Abstract
Background:
The exchange of health information between primary care providers (PCPs) and surgeons is critical during transitions of care for older patients with multiple comorbidities, however, it is unknown to what extent this process occurs. This study was designed to characterize the extent to which factors associated with older patient’s recovery, such as functional status, cognitive status, social status, and emotional factors are shared among PCPs and surgical providers during care transitions.
Materials & Methods:
We prospectively identified 15 patients over 60-years with ≥3 comorbidities referred for general and vascular surgery procedures at a VA and academic medical center. Semi-structured Critical Decision Method (CDM) interviews were conducted with patients along with their surgical providers and referring PCPs. Thematic content analysis was performed independently by 5 reviewers on the cognitive processes associated with functional status, cognitive status, social status, and emotional factors. Interrater reliability between providers and patients was assessed using Cohen’s kappa.
Results:
47 CDM interviews were conducted, which included 20 paired interviews between a PCP and a surgeon and 16 paired interviews that involved a patient and a provider. The majority of patients reported experiencing poor information exchange between their PCP and surgeon (58%) and feeling they were primarily responsible for communicating their own health information during care transitions (67%). In paired interviews between PCPs and surgeons, there was nearly perfect agreement for the shared knowledge of cognitive (kappa: 0.83) and emotional (kappa 1) factors. In contrast, there was only minimal agreement for shared knowledge of functional status (kappa 0.38) and social status (kappa: 0.34).
Conclusions:
Information exchange between PCPs and surgical providers is often discordant during transitions of surgical care for medically complex older patients, particularly when it pertains to communicating their functional or social status.
Keywords: care transitions, surgery, primary care, functional status, cognitive status, social status, communication
INTRODUCTION
Transitions of care for older patients undergoing major surgery and specialty care procedures can be complex and require detailed communication and care coordination.[1, 2] This is particularly true for patients with multiple chronic medical conditions where it is critical that health information is accurately shared or communicated between their primary care provider (PCP) and their surgeon before and after the surgical procedure. The concept of shared or distributed cognition between healthcare providers refers to the manner in which patient’s health information is mentally organized, represented, and equally distributed between members of a healthcare team.[3] Failure to communicate effectively and share a sense of common ground regarding both responsibilities, expectations, and the care plan has been shown to result in poor coordination of care between inpatient and outpatient providers and may account for up to 80% of adverse events occurring in elderly patients with chronic medical conditions after hospital discharge.[4, 5] This in turn leads to higher rates of hospital readmission, emergency room visits, and healthcare utilization following major surgery.[6, 7]
