Because syphilis infection facilitates acquisition and transmission of human immunodeficiency virus (HIV) (1,2), recent outbreaks of syphilis among men who have sex with men (MSM) in major U.S. cities (3), including San Francisco and Los Angeles (4,5), and reported increases in sexual risk behavior (5) have raised concerns about potential increases in HIV transmission. In 2002, MSM accounted for the majority of primary and secondary (P&S) syphilis cases in men reported in San Francisco (93%) and Los Angeles (81%). To investigate a potential change in HIV incidence associated with the syphilis outbreaks in the two cities, local, state, and federal health officials analyzed data from HIV counseling and testing centers and a municipal sexually transmitted disease (STD) clinic. This report describes the results of that investigation, which indicated that, as of 2002, the outbreaks of syphilis had not had a substantial impact on HIV incidence among MSM in these two cities. However, the continued increase in syphilis cases in MSM underscores the need for integrated HIV- and STD-prevention strategies to control syphilis outbreaks and prevent potential increases in HIV infections (6,7) and for further systematic studies of HIV incidence among MSM infected with syphilis.
For this analysis, numbers and characteristics of P&S syphilis cases among MSM in San Francisco and Los Angeles were determined from STD morbidity data. Rates of P&S syphilis per 100,000 MSM were calculated for the estimated 50,782 MSM living in San Francisco in 2001 (8). In 2002, approximately 47% and 18% of MSM with P&S syphilis in San Francisco and Los Angeles, respectively, had syphilis diagnosed at publicly funded sites, which included primarily STD clinics.
A sensitive/less sensitive HIV-1 enzyme immunoassay (EIA) (Vironostika HIV-1 Microelisa, bioMérieux, Durham, North Carolina) testing algorithm known as STARHS (9,10) was used to estimate HIV incidence by using stored blood specimens for 1) MSM receiving confidential HIV counseling and testing at the City Clinic (SFCC), San Francisco’s only municipal STD clinic, and 2) MSM receiving anonymous HIV counseling and testing at University of California at San Francisco AIDS Health Project (AHP) sites. For persons tested at AHP sites (1998–2002) and persons tested at SFCC (1998–2000), demographic and risk-factor information collected on the California HIV counseling and testing form was analyzed. For persons tested at SFCC (2001–2002), analogous information obtained from medical records was analyzed. Persons who tested reactive with the sensitive EIA and nonreactive with the less sensitive assay were considered recently HIV infected (mean seroconversion period: 170 days) (10). Annualized HIV incidence and 95% confidence intervals (CIs) based on a normal distribution were calculated; all reported p-values were obtained by using a chi-square test for trend.
In Los Angeles, data from the California and CDC HIV counseling and testing forms were used to calculate the percentages and characteristics of MSM with newly diagnosed infections. These patients had received a confidential or anonymous HIV test at publicly funded sites during 1998–2002.
San Francisco Surveillance Data
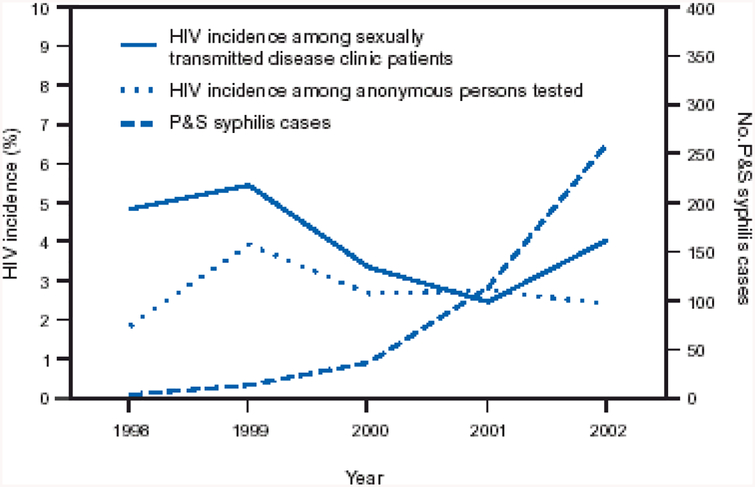
During 1998–2002, the number of P&S syphilis cases among MSM in San Francisco increased from four to 260 (Figure 1), and the P&S syphilis rate increased from eight to 512 per 100,000 MSM. In 2002, the median age of MSM P&S syphilis patients was 38 years; 70% were white, 14% were Hispanic, and 61% were HIV-infected. P&S syphilis cases among MSM at the SFCC also increased, from four in 1998 to 106 in 2002.
