Abstract
We assessed the interference between vaginal ring use and menses among women who participated in the qualitative component of the MTN-020/ASPIRE vaginal ring trial in Malawi, South Africa, Uganda and Zimbabwe (N = 214). A common reason for imperfect ring adherence and premature removal of the vaginal ring cited by participants related to vaginal bleeding or menses. Whereas self-reporting via survey questions suggested that the majority (60%) of women did not mind wearing the ring while menstruating, and did not remove it (91%) during menses, in the qualitative interviews women frequently described removing the ring during menses. Their reasons included hygiene, beliefs that the ring blocked the flow of menstrual blood, fears that the ring would come out with blood or during tampon removal, and concerns around an ‘overburdened’ vagina. Examining women’s narratives and subjective experiences related to menstruation helps build a better understanding of factors affecting ring use and adherence.
Keywords: Vaginal ring, Adherence, Menses, Menstruation, HIV prevention, Hygiene
Introduction
In many parts of the world, menstrual blood is seen as a polluting ‘dirty’ substance, and menstruating women are socialised to feel dirty and unclean [1–5]. The purpose of menstruation is perceived to be the expulsion of old blood, and its unobstructed flow is seen as important for maintaining health [6, 7]. Literature from across sub-Saharan Africa describes strong social norms that underpin practices to maintain vaginal hygiene during menstruation; furthermore, vaginal cleansing during menstruation, in order to remove menstrual blood, is common [8]. Menstruation is shrouded in disgust and shame [4], and social norms inform women of the need to hide the sight and smell of menstrual blood, especially from males; dominant cultural discourses portray menstruation as a ‘hygienic crisis’ that needs to be managed and concealed [3, 9].
Fears around the blockage of menstrual blood, and beliefs around the need to shed menstrual blood in order to cleanse the body and maintain health have been shown to impact women’s willingness to use products that alter the menstrual cycle, such as hormonal contraceptives [9, 10]. In order for novel HIV prevention technologies, like the vaginal ring, to be acceptable to women, researchers need to understand how the use of such products may interfere with women’s existing vaginal practices, including menstrual hygiene management. In addition, women’s concerns around how such a product could affect their menses must be considered. In previous vaginal ring studies, menses-related reasons, such as the desire to clean the ring and/or vagina and fears of heavier bleeding, were amongst the most commonly cited reasons for ring removals and expulsions [11, 12].
The MTN-020/ASPIRE study was a randomized, placebo-controlled, Phase III trial that evaluated the safety and effectiveness of a monthly dapivirine vaginal ring for HIV prevention amongst 2629 women enrolled at 15 sites across Malawi, South Africa, Uganda and Zimbabwe [13]. Acceptability of the ring was assessed qualitatively in a subset of ASPIRE participants, and while the ring was well accepted overall, women described removing, rinsing or cleaning their rings due to menses, because they felt unclean, and due to perceived side effects of ring usage including malodour [14].
In this paper we further examine qualitative data from ASPIRE, exploring women’s narratives around menstruation, as well as the dynamic between vaginal ring use and menstrual practices and how it may have impacted adherence. Narratives such as those presented in this data enable us to build an understanding of women’s attitudes, perceptions and behaviours related to wearing the vaginal ring while menstruating, shedding light on the lived experience of ring usage amongst women in these sub-Saharan African locations.
Methods
Study Design
Participants in the ASPIRE trial (August 2012–June 2015) were randomized to receive either an active or placebo vaginal ring, and followed for ≥ 12 months [13]. The dapivirine rings (DR) were made from flexible, opaque, cured silicone and contained 25 mg of antiretroviral dapivirine. The placebo rings (PR), contained no active pharmaceutical ingredient, but were manufactured with the same components as the drug-containing rings, except for a colourant dispersed in the silicone for the purpose of maintaining blinded conditions. All women were given general instructions at their enrolment visit and as needed throughout the study, regarding correct vaginal ring use, including during menses, and in case the ring fell out or was removed. In particular, women were instructed to leave the ring inserted “all day, every day”, and were told that “the ring should be kept inserted at all times including during menses, bathing, and sex”. For vaginal cleansing, women were also instructed not to insert anything intravaginally, but told that they could clean the labia and the outer genitalia with water and soap. In order to allay fears around the ring interfering with menstruation, women were reassured by on-going counselling that the ring would not block their menstrual flow, and that they could continue using their usual menstrual management method, including tampons. At three time points during the ASPIRE trial (baseline, month-3 and product discontinuation), participants completed questionnaires administered by study personnel as well as by audio computer assisted self-interviewing (ACASI).
The qualitative component of the ASPIRE trial was conducted concomitantly to the main trial across four countries: Malawi, Zimbabwe, Uganda and South Africa. As previously described [14], 214 qualitative participants were recruited into one of three interview modalities: single (IDI) or serials (SIDI) in-depth interviews, or focus group discussion (FGD), with 280 interviews completed.
Interviews and FGDs followed semi-structured guides administered by trained social scientists in local languages. Topics in both IDIs and FGDs included perceptions of the ring’s effect on menses (and vice versa), perceptions of hygiene, cleanliness/dirtiness of the ring relating to use during menses, and preferences around use/non-use of ring during menses. In addition, once-off and serial IDIs explored personal experiences of ring use (including ring removal or expulsion) during menses, changes in menstrual management and other vaginal practices and their relation to the study or ring use, changes in menstrual symptoms or cycle and feelings about these changes.
Analysis
Audio-recordings of interviews and FGDs were transcribed and translated into English. Qualitative data was analysed thematically. A codebook was developed iteratively through a deductive and inductive process, and NVivo11 software was used for coding all transcripts. Inter-coder reliability of > 90% for key codes was maintained among 10% of interviews [14]. For this analysis, we extracted data coded with the pre-determined code MENSES, which had been applied to any transcript data relating to menses. Menses related data were then underwent a further process of iterative analysis, in which themes emerged inductively through multiple rounds of revisiting and reflecting on the data, looking for patterns and meanings in order to gain insight and a deeper understanding of the material [15].
English translations of direct quotations are indicated by italic text and used to illustrate the themes that arose in the qualitative data; quotations are accompanied by the participant’s pseudonym and country, the interview modality, and details of whether the participant was using a placebo ring (PR) or an active dapivirine ring (DR).
For comparison, we also present the qualitative participants’ self-reporting of ring use with menstruation by survey questionnaires. During the ACASI survey, women were asked whether the ring was removed in the past 3 months because of menses (response options: Yes/No/Did not have menses in past 3 months) and specifically, “did you mind wearing the ring during menses? (Yes/No/Did not wear the vaginal ring during menses/Did not have menses during the study)” Furthermore, in an interviewer-administered survey women were asked if they were worried about wearing the ring during menses (Yes/No). Response frequencies are summarized by study visit; Chi square tests were used to compare differences between countries.
