Abstract
Background
Lower extremity injuries in soccer players are extremely common. Implementation of group injury prevention programs has gained popularity due to time and cost-effectiveness. Unfortunately, players with greater number of risk factors are most likely to sustain an injury, yet less likely to benefit from a group injury prevention program. The purpose of this study was to determine if targeting these high risk players with one-on-one treatment would result in a reduction in the number of risk factors they possess. The authors hypothesized that fifty percent or more of subjects receiving one-on-one intervention would have a reduction of ≥1 risk factor(s).
Study Design
Quasi-experimental pretest-posttest design.
Methods
Division I men's and women's soccer players were screened for modifiable risk factors using a battery of tests which assessed mobility, fundamental movement pattern performance, motor control, and pain. Players with ≥ 3 risk factors (“high risk”) received one-on-one treatment from a physical therapist via an algorithm twice per week for four weeks. Players with < 3 risk factors (“low risk”) did not receive one-on-one intervention.
Results
The proportion of treatment successes in the intervention group was 0.923 (95% CI 0.640-0.998). A significant proportion of high risk subjects (0.846) became low risk at posttest (p = 0.003). A significant between group difference was noted in risk factor change from pretest to posttest (p = 0.002), with the median risk factor change in the intervention group being -3.
Conclusion
Utilizing one-on-one interventions designed to target evidence-based risk factors is an effective strategy to eliminate LE musculoskeletal injury risk factors in high risk individuals.
Levels of Evidence
2b
Keywords: injury prevention, injury risk, soccer, movement system
INTRODUCTION
Injuries to the lower extremity (LE) are common in collegiate soccer players, with injuries to the ankle, knee and thigh having the highest incidence.1 Identification of risk factors presents a challenge to clinicians and coaching staffs. Many modifiable risk factors, or those factors that respond favorably to common rehabilitation techniques, have been identified for musculoskeletal injuries in soccer players and analogous populations. The volume of modifiable risk factors is overwhelming; thus many injury prevention programs, like Sportsmetrics™ or the Prevent Injury and Enhance Performance program, have focused on addressing the risk factors associated with a single joint or injury. This program specialization is not comprehensive and leaves athletes vulnerable to injuries at adjacent joints. Therefore, a battery of tests examining risk factors common to several LE injuries may provide a more comprehensive approach to injury prevention.
With the limited resources available to many clinicians and coaching staffs, tests to identify common risk factors should be field-expedient and cost-effective. Testing should also provide clear, fundamental impairments for clinicians to address. In a movement hierarchy, basic range of motion (ROM), flexibility, strength, balance, and movement pattern competency precedes development of higher level skills like running and jumping.2 Many commonly administered tests, such as the drop jump or Landing Error Scoring System, require athletes to use higher level skills. While these tests have demonstrated some utility in injury prediction,3,4 it may be more effective and efficient to establish basic movement competency prior to performing higher level tests. Risk factors can be categorized into three domains: mobility, fundamental patterns, and neuromuscular control.
Mobility: Mobility deficits, particularly in the hip and ankle, have been identified as risk factors for LE injury.5,6 Verrall et al found that hip external rotation (ER) ROM was significantly lower in athletes that went on to develop groin pain.5 Not only has total ankle dorsiflexion ROM shown a relationship to injury, but an asymmetry of ≥6.5 degrees was associated with a four-fold increase in risk for future musculoskeletal injury in a population of warrior athletes.7 Though deficits in trunk or core neuromuscular control has been identified as a risk factor for LE injuries, limited attention has been paid to trunk mobility. To date, no study has examined the relationship between thorax mobility and LE injury. The role of the trunk during walking and running tasks has long been documented biomechanically.8 Recently researchers have observed that trunk mobility is increased in subjects with chronic ankle instability during lower limb reaching tasks.9 Given that peripheral deficits can influence trunk mechanics, it is plausible that limitations in thorax mobility could influence LE mechanics thereby contributing to overall injury risk.