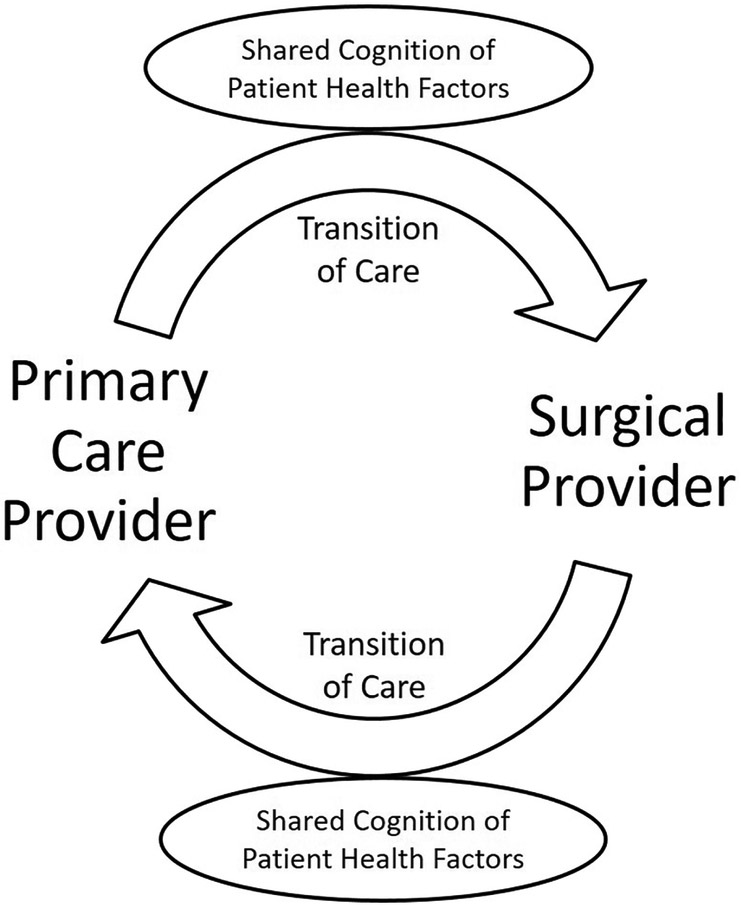
While the concept of shared cognition is known to be important for healthcare teams caring for common patients, it is not clear whether this process regularly occurs during transitions of care between PCP and surgical providers before and after surgery (Figure 1). In particular, it is unknown to what extent PCPs and surgical providers share comprehensive knowledge about a patient’s health status, including information about functional status, cognitive status, social status, and or emotional factors before and after a major surgical procedure. These health factors are important to communicate between inpatient and outpatient providers in addition to acute and chronic medical conditions because they may impact the ability of older patients to recovery from major surgery.[8, 9] However, the lack of time, failure to recognize the importance, and or inadequate means for communicating through electronic health record (EHR) systems between providers may limit shared cognition from occurring on a routine basis during surgical care transitions.
Figure 1.
Conceptual model of information exchange between primary care and surgical providers during transitions of surgical care
The objective of this study was to characterize the extent to which information regarding a medically complex older patient’s functional status, cognitive status, social status, and emotional factors are mutually shared among PCPs and surgical providers during transitions of surgical care. This was accomplished through a qualitative approach, which involved critical incident interviews with PCPs, surgical providers and patients to identify themes as well as to analyze the extent of agreement between different providers. We hypothesized that information exchange would be highly discordant between PCPs and surgical providers during transitions of surgical care.
METHODS
Study Design
Between September 2016 and August 2017, we performed a qualitative study consisting of semi-structured interviews using the Critical Decision Method (CDM), an adaptation of the Critical Incident Technique developed by Flanagan.[10] The CDM interviews were designed to enhance the understanding of issues surrounding knowledge (i.e. cognitive processing) and the exchange of information between primary care and surgical providers caring for older medically complex patients during transitions of surgical care (Table 1). This method emphasizes recall of specific patients and events and is particularly helpful in building the story. Interview techniques that ask about how work is done in general often lack the detail necessary to access shared mental representations of events. Medically complex older patients referred for surgery were first identified and then both paired and un-paired CDM interviews were conducted among the primary care and surgical providers that referred and evaluated the patient before and after surgery. Written informed consent was obtained from all participants. The study protocol and procedures were approved by the University of Utah Institutional Review Board and VA Research Review Committee.
Table 1.