FIGURE 1.
Number of primary and secondary (P&S) syphilis cases among men who have sex with men (MSM) and incidence of human immunodeficiency virus (HIV) among MSM in two HIV-testing populations, by year — San Francisco, California, 1998–2002
MSM receiving HIV testing had similar demographic characteristics and the two San Francisco testing populations. In 2002, at AHP and SFCC, respectively, the median age of these patients was 34 and 33 years; 70% and 61% were white, 3% and 6% were black, 11% and 19% were Hispanic, 12% and 14% were Asian/Pacific Islander (A/PI), and 4% and <1% were of other race/ethnicity.
Estimated HIV incidence among MSM who were tested in San Francisco was highest in 1999 (Figure 1, Table 1) and tended to decline from 1999 to 2002 at both sites; however, the trends were not statistically significant (p = 0.13 for AHP; p = 0.36 for SFCC). When injection-drug–using MSM were excluded from analyses, HIV incidence was lower (e.g., in 2002, incidence was 2.3% [95% CI = 1.0–3.5] at AHP and 3.3% [95% CI = 1.9–4.7] at SFCC), but temporal trends in HIV incidence were similar. Median age of the 42 MSM with incident HIV infection at these testing sites in 2002 was 32 years; 23 (55%) were white, and 12 (29%) were Hispanic.
TABLE 1.
Number and rata* of primary and secondary (P&S) syphilis cases among men who have sex with man (MSM†) and human immunodeficiency virus (HIV) incidence among MSM in two HIV-testing populations, by year—San Francisco, California 1998–2002
| Year | P&S syphilis cases | No. P&S syphilis cases at SFCC§ | MSM HIV testing at AIDS Health Project | MSM HIV testing at SFCC | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. testing | No. with incident HIV infection | HIV incidence (%) | (95% CI¶) | No. testing | No. with incident HIV infection | HIV incidence (%) | (95% CI) | ||||
| No. | Rate | ||||||||||
| 1998 | 4 | 8 | 4 | 2,726 | 23 | 1.8 | (1.1–2.6) | 791 | 17 | 4.8 | (2.5–7.1) |
| 1000 | 13 | 26 | a | 1,596 | 23 | 3.9 | (2.5–5.4) | 663 | 21 | 5.4 | (.3.1–7.6) |
| 2000 | 36 | 71 | 12 | 1,721 | 21 | 2.7 | (1.5–3.6) | 1,324 | 20 | 3.8 | (1.9–4.6) |
| 2001 | 113 | 223 | 42 | 1,762 | 22 | 2.3 | (1.6–3.9) | 1,274 | 14 | 2.5 | (1.2–3.7) |
| 2002 | 260 | 512 | 106 | 1,280 | 14 | 2.4 | (1.2–3.7) | 1,544 | 28 | 4.0 | (2.5–5.5) |
Per 100.000 men who have sex with men.
Men who reported having sex with men during the preceding 12 months.
San Francisco City Clinic.
Confidence interval.
HIV incidence was estimated by STARHS for men who had P&S syphilis diagnosed at SFCC in 2002 and 2003 and who accepted confidential HIV-antibody and STARHS testing. Of 74 men, 16 (22%) were HIV seropositive, and four (25%) of these had a recent HIV infection identified by STARHS; all four of these patients reported having had HIV-seronegative test results within the previous 2 years. On the basis of STARHS, estimated HIV incidence in this population was 13.9% per year (95% CI = 0.3–27.5).
