Abstract
We herein report the case of a 62-year-old man diagnosed with Legionella pneumonia while engaged in recovery work in a flooded area after the Heavy Rain Event of July 2018 in Japan. The patient was intubated and maintained on mechanical ventilation and continuous hemodiafiltration. He was also administered antimicrobial therapy with ciprofloxacin and azithromycin. After 53 days in the hospital, he was discharged. It is important to recognize the risk of Legionella infection and to take measures to prevent it during recovery work that involves exposure to water and soil after a flood disaster.
Keywords: Legionella, pneumonia, heavy rain, flood, disaster
Introduction
During the Heavy Rain Event of July 2018 in Japan, torrential rains were recorded over a large part of the country, particularly in western Japan. This disaster resulted in 224 deaths, the complete destruction of 6,758 buildings, and flooding of 8,567 dwellings above the floor level (1). Numerous people were forced to live in shelters after the disaster. Such floods can potentially increase risks of contracting communicable diseases, such as water- and vector-borne diseases, as well as of drowning, injuries, trauma, and hypothermia (2).
Legionella bacteria are environmental organisms found in water, such as lakes, streams, artificial water reservoirs, and soil. Typically, they are transmitted to humans via the inhalation of water- or soil-derived aerosols and can cause fulminant pneumonia or mild Pontiac fever (3). Following the Great East Japan Earthquake and Tsunami in 2011, four cases of Legionella pneumonia were reported in people who had nearly drowned (4-6). Although seawater inhibits the growth of Legionella pneumophila (7), the tsunami deposit was speculated to contain river or brackish water soil, in which this bacterium can survive.
The risk of Legionella pneumonia may increase during floods; however, this risk during recovery work after a disaster has not been sufficiently discussed. We herein report a case of Legionella pneumonia in a man engaged in recovery work after the Heavy Rain Event of July 2018.
Case Report
The patient was a 62-year-old man who was temporarily employed in recovery work in a region (Mabi-cho, Kurashiki, Japan) where embankments of the Odagawa River and its tributaries broke, resulting in flooding of a large area. He removed rubble, earth, and sand and was exposed to a large amount of earth and sand dust each day. He wore an unwoven mask. He had not traveled to a hot spring before or during the recovery work. Several days after starting the work, he developed diarrhea, coughing, general fatigue, and a fever. At six days after the onset of symptoms, he visited a hospital, where he was treated with beta-lactam antibiotics. However, his condition worsened after four days, and he was transferred to the emergency room at our hospital because of severe dyspnea.
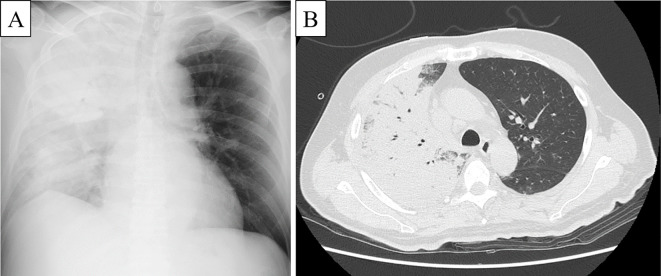
The patient was a former smoker (Brinkman index 50) and presented with a history of diabetes mellitus. A physical examination revealed a clear consciousness, high fever (37.7℃), tachycardia (128 bpm), normal blood pressure (102/67 mmHg), tachypnea (32 breaths per minute), and weak breath sounds in the right lung. His oxygen saturation measured by a pulse oximeter under the inhalation of oxygen at 10 L per minute was 80%. Laboratory tests revealed increased levels of leukocytes (17,700 /μL), neutrophils (16,992 /μL), HbA1c (7.1%); elevated serum levels of aspartic aminotransferase (133 IU/L), alanine transaminase (103 IU/L), lactate dehydrogenase (416 IU/L), blood urea nitrogen (69.4 mg/dL), creatinine (5.12 mg/dL), and C-reactive protein (36.02 mg/dL); and decreased serum levels of creatine kinase (68 U/L) and sodium (134 mEq/L). Chest X-ray showed consolidation in the right lung field, and computed tomography revealed consolidation with an air bronchogram in the right upper and middle lobes (Fig. 1). Gram staining of sputum and blood cultures was negative, but a urinary sample tested positive for Legionella, as assessed by ImmunocatchⓇ Legionella (Eiken Chemical, Tokyo, Japan); hence, Legionella pneumonia was diagnosed.