Phases and Description of Techniques Used During Critical Decision Method Interviews of Primary Care and Surgical Providers
| Phase | Description of Technique |
|---|---|
| Incident Identification | Providers were asked to recall the older patient and their involvement with evaluating or managing the care of the patient before or after surgery. |
| Timeline Verification | Providers were asked to provide a concise overview of the episode of care, including transitions, and identify key events on the timeline. |
| Deepening into Key Events | Providers were asked to provide details about the patient’s health state during their last evaluation or encounter, including their in-depth knowledge of the patient’s functional status, cognitive status, and social status. |
| “What If” Questions | Providers were asked what if questions as implicit cues to help uncover their knowledge of the patient, and determine what information they thought would be important to communicate to different providers during the patient’s transition of care. |
Participants and Setting
We identified a purposive sample of 15 medically complex older patients along with their primary care and surgical providers from an academic medical center and an affiliated Veterans Administrative (VA) hospital located in the intermountain west. Patients were eligible for interview if they were older than 60 years of age, had been diagnosed with at least three or more chronic medical conditions, and had been referred by their PCP for either an elective general or vascular surgery procedure. We included PCP’s that specialized in either internal medicine or family practice, and had referred one of their patients for surgery and/or saw the patient in outpatient setting after surgery. Surgical providers included either general or vascular surgeons that were referred an eligible patient and or performed an operative procedure. Referring and consulting providers were excluded if they did not share the same EHR system for accessing patient health information. Both PCPs and surgical providers received an email about the study and indicated their willingness to participate after a brief phone call. All participants underwent informed consent before interviews were conducted. We determined a priori that at least 10 interviews among patients, PCPs and surgical providers would be a sufficient sample to reach saturation in thematic content based on criteria established for phenomenological studies. [11]
Critical Decision Method Interviews
A specific protocol was devised for CDM interviews involving PCPs, surgical providers and patients (See Appendix 1a, 1b, and 1c). These interview protocols, developed by 3 of the co-authors (BB, CW, and GDF), followed the CDM techniques for eliciting key information regarding functional status, social factors, and cognitive factors that would impact a patient’s ability to take care of themselves and recover after surgery (Table 1). The interviewer used a standard introduction and set of questions, along with additional prompts as the interviews progressed. Prior to conducting the interview, the PCP and surgical providers were asked to review the patient’s chart to improve recall. One pilot interview was conducted with a provider to ensure relevance and clarity. All interviews were conducted within 2 weeks of the patient’s clinic visit by two experienced qualitative interviewers (JB and SS) in a location of the participant’s choice (i.e. office or private room) and were recorded and transcribed with permission. Each interview lasted between 30-60 minutes.
Data Analysis
The CDM interviews were recorded, transcribed, and analyzed using a systematic content analysis approach previously described by Srnka et al. and Ely et al [12, 13]. The analysis was conducted in the 5 steps recommended by Srnka, et al: 1) Interview recording and transcription; 2) Unitization of de-identified transcripts to facilitate coding. Each unit comprised a few sentences to a few paragraphs that captured a specific component of functional, cognitive or social status information; 3) Inductive coding of health information according to the approach recommended by Patton.[14] Emergent codes were independently entered into a codebook in Atlas.ti (Scientific Software Development GmbH, Berlin), and constant comparison was used to compare early codes with those from subsequent interviews. The research team met frequently throughout the process to identify new codes, refine prior codes, and resolve disagreements through group consensus. To mitigate interpretative bias in the codes assigned for patient’s functional status, cognitive status, social status, and emotional factors, all disagreements in codes were discussed until consensus was achieved; 4) Organization of codes into higher level concepts and salient themes; and 5) Assessment of agreement of codes between providers and patients. Calculation of interrater reliability (IRR) using Cohen’s kappa was performed to determine the extent by which health factors were agreed upon by PCPs and surgical providers (IRR = number of health factor agreements between providers/number of agreements + disagreements between providers). Statistical analyses were done using Stata 14.0 (StataCorp, College Station, TX)
RESULTS
Out of the 15 identified cases, a total 12 (80%) medically complex patients over 60 years of age were interviewed along with 35 healthcare providers, including 16 (46%) PCPs that had referred patients’ for either general or vascular surgery procedures at either the VA medical center or the affiliated University hospital. Among 47 total interviews conducted, 20 (43%) were paired between a PCP and a surgeon who were caring for a mutual patient during a transition of care. This involved 8 paired interviews between providers at the VA medical center and 12 paired interviews among providers at the University hospital. Another 16 (34%) interviews were paired between a patient and a provider. The demographics of patients and the practice settings for interviewed providers is shown in Table 2.
Table 2.
