Abstract
Background
There are inconsistencies in findings regarding the relationship of occupational loading with spinal degeneration or structural damage. Thus, a systematic review was conducted to determine the current state of knowledge on the association of occupational loading and spine degeneration on imaging.
Methods
We performed electronic searches on MEDLINE, CINAHL and EMBASE. We included cross-sectional, case control and cohort studies evaluating occupational loading as the exposure and lumbar spine structural findings on imaging as the outcomes. When possible, results were pooled.
Results
Seventeen studies were included in the review. Ten studies evaluated the association of occupational loading with disc degeneration (signal intensity), four of which were pooled into a meta-analysis. Of the 10 studies, only two did not identify a relationship between occupation loading and disc degeneration. A meta-analysis including four of the studies demonstrated an association between higher loading and degeneration for all spinal levels, with odds ratios between 1.6 and 3.3. Seven studies evaluated disc height narrowing and seven evaluate disc bulge, with six and five identifying an association of loading and with imaging findings respectively. Three studies evaluated modic changes and one identified and association with occupational load.
Conclusions
There was moderate evidence suggesting a modest association between occupational loading and disc degeneration (signal intensity), and low-quality evidence of an association between occupational loading and disc narrowing and bulging.
Keywords: Occupational load, Spine degeneration, Disc degeneration, Disc height, Imaging, Magnetic resonance imaging, X-ray
Background
The cumulative or repetitive injury model was once a dominant paradigm of spine degeneration [1]. Thus, heavy occupational physical loading activities have long been suspected of increasing spine degeneration. However, inconsistencies between study findings, with some supporting this association [2, 3] and other not [4, 5], have led to controversy and uncertainty about the relationship between physical loading and lumbar spine degeneration. Furthermore, recent studies suggest that the structures of the spinal column, including the intervertebral discs, adapt and may even benefit from greater routine physical loading [1].
Controversy still exists between the relationship of occupational load and low back pain [6]. However, given the subjective nature of pain evaluation and the high prevalence of back pain in general, studies depicting the association between pain and occupation load always have large room for bias. The use of objective measures of spine degeneration to evaluate the impact of occupational load on the spine can provide a solution to better understanding this relationship. The evaluation of spine degeneration on imaging is both a reliable and objective measure to evaluate the effects of repetitive load on the spine, which in turn may mediate the occurrence of back pain in this population. Although spine degeneration on imaging is not synonym of back pain, spine degeneration on imaging have been found to be associated with an increased risk for low back pain [7] and increased risk of recurrent episodes [8].
Given the inconsistencies in the literature about the association of occupational load and spine degeneration, the objective of this study was to systematically review the literature on the association of occupational loading and spine degeneration observed on imaging. Occupational loading was described as loading conditions occurring during occupational activities, such as lifting and manual handling or comparisons between specific occupations.
Methods
A protocol for the study was developed a priori following the PRISMA guidelines and Cochrane Handbook.
Data sources and searches
A computerised electronic search was performed to identify relevant articles. The search was conducted on MEDLINE (1946 to May 2019), CINAHL (1982 to May 2019) and EMBASE (1988 to May 2019). Key words included in our search were related to 3 domains: imaging (i.e. x-ray, radiograph), imaging findings (i.e. disc degeneration, disc height) and load (i.e. manual handling, occupational load). Subject subheadings and word truncations specific for each database were used. There was no language restriction. See Additional file 1 for search strategy section.
Two reviewers screened search results (titles and abstracts) for potentially eligible studies. A third independent reviewer resolved any disagreement for inclusion of trials. Authors were contacted if more information about the trial was needed to allow inclusion of the study.
We also performed a search on the reference lists of the included studies and a search on ISI Web of Sicence (May 2019) for papers that cited the included studies.
Study selection
Cross-sectional, case-control and cohort studies evaluating occupational loading as the exposure were eligible for inclusion. All studies that evaluated professional athletes and whole body vibration as a form of exposure were included on a separate review. In addition, the study had to evaluate the relationship of loading with lumbar spine structural findings evaluated on diagnostic imaging. Studies that used back pain as an outcome measure were not included. Studies that included patients with pre-existing conditions, such as disc herniation, were excluded from the review as they are more likely to have positive findings on imaging and may provide biased estimates for the relationship under investigation. Two reviewers screened the full text of potentially eligible studies and decided on inclusion. A third independent reviewer resolved any disagreement for inclusion of studies. The reviewers followed a research protocol developed prior to the beginning of the review, which included a checklist of inclusion criteria.
Data extraction and quality assessment
The methodological quality of the trials was assessed using the Newcastle Ottawa Quality Assessment scale [9, 10] for case-control and cohort studies. The maximum value of the scale is 9 (high quality) and the minimum value is 0 (lowest quality). The quality was assessed by independent raters and disagreements were resolved by a third rater. Methodological quality was not an inclusion criterion but was taken into consideration when making conclusions.
Two independent reviewers (LM and research assistants) extracted data from the included studies using a standardized data extraction form. Important characteristics of each study were extracted, such as type of loading, study design, type of imaging, patient population, affiliation of the authors, funding source, and study conclusions. We also extracted the type of outcomes used, and for continuous outcome measurements we extracted mean scores, standard deviations and sample size, and for dichotomous and ordinal outcomes, sample size and number of events per group.
Data synthesis and analysis
Results were pooled when trials were considered sufficiently homogenous with respect to participant characteristics, exposure and outcomes. I2 was calculated using RevMan 5 to assess statistical heterogeneity. A random effects model was used to pool all available outcomes. I2 was calculated to evaluate statistical heterogeneity of pooled outcomes [11]. When adequate data were presented from the original study, mean differences and standard deviations for continuous outcomes and odds ratios for dichotomous outcomes were calculated. When such information was not available, the information presented in each study was used for interpretation of the results.
The GRADE approach for grading the level of the evidence available was used to summarize the conclusion of this review [11]. Depending on the number and quality of the studies included in the review, the evidence was classified into high, moderate, low or very low quality evidence.
Results
Study selection
The electronic database search resulted in a total of 5363 articles after removing duplicates. Of these, 137 were selected as potentially eligible based on their title and abstract.
After full title screening a total of 16 studies were included in the review. An additional ISI web of science search showed 11 more potentially eligible studies, from which 1 was included in the review. Therefore, the final number of included studies was 17. (Flowchart_ Fig. 1).
Fig. 1.
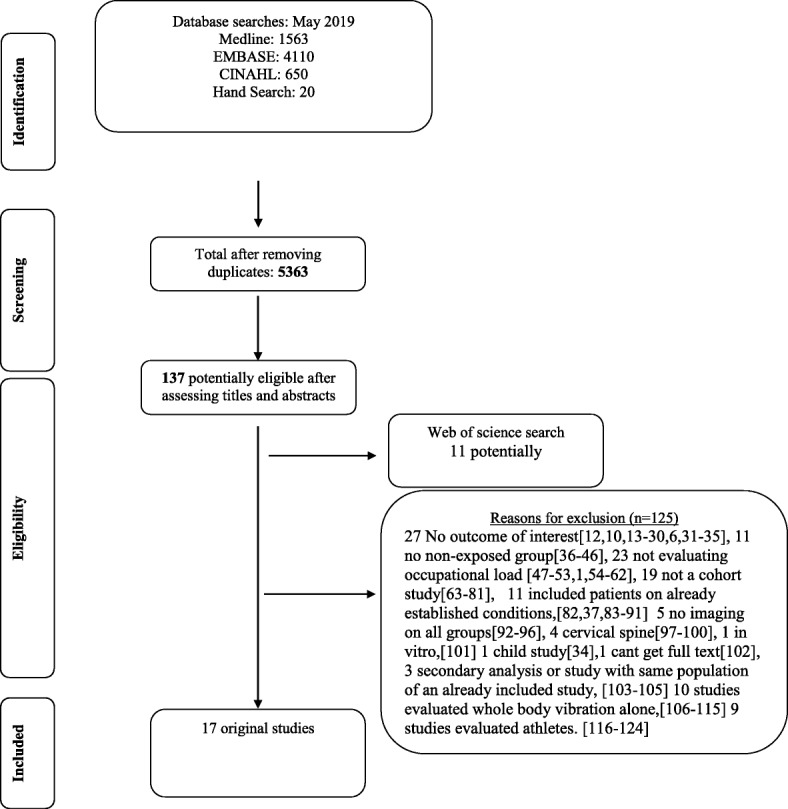
Flow chart of occupational load systematic review inclusion
125 Exclusion for graph only * 27 No outcome of interest [6, 10, 12–30, 31–35], 11 no non-exposed group [36–46], 23 not evaluating occupational load [1, 47–53, 54–62], 19 not a cohort study [63–81], 11 included patients on already established conditions, [37, 82–91] 5 no imaging on all groups [92–96], 4 cervical spine [97–100], 1 in vitro, [101] 1 child study [34], 1 cant get full text [102], 3 secondary analysis or study with same population of an already included study, [103–105] 10 studies evaluated whole body vibration alone, [106–115] 9 studies evaluated athletes [116–124].
Study characteristics
There were 16 original studies evaluating occupational load [2–5, 125–136] including 1 follow-up study [137]. Ten studies evaluated specific job requirements such as occupational lifting or job load summary score [2, 4, 127–130, 132, 133, 135–137] and six compared different types of occupation with different occupational requirements [3, 5, 125, 126, 131, 134]. See Table 1 for study characteristics.
Table 1.
