Abstract
Background
Thyroid cancer patients report unmet needs following diagnosis. However, little is known about their specific needs. Therefore, we sought to characterize the needs of patients with thyroid cancer prior to undergoing surgery.
Material and Methods
We conducted semi-structured interviews with 32 patients with papillary thyroid cancer following their preoperative surgical consultation. Data were analyzed using thematic content analysis.
Results
The central need of patients with thyroid cancer was a strong patient-surgeon relationship characterized by informational and emotional support, and respect for the patient as a person. Patients preferred disease and treatment related information to be individualized and to take into account aspects of their daily life. They wanted adequate time for asking questions with thoughtful answers tailored to their case. Patients additionally desired emotional support from the surgeon characterized by empathy and validation of their cancer experience. They particularly wanted surgeons to address their fears and anxiety. Patients also highly valued the surgeons’ ability to see beyond their disease and acknowledge them as a unique person with respect to their occupation, psychosocial state, and other individual characteristics. When surgeons met patients’ needs, they felt reassured, comfortable with their cancer diagnosis, and prepared for treatment. Suboptimal support increased patients’ anxiety particularly when they felt the surgeon minimized their concerns.
Conclusions and Relevance
Preoperatively, patients with thyroid cancer desire a strong patient-surgeon relationship. They rely on the surgeon to provide adequate informational and emotional support, and respect them as individuals. In turn, patients feel reassured and prepared for treatment.
Keywords: thyroid cancer, patient-doctor relationship, qualitative, reassurance, preoperative, cancer
Introduction
Over the last 30 years, the incidence of thyroid cancer has increased faster than other malignancy.1–4 As a result, thyroid cancer is now the most commonly diagnosed cancer in women ages 20 to 34.5 Most patients undergo a total thyroidectomy with or without a neck dissection and radioactive iodine ablation.6,7 These treatments lead to excellent long-term cancer outcomes for the vast majority of patients. As a result, the large pool of 800,000 thyroid cancer survivors continues to grow.8
Despite the effectiveness of treatment and excellent prognosis, thyroid cancer survivors have a reduced quality of life that is similar to or worse than those with more aggressive malignancies, such as breast or colon cancer.9–21 As a consequence, research largely focuses on survivorship. Similar to those with other cancers, patients with thyroid cancer are known to have significant unmet needs in the preoperative period.12,22–26 An international survey of over 2,300 thyroid cancer survivors found that fewer than 10% received psychological support at the time of diagnosis and less than 40% were provided clear written disease or treatment information.26 Nonetheless, little is known about patients’ specific needs and values prior to surgery.
We undertook this prospective study to better characterize the preoperative experience of patients with thyroid cancer. We utilized a qualitative approach to rigorously capture an in-depth understanding of what patients’ need and value in the preoperative period. Assessment of patients’ experiences in a prospective manner was critical to eliminating hindsight bias and reducing the effect of cognitive dissonance. By characterizing the experiences of patients’ with thyroid cancer, the results of this study will improve our ability to support these patients and likely those with other malignancies throughout their entire cancer treatment trajectory.
Materials and Methods
Design and Participant Recruitment
We performed semi-structured interviews with patients diagnosed with papillary thyroid cancer who were enrolled in a single-blinded, randomized clinical trial (RCT-Clinical Trial Registration Number NCT02138214; https://clinicaltrials.gov/ct2/show/NCT02138214). The interviews were a planned component of the RCT study design and data collection. The trial randomized patients to receiving or not receiving a prophylactic central neck dissection and assessed operative outcomes and patient experiences. We consented patients in clinic after meeting with their surgeon. Patients were eligible to participate if they were 18 years of age or older and had at least one thyroid nodule that measured ≥ 1cm with a cytologic or frozen section diagnosis of papillary thyroid cancer. Participants with lymph node metastases discovered pre- or intraoperatively were excluded. The University of Wisconsin-Madison Health Sciences Institutional Review Board approved this study.
Data Collection and Analysis
Interviews occurred between May 2014 and April 2016 after patients consulted with the surgeon and consented for the trial, but prior to surgical intervention and randomization. On average, 17 days elapsed between the time of consent and the interview (range 0 – 67 days). In the majority of cases, patients consented the same day as their consultation. Trained non-clinical research staff (n=9) interviewed all trial participants at a time and location convenient for the patient. Interviews lasted on average 1 hour (range 45 −120 minutes) and followed a piloted, semi-structured interview guide developed by the principal investigators (RSS, NC) in conjunction with a qualitative methodologist (CM). Interviews aimed to understand the preoperative experiences of patients with thyroid cancer. Questions probed about: (1) the patient’s diagnosis, (2) their experience with their surgeon, (3) advice they would give to the surgeon after the initial consultation, (3) advice they would give to a newly diagnosed patient, and (5) the effectiveness of communication with their care team. At the conclusion of each interview, participants completed a brief demographic survey and received $20. All interviews were transcribed verbatim and de-identified.
