Abstract
With the deepening of the researches on uric acid, especially in the study of metabolic diseases, uric acid has been found to be closely related to obesity, metabolic syndrome, nonalcoholic fatty liver disease, diabetes, and other metabolic diseases. Uric acid causes a series of pathophysiological changes through inflammation, oxidative stress, vascular endothelial injury, and so on and thus subsequently promotes the occurrence and development of diseases. This review confirmed the positive correlation between uric acid and diabetes mellitus and its chronic complications through the pathogenesis and clinical studies aspects.
1. Introduction
In recent years, human intake of foods such as those with the umami flavor (rich in purines), high added sugar (sucrose), and high fructose corn syrup have increased dramatically [1]. Fructose is the main component of added sugar. Unlike other sugars, fructose can cause mitochondrial oxidative stress [2, 3] and inhibits AMPK [4], and the subsequent intracellular ATP depletion [5] and nucleotide turnover lead to a significant increase in serum uric acid [6]. In addition to causing gout, many studies have shown that hyperuricemia is also closely related to cardiovascular diseases, metabolic syndrome, insulin resistance, and diabetes [7, 8]. However, its function is a matter of debate [9]. Here, we reviewed the effects of hyperuricemia on diabetes and its complications and concluded that high levels of uric acid is closely related to diabetes and its chronic complications.
1.1. Uric Acid Formation
In the human body, uric acid is the ultimate product of purine metabolism (Figure 1 [10]). It is generated in the liver. Purine nucleotides decompose to hypoxanthine and guanine, some of which can be recycled and phosphorylated into hypoxanthine nucleotides, while the remaining part is metabolized by xanthine dehydrogenase/oxidase (XDH/XO) enzymatic reaction to the terminal product uric acid. XDH/XO is mainly expressed in the parenchymal cells of the liver and small intestine. XDH has low reactivity and can be converted to XO. Uric acid production primarily depends on the amount of substrate and the activity of XO [11]. In the end, XDH/XO promotes the final steps in purine metabolism which convert hypoxanthine to xanthine and xanthine to UA [11]. The kidney also plays an important role in the regulation of blood uric acid levels. The circulating uric acid is easily filtered from the glomeruli into the renal tubule. About 90% of filtered UA is reabsorbed by the middle of the proximal convoluted tubule mainly by urate transporter 1 (URAT1) and glucose transporter 9 (GLUT9) [12], and the remaining excreted 10% is responsible for 60–70% of total body uric acid excretion [13, 14]. A small amount of uric acid secreted in the intestine is responsible for 30–40% [14]. The production and excretion rate of uric acid is relatively constant in healthy people. Changes in the uric acid content in body fluids can reflect the state of metabolism, immunity, and other functions of the human body. If the body produces too much uric acid or the excretion mechanism is degraded, the body will retain excessive uric acid. Hyperuricemia was defined as the circulating uric acid levels of more than 5.7 mg/dl for women and 7.0 mg/dl for men [15]. When the blood uric acid concentration exceeds the norm, the human body fluid becomes acidic, which affects the normal function of the human cells, subsequently leading to metabolic disease in the long term [16–18].
Figure 1.
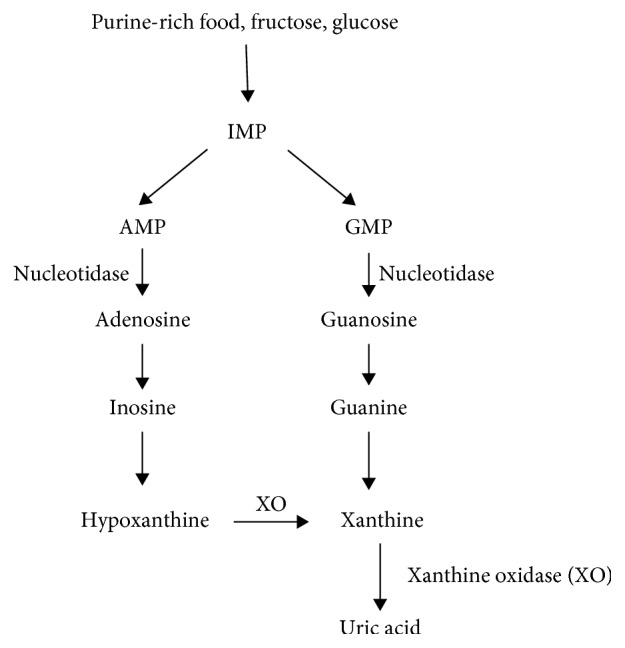
Process of purine metabolism in humans.
2. Pathological Mechanism of Uric Acid on Diabetes and Its Chronic Complications
2.1. Uric Acid and Diabetes
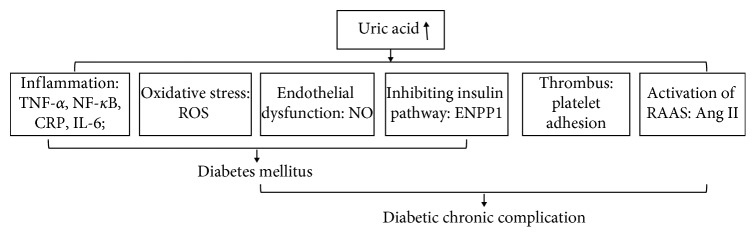
At present, many studies have shown that the relevant pathological mechanisms include some aspects as follows (Figure 2):
Inflammation. Increased uric acid levels in the blood promoted the expression of interleukin-1β (IL-1β), interleukin-6 (IL-6), tumor necrosis factor-α (TNF-α) [19], and CRP production [20]. In animal studies, the activation of inflammation induced by UA decreases insulin sensitivity in mice [21], and infusion of UA into mice can increase TNF-α levels and activate the classical inflammatory pathway [22]. In human studies, serum UA was positively associated with TNF-α, interleukin-6 and C-reactive protein in healthy people [23].
Oxidative Stress. Excessive uric acid will lead to an increase in reactive oxygen species (ROS) production, which leads to inflammation and dysfunction in the vessel [24]. UA is a powerful antioxidant that can remove superoxide and hydroxyl radicals in plasma, and UA has prooxidant effects in vascular tissue by increasing ROS production, such as H2O2 [24]. UA-mediated oxidative stress-induced lipid peroxidation, DNA damage, and activation of inflammatory factors finally lead to cellular damage [24]. Oxidative stress also can affect the expression of insulin gene, causing a decrease in insulin secretion [25].
