Abstract
Background:
Although there is evidence for heightened sexually transmitted disease (STD) acquisition among women who experienced sexual violence, little is known about their patterns of STD testing, STD diagnosis, and STD treatment.
Methods:
Data was drawn from cycle eight of the National Survey of Family Growth (2011–2013). Logistic regression analyses used SUDAAN to examine the link between forced sex and risky sexual behavior as well as forced sex and STD testing, diagnoses, treatment, and connection to care.
Results:
Women who experienced forced sex were more likely to have risky sex (adjusted odds ratio [AOR], 1.56; 95% confidence interval [CI], 1.08–2.24), risky partners (AOR, 1.90; 95% CI, 1.11–3.23), and report substance abuse (AOR, 1.80; 95% CI, 1.28–2.53) than women who never experienced forced sex. Women who reported forced sex were more likely to be tested for an STD (AOR, 1.67; 95% CI, 1.34–2.09), and be diagnosed with herpes (AOR, 1.94; 95% CI, 1.13–3.32), genital warts (AOR, 2.55; 95% CI, 1.90–3.41), and chlamydia (AOR, 1.83; 95% CI, 1.03–3.25) than those who have never had forced sex. Results indicated a direct relationship between particular STD diagnoses and treatment in the past 12 months (AOR, 6.81; 95% CI, 4.50–10.31). Further analyses indicate that forced sex moderated the link between STD diagnoses and STD treatment (AOR, 0.43; 95% CI, 0.19–0.98).
Conclusions:
Results indicate that women who reported experiencing forced sex were more likely to be diagnosed with chlamydia, herpes, and genital warts than women who never had forced sex. There may be a need to pay particular attention to women who experienced forced sex and a history of STDs to ensure that they are retained in care.
Sexually transmitted diseases (STDs) are a major public health concern in the United States, especially among women, who disproportionately experience long-term consequences of STD acquisition and transmission.1,2 A growing body of evidence suggests that women who have experienced sexual violence may be more vulnerable to STDs than women who have not experienced sexual violence.3–5 Sexual violence has been defined as a sexual act that is committed or attempted by another person without freely given consent of the victim or against someone who is unable to consent or refuse.6 Current estimates indicate that nearly 1 in 5 women in the United States will report experiencing rape at some time in their lives.7 Though sexual violence and STD acquisition are intersecting public health issues, they have most often been examined and addressed in isolation using discrete intervention and prevention approaches.8
There are multiple pathways which link women who have experienced sexual violence to STDs.9,10 For example, women victimized by sexual violence may have experienced high-risk sex, such as forced anal sex, and physical trauma makes one increasingly vulnerable to STD acquisition.11 Women in a relationship characterized by sexual violence may lack the power and resources to negotiate condom use, resulting in sex without condoms.12,13 Lastly, women with a history of sexual violence may engage in elevated levels of sexual risk taking, which can increase vulnerability to STDs over time.14,15 Data from emergency rooms, STD clinics, prenatal care settings and national data indicate that sexual violence is a critical risk factor for STD acquisition.16–20
Despite this evidence for heightened STD risk among women who have experienced sexual violence, relatively little is known about their patterns of STD testing, STD diagnosis, and STD treatment.21 Studies have previously examined the connection to STD services as a direct aftermath of a sexual assault episode, but less is known about the extent to which women with a history of sexual violence are connected to STD care or their relationship to the health care system.22,23 Scant research has explored the extent to which those who have experienced sexual violence are engaged in sexual health care, and whether they are retained in care if they are found to be at high-risk for STD acquisition. We seek to understand if a history of sexual violence moderates or attenuates the link between STD diagnoses and STD treatment. Are women who experienced sexual violence at some point in their life at greater risk for dropping out of STD care?
Prior work examining sexual violence and STDs has largely relied upon convenience samples and used multiple definitions of sexual violence, making findings difficult to generalize to the larger population.20,24,25 For example, components of sexual violence might include penetrative acts, coercion, sexual harassment, and noncontact acts. Without a consistent and uniform definition of sexual violence, it is difficult to understand how a history of violence may impact STD intervention efforts.6 This study uses the term forced sex to describe forced vaginal penetrative intercourse that is committed by another person without consent.
The current study analyzes data from a United States nationally representative sample of women and seeks to examine the unique patterns of STD care for those women who have experienced forced sex in their lifetime. Specifically, this study investigates whether women who have ever experienced forced sex are more likely to be at current risk for STD acquisition, tested for STDs, diagnosed with STDs, treated for STDs and connected to care. Understanding the complex pathways between forced sex, disease and care will enable STD care professionals to better meet the needs of women who have experienced violence.