Los Angeles Surveillance Data
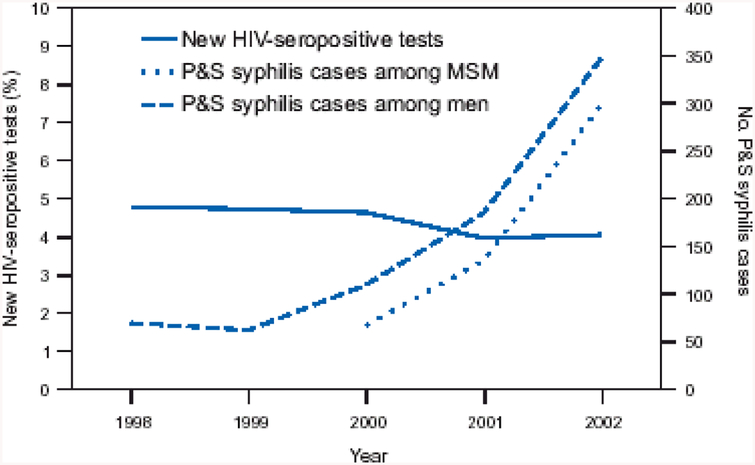
During 2000–2002, P&S syphilis cases among MSM in Los Angeles County increased from 67 to 299, accounting for the majority of male syphilis patients (Figure 2). In 2002, median age of MSM with P&S syphilis was 37 years; 51% were white, 31% were Hispanic, and 58% were HIV infected.
FIGURE 2.
Number of primary and secondary (P&S) syphilis cases among men who have sex with men (MSM) and percentage of newly identified human immunodeficiency virus (HIV)-seropositive MSM at county HIV-testing sites, by year—Los Angeles County, California, 1998–2002
MSM receiving HIV testing at Los Angeles County sites had similar demographic characteristics during 1998–2002. In 2002, the median age of 15,161 MSM who were tested was 32 years; 42% were white, 10% were black, 37% were Hispanic, 7% were A/PI, and 4% were of other race/ethnicity. The percentage of MSM with HIV newly diagnosed (i.e., without any previous HIV-positive test) decreased from 4.8% (608 of 12,693) in 1998 to 4.1% (615 of 15,161) in 2002 (p<0.001) (Table 2). In 2002, the 615 MSM who had newly diagnosed HIV had a median age of 32 years; 29% were white, 18% were black, and 45% were Hispanic. However, among MSM who had an HIV-negative test result within the previous 12 months, the percentage of men with a new HIV-positive test increased from 2.4% (102 of 4,196) in 1998 to 2.9% (186 of 6,446) in 2002 (p = 0.37).
TABLE 2.
Number of primary and secondary (P&S) syphilis cases among men who have sex with men (MSM) and number and percentage of human immunodeficiency virus (HIV)-seropositive MSM at county HIV-testing sites, by year—Los Angeles County California, 1995–2002
| Year | No. P&S syphilis patients* | No. patients tested for HlV† | HIV-positive patients | Newly diagnosed§ HIV-positive patients | ||
|---|---|---|---|---|---|---|
| No. | (%) | No. | (%) | |||
| 1998 | — | 12,693 | 759 | (6.0) | 608 | (4.8) |
| 1999 | — | 12,632 | 771 | (6.1) | 599 | (4.7) |
| 2000 | 67 | 12,527 | 717 | (5.7) | 581 | (4.6) |
| 2001 | 135 | 14,490 | 603 | (4.7) | 576 | (4.0) |
| 2002¶ | 299 | 15,161 | 702 | (4.6) | 615 | (4.1) |
MSM who reported having sex with men during the time they likely contracted primary (preceding 90 days) or secondary (preceding 200 days) syphilis.
MSM who reported having sex with men since their most recent HIV test or during the preceding 2 years.
MSM with no previous HIV-positive test.
Provisional data.
Editorial Note:
The number of new HIV infections among MSM at public HIV-testing sites in San Francisco and Los Angeles did not increase during 1999–2002, a period when syphilis cases among MSM increased substantially in both cities. Within the SFCC population, no temporal correlation was detected between an increase in the number of MSM P&S syphilis cases and the rates of new HIV infections among MSM who received HIV testing at this STD clinic. Whether the syphilis outbreaks are sentinel events indicating increased risk behavior that could eventually result in increased HIV incidence is not known.