Endothelial Dysfunction. Endothelial dysfunction is characterized by deficiencies in the synthesis and/or bioavailability of endothelium-derived NO [26]. In addition, UA reduces endothelial NO bioavailability in humans [27]. Uric acid inhibits proliferation and migration of endothelial cells and NO secretion [20]. UA can react with NO to form 6-aminouracil, UA-dependent ROS reacts with NO to form peroxynitrite, and UA can hold back L-arginine uptake and stimulate L-arginine degradation [6]. As a result of the effects of hyperglycemia and neurohormonal activation, UA levels are independently associated with endothelial dysfunction in animals and humans, thereby promoting hypertension [28].
Inhibiting Insulin Pathway. UA directly inhibits the trigger of insulin signaling pathway by an ectonucleotide pyrophosphatase/phosphodiesterase 1 (ENPP1) recruitment at the receptor level [29].
Figure 2.
Metabolism of uric acid leading to diabetes mellitus and its chronic complication.
All factors interference with glucose homeostasis and insulin sensitivity promotes the development of diabetes [30–32].
2.2. Uric Acid and Diabetic Chronic Complications
The aforementioned changes to diabetes are also directly related to the metabolic disorder: desulfation of glycosaminoglycans (GAGs) and formation of advanced glycation end products (AGE) and receptors (RAGE) [33]. It is widely believed that polyol bypass, protein kinase C, hexosamine activation, advanced glycosylation products (AGEs), increased hyperglycemia-induced mitochondria production of reactive oxygen species (ROS), inflammation, and endothelial dysfunction are the common pathogenic characteristics of chronic complications of diabetes mellitus [10,33–39], which mainly include macroangiopathy, microangiopathy, and neuropathy. Two other mechanisms are associated with chronic complications as follows (Figure 2):
Activation of RAAS. Uric acid can lead to the activation of the renin-angiotensin-aldosterone System (RAAS), through increasing the production of juxtaglomerular renin [40]. UA-induced ROS stimulated the increase of plasma angiotensin II which induced aldosterone release, leading to activation of RAAS [24, 41]. RAAS activation induced afferent renal arteriolopathy and tubulointerstitial fibrosis in rodent models [42]. In diabetes, RAAS activation causes a range of pathological changes including vascular dysfunction, high intraglomerular pressure, inflammation, and so on, leading to cardiovascular and renal complications [43].
Thrombus. Uric acid seems to trigger platelet adhesion and aggregation, thus favoring vascular thrombosis [44].
3. Epidemiology Studies
3.1. Uric Acid and Diabetes
The relationship between uric acid and diabetes has gradually become a hot topic of research, but controversy still exists. On the one hand, some study reported uric acid was not associated with diabetes. For example, Sluijs et al. [45] used a genetic score of 24 uric acid-related sites for Mendelian randomization studies, in the European prospective survey data—Cancer and Nutrition (EPIC) study, which was an interactive case-cohort study of vast number of subjects from eight European countries. In EPIC, after a mean of 10 years of follow-up, the results suggested that hyperuricemia was not salient associated with a higher risk of diabetes after adjusting for interference factors when their participant number was increased from 10,576 to 41,508. Similarly, a large prospective cohort study was performed by Li [46] who followed up 4412 nondiabetic patients for 4.7 years to study urate changes in glucose metabolism. They found the uric acid concentration was not related to an increased risk of type 2 diabetes mellitus (T2DM).
On the opposite hand, more clinical trials demonstrated uric acid was significantly associated with diabetes. For example, Bombelli et al. [47, 48] randomly selected 3,200 northern Italian residents between the ages of 25 and 74 and found that increased uric acid resulted in an increased risk of impaired fasting glucose (IFG), and people with higher median UA levels may also develop metabolic syndrome and diabetes. In women, serum uric acid (SUA) levels in the normal range were associated with an increased risk of new-onset diabetes compared with women with low-normal values [49]. Older adults with high levels of uric acid (6.0 mg/dl for men and 5.5 mg/dl for women) were more susceptible to metabolic syndrome and T2DM, especially in the 75–84 years age group [50]. Serum UA was an important predictor of risk of metabolic syndrome, diabetes, and hypertension in adult males [51]. However, the relationship between blood UA and decreased insulin sensitivity in patients with type 1 diabetes mellitus is weaker than in healthy subjects [52].
Through reading a large number of literature and studies, we believe that uric acid is closely related to diabetes. Poor lipid metabolism in individuals with higher UA levels may lead to increased fasting and postprandial insulin levels, high-sensitivity C-reactive protein, hepatic insulin resistance index, and decreased glomerular filtration rate and skeletal muscle insulin sensitivity; high levels of SUA may impair liver insulin sensitivity and insulin clearance [53]. Perticone F [54] was documented when hypertensive NGT ≥ 155 mmHg, and UA is closely related to 1-h postload glucose during an oral glucose tolerance. We [55] analyzed the clinical characteristics and islet function index of 403 newly diagnosed patients with T2DM (mean age, 50.21 ± 13.34 years old; 62.5% male) and analyzed the SUA levels according to gender. Multivariate linear regression analysis showed that SUA had an independent effect on insulin secretion in female patients; the islet β-cell function of male was also affected by SUA, age, body mass index (BMI), and blood lipids; SUA correlated positively with insulin secretion and the insulin resistance index in male patients.
In terms of gestational diabetes, Leng [56] found that the SUA level is positively related with the risk of T2DM and prediabetes in the Tianjin region of China gestational diabetes mellitus (GDM) prevention planning data. In the group with GDM and impaired glucose tolerance (IGT), the mean SUA level was significantly increased in early pregnancy, and a UA level of 3.95 mg/dl could predict GDM with 60% specificity and 100% sensitivity [57].