Participating Patient and Provider Characteristics
| Patient Characteristics | N=12 |
|---|---|
| Age, Mean (SD) | 68.75 (5.49) |
| Male Gender, n (%) | 10 (83) |
| Caucasian Race, n (%) | 12 (100) |
| Type of Surgical Referral | |
| - General Surgery, n (%) | 1 (8) |
| - Vascular Surgery, n (%) | 11 (92) |
| Facility Where Surgical Care Received | |
| - Academic Medical Center, n (%) | 7 (58) |
| - VA Medical Center, n (%) | 5 (42) |
| Provider Characteristics | N = 35 |
| Medical Specialty | |
| - Primary Care Provider, n (%) | 16 (46) |
| - General Surgeon, n (%) | |
| - Vascular Surgeon, n (%) | |
| Facility Where Referral or Surgery Occurred | |
| - Academic Medical Center, n (%) | 27 (77) |
| - VA Medical Center, n (%) | 8 (23) |
The thematic analysis of CDM interviews between providers and patients resulted in the following themes:
1. Uncertainly regarding who should take primary responsibility for information exchange during transitions of care.
The responsibility for information exchange during transitions of surgical care differed among older patients and their healthcare providers. The majority of older medically complex patients (67% of respondents) reported that they felt primarily responsible for communicating their own health status to the PCP & surgeon, including information regarding functional status, social status, and cognitive status. In comparison, PCPs expected patients to simply convey the surgical episode occurrence and not provide any potentially relevant details concerning these health factors. Similarly, surgical providers felt that it was not the patients’ responsibility to facilitate the exchange of critical information with PCPs. One surgeon relayed, “I wouldn’t use patients as a method to relay anything important. For example, if a patient were to report to their PCP “I got my gallbladder out, that’s fine. But if they report I got my gallbladder out and by the way I have cancer, that would be something I would need to report directly to the PCP.” Another surgical provider commented, “I think it should be a shared responsibility – part of the responsibility lies with the patient in terms of communicating with the PCP, but we need to facilitate to the greatest extent that we can.”
2. Variability in modes of communication between providers during transitions of surgical care.
The modes for conveying information between healthcare providers varied during care transitions before and after surgery. Both PCPs and surgical providers used the EHR to access patient health information and view other provider notes, but some relied heavily on different forms of inter-professional communication if they felt that knowledge sharing was important for a given patient. There was variability in the modes that providers used, including electronic messaging, telephone conversations, paper letters, or face-to-face interactions. From the perspective of patients, nearly all expressed the expectation that his or her PCP and Surgeon had at least one direct conversation about them before and after the surgical procedure. One patient relayed, “Oh yeah, I expect they all have pow-wows...they all get together, discuss and figure out the best approach.” Another reported, “When they both have hands in the pie, they need to tell each other what the hell is going on.” Yet despite recognizing the importance of communication between providers during transitions of care, the majority of patients (58%) still reported that they had experienced or detected some aspect of poor or incomplete information exchange between their PCP & surgeon.
3. Lack of shared cognition between PCP and surgical providers for specific patient health information.
There was often discordance between PCPs and surgical providers’ in their shared knowledge about a patient’s health status during transitions of care. This was most perceptible when asking about a patient’s functional status or social status, but less so when inquiring about cognitive status and or emotional factors (Table 3 and 4). One PCP described a patient as being “very independent” and “her functional status seemed to be just fine” whereas the surgical provider described the patient as “pretty frail which is why we chose to do the procedure laparoscopically.” This level of discordance was also found when discussing patients’ social status (Table 4). Surgeons often made comments like “I don’t know about the patient’s support or home status”, whereas the PCP frequently had a detailed understanding of the patient’s social support. This included knowing who the patient’s caregivers were and whether family members were available to help with the patients’ care after surgery.
Table 3.
