Abstract
Purpose:
Many children attend family child care homes (FCCHs), an important setting to influence children’s physical activity (PA) and sedentary behavior (SB). This study assessed children’s PA and SB while in FCCHs, characteristics of the FCCH PA environment, and relationships between the environment and child PA and SB.
Method:
Children ages 1.5–4.0 years (n = 495) were recruited from 165 FCCHs in North Carolina. Children’s moderate to vigorous PA and SB were measured via accelerometry for 3 days. FCCH PA environments were assessed over 2 days using the Environment and Policy Assessment and Observation for FCCHs. Ten subscores and an overall PA environment score (possible range: 0–30) were calculated; higher scores indicate better quality.
Results:
Children accumulated 30 (13) minutes of moderate to vigorous PA and 143 (42) minutes of SB in FCCHs daily. FCCHs scored low on the Environment and Policy Assessment and Observation for FCCHs, with an average overall score of 13 (2). FCCHs scored highest on screen time and screen time practices subscores, and lowest on PA education/professional development and PA policy subscores. Although no statistically significant associations were observed, some large Cohen d effect sizes were noted (eg, outdoor playtime subscore and moderate to vigorous PA).
Conclusions:
This study highlights opportunities to improve FCCHs and increase children’s behaviors (eg, providing adequate time and outdoor play spaces).
Keywords: health behavior, health promotion, pediatrics
Obtaining regular physical activity (PA) and avoiding excessive sedentary behavior (SB) are important for optimal growth and development throughout early childhood. Higher levels of PA are associated with a healthy weight status, improved bone and musculoskeletal health, gross motor development, and better cardiometabolic health (31). Furthermore, PA plays a role in cognitive development as well as children’s psychosocial well-being (15,30). PA and SBs formed early in childhood often track into adolescence and adulthood, underscoring the importance of promoting these behaviors very early in life (17). Yet nearly half of preschool-aged children fail to meet the PA recommendations needed for these health and developmental benefits (35).
Early care and education (ECE) programs are an important setting through which to reach young children and influence their PA and SBs (13). Most available research has come from studies in child care centers, the most common form of ECE program. Centers are typically larger organizations where providers care for children of a similar, narrow developmental range in separate classrooms. Studies with family child care homes (FCCHs) are very limited, yet they are the second most common arrangement of nonrelative child care in the United States, serving more than 1.5 million children under the age of 6 (19). These small businesses are generally owned by the child care provider and operated out his or her own home, where care is given to children from birth to 6 years usually by a sole provider. FCCH providers have unique challenges to providing care, often balancing their personal home and family life along with simultaneously providing care to children with a range of developmental capabilities (9). The limited research in this specific type of ECE setting suggests that many children attending FCCHs do not obtain sufficient activity (7,28). Even less is known about how the quality of the FCCH environment influences children’s PA and SB.
The physical environment of all ECE settings comprises multiple components that can influence young children’s PA and SBs as follows: provisions (eg, time, equipment); provider behaviors and practices; and organizational-level policies. Evidence from center-based studies shows that provisions such as time spent outdoors (29), available play space (5), and the presence of portable play equipment (4,5) can have a positive impact on children’s PA. In addition, provider practices including teacher-led PA (4) and verbal prompts for activity (10,12) positively influence children’s PA, as can policies on amount of required outdoor time (13). Furthermore, intervention evidence suggests that these various environmental characteristics can be modified within ECE centers, and improvements may result in increased child PA (42). Given the differences between centers and FCCHs, translation of effective center-based interventions for use with FCCHs would benefit from a better understanding of children’s activity at the FCCH and how FCCH environmental components are related to children’s PA.
Similar to studies within ECE centers, previous studies of PA and SB of children attending FCCHs or FCCH environments have investigated PA and SB estimates and differences by child gender and weight status (28) and assessed the relationship of PA and SB practices (7) in somewhat small samples. This study extends this prior research by a comprehensive assessment of the FCCH environment in a large sample of FCCHs and children attending FCCHs. The purpose of the current study was 3-fold: to quantify the PA of children enrolled in FCCHs, to assess FCCHs PA environments (40), and to determine which components of the FCCH environment were associated with children’s PA while in FCCHs. Based on findings from the center-based care literature, we hypothesized that children in FCCHs with more supportive PA environments (eg, providing more PA time or less screen time [ST]) would have higher levels of moderate to vigorous PA (MVPA) and lower amounts of SB.
Methods
This study used baseline data from an intervention trial, Keys to Healthy FCCHs, evaluating a FCCH-based intervention designed to increase children’s healthy eating and PA behaviors. A detailed description of the study protocol (23) and recruitment process (43) are provided elsewhere, but components relevant to the current study are described below. All study protocols were approved by the institutional review boards at the University of North Carolina at Chapel Hill and Duke University Medical Center and were registered prospectively at ClinicalTrials.gov ().