3.2. Uric Acid and Diabetic Chronic Complications
3.2.1. Uric Acid and Diabetic Macrovascular Disease
Diabetic macroangiopathy refers to atherosclerosis of blood vessels such as the aorta, coronary artery, basilar artery, renal artery, and peripheral arteries, especially in the heart and cerebrovascular diseases, which is caused by dysfunction of endothelial cells, advanced glycation end product (AGEs/RAGEs) system, the hexosamine pathway, inflammation, oxidant stress, protein kinase (PKC), and polyol [34–37]. Some clinical studies have shown a positive correlation between uric acid and diabetic macroangiopathy. Yan et al. [58] used Mendelian randomized analysis to determine whether there is a causal relationship between UA and diabetic macrovascular disease and found that the prevalence of diabetic macrovascular disease was significantly higher in the hyperuricemia group than in the healthy population, suggesting that UA and diabetic macrovascular disease are related. Indeed, the link between female-weighted genetic risk score (GRS) and diabetic macrovascular disease was greater than expected. Hyperuricemia was also observed to be associated with an increased incidence of atrial fibrillation in hospitalized patients with T2DM [59]. Hyperuricemia can increase the risk of sudden atrial fibrillation by approximately four-fold [60] and is associated with cardiovascular mortality [61]. Cardiovascular and cerebrovascular diseases are mainly caused by ischemia and hypoxia resulting from coronary atherosclerosis. Du et al. [62] performed a meta-analysis of patients with T2DM to determine whether SUA levels were associated with cerebral infarction and calculated the ratio of means (RoM) for SUA and the average cerebral infarction or average diabetes control ratio of individual studies and then compared it with the calculated 95% confidence intervals. The results showed that higher SUA levels might lead to cerebral infarction in patients with T2DM. Wang et al. [63] used the “Comprehensive Diabetes Prevention and Control Study (CRPCD)” data to explore the relationship between SUA and ischemic stroke in patients with T2DM in China. A total of 19,442 participants were enrolled in a cross-sectional study. The SUA level was significantly higher in patients over 60 years of age than in people under 60 years of age. Serum UA levels were independently and positively correlated with ischemic stroke in patients under 60 years of age, and it was characterized by U-type association in patients over 60 years of age. We speculated that the incidence of other established stroke risk factors such as hypertension, dyslipidemia, and chronic kidney disease increased with age would made it difficult to establish UA as an independent role in stroke.
Diabetic hyperglycemia causes metabolic abnormalities, which can affect systemic organs. Diabetic foot is caused by peripheral vascular disease, peripheral (motor, sensory, and autonomic) neuropathy, and excessive mechanical stress (repetitive external or minor trauma) in diabetic patients, leading to the destruction and deformity of the soft tissue and bone joint system of the foot [64]. The pathogenesis is partly the same as diabetic vascular and neuropathy complications [65]. Uric acid can be used as an independent risk factor to assess the development of diabetic foot [66].
3.2.2. Uric Acid and Diabetic Microangiopathy
Diabetic microangiopathy is a specific complication of diabetes. The typical changes comprise microcirculatory disorders and microvascular basement membrane thickening, which mainly lead to diabetic nephropathy (DN) [51] and diabetic retinopathy (DR) [67–70].
(1) Uric Acid and Diabetic Nephropathy. Diabetic nephropathy is a long-standing microvascular complication of diabetes and is the leading cause of end-stage renal disease in developed countries [10, 71]. As an inflammatory factor, UA increases oxidative stress and promotes the activation of the renin-angiotensin-aldosterone system (RAAS) [21, 41]. Therefore, UA levels are associated with the occurrence and development of DN and are independent risk factors for early kidney disease [72, 73], which help to predict microalbuminuria progression [74]. Serum UA and microalbuminuria levels were significantly positively correlated with renal disease in patients with T2DM [75]. Patients with higher SUA levels have poorer renal function, independent of glycated hemoglobin (HbA1c) or the duration of diabetes [76]. In T2DM, there is an independent and significant positive association between higher blood UA and an increased risk of a reduced glomerular filtration rate (eGFR) [77]. Blood UA levels greater than 5.5 mg/dl can predict chronic kidney disease of stage 3 and above in T2DM [78]. The level of SUA that protects against progression of type 2 diabetic nephropathy (diabetic kidney disease (DKD)) is lower than the current normal value. The optimal cut-off value is 377.5 µmol/l (6.3 mg/dl) for men and 309.0 μmol/l (5.2 mg/dl) for women [79]. In Chinese patients with T2DM, UA-related alleles such as SLC2A9 rs11722228 (solute carrier family 2 member 9), SLC2A9 rs3775948, and ABCG2 rs2231142 (ATP binding cassette subfamily G member 2) may affect susceptibility to DKD [80]. Contrast-enhanced ultrasound (CEUS) was used to show renal microvascular hyperperfusion, with a decreased glomerular filtration rate and reduced UA excretion in patients with DKD [81]. Xanthine oxidase (XO) is a very important enzyme that is responsible for the conversion of sulfhydryl groups to UA. Elevation of UA by 1 μmol/l enhanced the probability of albuminuria by 1.5%, and a rise in XO activity of 1 U/l also increased the probability of albuminuria by 1.5%. In diabetes, both XO and uric acid are independently associated with albuminuria [82].
In patients with type 1 diabetes without complications, higher UA levels are associated with lower GFR, which is due to UA-mediated increased resistance in afferent renal arteriole promoting the renal microcirculation ischemia [83, 84].
In type 1 diabetes, kidney damage is more common in men whose SUA and creatinine concentrations and the albumin excretion rate are higher than those in female patients. Indeed, hyperglycemia adversely affects the activity of estrogen receptors (ER) and this may be gender-specific. The progression of renal disease in men with T1D is associated with a decline in free estradiol levels [85], and 17β-estradiol shows antioxidant, antiapoptotic, and anti-inflammatory properties [86]. The SUA level in boys but not girls with T1D was positively correlated with subclinical inflammation marker levels (CRP, IL-6, TNF-α), renal function indicators (albumin excretion rate, cystatin-C level), and blood pressure; it was negatively correlated with anti-inflammatory IL-10 [87].
(2) Uric Acid and Diabetic Retinopathy. Diabetic retinopathy (DR) is a specific fundus lesion that is the main cause of blindness in patients with diabetes [88]. Based on the changes of haemodynamics or vascular geometry, vascular injury is considered to be the prime motivator for the initiation and progression of DR, including pericytosis, platelet aggregation, thickening of basement membrane, and neuroglial damage [89]. The blood retinal barrier, as precondition to vision acuity, is vulnerable to injury during the progression of DR. This is a consequence of the interplay of AGE, hexosamine, polyol, inflammation, NO decline, oxidative stress, PKC, and RAS [38]. Uric acid is closely related to these pathological changes. Clinically, DR is classified into nonproliferative diabetic retinopathy (NPDR) (also known as simple type or background type) and proliferative diabetic retinopathy (PDR), according to whether or not retinal neovascularization occurs [90]. In Chinese patients with T2DM, reduction in urinary uric acid excretion (UUAE) is an independent risk factor for DR [91]. Elevated SUA levels are significantly associated with albuminuria and DR severity [92], but not with the retinal nerve fibre layer or macular thickness [93]. A study reported that increased SUA levels were associated with an increased severity of DR in Taiwan [94]. Kuwata [95] analyzed data from 1839 patients with T2DM in Japan by gender stratification and found that higher SUA levels were associated with an increased risk of DR in men, but not in women. The results showed sex hormones play an important role in the metabolism of uric acid, which deserved to discuss the specific mechanism further.