Four team members (RSS, NC, CM, JO) thematically analyzed a subset of interview transcripts (n=8) to develop an initial coding framework.27 After the open coding process, trained study team members coded all transcripts using NVivo software (QSR International, Victoria, Australia). A constant comparative method allowed us to continuously integrate emerging themes into the codebook and recode previously coded transcripts. Themes and coding structures were compared and discrepancies resolved by consensus. The overall inter-coder reliability of the trained coders was excellent (kappa >0.77).
After the open coding period, two members of the research team (SCP and EW) analyzed codes related to (1) communication, (2) barriers and facilitators of care, and (3) fear and anxiety to identify any patterns as part of the higher level analysis that aimed to characterize patients’ preoperative experience, focusing on their needs and values.27 Analysis continued until we reached saturation. The entire study team met regularly during this process to discuss the descriptive summaries and collaboratively develop a model that represents the patient experience and needs. Throughout this manuscript, participants are referred to by number to demonstrate the range of responses. For example, participant 8 is referred to as P-8.
Results
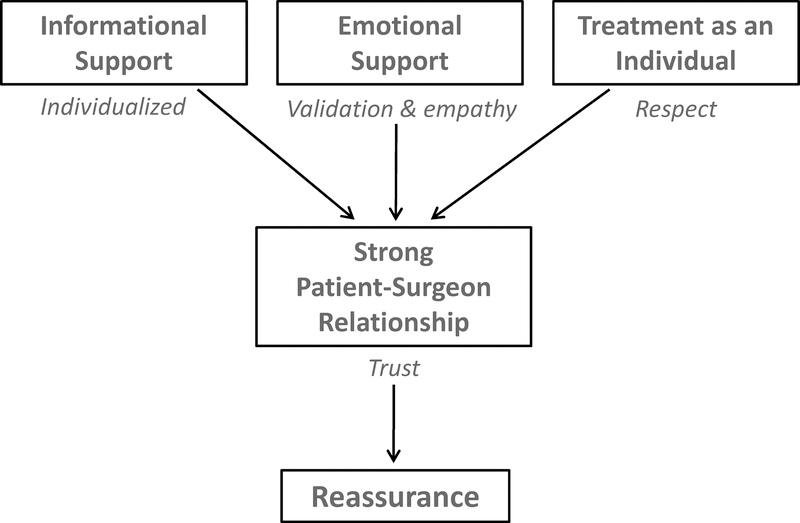
Of the 38 patients with papillary thyroid cancer who consented to participate in the trial, 32 participated in a semi-structured interview prior to undergoing surgery and are included in this analysis. Five patients withdrew from the trial prior completing an interview, and the audio-recording of one patient was unable to be transcribed and coded. These patients were seen by 7 surgeons. Table 1 presents the socio-demographic characteristics of the participants. The main theme that emerged was the need for a strong relationship with their surgeon that provides reassurance. Three key, interrelated parts of a successful patient-surgeon relationship included: (1) being provided adequate informational support, (2) receiving ample emotional support, and (3) being treated as an individual (Figure 1).
Table 1.
Participant Demographics and Clinical Characteristics (n=32)
| Characteristic | No. (%) |
|---|---|
| Age at consent, mean (SD), yrs | 47 (12) |
| Female | 24 (75) |
| Caucasian | 32 (100) |
| Education | |
| Some college/Associates degree graduates | 9 (28) |
| College graduate | 9 (28) |
| Graduate degree | 14 (44) |
| Currently employeda | 23 (82) |
| Marriedb | 21 (70) |
| Past surgeryc | 26 (87) |
| One or more chronic conditionsb | 16 (52) |
| Personal history of cancerc | 5 (16) |
| Family history of cancerc | 23 (74) |
| Incidentally discovered thyroid nodule | 9 (29) |
Four respondents did not provide the indicated information (n=28)
Two respondents did not provide the indicated information (n=30)
One respondent did not provide the indicated information (n=31)
Figure.
The central need of patients with thyroid cancer prior to surgery was a strong patient-surgeon relationship characterized by informational and emotional support as well as respect for the them as an individual. Development of a strong relationship provided patients with a profound sense of reassurance and adequately prepared them for surgery.