METHODS
Study Population
Data for this study was drawn from cycle eight of the National Survey of Family Growth (NSFG 2011–2013). The NSFG is a U.S. cross-sectional, multistage nationally representative survey of individuals living in households who are aged 15 to 44 years. Survey information on design and sampling procedures have been previously described and published elsewhere.26,27 Trained staff interviewed participants and sensitive questions (e.g., forced sex) were collected using Audio Computer-Assisted Self-Interviewing. Eligible participants were female, 18 years or older, and reported having had sexual intercourse.
Measures
National Survey of Family Growth collects data on forced sex by asking two questions: (1) “would you say that this first vaginal intercourse was voluntary or not voluntary, that is, did you choose to have sex of your own free will or not?” and (2) “at any time in your life/besides the time you already reported have you ever been forced by a male to have vaginal intercourse against your will?” The two questions are not necessarily mutually exclusive and in order to obtain the most accurate and nationally representative estimate, we computed a forced sex variable using the two questions. Participants who answered yes to either of these two questions were included in the group of women who had experienced forced sex by a male.
We computed 3 outcome measures of sexual risk: risky sexual behavior was defined as having two or more male sex partners in the past 12 months, no condom use at last sex, and/or taking or giving money or drugs to a male in exchange for sex in the past 12 months. Risky partners was defined as having a male partner who had sex with other males in the past 12 months, having a male sex partner who injects intravenous drugs in the past 12 months, and/or having an HIV+ male sex partner in the past 12 months. Substance use was defined as having four or more drinks within a couple of hours in the past 30 days and/or the use of crack, cocaine, crystal methamphetamine or non-prescription injection drugs in the past 12 months. The constructed variables were adapted from National Health Statistics Reports.28
Our study also included a number of STD outcome variables. Data on chlamydia, gonorrhea, syphilis, herpes, and genital warts was collected from the question: “have you ever been told by a doctor or other medical care provider that you had [specific STD]?” Participants were asked if they had been diagnosed with chlamydia or gonorrhea in the past 12 months and diagnosed with syphilis, herpes and genital warts in their lifetime. A recode for STD testing was computed from 2 testing variables in NSFG: “in the last 12 months, have you been tested for chlamydia?” and “in the past 12 months, have you been tested for any other (other than chlamydia) STD like gonorrhea, herpes, or syphilis?” We computed three different STD diagnoses variables to explore possible moderation effects on STD treatment outcomes. One variable included all individual STDs described above, the second included only the 12-month measures of STD (chlamydia and gonorrhea) and the third included lifetime measures of STDs (herpes and genital warts).
Lastly, the outcome variable STD treatment asked respondents: “in the last 12 months have you been treated or received medication from a doctor or other medical care provider for STD like gonorrhea, chlamydia, herpes, or syphilis?”
Age at interview, race/ethnicity, education, and poverty level were included as demographic variables in all of our models. Age was categorized as: 18–24 years, 25–34 years, and 35–44 years; race/ethnicity included Hispanic, non-Hispanic white, non-Hispanic Black, and other race/ethnicity. Education was categorized as: less than high school/General Education Development (GED), high school or GED diploma, and more than high school. Poverty level was categorized as 0% to 133% (Medicare eligible), and 134% to 500% (not Medicare eligible).
Statistical Analysis
Statistical analysis was conducted using SAS version 9.3 (SAS Institute Inc., Cary, NC) and SUDAAN 11.0.1 (Research Triangle Institute, Durham, NC). We used SAS survey procedures to calculate the distribution of the demographic characteristics and 95% confidence intervals (95% CI), as well as to calculate the Rao-Scott χ2 statistic to compare women who experienced forced sex to women who did not experience this. Logistic regression analyses were conducted using SAS-callable SUDAAN to examine the relationship between forced sex and current risky sexual behavior as well as forced sex and STD testing, diagnoses, treatment, and connection to care. We conducted moderation analyses to examine whether forced sex may moderate the relationship between STD diagnoses and treatment. These moderation analyses aim to examine whether the link between STD diagnoses and treatment may change based on a history of forced sex. All models controlled for demographic characteristics (age at interview, race/ethnicity, poverty level and education).