3.2.3. Uric Acid and Diabetic Peripheral Neuropathy
Diabetic neuropathy is one of the most common chronic complication of diabetes [96], characterized by damage to nerve glial cells, axons, and endothelial cells, and the morbidity from 30% to 50% in T2DM [97]. Diabetic peripheral neuropathy (DPN) is the main clinical manifestation of sensory and autonomic nerve symptoms, distal symmetry polyneuropathy, and motor neuropathy are the most common types of DPN [98]. The pathophysiology changes conclude polyol pathway, PKC activity, increased AGEs, oxidative stress (ROS), inflammation (IL-1β, IL-6, TNFα, and COX-2), microvascular alterations (endothelial dysfunction), nerve degeneration and regrowth (MMPs, Schwann cells and ECM), and the changes of the blood-nerve barrier [39, 99, 100]. Lin et al. [101] observed significant differences in the ratio of motor and sensory nerve amplitude and conduction velocity (CV) parameters between groups with different blood UA levels (both P < 0.05). Blood UA levels were negatively correlated with the ratio of motor and sensory nerve amplitude and CV. Blood UA at 9 mg/dl and total cholesterol of 5.2 mmol/l were significantly associated with DPN in patients who had suffered from T2DM for more than 10 years. Yu et al. [102] performed a meta-analysis of 1388 patients with T2DM with peripheral neuropathy and in 4746 patients without peripheral neuropathy and showed that SUA levels were significantly elevated in patients with diabetes complicated with peripheral neuropathy and that increased hyperuricemia was related with increased risk of peripheral neuropathy.
4. Conclusion
Complex genetic and environmental factors contribute to causing diabetes, and chronic complications of diabetes may occur throughout the body. The pathogenesis of T2DM is complex, involving various interacting factors. Its increased incidence rate is a great concern worldwide. Hyperuricemia is closely related to the development of diabetes and its chronic complications. Many animal and human experiments have confirmed that UA mainly affects diabetes and its complications through inflammation, oxidative stress, endothelial function damage, and other effects. We call for further researches to explore the molecular mechanism, especially in the direct effect of uric acid on insulin secretion.
Acknowledgments
This study was supported by the National Natural Science Foundation of China (no. 81370872). The authors are indebted to the Department of Endocrinology, Zhongnan Hospital of Wuhan University, for providing suggestion during the preparation of the manuscript.
Conflicts of Interest
The authors declare that there are no conflicts of interest related with the publication of this paper.
Authors' Contributions
Qing Xiong and Jie Liu contributed equally to this work.
References
- 1.Hannou S. A., Haslam D. E., McKeown N. M., Herman M. A. Fructose metabolism and metabolic disease. Journal of Clinical Investigation. 2018;128(2):545–555. doi: 10.1172/jci96702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lanaspa M. A., Cicerchi C., Garcia G., et al. Counteracting roles of AMP deaminase and AMP kinase in the development of fatty liver. PLoS One. 2012;7(11) doi: 10.1371/journal.pone.0048801.e48801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lanaspa M. A., Sanchez-Lozada L. G., Choi Y.-J., et al. Uric acid induces hepatic steatosis by generation of mitochondrial oxidative stress. Journal of Biological Chemistry. 2012;287(48):40732–40744. doi: 10.1074/jbc.m112.399899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cicerchi C., Li N., Kratzer J., et al. Uric acid-dependent inhibition of AMP kinase induces hepatic glucose production in diabetes and starvation: evolutionary implications of the uricase loss in hominids. The FASEB Journal. 2014;28(8):3339–3350. doi: 10.1096/fj.13-243634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ishimoto T., Lanaspa M. A., Le M. T., et al. Opposing effects of fructokinase C and A isoforms on fructose-induced metabolic syndrome in mice. Proceedings of the National Academy of Sciences. 2012;109(11):4320–4325. doi: 10.1073/pnas.1119908109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnson R. J., Nakagawa T., Sanchez-Lozada L. G., et al. Sugar, uric acid, and the etiology of diabetes and obesity. Diabetes. 2013;62(10):3307–3315. doi: 10.2337/db12-1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gagliardi A. C. M., Miname M. H., Santos R. D. Uric acid: a marker of increased cardiovascular risk. Atherosclerosis. 2009;202(1):11–17. doi: 10.1016/j.atherosclerosis.2008.05.022. [DOI] [PubMed] [Google Scholar]
- 8.Du T., Sun X., Lu H., et al. Associations of serum uric acid levels with cardiovascular health factors:Differences by sex, age and body mass index in Chinese participants. European Journal of Internal Medicine. 2014;25(4):388–393. doi: 10.1016/j.ejim.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 9.Johnson R. J., Merriman T., Lanaspa M. A. Causal or noncausal relationship of uric acid with diabetes: table 1. Diabetes. 2015;64(8):2720–2722. doi: 10.2337/db15-0532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lytvyn Y., Perkins B. A., Cherney D. Z. I. Uric acid as a biomarker and a therapeutic target in diabetes. Canadian Journal of Diabetes. 2015;39(3):239–246. doi: 10.1016/j.jcjd.2014.10.013. [DOI] [PubMed] [Google Scholar]
- 11.Sochett E. B., Cherney D. Z. I., Curtis J. R., Dekker M. G., Scholey J. W., Miller J. A. Impact of renin angiotensin system modulation on the hyperfiltration state in type 1 diabetes. Journal of the American Society of Nephrology. 2006;17(6):1703–1709. doi: 10.1681/asn.2005080872. [DOI] [PubMed] [Google Scholar]
- 12.Bobulescu I. A., Moe O. W. Renal transport of uric acid: evolving concepts and uncertainties. Advances in Chronic Kidney Disease. 2012;19(6):358–371. doi: 10.1053/j.ackd.2012.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maesaka J., Fishbane S. Regulation of renal urate excretion: a critical review. American Journal of Kidney Diseases. 1998;32(6):917–933. doi: 10.1016/s0272-6386(98)70067-8. [DOI] [PubMed] [Google Scholar]