Informational Support
Thyroid cancer patients in this study strongly desired informational support from their surgeon at their initial consultation (Table 1). Participants wanted details about multiple aspects of their disease and treatment including: their diagnosis, prognosis, treatment options, details of the surgery, possible complications, the surgeon’s experience and complication rates, postoperative recovery, logistics related to their treatment and follow-up, and radioactive iodine (Table 2). Gaining knowledge from their surgeon about these aspects of the treatment continuum reassured and empowered participants, providing them with a greater sense of control. Participants also wanted their surgeon to provide information that was individualized and specific to their case. This finding was particularly pronounced in patients whose job involved using their voice professionally. Participant 16 exemplified this need by describing: “[My voice] is my big concern. It’s almost more of a concern than the cancer itself. And they talked about finding the vocal cord and getting it out of the way, so that was very reassuring. I felt instantly comfortable.”
Table 2.
Specific Needs of Patients with Thyroid cancer that Contribute to a Strong Patient-Surgeon Relationship and Reassurance
| Patient Need | Description | Exemplary Quotations |
|---|---|---|
| Informational Support | Patients desired information about all aspects of care from the diagnosis, treatment options, surgery, to postoperative care. Having knowledge eased patients’ worries and provided peace of mind, while a lack of information caused distress. Patients particulary appreciated having their questions answered. | “Telling me about surgery really helped me understand what was going to happen, and what was important to think about. I felt much more relaxed and less fearful.” (P-33) |
| “The surgeon went over all the options, and I was very comfortable for someone who was just told that they have cancer.” (P-23) | ||
| “I felt better after talking to [the surgeon], ‘cause s/he went into good detail, and went over everything.” (P-34) | ||
| “[The surgeon] said, 99% of the time the cancer would go to the lymph nodes first, and s/he didn’t see that, so that was reassuring.” (P-27) | ||
| “[The surgeon] was open to questions. Like, any question and wasn’t like, ‘Oh, don’t worry about it.’ S/he answered everything and wasn’t like, ‘alright, cancer, bye’. That wouldn’t be very good.” (P-21) | ||
| “Well, if I don’t do anything, will I die? Like [the surgeon] didn’t really explain what my options were, it was just like…let’s move this right along.” (P-29) | ||
| Emotional Support | Patients needed emotional support from the surgeon. Actions that were comforting to patients, included surgeons taking their time, listening, and providing general support. A lack of support was anxiety inducing for patients. While most patients wanted emotional support, a few did not. | “[The surgeon] was very caring and very professional, you know? So that made me feel less worried.” (P-6) |
| “The [surgeon] did a great job being thorough and sensitive and taking time to listen.” (P-13) | ||
| “I want them to say, ‘You’ll be just fine,’ because I want that reassurance in my brain, in my head, that I’ll be just fine.” (P-18) | ||
| “I was not impressed with [the surgeon’s] bedside manner. It lacked the compassion that I think you need to have with people that are dealing with such a tremendous diagnosis.” (P-20) | ||
| “They wanted to spend a lot of time explaining, discussing, and coddling. I’m not that kind of person.” (P-7) | ||
| Treatment as an Individual | Patients wanted to be seen as a unique person by the surgeon. They preferred a personalized approach taking into account specifics of their case. Not meeting this need was discounting. | “Make a relationship [with the surgeon] so that when they’re cutting your throat… you’re that individual and not, ‘the 8th patient we’ve done today.’” (P-9, giving advice to future patients) |
| “Statistically is a question that might not be concerning to you, but it’s still concerning to me, the patient.” (P-12, giving advice to the surgeon) | ||
| “Make sure whatever generalization you’re doing, it’s specific for what you’re seeing in this individual.” (P-16, giving advice to the surgeon) | ||
| “I didn’t really feel like I was the only patient. You know, you want to feel like they’re gonna take care of you, and I didn’t really get that feeling.” (P-20) |
P-#: Participant number
Another vital avenue for obtaining information came from participants being able to ask the surgeon questions. For example, when Participant 9 was asked about what advice s/he would give to a future patient, the advice was: “Learn everything that you can…get as much knowledge as you can…it comes back to being able to ask questions.” One participant appreciated having “time [before the consultation] to think of questions and read a little” (P-21), while another advised future patients to bring another person to the appointment who can think of other questions. When surgeons fully answered the questions, participants felt “comfortable” (P-6 and P-16), “confident” (P-6), “calmer” (P-21), “less unsettled” (P-9), and “ready to go” (P-23). However, when surgeons failed to adequately respond to questions, participants experienced increased worry and felt unsettled. For example, if a surgeon said, “Don’t worry about it” without providing additional information, participants felt “dismissed” (P-8) and “rushed” (P-21).