Agreement Among Providers for Shared Cognition of Different Types of Patient Health Information
| Content of Patient Health Information |
Definitions & Description | Cohen’s Kappa |
|---|---|---|
| Functional Status | A patient’s ability to perform daily activities required to meet basic needs and maintain health. This includes functional mobility to move around his or her environment to complete these activities. | 0.38 |
| Cognitive Status | A patient’s ability to remember, learn new things, concentrate and make decisions that affect their everyday life. | 0.83 |
| Social Status | A patient’s living environment outside of the hospital, including extent of support from caregivers and family members. This may be influenced by marital status, place of residence, income, employment, education, and religion. | 0.34 |
| Emotional Factors | A patient’s mental state that is associated with their mood, thoughts or feelings, behavioral responses, temperament, personality, and disposition. | 1.00 |
Table 4.
Representative quotations from Critical Decision Method interviews that illustrate discordance in assessment of functional status and social status between providers and patients during transitions of care.
| Functional Status | |
|---|---|
| Patient: “I go out to lunch with my friends and play tennis – I play quite well. I also take care of my grandkids and clean my house.” | Surgeon: “She has cancer and so she is pretty frail.” |
| PCP: “Her functional status seemed to be just fine. I don’t know any other specifics about her.” | Surgeon: “She is pretty frail which is why we chose to do this procedure laparoscopically.” |
| Social Status | |
| PCP: “He has a lot of social stuff going on.He has a lot of drama with his step-son who was recently kicked out of the house. And he is the primary caregiver for his wife.” | Patient: “My wife will take care of me. She will change my dressing but I generally keep track of myself.” |
| Surgeon: “I don’t know where the patient went after discharge. I don’t know about the patient’s support or home status. I would just be guessing based on his appearance and how well put together he was.” | PCP: “He was discharged to his home with home health and then had a follow up appointment with myself.” |
The degree of agreement among specific types of information exchanged between PCPs and surgical providers was further measured by paired interviews. As shown in Table 3, there was only minimal agreement for shared knowledge of a mutual patient’s functional status (kappa=0.38) and or social status (kappa=0.34). This discordance in information exchange for functional and social status factors was echoed by comments from PCPs, surgeons, and patients alike. In contrast, there was nearly perfect agreement for the shared knowledge of a patient’s cognitive status (kappa=0.83) and their emotional factors (kappa: 1.0).
DISCUSSION:
The transition of care before and after elective surgery for older patients often requires information exchange between a referring PCP and the surgical specialist. In this qualitative study, we found evidence of poor information exchange between PCPs and surgeon to some extent in over half of interviewed patients during transitions of surgical care. In terms of information domains, there was evidence of significant shared knowledge of patient’s cognitive and emotional factors, but in contrast, there was discordance among provider’s knowledge when it came to describing a patient’s functional and social status. The reason for these differences across domains is not clear, but could emerge from the mode by which social and functional information is recorded and shared. These data highlight the need for further research into this area in order to design improved methods to ensure that patient health information is communicated and understood by all providers caring for older medically complex patients during transitions of surgical care.
Communication between health care providers, commonly referred to as handoffs, denotes the transfer of care from one provider to another, and involve the explicit transfer of patients’ medical information and responsibility for patient care.[15] This process involves all types of transitions of care that occur within a hospital inpatient setting, as well as between providers in outpatient healthcare settings including primary care clinics and skilled nursing facilities (SNF). Prior work has shown that handoffs between providers are prone to miscommunication and errors during care transitions, particularly among older patients with multiple medical conditions and polypharmacy[16, 17] and those being discharged to SNFs [18]. This includes a high prevalence of unintended discontinuity of care as older patients transition to the outpatient settings, such as medications ordered by inpatient providers that were not continued after discharge.[19] These types of errors may even result when care expectations are documented in the EHR but not directly communicated between providers in different practice settings [2]. In cases where information is only documented in the EHR, there is limited opportunity to confirm whether expectations and knowledge about the patient has been adequately conveyed and understood during the handoff. Further, providers do not always read everything documented in the prior notes.