Fundamental Patterns: Asymmetry in fundamental patterns has also been associated with an increase in injury risk. For example, asymmetry identified by the Functional Movement ScreenTM (FMSTM) has been associated with an increased odds for a time-loss musculoskeletal injury in athletes.10,11 Presence of pain during this movement testing also increases risk for injury. In a population of Army soldiers, the presence of pain with performance of fundamental patterns led to ORs (odds ratios) ranging from 1.50 to 3.51 for future musculoskeletal injury.12
Neuromuscular Control: Deficits in neuromuscular control have also been identified as a risk factor for LE injuries. Zazulak et al identified an association between knee injuries and increased trunk displacement measures following an unanticipated trunk perturbation in collegiate athletes.13 Wilkerson et al reported ORs for core or lower extremity strain of up to 4.17 in American football players with decreased trunk flexion hold times (<161 seconds).14 Finally, low composite score on the Lower Quarter Y Balance Test (YBT-LQ), a measure of dynamic neuromuscular control, has also been associated with increased risk of injury in athletic populations.15 Asymmetry in the anterior direction on the YBT-LQ, defined as > 4 cm difference in reach distance, has been shown to increase risk for LE injury in active populations.15,16
While evidence suggests that overall injury rates in soccer players have declined in recent years, non-contact injuries—which are largely preventable—are on the rise.1 Individual athletes will differ on the presence of risk factors and deficits, all in varying degrees of severity, leaving some to reap the benefits of consistent performance of an injury prevention program while others do not. This is concerning because recent evidence suggests a somewhat linear relationship in regards to number of risk factors and risk for future injury. In a population of warrior athletes, the odds of sustaining an injury increased significantly in the presence of three to five risk factors compared to two or less, with ORs ranging from 4.60-6.70.7 Additionally, collegiate athletes with the greatest number of risk factors were 3.4 times more likely to sustain a non-contact LE injury than those athletes with the least number of risk factors.17
Taken collectively, these results suggest that athletes with a greater number of risk factors are at the highest risk for injury, and may benefit from a more individualized approach to decrease risk. Identifying these high risk individuals using tests designed to capture risk factors common to multiple LE injuries would allow for more efficient resource allocation, giving clinicians the opportunity to focus injury prevention efforts on the individuals that need it most. Therefore, the purpose of this study was to determine if targeting these high risk players with one-on-one treatment would result in a reduction in the number of risk factors they possess. The authors hypothesized that fifty percent or more of players treated with one-on-one interventions will have a reduction of ≥1 risk factors.
METHODS
Data Collection Procedures
The study utilized a quasi-experimental pretest-posttest design. Returning men's and women's division I soccer players at a local university were recruited in March 2017 for this study. Study volunteers were issued and signed an informed consent. Informed consent and all study procedures were approved by the Institutional Review Board of the University of Kentucky and the University of Evansville. Players were excluded from the study if any of the following were present: current musculoskeletal injury resulting in practice or workout restrictions from a healthcare provider; recent (within 3 months) surgery; other non-musculoskeletal issue resulting in practice or workout restrictions from a healthcare provider; current recipient of musculoskeletal care from other healthcare provider.
All data collection procedures took place in a laboratory classroom on campus. Players completed a demographic form, which included gender and player position, as well as medical, surgical, and injury history information. Height and weight were measured using a standard beam scale with height rod. Subjects were then measured for limitations in active ROM in three areas: closed chain ankle dorsiflexion, hip ER, and thorax rotation. All ROM values were captured as a continuous measurement, then dichotomized as “risk factor present/risk factor absent” based on normative values for each measurement. All definitions for risk factor presence are summarized in Table 1. Closed chain ankle dorsiflexion was measured in degrees using an inclinometer at the most distal aspect of the tibial tuberosity, with the subject in a half-kneeling position. Hip ER was measured passively in degrees using an inclinometer placed just superior to the lateral malleolus with the subject in prone. Finally, thorax rotation was measured in degrees with an inclinometer, with the subject in a lumbar locked position (full hip and knee flexion, full lumbar flexion). The subject's non-testing elbow was placed at his or her midline on the testing surface, with the dorsal aspect of the testing hand placed in the lumbosacral area. The inclinometer was centered at C7 interspace and the subject was asked to upwardly rotate toward the testing arm and ceiling.