RESULTS
Bivariate Analyses
Participant Characteristics
Approximately 1 in 5 women reported experiencing forced sexual intercourse in their lifetime (19.5%). Of those women who experienced forced sex, the majority (80.2%) were at least 25 years of age at the time of the interview. Of those women who ever experienced forced sex, 58.4% were white, 18.2% Hispanic, and 17.9% black. Approximately 40% of the women who experienced forced sex were eligible for Medicaid, and about 30% had a high-school degree or GED equivalent. Statistical demographic differences were found between those women who did and did not experience forced sex (Table 1). Logistic regression analyses control for these demographics and adjusted odds ratios are therefore reported.
TABLE 1.
Descriptive Statistics and Key Study Variables for Females in NSFG (2011–2013), Reporting and Not Reporting Lifetime Forced Sexual Intercourse (N = 4962)
| Total N | Forced Sex (n = 1048) | No Forced Sex (n = 3914) | |||
|---|---|---|---|---|---|
| N (Weighted Percentage) | (95% CI) | N (Weighted Percentage) | (95% CI) | ||
| Age at interview, y* | |||||
| 18–24† | 1386 | 217 (19.78) | 15.74–23.82 | 1169 (27.03) | 24.51–29.55 |
| 25–34 | 2034 | 449 (36.79) | 31.93–41.65 | 1585 (37.97) | 35.68–40.26 |
| 35–44† | 1542 | 382 (43.41) | 38.40–18.43 | 1160 (34.98) | 32.50–37.47 |
| Race/ethnicity* | |||||
| Hispanic | 1268 | 226 (18.19) | 14.00–22.38 | 1042 (20.03) | 15.56–24.51 |
| White | 2340 | 517 (58.41) | 52.76–64.05 | 1823 (59.57) | 54.99–64.15 |
| Black† | 1074 | 250 (17.87) | 13.77–21.96 | 824 (13.44) | 10.82–16.07 |
| Other | 280 | 55 (5.52) | 2.21–8.82 | 225 (6.94) | 3.08–10.80 |
| Poverty level* | |||||
| 0–133%† | 2049 | 530 (42.80) | 38.02–17.57 | 1519 (32.38) | 29.48–35.28 |
| 134–500%† | 2913 | 518 (57.19) | 52.42–61.97 | 2395 (67.61) | 64.71–70.51 |
| Education* | |||||
| Less than high school | 681 | 160 (11.99) | 9.55–14.42 | 521 (10.86) | 9.13, 12.58 |
| High school or GED† | 1452 | 324 (31.27) | 26.71–35.82 | 1128 (26.25) | 23.70–28.81 |
| More than high school† | 2829 | 564 (56.73) | 51.69–61.77 | 2265 (62.88) | 59.45–66.30 |
| Risk behavior | |||||
| Risky sexual behavior*‡ | 1258 | 352 (69.09) | 62.54–75.65 | 906 (57.85) | 53.70–61.99 |
| Risky partners*§ | 150 | 56 (5.01) | 3.11–6.91 | 94 (2.45) | 1.69–3.22 |
| Substance use*¶ | 591 | 166 (19.15) | 14.36–23.94 | 425 (12.60) | 11.13–14.07 |
| STD testing*∥ | 1746 | 466 (37.93) | 33.31–2.55 | 1280 (27.90) | 25.31–30.50 |
| Diagnoses | |||||
| Chlamydia*∥ | 113 | 38 (2.11) | 1.15–3.08 | 75 (1.25) | 0.86–1.63 |
| Gonorrhea∥ | 59 | 19 (0.78) | 0.20–1.37 | 40 (0.73) | 0.37–1.09 |
| Syphilis** | 32 | 10 (0.56) | 0.19–0.93 | 22 (0.29) | 0.14–0.44 |
| Herpes*,** | 202 | 71 (6.52) | 4.32–8.72 | 131 (3.34) | 2.34–4.34 |
| Genital warts*,** | 526 | 175 (18.85) | 15.07–22.62 | 351 (8.75) | 7.72–9.79 |
| STD treatment∥ | 272 | 87 (5.68) | 4.03–7.34 | 185 (4.05) | 2.97–5.13 |
χ2 test, P < 0.05.
Post hoc comparison tests indicate category is statistically different across forced sex categories (P < 0.05).
Risky sex is defined as (1) no condom use at last sex, (2) having two or more male sex partners in the past 12 months, or (3) taking or giving money or drugs to a male in exchange for sex in the past 12 months.