Sample Recruitment
Family child care homes in 26 counties in central North Carolina were identified from a publicly available database (20) to target for recruitment. Community partners who had existing relationships with FCCHs introduced the project to FCCH providers. This was followed by direct recruitment efforts via mailed invitations and telephone calls. During telephone calls, recruitment staff reviewed study details and confirmed FCCH eligibility. FCCHs were eligible if they had at least two 1.5- to 4-year-old children enrolled, served at least 1 meal and 1 snack daily, had been in business for at least 2 years, and had no plans to close in the coming year. Project staff worked with interested and eligible centers to obtain consent from parents of 1.5- to 4-year-old children enrolled in the FCCH. Consent for at least 2 children had to be given for a FCCH to enroll in the study. The total recruited sample was 166 FCCHs and 496 children.
Data Collection
Data were collected during 2 day-long visits with each participating FCCH provider; visits were spread across 3 days (eg, Monday and Wednesday, Tuesday and Thursday). Measures assessed child and provider PA, anthropometrics, and demographics, as well as the FCCH PA environment. Data collectors were trained and certified on all study protocols before conducting visits.
Physical Activity.
On the morning of the first day, the data collector fit participating children and providers with ActiGraph GT3X+ accelerometers (ActiGraph, Pensacola, FL). Accelerometers were attached to a belt placed over the right hip. Children wore accelerometers for 3 consecutive days (1) and providers for 7 days, except while sleeping at night or participating in water-based activities.
Once accelerometers were returned, data were downloaded and processed using the ActiLife software (ActiGraph) and specifying a 15-second epoch for children and 60-second epoch for providers. A 15-second epoch was used for children to capture the sporadic nature of their movement. The National Health and Nutrition Examination Survey nonwear algorithm was then applied to differentiate periods of wear and nonwear (33). In this algorithm, nonwear periods are defined as intervals of at least 60 consecutive minutes of 0 counts, allowing for 1 to 2 minutes of counts between 0 and 100. Data from the child care day were isolated using time stamps collected on the environmental assessment described below. For a child’s data to be considered usable, at least 2.5 hours of wear at child care (excluding naps) on at least 2 days was required. This criterion was used to include children in FCCHs that operated as half-day programs. Provider wear criteria required at least 6 hours of wear during FCCH hours on at least 2 days. One FCCH had data on only 1 child, which was deemed insufficient to represent the FCCH and was excluded from analyses. This resulted in a total analytic sample of 495 children.
Age-appropriate cut points were applied to calculate minutes of PA intensities and SB during the FCCH day. Child cut points were <25 counts per 15 seconds for SB (excluding naps), 25 to 573 counts per 15 seconds for light PA, and ≥ 574 counts per 15 seconds for MVPA (8,24). Adult cut points were <100 counts per minute for SB and >2020 counts per minute for MVPA (33). The length of the child care day varied across FCCHs; therefore, estimates were expressed as minutes per hour.
Anthropometries.
During the visit, the data collector measured height and weight of participating children and the FCCH provider. Height was measured to the nearest 1/8 in using a Shorr portable stadiometer (Shorr Productions, LLC, Olney, MD). Weight was measured to the nearest 0.1 pound using a Seca model 874 portable electronic scale (Seca Corporation, Columbia, MD). All measures were taken in light clothing with shoes removed. Height and weight measures were taken twice. If the difference between the 2 measures exceeded predetermined criterion (>1/4 in or 0.3 pound for children and >1/4 in or 1 pound for providers), a third measure was taken. The 2 closest measures were averaged. Body mass index (BMI, in kilogram per meter squared) was calculated from height and weight data. For children, BMI was used to calculate age- and sex-specific BMI percentiles. Growth standards from the World Health Organization were used for children under 2 years old (44), whereas reference data from the Centers for Disease Control and Prevention were used for children 2 years and older (18).
Demographic Surveys.
Demographic information was collected from parents of participating children and the FCCH provider. The parent demographic survey captured child date of birth, race/ethnicity, and sex. FCCH providers reported their own age, race/ethnicity, and education. Providers also reported FCCH characteristics, including participation in the Child and Adult Care Food Program and the FCCH’s rating in the North Carolina quality rating and improvement system.
PA Environment.
The PA environment at the FCCH was assessed using the Environment and Policy Assessment and Observation for FCCHs (EPAO-FCCH), which was modified for use with FCCHs and updated to align with current best practices. The EPAO-FCCH is a comprehensive measure of the nutrition- and PA-related provisions, practices, and policies within FCCHs and has demonstrated good reliability and validity evidence (40). The EPAO-FCCH is a full-day observation, beginning with the first meal of the day and continuing until the majority of the children leave the FCCH that day, as well as a review of policy and education documents (eg, parent handbook, newsletters, sample contract, training documents).