Table 1.
Risk factor definitions and criteria for pass or fail (absent or present).
| Risk Factors | Test | Dichotomous Pass (Risk Factor Absent) | Dichotomous Fail (Risk Factor Present) |
|---|---|---|---|
| Thorax mobility28,29 | Lumbar locked thorax rotation | ≥50 ° | <50 ° |
| Ankle mobility7 | Closed Kinetic Chain Dorsiflexion | Asymmetry of < 5 ° or no asymmetry | Asymmetry of ≥ 5 ° |
| Ankle mobility30 | Closed Kinetic Chain Dorsiflexion | ≥35 ° | <35 ° |
| Hip mobility31,32 | Prone passive ER | ≥40 ° | <40 ° |
| Fundamental movement10,11 | Supine active straight leg raise | Lateral malleolus of leg raised clears superior patella of contralateral leg | Lateral malleolus of leg raised does not clear superior patella of contralateral leg |
| Fundamental movement10,11 | Standing lunge | Able to complete a lunge pattern with feet 1 tibia length apart in tandem | Unable to complete lunge pattern with feet 1 tibia length apart in tandem |
| Fundamental movement10,11 | Standing hurdle step | Able to clear hurdle 1 tibia length from the floor, tap heel on the floor, then return to start position | Unable to clear hurdle 1 tibia length from the floor, tap heel on the floor, then return to start position |
| Neuromuscular Control19 | YBT-UQ | Men: ≥ 85.1%, Women: ≥ 83.9% | Men: < 85.1%, Women: < 83.9% |
| Neuromuscular Control15,16 | YBT-LQ | Anterior reach asymmetry of <4 cm | Anterior reach asymmetry of ≥4 cm |
| Neuromuscular Control15 | YBT-LQ | >95% | ≤95% |
| # of painful patterns7 | Pain with movement testing | No pain reported | Pain reported |
Neuromuscular control was assessed next using the YBT-LQ and YBT-UQ, using procedures as described by Plisky et al18 and Gorman et al,19 respectively. Briefly, the YBT-LQ requires subjects to stand on one leg on the testing kit and push an indicator box as far as possible with the contralateral leg in the anterior, posteromedial, and posterolateral directions. For the YBT-UQ, subjects were in a push up position on the testing kit and instructed to push the indicator box in the medial, inferolateral and superolateral directions, respectively, as far as possible. All procedures were performed bilaterally.
Finally, fundamental movement was measured using three tasks: active straight leg raise, hurdle step, and in-line lunge. These fundamental tasks are components of the FMSTM, and were performed and scored as previously described.20,21 A risk factor was considered present if a subject scored a zero or a one. Additionally, a continuous measure of hip flexion ROM accompanied the active straight leg raise task, with an inclinometer placed at the superior aspect of the patella.
Raters
Nine raters were used during the screening process, each assigned to a specific station. Height and weight, upper and lower extremity length were measured by physical therapy students, while all other measurements were collected by licensed physical therapists with 1-15 years of experience. Those raters with the fewest years of experience were enrolled in a sports residency, and those raters with the most experience were board certified in either sports or orthopedics. Each rater was trained in data collection procedures for his or her assigned station with verbal instructions and demonstrations. Each rater then performed data collection procedures on 10 individuals in front of the primary investigator to ensure procedures were followed and results were interpreted accurately.
