles. The RCT found that the Explore Transplant @ Home eight month modular print, video, and texting program improved Black and low income patients’ knowledge and informed decision-making compared to standard education provided within dialysis centers. While the trial also assessed the value of a health educator to further enhance learning, increases in transplant knowledge over time were not improved if ETH patients had additional support from an educator compared to just receiving modular education directly.
In comparison to control group, both ETH programs were shown to significantly increase, from pre- to post-intervention, transplant knowledge and informed decisions about whether to start KT evaluation and whether to pursue DDKT or LDKT. The differences in increases in knowledge observed in this trial for both ETH conditions compared to the control group were over a longer period of time and of similar magnitude to differences in changes over time between educational interventions presented in shorter time frames in other transplant education trials.27, 28 Patients who received the patient-guided, rather than educator-guided, intervention had the highest proportion of patients reporting that they could make informed transplant decisions. Patients most likely to benefit from receiving supplemental ETH education included patients who already saw the benefits of LDKT at the start of the trial and those who had insufficient social support.
Finally, patient-guided intervention patients were marginally more likely to take small steps like talking about interest in LDKT with their families than control group patients. The same was not true for educator-guided intervention patients, except in the subgroup of patients with more than a high school education. These results resemble those from the Talking About Living Kidney Donation (TALK) program trial, which compared the efficacy of a print and video program on its own and accompanied by in-person social worker discussions about LDKT on CKD patients’ steps toward beginning transplant evaluation.29 Though the TALK trial found that the discussion-oriented, social worker intervention had a higher predicted probability of taking additional steps in comparison to the education-only group, this trial also found that significantly higher proportions of patients in the education-only group took key steps like completing the transplant evaluation. Considering the results of the TALK trial and the present study, it remains unclear whether discussions, either in-person or by telephone about DDKT or LDKT improve the chances of kidney patients pursuing transplant.
Because the intervention spanned eight months, there was variability in the delivery of the intervention components and survey completion rates, which could lead to bias in the study findings. For example, 16% of educator-guided intervention patients did not complete four telephone sessions with an educator. Thus, in addition to the modified ITT results, we reported a supplemental analysis using only patients fully adherent to the intervention protocol. Similarly, a higher proportion of control patients completed the follow-up surveys versus intervention patients. control patients were only required to complete the two surveys to receive the financial incentives and may have been less burdened from participating than intervention patients who received calls, texts, postcards, and mailings, and completed the surveys. Future studies should further explore the value of coaching, reduce the number of educational touchpoints, or use a shorter timeframe to ensure better adherence to the intervention. Other limitations include lack of dialysis center-level randomization. While center-level randomization would have prevented contamination due to communication among patients across educational arms, this risk was lower because the ETH program was mailed to patients’ homes, with no interventions occurring at dialysis centers. Additionally, our measures of informed decision-making were single-item subjective reports and were not verified with other sources of information collected from the patients, which may lead to some bias. Further, the presence of missing follow-up data requires the fairly strong, and untestable, assumption of missing completely at random for causal interpretation. Finally, due to funder requirements, no hard clinical end points, such as evaluation completion or receipt of DDKT or LDKT, could be examined. Future studies of this program must investigate impact on these outcomes.
In conclusion, this study establishes the efficacy of the Explore Transplant @ Home program in two forms to increase learning and informed decision-making for Black and low SES patients. A broader implication is that delivering educational content to patients directly, with the option of short phone conversations with educators, may help increase knowledge and informed transplant decision-making for large numbers of patients on dialysis without placing additional burdens on dialysis providers.
Supplementary Material
Acknowledgements:
Thank you to the team of research assistants who supported this program, including Lizeth Ambriz, AuBre Parnicky, Marisa Torres, and Grace Park, and to Amanda Faye Lipsey, for her assistance in preparing and editing this manuscript, as funded by the Terasaki Research Institute.