Environment and Policy Assessment and Observation for family child care homes data were used to describe key environmental components, to assess compliance with PA best practices for FCCHs, and to calculate environmental component subscores and an overall environment score. First, EPAO-FCCH data were summarized (eg, minutes of morning and afternoon outdoor play time summed and averaged between observation days). Second, the EPAO-FCCH scoring rubric was used to rate the FCCH PA environment according to the summarized observation data. The rubric assesses compliance with PA, ST, and outdoor play and learning best practices (27 practices) that were previously identified by Go Nutrition and Physical Activity Self-Assessment for Child Care (NAPSACC) for FCCHs (41). Best practices are scored on a 0 to 3 scale, with 0 indicating minimally acceptable practice and 3 indicating full compliance. These 27 best practices are categorized into 10 environmental components and averaged to produce component subscores (Table 1). Environmental components include: PA time provided, indoor play equipment, PA practices, PA education and professional development, PA policy, outdoor playtime provided, outdoor play environment, ST, ST practices, and ST policy. Subscores are then summed to determine the overall PA environment score, with potential scores ranging from 0 to 30. Higher subscores and overall score indicate better adherence to best practice standards (higher quality environments).
Table 1.
EPAO-FCCH PA Subscores
| EPAO subscore | Number of items | Subscore description |
|---|---|---|
| PA time provided | 3 | Amount of time allotted for PA each day |
| Indoor play equipment | 2 | Types and availability of portable play equipment and PA-related classroom materials (books and posters/pictures) |
| PA practices | 3 | Interactions between teachers and children around PA (eg, PA is not withheld as punishment for bad behavior) |
| PA education and professional development | 4 | Frequency and content of parent and child education, teacher professional development covering children’s PA |
| PA policy | 1 | Comprehensive, written policy including content around PA amount, equipment, and teacher practices |
| Outdoor playtime | 2 | Amount of time and number of play sessions allotted for outdoor playtime |
| Outdoor play environment | 5 | Presence and availability of portable play equipment, number of play spaces, and presence of shaded areas |
| Screen time | 4 | Amount of screen time provided, use of solely commercial-free and educational shows, and presence of televisions |
| Screen time practices | 2 | Interactions between teachers and children during screen time (eg, teachers talk with children about what they watch) |
| Screen time policy | 1 | Comprehensive, written policy including content around screen time type, use, and teacher practices |
Abbreviations: EPAO-FCCH, Environment and Policy Assessment and Observation for family child care homes; PA, physical activity. Note: All subscores are scored such that higher scores indicate better compliance with Go NAPSACC best practice standards and higher quality FCCH environments.
Statistical Analysis
Means and SDs were calculated for children’s activity behaviors and EPAO-FCCH variables. Two mixed-effects models were fit to quantify associations between child activity behaviors during the child care day and EPAO-FCCH subscores, 1 for MVPA and 1 for SB. In both models, activity behaviors were expressed as minutes per hour. Random effects were included to account for clustering of children within FCCHs. EPAO-FCCH subscores were dichotomized using a median split. Additional characteristics (ie, child age, sex, FCCH Child and Adult Care Food Program participation, provider MVPA) were examined as potential confounders based on previous literature. These variables were not included in final models of the FCCH environment and child behaviors as they did not change the magnitude or precision of associations. Cohen d effect sizes were calculated to quantify relationships beyond sample size constraints (6). Analyses were performed in SAS (v9.3; SAS Institute, Cary, NC). No formal power analysis was conducted prior to this study as this was a secondary analysis of existing data.
Results
Sample Characteristics
Children (n = 495) were approximately 3 years old, and most children were either non-Hispanic black (63%) or non-Hispanic white (25%) (Table 2). The average child BMI percentile was 64%. FCCH providers (n = 165) were all female and on average 49 years old. The majority were non-Hispanic black (74%). In addition, the majority of providers were overweight or obese (90%; BMI > 25).
Table 2.
Sample Characteristics
| Providers (n = 165) | Children (n = 495) | |
|---|---|---|
| Age (mean), y | 49.3 (9.1) | 2.9 (0.9) |
| Female | 165 (100%) | 250 (50%) |
| Race | ||
| Non-Hispanic black | 123 (74%) | 314 (63%) |
| Non-Hispanic white | 28 (17%) | 123 (25%) |
| Other | 15 (9%) | 58 (12%) |
| BMI measures (mean) | ||
| BMI, kg/m2 | 33.3 (7.5) | 16.8 (1.9) |
| BMI percentile | n/a | 63.9% (28.8%) |
| Educationa | ||
| High school diploma or GED | 41 (25%) | |
| Associate’s degree or 60 credit hours | 82 (49%) | |
| Bachelor’s degree or higher | 42 (25%) | |
| CACFP participantb | 155 (91%) | |
| FCCH star rating (mean)c | 3.8 (1.0) |
Abbreviations: BMI, body mass index; CACFP, Child and Adult Care Food Program; FCCH, family child care home; GED, general equivalency diploma.
One provider did not report education level.
CACFP is a national program that provides reimbursement to providers serving meals and snacks to eligible children from low-income families and was used in this study to indicate those FCCH that serve lower income children.
Star rating is the North Carolina quality rating and improvement system, which rates FCCHs on a scale from 1 (low) to 5 (high). This rating system is not specifically linked to physical activity but indicates overall quality.