Study characteristics
| Author | Methodological Quality | Imaging | Study Design | Participant information |
|---|---|---|---|---|
| Arevalo et al. 2014 | 5 | MRI | Retrospective cohort study |
N = 652; 326 patients with established diagnosis of lumbar disc herniation on MRI and 326 patients without herniation. Age range was assessed but not reported. |
| Battie et al. 1995 | 6 | MRI | Cross sectional |
Monozygotic twin pairs from the Finnish Twin Cohort selected based on loading discordances. (n = 230 twins or 115 pairs) Age range from 35 to 69 years. |
| Biering-Sorense et al. 1985 | 4 | x-ray | Longitudinal cohort study |
666 participants taking part in a population study of 60-yerar-old inhabitants from the area around Glostrip Hospital in the suburbs of Copenhagen. All participants were either 50 or 60 years of age. |
| Brinckmann et al. 1998 | 5 | x-ray | Retrospective cohort study |
355 subjects with long term exposure to heavy physical load (from different professions) and 737 healthy controls compiled from healthy unexposed subjects. Participants were between 17 to 57 years old. |
| Elfering et al. 2002 | 3 | MRI | longitudinal cohort study |
46 asymptomatic patients from a group of 2000 trauma patients presenting to the university trauma clinic with minor extremity injuries with complete recovery. Participants were between 20 and 50 years of age. |
| Frymoyer et al. 1984 | 3 | x-ray | Cross sectional (retrospective) |
321 random patients from a sample of 1221 from a previous study. Only 285 were included in the occupation vs imaging study due to reasons such as imaging quality Participants were between 18 an d55 years of age. |
| Han et al. 2017 | 6 | MRI and x-ray | Cross sectional |
210 patients with low back pain attending the hospital. All underwent imaging evaluation and responded to questionnaires about workload. Age ranged from 40 to 60 years. |
| Hangai et al. 2008 | 4 | MRI | cross sectional |
Recruited over 50 year old to participate in a health promotion program though newspapers in Japan. Those with imaging were recruitment. N = 270 (1350 discs) All participants were between 51 and 86 years. |
| Hartwig et al. 1997 | 4 | MRI | Cross sectional |
Recruited 142 participants from 35 to 50 years old that were either nurse (n = 54), construction workers (n = 51) or controls (n = 37). Unclear how controls were selected All patients were between 35 and 50 years old. |
| Hung et al. 2014 | 6 | MRI | Cross sectional |
553 workers that carry heavy loads (fruit market workers) versus walk in clinic patients (most commonly diagnosis was common cold). After that all participants were assessed using questionnaires and functional assessment for the amount of lifting load and then categorized into either low, intermediate, or high lifting loads. Participants were between 20 and 65 years old. |
| Luoma et al. 1998 | 8 | MRI | cross sectional |
Patients were extracted from a cohort participating in a study evaluating occupational effects of LBP. (n = 164, 53 drivers, 51 carpenters and 60 office workers). Participants were between 40 and 45 years old. |
| Munoz-Gomez et al. 1980 | 5 | x-ray | Cross sectional |
Workers from an industry All participants were between 19 to 63 years of age. |
| Riihimaki et al. 1990 | 6 | x-ray | cross sectional |
N = 417 Male workers. 216 concrete reinforcement workers of an specific area were included and 201 house painters from a local union. Painters were matched with concrete workers based on a 5-year strata. Participants were between 25 to 54 years of age. |
| Savage et al. 1997 | 4 | MRI | cross sectional (only 60% participated in the longitudinal cohort) |
Volunteers from different occupations. N = 149 (24 ambulance men, 16 hospital porters, 40 car production workers, 12 brewery drayman and 57 office workers). All participants were between 20 and 58 years of age and were divided in two groups 20–30 and 31 to 58 years. |
| Schenk et al. 2006 | 7 | MRI | Cross sectional - case control |
N = 109 staff of local hospital that worked at least 20 h per week. (57 nurses and 52 administration workers) All participants were between 45 and 62 years old. |
| Videman et al. 2006 | 7 | MRI | longitudinal cohort study |
Monozygotic twin pairs from the Finnish Twin Cohort selected based on smoking, exercise or occupational loading discordance. (n = 140 twins or 70 pairs). All participants were between 35 to 69 years of age. |
| Videman et al. 2007 | 7 | MRI | restrospective cohort study |
N = 600 patients from the Finnish Twin Cohort. 474 were included in the model for disc signal and 513 in the model for disc height (inclusion was dependent on availability or imaging and occupational data) All participants were between 35 to 70 years of age. |
Methodological quality was assessed using the Newcastle Ottowa Assessment Scale for case control studies or cohort studies accordingly. Scores are given in starts with a maximum (higher quality) of 9 starts
Methodological quality
The methodological quality demonstrated an overall moderate level of quality, with a minimum of 3, a maximum score of 8, and a median and interquartile range of 5 and 3. The items of the methodological quality scale that were not present in most studies were control of potentially confounding factors and reporting of the response rate of each group.
Three studies included the same population from the Finnish Twin Spine study, but answered different questions related to different outcomes. These studies represent the strongest form of evidence given that controls are identical twins, minimizing possible confounding and familial aggregation [127, 128].
Outcomes
Ten studies evaluated the impact of loading on disc degeneration, generally assessed through disc signal intensity, representing disc desiccation [2–5, 126–129, 133, 134, 137]. The primary method of evaluating disc degeneration is through observing disc signal intensity on imaging. Disc degeneration is often associated with a whiter less translucent appearance of the disc [126]. Of these 10 studies only two did not find significant differences between groups [3, 129] and one study found more degeneration in those with less load [127]. In one study we were not able to assess whether statistical differences existed [134]. Seven studies identified some significant difference between loading groups with more load being associated with more degeneration, although we were not able to pool the results given the differences in types of loads and outcomes measured [2, 4, 5, 126–128, 133]. For all comparisons odds ratios when calculated varied between 1.89 to 3.7. A summary of the findings is presented in Table 2. One additional study looked at an overall measure of degeneration that included a combination of factors, and found that occupational loading was associated with the overall degeneration measurements [130].
Table 2.
Exposure and results of each study included in the review that evaluated occupational load
| Study | Type of loading or exposure | Outcomes | Study results and RevMan analysis |
|---|---|---|---|
| Disc degeneration | |||
| Battie et al. 1995 | job code (1–4), total occupational lifting (day), mean time working twisted/bent, mean time sitting at work, occupation driving (hrs lifetime) | Disc degeneration (signal intensity) | There was an association between job code (0–4), occupational lifting and occupational sitting with disc degeneration. Greater occupational loading/lifting was associated with greater disc degeneration but associations were small (r = 0.18–0.31) Those with sitting had less disc degeneration. |
| Biering-Sorensen et al. 1985 | work is sedentary, light manual or heavy manual; worker undertakes heavy manual work, amount of physical activity at work | Relative disc degeneration (method was unclear) (for each level from L1 to S1) | RevMan: there was statistically significantly greater for L4 disc degeneration in daily manual workers compared to seldom manual workers (OR = 2.27; 95% CI 1.21 to 4.25), but no difference in disc degeneration at L5 (OR = 1.21; 95% CI 0.44 to 3.36) for physical activity at work. All other comparisons for disc degeneration were not significant but data was not presented. |
| Elfering et al. 2002 | Frequent lifting or carrying heavy objects, forward bending, vibration, sedentary activity, working night shifts |
Disc degeneration (1–5 Pearce score) (summary score for all levels together) |
The association of working night shifts and disc degeneration did not reach statistical significance (OR = 9.58 95% CI 1.00 to 91.62) |
| Hangai et al. 2008 | Lifting more than 10 kg for more than one third of the working hours. | Disc degeneration (signal intensity with modified Pirfmann’s classification) (for each level from L1 to S1) | RevMan: Occupational lifting was not significantly associated with degeneration at any of the levels. L1 L2 (OR = 3.16 95% CI 0.37 to 26.75), L2 L3 (OR = 1.92 95% CI 0.20 to 18.61), L3 L4 (OR = 1.34 95% CI 0.05 to 38.91), L4 L5 (OR = 2.23 95% CI 0.21 to 23.84) and L5S1 (OR = 1.48 95% CI 0.09 to 23.88) |
| Hartwig et al. 1997 | Nurse, construction workers and controls | Unclear disc degeneration measure assessed as mono, bi, tri or multi-segmental. | Not enough data to calculate an odds ratio. Results suggest that 17% of patients with high workload had mono-segmental degeneration as opposed to 29% of those with no workload, suggesting that those with more workload had degeneration at more levels. |
| Hung et al. 2014 | Workers that carry heavy loads divided into low, intermediate and moderate lifting loads. | Disc dehydration (T2-weigthed signal intensity loss | There was a statistically significant difference in disc degeneration (dehydration) between lifting loads for L1 L2 (OR = 2.4 95% CI 1.4 to 4.0), L2 L3 (OR = 3.3 95% CI 1.3 to 3.2), L3 L4 (OR = 3.7 95% CI 2.4 to 3.5), L4 L5 (OR = 4.9 95% CI 3.0 to 8.0) and L5S1 (OR = 3.6 95% CI 2.3 to 5.7) when comparing the high load to the low load groups. There was also a significant difference between the intermediate and low load groups for L2 L3, L3 L4, L4 L5 and L5S1. |