Support: This project received support from the NIH NCATS UCLA CTSI, Grant Number UL1TR001881, and from the Health Resources and Services Administration, Grant Number R39OT25725. The funding organizations had no role in the study design; collection, analysis, and interpretation of data; writing of the report, or the decision to submit for publication.
Funding Source: This project was funded by the NIH and HRSA.
Footnotes
Supplementary Material
Table S1. Dialysis patient participant characteristics in the per education protocol subgroup.
Table S2. Difference-in-differences analysis of pre- to post-change between educational conditions in transplant knowledge, LDKT attitudes, and DDKT attitudes in the per education protocol subgroup.
Table S3. Number of new steps taken from pre- to post-survey in the per education protocol subgroup.
Supplementary Material Descriptive Text for Online Delivery
Supplementary File (PDF). Tables S1–S3.
Financial Disclosure: Dr. Amy D. Waterman, PhD owns the intellectual property to the transplant education product Explore Transplant and has licensed it at no cost to a nonprofit, Health Literacy Media (HLM), which retains all sales revenue. Dr Waterman serves as an unpaid consultant to HLM to ensure the accuracy of educational content. The remaining authors declare that they have no relevant financial interests.
Prior Presentation: Aspects of this work were presented at the 2018 American Transplant Congress.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Saran R, Robinson B, Abbott KC, et al. US Renal Data System 2017 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am J Kidney Dis 2018; 71(3)(suppl 1):S1–S676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Neipp M, Karavul B, Jackobs S, et al. Quality of life in adult transplant recipients more than 15 years after kidney transplantation. Transplantation 2006;81(12): 1640–1644. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Medicare & Medicaid Services. Medicare and Medicaid Programs; Conditions for Coverage for End-Stage Renal Disease Facilities; Final Rule. In: Department of Health and Human Services, ed. Vol 73 Baltimore, MD: Federal Register; 2008. [PubMed] [Google Scholar]
- 4.Hall EC, James NT, Garonzik Wang JM, et al. Center-level factors and racial disparities in living donor kidney transplantation. Am J Kidney Dis 2012;59(6): 849–857. [DOI] [PubMed] [Google Scholar]
- 5.Waterman AD, Peipert JD, Hyland SS, McCabe MS, Schenk EA, Liu J. Modifiable patient characteristics and racial disparities in evaluation completion and living donor transplant. Clin J Am Soc Nephrol 2013;8(6): 995–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alvaro EM, Siegel JT, Turcotte D, Lisha N, Crano WD, Dominick A. Living kidney donation among Hispanics: a qualitative examination of barriers and opportunities. Prog Transplant 2008;18(4): 243–250. [DOI] [PubMed] [Google Scholar]
- 7.Gordon EJ, Mullee JO, Ramirez DI, et al. Hispanic/Latino concerns about living kidney donation: a focus group study. Prog Transplant 2014;24(2): 152–162. [DOI] [PubMed] [Google Scholar]
- 8.Wachterman MW, McCarthy EP, Marcantonio ER, Ersek M. Mistrust, Misperceptions, and Miscommunication: A Qualitative Study of Preferences About Kidney Transplantation Among African Americans. Transplantation Proceedings 2015;47(2): 240–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johns TS, Estrella MM, Crews DC, et al. Neighborhood socioeconomic status, race, and mortality in young adult dialysis patients. J Am Soc Nephrol 2014;25(11): 2649–2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hinck BD, Naelitz BD, Jackson B, Howard M, Nowacki A, Modlin CS. Assessing Transplant Attitudes: Understanding Minority Men’s Perspectives on the Multifarious Barriers to Organ Donation. Journal of racial and ethnic health disparities 2017;4(4): 580–586. [DOI] [PubMed] [Google Scholar]
- 11.Axelrod DA, Dzebisashvili N, Schnitzler MA, et al. The interplay of socioeconomic status, distance to center, and interdonor service area travel on kidney transplant access and outcomes. Clin J Am Soc Nephrol 2010;5(12): 2276–2288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herring AA, Woolhandler S, Himmelstein DU. Insurance status of U.S. organ donors and transplant recipients: the uninsured give, but rarely receive. Int J Health Serv 2008;38(4): 641–652. [DOI] [PubMed] [Google Scholar]