- 14.Sorensen L. B., Levinson D. J. Origin and extrarenal elimination of uric acid in man. Nephron. 1975;14(1):7–20. doi: 10.1159/000180432. [DOI] [PubMed] [Google Scholar]
- 15.Gibson T. J. Hypertension, its treatment, hyperuricaemia and gout. Current Opinion in Rheumatology. 2013;25(2):217–222. doi: 10.1097/bor.0b013e32835cedd4. [DOI] [PubMed] [Google Scholar]
- 16.Bonakdaran S., Kharaqani B. Association of serum uric acid and metabolic syndrome in type 2 diabetes. Current Diabetes Reviews. 2014;10(2):113–117. doi: 10.2174/1573399810666140228160938. [DOI] [PubMed] [Google Scholar]
- 17.Li Y.-l., Xie H., Musha H., et al. The risk factor Analysis for type 2 diabetes mellitus patients with nonalcoholic fatty liver disease and positive correlation with serum uric acid. Cell Biochemistry and Biophysics. 2015;72(3):643–647. doi: 10.1007/s12013-014-0346-1. [DOI] [PubMed] [Google Scholar]
- 18.Viazzi F., Leoncini G., Vercelli M., Deferrari G., Pontremoli R. Serum uric acid levels predict new-onset type 2 diabetes in hospitalized patients with primary hypertension: the MAGIC study. Diabetes Care. 2011;34(1):126–128. doi: 10.2337/dc10-0918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnson R. J., Kang D.-H., Feig D., et al. Is there a pathogenetic role for uric acid in hypertension and cardiovascular and renal disease? Hypertension. 2003;41(6):1183–1190. doi: 10.1161/01.hyp.0000069700.62727.c5. [DOI] [PubMed] [Google Scholar]
- 20.Kang D.-H., Park S.-K., Lee I.-K., Johnson R. J. Uric acid-induced C-reactive protein expression: implication on cell proliferation and nitric oxide production of human vascular cells. Journal of the American Society of Nephrology. 2005;16(12):3553–3562. doi: 10.1681/asn.2005050572. [DOI] [PubMed] [Google Scholar]
- 21.Chaudhary K., Malhotra K., Sowers J., Aroor A. Uric acid-key ingredient in the recipe for cardiorenal metabolic syndrome. Cardiorenal Medicine. 2013;3(3):208–220. doi: 10.1159/000355405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maahs D. M., Caramori L., Cherney D. Z. I., et al. Uric acid lowering to prevent kidney function loss in diabetes: the preventing early renal function loss (PERL) allopurinol study. Current Diabetes Reports. 2013;13(4):550–559. doi: 10.1007/s11892-013-0381-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kirilmaz B., Asgun F., Alioglu E., et al. High inflammatory activity related to the number of metabolic syndrome components. The Journal of Clinical Hypertension. 2010;12(2):136–144. doi: 10.1111/j.1751-7176.2009.00229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yu M. A., Sanchez-Lozada L. G., Johnson R. J., et al. Oxidative stress with an activation of the renin-angiotensin system in human vascular endothelial cells as a novel mechanism of uric acid-induced endothelial dysfunction. Journal of Hypertension. 2010;28(6):1234–1242. doi: 10.1097/hjh.0b013e328337da1d. [DOI] [PubMed] [Google Scholar]
- 25.Matsuoka T., Kajimoto Y., Watada H., et al. Glycation-dependent, reactive oxygen species-mediated suppression of the insulin gene promoter activity in HIT cells. Journal of Clinical Investigation. 1997;99(1):144–150. doi: 10.1172/jci119126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hsueh W. A., Lyon C. J., Quiñones M. J. Insulin resistance and the endothelium. The American Journal of Medicine. 2004;117(2):109–117. doi: 10.1016/j.amjmed.2004.02.042. [DOI] [PubMed] [Google Scholar]
- 27.Zoccali C., Maio R., Mallamaci F., Sesti G., Perticone F. Uric acid and endothelial dysfunction in essential hypertension. Journal of the American Society of Nephrology. 2006;17(5):1466–1471. doi: 10.1681/asn.2005090949. [DOI] [PubMed] [Google Scholar]
- 28.Erdogan D., Gullu H., Caliskan M., et al. Relationship of serum uric acid to measures of endothelial function and atherosclerosis in healthy adults. International Journal of Clinical Practice. 2005;59(11):1276–1282. doi: 10.1111/j.1742-1241.2005.00621.x. [DOI] [PubMed] [Google Scholar]
- 29.Tassone E. J., Cimellaro A., Perticone M., et al. Uric acid impairs insulin signaling by promoting Enpp1 binding to insulin receptor in human umbilical vein endothelial cells. Frontiers in Endocrinology. 2018;9(98) doi: 10.3389/fendo.2018.00098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Perticone F., Maio R., Sciacqua A., et al. Endothelial dysfunction and C-reactive protein are risk factors for diabetes in essential hypertension. Diabetes. 2008;57(1):167–171. doi: 10.2337/db07-1189. [DOI] [PubMed] [Google Scholar]
- 31.Baldwin W., McRae S., Marek G., et al. Hyperuricemia as a mediator of the proinflammatory endocrine imbalance in the adipose tissue in a murine model of the metabolic syndrome. Diabetes. 2011;60(4):1258–1269. doi: 10.2337/db10-0916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Spiga R., Marini M. A., Mancuso E., et al. Uric acid is associated with inflammatory biomarkers and induces inflammation via activating the NF-κB signaling pathway in HepG2 cells. Arteriosclerosis, Thrombosis, and Vascular Biology. 2017;37(6):1241–1249. doi: 10.1161/atvbaha.117.309128. [DOI] [PubMed] [Google Scholar]
- 33.Coccheri S. Approaches to prevention of cardiovascular complications and events in diabetes mellitus. Drugs. 2007;67(7):997–1026. doi: 10.2165/00003495-200767070-00005. [DOI] [PubMed] [Google Scholar]
- 34.Laight D., Carrier M. J., Anggard E. E. Antioxidants, diabetes and endothelial dysfunction. Cardiovascular Research. 2000;47(3):457–464. doi: 10.1016/s0008-6363(00)00054-7. [DOI] [PubMed] [Google Scholar]