| Luoma et al. 1998 | Drivers, carpenters and office workers | Disc signal intensity (L2 L3-L5S1) | RevMan: There were no differences between groups. L2 L3 (OR = 0.55 95% CI 0.16 to 1.96), L3 L4 (OR = 1.50 95% CI 0.66 to 3.42), L4 L5 (OR = 2.04 95% CI 1.35 to 3.08) and L5S1 (OR = 1.30 95% CI 0.70 to 2.43) |
| Savage et al. 1997 | ambulance workers, hospital porters, car production workers, brewery drayman and office workers | Disc degeneration (signal intensity) (all levels together) | RevMan: There was no difference between groups in relation to disc degeneration. Car production vs office workers (OR = 1.00 95% CI 0.34 to 2.94); hospital porters vs office workers (OR = 1.63 95% CI 0.45 to 5.91 |
| Schenk et al. 2006 | nurses and office workers | Disc degeneration (signal intensity) (1–5) | RevMan: Disc degeneration was different between occupational groups for grade 2 with more degeneration in nurses (OR: 1.89; 95% CI 1.34 to 2.66, n = 544 all levels) and grade 4 with more degeneration in office workers (OR = 0.50 95% CI 0.29 to 0.86). There was no difference for grade 3 (OR = 1.14 95% CI 0.80 to 1.64) and grade 5 (OR = 0.75 95% CI 0.37 to 1.52), |
| Videman et al. 2007 |
Job code (1–4) History of lifting at work (1000 kg) |
Disc signal intensity (L1-S1) | There was a significant association between history of lifting at work and signal intensity in the opposite direction (better signal with more load (Regression coefficient 0.001, p = 0.002), there was no association of occupational loading scoring and disc degeneration. |
| Disc height | |||
| Battie et al. 1995 | job code (1–4), total occupational lifting (day), mean time working twisted/bent, mean time sitting at work, occupation driving (hr lifetime) | Disc height | There was an association between job code (0–4), occupational lifting and occupational sitting with disc height but the association was not strong r = −0.22) |
| Biering-Sorensen et al. 1985 | work is sedentary, light manual or heavy manual; worker undertakes heavy manual work, amount of physical activity at work | Disc height (for each level from L1 to S1) | There were no significant differences for disc height |
| Brinckmann et al. 1998 | Different occupations such as mining, steelworkers and normative data of unexposed individuals | Disc height (for each level from T12 to S1) | Occupational loading was associated with a smaller disc height at a few spinal levels, particularly in those working in underground mines. |
| Hung et al. 2014 | Workers that carry heavy loads divided into low, intermediate and moderate lifting loads. | Disc height narrowing (Farfan method. L4 L5 and L5S1 | RevMan: There were significant differences between groups for disc height narrowing at L5S1 (OR = 5.8 (2.7 to 13.6)). |
| Riihimaki et al. 1990 | Concrete reinforcement workers and house painters | Disc space narrowing (0–5 for each level) | RevMan: Concrete workers had greater disc height narrowing overall (OR = 2.19; 95% CI 1.34 to 3.58), L3 L4 (OR = 5.34; 95% CI 1.17 to 24.39) and L4 L5 (OR = 2.54; 95% CI 1.26 to 5.11) than painters. There was no difference at L1 L2 (OR = 2.84 95% CI 0.57 to 14.25), L2 L3 (OR = 0.93 95% CI 0.13 to 6.66) and L5S1 (OR = 1.35 95% CI 0.73 to 2.48). |
| Videman et al. 2006 | Job code (1–4), occupational driving, maximum weight lifted at work (kg) | Disc height narrowing | There was an association between occupational lifting and changes in degeneration over 5 years. (0.1 points/disc decrease in disc height = 0.021) |
| Videman et al. 2007 | Job code (1–4) | Disc height T12-S1) | There was an association between lifetime occupational loading score and disc height (regression coefficient 0.038, p = 0.004) and no association between history of lifting at work and disc height. |
| Overall measure of degeneration | |||
| Munoz-Gomez et al. 1980 | Work load calculated as above or below the general average | Degeneration (osteophytes, disc bulge and costotransversal arthrosis) | RevMan: Those with occupational load greater than the average had greater degeneration (OR = 1.63; 95% CI 1.03 to 2.57). |
| Disc Bulge or herniation | |||
| Arevalo et al. 2014 | Heavy physical work activities | Disc herniation | There was an association between heavy physical work and disc herniation (OR = 2.0; 95%CI 1.42 to 2.76) |
| Battie et al. 1995 | job code (1–4), total occupational lifting (day), mean time working twisted/bent, mean time sitting at work, occupation driving (hr lifetime) |
Disc bulging (summary score for upper T12-L4 and lower lumbar spine L4-S1) |
There was no association between occupational loading and disc bulging |
| Hung et al. 2014 | Workers that carry heavy loads divided into low, intermediate and moderate lifting loads. | disc bulging, L4 L5 and L5S1 | There was a statistically significant difference in disc bulging between lifting categories for L2 L3 (OR = 3.8 (2.3 to 6.3)), L3 L4 (OR = 3.6(2.4 to 5.6)), L4 L5 (OR = 3.1 (2.0 to 4.9) and (L5S1 (OR = 2.6 (1.7 to 4.0) when comparing the high load to the low load groups. |
| Luoma et al. 1998 | Drivers, carpenters and office workers | Disc bulging | RevMan: Carpenters were more likely to have posterior disc bulging at L3 L4 OR = 2.73; 95% CI 1.12 to 6.64) and anterior bulging at L45 (OR = 2.86; 95% CI 1.05 to 7.79) when compared to the sedentary group. There was no difference for anterior disc bulging at L2 L3 (OR = 2.60 95% CI 0.74 to 9.22), L3 L4 (OR = 3.0 95% CI 0.86 to 10.41) and L5S1 (OR = 1.39 95% CI 0.49 to 3.92) or posterior disc bulging at L2 L3 (OR = 2.53 95% CI 0.60 to 10.69), L4 L5 (OR = 1.92 95% CI 0.89 to 4.16) and L5S1 (OR = 1.33 95% CI 0.95 to 1.87) |
| Schenk et al. 2006 | nurses and office workers | Disc abnormalities (bulging, protusion, extrusion, etc) | RevMan: There was no significant difference in disc bulging between groups. (OR = 1.33 95% CI 0.95 to 1.97) |
| Videman et al. 2006 | Job code (1–4), occupational driving, maximum weight lifted at work (kg) | Disc bulging | There was an association between occupational lifting and disc bulging (0.07 points/disc increase in disc height = 0.065) |
| Modic changes | |||
| Elfering et al. 2002 | Summary score from 0 to 4 combining of lifting or carrying heavy objects, forward bending, vibration and sedentary work | Modic changes (summary score for all levels together) | Occupational loading was not associated Modic changes |
| Han et al. 201 | Work was self-reported and rated as light physical (mainly walking, moderate physical work (sitting/walking) and hard physical work (heavy working) | Modic changes assessed according to Modic et al. and graded into Type I, II or II. | There was a significant difference in the incidence of modic changes according to the level of physical work. In total 8 of 54 (15%) of those with light physical work had modic changes, 16 of 99 (26%) of those with moderate physical load and 23 of 57 (40%) of those with hard physical work had modic changes |
| Schenk et al. 2006 | nurses and office workers | Modic changes | RevMan: There was no difference in Modic changes between groups. (OR = 0.91 95% CI 0.52 to 1.58), |
| Schmorl’s nodes | |||
| Frymoyer et al. 1984 | Lifting | Schmorl’s nodes | There was no association between lifting and the spine outcomes evaluated. |
| Endplate abnormalities | |||
| Riihimaki et al. 1990 | Concrete reinforcement workers and house painters | Endplate sclerosis | RevMan: There was no difference in endplate sclerosis between groups. Overall (OR = 1.97 95% CI 0.96 to 4.05), L1 L2 (OR = 4.70 95% CI 0.22 to 98.43), L2 L3 (OR = 2.84 95% CI 0.57 to 14.25), L3 L4 (OR = 0.93 95% CI 0.13 to 6.66), L4 L5 (OR = 2.84 95% CI 0.57 to 14.25) and L5S1 (OR = 0.83 95% CI 0.33 to 2.09) |
| Videman et al. 2006 | Job code (1–4), occupational driving, maximum weight lifted at work (kg) | Upper endplate irregularities | There was no association between occupational lifting and changes in endplate abnormalities over a 5-year follow-up. |
| Osteophytes | |||
| Frymoyer et al. 1984 | Lifting | Osteophytes | There was no association between lifting and the spine outcomes evaluated. |
| Riihimaki et al. 1990 | Concrete reinforcement workers and house painters | Anterior and posterior spondylophytes | RevMan: Concrete workers had more spondylophytes at L1 L2 (OR = 3.68; 95% CI 1.20 to 11.27), L4 L5 spondylophytes (OR = 3.68; 95% CI 1.20 to 11.27) than painters. There was no difference for overall (OR = 1.68 95% CI 1.05 to 2.69), L2 L3 (OR = 1.84 95% CI 0.84 to 4.06), L3 L4 (OR = 1.97 95% CI 0.96 to 4.05) and L5S1 (OR = 1.43 95% CI 0.63 to 3.25). |
| Videman et al. 2006 | Job code (1–4), occupational driving, maximum weight lifted at work (kg) | Osteophytes | There was no association between occupational lifting and changes in osteophytes over time. |
| High Intensity Zones | |||
| Videman et al. 2006 | Job code (1–4), occupational driving, maximum weight lifted at work (kg) | High intensity zones (signal intensity) | There was no association between occupational lifting and changes in high intensity zones over time. |
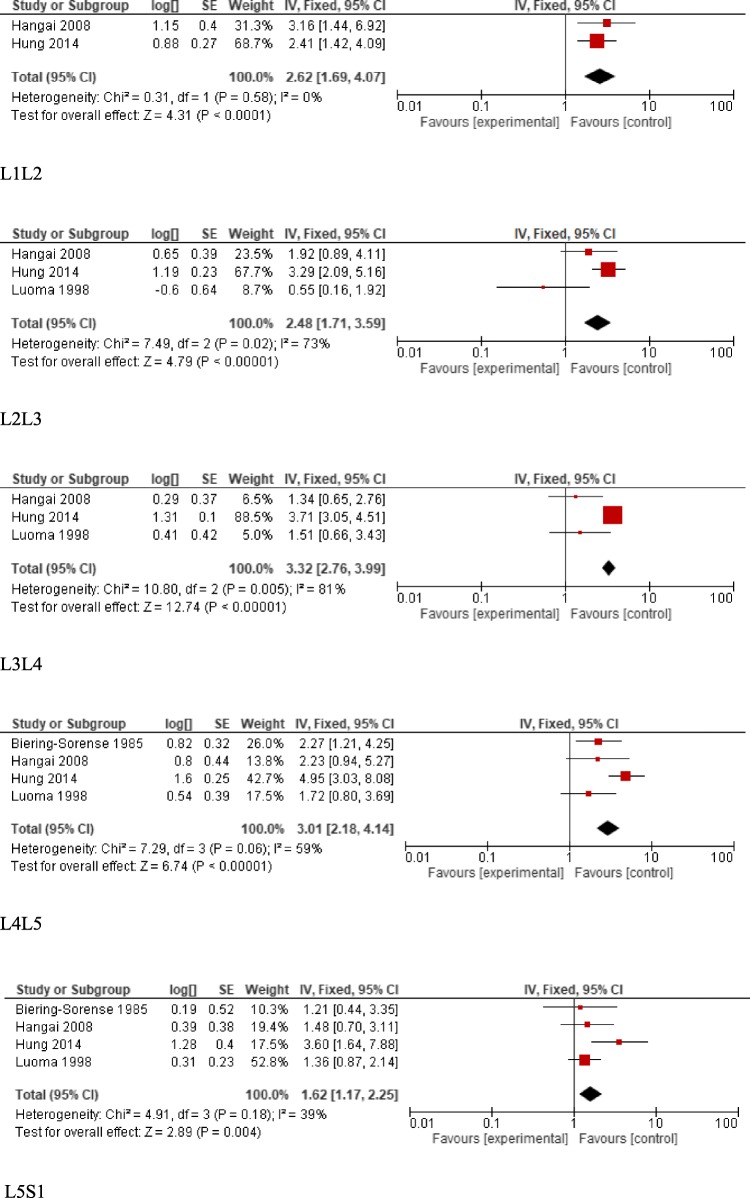
We were able to pool the results of 4 studies evaluating the association of disc degeneration with different types of occupational load for different spine levels [2–4, 133]. The results demonstrated that for all levels evaluated, including L1-S1, there was a statistically significant difference between loading groups with more degeneration associated with greater loading. Forest plost are presented in Fig. 2.