The ASPIRE study protocol, including the qualitative component, was approved by each study site’s Institutional Review Boards and was overseen by the regulatory infrastructure of the US National Institute of Health and the Microbicide Trials Network. All participants provided written informed consent.
Results
The 214 women in the ASPIRE qualitative sample were aged between 18 and 42 (mean age of 26 years) and were followed for an average of 24 months (median 24.5, inter-quartile range 21–30 months). Several background characteristics, including education, marital status, and menstrual practices, differed significantly by country (Table 1). At enrolment, 12% (n = 25) indicated they had worries about wearing the ring during menses.
Table 1.
Baseline characteristics, attitudes and behaviours of qualitative participants in the ASPIRE trial (August 2012–June 2015)
| Malawi |
South Africa |
Uganda |
Zimbabwe |
Total |
p value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | ||
| 38 | (100) | 98 | (100) | 39 | (100) | 39 | (100) | 214 | (100) | ||
| Mean age, years (median, range) | 24.7 | (24, 18–32) | 25.6 | (25, 18–42) | 28.2 | (27, 18–42) | 28.6 | (27, 18–40) | 26.5 | (26, 18–42) | 0.001 |
| Parity > 0 | 38 | (100) | 95 | (97) | 39 | (100) | 39 | (100) | 211 | (99) | 0.31 |
| Currently married | 31 | (82) | 7 | (7) | 28 | (72) | 30 | (77) | 96 | (45) | < 0.001 |
| Completed secondary school | 3 | (8) | 48 | (49) | 1 | (3) | 18 | (46) | 70 | (33) | < 0.001 |
| Had a primary sex partner during the past 3 months | 38 | (100) | 98 | (100) | 39 | (100) | 38 | (97) | 213 | (100) | 0.21 |
| Had same primary partner for last 3 months | 36 | (95) | 96 | (98) | 37 | (95) | 37 | (97) | 206 | (97) | 0.70 |
| Primary partner HIV status | 0.01 | ||||||||||
| HIV Positive | 0 | (0) | 1 | (1) | 0 | (0) | 3 | (8) | 4 | (2) | |
| HIV Negative | 28 | (74) | 59 | (60) | 23 | (59) | 15 | (40) | 125 | (59) | |
| Don’t know | 10 | (26) | 38 | (39) | 16 | (41) | 20 | (53) | 84 | (39) | |
| Had any other sex partners in the past 3 months | 7 | (18) | 9 | (9) | 16 | (41) | 4 | (10) | 36 | (17) | < 0.001 |
| Condom used in the last act of vaginal sex | 10 | (26) | 57 | (58) | 14 | (36) | 20 | (51) | 101 | (47) | 0.005 |
| Menstruation in past 3 months | 32 | (84) | 68 | (69) | 34 | (87) | 36 | (92) | 170 | (79) | 0.01 |
| Vaginal practices to control menstrual bleeding, if menses in past 3 months | |||||||||||
| Tissue/toilet paper/cloth inside the vagina | 6 | (19) | 1 | (2) | 2 | (6) | 4 | (11) | 13 | (8) | 0.02 |
| Tissue/toilet paper/cloth in underwear | 22 | (69) | 1 | (2) | 13 | (38) | 8 | (22) | 44 | (26) | <0.001 |
| Tampon | 0 | (0) | 10 | (15) | 0 | (0) | 0 | (0) | 10 | (6) | 0.001 |
| Sanitary pad | 10 | (31) | 62 | (91) | 24 | (71) | 29 | (81) | 125 | (74) | < 0.001 |
| Worried about wearing ring during menses, at enrolment | 8 | (21) | 10 | (10) | 6 | (15) | 1 | (3) | 25 | (12) | 0.07 |
At the month-3 visit, 93% of women (191/205) reported via ACASI that they had used the ring in the past 3 months. Of those, 26% removed the ring at least once. More women in Uganda reported removal (40%, 14/35), and very few in Zimbabwe (6%, 2/33). Nine women (5%) disclosed they removed the ring because they “had or were expecting menses”; those who did were in South Africa (n = 5) or Uganda (n = 4), (Table 2). Overall, only 4% expressed worry about wearing the ring during menses.
Table 2.
Reported ring use within past 3 months by ACASI at the 3-month visit and at product use end visit, by country
| 3-Month |
Product use end visit |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Used ring | Removed ring at least once |
Removed ring because of menses |
Used ring | Removed ring at least once |
Removed ring because of menses |
|||||
| N | N | (R%) | N | (R%) | N | N | (R%) | N | (R%) | |
| Total | 191 | 50 | (26) | 9 | (5) | 178 | 25 | (14) | 4 | (2) |
| Malawi | 37 | 7 | (19) | 0 | (0) | 30 | 3 | (10) | 0 | (0) |
| South Africa | 86 | 27 | (31) | 5 | (6) | 78 | 11 | (14) | 3 | (4) |
| Uganda | 35 | 14 | (40) | 4 | (11) | 35 | 9 | (26) | 0 | (0) |
| Zimbabwe | 33 | 2 | (6) | 0 | (0) | 35 | 2 | (6) | 1 | (3) |
At the product discontinuation visit, 92% (178/193) of women reported using the ring in the past 3 months. The proportion reporting any removal decreased to 14%, with Uganda remaining the site with the highest reports (26%, 9/35). Four women stated that removal was because of menses (Table 2). Overall, 91% indicated that they wore the ring during menses. Of those, 40% (n = 70) replied affirmatively to the question “did you mind wearing the ring during menses?” More women in Uganda (92%) and Malawi (61%) said they minded compared to only 2% of Zimbabweans (p < 0.001, Fig. 1). There was no association between minding wearing the ring during menses and study arm (DR vs. PR), p = 0.86. Only 2 women (1%) reported that the ring ever came out on its own during menses.
Fig. 1.
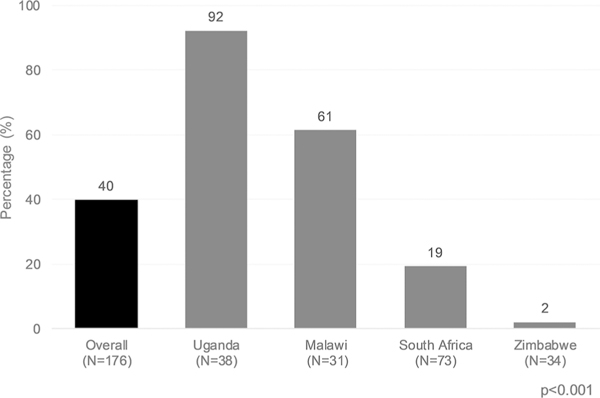
The proportion of the qualitative sample, overall and by country, who minded wearing the ring during menses during the ASPIRE trial (August 2012–June 2015)
Qualitative data revealed that while some women did not experience any issues wearing the ring during menses, others reported a variety of factors that contributed to menses-related ring removals, including concerns about menstrual blood flow blockage, malodour, pain or discomfort, or hygienic concerns. Other menses-related ring experiences highlighted from the qualitative data include narratives of ring expulsions during menses and the ring’s effect on menstrual management practices.