Child and Provider PA and SB
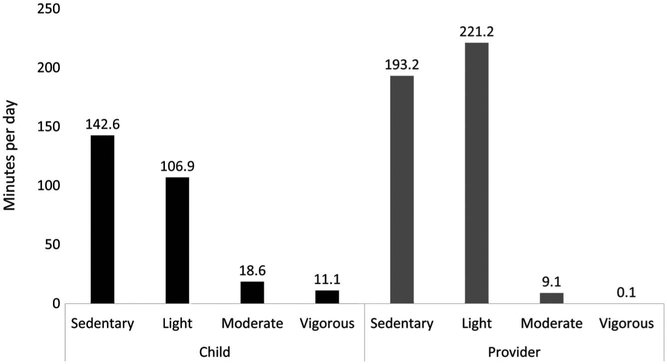
Average accelerometer wear time was 6.5 (1.4) hours for children and 7.1 (1.3) hours for providers. During the FCCH day, children accumulated an average of 143 (42) minutes of sedentary time and 30 (13) minutes of MVPA (Figure 1). Average total PA (ie, nonsedentary time) was 136.5 (2.6) minutes, and the average counts per minute estimate was 557 (12) (data not shown). Providers accumulated an average of 193.2 (58.4) minutes of SB and engaged in 9.1 (8.8) minutes of MVPA during FCCH hours.
Figure 1 —
Child and provider physical activity and sedentary behavior estimates. Child and provider daily physical activity and sedentary behavior estimates were obtained from accelerometry. Child sedentary estimate excludes nap time.
FCCH PA Environment
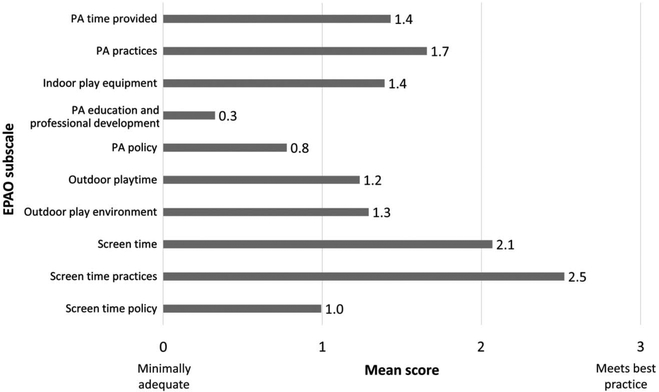
Children were provided an average of 44 (33) minutes of outside play time and 15 (12) minutes of teacher-led PA (either indoor or outdoor) each day. The overall quality of the FCCH PA environment was poor as shown in Figure 2. FCCHs scored highest on the ST (2.1 [0.6]) and ST practices (2.5 [0.6]). Subscores with the lowest scores were PA education and professional development (0.3 [0.3]) and PA policy (0.8 [0.7]). The overall PA score could range from 0 to 30; the scores in our sample ranged from 6.8 to 17.4, with an average score of 12.7 (2.1).
Figure 2 —
EPAO-FCCH subscores. Average subscores for the 10 environmental components measured in the EPAO-FCCH are presented. Individual items were averaged into a subscore, and the subscores were summed to the overall environmental score. EPAO-FCCH indicates Environment and Policy Assessment and Observation for family child care homes; PA, physical activity.
Relationships Between FCCH Environment and Child PA and Sedentary Behavior
Associations of minutes per hour of child MVPA or SB and total FCCH environment score were generally weak and did not reach statistical significance (Table 3). Several environmental subscores showed strong relationships with child accelerometer outcomes in the expected directions based on large Cohen d estimates (≥0.8) (6). PA time provided and outdoor playtime were positively associated with children’s MVPA (Cohen d =1.29 and 1.58, respectively). PA time provided, outdoor play environment, and PA education and professional development were negatively associated with children’s sedentary time (Cohen d = 1.26, 0.97, 0.88, respectively). Although most associations were in the expected direction, there were a few exceptions. There was a negative association between ST practices and children’s hourly MVPA (Cohen d = 1.65) and a positive association between the ST and children’s sedentary time (Cohen d =1.88). For these associations, better ST practices (eg, lower amount of ST, televisions not visible in home) were associated with less MVPA and more SB.
Table 3.
Relationships Between EPAO-FCCH Subscores and Child PA and SB
| MVPA, min/h | SB, min/h | |||
|---|---|---|---|---|
| β estimate (95% CI)a | ES | β estimate (95% CI) | ES | |
| Intercept | 5.46 (3.52 to 7.41) | 38.38 (33.14 to 43.62) | ||
| PA time provided | 0.28 (−0.16 to 0.73) | 1.29 | −0.85 (−2.05 to 0.34) | −1.26 |
| PA practices | 0.09 (−0.77 to 0.95) | 0.44 | 0.20 (−2.12 to 2.52) | 0.82 |
| Indoor play equipment | 0.31 (−0.31,0.94) | −0.24 | 0.45 (−1.19 to 2.09) | 0.54 |
| PA education and professional development | −0.10 (−0.75 to 0.56) | −0.31 | −0.64 (−2.09 to 0.80) | −0.88 |
| PA policy | −0.15 (−0.53 to 0.22) | −0.11 | 0.42 (−0.58 to 1.43) | 1.60 |
| Outdoor playtime | 0.32 (−0.08 to 0.72) | 1.58 | 0.09 (−1.47 to 1.66) | 0.12 |
| Outdoor play environment | −0.48 (−1.34 to 0.38) | 0.28 | −0.80 (−2.43 to 0.83) | −0.97 |
| Screen time | −0.18 (−0.78 to 0.42) | 0.04 | 1.62 (−0.07 to 3.30) | 1.88 |
| Screen time practices | −0.34 (−0.92 to 0.23) | −1.65 | 1.07 (−0.48 to 2.62) | 0.01 |
| Screen time policy | −0.07 (−0.83 to 0.69) | −1.30 | 1.72 (−1.55 to 5.00) | 1.04 |
Abbreviations: CI, confidence interval; EPAO-FCCH, Environment and Policy Assessment and Observation for family child care homes; ES, effect size; MVPA, moderate to vigorous PA; PA, physical activity; SB, sedentary behavior.