Fig. 2.
Disc degeneration (signal intensity) forest plots for each spinal level, L1-S1
Seven studies evaluated disc height [2, 125, 127, 128, 131, 133, 137]. Disc height can be measured on imaging using quantitative or qualitative measures and is a surrogate measure of disc degeneration. Of the seven studies evaluating disc height only one did not find a significant difference in disc height between groups [2]. The other six studies identified some type of influence of occupation load with disc height, with greater load being associated with narrower discs. Four studies identified an overall relationship of loading with disc height, without focusing on specific levels [125, 127, 128, 137] and the other studies found different levels to be significantly different [131, 133].
Seven studies evaluated a difference in the prevalence of disc bulge or herniation [3, 126, 128, 130, 133, 136, 137]. Disc bulges or herniations were primarily evaluated through visual observation of images. Of the seven studies, five identified a significant difference between loading groups [3, 128, 133, 136, 137]. Three studies evaluated the prevalence of all lumbar levels together [128, 136, 137] while two studies found difference for different levels, [3, 133] which varied between the studies. When calculated, odd ratios varied between 2.0 to 3.1.
Three studies evaluated Modic changes [126, 129, 135]. Modic changes represent lesions of the vertebral endplate that is adjacent to the bone marrow. Modic changes are often assessed qualitatively [135]. In this review only one study [135] identified a relationship of modic changes with occupation load. One study evaluated the prevalence of Schmorl’s nodes [132]. These are small protrusion of the disc into the vertebral body. The one study included in this review did not identify a relationship of nodes with occupational loading groups. Two studies evaluated the presence of other endplate abnormalities, [125, 137] with only one study identifying a difference between loading groups [137]. Finally, three studies evaluated the presence of osteophytes [125, 132, 137] with two studies identifying greater prevalence of osteophytes in those with greater load [125, 137].
Discussion
The results of this study suggest that there is moderate grade evidence of an association between occupational loading and disc degeneration in terms of signal intensity. There is low quality grade evidence between loading and disc height, with inconsistent results between levels. There is low quality evidence for an association of disc bulging with occupational loading, again with inconsistent results among spinal levels. There is low quality evidence of an association between occupational loading and osteophytes, Modic changes, Schmorl’s nodes and other endplate abnormalities.
The results do suggest that occupations with greater physical loading are associated with modestly greater spine degeneration although differences in loading conditions and outcomes between studies make it is difficult to draw strong, specific conclusions. This is especially true given that positive results were inconsistently found at different spinal levels and for different outcomes. Thus, it remains difficult to draw conclusions about which type of loading may negatively affect which type of degenerative or structural findings. Additionally, different imaging methods were used (e.g. MRI, CTScans and x-rays) and different methods to assess spine degeneration make it difficult to draw conclusions.
Limitations of the review are primarily related to the heterogeneity of the studies included. There was a wide range of types of occupational loading studied and a wide range of outcomes evaluated. Thus, although odds ratios were presented in the original manuscripts for most of the studies, it was not possible to pool the great majority of results and the findings of the review, therefore, were presented qualitatively. Finally, the poor methodological quality of some of the studies, with only a small portion assessing degeneration longitudinally, limits interpretation regarding the progression of spine degeneration.
Future research should focus on more longitudinal studies, where the development of spinal degeneration can be followed over time, with an adequate follow-up period to allow for structural changes to occur. Monozygotic twin studies should be considered, given the strength of twin study designs in minimizing possible confounding. Furthermore, individual loading exposures should be taken in consideration, especially as the activities and loading involved in any one profession can vary significantly. More specifically, the type and magnitude of loading should be depicted and evaluated in greater detail. Finally, with the advance of imaging techniques and measurement procedures, a wide variety of measures of spinal degeneration and pathology has resulted. Guidelines for measurement and better standardization of spine imaging phenotypes are needed to allow study comparisons and pooling of data to facilitate interpretation of the collective body of related research.
Conclusion
The results of this study suggest that there is moderate grade evidence of an association between occupational loading and disc degeneration in terms of signal intensity (disc degeneration). There is low or very low-quality grade evidence between loading and disc height, disc bulging, osteophytes, Modic changes, Schmorl’s nodes and other endplate abnormalities. While there seems to be a modest association between heavy occupational loading and spinal degenerative findings, the limitations of the results found in this review provide a weak foundation for practical applications and related health policies.
Supplementary information
Additional file 1. Search strategy section.
Acknowledgments
We would like to thank the research assistants that worked in this study and helped with data collection; Kenny Noguchi, Jennifer Nelson, Demian Carson and Christine Ha.
Abbreviations
- CI
Confidence Interval
- CTScans
Computerized Tomography scan
- GRADE
Grading of Recommendations, Assessment, Development and Evaluations
- LBP
Low Back Pain
- MRI
Magnetic Resonance Imaging
- OR
Odds ratio
- r
correlation
Authors’ contributions
LM conceptualized the study, conducted searchers, data extraction, data analysis, interpretation and write up of the manuscript. MCB conceptualized the study, conducted data analysis, interpretation and write up of the manuscript. All authors have read and approved the final version of this manuscript.
Funding
No funding.
Availability of data and materials
The sources of data used in this study are available within the manuscripts and its supplementary files.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests. Dr. Macedo is an associate editor of BMC Musculoskeletal Disorders.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12891-019-2835-2.
References
- 1.Videman T, Gibbons LE, Kaprio J, Battie MC. Challenging the cumulative injury model: positive effects of greater body mass on disc degeneration. Spine J. 2010;10(1):26–31. doi: 10.1016/j.spinee.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 2.Biering-Sorensen F, Hansen FR, Schroll M, Runeborg O. The relation of spinal x-ray to low-back pain and physical activity among 60-year-old men and women. Spine. 1985;10(5):445–451. doi: 10.1097/00007632-198506000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Luoma K, Riihimaki H, Raininko R, Luukkonen R, Lamminen A, Viikari-Juntura E. Lumbar disc degeneration in relation to occupation. Scand J Work Environ Health. 1998;24(5):358–366. doi: 10.5271/sjweh.356. [DOI] [PubMed] [Google Scholar]
- 4.Hangai M, Kaneoka K, Kuno S, Hinotsu S, Sakane M, Mamizuka N, Sakai S, Ochiai N. Factors associated with lumbar intervertebral disc degeneration in the elderly. Spine J. 2008;8(5):732–740. doi: 10.1016/j.spinee.2007.07.392. [DOI] [PubMed] [Google Scholar]
- 5.Savage RA, Whitehouse GH, Roberts N. The relationship between the magnetic resonance imaging appearance of the lumbar spine and low back pain, age and occupation in males. Eur Spine J. 1997;6(2):106–114. doi: 10.1007/BF01358742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Luoma K, Riihimaki H, Luukkonen R, Raininko R, Viikari-Juntura E, Lamminen A. Low back pain in relation to lumbar disc degeneration. Spine. 2000;25(4):487–492. doi: 10.1097/00007632-200002150-00016. [DOI] [PubMed] [Google Scholar]
- 7.Chou D, Samartzis D, Bellabarba C, Patel A, Luk KDK, Kisser JMS, Skelly AC. Degenerative magnetic resonance imaging changes in patients with chronic low Back pain a systematic review. Spine. 2011;36(21):S43–S53. doi: 10.1097/BRS.0b013e31822ef700. [DOI] [PubMed] [Google Scholar]
- 8.Hancock MJ, Maher CG, Petocz P, Lin CC, Steffens D, Luque-Suarez A, Magnussen JS. Risk factors for a recurrence of low back pain. Spine J. 2015;15:2360–2368. doi: 10.1016/j.spinee.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 9.The Newcastle-Ottowa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses (2011) Ottawa Hospital Research Institute.
- 10.Gibbons LE, Videman T, Battie MC. Isokinetic and psychophysical lifting strength, static back muscle endurance, and magnetic resonance imaging of the paraspinal muscles as predictors of low back pain in men. Scand J Rehabil Med. 1997;29(3):187–191. [PubMed] [Google Scholar]
- 11.Higgins JPT, Green S Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 [updated March 2011]. In: the Cochrane library. Chichester, UK: John Wiley & Sons, Ltd.