Ring Did Not Interfere with Menses
Through quantitative reporting, ring removal during menses was lowest amongst Zimbabwean women. Similar to reporting via ACASI, Zimbabwean women also described qualitatively that they did not mind wearing the ring during menses. Mudiwa articulated that she did not perceive the flow of menstrual blood to be affected by the ring: “you are not stopped from doing anything when you have inserted the ring… even menses, you will be having them… it doesn’t change anything… it will just be the same… you just have your menses as usual… it (blood) just flows like it should” (PR, SIDI, Harare, Zimbabwe). Although quantitative reporting of ring removal was higher amongst women from other sites, similar views on the ring’s non-interference with menses were also expressed qualitatively by some women in South Africa, Uganda and Malawi; for example by Bettina: “You do not feel anything even if you have the ring inserted during menses. you remain comfortable. It does not bring any changes, you remain as you would be if you did not have it” (PR, SIDI, Kampala, Uganda).
When asked to consider whether given the choice of leaving the ring in during menses, or removing it, Rufaro explained that there would be no reason to remove the ring during menses, as the ring caused her no discomfort: “I would choose to use the ring during menses… because I do not feel anything when I have the ring, whether I am not having menses or I am having menses… it does not… cause pain or prolong menses… (menses) is the same” (PR, SIDI, Harare, Zimbabwe). Similarly, Amahle explained that she never removed the ring during menses because the ring did not interfere with any of her body’s natural processes: “I have my normal periods… it (ring) does not interfere with anything, there is no change in my body or in my lifestyle because of the ring, it’s just like a natural thing” (PR, SIDI, Johannesburg, South Africa).
For those women who thought the ring should be kept inserted during menses, being at risk of contracting HIV was a key motivating factor, as described by Kudzai: “you may take it (ring) out during menses and then your partner might say he wants to have sex with you… so when you remove it, that is when you will get infected (with HIV)” (PR, SIDI, Harare, Zimbabwe). Several women in Malawi commented that the ring should not be removed during menses, to ensure that its protective properties were maintained. When asked her preference on whether she’d prefer to remove the ring during menses or not, Ujana explained that removing it would be counterproductive, at put her at risk: “I would prefer using the ring while in menses… the ring doesn’t affect menses… (and) if I remove it, the medication in the ring will not work as it was supposed to (protect from HIV), so it’s better to keep it inside” (PR, SIDI, Lilongwe, Malawi). Despite cultural prohibitions against having sex during menses, Telezi said that men sometimes forcibly have sex with a menstruating woman, and thus it would be important for her to be protected against HIV: “what would be the benefit of removing it (ring)… There are some men who force you to have sex with them while you are in menses, despite telling them it is not appropriate, they just force you… (if) you have removed the ring, there is that possibility of getting infected” (DR, SIDI, Lilongwe, Malawi).
Ring Interfered with Menses
In contrast to the views presented above, beliefs that the ring interfered with menses were salient at all the study sites. Although few women reported removing the ring because of menses via ACASI, in qualitative interviews women shared experiences of removing the ring because of perceived interference with menses.
Blockage of Menstrual Flow
Unlike the narratives from the Zimbabwean women described above, the belief that “the ring causes the blood to not come out” (FGD, Johannesburg, South Africa) was salient across all sites. One contributing factor to women’s concern about the ring causing blockages was their belief in the importance of expelling menstrual blood from the body to maintain health, as articulated by Nozipho: “if ever the menstruation does not come out it creates this big stomach and it affects the inside. you will feel pains” (DR, SIDI, Johannesburg, South Africa). The importance of unhindered blood flow being a reason for women removing the ring during menses was voiced by Funeka: “having blood which had stayed (blocked inside vagina) for weeks!…blood which is supposed to be out of my body is still staying in my body” (PR, SIDI, Johannesburg, South Africa). Miremba’s explanation for her light menstrual bleeding was that “the vaginal ring had blocked the passage. contributing to little blood flow” (DR, SIDI, Kampala, Uganda). Rudo interpreted her menstrual blood clots as a sign of the ring blocking blood flow: “the blood would come out with clots… I thought that maybe it (ring) is the one causing it. blocking the other blood” (DR, SIDI, Harare, Zimbabwe).
Releasing the obstructed blood flow was cited as a key reason why women removed the ring during menses, as Miremba described: “there was little blood coming out, so I got worried thinking maybe the vaginal ring had blocked the passage…(so) I removed it” (DR, SIDI, Kampala, Uganda). In a later interview Miremba explained candidly: “I thought the ring was blocking blood from flowing out. So I removed it, washed off the blood, and replaced (reinserted) it… so that blood flows out easily”. Likewise Chido described her removal of the ring to clean her vagina of blood clots and enable blood to flow freely: “I removed it (ring) because I wanted to thoroughly clean, to remove all the blood clots… the ring might have blocked some of the clots so I wanted to let all the blood come out” (DR, SIDI, Harare, Zimbabwe). Further, Buhle believed that the ring prolonged menses by blocking blood flow: “if I take it (ring) out then everything (blood) would just flow out quickly and finish… it blocks somewhere somehow… (blood) stays inside” (PR, SIDI, Johannesburg, South Africa).
Not all women shared the perception that the ring created blockages, some were of the view that menstrual blood continued “flowing out very well” (FGD, Kampala, Uganda). Mercy explained that wearing a vaginal ring “doesn’t change anything… you just have your menses as usual… it (blood) just flows like it should” (DR, SIDI, Harare, Zimbabwe). Aneni commented that as her blood flow was uninterrupted, she saw no reason to remove the ring: “it doesn’t affect anything. the blood comes out normally. So there is no need to remove the ring” (DR, SIDI, Harare, Zimbabwe).
Blood Discolouration
In addition to women’s concerns about the appearance and cleanliness of the ring on removal, the appearance of menstrual blood was also important. Women in South Africa spoke of the ring’s effect on changing the colour of their menstrual blood; Kholwa complained that the ring made her menstrual blood black: “the ring changes the colour of my menses, it is no longer red, it is now black. this ring makes menstruation black… I was scared of the black blood”‘ (PR, SIDI, Johannesburg, South Africa). Thabisa suggested that the blackness of her menstrual blood was caused by the chemicals in the ring: “my blood came out very thick and black… it was the ring… I don’t know how and I didn’t understand why. before I used the ring my blood was normal. maybe the ring that I was using had medication and somewhere somehow my body was reacting” (DR, SIDI, Johannesburg, South Africa).