- 35.Laight D. W., Carrier M. J., Änggård E. E. Endothelial cell dysfunction and the pathogenesis of diabetic macroangiopathy. Diabetes/Metabolism Research and Reviews. 1999;15(4):274–282. doi: 10.1002/(sici)1520-7560(199907/08)15:4<274::aid-dmrr46>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 36.Madonna R., Pieragostino D., Balistreri C. R., et al. Diabetic macroangiopathy: pathogenetic insights and novel therapeutic approaches with focus on high glucose-mediated vascular damage. Vascular Pharmacology. 2018;107:27–34. doi: 10.1016/j.vph.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 37.Madonna R., De Caterina R. Cellular and molecular mechanisms of vascular injury in diabetes—Part I: pathways of vascular disease in diabetes. Vascular Pharmacology. 2011;54(3–6):68–74. doi: 10.1016/j.vph.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 38.Mahajan N., Arora P., Sandhir R. Perturbed biochemical pathways and associated oxidative stress lead to vascular dysfunctions in diabetic retinopathy. Oxidative Medicine and Cellular Longevity. 2019;2019:16. doi: 10.1155/2019/8458472.8458472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bönhof G. J., Herder C., Strom A., Papanas N., Roden M., Ziegler D. Emerging biomarkers, tools, and treatments for diabetic polyneuropathy. Endocrine Reviews. 2019;40(1):153–192. doi: 10.1210/er.2018-00107. [DOI] [PubMed] [Google Scholar]
- 40.Mazzali M., Hughes J., Kim Y.-G., et al. Elevated uric acid increases blood pressure in the rat by a novel crystal-independent mechanism. Hypertension. 2001;38(5):1101–1106. doi: 10.1161/hy1101.092839. [DOI] [PubMed] [Google Scholar]
- 41.Filiopoulos V., Hadjiyannakos D., Vlassopoulos D. New insights into uric acid effects on the progression and prognosis of chronic kidney disease. Renal Failure. 2012;34(4):510–520. doi: 10.3109/0886022x.2011.653753. [DOI] [PubMed] [Google Scholar]
- 42.Mazzali M., Kanellis J., Han L., et al. Hyperuricemia induces a primary renal arteriolopathy in rats by a blood pressure-independent mechanism. American Journal of Physiology-Renal Physiology. 2002;282(6):F991–F997. doi: 10.1152/ajprenal.00283.2001. [DOI] [PubMed] [Google Scholar]
- 43.Zatz R., Meyer T. W., Rennke H. G., Brenner B. M. Predominance of hemodynamic rather than metabolic factors in the pathogenesis of diabetic glomerulopathy. Proceedings of the National Academy of Sciences. 1985;82(17):5963–5967. doi: 10.1073/pnas.82.17.5963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ginsberg M. H., Kozin F., O’Malley M., McCarty D. J. Release of platelet constituents by monosodium urate crystals. Journal of Clinical Investigation. 1977;60(5):999–1007. doi: 10.1172/jci108880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sluijs I., Holmes M. V., van der Schouw Y. T., et al. A mendelian randomization study of circulating uric acid and type 2 diabetes. Diabetes. 2015;64(8):3028–3036. doi: 10.2337/db14-0742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li X., Meng X., Gao X. C., et al. Elevated serum xanthine oxidase activity is associated with the development of type 2 diabetes: a prospective cohort study. Diabetes Care. 2018;41(4):884–890. doi: 10.2337/dc17-1434. [DOI] [PubMed] [Google Scholar]
- 47.Bombelli M., Quarti-Trevano F., Tadic M., et al. Uric acid and risk of new-onset metabolic syndrome, impaired fasting glucose and diabetes mellitus in a general Italian population. Journal of Hypertension. 2018;36(7):1492–1498. doi: 10.1097/hjh.0000000000001721. [DOI] [PubMed] [Google Scholar]
- 48.Anothaisintawee T., Lertrattananon D., Thamakaison S., et al. Direct and indirect effects of serum uric acid on blood sugar levels in patients with prediabetes: a mediation analysis. Journal of Diabetes Research. 2017;2017:6. doi: 10.1155/2017/6830671.6830671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shani M., Vinker S., Dinour D., et al. High normal uric acid levels are associated with an increased risk of diabetes in lean, normoglycemic healthy women. The Journal of Clinical Endocrinology and Metabolism. 2016;101(10):3772–3778. doi: 10.1210/jc.2016-2107. [DOI] [PubMed] [Google Scholar]
- 50.Chang J.-B., Chen Y.-L., Hung Y.-J., et al. The role of uric acid for predicting future metabolic syndrome and type 2 diabetes in older people. The Journal of Nutrition, Health and Aging. 2017;21(3):329–335. doi: 10.1007/s12603-016-0749-3. [DOI] [PubMed] [Google Scholar]
- 51.Chen Y.-Y., Kao T.-W., Yang H.-F., et al. The association of uric acid with the risk of metabolic syndrome, arterial hypertension or diabetes in young subjects- an observational study. Clinica Chimica Acta. 2018;478:68–73. doi: 10.1016/j.cca.2017.12.038. [DOI] [PubMed] [Google Scholar]
- 52.Bjornstad P., Snell-Bergeon J. K., McFann K., et al. Serum uric acid and insulin sensitivity in adolescents and adults with and without type 1 diabetes. Journal of Diabetes and Its Complications. 2014;28(3):298–304. doi: 10.1016/j.jdiacomp.2013.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fiorentino T. V., Sesti F., Succurro E., et al. Higher serum levels of uric acid are associated with a reduced insulin clearance in non-diabetic individuals. Acta Diabetologica. 2018;55(8):835–842. doi: 10.1007/s00592-018-1153-8. [DOI] [PubMed] [Google Scholar]
- 54.Perticone F., Sciacqua A., Perticone M., et al. Serum uric acid and 1-h postload glucose in essential hypertension. Diabetes Care. 2012;35(1):153–157. doi: 10.2337/dc11-1727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hu Y., Liu J., Li H., et al. The association between elevated serum uric acid levels and islet β-cell function indexes in newly diagnosed type 2 diabetes mellitus: a cross-sectional study. PeerJ. 2018;6:p. e4515. doi: 10.7717/peerj.4515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Leng J., Wang L., Wang J., et al. Uric acid and diabetes risk among Chinese women with a history of gestational diabetes mellitus. Diabetes Research and Clinical Practice. 2017;134:72–79. doi: 10.1016/j.diabres.2017.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Aker S. S., Yuce T., Kalafat E., et al. Association of first trimester serum uric acid levels gestational diabetes mellitus development. Journal of Turkish Society of Obstetric and Gynecology. 2016;13(2):71–74. doi: 10.4274/tjod.69376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yan D. D., Wang J., Jiang F., et al. A causal relationship between uric acid and diabetic macrovascular disease in Chinese type 2 diabetes patients: a Mendelian randomization analysis. International Journal of Cardiology. 2016;214:194–199. doi: 10.1016/j.ijcard.2016.03.206. [DOI] [PubMed] [Google Scholar]