Risky partners is defined as (1) having a male partner who had sex with other males in the past 12 months or (2) having a male sex partner who injects intravenous drugs in the past 12 months, or (3) having an HIV+ male sex partner in the past 12 months.
Substance use is defined as (1) 4 or more drinks in within a couple of hours in the past 30 days or (2) the use of crack, cocaine, crystal, or non-prescription injection drugs in the past 12 months.
12-month measure.
Lifetime measure.
Sexual Risk Behavior
In terms of sexual risk behavior, 69.1% of women who experienced forced sex also engaged in recent risky sexual behavior. In addition, 5.0% of women who reported forced sex also reported having a risky partner in the past year. Nearly 20% of women who reported lifetime forced sex also reported engaging in substance abuse in the past year. Women who ever experienced forced sex were significantly more likely than women who had never experienced forced sex to engage in recent risky sexual behavior to report risky partners in the past year and engage in substance abuse in the past year (all P < 0.01) (Table 1).
STD Testing, Diagnoses, and Treatment
Of those women who reported forced sex, nearly four out of ten had an STD test in the past year (37.9%). Data indicates that 2.1% of those women who have ever experienced forced sex have been diagnosed with chlamydia in the past year. Under 1% have been diagnosed with gonorrhea in the past year or ever diagnosed with syphilis. In addition, 18.9% have ever been diagnosed with genital warts and 6.5% with herpes. Only 5.7% of women who have ever experienced forced sex reported being treated for an STD in the past year (Table 1).
Women who reported forced sex were significantly more likely to be tested for an STD in the past 12 months than those women who never experienced forced sex. Women who experienced forced sex were also significantly more likely to have ever been diagnosed with herpes and genital warts than women who have never experienced forced sex (all P < 0.01). They were also more likely to be diagnosed with chlamydia in the past year than women who never experienced forced sex (P < 0.05). There were no significant difference between those women who experienced forced sex and never experienced forced sex and receiving STD treatment in the past 12 months (Table 1).
Multivariate Analyses
History of Forced Sex Predicting Current Sexual Risk and STD Care
Controlling for demographic characteristics, women who experienced forced sexual intercourse were more likely to have risky sex (adjusted odds ratio [AOR], 1.56; 95% CI, 1.08–2.24), risky partners (AOR, 1.90; 95% CI, 1.11–3.23), and report substance abuse (AOR, 1.80; 95% CI, 1.28–2.53) than women who never experienced forced sex (Table 2).
TABLE 2.
Adjusted Odds Ratios for the Effects of Lifetime Forced Sex on Reported Risky Sexual Behavior, Risky Partners, and Substance Abuse for Females in NSFG (2011–2013).*
| Risk Behavior | |||
|---|---|---|---|
| Risky sexual behavior,† n = 1972 | Risky partners,‡ n = 4230 | Substance use,§n = 3913 | |
| AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | |
| Forced sex | 1.56 (1.08–2.24) | 1.90 (1.11–3.23) | 1.80 (1.28–2.53) |
Results in bold emphasis are statistically significant at the P < 0.05 level.
Age at interview, race/ethnicity, poverty level and education are all controlled for in these analyses.
Risky sex is defined as (1) no condom use at last sex, (2) having two or more male sex partners in the past 12 months, or (3) taking or giving money or drugs to a male in exchange for sex in the past 12 months.
Risky partners is defined as (1) having a male partner who had sex with other males in the past 12 months or (2) having a male sex partner who injects intravenous drugs in the past 12 months, or (3) having an HIV+ male sex partner in the past 12 months.
Substance use is defined as (1) 4 or more drinks in within a couple of hours in the past 30 days or (2) the use of crack, cocaine, crystal, or non-prescription injection drugs in the past 12 months.
Women who reported ever experiencing forced sex were more likely to be tested for an STD in the past 12 months (AOR, 1.67; 95% CI, 1.34–2.09), and ever be diagnosed with herpes (AOR, 1.94; 95% CI, 1.13–3.32), genital warts (AOR, 2.55; 95% CI, 1.90–3.41), and chlamydia (AOR, 1.83; 95% CI, 1.03–3.25) but no more likely to be diagnosed with gonorrhea or syphilis than those who have never had forced sex. There was no relationship between STD treatment in the past 12 months and forced sex (Table 3). No demographic variables were found to have consistently moderated the effect of forced sex on any outcome measure.
TABLE 3.