Figure 1.
Chest X-ray showed consolidation in the right lung field (A). Computed tomography revealed consolidation with an air bronchogram in the right upper and middle lobes (B).
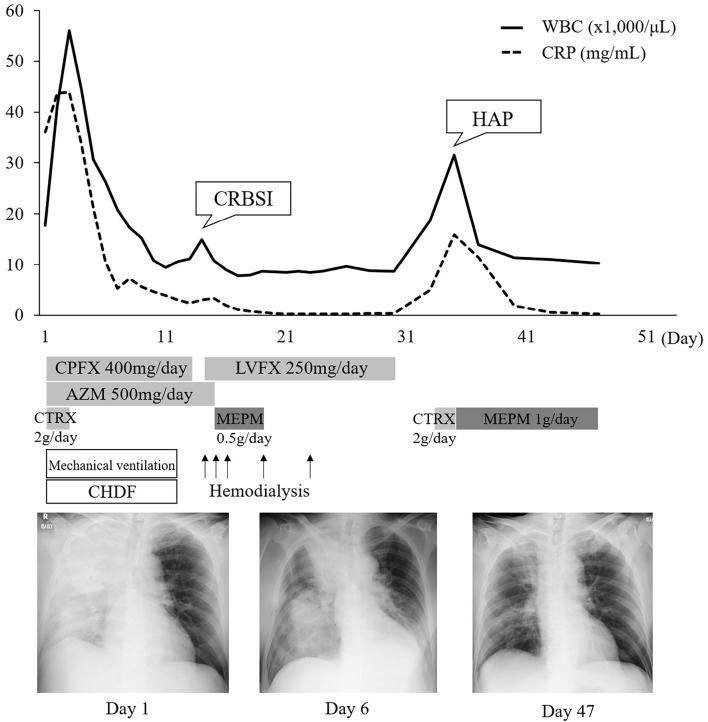
The patient was intubated and maintained on mechanical ventilation and continuous hemodiafiltration. He was also administered antimicrobial therapy with ciprofloxacin and azithromycin (Fig. 2). His respiratory condition and renal function gradually improved. He was extubated on day 12 and withdrawn from hemodialysis on day 23 of hospitalization. Antimicrobial treatment for Legionella pneumonia was administered for two weeks. However, the patient developed hemorrhagic gastric ulcer, catheter-related bloodstream infection by Acinetobacter baumannii, and hospital-acquired pneumonia, all of which were successfully resolved. His serum creatinine levels had improved to 1.36 mg/dL when he was discharged on day 53 of hospitalization.
Figure 2.
The clinical course. WBC: white blood cell count, CRP: C-reactive protein, CRBSI: catheter-related bloodstream infection, HAP: hospital-acquired pneumonia, CPFX: ciprofloxacin, LVFX: levofloxacin, AZM: azithromycin, CTRX: ceftriaxone, MEPM: meropenem, CHDF: continuous hemodiafiltration
Discussion
The rates of pneumonia incidence and pneumonia-related mortality increase in the event of a disaster (8-10). After the Great Hanshin-Awaji Earthquake in Japan in 1995, many people, mostly elderly, developed pneumonia because of the unhealthy conditions of the temporary shelters in which they stayed (shelter pneumonia) (11,12). Following the Great East Japan Earthquake and Tsunami in 2011, a high incidence of shelter pneumonia was again reported because of crowding, low temperatures, psychological stress, and a lack of medical supplies (8). In addition, many elderly people receiving care in nursing homes developed aspiration pneumonia because of the sudden change in their environment resulting from the disaster (9). Thus, most cases of disaster-related pneumonia are shelter pneumonia or aspiration pneumonia acquired in nursing homes.