- 12.Riihimaki H, Wickstrom G, Hanninen K, Mattsson T, Waris P, Zitting A. Radiographically detectable lumbar degenerative changes as risk indicators of back pain. A cross-sectional epidemiologic study of concrete reinforcement workers and house painters. Scand J Work Environ Health. 1989;15(4):280–285. doi: 10.5271/sjweh.1855. [DOI] [PubMed] [Google Scholar]
- 13.Edeiken J, Karasick D. Use of radiography for screening employees for risk of low-back disability. J Occup Med. 1986;28(10):995–997. doi: 10.1097/00043764-198610000-00019. [DOI] [PubMed] [Google Scholar]
- 14.Campbell C, Muncer SJ. The causes of low back pain: a network analysis. Soc Sci Med. 2005;60(2):409–419. doi: 10.1016/j.socscimed.2004.05.013. [DOI] [PubMed] [Google Scholar]
- 15.Drerup B, Granitzka M, Assheuer J, Zerlett G. Assessment of disc injury in subjects exposed to long-term whole-body vibration. Eur Spine J. 1999;8(6):458–467. doi: 10.1007/s005860050205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frymoyer JW, Rosen JC, Clements J, Pope MH. Psychologic factors in low-back-pain disability. Clin Orthop. 1985;195:178–184. [PubMed] [Google Scholar]
- 17.Karahan A, Kav S, Abbasoglu A, Dogan N. Low back pain: prevalence and associated risk factors among hospital staff. J Adv Nurs. 2009;65(3):516–524. doi: 10.1111/j.1365-2648.2008.04905.x. [DOI] [PubMed] [Google Scholar]
- 18.Mazloum A, Nozad H, Kumashiro M. Occupational low back pain among workers in some small-sized factories in Ardabil, Iran. Ind Health. 2006;44(1):135–139. doi: 10.2486/indhealth.44.135. [DOI] [PubMed] [Google Scholar]
- 19.Mhaskar VA, Pai S. Does the occupational activity level affect the quality of life of patients treated with epidural steroid injections for lumbar disc herniations? Asian Spine J. 2012;6(2):131–135. doi: 10.4184/asj.2012.6.2.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Omokhodion FO, Sanya AO. Risk factors for low back pain among office workers in Ibadan, Southwest Nigeria. Occup Med. 2003;53(4):287–289. doi: 10.1093/occmed/kqg063. [DOI] [PubMed] [Google Scholar]
- 21.Palmer KT, Harris CE, Griffin MJ, Bennett J, Reading I, Sampson M, Coggon D. Case-control study of low-back pain referred for magnetic resonance imaging, with special focus on whole-body vibration. Scand J Work Environ Health. 2008;34(5):364–373. doi: 10.5271/sjweh.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seidler A, Bolm-Audorff U, Heiskel H, Henkel N, Roth-Kuver B, Kaiser U, Bickeboller R, Willingstorfer WJ, Beck W, Elsner G. The role of cumulative physical work load in lumbar spine disease: risk factors for lumbar osteochondrosis and spondylosis associated with chronic complaints. Occup Environ Med. 2001;58(11):735–746. doi: 10.1136/oem.58.11.735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seidler A, Bolm-Audorff U, Siol T, Henkel N, Fuchs C, Schug H, Leheta F, Marquardt G, Schmitt E, Ulrich PT, Beck W, Missalla A, Elsner G. Occupational risk factors for symptomatic lumbar disc herniation; a case-control study. Occup Environ Med. 2003;60(11):821–830. doi: 10.1136/oem.60.11.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Videman T, Battie MC, Gibbons LE, Maravilha K, Manninen H, Kaprio J. Associations between back pain history and lumbar MRI findings. Spine. 2003;28(6):582–588. doi: 10.1097/01.BRS.0000049905.44466.73. [DOI] [PubMed] [Google Scholar]
- 25.Dasinger LK, Krause N, Deegan LJ, Brand RJ, Rudolph L. Physical workplace factors and return to work after compensated low back injury: a disability phase-specific analysis. J Occup Environ Med. 2000;42(3):323–333. doi: 10.1097/00043764-200003000-00015. [DOI] [PubMed] [Google Scholar]
- 26.Zhang YG, Sun Z, Zhang Z, Liu J, Guo X. Risk factors for lumbar intervertebral disc herniation in Chinese population: a case-control study. Spine. 2009;34(25):E918–E922. doi: 10.1097/BRS.0b013e3181a3c2de. [DOI] [PubMed] [Google Scholar]
- 27.Alund M, Larsson SE, Lewin T. Work-related persistent neck impairment: a study on former steelworks grinders. Ergonomics. 1994;37(7):1253–1260. doi: 10.1080/00140139408964903. [DOI] [PubMed] [Google Scholar]
- 28.Schwarze S, Notbohm G, Hartung E, Dupuis H. Effects of whole-body vibrations on the lumbar spine. Arbeitsmed Sozialmed Umweltmed. 1998;33(10):429–442. [Google Scholar]
- 29.J-y J, S-l H, K-p L, Zhu J, J-l Z, Liao Y-h, Guan X, Wang X-r, Huang F. Epidemiological investigation of back pain and spondyloarthritis in Shougang resident communities. Chung Hua Nei Ko Tsa Chih. 2010;49(10):832–835. [PubMed] [Google Scholar]
- 30.Boos N, Semmer N, Elfering A, Schade V, Gal I, Zanetti M, Kissling R, Buchegger N, Hodler J, Main CJ. Natural history of individuals with asymptomatic disc abnormalities in magnetic resonance imaging: predictors of low back pain-related medical consultation and work incapacity. Spine. 2000;25(12):1484–1492. doi: 10.1097/00007632-200006150-00006. [DOI] [PubMed] [Google Scholar]
- 31.Dupuis H, Zerlett G. Whole -body vibration and disorders of the spine. Int Arch Occup Environ Health. 1987;59(4):323–336. doi: 10.1007/BF00405276. [DOI] [PubMed] [Google Scholar]
- 32.Schenk P, Laubli T, Hodler J, Klipstein A. Symptomatology of recurrent low back pain in nursing and administrative professions. Eur Spine J. 2007;16(11):1789–1798. doi: 10.1007/s00586-007-0346-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Virtanen IM, Karppinen J, Taimela S, Ott J, Barral S, Kaikkonen K, Heikkila O, Mutanen P, Noponen N, Mannikko M, Tervonen O, Natri A, Ala-Kokko L. Occupational and genetic risk factors associated with intervertebral disc disease. Spine. 2007;32(10):1129–1134. doi: 10.1097/01.brs.0000261473.03274.5c. [DOI] [PubMed] [Google Scholar]
- 34.Tertti M, Paajanen H, Kujala UM, Alanen A, Salmi TT, Kormano M. Disc degeneration in young gymnast. A magnetic resonance imaging study. Am J Sports Med. 1990;18(2):206–208. doi: 10.1177/036354659001800216. [DOI] [PubMed] [Google Scholar]
- 35.Tang CB, Cai RT, Yang L, Zhang GG, Li Y, Lu QF, Laurig W, Angerman K. An epidemiological study on the relationship between musculoskeletal disorders and work load. J Tongji Med Univ. 1995;15(1):59–64. doi: 10.1007/BF02887888. [DOI] [PubMed] [Google Scholar]
- 36.Leinonen V, Kankaanpaa M, Vanharanta H, Airaksinen O, Hanninen O. Back and neck extensor loading and back pain provocation in urban bus drivers with and without low back pain. Pathophysiology. 2005;12(4):249–255. doi: 10.1016/j.pathophys.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 37.Seidler A, Euler U, Bolm-Audorff U, Ellegast R, Grifka J, Haerting J, Jager M, Michaelis M, Kuss O. Physical workload and accelerated occurrence of lumbar spine diseases: risk and rate advancement periods in a German multicenter case-control study. Scand J Work Environ Health. 2011;37(1):30–36. doi: 10.5271/sjweh.3121. [DOI] [PubMed] [Google Scholar]
- 38.Bos E, Krol B, van der Star L, Groothoff J. Risk factors and musculoskeletal complaints in non-specialized nurses, IC nurses, operation room nurses, and X-ray technologists. Int Arch Occup Environ Health. 2007;80(3):198–206. doi: 10.1007/s00420-006-0121-8. [DOI] [PubMed] [Google Scholar]
- 39.Granhed H, Morelli B. Low back pain among retired wrestlers and heavyweight lifters. Am J Sports Med. 1988;16(5):530–533. doi: 10.1177/036354658801600517. [DOI] [PubMed] [Google Scholar]
- 40.Tiemessen IJH, Hulshof CTJ, Frings-Dresen MHW. Low back pain in drivers exposed to whole body vibration: analysis of a dose-response pattern. Occup Environ Med. 2008;65(10):667–675. doi: 10.1136/oem.2007.035147. [DOI] [PubMed] [Google Scholar]
- 41.Macdonald EB, Porter R, Hibbert C, Hart J. The relationship between spinal canal diameter and back pain in coal miners. Ultrasonic measurement as a screening test? J Occup Med. 1984;26(1):23–28. doi: 10.1097/00043764-198401000-00006. [DOI] [PubMed] [Google Scholar]
- 42.Aharony S, Milgrom C, Wolf T, Barzilay Y, Applbaum YH, Schindel Y, Finestone A, Liram N. Magnetic resonance imaging showed no signs of overuse or permanent injury to the lumbar sacral spine during a special forces training course. Spine J. 2008;8(4):578–583. doi: 10.1016/j.spinee.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 43.Landau DA, Chapnick L, Yoffe N, Azaria B, Goldstein L, Atar E. Cervical and lumbar MRI findings in aviators as a function of aircraft type. Aviat Space Environ Med. 2006;77(11):1158–1161. [PubMed] [Google Scholar]