While participants strongly desired the surgeon to be the primary source of information, they did seek information from the internet and other medical professionals, such as primary care physicians and endocrinologists. When participants perceived that these outside sources were unreliable or false, they experienced increased anxiety. For example, Participant 28 stated, “When you Google ‘thyroid cancer’, the stuff you might come up with is, ‘You’re gonna have leukemia in 6 months!’”
Emotional Support
In addition to desiring informational support, patients sought direct emotional support from their surgeon. Expression of compassion and empathy by the surgeon was a critical source of reassurance (Table 2). Comments such as, “Almost certainly you’re not going to need any radiation or chemo...”, or, “You will be taking the thyroid hormone pill daily, and once we get that adjusted, you should be good to go” (P-3) reassured patients because they perceived their disease as less severe. By contrast, patients were distressed when they felt that the surgeon failed to offer an empathetic response (Table 2).
Participants also desired emotional support from the surgeon through validation of their cancer experience. Participant 16 articulated this point by saying, “Cancer is cancer. It’s hard to deal with. There’s such a glut of emotion. [The surgeon] was still very sensitive to the fact that, anytime you say cancer it freaks you out.” Despite the excellent prognosis of thyroid cancer and low likelihood of metastasis, the diagnosis elicited significant anxiety and fear from the “C-word.” Many participants feared poor outcomes, such as metastasis or death, especially if they had a long wait to see the surgeon or had a prior negative cancer-related experience. When surgeons directly addressed patients’ fears and provided emotional support, patients felt reassured. However, when a surgeon did not respond to emotional cues, participants felt, “shell-shocked” (P-21). Participant 18 described, “I feel horrible, because I’m worried about it. It’s all I think about!”
In addition to needing support related to their cancer diagnosis, participants desired reassurance from the surgeon about surgery and the postoperative period. Participants wanted the surgeon to address their anxiety about being “sliced and diced” (P-2), experiencing pain, having a noticeable scar, bleeding, and voice changes. However, not all patients experienced anxiety related to surgery and minimized the possibility of complications because they saw surgery as a necessary step to removing the cancer. Some participants had anxiety about the postoperative logistics of surgery, because their surgeon planned to send them home the same day. On the other hand, others were reassured that the procedure was performed on an outpatient basis.
The desire for emotional support from the surgeon was an overarching need of the patients with thyroid cancer, but intersected at times with their similar need for emotional support from external sources, such as family, other professionals, or survivors. One participant wanted their surgeon to assess how “solid” their external support system was (P-19). When discussing the impact of knowing or talking to a survivor, participants described feeling either reassured or anxious regardless if they were introduced to the survivor by the surgeon. For example, one participant was reassured, “because [the survivor] is still there” (P-29), while another expressed concerns that “everyone else’s little stories” (P-2) might increase their anxiety.
Treatment as an Individual
Patients with papillary thyroid cancer also desired their surgeon to see and treat them as an individual with unique traits, personalities, sources of happiness, and satisfactions (Table 2). Participants wanted surgeons to recognize the how the cancer diagnosis impacted their daily life, such as the need to miss school or work. This need for attention to individual characteristics was most pronounced in voice-dependent professionals, like singers and teachers, because of the risks of thyroidectomy related to the recurrent laryngeal nerve and resulting damage to their voice. Being treated as an individual by the surgeon was a significant source of reassurance. For example, Participant 16 stated, “[The surgeon]...was very aware and sensitive to my situation, um, and how I use my voice... and changed the conversation or the focus of the explanation to fit. … that was reassuring.” On the contrary, when participants did not feel as though they were being treated as individuals, this shortcoming undermined the patient-surgeon relationship (Table 2). Participant 8 gave the following advice to surgeons,“Don’t forget that you’re treating a patient. You’re not treating statistics. You’re not treating a disease. You’re treating a patient.”
The participants also expressed an appreciation for a bedside manner that respected them as individuals. Participants cited specific surgeon behaviors that engendered honesty and trust. For instance, surgeons provided reassurance or calmed patients through actions like eye contact, direct speech, humor, and being comfortable in the patient’s space. Participant 19 described this interaction by saying, “The [surgeon] looked directly at me, spoke directly to me, was comfortable in my body space. S/he wasn’t one of those doctors that push their chair back. S/he was comfortable.”