Groups
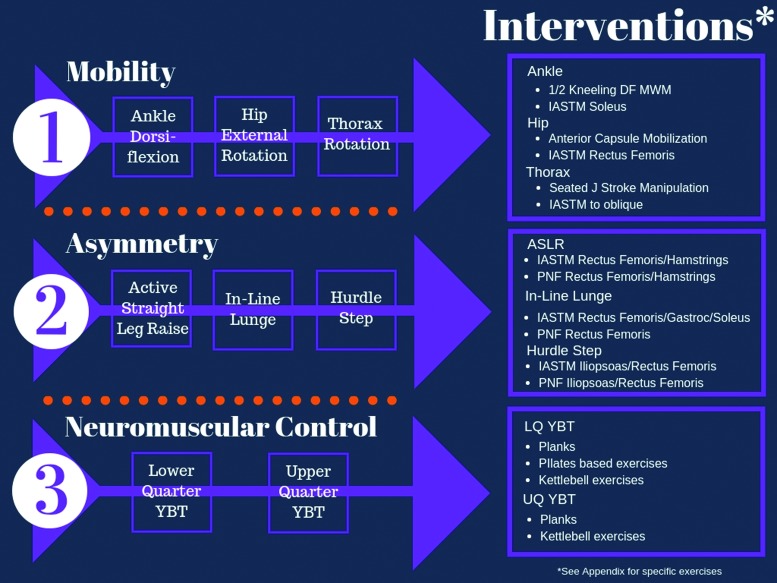
Determination of risk factor presence was performed by the primary investigator after data collection was complete, based on previously established criteria. Subjects with ≥ 3 risk factors were in the intervention group, and were treated one-on-one by a physical therapist according to the algorithm in Figure 1 where risk factors are treated according to rank. All treatments were provided by one of two physical therapists (PTs) based on the availability of subjects. Both PTs were assistant professors in a doctor of physical therapy program and have certifications in strength and conditioning (CSCS). Both have board certifications, one in sports and one in orthopedics, with eight and ten years of experience, respectively. All identified risk factors were treated according to a treatment algorithm, where risk factors were ranked from top to bottom, and left to right (Figure 1). For example, all mobility deficits were treated first before addressing any deficits in fundamental patterns or neuromuscular control. Additionally, deficits within each category were treated according to rank: therefore, ankle dorsiflexion limitations were treated prior to hip ER or thorax rotation restrictions. Each deficit has an associated treatment “package” that includes manual therapy treatment and corrective exercises designed to reinforce manual treatment and improve neuromuscular control (Figure 1; NOTE: descriptions and pictures of all interventions are included in the Appendix). Treatment sessions lasted approximately 20 minutes and occurred in addition to regular practice and games. All treatments provided during one-on-one sessions were performed in the athletic training room and were documented in a treatment log, and compliance with one-on-one sessions was defined a priori as attendance of ≥90% of scheduled sessions. Players were treated 1-2 times per week for five weeks, and were instructed in home exercises to be performed independently between sessions.
Figure 1.
Intervention algorithm and associated treatment “packages”. Risk factors are ranked from top to bottom and left to right.
Subjects with < 3 risk factors were placed in the control group and did not receive one-on-one intervention. Additionally, subjects that met the criteria to receive one-on-one intervention but declined treatment were also placed in the control group. The control group returned for posttesting only.
Statistical Methods
The null hypothesis assumed that 5% of players will experience a reduction in one or more risk factors by chance, with an alternative hypothesis of ≥50% of players receiving the intervention program will experience a reduction in one or more risk factors. With a 2-tailed alpha level of significance equal to 0.05, seven players were needed in the intervention program to have >80% power to detect the hypotheses described above based on a one-sample binomial test. Compliance, defined as attendance of 90% or more of the scheduled one-on-one sessions, is required to assess the effectiveness of the program. It is expected that 15% of players enrolled in the study will be non-compliant and another 15% will experience an injury, both excluding them from per protocol analysis. Therefore, three additional subjects were enrolled for a total of 10 in the intervention program to retain adequate power.
All data were analyzed using SPSS statistical software (IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY). Descriptive statistics will be calculated for all subjects. The primary outcome variable is the proportion of treatment successes, defined as a reduction in one or more risk factors in a single athlete, which will be estimated with a 95% confidence interval. Secondary outcomes including the number of risk factors changed during the intervention as well as pre to post change in assessment outcomes were evaluated using paired t-tests with associated 95% confidence intervals.