Absorption of Menstrual Blood
Some women believed that the ring absorbed menstrual blood, causing abnormal flow or infection. Thandeka said “blood was not coming out, it felt like it (vagina) is closed. the blood was in the ring” (FGD, Johannesburg, South Africa). Njemile said that the ring became heavy from absorbing menstrual blood, and needed to be cleaned: “this ring felt heavy. so whenever I was having menses I was removing it. I felt more comfortable when I cleaned it and reinserted it” (PR, SIDI, Lilongwe, Malawi). The natural discolouring of the silicone vaginal ring with use, was seen as proof that it was absorbing blood, as Nandi explained in Zulu: “I thought that it (ring) consumes/eats (idla) my blood… when I removed it, it was red… my blood was getting absorbed by the ring” (PR, SIDI, Johannesburg, South Africa).
Smell
Linked to the perception of the ring absorbing menstrual blood, Sihle believed that this was the reason an unpleasant odour occurred when she removed the ring: “there was a bad smell… when the ring came out, that’s when the bad smell came. It was a strong smell… it was smelling because… the ring had absorbed the blood” (PR, SIDI, Durban, South Africa). Narratives associating an unpleasant odour during menses with ring use were common amongst women, most notably from South Africa and Zimbabwe. Zoliswa explained that the ring became malodourous “the ring smells bad… inside me it smells”, and caused a build up of residual blood which would come out as a thick substance, akin to having a miscarriage: “it (ring) keeps the dirt (menstrual blood) and after sometime when you are done (menstruating). something like mud which has a bad smell comes out… it feels like I’m having a miscarriage” (DR, SIDI, Durban, South Africa). Blood clots forming around the ring was also associated with malodour, as Onai explained: “when you come to remove it (ring) now, it would smell because the blood would have clotted on the ring” (FGD, Harare, Zimbabwe). The malodour issue, coupled with ring discolouration from menses and the perception that the ring was dirty, were amongst the reasons women gave for removing their rings to wash them. Not all women shared the view that the ring absorbed and retained blood, as evidenced by discolouration. For example Mariam perceived the ring to be self-cleaning: “the blood has a way of not sticking to it (ring). it cleans itself. Even when I was in my periods and removed it… I find it clean, not stained… even if you keep it inside during menses, you find it clean when you remove it” (DR, SIDI, Kampala, Uganda).
Pain
Women from all three South African study sites reportedly experienced unpleasant side effects from wearing the ring while menstruating. Lerato described increased menstrual cramping: “during menses I feel the pain… (cramping) is more painful now… I didn’t have this pain before I started using the ring” (PR, SIDI, Durban, South Africa). Sanele echoed this: “I had a lot of pains before and after my periods. after I started using the ring those pains were very hard (severe)” (DR, SIDI, Johannesburg, South Africa). Dumi believed that her period pains were due to the ring sitting in the uterus: “period pains are too much when you have that thing (ring)… very strong… which is why I keep asking if the ring sits in the womb… because really… those pains are unbearable” (DR, SIDI, Cape Town, South Africa).
In contrast to these views, there were also women at all the sites who said that they had not experienced any increase in period pains since using the ring. Nema articulated the view that period pains cannot be ascribed to ring use: “I usually have lower abdominal pains during my menses. I cannot say it is because of the ring” (DR, SIDI, Lilongwe, Malawi).
Discomfort
Discomfort was another theme that arose in women’s narratives about ring use during menses. Janet described experiencing vaginal itchiness during menses since using the ring: “before I started using the vaginal ring, I would not get itchy down in my private parts, but when I started using it, whenever I am approaching my periods, I feel itchy… I am even forced to scratch myself ‘ (PR, SIDI, Kampala, Uganda). Alleviating the itching was the reason Wadzai removed her ring: “I experienced itchiness during menses… the itching will be serious. when I removed the ring. I would feel that the itchiness became better ‘ (PR, SIDI, Harare, Zimbabwe).
Women, particularly in South Africa, suggested that inserting and wearing the ring during menses created additional discomfort at a time when their bodies are already uncomfortable, dealing with heavy blood flow and other menstrual symptoms. Siphiwe commented: “the ring was inside me but when… menstruating… I was uncomfortable… when I put it (ring) in… I was disgusted because the periods were heavy… the blood did not stop so I was like, ‘Argh! I still have to put in this ring as well’…but I am menstruating” (PR, SIDI, Cape Town, South Africa). Related to additional discomfort caused by the ring, several women in South Africa remarked on their feelings that using the ring, in combination with contraceptives and/or menstrual management products, meant that “there’s too much (in the vagina)” (PR, SIDI, Cape Town, South Africa). Phiwo ascribed her period pains to using the ring concurrently with tampons: “when I was on my periods, I had a lower back pain… I normally don’t experience that… when I menstruate I use tampons and I have the ring inside too, maybe that is why I have period pains” (DR, SIDI, Johannesburg, South Africa). Liyana, who used tampons and had an intrauterine contraceptive device (IUCD) fitted, said: “I sometimes feel loaded, and feel back pains. when I am in periods I feel that my body is loaded. all these things go through to my womb… my womb now feels like ‘no ways’… I have inserted the loop (IUCD) in my vagina, a Lillet (tampon)… and the ring also… my vagina was overloaded” (PR, SIDI, Johannesburg, South Africa). Dudu said that she would feel like a robot or a machine if she had so many foreign objects in her vagina at once: “I was concerned that Yhoo! I would be having many things in my vagina. I have the ring and the loop (IUCD). I am carrying a lot of things down there… like Terminator (robotic movie character)” (FGD, Johannesburg, South Africa).
Vaginal Hygiene and the Ring
Removing Ring for Cleansing
One of the most prominent themes in the qualitative data was the importance of maintaining a sense of hygiene during menses. Several women at the South African sites described feeling ‘unclean’; as articulated by Anathi: “I removed it (ring) and washed it because I felt dirty with it inside me” (FGD, Johannesburg, South Africa). The feeling of being unclean made Babalwa uncomfortable, as she expressed in isiXhosa: “the ring is making me feel uncomfortable… like I am not clean (andihlambanga)” (DR, SIDI, Cape Town, South Africa). The thought of the ring remaining dirty/bloody after the end of her period, made Velaphi feel disgusting: “you have your periods and after that you are clean. But that ring (is still dirty)?!… I removed the ring after menses… I brought it to the doctor and told them that I am feeling disgusted… because it wasn’t washed” (DR, SIDI, Johannesburg, South Africa).