Discussion
The results of this study indicate that patients with papillary thyroid cancer strongly value the patient-surgeon relationship and want to be seen for who they are as a person and not just for their disease. These patients have substantial informational and emotional support needs that they prefer to be met by the surgeon and tailored to their case. When surgeons satisfy these needs, patients feel reassured, less anxious, and more positive about the treatment process and outcomes. These findings are important because they identify several areas where surgeons can improve the preoperative care of these cancer patients. To our knowledge, this study is the first prospective, qualitative evaluation of patients with thyroid cancer in the preoperative period.
One area for improvement lies within the patient-surgeon relationship and the opportunity to develop a strong connection. Strategies to strengthen the patient-surgeon bond and engender trust include enhancing surgeons’ communication skills, their ability to advocate for patients, their proficiency in eliciting patients’ preferences, and measurement of patient-centered outcomes.28–30 The need for a strong relationship with the treating clinician has been shown in patients with other malignancies. 31,32 Previously published data demonstrate that cancer patients who perceive a strong, positive relationship with their provider are more satisfied, have a better outlook on life, report higher decision quality, and may live longer.28,29,33–36 Alternatively, poor patient-provider communication can negatively influence patients’ psychosocial state, symptoms, treatment decisions, and quality of life.35 Because of the importance of the patient-surgeon communication and trust, quality improvement efforts need to ensure that we are adequately meeting patients needs starting from the initial consultation. To make progress in this area, measurement of patients’ perceptions of their preoperative experience will be critical for providing actionable feedback for providers.
Our results indicate that another area that warrants attention and can be improved is informational support in the preoperative period. We show that when patients’ information needs are satisfied, they feel reassured and confident. Patients also prefer the surgeon to be the primary source of information and want ample time to ask questions. This finding is consistent with Sawka et al. who revealed that physician counseling was the most important information source for patients with thyroid cancer postoperatively when discussing radioactive iodine.37 Studies of thyroid and other cancer survivors similarly show that being able to ask questions is crucial, but often is not possible due to time constraints.15,35,37–39. Ensuring that the information is individualized was a strong preference of our study participants which has also been shown in those with other cancers.40 Strategies to fill these information gaps include improving information materials, which may require including stakeholders in the design. Surgeons can also learn better assess patients’ informational needs and style of information seeking, which may not be overt, but hidden in statements about emotional concerns, such as “I am worried about the cancer spreading.”41 Additional research needs to identify the optimal content, context, and timing of information provision to be maximally effective keeping in mind that patients’ preferences for information differs.31 A multi-modality, team approach to meeting patients needs may enhance the experience of these and other patients.
Emotional support is the other key area that we identified as critical for patients with thyroid cancer in the preoperative period. Data in thyroid and other cancer survivors demonstrate that psychosocial and emotional support needs are often not met preoperatively.12,22−26 In addition, a lack of emotional support can result in erosion of trust in the physician, increased psychological distress, poor decision-making, dissatisfaction, and decreased quality of life.31,35,42,43 Research shows that physicians who express a higher level of empathy have a more accurate understanding of cancer patients’ unmet needs. This empathy also provides reassurance and non-abandonment when breaking bad news, decreases physiologic arousal, and improves both information recall and long-term satisfaction.28,44–48 Our results and those of others suggest that clinician can learn behaviors that improve this emotional support, such as eliciting and validating patients’ emotions, offering encouragement, avoiding interruptions, and allowing time for patients to discuss expectations and voice concerns.31 These actions improve emotional support and are critical to building trust within the patient-surgeon relationship. Our data suggest this emotional support should also be individualized and for those patients with thyroid cancer, the “good cancer” terminology should be avoided.49–51
While we identified several areas where we can improve the preoperative experience of patients with thyroid and likely other cancers, our study also has limitations. This investigation was performed at a single institution where the patient population is predominantly white and well-educated which may influence their needs and values. Patients with thyroid cancer in other cultural or geographical settings may have needs that we did not identify. Our study also did not include patients with microcarcinomas (≤1 cm thyroid cancers), indeterminate nodules, more advanced disease, or other thyroid cancer. These populations may have different reactions to their diagnosis or different cancer experiences. Therefore, further analysis is needed to determine if our findings are valid in these patient groups. Despite these weaknesses, similar prospective qualitative data in this or similar patient populations do not exist.
Conclusion
In summary, this study demonstrates that patients with thyroid cancer have a clear need for a strong patient-surgeon relationship, characterized by informational and emotional support as well as respect for the individual. When these needs were met, patients experienced a deep-seated sense of reassurance, whereas unmet needs increased worry and anxiety. Studies show that meeting patients’ needs improves communication and outcomes, including health-related quality of life. Because quality of life is an outcome known to be worse in patients with thyroid cancer compared to those with other more aggressive malignancies, further work in this area is necessary. In the early 1900’s, William Osler taught, “Care more for the individual patient than for the special features of the disease…Put yourself in his [or her] place…The kindly word, the cheerful greeting, the sympathetic look – these the patient understands.” Nearly 100 years later, a gap remains in providing patients with adequate support. This study highlights areas where we can improve the preoperative experience for patients with thyroid cancer, and likely other malignant diseases. We anticipate that increasing surgeons’ repertoire of skills in developing a robust patient-surgeon relationship will be critical to improving patient outcomes.