Adjusted Odds Ratios for the Effects of Lifetime Forced Sex Predicting 12-Month STD Testing, Diagnoses, and 12-Month STD Treatment for Females in NSFG (2011–2013)*
| Testing | Diagnoses | Treatment | |||||
|---|---|---|---|---|---|---|---|
| n = 4938 | Chlamydia† n =4955 | Gonorrhea† n=4956 | Syphilis‡ n =4958 | Herpes‡ n =4957 | Warts‡ n = 4957 | n=4954 | |
| AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | |
| Forced sex | 1.67 (1.34–2.09) | 1.83 (1.03–3.25) | 1.08 (0.44–2.70) | 1.68 (0.74–3.81) | 1.94 (1.13–3.32) | 2.55 (1.90–3.41) | 1.44 (0.95–2.18) |
Results in bold emphasis are statistically significant at the P < 0.05 level.
Age at interview, race/ethnicity, poverty level and education are all controlled for in these analyses.
12-month measure;
= lifetime measure.
Understanding the Link between Forced Sex and Current STD Treatment
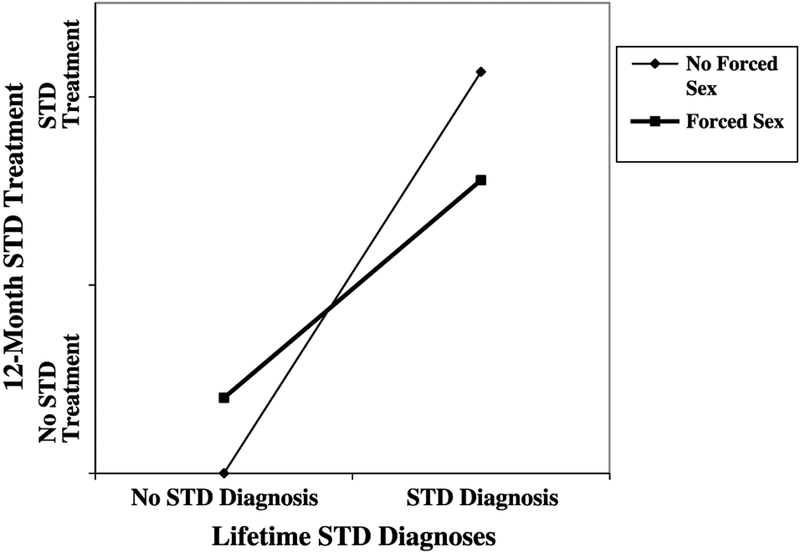
Results indicated a direct relationship between lifetime STD diagnoses (herpes and genital warts) and STD treatment in the past 12 months (AOR, 6.81; 95% CI, 4.50–10.31). Further analyses indicated that forced sex moderated the link between lifetime STD diagnoses and STD treatment (AOR, 0.43; 95% CI, 0.19–0.98), suggesting that women who experienced forced sex and had ever been diagnosed with herpes or genital warts were less likely to receive treatment in the past 12 months than those women who had not experienced forced sex (Table 4; Fig. 1).
TABLE 4.
Odds Ratios for the Moderation Effect of Lifetime Herpes and Genital Warts Diagnoses and Lifetime Forced Sex Predicting 12-Month STD Treatment for Females in NSFG (2011–2013) (N = 4951)
| OR (95% CI) | |
|---|---|
| Age at interview | |
| 18–24 | 2.72 (1.50–4.90) |
| 25–34 | 1.84 (1.04–3.28) |
| 35–14 | Reference Cat. |
| Race/ethnicity | |
| Hispanic | 1.13 (0.67–1.92) |
| White | Reference Cat. |
| Black | 2.15 (1.39–3.31) |
| Other | 1.75 (0.65–4.70) |
| Poverty level | |
| 0–133% | Reference Cat. |
| 134–500% | 0.74 (0.51–1.07) |
| Education | |
| Less than high school | 1.78 (0.94–3.40) |
| High school or GED | 1.27 (0.77–2.10) |
| More than high school | Reference Cat. |
| Forced sex | 1.52 (0.92–2.51) |
| Diagnoses | 8.51 (4.98–14.54) |
| Diagnoses × forced sex | 0.43 (0.19–0.98) |
Results in bold emphasis are statistically significant at the P < 0.05 level. Cat indicates category.
Figure 1.
Interaction between lifetime forced sex and lifetime STD diagnoses (herpes and warts), predicting receipt of STD treatment in the past 12 months (NSFG 2011–2013). Categories are dichotomous, such that a STD diagnosis was present or absent and STD treatment has either been reported by participants as received or not received.