With the ring inserted, many women felt it was not possible to maintain proper vaginal hygiene during menses, as Lindi voiced: “the ring becomes dirty because of the blood, and it irritates me that I cannot wash my vagina properly because of the ring” (DR, SIDI, Durban, South Africa). As such, women removed their rings to rid themselves of smell and ‘dirt’, as Nonki explained in isiXhosa: “that smell… in your menses you need to wash and insert your finger… if you have the ring you can’t wash your vagina properly… (during) heavy menstruation I take it out and rinse it… if I see that I am very dirty/unclean (ndingcolile kakhulu)” (DR, SIDI, Cape Town, South Africa). Although this theme was most salient amongst South African women, participants at other sites also complained that the ring made it difficult to attain desired hygiene standards, as Limbani explained: “during menses, this is the time a woman needs to bathe thoroughly… blood may get trapped on the ring, will I not smell?… when I expel clots, would these not get stuck?… a woman should remove the ring while in menses because of challenges to her cleanliness” (DR, SIDI, Lilongwe, Malawi).
Ring’s Interference with Vaginal Cleansing During Menses
As mentioned above, the insertion of a finger into the vagina was a commonly cited method for cleansing during menses by women at all sites. Thoko explained that it was necessary to clean blood clots from the vagina with a finger, especially when wearing the ring: “I expel many clots during menses… I insert fingers to remove the clots, which are stuck in the vagina, especially on the ring” (PR, SIDI, Lilongwe, Malawi). Some women reported that they had modified their usual vaginal cleansing practices during menses as a result of counselling they had received from study staff. Tasiya expressed frustration that she had been instructed to discontinue her usual vaginal cleansing practices: “during menses maybe some blood will remain behind… (but) the aunties (study staff) would say inserting fingers (into vagina) is not supposed to be done… something you are used to… you feel comfortable if you insert the finger, but now I was no longer clean like in the past” (PR, SIDI, Harare, Zimbabwe). The desire to feel clean led some women, especially in Uganda, to ignore instructions to restrain from inserting fingers inside their vaginas for cleaning, as described by Grace: “they prohibited us to wash inside the vagina… they told us not to wash inside even if it is during menses, but for me, I wash inside (anyway) to remove the blood’ (FGD, Kampala, Uganda).
Ring Expulsion During Menses
In addition to removals of the vaginal ring, unintentional expulsion of the ring during menses was also explored. At their last study visit, only 1% of women reported that the ring had ever come out during menses. However, in the qualitative data, a few women, most notably from Uganda, described experiences of the ring falling out during menses, for example while urinating, as Susan explained: “I never removed it (ring), but… it came out during menses… it came out on its own when I had gone to urinate” (PR, SIDI, Kampala, Uganda). Reme said her ring came out regularly during menses: “whenever I am in my periods it (ring) disturbs me… it slides out, I think because the uterus is soft… whenever I urinate the last bits of the urine has blood in it and you feel the ring wants to fall out” (DR, SIDI, Kampala, Uganda).
Ring’s Effect on Menstrual Management Practices
The majority of women in South Africa (62%), Uganda (71%), and Zimbabwe (81%) used sanitary pads for menstrual management; in Malawi the majority of women (69%) reported using tissue/toilet paper/cloth in their underwear. Tampon use was only reported by a minority (15%) of South African women (Table 1).
Women were also asked to qualitatively describe their menstrual management practices. Several South African women said that they believed the vaginal ring was incompatible with tampons, so elected to use sanitary pads instead. Phelisa experienced difficulty inserting tampons properly while wearing the ring, so reverted to using sanitary pads: “It was hard to get the tampon in… even if I am walking I have to keep fixing it (adjusting tampon)… so I use sanitary towels now… I don’t like the sanitary towel because it cuts (chafes)… (but) it’s best to use (with the ring)” (PR, SIDI, Cape Town, South Africa). Noxolo removed the ring during menses due to her worry that “the tampon would disturb the position of the ring… it made me feel uncomfortable, the tampon and the ring in the same place”. She spoke candidly about her removal of the ring during menses due to her fear that the ring would come out when she removed her tampon: “I would feel uncomfortable when I was pulling out a used tampon… scared that when you remove the tampon the ring will come out… So during my periods I used to remove it (ring). after menses you put it (ring) back” (DR, SIDI, Johannesburg, South Africa). A minority of tampon users, such as Olwethu, felt that wearing the ring concurrently with a tampon created no problems: “I don’t feel it (ring), I don’t feel that there is something inside… it was not disturbing me… a Lillet (tampon) is just the same as a penis, because the penis also goes in (while you’re wearing a ring)… it is not disturbing anything, and the Lillets are just the same. Even when you pull it (tampon) out when it is full, you don’t feel that there is something else (ring) inside, only a Lillet will come out” (PR, SIDI, Johannesburg, South Africa).
Discussion
The data presented in this paper comprise of quantitative reporting of ring use and removal, combined with qualitative data describing various aspects related to using or removing the vaginal ring during menses, amongst 214 women from Malawi, Zimbabwe, Uganda and South Africa who participated in the ASPIRE trial. Overall, at their product discontinuation visit, 40% of women reported quantitatively that they minded wearing the ring during menses, although this sentiment differed significantly by country. Similar country-specific sentiments regarding ring use during menses were reflected in qualitative interviews. However, qualitative findings diverged from quantitative results in reports of ring removal. Although by quantitative self-reports, fewer than 1 in 20 women reported removing the ring because of menses, in the intimate context of individual IDIs, women from all sites admitted to menses-related removals, suggesting ‘imperfect’ use. In addition to intentional ring removal, a few women described unintentional ring expulsion during menses and urination, a problem that has been described previously [16]. Similarly, in ACASI very few women reported removal or expulsion during menses.
In the qualitative data, the salient reasons cited for ring removal during menses were (1) fears that the ring blocked blood flow, (2) a desire to be hygienic/feel clean, and perceived interference of the ring with familiar hygienic/menstrual practices, and (3) a more minor theme which only occurred South Africa, the perception of vaginal ‘overload’ with concurrent tampon, IUCD and ring use. Amongst the narratives of interference, women listed several effects that the ring had on menses including increased cramping, heavier bleeding, and clotting. There were also reports that the ring made the vagina itchy and malodourous. There appeared to be no connection between women’s perceptions and experiences of blockage of or interference with menstrual flow based on whether women were using the dapivirine or placebo ring. Those women who expressed attitudes relating to the ring’s non-interference in menses were mainly due to the perception that the blood flow was not interrupted, and the ring was necessary for continuous protection against HIV.