Acknowledgments
These data were presented at the 102nd Annual American College of Surgeons Meeting in Washington, DC on October 20th, 2016.
Funding Soures: This work was supported by the University of Wisconsin Carbone Cancer Center Support Grant P30 CA014520 and the National Cancer Institute of the National Institutes of Health (NIH) award number R01 CA176911. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. In addition, the NIH did not play a role in the design or conduct of the study; data collection, management, analysis or interpretation; manuscript preparation, review, or approval; and decision to submit the manuscript for publication. The Prinicipal Investigator/Senior Author had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Disclosures: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Davies L, Morris LG, Haymart M, et al. American Association of Clinical Endocrinologists and American College of Endocrinology Disease State Clinical Review: The Increasing Incidence of Thyroid Cancer. Endocrine practice : official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. 2015;21(6):686–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davies L, Welch HG. Current thyroid cancer trends in the United States. JAMA otolaryngology-- head & neck surgery. 2014;140(4):317–322. [DOI] [PubMed] [Google Scholar]
- 3.Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973–2006. JAMA : the journal of the American Medical Association. 2006;295(15):2164–2167. [DOI] [PubMed] [Google Scholar]
- 4.A Snap Shot of Thyroid Cancer: Incidence and Mortality. National Cancer Institute; [Webpage]. http://www.cancer.gov/research/progress/snapshots/thyroid. Accessed June 11, 2018. [Google Scholar]
- 5.American Cancer Society. Cancer Facts & Figures 2017. Atlanta: American Cancer Society; 2017. [Google Scholar]
- 6.Bilimoria KY, Bentrem DJ, Ko CY, et al. Extent of surgery affects survival for papillary thyroid cancer. Annals of surgery. 2007;246(3):375–381; discussion 381–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adam MA, Pura J, Gu L, et al. Extent of surgery for papillary thyroid cancer is not associated with survival: an analysis of 61,775 patients. Annals of surgery. 2014;260(4):601–605; discussion 605–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miller KD, Siegel RL, Lin CC, et al. Cancer treatment and survivorship statistics, 2016. CA: a cancer journal for clinicians. 2016;66(4):271–289. [DOI] [PubMed] [Google Scholar]
- 9.Applewhite MK, James BC, Kaplan SP, et al. Quality of Life in Thyroid Cancer is Similar to That of Other Cancers with Worse Survival. World journal of surgery. 2016;40(3):551–561. [DOI] [PubMed] [Google Scholar]
- 10.Husson O, Haak HR, Buffart LM, et al. Health-related quality of life and disease specific symptoms in long-term thyroid cancer survivors: a study from the population-based PROFILES registry. Acta oncologica. 2013;52(2):249–258. [DOI] [PubMed] [Google Scholar]
- 11.Husson O, Nieuwlaat WA, Oranje WA, Haak HR, van de Poll-Franse LV, Mols F. Fatigue among short- and long-term thyroid cancer survivors: results from the population-based PROFILES registry. Thyroid : official journal of the American Thyroid Association. 2013;23(10):1247–1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morley SGM. Support Needs and Survivorship Concerns of Thyroid Cancer Patients. Thyroid : official journal of the American Thyroid Association. 2015;25(6):649–656. [DOI] [PubMed] [Google Scholar]
- 13.van de Wal M, van de Poll-Franse L, Prins J, Gielissen M. Does fear of cancer recurrence differ between cancer types? A study from the population-based PROFILES registry. Psychooncology. 2016;25(7):772–778. [DOI] [PubMed] [Google Scholar]
- 14.Aschebrook-Kilfoy B, Schechter RB, Shih YC, et al. The clinical and economic burden of a sustained increase in thyroid cancer incidence. Cancer Epidemiol Biomarkers Prev. 2013;22(7):1252–1259. [DOI] [PubMed] [Google Scholar]
- 15.Singer S, Husson O, Tomaszewska IM, et al. Quality-of-Life Priorities in Patients with Thyroid Cancer: A Multinational European Organisation for Research and Treatment of Cancer Phase I Study. Thyroid : official journal of the American Thyroid Association. 2016;26(11):1605–1613. [DOI] [PubMed] [Google Scholar]