No forced sex moderation effects were found between 12-month diagnoses and treatment or between all diagnoses (12-month and lifetime) and treatment.
DISCUSSION
This study used nationally representative data of women aged 15 to 44 years, which allowed us to make inferences at a population level. By focusing on multiple aspects of care for women who experienced forced sex, this paper makes a unique contribution by moving beyond associations between forced sex and sexual risk-taking. We focused on the acquisition of STDs and the diagnosis of specific STDs; this is especially relevant as much previous work has only focused on HIV or undifferentiated STDs diagnoses.20 In addition, moderation analyses begin to reveal how women who have experienced forced sex in the past may presently engage in STD care.
The results of this study indicate that approximately one out of every five women ever experienced forced vaginal intercourse, which is consistent with previous U.S. national estimates.7 Such prevalence suggests that women who experienced forced sex are an important and sizable population of women. Multivariate analyses, controlling for sociodemographics, suggest that women who experienced forced sex were about two times more likely to engage in risky sexual behavior, report risky partners, and engage in substance abuse in the past year than women who never experienced forced sex. These findings are consistent with previous studies focused on the impact of sexual violence on HIV/STD risk behaviors.14,15 Multivariate analyses indicate that women who experienced forced sex were significantly more likely to be diagnosed with chlamydia in the past year and herpes and genital warts in their lifetime than women who never experienced forced sex. Such results suggest that women who experience forced sex may have an elevated need for sexual health services, regardless of when the forced sex occurred. Gonorrhea and syphilis did not demonstrate statistically significant relationship to forced sex, but followed a similar trend to the all of the measured STDs; this may have been due to the small number of women who reported gonorrhea and syphilis diagnosis.
Our analyses indicate that experiencing forced sex increases the odds of engaging in risky sex and STD diagnosis. Results indicate that those who experience forced sex are engaged in basic health care; these women reported higher odds of STD testing in comparison to women who never experienced forced sex. A direct association was found between lifetime STD diagnoses and STD treatment, and forced sex appeared to moderate this link. That is, women who ever had an STD diagnosis and reported forced sex were less likely to receive STD treatment than women who never experienced forced sex. This finding may indicate that women who experience forced sex and have a history of STD diagnoses may be falling out of treatment due to missed opportunities for health providers to identify them as an at-risk group. Forced sex may moderate or attenuate the link between STD diagnoses and treatment due to other ecologic factors affecting women who have experienced forced sex, such as stigma, lack of partner notification, unstable housing, family factors, economic instability, and the negative physical effects stemming from forced sex.1,3,8,10 Previous research also indicates that those who have experienced sexual violence are less likely to receive needed services and more likely to have a poor relationship with their health care provider.29
Taking a comprehensive sexual health history during a medical visit often leads to risk-reduction counseling and the ability to identify women who may be at heightened risk for acquiring STDs. Per CDC and National Coalition for Sexual Health guidelines,30 in a comprehensive sexual history, medical staff would include questions covering sexual orientation, frequency of sexual activity, number of partners, and type of sexual activity. However, research indicates that comprehensive sexual histories are taken relatively rarely,31 even when indicated.32–35 Compounding these barriers, the majority of sexual health history instruments and guides do not ask women about experiences of sexual violence and unwanted sex.30 However, based on the results of this study, taking a sexual history which includes questions on sexual violence and unwanted sex can better allow the attending health care provider to understand current ailments and potential health sequelae.
Limitations and Future Directions
A limitation of our study was that we had limited context on the forced sex event(s); previous research shows that frequency of forced sex,36 whether the sex occurred as a child and/or adult,37 and type of perpetrator relationship38 all have potential implications for ongoing medical care. As well, with just 1 time point of data, we cannot sequence if the STD treatment was in response to an STD diagnosis captured here, or even if the STD diagnosis was directly related to a forced sex episode. We were limited by the time frames available within the data; understanding how all STDs variables operated within a 12-month period, for example, would shed additional light on our findings. Longitudinal work on violence, STD contraction, and care would further clarify links among these complex indicators and allow for a better understanding of the temporality among forced sex, diagnoses, and treatment. Our study focused exclusively on forced penile-vaginal intercourse and did not include other forms of unconsented and unwanted sex. Last, the data were self-reported; however, Audio Computer-Assisted Self-Interviewing was used, which has been shown to offer participants greater comfort in reporting on sensitive topics.39
Overall, our hope is that this study can begin to clarify the relationship between forced sex, STD acquisition and STD care and the important role providers can play in caring for this vulnerable population of women.