The findings of this ecological analysis are subject to at least five limitations. First, whereas the overall P&S syphilis morbidity data were reported from both private and public providers, with the majority of MSM P&S syphilis cases being reported from private sources, HIV incidence (San Francisco) and new HIV diagnoses (Los Angeles) could be examined only for select populations at publicly funded HIV-testing sites. MSM attending public HIV-testing venues might differ in their demographics and risk behaviors from MSM who seek HIV testing from private providers or who have not been HIV tested. Second, changes in testing practices and number and characteristics of MSM in the two public HIV-testing populations might weaken inferences about trends in HIV incidence or new HIV diagnoses among these populations. Analyses might include persons who tested anonymously and repeatedly at SFCC, AHP, and Los Angeles HIV-testing sites, and potential changes in repeat HIV-testing patterns over time could affect HIV incidence trends. Third, the proportion of oral HIV antibody tests performed for MSM at AHP sites increased from 11% in 1998 to 36% in 2002, thus increasing the proportion of patients tested who were excluded from STARHS-based estimates of HIV incidence. Fourth, STARHS might misclassify a small percentage of persons with long-standing infection as recently infected and vice versa (9,10). Finally, the SFCC estimate of HIV incidence among MSM with P&S syphilis (13.9% per year) has wide associated variability (95% CI = 0.3–27.5) and must be interpreted with caution because not all male syphilis patients accepted HIV testing.
Despite the high HIV incidence in men with P&S syphilis, HIV incidence rates among MSM tested at large public sites in San Francisco and Los Angeles did not increase during 1999–2002. This stability likely is because 1) the number of new syphilis cases is small compared with the numbers of MSM at risk for HIV infection and 2) in both cities more than half of the MSM P&S syphilis patients had longstanding HIV infection before they acquired syphilis. However, if the outbreaks of syphilis continue unabated, HIV incidence among MSM at public HIV-testing sites and in the larger MSM community might increase. Recommendations include behavioral risk assessment, frequent STD screening, and prompt treatment of syphilis in HIV-infected persons and their partners to control syphilis outbreaks and prevent a potential increase in HIV infections.
Footnotes
Publisher's Disclaimer: Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electron6ic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402–9371; telephone: (202) 512–1800. Contact GPO for current prices.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.
References to non-CDC sites on the Internet are provided as a service to MMWR readers and do not constitute or imply endorsement of these organizations or their programs by CDC or the U.S. Department of Health and Human Services. CDC is not responsible for the content of pages found at these sites. URL addresses listed in MMWR were current as of the date of publication.
References
- 1.Wasserheit JN. Epidemiological synergy: interrelationships between human immunodeficiency virus infection and other sexually transmitted diseases. Sex Transm Dis 1992;19:61–77. [PubMed] [Google Scholar]
- 2.Buchacz K, Patel P, Taylor M, Kerndt PR, Holmberg SD, Klausner JD. Syphilis infection increases HIV viral load in HIV-infected men [Abstract T2-L204]. Presented at the National HIV Prevention Conference, Atlanta, Georgia, July 27–30, 2003. [Google Scholar]
- 3.CDC. Primary and secondary syphilis—United States, 2002. MMWR 2003;52:1117–20. [PubMed] [Google Scholar]
- 4.CDC. Outbreak of syphilis among men who have sex with men—Southern California, 2000. MMWR 2001;50:117–20. [PubMed] [Google Scholar]
- 5.Chen SY, Gibson S, Katz MH, et al. Continuing increases in sexual risk behavior and sexually transmitted diseases among men who have sex with men: San Francisco, California, 1999–2001. Am J Public Health 2002;92:1387–8. [PMC free article] [PubMed] [Google Scholar]
- 6.King JB, Samuel M, Kent C, Klausner J. Recent early syphilis, gonorrhea and chlamydia among men who have sex with men increase risk for recent HIV seroconversion—San Francisco, 2002–2003 [Abstract T2-L203]. Presented at the National HIV Prevention Conference, July 27–30, 2003. [Google Scholar]
- 7.CDC. Increases in HIV diagnoses in 29 states, 1999–2002. MMWR 2003;52:1145–8. [PubMed] [Google Scholar]
- 8.San Francisco Department of Public Health, AIDS Office. The HIV/AIDS Epidemiology Annual Report 2002. Available at http://www.dph.sf.ca.us/reports/std/hivaidsannlrpt2002.pdf.
- 9.Janssen RS, Satten GA, Stramer SL, et al. New testing strategy to detect early HIV-1 infection for use in incidence estimates and for clinical and prevention purposes. JAMA 1998;280:42–8. [DOI] [PubMed] [Google Scholar]
- 10.Kothe D, Byers RH, Caudill SP, et al. Performance characteristics of a new less sensitive HIV-1 enzyme immunoassay for use in estimating HIV seroincidence. J Acquir Immune Defic Syndr 2003;33:625–34. [DOI] [PubMed] [Google Scholar]