- 16.Gamper EM, Wintner LM, Rodrigues M, et al. Persistent quality of life impairments in differentiated thyroid cancer patients: results from a monitoring programme. European journal of nuclear medicine and molecular imaging. 2015;42(8):1179–1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singer S, Lincke T, Gamper E, et al. Quality of life in patients with thyroid cancer compared with the general population. Thyroid : official journal of the American Thyroid Association. 2012;22(2):117–124. [DOI] [PubMed] [Google Scholar]
- 18.Costa RV, Pakenham KI. Associations between benefit finding and adjustment outcomes in thyroid cancer. Psycho-oncology. 2012;21(7):737–744. [DOI] [PubMed] [Google Scholar]
- 19.Hoftijzer HC, Heemstra KA, Corssmit EP, van der Klaauw AA, Romijn JA, Smit JW. Quality of life in cured patients with differentiated thyroid carcinoma. The Journal of clinical endocrinology and metabolism. 2008;93(1):200–203. [DOI] [PubMed] [Google Scholar]
- 20.Tagay S, Herpertz S, Langkafel M, et al. Health-related Quality of Life, depression and anxiety in thyroid cancer patients. Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation. 2006;15(4):695–703. [DOI] [PubMed] [Google Scholar]
- 21.Tagay S, Herpertz S, Langkafel M, et al. Health-related quality of life, anxiety and depression in thyroid cancer patients under short-term hypothyroidism and TSH-suppressive levothyroxine treatment. European journal of endocrinology / European Federation of Endocrine Societies. 2005;153(6):755–763. [DOI] [PubMed] [Google Scholar]
- 22.Goldfarb M, Casillas J. Unmet information and support needs in newly diagnosed thyroid cancer: comparison of adolescents/young adults (AYA) and older patients. Journal of cancer survivorship : research and practice. 2014;8(3):394–401. [DOI] [PubMed] [Google Scholar]
- 23.Husson O, Mols F, Oranje WA, et al. Unmet information needs and impact of cancer in (long-term) thyroid cancer survivors: results of the PROFILES registry. Psycho-oncology. 2014;23(8):946–952. [DOI] [PubMed] [Google Scholar]
- 24.Sawka AM, Brierley JD, Tsang RW, Rotstein L, Ezzat S, Goldstein DP. Unmet Information Needs of Low-Risk Thyroid Cancer Survivors. Thyroid : official journal of the American Thyroid Association. 2016;26(3):474–475. [DOI] [PubMed] [Google Scholar]
- 25.Sawka AM, Ezzat S, Goldstein DP. Letter to the Editor: Exploring the Life Impact of Treated Low-Risk Thyroid Cancer. Endocrine Practice. 2016;22(4):513–514. [DOI] [PubMed] [Google Scholar]
- 26.Banache R, Bartes B, Farnell K, et al. Results of the Thyroid Cancer Alliance international patient/survivor survey: Psychosocial/informational support need, treatment side effects and international differences in care. Hormones. 2013;12(3):428–438. [DOI] [PubMed] [Google Scholar]
- 27.Charmaz K Constructing Grounded Theory: A Practical Guide Through Qualitative Analysis. London: Sage Publications LTD; 2006. [Google Scholar]
- 28.Weng HC, Steed JF, Yu SW, et al. The effect of surgeon empathy and emotional intelligence on patient satisfaction. Advances in health sciences education : theory and practice. 2011;16(5):591–600. [DOI] [PubMed] [Google Scholar]
- 29.Axelrod DA, Goold SD. Maintaining trust in the surgeon-patient relationship: Challenges for the new millennium. Archives of surgery. 2000;13:55–61. [DOI] [PubMed] [Google Scholar]
- 30.Kruser JM, Taylor LJ, Campbell TC, et al. “Best Case/Worst Case”: Training Surgeons to Use a Novel Communication Tool for High-Risk Acute Surgical Problems. Journal of pain and symptom management. 2017;53(4):711–719.e715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Epstein RM, Street RL. Patient-Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering. National Cancer Institute,. NIH Publication No. 07–6225.:Bethesda, MD, 2007. [Google Scholar]
- 32.Thorne SE, Kuo M, Armstrong EA, McPherson G, Harris SR, Hislop TG. ‘Being known’: patients’ perspectives of the dynamics of human connection in cancer care. Psycho-oncology. 2005;14(10):887–898; discussion 899–900. [DOI] [PubMed] [Google Scholar]
- 33.Martinez KA, Resnicow K, Williams GC, et al. Does physician communication style impact patient report of decision quality for breast cancer treatment? Patient education and counseling. 2016;99(12):1947–1954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Levinson W, Chaumeton N. Communication between surgeons and patients in routine office visits. Surgery. 1999;125(2):127–134. [PubMed] [Google Scholar]