β estimates are from models fit for either child MVPA or SB. Each of the 10 subscores was included in the model. Additional adjustment for demographic characteristics is not presented, as no characteristics were identified as important confounders. EPAO-FCCH subscores are hypothesized to be related positively with MVPA and negatively with SB. No associations reached statistical significance at an α = .05 level.
Discussion
The current study assessed the PA and SB of young children attending FCCHs, described the PA environment of FCCHs, and examined associations between children’s activity behaviors and FCCHs’ environments among a sample of FCCHs in North Carolina. Key findings from this study are the poor activity profiles of children while attending FCCHs and the lack of environmental supports in FCCHs to support child activity. Furthermore, 4 components of the FCCH environment were associated with either increased PA or decreased sedentary time (ie, PA time provided, PA education and professional development, outdoor playtime, and outdoor play environment). However, 2 environmental components had associations in the opposite direction (ie, ST and ST practices). None of these associations reached statistical significance but corresponded with large Cohen d effect sizes (6). Results from this study can inform future interventions or policy efforts focused on improving PA of children attending FCCHs by identifying aspects of the FCCH environment that could be targeted.
Findings from this study call attention to the need to increase the PA that children receive while at child care. Nearly all children (91%) obtained the 15 minutes of nonsedentary time per child care hour recommended by the National Academy of Medicine (formerly, Institute of Medicine) (16). However, very little of children’s nonsedentary time was MVPA, only about 5 minutes per hour. This finding is consistent with 2 other FCCH-based studies (7,28). Together, these studies suggest that children in FCCHs have lower levels of MVPA than children attending child care centers (2,14,22,25–27). Recent 24-hour movement guidelines from Australia (21) and Canada (32) recommend that a healthy 24 hours for children 1 year and older should include ≥180 minutes of total activity and for 3- to 4-year-olds also include 60 minutes of “energetic play” (ie, MPVA). Projecting the partial-day data in this study to a full 8-hour day of care, children in full-day care in FCCHs could accumulate 172 minutes of total PA and about 40 minutes of energetic play. Although this estimate includes data from children less than 3, for whom there are no agreed on recommendations for a specific amount of energetic play, the wide gap between PA levels measured in this sample and the recommendations highlight the need to improve young children’s PA behaviors. FCCH programs could help children meet this recommendation by providing more opportunities for energetic play.
Although not a primary focus of the study, the low levels of FCCH providers are notable—providers accumulated an average of 9 minutes of MVPA during FCCH hours. The FCCH day accounted for about 50% of providers’ total accelerometer wear time, and providers do not compensate for these low levels of PA outside of the FCCH day. Only 1 provider accumulated the recommended 60 minutes of MVPA daily (data not shown) (37). This suggests that efforts to improve FCCH environments may need to include a focus on changing providers’ opinions of PA or their PA and SBs to positively impact those of children in their care.
Low EPAO-FCCH environmental subscores suggest that intervention efforts are needed across all aspects of the environment; however, priority targets should be identified so that interventions may have the greatest impact under realistic constraints, such as time and funding. These low scores are of great concern because best practice standards used to score the EPAO-FCCH were developed specifically for FCCHs, informed by current research evidence for ECE settings and by practitioners with expertise in FCCHs (41). Thus, these standards should be feasible for FCCH providers to meet. Based on these data, particular attention should be paid to standards regarding PA education and professional development, as well as PA and ST policies, as these were the environmental components with the lowest scores. Notably, a little more than half (64%) had received training on PA. Findings from this study suggest that PA time provided, PA education and professional development, outdoor playtime, and outdoor play environment may be important environmental components to target, given their stronger associations with child activity behaviors. Similar environmental components have been identified as important for centers, specifically time provided and physical spaces (4,10,11,38,39). For these components, intervention strategies that have been successful in center-based interventions may also be successful in FCCHs (eg, increasing outdoor playtime) (36). Future interventions must help providers prioritize PA even when faced with competing demands related to young children’s development (eg, literacy and numeracy objectives).