Narratives around blood clots and blockage were a key theme in the ASPIRE qualitative data on menses amongst women in both the active and placebo ring groups. Women regarded ‘low blood flow’, prolonged menses, and blood clotting as proof that the ring was blocking menstrual blood, and voiced concerns that the ring interfered with the expulsion of dirty blood by blocking blood clots, or absorbing menstrual blood, as exemplified by the discolouration of the ring. Both placebo and active vaginal rings that women were using were made from silicone, which discolours with use; in a previous study women also viewed ring discolouration as a result of using the ring during menses [17]. Despite being provided with adherence counselling at each study visit during ASPIRE, which included specific advice that the ring would not block their menstrual flow, many women explained that they had removed their rings for this reason. Of importance to note is that while mechanistically the vaginal ring is unlikely to interfere with menstruation from a clinical point of view, women still may perceive that their menstrual flow was blocked. Women’s perceptions and feelings of having cramps or experiencing heaviness may be accentuated by the knowledge of wearing a ring. Understanding these perceptions is important and useful information for future implementation studies with the ring. Study counsellors were instructed and trained to invite the participant to share their experiences and not to accuse or shame the participants about anything they say.
The importance of flow was also evident in the narratives of those women who spoke positively of the ring; these women implied that as long as the ring did not obstruct the flow of menstrual blood, they had no issue keeping it inserted. Notions of the importance of the unobstructed flow of menstrual blood are evident in various settings, and understandings of illness are related to this flow being blocked [18]. In many societies in sub-Saharan Africa and elsewhere, the unhindered flow of menstrual blood is seen as important to rid the body of dirty blood, cleansing the womb, and maintaining good health [1, 6, 7, 9, 19]. The conception of flow and blockage has been written about within the context of the acceptability of HIV prevention products; Stadler and Saethre described this conception of good health being dependent on the maintenance of balance of substances within the body, through the flow of fluids which works to expel polluting substances [20].
During the study, women received instructions not to remove their vaginal rings at any time, including to wash it during menses, and to only clean their vulvas externally. In response to the framing of menstrual blood as a polluting and dirty substance (a second manuscript from the ASPIRE data reports on this) comes the desire to remove these dirty substances, and the engagement in practices to do so. Vaginal practices during menses, especially those related to cleansing and removing menstrual blood, are common across Africa [8]. Women engage in vaginal cleansing and menstrual management practices in order to maintain hygiene standards, and to control and contain the polluting menstrual blood [8]. Demonstrating the importance of vaginal hygiene, many women in ASPIRE said that in spite of the instructions they received around vaginal cleansing, they would insert a finger inside the vagina to remove clotted blood, to feel ‘clean’ and rid themselves of malodour. Several women suggested that it was only possible to thoroughly cleanse the vagina without the ring still inserted. Further, they spoke of their desire to remove the ring to enable them to wash thoroughly and remove any trace of menstrual blood, and if they were prevented from doing so, they felt unclean. Some expressed frustration about being told that they should discontinue their usual vaginal cleansing practices during menses because of study participation; they felt unclean and unsettled as a result of not being able to wash out menstrual blood in the manner they were accustomed to. Previous vaginal ring studies have also found that participants removed their rings during menses to periodically clean their vaginas, despite receiving instructions not to do so [11, 16]. Another study conducted in South Africa also found that women who were concerned around the ill effects of ‘dirty wombs’ and blocked menstrual blood, would engage in washing practices to expel and cleanse [10].
In South Africa where tampons are accessible, women were apprehensive about having an ‘overloaded vagina’ when using a vaginal ring in combination with an IUCD and/or a tampon. The majority of tampon users cited concurrent ring and tampon use as problematic; only one tampon user said she faced no challenges and felt no concern using the two products at the same time. American women in a vaginal ring study also expressed concern about the overcrowding of the vagina by using a tampon and a ring simultaneously, and a deterrent for use during menses. Like participants in ASPIRE, there was also concern about a tampon displacing the ring [12].
Limitations
Although reports of ring removal differed between qualitative and quantitative interviews, this misalignment of findings may have been contributable to the timing of the interviews. Specifically, through ACASI women were only asked about ring removal within the past 3 months at two time points (at the 3-month visit and product discontinuation visit); they were not asked if they had ever removed the ring because of menses. However, another possible reason for the misalignment could be that in the intimate setting of qualitative interviews, particularly serial interviews, women felt more comfortable speaking candidly about their removals and interference of the ring during menses. Serial interviews (multiple interviews over time) are known to be helpful in building rapport and eliciting more honest answers, which may counteract participants’ unwillingness to disclose undesirable behaviours, such as ring removals. Additionally, the use of serial interviews provides opportunity for participants to self-reflect on the motivations for their behaviours and decision making [21]. FGDs as a research methodology are used with the intention of promoting self-disclosure amongst respondents; however this is not always the case as some people may be reluctant to disclose personal information in a group situation, while others become more candid in the context of the anonymity afforded by the group setting, especially when others are disclosing similar sentiments [22]. One limitation of the method is that there may be a likelihood of more socially acceptable opinions dominating the discussion [23]. Despite enhanced confidentiality, social desirability bias may have influenced participants’ ACASI responses, particularly when reporting non-adherence to the study product [24, 25]. Regardless of reporting methods employed, participants may deliberately underreport behaviours that are undesirable [26].
Another limitation relates to the pain and discomfort that women experienced around menses. Participants were started on contraceptive methods at entry into the ASPIRE study, which may have resulted in changes in menstrual patterns and/or menstrual pain, and is likely to have impacted women’s experience of the using the vaginal ring, and confounded women’s perceptions of the ring’s interference with menses. In the next trial, REACH/MTN-034, (https://mtnstopshiv.org/research/studies/mtn-034), the possible confounding of contraceptive methods and vaginal ring was taken into account, and the study design includes a leadin period where new participants are put on contraceptives and only after 2 months, start using the dapivirine ring, to separate side effects of one versus the other.
Implications and Recommendations
Menstrual hygiene and management practices are shaped by cultural concepts of hygiene and sexuality that are also likely to affect the acceptability of microbicides inserted into the vagina [8]. As seen from this study, one salient factor to women removing the ring during menses was their concerns around blockage of blood. It is possible that for these women, the idea of having any product that stays inside the vagina will prompt fears of blockage. Although in ASPIRE, rings were well accepted [14], and adherence was generally high based on objective measures of use [13], such concerns from women about the product not fitting into their preferred hygienic and menstrual practices are valid and should be taken seriously, especially for future real-world use. Another major concern that women expressed related to the vaginal ring impeding their ability to maintain optimal vaginal hygiene, especially during menses, a time when the maintenance of hygiene is particularly important. As the data from this, and other studies show, women may decide to clean and/or remove a vaginal ring during or after menses, even if they receive instruction not to do so [12]. Notably, ASPIRE was a Phase III trial, and thus specific precautions were made to limit the chances of reducing effectiveness such as any removals or cleaning of the ring; as such, further research to understand ring use in a more real world setting is critical.