- 35.Thorne SE, Bultz BD, Baile WF. Is there a cost to poor communication in cancer care?: a critical review of the literature. Psycho-oncology. 2005;14(10):875–884; discussion 885–876. [DOI] [PubMed] [Google Scholar]
- 36.Frenkel M, Engebretson JC, Gross S, et al. Exceptional patients and communication in cancer care-are we missing another survival factor? Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2016;24(10):4249–4255. [DOI] [PubMed] [Google Scholar]
- 37.Sawka AM, Straus S, Rodin G, et al. Thyroid cancer patient perceptions of radioactive iodine treatment choice: Follow-up from a decision-aid randomized trial. Cancer. 2015;121(20):3717–3726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Venetis MK, Robinson JD, Kearney T. Consulting with a surgeon before breast cancer surgery: patient question asking and satisfaction. Journal of health communication. 2013;18(8):943–959. [DOI] [PubMed] [Google Scholar]
- 39.Robinson JD, Hoover DR, Venetis MK, Kearney TJ, Street RL Jr. Consultations between patients with breast cancer and surgeons: a pathway from patient-centered communication to reduced hopelessness. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2013;31(3):351–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Davidson R, Mills ME. Cancer patients’ satisfaction with communication, information and quality of care in a UK region. European journal of cancer care. 2005;14(1):83–90. [DOI] [PubMed] [Google Scholar]
- 41.Korsvold L, Mellblom AV, Lie HC, Ruud E, Loge JH, Finset A. Patient-provider communication about the emotional cues and concerns of adolescent and young adult patients and their family members when receiving a diagnosis of cancer. Patient education and counseling. 2016;99(10):1576–1583. [DOI] [PubMed] [Google Scholar]
- 42.Bonito A, Horowitz N, McCorkle R, Chagpar AB. Do healthcare professionals discuss the emotional impact of cancer with patients? Psycho-oncology. 2013;22(9):2046–2050. [DOI] [PubMed] [Google Scholar]
- 43.Nelson JE, Gay EB, Berman AR, Powell CA, Salazar-Schicchi J, Wisnivesky JP. Patients rate physician communication about lung cancer. Cancer. 2011;117(22):5212–5220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sep MS, van Osch M, van Vliet LM, Smets EM, Bensing JM. The power of clinicians’ affective communication: how reassurance about non-abandonment can reduce patients’ physiological arousal and increase information recall in bad news consultations. An experimental study using analogue patients. Patient education and counseling. 2014;95(1):45–52. [DOI] [PubMed] [Google Scholar]
- 45.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne. 1995;152(9):1423–1433. [PMC free article] [PubMed] [Google Scholar]
- 46.Heyland DK, Allan DE, Rocker G, Dodek P, Pichora D, Gafni A. Discussing prognosis with patients and their families near the end of life: impact on satisfaction with end-of-life care. Open medicine : a peer-reviewed, independent, open-access journal. 2009;3(2):e101–110. [PMC free article] [PubMed] [Google Scholar]
- 47.Lelorain S, Bredart A, Dolbeault S, et al. How does a physician’s accurate understanding of a cancer patient’s unmet needs contribute to patient perception of physician empathy? Patient education and counseling. 2015;98(6):734–741. [DOI] [PubMed] [Google Scholar]
- 48.Lelorain S, Bredart A, Dolbeault S, Sultan S. A systematic review of the associations between empathy measures and patient outcomes in cancer care. Psycho-oncology. 2012;21(12):1255–1264. [DOI] [PubMed] [Google Scholar]
- 49.Gallop K, Kerr C, Simmons S, McIver B, Cohen EE. A qualitative evaluation of the validity of published health utilities and generic health utility measures for capturing health-related quality of life (HRQL) impact of differentiated thyroid cancer (DTC) at different treatment phases. Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation. 2015;24(2):325–338. [DOI] [PubMed] [Google Scholar]
- 50.Easley JMB, Robinson L. Its the “Good” Cancer, So Who Cares? Percieved Lack of Support_Among Young Thyroid Cancer Survivors. Oncology Nursing Forum. 2013;40(6):596–600. [DOI] [PubMed] [Google Scholar]
- 51.Randle RW, Bushman N, Orne J, et al. Papillary thyroid cancer: The good and the bad of the “good cancer”. Thyroid : official journal of the American Thyroid Association. 2017;In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]