Understanding the complex pathways between forced sex, disease and can enable medical professionals to best meet the health needs of women victimized by violence.
Footnotes
Conflict of Interest Disclosure: None declared.
REFERENCES
- 1.Centers for Disease Control and Prevention. Ten ways STDs impact women differently from men. Atlanta: U.S: Department of Health and Human Services; 2011. [Google Scholar]
- 2.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2015. Atlanta: U.S: Department of Health and Human Services; 2016. [Google Scholar]
- 3.Coker AL. Does physical intimate partner violence affect sexual health? A systematic review. Trauma Violence Abuse 2007; 8:149–177. [DOI] [PubMed] [Google Scholar]
- 4.Miller E, Decker MR, Silverman JG, et al. Migration, sexual exploitation, and women’s health: a case report from a community health center. Violence Against Women 2007; 13:486–497. [DOI] [PubMed] [Google Scholar]
- 5.Black MC, Basile KC, Breiding MJ, et al. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 summary report National Center for Injury Prevention and Control, Centers for Disease Control and Prevention: Atlanta, GA, 2010. [Google Scholar]
- 6.Basile KC, Smith SG, Breiding MJ, et al. Sexual violence surveillance: Uniform definitions and recommended data elements, version 2.0 National Center for Injury Prevention and Control, Centers for Disease Control and Prevention.: Atlanta, GA, 2014. [Google Scholar]
- 7.Black MC, Basile KC, Breiding MJ, et al. National intimate partner and sexual violence survey National Center for Injury Prevention and Control, Centers for Disease Control and Prevention: Atlanta, GA, 2011. [Google Scholar]
- 8.Campbell JC, Moracco KE, Saltzman LE. Future directions for violence against women and reproductive health: Science, prevention, and action. Matern Child Health J 2000; 4:149–154. [DOI] [PubMed] [Google Scholar]
- 9.Jewkes RK, Dunkle K, Nduna M, et al. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: A cohort study. Lancet 2010; 376:41–48. [DOI] [PubMed] [Google Scholar]
- 10.Campbell JC, Baty ML, Ghandour R, et al. The intersection of intimate partner violence against women and HIV/AIDS: A review. Int J Inj Contr Saf Promot 2008; 15:221–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dunkle KL, Jewkes RK, Brown HC, et al. Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. Lancet 2004; 363:1415–1421. [DOI] [PubMed] [Google Scholar]
- 12.Kalichman SC, Williams EA, Cherry C, et al. Sexual coercion, domestic violence, and negotiating condom use among low-income African American women. J Womens Health 1998; 7:371–378. [DOI] [PubMed] [Google Scholar]
- 13.Moorea AM, Frohwirtha L, Miller E. Male reproductive control of women who have experienced intimate partner violence in the United States. Soc Sci Med 2010; 70:1737–1744. [DOI] [PubMed] [Google Scholar]
- 14.Bauer HM, Gibson P, Hernandez M, et al. Intimate partner violence and high-risk sexual behaviors among female patients with sexually transmitted diseases. Sex Transm Dis 2002; 29:411–416. [DOI] [PubMed] [Google Scholar]
- 15.Shrier LA, Pierce JD, Emans SJ, et al. Gender differences in risk behaviors associated with forced or pressured sex. Arch Pediatr Adolesc Med 1998; 152:57–63. [DOI] [PubMed] [Google Scholar]
- 16.Thompson NJ, Potter JS, Sanderson CA, et al. The relationship of sexual abuse and HIV risk behaviors among heterosexual adult female STD patients. Child Abuse Negl 1997; 21:149–156. [DOI] [PubMed] [Google Scholar]
- 17.El-Bassel N, Gilbert L, Krishnan S, et al. Partner violence and sexual HIV-risk behaviors among women in an inner-city emergency department. Violence Vict 1998; 13:377–393. [PubMed] [Google Scholar]
- 18.Wu E, El-Bassel N, Witte SS, et al. Intimate partner violence and HIV risk among urban minority women in primary health care settings. AIDS Behav 2003; 7:291–301. [DOI] [PubMed] [Google Scholar]
- 19.Martin SL, Kilgallen B, Tsui AO, et al. Sexual behaviors and reproductive health outcomes: Associations with wife abuse in India. JAMA 1999; 282:1967–1972. [DOI] [PubMed] [Google Scholar]