- 59.Mantovani A., Rigolon R., Pichiri I., et al. Hyperuricemia is associated with an increased prevalence of atrial fibrillation in hospitalized patients with type 2 diabetes. Journal of Endocrinological Investigation. 2016;39(2):159–167. doi: 10.1007/s40618-015-0354-z. [DOI] [PubMed] [Google Scholar]
- 60.Mantovani A., Rigolon R., Civettini A., et al. Hyperuricemia is associated with an increased prevalence of paroxysmal atrial fibrillation in patients with type 2 diabetes referred for clinically indicated 24-h Holter monitoring. Journal of Endocrinological Investigation. 2018;41(2):223–231. doi: 10.1007/s40618-017-0729-4. [DOI] [PubMed] [Google Scholar]
- 61.Ilundain-González A. I., Gimeno-Orna J. A., Sáenz-Abad D., Pons-Dolset J., Cebollada-del Hoyo J., Lahoza-Pérez M. d. C. Influencia de los niveles de ácido úrico sobre el riesgo de mortalidad cardiovascular a largo plazo en pacientes con diabetes de tipo 2. Endocrinología, Diabetes Y Nutrición. 2018;65(6):335–341. doi: 10.1016/j.endien.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 62.Du L., Ma J., Zhang X. Higher serum uric acid may contribute to cerebral infarction in patients with type 2 diabetes mellitus: a meta-analysis. Journal of Molecular Neuroscience. 2017;61(1):25–31. doi: 10.1007/s12031-016-0848-y. [DOI] [PubMed] [Google Scholar]
- 63.Wang L., Hu W., Miao D. D., et al. Relationship between serum uric acid and ischemic stroke in a large type 2 diabetes population in China: a cross-sectional study. Journal of the Neurological Sciences. 2017;376:176–180. doi: 10.1016/j.jns.2017.03.023. [DOI] [PubMed] [Google Scholar]
- 64.Armstrong D. G., Boulton A. J. M., Bus S. A. Diabetic foot ulcers and their recurrence. New England Journal of Medicine. 2017;376(24):2367–2375. doi: 10.1056/nejmra1615439. [DOI] [PubMed] [Google Scholar]
- 65.Volmer-Thole M., Lobmann R. Neuropathy and diabetic foot syndrome. International Journal of Molecular Sciences. 2016;17(6) doi: 10.3390/ijms17060917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ye X., Cao Y., Gao F., et al. Elevated serum uric acid levels are independent risk factors for diabetic foot ulcer in female Chinese patients with type 2 diabetes. Journal of Diabetes. 2014;6(1):42–47. doi: 10.1111/1753-0407.12079. [DOI] [PubMed] [Google Scholar]
- 67.Jaap A. J., Tooke J. E. Pathophysiology of microvascular disease in non-insulin-dependent diabetes. Clinical Science. 1995;89(1):3–12. doi: 10.1042/cs0890003. [DOI] [PubMed] [Google Scholar]
- 68.Hanssen K. F. Blood glucose control and microvascular and macrovascular complications in diabetes. Diabetes. 1997;46(2):S101–S103. doi: 10.2337/diab.46.2.s101. [DOI] [PubMed] [Google Scholar]
- 69.Persson F., Rossing P. Diagnosis of diabetic kidney disease: state of the art and future perspective. Kidney International Supplements. 2018;8(1):2–7. doi: 10.1016/j.kisu.2017.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Semeraro F., Morescalchi F., Cancarini A., et al. Diabetic retinopathy, a vascular and inflammatory disease: therapeutic implications. Diabetes and Metabolism. 2019 doi: 10.1016/j.diabet.2019.04.002. pii: S1262-3636(19)30062-X. [DOI] [PubMed] [Google Scholar]
- 71.Chang Y.-H., Lei C.-C., Lin K.-C., Chang D.-M., Hsieh C.-H., Lee Y.-J. Serum uric acid level as an indicator for CKD regression and progression in patients with type 2 diabetes mellitus-a 4.6-year cohort study. Diabetes/Metabolism Research and Reviews. 2016;32(6):557–564. doi: 10.1002/dmrr.2768. [DOI] [PubMed] [Google Scholar]
- 72.De Cosmo S., Viazzi F., Pacilli A., et al. Serum uric acid and risk of CKD in type 2 diabetes. Clinical Journal of the American Society of Nephrology. 2015;10(11):1921–1929. doi: 10.2215/cjn.03140315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Li G. X., Jiao X. H., Cheng X. B. Correlations between blood uric acid and the incidence and progression of type 2 diabetes nephropathy. European Review for Medical and Pharmacological Sciences. 2018;22(2):506–511. doi: 10.26355/eurrev_201801_14202. [DOI] [PubMed] [Google Scholar]
- 74.Hayashino Y., Okamura S., Tsujii S., Ishii H. Association of serum uric acid levels with the risk of development or progression of albuminuria among Japanese patients with type 2 diabetes: a prospective cohort study [Diabetes Distress and Care Registry at Tenri (DDCRT 10)] Acta Diabetologica. 2016;53(4):599–607. doi: 10.1007/s00592-015-0825-x. [DOI] [PubMed] [Google Scholar]
- 75.Latif H., Iqbal A., Rathore R., et al. Correlation between serum uric acid level and microalbuminuria in type-2 diabetic nephropathy. Pakistan Journal of Medical Sciences. 2017;33(6):1371–1375. doi: 10.12669/pjms.336.13224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pizarro M. H., Santos D. C., Barros B. S. V., et al. Serum uric acid and renal function in patients with type 1 diabetes: a nationwide study in Brazil. Diabetology and Metabolic Syndrome. 2018;10 doi: 10.1186/s13098-018-0324-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wang J., Yu Y. K., Li X. W., et al. Serum uric acid levels and decreased estimated glomerular filtration rate in patients with type 2 diabetes: a cohort study and meta-analysis. Diabetes/Metabolism Research and Reviews. 2018;34(7) doi: 10.1002/dmrr.3046. [DOI] [PubMed] [Google Scholar]
- 78.Kim W. J., Kim S. S., Bae M. J., et al. High-normal serum uric acid predicts the development of chronic kidney disease in patients with type 2 diabetes mellitus and preserved kidney function. Journal of Diabetes and Its Complications. 2014;28(2):130–134. doi: 10.1016/j.jdiacomp.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 79.Bartáková V., Kuricová K., Pácal L., et al. Hyperuricemia contributes to the faster progression of diabetic kidney disease in type 2 diabetes mellitus. Journal of Diabetes and Its Complications. 2016;30(7):1300–1307. doi: 10.1016/j.jdiacomp.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 80.Yan D. D., Wang J., Jiang F., et al. Association between serum uric acid related genetic loci and diabetic kidney disease in the Chinese type 2 diabetes patients. Journal of Diabetes and Its Complications. 2016;30(5):798–802. doi: 10.1016/j.jdiacomp.2016.02.018. [DOI] [PubMed] [Google Scholar]