One of most common handoffs involves the information exchange between PCP and surgeon, with over 50 million episodes of surgical care in the United States annually [20, 21]. Prior efforts to explore handoffs during episodes of surgical care have focused primarily on provider communication occurring within the hospital during the perioperative period, including in the operating room [22-24] within the postoperative recovery unit [25], and within clinical units in the inpatient hospital setting [24, 26, 27]. Many of these studies have focused on interdisciplinary team handoffs or communication between providers with different levels of training and experience [24, 28]. And at least one recent study evaluated gaps in provider communication as patients experienced several transitions of care during a single surgical hospitalization [29]. However, this is the first study to evaluate the types of specific information gaps that exist between providers during inpatient and outpatient care transitions before or after surgery. Our findings highlight two important patient health factors – functional status and social status – where surgeons do not have a shared mental model or joint understanding with the referring PCPs or their own patients.
Understanding the functional, social, and or mental status of older surgical patients transitioned between PCP and surgical providers is important because these areas are crucial to recovery and deficits in this area may necessitate specific approaches to both clinical, custodial, and post-discharge care.[30] In particular, recognizing when patients have functional impairment or lack of social support provides surgeons information that may significantly impact clinical decision making, including the need to offer less invasive surgical procedures, increase involvement by family and caregivers, or order more home follow-up visits. Nevertheless, our study showed that there was very little evidence of shared knowledge between providers and their patients for these specific health factors. Reasons for a lack of communication in these domains may be related to the mode by which this class of information is usually recorded in the EMR and perhaps even by the role of the person who collects and records this class of data. The current national discussion on the difficulty and importance of identifying the social determinants of health in the EMR may relate to the findings in this study. (Hollister and Bonham) Our findings agree with prior work showing that clinical cognition rarely distributes equally among healthcare providers.[3, 31]
Several conceptual models have been proposed to try and better understand ways to improve shared cognition in medical decision making. One framework is known as the Decision Space Model, whereby healthcare providers depend on the patient for information about their health states and personal values.[3] In comparison, the joint cognitive system (JCS) considers the information space to be jointly held across healthcare providers and their artefacts as part of a larger system. rely upon each other for shared cognition, which is measured by goal alignment, control and co-agency. [32] To prevent gaps in shared cognition for complex patients, the JCS model emphasizes the use of information systems such as the EHR to organize knowledge, coordinate goals, and facilitate cognitive processing.
The potential for using health information technology (HIT) applications within EHR systems to improve the exchange of healthcare information has been recognized over the past decade.[33, 34] In particular, the use of software applications to facilitate provider communication has primarily focused on improving the transfer and exchange of discharge information. [35] Interventions such as computer-generated discharge summaries can standardize the information transferred to outpatient PCPs, facilitate timelier and more consistent follow-up care for referrals, and improve the quality of documentation. [36-38] However, existing HIT applications rely upon the one-way transfer of information, which does not allow inpatient and outpatient healthcare providers to know whether their clinical expectations and goals of patient care are aligned. Specifically, health information exchanged between referring PCPs and surgical specialists within current EHR platforms does not allow the feedback of shared knowledge to close the loop (Figure 1). New interoperable HIT applications are needed to permit a more dynamic exchange of information within the EHR and promote shared cognition.
There are several limitations to this study. To start, this study only sampled patients and providers at two geographically similar medical institutions in the intermountain west. While these hospitals serve patients in urban, rural, academic and community settings, there may be a sample bias and the responses from PCPs and surgical providers may not be generalizable to healthcare providers in other regions across the US. In addition, data collection was constrained to questions asked as part of the interview script during individual interviews. Second, we only included patients undergoing vascular and general surgery procedures, although the content of shared information should be universal for other surgical patient populations. Third, providers may have provided responses to questions during interviews that were affected by social desirability and recall bias. To minimize this, all interviews were conducted by non-medical staff in private office settings and we asked participants to review the medical chart before the interview. Fourth, demographic information was not collected on providers beyond their specialty and practice setting. Finally, no direct patient or provider participant observation took place and thus it is impossible to affirm the exact quality or content of information exchanged and how providers responded to each patient’s case.