RESULTS
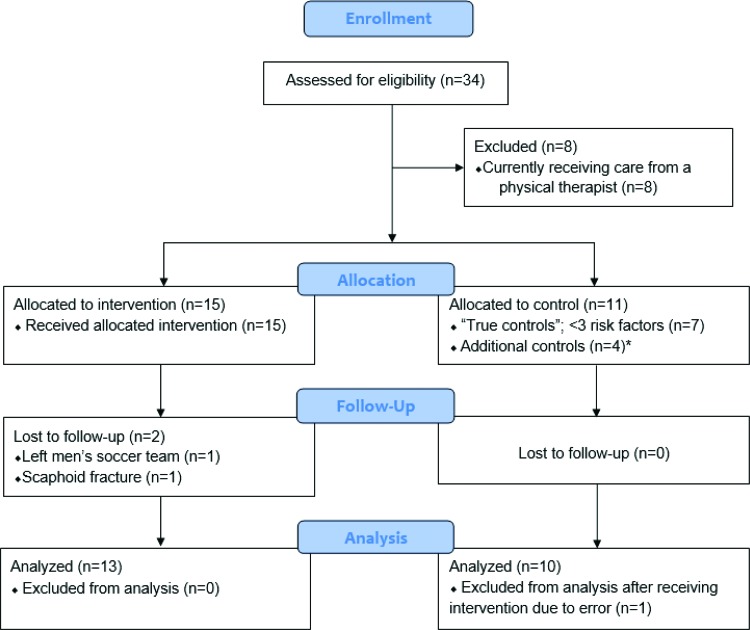
Fifteen subjects received one-on-one intervention. Ninety-three percent of treatments were provided by one PT. Two subjects in the intervention group were lost to follow up (Figure 2). Seven subjects were “true controls”, having < 3 risk factors at pretest. Four additional subjects originally allocated to the intervention group declined one-on-one intervention and returned only for follow up testing. The data from these four subjects was combined with the “true controls” to form the control group utilized in the final analysis. Finally, one subject in the control group was treated two times due to error. This subject was excluded, leaving 10 subjects in the control group for final analysis.
Figure 2.
CONSORT flowchart. *Subjects were originally allocated to the intervention group, but declined treatment and attended posttesting only. These subjects’ data was combined with the “true controls” in the final analysis.
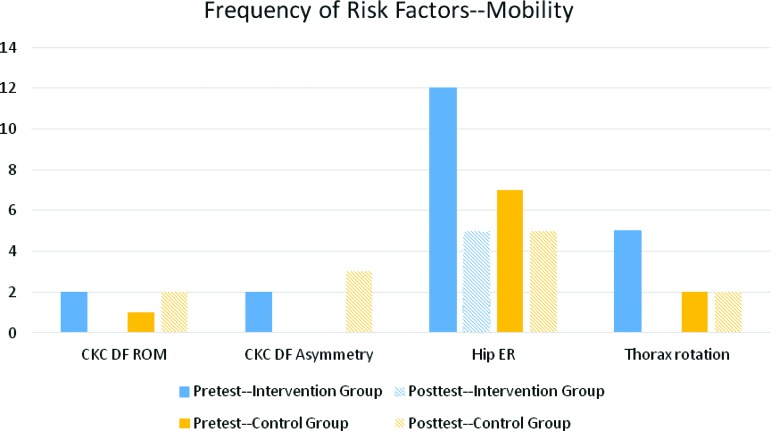
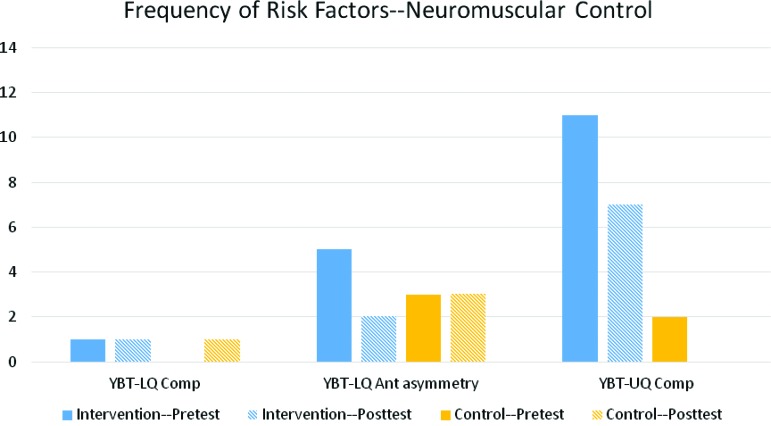
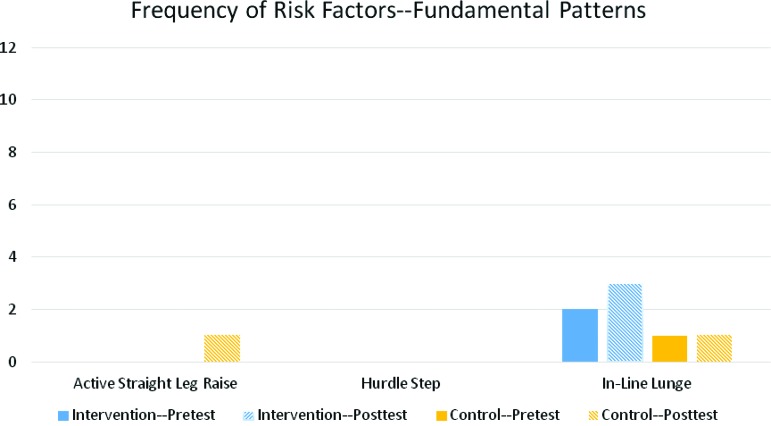
There were 13 subjects in the intervention group (8 males, 5 females) with a mean height of 70.58 ± 4.30 and a mean weight of 171.85 ± 20.36. The control group had 10 subjects (9 males, 1 female) with a mean height of 70.10 ± 2.44 and a mean weight of 169.80 ± 18.10. There were no significant differences observed between groups at pretest. The frequency of risk factors present at pretest and posttest both for the intervention and control groups are summarized in Figures 3-5.
Figure 3.
Frequency of mobility risk factors at pretest and posttest by group. Abbreviations: Closed kinetic chain dorsiflexion (CKC DF); Range of motion (ROM); External rotation (ER).
Figure 5.
Frequency of neuromuscular control risk factors at pretest and posttest by group. Abbreviations: Lower quarter Y Balance Test (YBT-LQ); Anterior (Ant); Upper quarter Y Balance Test (YBT-UQ).
Figure 4.