- 44.Baumann F, Beck A. Work-related spinal damage in jet pilots due to extreme acceleration. Z Orthop Ihre Grenzgeb. 1975;113(4):645–648. [PubMed] [Google Scholar]
- 45.Kristen H, Lukeschitsch G, Ramach W. Investigation of the lumbar vertebral column in light-transport workers. Arbeitsmed Sozialmed Praventivmed. 1981;16(9):226–229. [Google Scholar]
- 46.Sharma A, Lancaster S, Bagade S, Hildebolt C. Early pattern of degenerative changes in individual components of intervertebral discs in stressed and nonstressed segments of lumbar spine: an in vivo magnetic resonance imaging study. Spine. 2014;39(13):1084–1090. doi: 10.1097/BRS.0000000000000265. [DOI] [PubMed] [Google Scholar]
- 47.Videman T, Battie MC, Gibbons LE, Manninen H, Gill K, Fisher LD, Koskenvuo M. Lifetime exercise and disk degeneration: an MRI study of monozygotic twins. Med Sci Sports Exerc. 1997;29(10):1350–1356. doi: 10.1097/00005768-199710000-00012. [DOI] [PubMed] [Google Scholar]
- 48.Kelsey JL. An epidemiological study of the relationship between occupations and acute herniated lumbar intervertebral discs. Int J Epidemiol. 1975;4(3):197–205. doi: 10.1093/ije/4.3.197. [DOI] [PubMed] [Google Scholar]
- 49.Auerbach JD, Weidner ZD, Milby AH, Diab M, Lonner BS. Musculoskeletal disorders among spine surgeons: results of a survey of the scoliosis research society membership. Spine. 2011;36(26):E1715–E1721. doi: 10.1097/BRS.0b013e31821cd140. [DOI] [PubMed] [Google Scholar]
- 50.Bishop MD, Horn ME, Lott DJ, Arpan I, George SZ. Magnitude of spinal muscle damage is not statistically associated with exercise-induced low back pain intensity. Spine J. 2011;11(12):1135–1142. doi: 10.1016/j.spinee.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Boos N, Rieder R, Schade V, Spratt KF, Semmer N, Aebi M. 1995 Volvo award in clinical sciences. The diagnostic accuracy of magnetic resonance imaging, work perception, and psychosocial factors in identifying symptomatic disc herniations. Spine. 1995;20(24):2613–2625. doi: 10.1097/00007632-199512150-00002. [DOI] [PubMed] [Google Scholar]
- 52.Liuke M, Solovieva S, Lamminen A, Luoma K, Leino-Arjas P, Luukkonen R, Riihimaki H. Disc degeneration of the lumbar spine in relation to overweight. Int J Obes. 2005;29(8):903–908. doi: 10.1038/sj.ijo.0802974. [DOI] [PubMed] [Google Scholar]
- 53.Mattila VM, Sillanpää P, Visuri T, Pihlajamäki H. Incidence and trends of low back pain hospitalisation during military service--an analysis of 387,070 Finnish young males. BMC Musculoskelet Disord. 2009;10:10. doi: 10.1186/1471-2474-10-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Carragee EJ, Alamin TF, Miller JL, Carragee JM. Discographic, MRI and psychosocial determinants of low back pain disability and remission: a prospective study in subjects with benign persistent back pain. Spine J. 2005;5(1):24–35. doi: 10.1016/j.spinee.2004.05.250. [DOI] [PubMed] [Google Scholar]
- 55.Simmons ED, Jr, Guntupalli M, Kowalski JM, Braun F, Seidel T. Familial predisposition for degenerative disc disease. A case-control study. Spine. 1996;21(13):1527–1529. doi: 10.1097/00007632-199607010-00007. [DOI] [PubMed] [Google Scholar]
- 56.Sambrook PN, MacGregor AJ, Spector TD. Genetic influences on cervical and lumbar disc degeneration: a magnetic resonance imaging study in twins. Arthritis Rheum. 1999;42(2):366–372. doi: 10.1002/1529-0131(199902)42:2<366::AID-ANR20>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 57.Karppinen J, Daavittila I, Solovieva S, Kuisma M, Taimela S, Natri A, Haapea M, Korpelainen R, Niinimaki J, Tervonen O, Ala-Kokko L, Mannikko M. Genetic factors are associated with modic changes in endplates of lumbar vertebral bodies. Spine. 2008;33(11):1236–1241. doi: 10.1097/BRS.0b013e318170fd0e. [DOI] [PubMed] [Google Scholar]
- 58.Livshits G, Popham M, Malkin I, Sambrook PN, MacGregor AJ, Spector T, Williams FMK. Lumbar disc degeneration and genetic factors are the main risk factors for low back pain in women: the UK twin spine study. Ann Rheum Dis. 2011;70(10):1740–1745. doi: 10.1136/ard.2010.137836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Aggrawal ND, Kaur R, Kumar S, Mathur DN. A study of changes in the spine in weight lifters and other athletes. Br J Sports Med. 1979;13(2):58–61. doi: 10.1136/bjsm.13.2.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pye SR, Reid DM, Adams JE, Silman AJ, O'Neill TW. Influence of weight, body mass index and lifestyle factors on radiographic features of lumbar disc degeneration. Ann Rheum Dis. 2007;66:426–427. doi: 10.1136/ard.2006.057166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cheung KMC, Karppinen J, Chan D, Ho DWH, Song Y-Q, Sham P, Cheah KSE, Leong JCY, Luk KDK. Prevalence and pattern of lumbar magnetic resonance imaging changes in a population study of one thousand forty-three individuals. Spine. 2009;34(9):934–940. doi: 10.1097/BRS.0b013e3181a01b3f. [DOI] [PubMed] [Google Scholar]
- 62.Suri P, Hunter DJ, Boyko EJ, Rainville J, Guermazi A, Katz JN. Physical activity and associations with computed tomography-detected lumbar zygapophyseal joint osteoarthritis. Spine J. 2015;15(1):42–49. doi: 10.1016/j.spinee.2014.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Franco JL (2008) Modic changes: "Age, si quid agis"... Eur Spine J 2006 Sep;15(9):1312-1319. Eur Spine J 17 (12):1766–1768. [DOI] [PMC free article] [PubMed]
- 64.Rainville J, Kim RS, Katz JN. A review of 1985 Volvo award winner in clinical science: objective assessment of spine function following industrial injury: a prospective study with comparison group and 1-year follow-up. Spine. 2007;32(18):2031–2034. doi: 10.1097/BRS.0b013e318133fc92. [DOI] [PubMed] [Google Scholar]
- 65.Williams FM, Sambrook PN. Neck and back pain and intervertebral disc degeneration: role of occupational factors. Baillieres Best Pract Res Clin Rheumatol. 2011;25(1):69–79. doi: 10.1016/j.berh.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 66.Chaffin DB. Manual materials handling: the cause of over-exertion injury and illness in industry. J Environ Pathol Toxicol. 1979;2(5):31–66. [PubMed] [Google Scholar]
- 67.Harley WJ. Lost time back injuries: their rrelationship to heavy work and preplacement back x-rays. J Occup Med. 1972;14(8):611–614. [PubMed] [Google Scholar]
- 68.Borenstein DG, Burton JR. Lumbar spine disease in the elderly. J Am Geriatr Soc. 1993;41(2):167–175. doi: 10.1111/j.1532-5415.1993.tb02053.x. [DOI] [PubMed] [Google Scholar]
- 69.Williams FMK, Popham M, Livshits G, Sambrook PN, Spector TD, MacGregor AJ. A response to Videman et al., "challenging the cumulative injury model: positive effects of greater body mass on disc degeneration". Spine J. 2010;10(6):571–572. doi: 10.1016/j.spinee.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 70.Videman T, Nurminen M, Troup JD. 1990 Volvo award in clinical sciences. Lumbar spinal pathology in cadaveric material in relation to history of back pain, occupation, and physical loading. Spine. 1990;15(8):728–740. [PubMed] [Google Scholar]
- 71.Arun R, Freeman BJ, Scammell BE, McNally DS, Cox E, Gowland P. 2009 ISSLS prize winner: what influence does sustained mechanical load have on diffusion in the human intervertebral disc?: an in vivo study using serial postcontrast magnetic resonance imaging. Spine. 2009;34(21):2324–2337. doi: 10.1097/BRS.0b013e3181b4df92. [DOI] [PubMed] [Google Scholar]
- 72.Belfi LM, Ortiz AO, Katz DS. Computed tomography evaluation of spondylolysis and spondylolisthesis in asymptomatic patients. Spine. 2006;31(24):E907–E910. doi: 10.1097/01.brs.0000245947.31473.0a. [DOI] [PubMed] [Google Scholar]
- 73.Boos N, Rieder R, Schade V, Spratt KF, Semmer N, Aebi M. The diagnostic accuracy of magnetic resonance imaging, work perception, and psychosocial factors in identifying symptomatic disc herniations. Spine. 1995;20(24):2613–2625. doi: 10.1097/00007632-199512150-00002. [DOI] [PubMed] [Google Scholar]
- 74.Farfan HF, Cossette JW, Robertson GH, Wells RV, Kraus H. The effects of torsion on the lumbar intervertebral joints: the role of torsion in the production of disc degeneration. J Bone Joint Surg Am. 1970;52(3):468–497. doi: 10.2106/00004623-197052030-00006. [DOI] [PubMed] [Google Scholar]
- 75.Gunning JL, Callaghan JP, McGill SM. Spinal posture and prior loading history modulate compressive strength and type of failure in the spine: a biomechanical study using a porcine cervical spine model. Clin Biomech. 2001;16(6):471–480. doi: 10.1016/S0268-0033(01)00032-8. [DOI] [PubMed] [Google Scholar]