In addition to a focus on priority target areas within FCCH providers, successful intervention efforts will need to address the unique challenges faced by FCCH providers. For example, FCCH providers generally care for a range of children from infants to preschoolers, who are at different developmental stages. As such, the limited indoor and outdoor play areas and time provided for PA programming must accommodate the needs all ages of children. Interventions must help providers effectively navigate these challenges. Providing information on how to create play areas that support infant, toddler, and preschooler activity in a limited space or ideas for providing teacher-led activities that accommodate the different levels of motor skills of toddlers and preschoolers could be helpful. The counterintuitive findings showing that ST and ST practices were negatively associated with children’s MVPA suggest that FCCH providers use screens differently. Data collectors often observed that ST was not a sedentary activity but instead was used to lead active play sessions (eg, using a YouTube video to lead a music and movement session). Although most recommendations suggest limiting ST in child care, it may provide a useful resource for FCCH providers trying to provide teacher-led activities that appeal to different ages of children. Overall, FCCH providers must be able to navigate the challenges unique to the FCCH setting, prioritize PA, and implement a quality PA program, so that the FCCHs can support healthy behaviors in children.
This study is the largest of children attending FCCHs and is strengthened by the use of rigorous, objective measurements of child activity behaviors and direct observations of the FCCH environment. Measuring PA and SBs across 3 days may not fully represent usual behavior, although evidence suggests that it may be sufficient to capture in-school PA (1). In addition, this study used the same accelerometer cut points for all children in the study, including those between 1.5 and 2 years old. This likely would not have impacted SB estimates but may have underestimated MVPA in the few toddlers present in the sample (34). Furthermore, the homogenous sample may limit generalizability to other FCCHs and may have resulted in a lack of sufficient variation and thereby power to detect important relationships. Finally, the cross-sectional nature of the data precludes us from making causal inferences. Low variability of children’s PA levels and the FCCH environment may explain, in part, the lack of significant associations identified; however, this is likely not a measurement issue, as there is evidence from this study of significant relationships between the nutrition FCCH environment and children’s eating behaviors (3).
Conclusions
Family child care homes are an important setting for young children’s growth and development; however, our results indicate that these environments are not currently ideal for supporting healthy PA habits in children. Future studies with more diverse samples will be important for understanding these relationships in contexts different than those in our sample, who were predominantly non-Hispanic black, low to middle income, and residing in North Carolina and for identifying the best areas of the FCCH environment to include in intervention efforts.
Acknowledgments
The authors would like to thank the family child care home providers, parents, and children who participated in the study and the data collectors for their dedication to the project. This work is supported by the National Heart, Lung, and Blood Institute at the National Institutes of Health (R01HL10839005). Additional support was provided by Center for Health Promotion and Disease Prevention at the University of North Carolina at Chapel Hill (UNC), which is a Prevention Research Center funded through a Cooperative Agreement with the Centers for Disease Control and Prevention (U48-DP005017) and by the CHAI Core, part of the UNC Nutrition Obesity Research Center funded by the National Institutes of Health (DK056350). The content is solely the responsibility of the authors and does not necessarily represent the official views of any funders. The authors do not have conflicts of interest to disclose. R.B. led data collection, and along with S.M. performed data cleaning. S.M. led data analysis along with C.N. and A.E.V. S.M. led the writing of the manuscript with all authors contributing to the writing and editing of the manuscript. D.S.W. and T.O., as Co-Principal Investigator’s for the Keys study (the data source for this manuscript), also directed the study’s overall design, development, and implementation. All authors have read and approved the final version of the manuscript.
Footnotes
Abbreviations: EPAO-FCCH, Environment and Policy Assessment and Observation for family child care homes; PA, physical activity. Note: All subscores are scored such that higher scores indicate better compliance with Go NAPSACC best practice standards and higher quality FCCH environments.
Contributor Information
Stephanie Mazzucca, Center for Health Promotion and Disease Prevention, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.; Prevention Research Center in St. Louis, Brown School, Washington University in St. Louis, St. Louis, MO, USA.
Cody Neshteruk, Center for Health Promotion and Disease Prevention, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.; Department of Nutrition, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.
Regan Burney, Center for Health Promotion and Disease Prevention, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA..
Amber E. Vaughn, Center for Health Promotion and Disease Prevention, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.
Derek Hales, Center for Health Promotion and Disease Prevention, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.; Department of Nutrition, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.
Truls Østbye, Community and Family Medicine, Duke University School of Medicine, Durham, NC, USA..
Dianne Ward, Center for Health Promotion and Disease Prevention, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.; Department of Nutrition, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.