- 20.Stockman JK, Campbell JC, Celentano DD. Sexual violence and HIV risk behaviors among a nationally representative sample of heterosexual American women: The importance of sexual coercion. J Acquir Immune Defic Syndr 2010; 53:136–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guttmacher. Understanding intimate partner violence as a sexual and reproductive health and rights issue in the United States. Guttmacher Pol Rev 2016:19. [Google Scholar]
- 22.Parsons L, Goodwin MM, Petersen R. Violence against women and reproductive health: Toward defining a role for reproductive health care services. Matern Child Health J 2000; 4:135–140. [DOI] [PubMed] [Google Scholar]
- 23.Coker AL, Davis KE, Arias I, et al. Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med 2002; 23:260–268. [DOI] [PubMed] [Google Scholar]
- 24.Ellsberg M, Heise L, Peña R, et al. Researching domestic violence against women: Methodological and ethical considerations. Stud Fam Plann 2001; 32:1–16. [DOI] [PubMed] [Google Scholar]
- 25.Garcia-Moreno C, Heise L, Jansen HA, et al. Public health. Violence against women. Science 2005; 310:1282–1283. [DOI] [PubMed] [Google Scholar]
- 26.Groves RM, Mosher WD, Lepkowski J, et al. Planning and development of the continuous National Survey of Family Growth. National Center for Health Statistics. Vital Health Stat 1(48). 2009. Available from: http://www.cdc.gov/nchs/data/series/sr_01/sr01_048.pdf. [PubMed] [Google Scholar]
- 27.Lepkowski JM, Mosher WD, Davis KE, et al. The 2006–2010 National Survey of Family Growth: Sample design and analysis of a continuous survey. National Center for Health Statistics. Vital Health Stat 2(150) 2010. Available from: http://www.cdc.gov/nchs/data/series/sr_02/sr02_150.pdf. Accessed September 23, 2016. [PubMed] [Google Scholar]
- 28.Chandra A, Billioux VG, Copen CE, et al. HIV risk-related behaviors in the United States household population aged 15–44: Data from the National Survey of Family Growth, 2002 and 2006–2010 In: National health statistics reports; no 46. Hyattsville, MD: National Center for Health Statistics, 2012. [PubMed] [Google Scholar]
- 29.Plichta SB. Interactions between victims of intimate partner violence against women and the health care system: Policy and practice implications. Trauma Violence Abuse 2007; 8:226–239. [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. A guide to taking a sexual history. Atlanta: U.S: Department of Health and Human Services; 2011. Available from: https://www.cdc.gov/std/treatment/SexualHistory.pdf. Accessed December 2, 2016. [Google Scholar]
- 31.Goyal MK, Witt R, Hayes KL, et al. Clinician adherence to recommendations for screening of adolescents for sexual activity and sexually transmitted infection/human immunodeficiency virus. J Pediatr 2014; 165:343–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fiscus LC, Ford CA, Miller WC. Infrequency of sexually transmitted disease screening among sexually experienced U.S. female adolescents. Perspect Sex Reprod Health 2004; 36:233–238. [DOI] [PubMed] [Google Scholar]
- 33.Torkko KC, Gershman K, Crane LA, et al. Testing for Chlamydia and sexual history taking in adolescent females: results from a statewide survey of Colorado primary care providers. Pediatrics 2000; 106:E32. [DOI] [PubMed] [Google Scholar]
- 34.Alexander SC, Fortenberry JD, Pollak KI, et al. Sexuality talk during adolescent health maintenance visits. JAMA Pediatr 2014; 168: 163–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Skelton JR, Matthews PM. Teaching sexual history taking to health care professionals in primary care. Med Educ 2001; 35:603–608. [DOI] [PubMed] [Google Scholar]
- 36.Coker AL, Smith PH, McKeown RE. Frequency and correlates of intimate partner violence by type: physical, sexual, and psychological battering. Am J Public Health 2000; 90:553–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Paolucci EO, Genuis ML, Violato C. A meta-analysis of the published research on the effects of child sexual abuse. J Psychol 2001; 135: 17–36. [DOI] [PubMed] [Google Scholar]
- 38.Campbell JC. The health consequences of intimate partner violence. Lancet 2002; 359:1509–1514. [DOI] [PubMed] [Google Scholar]
- 39.Turner CF, Ku L, Rogers SM, et al. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science 1998; 280:867–873. [DOI] [PubMed] [Google Scholar]