- 76.Olsewski JM, Schendel MJ, Wallace LJ, Ogilvie JW, Gundry CR. Magnetic resonance imaging and biological changes in injured intervertebral discs under normal and increased mechanical demands. Spine. 1996;21(17):1945–1951. doi: 10.1097/00007632-199609010-00001. [DOI] [PubMed] [Google Scholar]
- 77.Bible JE, Choemprayong S, O'Neill K, Devin CJ, Spengler DM. Whole-body vibration. Is there a causal relationship to specific imaging findings of the spine? Spine. 2012;37(21):E1348–E1355. doi: 10.1097/BRS.0b013e3182697a47. [DOI] [PubMed] [Google Scholar]
- 78.Gooyers CE, McMillan RD, Howarth SJ, Callaghan JP. The impact of posture and prolonged cyclic compressive loading on vertebral joint mechanics. Spine. 2012;37(17):E1023–E1029. doi: 10.1097/BRS.0b013e318256f9e6. [DOI] [PubMed] [Google Scholar]
- 79.Stemper BD, Baisden J, Yogamandan N, Pintar FA, Tarima S, Xiang Q, Paskoff GR, Shender BS. Lumbar spine injury tolerance during high-rate axial loading. Spine J. 2013;13:13S–14S. doi: 10.1016/j.spinee.2013.07.061. [DOI] [Google Scholar]
- 80.Brinckmann P, Frobin W, Biggemann M, Hilweg D, Seidel S, Burton K, Tillotson M, Sandover J, Atha J, Quinnell R. Quantification of overload injuries to thoracolumbar vertebrae and discs in persons exposed to heavy physical exertions or vibration at the work-place. Clin Biomech. 1994;9(SUPPL. 1):S1–S83. doi: 10.1016/0268-0033(94)90074-4. [DOI] [PubMed] [Google Scholar]
- 81.Arora M, Paoloni JA, Kandwal P, Diwan AD. Are fast-bowlers prone to back injuries? Prevalence of lumbar spine injuries in fast-bowlers: review of MRI-based studies. Asian J Sports Med. 2014;5(4):e24291. doi: 10.5812/asjsm.24291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Seidler A, Bergmann A, Jager M, Ellegast R, Ditchen D, Elsner G, Grifka J, Haerting J, Hofmann F, Linhardt O, Luttmann A, Michaelis M, Petereit-Haack G, Schumann B, Bolm-Audorff U. Cumulative occupational lumbar load and lumbar disc disease--results of a German multi-center case-control study (EPILIFT) BMC Musculoskelet Disord. 2009;10:48. doi: 10.1186/1471-2474-10-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sun ZM, Ling M, Chang YH, Liu ZZ, Xu HH, Gong LQ, Liu J, Zhang YG. Case-control study of the risk factors of lumbar intervertebral disc herniation in 5 northern provinces of China. Nan Fang Yi Ke Da Xue Xue Bao. 2010;30(11):2488–2491. [PubMed] [Google Scholar]
- 84.Nienhaus A, Elsner G, Beck W. Degenerative discopathies of occupational origin in the region of the lumbar spine. Arbeitsmed Sozialmed Praventivmed. 1992;27(10):415–422. [Google Scholar]
- 85.Liu S, Zhang H, Liu X, Shen Y, Dai W, Ju Z, Ma J, Xu W. Study on vertebral degenerations of coal miners with low back pain by means of computerized tomography. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2002;20(1):10–12. [PubMed] [Google Scholar]
- 86.Bergmann A, Meisel HJ, Bolm-Audorff U, Ditchen D, Ellegast R, Elsner G, Grifka J, Haerting J, Hoffmann F, Jager M, Linhardt O, Luttmann A, Michaelis M, Petereit-Haack G, Schumann B, Seidler A (2010) Physical workload - a relevant factor for developing lumbar disc diseases (German spine study epilift). Spine conference (journal article):38th.
- 87.Mariconda M, Galasso O, Imbimbo L, Lotti G, Milano C. Relationship between alterations of the lumbar spine, visualized with magnetic resonance imaging, and occupational variables. Eur Spine J. 2007;16(2):255–266. doi: 10.1007/s00586-005-0036-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Vanharanta H, Heliovaara M, Korpi J, Troup JD. Occupation, work load and the size and shape of lumbar vertebral canals. Scand J Work Environ Health. 1987;13(2):146–149. doi: 10.5271/sjweh.2076. [DOI] [PubMed] [Google Scholar]
- 89.Shambrook J, McNee P, Harris E, Kim M, Sampson M, Palmer K, Coggan D. Clinical presentation of low back pain and association with risk factors according to findings on magnetic resonance imaging. Pain. 2011;152:1659–1665. doi: 10.1016/j.pain.2011.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Saberi H, Rahimi L, Jahani L. A comparative MRI study of upper and lower lumbar motion segments in patients with low back pain. J Spinal Disord Tech. 2009;22(7):507–510. doi: 10.1097/BSD.0b013e3181927051. [DOI] [PubMed] [Google Scholar]
- 91.Palmer KT, Griffin M, Ntani G, Shambrook J, McNee P, Sampson M, Harris EC, Coggon D. Professional driving and prolapsed lumbar intervertebral disc diagnosed by magnetic resonance imaging: a case-control study. Scand J Work Environ Health. 2012;38(6):577–581. doi: 10.5271/sjweh.3273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Rossi A, Marino G, Barbieri L, Borrelli A, Onofri C, Rolli M, Baldi R. Backache from exertion in health personnel of the Istituti Ortopedici Rizzoli in Bologna. A case-control study of the injury phenomenon in the 10-year period of 1987-1996. Epidemiol Prev. 1999;23(2):98–104. [PubMed] [Google Scholar]
- 93.Bridger RS, Groom MR, Jones H, Pethybridge RJ, Pullinger N. Task and postural factors are related to back pain in helicopter pilots. Aviat Space Environ Med. 2002;73(8):805–811. [PubMed] [Google Scholar]
- 94.Nohejl J, Dostal C, Faberova R, Malecek J, Roth Z, Trnavsky K. Preliminary results of an epidemiological study of back pain in a Prague population. Czech Med. 1987;10(2):117–124. [PubMed] [Google Scholar]
- 95.Birlik G. Occupational exposure to whole body vibration-train drivers. Ind Health. 2009;47(1):5–10. doi: 10.2486/indhealth.47.5. [DOI] [PubMed] [Google Scholar]
- 96.Elsner G, Nienhaus A, Beck W. Occupationally-induced degenerative discopathies in the area of the lumbar spine. Soz Praventivmed. 1997;42(3):144–154. doi: 10.1007/BF01300565. [DOI] [PubMed] [Google Scholar]
- 97.Hamalainen O, Vanharanta H, Kuusela T. Degeneration of cervical intervertebral disks in fighter pilots frequently exposed to high +Gz forces. Aviat Space Environ Med. 1993;64(8):692–696. [PubMed] [Google Scholar]
- 98.Joosab M, Torode M, Rao PV. Preliminary findings on the effect of load-carrying to the structural integrity of the cervical spine. Surg Radiol Anat. 1994;16(4):393–398. doi: 10.1007/BF01627659. [DOI] [PubMed] [Google Scholar]
- 99.Kartal A, Yildiran I, Senkoylu A, Korkusuz F. Soccer causes degenerative changes in the cervical spine. Eur Spine J. 2004;13(1):76–82. doi: 10.1007/s00586-003-0623-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Danckwerth F, Castro WHM, Assheuer J. Morphological changes at the cervical spine among professional string instrument players? Zentralbl Arbeitsmed Arbeitsschutz Ergonomie. 1996;46(10):362–369. [Google Scholar]
- 101.Wang Y, Owoc JS, Boyd SK, Videman T, Battie MC. Occupational loading may not affect the association between vertebral trabecular bone and intervertebral disc narrowing. Bone. 2013;57(2):375–376. doi: 10.1016/j.bone.2013.09.005. [DOI] [PubMed] [Google Scholar]
- 102.Bakhtiar CS, Suneetha S, Vijay R. Conservative approaches benefit occupation-related backaches in milk-vendors and goldsmiths. Indian J Occup Environ Med. 2002;6(4):186–188. [Google Scholar]
- 103.Kuisma M, Karppinen J, Niinimaki J, Ojala R, Haapea M, Heliovaara M, Korpelainen R, Taimela S, Natri A, Tervonen O. Modic changes in endplates of lumbar vertebral bodies: prevalence and association with low back and sciatic pain among middle-aged male workers. Spine. 2007;32(10):1116–1122. doi: 10.1097/01.brs.0000261561.12944.ff. [DOI] [PubMed] [Google Scholar]
- 104.Battie MC, Videman T, Levalahti E, Gill K, Kaprio J. Heritability of low back pain and the role of disc degeneration. Pain. 2007;131:272–280. doi: 10.1016/j.pain.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 105.Videman T, Battie MC, Parent E, Gibbons LE, Vainio P, Kaprio J. Progression and determinants of quantitative magnetic resonance imaging measures of lumbar disc degeneration: a five-year follow-up of adult male monozygotic twins. Spine. 2008;33(13):1484–1490. doi: 10.1097/BRS.0b013e3181753bb1. [DOI] [PubMed] [Google Scholar]
- 106.Hendriksen IJ, Holewijn M. Degenerative changes of the spine of fighter pilots of the Royal Netherlands air Force (RNLAF) Aviat Space Environ Med. 1999;70(11):1057–1063. [PubMed] [Google Scholar]
- 107.Kuisma M, Karppinen J, Haapea M, Niinimaki J, Ojala R, Heliovaara M, Korpelainen R, Kaikkonen K, Taimela S, Natri A, Tervonen O. Are the determinants of vertebral endplate changes and severe disc degeneration in the lumbar spine the same? A magnetic resonance imaging study in middle-aged male workers. BMC Musculoskelet Disord. 2008;9:51. doi: 10.1186/1471-2474-9-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kumar A, Varghese M, Mohan D, Mahajan P, Gulati P, Kale S. Effect of whole-body vibration on the low back. A study of tractor-driving farmers in North India. Spine. 1999;24(23):2506–2515. doi: 10.1097/00007632-199912010-00013. [DOI] [PubMed] [Google Scholar]