- 81.Wang L., Cheng J. F., Sun L. P., et al. Use of contrast-enhanced ultrasound to study relationship between serum uric acid and renal microvascular perfusion in diabetic kidney disease. BioMed Research International. 2015;2015:10. doi: 10.1155/2015/732317.732317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Klisic A., Kocic G., Kavaric N., Jovanovic M., Stanisic V., Ninic A. Xanthine oxidase and uric acid as independent predictors of albuminuria in patients with diabetes mellitus type 2. Clinical and Experimental Medicine. 2018;18(2):283–290. doi: 10.1007/s10238-017-0483-0. [DOI] [PubMed] [Google Scholar]
- 83.Lytvyn Y., Škrtić M., Yang G. K., Yip P. M., Perkins B. A., Cherney D. Z. I. Glycosuria-mediated urinary uric acid excretion in patients with uncomplicated type 1 diabetes mellitus. American Journal of Physiology-Renal Physiology. 2015;308(2):F77–F83. doi: 10.1152/ajprenal.00555.2014. [DOI] [PubMed] [Google Scholar]
- 84.Lytvyn Y., Škrtić M., Yang G. K., et al. Plasma uric acid effects on glomerular haemodynamic profile of patients with uncomplicated Type 1 diabetes mellitus. Diabetic Medicine. 2016;33(8):1102–1111. doi: 10.1111/dme.13051. [DOI] [PubMed] [Google Scholar]
- 85.Maric C., Forsblom C., Thorn L., Wadén J., Groop P.-H. Association between testosterone, estradiol and sex hormone binding globulin levels in men with type 1 diabetes with nephropathy. Steroids. 2010;75(11):772–778. doi: 10.1016/j.steroids.2010.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Miller A. A., Drummond G. R., Mast A. E., Schmidt H. H. H. W., Sobey C. G. Effect of gender on NADPH-oxidase activity, expression, and function in the cerebral circulation. Stroke. 2007;38(7):2142–2149. doi: 10.1161/strokeaha.106.477406. [DOI] [PubMed] [Google Scholar]
- 87.Slominski B., Skrzypkowska M., Ryba-Stanislawowska M., et al. Sex-related association of serum uric acid with inflammation, kidney function and blood pressure in type 1 diabetic patients. Pediatric Diabetes. 2018;19(5):1014–1019. doi: 10.1111/pedi.12670. [DOI] [PubMed] [Google Scholar]
- 88.Flaxman S. R., Bourne R. R. A., Resnikoff S., et al. Global causes of blindness and distance vision impairment 1990-2020: a systematic review and meta-analysis. The Lancet Global Health. 2017;5(12):e1221–e1234. doi: 10.1016/S2214-109X(17)30393-5. [DOI] [PubMed] [Google Scholar]
- 89.Fletcher E., Phipps J., Ward M., Puthussery T., Wilkinson-Berka J. Neuronal and glial cell abnormality as predictors of progression of diabetic retinopathy. Current Pharmaceutical Design. 2007;13(26):2699–2712. doi: 10.2174/138161207781662920. [DOI] [PubMed] [Google Scholar]
- 90.Santiago A. R., Boia R., Aires I. D., et al. Sweet stress: coping with vascular dysfunction in diabetic retinopathy. Frontiers in Physiology. 2018;9:p. 820. doi: 10.3389/fphys.2018.00820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Li L.-X., Lu J.-X., Shuai H.-P., et al. Decreased urine uric acid excretion is associated with diabetic retinopathy but not with lower limb atherosclerosis in hospitalized patients with type 2 diabetes. Atherosclerosis. 2015;242(1):13–18. doi: 10.1016/j.atherosclerosis.2015.06.051. [DOI] [PubMed] [Google Scholar]
- 92.Liang C. C., Lin P. C., Lee M. Y., et al. Association of serum uric acid concentration with diabetic retinopathy and albuminuria in Taiwanese patients with type 2 diabetes mellitus. International Journal of Molecular Sciences. 2016;17(8) doi: 10.3390/ijms17081248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Vinuthinee-Naidu M. N., Zunaina E., Azreen-Redzal A., et al. Correlation of retinal nerve fibre layer and macular thickness with serum uric acid among type 2 diabetes mellitus. BMC Ophthalmology. 2017;17 doi: 10.1186/s12886-017-0486-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lee J.-J., Yang I.-H., Kuo H.-K., et al. Serum uric acid concentration is associated with worsening in severity of diabetic retinopathy among type 2 diabetic patients in Taiwan-A 3-year prospective study. Diabetes Research and Clinical Practice. 2014;106(2):366–372. doi: 10.1016/j.diabres.2014.07.027. [DOI] [PubMed] [Google Scholar]
- 95.Kuwata H., Okamura S., Hayashino Y., et al. Serum uric acid levels are associated with increased risk of newly developed diabetic retinopathy among Japanese male patients with type 2 diabetes: a prospective cohort study (diabetes distress and care registry at Tenri [DDCRT 13]) Diabetes/Metabolism Research and Reviews. 2017;33(7):p. e2905. doi: 10.1002/dmrr.2905. [DOI] [PubMed] [Google Scholar]
- 96.Dyck P. J., Kratz K. M., Karnes J. L., et al. The prevalence by staged severity of various types of diabetic neuropathy, retinopathy, and nephropathy in a population-based cohort: the Rochester Diabetic Neuropathy Study. Neurology. 1993;43(4):p. 817. doi: 10.1212/wnl.43.4.817. [DOI] [PubMed] [Google Scholar]
- 97.Peltier A., Goutman S. A., Callaghan B. C. Painful diabetic neuropathy. BMJ. 2014;348(1):p. g1799. doi: 10.1136/bmj.g1799. [DOI] [PubMed] [Google Scholar]
- 98.Pop-Busui R., Boulton A. J. M., Feldman E. L., et al. Diabetic neuropathy: a position statement by the American diabetes association. Diabetes Care. 2017;40(1):136–154. doi: 10.2337/dc16-2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Shillo P., Sloan G., Greig M., et al. Painful and painless diabetic neuropathies: what is the difference? Current Diabetes Reports. 2019;19(6):p. 32. doi: 10.1007/s11892-019-1150-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Richner M., Ferreira N., Dudele A., et al. Functional and structural changes of the blood-nerve-barrier in diabetic neuropathy. Frontiers in Neuroscience. 2018;12:p. 1038. doi: 10.3389/fnins.2018.01038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lin X., Xu L., Zhao D., Luo Z., Pan S. Correlation between serum uric acid and diabetic peripheral neuropathy in T2DM patients. Journal of the Neurological Sciences. 2018;385:78–82. doi: 10.1016/j.jns.2017.11.034. [DOI] [PubMed] [Google Scholar]
- 102.Yu S., Chen Y., Hou X., et al. Serum uric acid levels and diabetic peripheral neuropathy in type 2 diabetes: a systematic review and meta-analysis. Molecular Neurobiology. 2016;53(2):1045–1051. doi: 10.1007/s12035-014-9075-0. [DOI] [PubMed] [Google Scholar]