CONCLUSIONS
Information exchange between PCPs and surgical providers during care transitions relies on extracting information from the patient and the EHR. These methods do not adequately support shared cognition when managing medically complex older patients, leading to fragmented care. Our study shows that information regarding a patient’s functional status and social status are specifically not often mutually shared or appreciated by providers caring for the same patient. These findings highlight the need for interoperable communication tools within the EHR to improve information exchange and support shared cognition during care transitions between different providers.
ACKNOWLEDGEMENTS
This work was supported by a grant from the National Institute of Aging (NIA), National Institutes of Health (1R03AG050884-01). The authors gratefully acknowledge the assistance of Elizabeth Turner for transcribing all 47 interview audio recordings.
Footnotes
Disclosure: The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Press MJ, Instant replay--a quarterback’s view of care coordination. N Engl J Med, 2014. 371(6): p. 489–91. [DOI] [PubMed] [Google Scholar]
- 2.Slager S, et al. , Information Exchange Between Providers During Transitions of Surgical Care: Communication, Documentation and Sometimes Both. Stud Health Technol Inform, 2017. 234: p. 303–308. [PMC free article] [PubMed] [Google Scholar]
- 3.Lippa KD, et al. , Navigating the Decision Space: Shared Medical Decision Making as Distributed Cognition. Qual Health Res, 2017. 27(7): p. 1035–1048. [DOI] [PubMed] [Google Scholar]
- 4.Giardina TD, et al. , Root cause analysis reports help identify common factors in delayed diagnosis and treatment of outpatients. Health Aff (Millwood), 2013. 32(8): p. 1368–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kripalani S, et al. , Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA, 2007. 297(8): p. 831–41. [DOI] [PubMed] [Google Scholar]
- 6.Acher AW, et al. , Improving Patient-Centered Transitional Care after Complex Abdominal Surgery. J Am Coll Surg, 2017. 225(2): p. 259–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boling PA, Care transitions and home health care. Clin Geriatr Med, 2009. 25(1): p. 135–48, viii. [DOI] [PubMed] [Google Scholar]
- 8.van Deudekom FJ, et al. , Functional and cognitive impairment, social environment, frailty and adverse health outcomes in older patients with head and neck cancer, a systematic review. Oral Oncol, 2017. 64: p. 27–36. [DOI] [PubMed] [Google Scholar]
- 9.Oresanya LB, Lyons WL, and Finlayson E, Preoperative assessment of the older patient: a narrative review. JAMA, 2014. 311(20): p. 2110–20. [DOI] [PubMed] [Google Scholar]
- 10.Flanagan JC, The critical incident technique. Psychol Bull, 1954. 51(4): p. 327–58. [DOI] [PubMed] [Google Scholar]
- 11.Morse JM, Analytic Strategies and Sample Size. Qual Health Res, 2015. 25(10): p. 1317–8. [DOI] [PubMed] [Google Scholar]
- 12.Srnka KJ and Koeszegi ST, From Words to Numbers: How to Transform Qualitative Data into Meaningful Quantitative Results. Schmalenbach Business Review, 2007. 59(1): p. 29–57. [Google Scholar]
- 13.Ely JW, et al. , Analysis of questions asked by family doctors regarding patient care. BMJ, 1999. 319(7206): p. 358–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.MQ P, Qualitative research and evaluation methods. 3rd ed. 2002, Thousand Oaks, CA: Sage Publications. [Google Scholar]
- 15.Abraham J, Kannampallil TG, and Patel VL, Bridging gaps in handoffs: a continuity of care based approach. J Biomed Inform, 2011. 45(2): p. 240–54. [DOI] [PubMed] [Google Scholar]
- 16.Loffler C, et al. , Optimizing polypharmacy among elderly hospital patients with chronic diseases--study protocol of the cluster randomized controlled POLITE-RCT trial. Implement Sci, 2014. 9: p. 151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leape LL, et al. , Systems analysis of adverse drug events. ADE Prevention Study Group. JAMA, 1995. 274(1): p. 35–43. [PubMed] [Google Scholar]
- 18.King BJ, et al. , The consequences of poor communication during transitions from hospital to skilled nursing facility: a qualitative study. J Am Geriatr Soc, 2013. 61(7): p. 1095–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moore C, et al. , Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med, 2003. 18(8): p. 646–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease Control. Web-based National Hospital Discharge Survey. 2014. [cited 2014 April 25].