- 109.Videman T, Simonen R, Usenius J, Osterman K, Battie M. The long-term effects of rally driving on spinal pathology. Clin Biomech. 2000;15(2):83–86. doi: 10.1016/S0268-0033(99)00047-9. [DOI] [PubMed] [Google Scholar]
- 110.Sovelius R, Salonen O, Lamminen A, Huhtala H, Hamalainen O. Spinal MRI in fighter pilots and controls: a 13-year longitudinal study. Aviat Space Environ Med. 2008;79(7):685–688. doi: 10.3357/ASEM.2249.2008. [DOI] [PubMed] [Google Scholar]
- 111.Battie MC, Videman T, Gibbons LE, Manninen H, Gill K, Pope M, Kaprio J. Occupational driving and lumbar disc degeneration: a case-control study. Lancet. 2002;360(9343):1369–1374. doi: 10.1016/S0140-6736(02)11399-7. [DOI] [PubMed] [Google Scholar]
- 112.Aydog ST, Turbedar E, Demirel AH, Tetik O, Akin A, Doral MN. Cervical and lumbar spinal changes diagnosed in four-view radiographs of 732 military pilots. Aviat Space Environ Med. 2004;75(2):154–157. [PubMed] [Google Scholar]
- 113.Byeon JH, Kim JW, Jeong HJ, Sim YS, Kim DK, Choi JK, Im HJ, Kim GC. Degenerative changes of spine in helicopter pilots. Ann Rehabil Med. 2013;37(5):706–712. doi: 10.5535/arm.2013.37.5.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Fischer V, Witt AN, Troeger C. Vibration-induced injuries to the vertebral column of helicopter pilots. Arbeitsmed Sozialmed Praventivmed. 1980;15(7):161–163. [Google Scholar]
- 115.Christ W, Dupuis H (1968) Studies on the possibility of physical damage to the spinal area in tractor operators. II. Report on the 2d mass examination of 137 young farmers. Med welt 37 (journal article):1967-1972. [PubMed]
- 116.Kaneoka K, Shimizu K, Hangai M, Okuwaki T, Mamizuka N, Sakane M, Ochiai N. Lumbar intervertebral disk degeneration in elite competitive swimmers - a case control study. Am J Sports Med. 2007;35(8):1341–1345. doi: 10.1177/0363546507300259. [DOI] [PubMed] [Google Scholar]
- 117.Baranto A, Hellstrom M, Cederlund CG, Nyman R, Sward L. Back pain and MRI changes in the thoraco-lumbar spine of top athletes in four different sports: a 15-year follow-up study. Knee Surg Sports Traumatol Arthrosc. 2009;17(9):1125–1134. doi: 10.1007/s00167-009-0767-3. [DOI] [PubMed] [Google Scholar]
- 118.Ichikawa N, Ohara Y, Morishita T, Taniguichi Y, Koshikawa A, Matsukura N. An aetiological study on spondylolysis from a biomechanical aspect. Br J Sports Med. 1982;16(3):135–141. doi: 10.1136/bjsm.16.3.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Videman T, Sarna S, Battie MC, Koskinen S, Gill K, Paananen H, Gibbons L. The long-term effects of physical loading and exercise lifestyles on back-related symptoms, disability, and spinal pathology among men. Spine. 1995;20(6):699–709. doi: 10.1097/00007632-199503150-00011. [DOI] [PubMed] [Google Scholar]
- 120.Rachbauer F, Sterzinger W, Eibl G. Radiographic abnormalities in the thoracolumbar spine of young elite skiers. Am J Sports Med. 2001;29(4):446–449. doi: 10.1177/03635465010290041101. [DOI] [PubMed] [Google Scholar]
- 121.Ozturk B, Gunduz OH, Ozoran K, Bostanoglu S. Effect of continuous lumbar traction on the size of herniated disc material in lumbar disc herniation. Rheumatol Int. 2006;26(7):622–626. doi: 10.1007/s00296-005-0035-x. [DOI] [PubMed] [Google Scholar]
- 122.Nagashima M, Abe H, Amaya K, Matsumoto H, Yanaihara H, Nishiwaki Y, Toyama Y, Matsumoto M. Risk factors for lumbar disc degeneration in high school American football players a prospective 2-year follow-up study. Am J Sports Med. 2013;41(9):2059–2064. doi: 10.1177/0363546513495173. [DOI] [PubMed] [Google Scholar]
- 123.Kraft CN, Pennekamp PH, Becker U, Young M, Diedrich O, Luering C, von Falkenhausen M. Magnetic resonance imaging findings of the lumbar spine in elite horseback riders correlations with Back pain, body mass index, trunk/leg-length coefficient, and riding discipline. Am J Sports Med. 2009;37(11):2205–2213. doi: 10.1177/0363546509336927. [DOI] [PubMed] [Google Scholar]
- 124.Vadala G, Russo F, Battisti S, Stellato L, Martina F, Del Vescovo R, Giacalone A, Borthakur A, Zobel BB, Denaro V. Early intervertebral disc degeneration changes in asymptomatic weightlifters assessed by t1p-magnetic resonance imaging. Spine. 2014;39(22):1881–1886. doi: 10.1097/BRS.0000000000000554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Riihimaki H, Mattsson T, Zitting A, Wickstrom G, Hanninen K, Waris P. Radiographically detectable degenerative changes of the lumbar spine among concrete reinforcement workers and house painters. Spine. 1990;15(2):114–119. doi: 10.1097/00007632-199002000-00013. [DOI] [PubMed] [Google Scholar]
- 126.Schenk P, Laubli T, Hodler J, Klipstein A. Magnetic resonance imaging of the lumbar spine: findings in female subjects from administrative and nursing professions. Spine. 2006;31(23):2701–2706. doi: 10.1097/01.brs.0000244570.36954.17. [DOI] [PubMed] [Google Scholar]
- 127.Videman T, Levalahti E, Battie MC. The effects of anthropometrics, lifting strength, and physical activities in disc degeneration. Spine. 2007;32(13):1406–1413. doi: 10.1097/BRS.0b013e31806011fa. [DOI] [PubMed] [Google Scholar]
- 128.Battie MC, Videman T, Gibbons LE, Fisher LD, Manninen H, Gill K (1995) 1995 Volvo award in clinical sciences. Determinants of lumbar disc degeneration. A study relating lifetime exposures and magnetic resonance imaging findings in identical twins Spine 20 (24):2601–2612. [PubMed]
- 129.Elfering A, Semmer N, Birkhofer D, Zanetti M, Hodler J, Boos N. Risk factors for lumbar disc degeneration: a 5-year prospective MRI study in asymptomatic individuals. Spine. 2002;27(2):125–134. doi: 10.1097/00007632-200201150-00002. [DOI] [PubMed] [Google Scholar]
- 130.Munoz-Gomez J, Bernades-Bernat E, Valenzuela-Castano A, Duro-Pujol JC. Clinico-radiological correlation of the dorsal spine in a population of workers. Rev Rhum Mal Osteoartic. 1980;47(3):175–180. [PubMed] [Google Scholar]
- 131.Brinckmann P, Frobin W, Biggeman M, Tillotson M, Burton K. Quantification of overload injuries to thoracolumbar vertebrae and discs in persons exposed to heavy physical exertions or vibration at the workplace. Part II. Occurrence and magnitude of overload injury in exposed cohorts. Clin Biomech. 1998;13(SUPPL. 2):S36. doi: 10.1016/s0268-0033(98)00050-3. [DOI] [PubMed] [Google Scholar]
- 132.Frymoyer JW, Newberg A, Pope MH, Wilder DG, Clements J, MacPherson B. Spine radiographs in patients with low-back pain. An epidemiological study in men. J Bone Joint Surg Am. 1984;66(7):1048–1055. doi: 10.2106/00004623-198466070-00011. [DOI] [PubMed] [Google Scholar]
- 133.Hung YJ, Shih TT, Chen BB, Hwang YH, Ma LP, Huang WC, Liou SH, Ho IK, Guo YL. The dose-response relationship between cumulative lifting load and lumbar disk degeneration based on magnetic resonance imaging findings. Phys Ther. 2014;94(11):1582–1593. doi: 10.2522/ptj.20130095. [DOI] [PubMed] [Google Scholar]
- 134.Hartwig E, Hoellen I, Liener U, Kramer M, Wickstroem M, Kinzl L. Occupational disease 2108. Degeneration pattern in magnetic resonance tomography of the lumbar spine in patient with differential weight-bearing activity. Unfallchirurg. 1997;100(11):888–894. doi: 10.1007/s001130050209. [DOI] [PubMed] [Google Scholar]
- 135.Han C, Kuang MJ, Ma JX, Ma XL. Prevalence of Modic changes in the lumbar vertebrae and their associations with workload, smoking and weight in northern China. Sci Rep. 2017;7:46341. doi: 10.1038/srep46341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Arevalo G, Varela C, Gijon L, Rosas ML, Arevalo F. Modifiable risk factors and lumbar disc herniation: results of a case control study in 652 patients. Ann Phys Rehabil Med. 2014;57:e197. doi: 10.1016/j.rehab.2014.03.718. [DOI] [Google Scholar]
- 137.Videman T, Battie MC, Ripatti S, Gill K, Manninen H, Kaprio J. Determinants of the progression in lumbar degeneration: a 5-year follow-up study of adult male monozygotic twins. Spine. 2006;31(6):671–678. doi: 10.1097/01.brs.0000202558.86309.ea. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Search strategy section.
Data Availability Statement
The sources of data used in this study are available within the manuscripts and its supplementary files.