Removal of vaginal rings during menses has implications for the efficacy of and protection afforded by the ring. Concerns such as these would have to be addressed for optimizing the acceptability of a technology such as the vaginal ring; notably, the severity of these concerns appear to vary across settings and thus messaging would have to be contextualised. In future ring studies, more tailored counselling, targeted discussion during ‘adherence clubs’ and/or use of ring ‘ambassadors’ could enable women to understand that the ring does not hamper the flow of menstrual blood, helping to discourage removing the ring during menses.
However, it is also possible that the ring is not the right HIV prevention choice for certain women; thus, providing options is critical, so women can decide whether they prefer to use the ring or another HIV prevention product that fits better with her lifestyle [27]. The follow-up HIV Open-label Prevention Extension (HOPE/MTN-025) trial implemented this choice among ASPIRE participants (https://mtnstopshiv.org/research/studies/mtn-025), and preference for the vaginal ring versus oral PrEP will be formally assessed in the REACH/MTN-034 trial. Next generation HIV prevention products, including vaginal rings, should be designed with the recognition that they may be used imperfectly e.g. removed for variable time periods. Further research is warranted to define the limits of permissible removals [12] and to explore the implications of hygienic practices on ring effectiveness. Other suggestions to address women’s concerns may include the synchronisation of monthly replacements of the vaginal ring with menses, so that women would be issued with a clean ring after menses, or the development of a product that does not have to be worn during menses [17].
Conclusions
These narratives shed novel light on the lived experience of ring usage amongst women in these sub-Saharan African settings, enabling us to build an understanding of women’s attitudes, perceptions and behaviours relating to using the vaginal ring while menstruating. Removal of the ring during menses appear to have been more common than acknowledged in survey data and are important to consider in future real-world ring use settings. It also appears that existing menstrual management and hygiene practices may have led to imperfect ring use in ASPIRE, affecting women’s experiences of the ring. This could potentially compromise the ring’s real-world effectiveness, although the foregiveness of the dapivirine ring to short period removals is not currently known [12, 28]. Clearly, menstruation and menses related practices affect the acceptability of vaginal rings; therefore it is crucial to understand women’s experiences of using the vaginal ring while menstruating to better appreciate the impact of practices relating to ring removal, vaginal hygiene, and menstrual management on product dosing and real world effectiveness [8, 29]. This knowledge can help inform educational materials and messaging around the ring, and possibly the design and development of vaginal rings that can retain their efficacy and ability to deliver the active drug even with periodic removals and cleansing practices [30].
Acknowledgements
The study was designed and implemented by the Microbicide Trials Network (MTN) and funded by the National Institute of Allergy and Infectious Diseases (UM1AI068633, UM1AI068615, UM1AI106707), with co-funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Institute of Mental Health, all components of the U.S. National Institutes of Health (NIH). The work presented here was funded by NIH grants UM1AI068633. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The International Partnership for Microbicides (IPM) supplied the vaginal rings used in this study. Study Team Leadership Jared Baeten, University of Washington (Protocol Chair); Thesla Palanee-Phillips, Wits Reproductive Health and HIV Institute (Protocol Co-chair); Elizabeth Brown, Fred Hutchinson Cancer Research Center (Protocol Statistician); Lydia Soto-Torres, US National Institute of Allergy and Infectious Diseases (Medical Officer); Katie Schwartz, FHI 360 (Clinical Research Manager). Study sites and site Investigators of Record Malawi, Blantyre site (Johns Hopkins University, Queen Elizabeth Hospital): Bonus Maka-nani. Malawi, Lilongwe site (University of North Carolina, Chapel Hill): Francis Martinson. South Africa, Cape Town site (University of Cape Town): Linda-Gail Bekker. South Africa, Durban – Botha’s Hill, Chatsworth, Isipingo, Tongaat, Umkomaas, Verulam sites (South African Medical Research Council): Vaneshree Govender, Samantha Siva, Zakir Gaffoor, Logashvari Naidoo, Arendevi Pather, and Nitesha Jeenarain. South Africa, Durban, eThekwini site (Center for the AIDS Programme for Research in South Africa): Gonasagrie Nair. South Africa, Johannesburg site (Wits Reproductive Health and HIV Institute): Thesla Palanee-Phillips. Uganda, Kampala site (John Hopkins University, Makerere University): Flavia Matovu. Zimbabwe, Chitung-wiza, Seke South and Zengeza sites (University of Zimbabwe College of Health Sciences Clinical Trials Unit): Nyaradzo Mgodi. Zimbabwe, Harare, Spilhaus site (University of Zimbabwe College of Health Sciences Clinical Trials Unit):): Felix Mhlanga. Data management was provided by The Statistical Center for HIV/AIDS Research & Prevention (Fred Hutchinson Cancer Research Center, Seattle, WA) and site laboratory oversight was provided by the Microbicide Trials Network Laboratory Center (Pittsburgh, PA). For qualitative data, management was provided by the Women’s Global Health Imperative Program (RTI International, San Francisco, CA).
Funding The study was designed and implemented by the Microbicide Trials Network (MTN) and funded by the National Institute of Allergy and Infectious Diseases (UM1AI068633, UM1AI068615, UM1AI106707), with co-funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Institute of Mental Health, all components of the U.S. National Institutes of Health (NIH). The work presented here was funded by NIH Grants UM1AI068633.
The members of the MTN-020/ASPIREStudy Team are listed in the acknowledgments.
Footnotes
Compliance with Ethical Standards
Conflict of interest All author declares that they have no conflict of interest.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants included in the study.