In addition, disaster-related pneumonia includes cases occurring at the time of a disaster as well as during the subsequent recovery work. For instance, “tsunami lung” occurs in people who nearly drown during the acute phase of a tsunami. It is caused by the aspiration of water and soil containing microbes, such as Legionella, Escherichia coli, Pseudomonas aeruginosa, Stenotrophomonas maltophilia, Burkholderia cepacian, Scedosporium, and Aspergillus sp. (4-6,13). Three cases of Legionella pneumonia were reported during the decontamination work following the Fukushima Daiichi nuclear plant disaster (14). Decontamination work includes operations such as the removal of topsoil in mountainous areas and cleaning of roads and roofs of residential buildings with high-pressure water. Workers engaged in such tasks are frequently exposed to water and soil, and occupational environments with exposure to water and soil have been proposed to carry an increased risk of Legionella infection (15). Furthermore, people living in areas where Legionella longbeachae is commonly found in the soil, such as parts of Australia and New Zealand, should be educated regarding strategies to prevent inhalation of the organism when working with soil or compost (16), such as wearing mask and gloves, washing hands, avoiding touching the face when exposed to soil, or opening compost bags away from the face and keeping them close to the ground while carrying them. After a flood disaster, recovery workers exposed to soil should follow such recommendations in order to minimize the risk of infection.
In addition, some individuals may have risk factors for Legionella infection. The presence of a compromised immune system, diabetes mellitus, binge drinking, smoking, and age of more than 50 years old reportedly facilitates disease development (17). Our patient presented with several of these risk factors, including diabetes mellitus, smoking, and older age (62 years old). People engaged in recovery work after a disaster who are at an increased risk for Legionella infection should be particularly careful. In addition, medical staff should consider Legionella infection in patients exposed to water and soil. Legionella pneumonia can present with atypical symptoms, such as gastrointestinal symptoms, and a delayed diagnosis can be fatal (18).
Our patient presented with concomitant acute kidney injury. Rhabdomyolysis complicated by Legionella infection can induce renal dysfunction. In our patient, the serum creatine kinase level was not elevated, and there was no rhabdomyolysis; severe dehydration may therefore have caused his renal dysfunction. In a previous study, immunostaining revealed direct infection with Legionella bacteria in the renal tissue of a patient with tubulointerstitial nephritis (19). In our patient, because we did not perform a renal biopsy, direct infection with Legionella bacteria in the renal tissues could not be ruled out.
Fluoroquinolone or macrolide monotherapy is the standard treatment of Legionella pneumonia. According to a retrospective study examining the antimicrobial treatment of severe Legionella pneumonia, a combination therapy of fluoroquinolone and macrolide was administered to some patients, so this same approach was practiced in the present case (20). Combination therapy is considered a viable treatment option for severe Legionella pneumonia; however, the efficacy of combination therapy has not been examined in prospective studies, so further research is warranted.
In conclusion, we reported a case of Legionella pneumonia in a man exposed to soil and water while engaged in recovery work after the Heavy Rain Event of July 2018. In the wake of recent disasters in Japan, many volunteers with an unclear health status have been involved in the recovery work alongside employed workers. Therefore, it is important to spread awareness regarding risk of Legionella infection and strategies to prevent it when engaged in recovery work after a flood disaster, during which workers are exposed to water and soil.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Fire and Disaster Management Agency of the Ministry of Internal Affairs and Communications. About the heavy rain events of July 2018 (Version 58), 2018 (in Japanese) [Internet]. [cited 2019 Jan 5]. Available from: http://www.fdma.go.jp/bn/e53c0e191d5cc01960e336b73c502b0d1f33dacd.pdf