- 21.Forrest CB, A typology of specialists’ clinical roles. Arch Intern Med, 2009. 169(11): p. 1062–8. [DOI] [PubMed] [Google Scholar]
- 22.Lingard L, et al. , Communication failures in the operating room: an observational classification of recurrent types and effects. Qual Saf Health Care, 2004. 13(5): p. 330–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lingard L, et al. , Team communications in the operating room: talk patterns, sites of tension, and implications for novices. Acad Med, 2002. 77(3): p. 232–7. [DOI] [PubMed] [Google Scholar]
- 24.Nagpal K, et al. , Information transfer and communication in surgery: a systematic review. Ann Surg, 2010. 252(2): p. 225–39. [DOI] [PubMed] [Google Scholar]
- 25.Anwari JS, Quality of handover to the postanaesthesia care unit nurse. Anaesthesia, 2002. 57(5): p. 488–93. [DOI] [PubMed] [Google Scholar]
- 26.Greenberg CC, et al. , Patterns of communication breakdowns resulting in injury to surgical patients. J Am Coll Surg, 2007. 204(4): p. 533–40. [DOI] [PubMed] [Google Scholar]
- 27.Mills P, Neily J, and Dunn E, Teamwork and communication in surgical teams: implications for patient safety. J Am Coll Surg, 2008. 206(1): p. 107–12. [DOI] [PubMed] [Google Scholar]
- 28.Williams RG, et al. , Surgeon information transfer and communication: factors affecting quality and efficiency of inpatient care. Ann Surg, 2007. 245(2): p. 159–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nagpal K, et al. , A systematic quantitative assessment of risks associated with poor communication in surgical care. Arch Surg, 2010. 145(6): p. 582–8. [DOI] [PubMed] [Google Scholar]
- 30.Boockvar KS, Fridman B, and Marturano C, Ineffective communication of mental status information during care transfer of older adults. J Gen Intern Med, 2005. 20(12): p. 1146–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Feufel MA, Robinson FE, and Shalin VL, The impact of medical record technologies on collaboration in emergency medicine. Int J Med Inform, 2011. 80(8): p. e85–95. [DOI] [PubMed] [Google Scholar]
- 32.Thraen I, et al. , Characterizing “information transfer” by using a Joint Cognitive Systems model to improve continuity of care in the aged. Int J Med Inform, 2012. 81(7): p. 435–41. [DOI] [PubMed] [Google Scholar]
- 33.Electronic tools for health information exchange: an evidence-based analysis. Ont Health Technol Assess Ser, 2013. 13(11): p. 1–76. [PMC free article] [PubMed] [Google Scholar]
- 34.Collier R, New tools to improve safety of electronic health records. CMAJ, 2014. 186(4): p. 251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Motamedi SM, et al. , The efficacy of computer-enabled discharge communication interventions: a systematic review. BMJ Qual Saf. 20(5): p. 403–15. [DOI] [PubMed] [Google Scholar]
- 36.Halasyamani L, et al. , Transition of care for hospitalized elderly patients-- development of a discharge checklist for hospitalists. J Hosp Med, 2006. 1(6): p. 354–60. [DOI] [PubMed] [Google Scholar]
- 37.Kripalani S, et al. , Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med, 2007. 2(5): p. 314–23. [DOI] [PubMed] [Google Scholar]
- 38.Reinke CE, et al. , Timeliness and quality of surgical discharge summaries after the implementation of an electronic format. Am J Surg, 2014. 207(1): p. 7–16. [DOI] [PubMed] [Google Scholar]