References
- 1.Addy CL, Trilk JL, Dowda M, Byun W, Pate RR. Assessing preschool children’s physical activity: how many days of accelerometry measurement. Pediatr Exerc Sci. 2014;26(1):103–9. doi: 10.1123/pes.2013-0021 [DOI] [PubMed] [Google Scholar]
- 2.Beets MW, Bornstein D, Dowda M, Pate RR. Compliance with national guidelines for physical activity in U.S. preschoolers: measurement and interpretation. Pediatrics. 2011;127(4):658–64. doi: 10.1542/peds.2010-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benjamin-Neelon SE, Vaughn AE, Tovar A, Østbye T, Mazzucca S, Ward DS. The family child care home environment and children’s diet quality. Appetite. 2018;126:108–13. doi: 10.1016/j.appet.2018.03.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bower JK, Hales DP, Tate DF, Rubin DA, Benjamin SE, Ward DS. The childcare environment and children’s physical activity. Am J PrevMed. 2008;34(1):23–9. doi: 10.1016/j.amepre.2007.09.022 [DOI] [PubMed] [Google Scholar]
- 5.Brown WH, Pfeiffer KA, McIver KL, Dowda M, Addy CL, Pate RR. Social and environmental factors associated with preschoolers’ non-sedentary physical activity. Child Dev. 2009;80(1):45–58. doi: 10.1111/j.1467-8624.2008.01245.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen J Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 7.Delaney SL, Monsivais P, Johnson DB. Physical activity levels in family child care homes. J Phys Act Health. 2014;11(7):1362–6. doi: 10.1123/jpah.2012-0297 [DOI] [PubMed] [Google Scholar]
- 8.Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci. 2008;26(14):1557–65. doi: 10.1080/02640410802334196 [DOI] [PubMed] [Google Scholar]
- 9.Fees B, Trost S, Bopp M, Dzewaltowski DA. Physical activity programming in family child care homes: providers’ perceptions of practices and barriers. J Nutr Educ Behav. 2009;41(4):268–73. doi: 10.1016/j.jneb.2008.01.013 [DOI] [PubMed] [Google Scholar]
- 10.Gubbels JS, Kremers SP, van Kann DH, et al. Interaction between physical environment, social environment, and child characteristics in determining physical activity at child care. Health Psychol. 2011;30(1):84–90. doi: 10.1037/a0021586 [DOI] [PubMed] [Google Scholar]
- 11.Gubbels JS, Van Kann DHH, Jansen MWJ. Play equipment, physical activity opportunities, and children’s activity levels at childcare. J Environ Public Health. 2012;326520. doi: 10.1155/2012/326520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Henderson KE, Grode GM, O’Connell ML, Schwartz MB. Environmental factors associated with physical activity in childcare centers. Int J Behav Nutr Phys Act. 2015;12:43. doi: 10.1186/s12966-015-0198-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hinkley T, Crawford D, Salmon J, Okely AD, Hesketh K. Preschool children and physical activity: a review of correlates. Am J Prev Med. 2008;34(5):435–41. doi: 10.1016/j.amepre.2008.02.001 [DOI] [PubMed] [Google Scholar]
- 14.Hinkley T, Salmon J, Okely AD, Crawford D, Hesketh K. Preschoolers’ physical activity, screen time, and compliance with recommendations. Med Sci Sports Exerc. 2012;44(3):458–65. doi: 10.1249/MSS.0b013e318233763b [DOI] [PubMed] [Google Scholar]
- 15.Hinkley T, Teychenne M, Downing KL, Ball K, Salmon J, Hesketh KD. Early childhood physical activity, sedentary behaviors and psychosocial well-being: a systematic review. PrevMed. 2014;62:182–92. doi: 10.1016/j.ypmed.2014.02.007 [DOI] [PubMed] [Google Scholar]
- 16.Institute of Medicine. Early Childhood Obesity Prevention Policies. Washington, DC: The National Academies Press; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jones RA, Hinkley T, Okely AD, Salmon J. Tracking physical activity and sedentary behavior in childhood: a systematic review. Am J Prev Med. 2013;44(6):651–8. doi: 10.1016/j.amepre.2013.03.001 [DOI] [PubMed] [Google Scholar]
- 18.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat. 2002;11(246):1–190. [PubMed] [Google Scholar]
- 19.Laughlin L Who’s Minding the Kids? Child Care Arrangements: Spring 2011. Washington, DC:U.S. Census Bureau; 2013. [Google Scholar]
- 20.North Carolina Division of Child Development and Early Education. Child care facility search site. Available from: http://ncchildcaresearch.dhhs.state.nc.us/search.asp?lang=English
- 21.Okely AD, Ghersi D, Hesketh KD, et al. A collaborative approach to adopting/adapting guidelines—The Australian 24-hour movement guidelines for the early years (birth to 5 years): an integration of physical activity, sedentary behavior, and sleep. BMC Public Health. 2017;17 Suppl 5:869. doi: 10.1186/s12889-017-4867-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oliver M, Schofield GM, Kolt GS. Physical activity in preschoolers: understanding prevalence and measurement issues. Sports Med. 2007; 37(12):1045–70. doi: 10.2165/00007256-200737120-00004 [DOI] [PubMed] [Google Scholar]