- 2. Gayer M, Connolly MA. Chapter 5: Communicable disease control after disasters. In: Public Health Consequences of Disasters. 2nd ed. Noji EK, Ed. Oxford University Press, Oxford, 2005(in revision). [Google Scholar]
- 3. Stout JE, Yu VL. Legionellosis. New Engl J Med 337: 682-687, 1997. [DOI] [PubMed] [Google Scholar]
- 4. Ebisawa K, Yamada N, Okada S, et al. Combined Legionella and Escherichia coli lung infection after a tsunami disaster. Intern Med 50: 2233-2236, 2011. [DOI] [PubMed] [Google Scholar]
- 5. Nakadate T, Nakamura Y, Yamauchii K, Endo S. Two cases of severe pneumonia after the 2011 Great East Japan Earthquake. Western Pac Surveill Response J 3: 67-70, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Inoue Y, Fujino Y, Onodera M, et al. Tsunami lung. J Anesth 26: 246-249, 2012. [DOI] [PubMed] [Google Scholar]
- 7. Tsuchiya Y, Terao M, Fujimoto T, Nakamura K, Yamamoto M. Effects of Japan Sea proper water on the growth of Legionella pneumophila, Escherichia coli, and Staphylococcus aureus. Environ Health Prev Med 10: 233-238, 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Daito H, Suzuki M, Shiihara J, et al. Impact of the Tohoku earthquake and tsunami on pneumonia hospitalisations and mortality among adults in northern Miyagi, Japan: a multicentre observational study. Thorax 68: 544-550, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yamanda S, Hanagama M, Kobayashi S, et al. The impact of the 2011 Great East Japan Earthquake on hospitalisation for respiratory disease in a rapidly aging society: a retrospective descriptive and cross-sectional study at the disaster base hospital in Ishinomaki. BMJ Open 3: e000865, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Shibata Y, Ojima T, Tomata Y, et al. Characteristics of pneumonia deaths after an earthquake and tsunami: an ecological study of 5.7 million participants in 131 municipalities, Japan. BMJ Open 6: e009190, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Osaki Y, Minowa M. Factors associated with earthquake deaths in the great Hanshin-Awaji earthquake, 1995. Am J Epidemiol 153: 153-156, 2001. [DOI] [PubMed] [Google Scholar]
- 12. Takakura R, Himeno S, Kanayama Y, et al. Follow-up after the Hanshin-Awaji earthquake: diverse influences on pneumonia, bronchial asthma, peptic ulcer and diabetes mellitus. Intern Med 36: 87-91, 1997. [DOI] [PubMed] [Google Scholar]
- 13. Kawakami Y, Tagami T, Kusakabe T, et al. Disseminated aspergillosis associated with tsunami lung. Respir Care 57: 1674-1678, 2012. [DOI] [PubMed] [Google Scholar]
- 14. Sawano T, Tsubokura M, Ozaki A, Leppold C, Kato S, Kambe T. Legionnaires' disease as an occupational risk related to decontamination work after the Fukushima nuclear disaster: a case report. J Occup Health 60: 271-274, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Principe L, Tomao P, Visca P. Legionellosis in the occupational setting. Environmental Research 152: 485-495, 2017. [DOI] [PubMed] [Google Scholar]
- 16. Kenagy E, Priest PC, Cameron CM, et al. Risk factors for Legionella longbeachae Legionnaires' disease, New Zealand. Emerg Infect Dis 23: 1148-1154, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ginevra C, Duclos A, Vanhems P, et al. Host-related risk factors and clinical features of community-acquired legionnaires disease due to the Paris and Lorraine endemic strains, 1998-2007, France. Clin Infect Dis 49: 184-191, 2009. [DOI] [PubMed] [Google Scholar]
- 18. Sopena N, Sabrià-Leal M, Pedro-Botet ML, et al. Comparative study of the clinical presentation of Legionella pneumonia and other community-acquired pneumonias. Chest 113: 1195-1200, 1998. [DOI] [PubMed] [Google Scholar]
- 19. Shah A, Check F, Baskin S, Reyman T, Menard R. Legionnaires' disease and acute renal failure: case report and review. Clin Infect Dis 14: 204-207, 1992. [DOI] [PubMed] [Google Scholar]
- 20. Cecchini J, Tuffet S, Sonneville R, et al. Antimicrobial strategy for severe community-acquired legionnaires'disease: a multicentre retrospective observational study. J Antimicrob Chemother 72: 1502-1509, 2017. [DOI] [PubMed] [Google Scholar]