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jewkes RK, Wood K. Problematizing pollution: dirty wombs, ritual pollution, and pathological processes. Med Anthropol. 1999;18(2):163–86. [Google Scholar]
- 2.Tamiru S, Mamo K, Acidria P, Mushi R, Ali CS, Ndebele L. Towards a sustainable solution for school menstrual hygiene management: cases of Ethiopia, Uganda, South-Sudan, Tanzania, and Zimbabwe. Waterlines. 2015;34(1):92–102. [Google Scholar]
- 3.Hawkey AJ, Ussher JM, Perz J, Metusela C. Experiences and constructions of menarche and menstruation among migrant and refugee women. Qualitative Health Research. 2017;27(10):1473–90. [DOI] [PubMed] [Google Scholar]
- 4.Johnston-Robledo I, Chrisler JC. The menstrual mark: menstruation as social stigma. Sex Roles. 2011;68(1–2):9–18. [PubMed] [Google Scholar]
- 5.Scheff TJ. Shame in self and society. Symb Inter. 2003;26(2):239–62. [Google Scholar]
- 6.Farage MA, Miller KW, Davis A. Cultural aspects of menstruation and menstrual hygiene in adolescents. Expert Rev Obstet Gynecol. 2011;6(2):127. [Google Scholar]
- 7.Laher F, Todd CS, Stibich MA, Phofa R, Behane X, Mohapi L, et al. Role of menstruation in contraceptive choice among HIV-infected women in Soweto, South Africa. Contraception. 2010;81(6):547–51. [DOI] [PubMed] [Google Scholar]
- 8.Allen CF, Desmond N, Chiduo B, Medard L, Lees SS, Vallely A, et al. Intravaginal and menstrual practices among women working in food and recreational facilities in Mwanza, Tanzania: implications for microbicide trials. AIDS Behav. 2010;14(5):1169–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scorgie F, Foster J, Stadler J, Phiri T, Hoppenjans L, Rees H, et al. “Bitten By Shyness”: menstrual hygiene management, sanitation, and the quest for privacy in South Africa. Med Anthropol. 2015;35(2):161–76. [DOI] [PubMed] [Google Scholar]
- 10.Wood K, Jewkes R. Blood blockages and scolding nurses: barriers to adolescent contraceptive use in South Africa. Reproductive Health Matters. 2006;14(27):109–18. [DOI] [PubMed] [Google Scholar]
- 11.Montgomery ET, van der Straten A, Cheng H, Wegner L, Masenga G, von Mollendorf C, et al. Vaginal ring adherence in Sub-Saharan Africa: expulsion, removal, and perfect use. AIDS Behav. 2012;16(7):1787–98. [DOI] [PubMed] [Google Scholar]
- 12.Watnick D, Keller MJ, Stein K, Bauman LJ. Acceptability of a ten-ofovir disoproxil fumarate vaginal ring for HIV prevention among women in New York City. AIDS Behav. 2017;22(2):421–36. [DOI] [PubMed] [Google Scholar]
- 13.Baeten JM, Palanee-Phillips T, Brown ER, Schwartz K, Soto-Torres LE, Govender V, et al. Use of a vaginal ring containing dapivirine for HIV-1 prevention in women. N Engl J Med. 2016;22:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Montgomery ET, van der Straten A, Chitukuta M, Reddy K, Woeber K, Atujuna M, et al. Acceptability and use of a dapivirine vaginal ring in a phase III trial. AIDS. 2017;31(8):1159–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Srivastava P, Hopwood N. A practical iterative framework for qualitative data analysis. Int J Qual Methods. 2009;8(1):76–84. [Google Scholar]
- 16.Nel A, Bekker L-G, Bukusi E, Hellström E, Kotze P, Louw C, et al. Safety, acceptability and adherence of dapivirine vaginal ring in a microbicide clinical trial conducted in multiple countries in Sub-Saharan Africa. PLoS ONE. 2016;11(3):e0147743–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van der Straten A, Panther L, Laborde N, Hoesley CJ, Cheng H, Husnik MJ, et al. Adherence and acceptability of a multidrug vaginal ring for HIV prevention in a phase i study in the United States. AIDS Behav. 2016;20(11):2644–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vallely A, Fitzgerald L, Fiya V, Aeno H, Kelly A, Sauk J, et al. Intravaginal practices and microbicide acceptability in Papua New Guinea: implications for HIV prevention in a moderate-prevalence setting. BMC Res Notes. 2012;5(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Green EC. Purity, pollution and the invisible snake in Southern Africa. Med Anthropol. 1996;17(1):83–100. [DOI] [PubMed] [Google Scholar]
- 20.Stadler J, Saethre E. Blockage and flow: intimate experiences of condoms and microbicides in a South African clinical trial. Culture Health Sex. 2011;13(1):31–44. [DOI] [PubMed] [Google Scholar]
- 21.Collumbien M, Busza J, Cleland J, Campbell O. Social science methods for research on sexual and reproductive health. Geneva. 2012;14:1–101. [Google Scholar]
- 22.Hollander JA. The social contexts of focus groups. J Contemp Ethnogr. 2004;33(5):602–37. [Google Scholar]
- 23.Using Smithson J. and analysing focus groups: limitations and possibilities. Int J Res Methodol. 2000;3(2):103–19. [Google Scholar]
- 24.Mensch BS, Hewett PC, Abbott S, Rankin J, Littlefield S, Ahmed K, et al. Assessing the reporting of adherence and sexual activity in a simulated microbicide trial in South Africa: an interview mode experiment using a placebo gel. AIDS Behav. 2011;15(2):407–21. [DOI] [PubMed] [Google Scholar]
- 25.Mensch BS, Richardson BA, Husnik M, Brown ER, Kiweewa FM, Mayo AJ, et al. Vaginal ring use in a phase 3 microbicide trial: a comparison of objective measures and self-reports of non-adherence in ASPIRE for the MTN-020/ASPIRE study team. AIDS Behav. 2018;23:504–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Turner AN, De Kock AE, Meehan-Ritter A, Blanchard K, Sebola MH, Hoosen AA, et al. Many vaginal microbicide trial participants acknowledged they had misreported sensitive sexual behavior in face-to-face interviews. J Clin Epidemiol. 2009;62(7):759–65. [DOI] [PubMed] [Google Scholar]
- 27.van der Straten A, Agot K, Ahmed K, Weinrib R, Browne EN, Manenzhe K, et al. The Tablets, Ring, Injections as Options (TRIO) study: what young African women chose and used for future HIV and pregnancy prevention. J Int AIDS Soc. 2018;21(3):e25094–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen BA, Panther L, Marzinke MA, Hendrix CW, Hoesley CJ, van der Straten A, et al. Phase 1 Safety, Pharmacokinetics, and Pharmacodynamics of Dapivirine and Maraviroc Vaginal Rings. JAIDS J Acquir Immune Defic Syndr. 2015;70(3):242–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gfos M, Pool R, Mzimela MA, Ndlovu HB, McCormack S, Elford J, et al. The Implications of Post-coital Intravaginal Cleansing for the Introduction of Vaginal Microbicides in South Africa. AIDS Behav. 2013;18(2):297–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morrow Guthrie K, Vargas S, Shaw JG, Rosen RK, van den Berg JJ, Kiser PF, et al. The promise of intravaginal rings for prevention: user perceptions of biomechanical properties and implications for prevention product development. PLoS ONE. 2015;10(12):e0145642–17. [DOI] [PMC free article] [PubMed] [Google Scholar]