- 23.Østbye T, Mann CM, Vaughn AE, et al. The keys to healthy family child care homes intervention: study design and rationale. Contemp Clin Trials. 2015;40:81–9. doi: 10.1016/j.cct.2014.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pate RR, Almeida MJ, McIver KL, Pfeiffer KA, Dowda M. Validation and calibration of an accelerometer in preschool children. Obesity. 2006;14(11):2000–6. doi: 10.1038/oby.2006.234 [DOI] [PubMed] [Google Scholar]
- 25.Pate RR, O’Neill JR, Brown WH, Pfeiffer KA, Dowda M, Addy CL. Prevalence of compliance with a new physical activity guideline for preschool-age children. Child Obes. 2015;11(4):415–20. doi: 10.1089/chi.2014.0143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pate RR, Pfeiffer KA, Trost SG, Ziegler P, Dowda M. Physical activity among children attending preschools. Pediatrics. 2004;114(5):1258–63. doi: 10.1542/peds.2003-1088-L [DOI] [PubMed] [Google Scholar]
- 27.Reilly JJ. Low levels of objectively measured physical activity in preschoolers in child care. Med Sci Sports Exerc. 2010;42(3):502–7. doi: 10.1249/MSS.0b013e3181cea100 [DOI] [PubMed] [Google Scholar]
- 28.Rice KR, Trost SG. Physical activity levels among children attending family day care. J Nutr Educ Behav. 2014;46(3):197–202. doi: 10.1016/j.jneb.2013.09.001 [DOI] [PubMed] [Google Scholar]
- 29.Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc. 2000;32(5): 963–75. doi: 10.1097/00005768-200005000-00014 [DOI] [PubMed] [Google Scholar]
- 30.Tandon PS, Tovar A, Jayasuriya AT, et al. The relationship between physical activity and diet and young children’s cognitive development: a systematic review. Prev Med Rep. 2016;3:379–90. doi: 10.1016/j.pmedr.2016.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Timmons BW, LeBlanc AG, Carson V, et al. Systematic review of physical activity and health in the early years (aged 0–4 years). Appl Physiol Nutr Metab. 2012;37(4):773–92. doi: 10.1139/h2012-070 [DOI] [PubMed] [Google Scholar]
- 32.Tremblay MS, Chaput JP, Adamo KB, et al. Canadian 24-hour movement guidelines for the early years (0–4 years): an integration of physical activity, sedentary behaviour, and sleep. BMC Public Health. 2017;17 Suppl 5:874 doi: 10.1186/s12889-017-4859-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8. doi: 10.1249/mss.0b013e31815a51b3 [DOI] [PubMed] [Google Scholar]
- 34.Trost SG, Fees BS, Haar SJ, Murray AD, Crowe LK. Identification and validity of accelerometer cut-points for toddlers. Obesity. 2012;20(11):2317–9. doi: 10.1038/oby.2011.364 [DOI] [PubMed] [Google Scholar]
- 35.Tucker P The physical activity levels of preschool-aged children: a systematic review. Early Child Res Q. 2008;23(4):547–58. doi: 10.1016/j.ecresq.2008.08.005 [DOI] [Google Scholar]
- 36.Tucker P, Vanderloo LM, Johnson AM, et al. Impact of the Supporting Physical Activity in the Childcare Environment (SPACE) intervention on preschoolers’ physical activity levels and sedentary time: a single-blind cluster randomized controlled trial. Int J Behav Nutr Phys Act. 2017;14(1):120. doi: 10.1186/s12966-017-0579-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.US Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Hyattsville, MD; 2008. [Google Scholar]
- 38.Vanderloo LM, Tucker P, Johnson AM, Burke SM, Irwin JD. Environmental influences on preschoolers’ physical activity levels in various early-learning facilities. Res Q Exerc Sport. 2015;86(4):360–70. doi: 10.1080/02701367.2015.1053105 [DOI] [PubMed] [Google Scholar]
- 39.Vanderloo LM, Tucker P, Johnson AM, van Zandvoort MM, Burke SM, Irwin JD. The influence of centre-based childcare on preschoolers’ physical activity levels: a cross-sectional study. Int J Environ Res Public Health. 2014;11(2):1794–802. doi: 10.3390/ijerph110201794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vaughn AE, Mazzucca S, Burney R, et al. Assessment of nutrition and physical activity environments in family child care homes: modification and psychometric testing of the environment and policy assessment and observation. BMC Public Health. 2017;17(1):680. doi: 10.1186/s12889-017-4686-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ward D, Morris E, McWilliams C, et al. Go NAP SACC: Nutrition and Physical Activity Self-Assessment for Child Care. 2nd ed. Center for Health Promotion and Disease Prevention and Department of Nutrition, University of North Carolina at Chapel Hill; 2014. Available from: https://gonapsacc.org/resources/nap-sacc-materials/GoNAPSACCICPA_2014_Copyright.pdf [Google Scholar]
- 42.Ward DS, Vaughn AE, Burney RV, Østbye T. Recruitment of family child care homes for an obesity prevention intervention study. Contemp Clin Trials Commun. 2016;3:131–8. doi: 10.1016/j.conctc.2016.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ward DS, Vaughn AE, McWilliams C, Hales D. Interventions for increasing physical activity at child care. Med Sci Sports Exerc. 2010;42(3):526–34. doi: 10.1249/MSS.0b013e3181cea406 [DOI] [PubMed] [Google Scholar]
- 44.WHO Multicentre Growth Reference Study Group. WHO child growth standards based on length/height, weight and age. Acta Paediatr Suppl. 2006;450:76–85. [DOI] [PubMed] [Google Scholar]