- 13.Laurentine KA, Bramstedt KA. Too poor for transplant: finance and insurance issues in transplant ethics. Prog Transplant 2010;20(2): 178–185. [DOI] [PubMed] [Google Scholar]
- 14.McSorley A-MM, Peipert JD, Gonzalez C, et al. Dialysis Providers’ Perceptions of Barriers to Transplant for Black and Low-Income Patients: A Mixed Methods Analysis Guided by the Socio-Ecological Model for Transplant. World Medical & Health Policy 2017;9(4): 399–416. [Google Scholar]
- 15.Rodrigue JR, LaPointe Rudow D, Hays R, American Society of T. Living Donor Kidney Transplantation: Best Practices in Live Kidney Donation--Recommendations from a Consensus Conference. Clin J Am Soc Nephrol 2015;10(9): 1656–1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ruck JM, Zhou S, Thomas AG, et al. Electronic messaging and communication with living kidney donors. Clin Transplant 2018;32(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev 2010;32(1): 56–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang TC, Huang JL, Ho WC, Chiou AF. Effects of a supportive educational nursing care programme on fatigue and quality of life in patients with heart failure: a randomised controlled trial. European journal of cardiovascular nursing : journal of the Working Group on Cardiovascular Nursing of the European Society of Cardiology 2016;15(2): 157–167. [DOI] [PubMed] [Google Scholar]
- 19.Reilly-Spong M, Reibel D, Pearson T, Koppa P, Gross CR. Telephone-adapted mindfulness-based stress reduction (tMBSR) for patients awaiting kidney transplantation: Trial design, rationale and feasibility. Contemp Clin Trials 2015;42: 169–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vaiva G, Vaiva G, Ducrocq F, et al. Effect of telephone contact on further suicide attempts in patients discharged from an emergency department: randomised controlled study. BMJ 2006;332(7552): 1241–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Waterman AD, McSorley AM, Peipert JD, et al. Explore Transplant at Home: a randomized control trial of an educational intervention to increase transplant knowledge for Black and White socioeconomically disadvantaged dialysis patients. BMC Nephrol 2015;16: 150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Waterman AD, Robbins ML, Paiva AL, et al. Measuring kidney patients’ motivation to pursue living donor kidney transplant: development of stage of change, decisional balance and self-efficacy measures. J Health Psychol 2015;20(2): 210–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Waterman AD, Robbins ML, Paiva AL, Hyland SS. Kidney patients’ intention to receive a deceased donor transplant: development of stage of change, decisional balance and self-efficacy measures. J Health Psychol 2010;15(3): 436–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med 1993;118(8): 622–629. [DOI] [PubMed] [Google Scholar]
- 25.LaVeist TA, Isaac LA, Williams KP. Mistrust of health care organizations is associated with underutilization of health services. Health Serv Res 2009;44(6): 2093–2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Waterman AD, Peipert JD, Xiao H, et al. Education Strategies in Dialysis Centers Associated with Increased Transplant Wait-listing Rates. Transplantation 2019;In Press. [DOI] [PMC free article] [PubMed]
- 27.Rodrigue JR, Paek MJ, Egbuna O, et al. Making house calls increases living donor inquiries and evaluations for blacks on the kidney transplant waiting list. Transplantation 2014;98(9): 979–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rodrigue JR, Cornell DL, Lin JK, Kaplan B, Howard RJ. Increasing live donor kidney transplantation: a randomized controlled trial of a home-based educational intervention. Am J Transplant 2007;7(2): 394–401. [DOI] [PubMed] [Google Scholar]
- 29.Boulware LE, Hill-Briggs F, Kraus ES, et al. Effectiveness of educational and social worker interventions to activate patients’ discussion and pursuit of preemptive living donor kidney transplantation: a randomized controlled trial. Am J Kidney Dis 2013;61(3): 476–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