Frequency of asymmetry in fundamental pattern risk factors at pretest and posttest by group.
The primary outcome was proportion of treatment successes in the intervention group, which was defined a priori as a reduction of ≥1 risk factors. Of the 13 subjects treated with one-on-one intervention, 12 had a reduction of at least one risk factor at posttest, therefore the proportion of treatment successes was 0.923 (95% CI 0.640-0.998). All 13 subjects in the intervention group had ≥3 risk factors at pretest (“high risk”) and at posttest, 84.6% had < 3 risk factors (“low risk”). A McNemar's test, a form of the Chi-square statistic where subjects act as their own control,22 was used to determine significant changes in risk category. The 2 × 2 contingency table for the intervention group is presented in Table 2. The number of subjects changing from a high risk category at pretest to a low risk category at posttest was statistically significant (p = 0.003). Finally, only 10 of the 13 subjects treated with one-on-one intervention were compliant with treatment (attending ≥ 90% of sessions). Of the 10 compliant subjects, 100% had a reduction of at least one risk factor at posttest. The proportion of treatment successes for compliant subjects was 1.00 (95% CI 0.69-1.00).
Table 2.
2 2 table for McNemar's analysis.
| Posttest | ||||
|---|---|---|---|---|
| High Risk | Low Risk | Total | ||
| Pretest | High Risk (≥ 3 risk factors) | 2 | 11 | 13 |
| Low Risk (<3 risk factors) | 0 | 0 | 0 | |
| Total | 2 | 11 | 13 | |
Because the number of painful patterns and total number of risk factors were not normally distributed, a Mann-Whitney U test was performed to determine differences between groups (Table 3). The median number of painful patterns (or tests) in both groups was zero, and changes from pretest to posttest between groups was not statistically significant (p = 0.278). The median reduction of risk factors was -3 and -1 for the intervention and control groups, respectively. The difference in change in risk factors between groups was statistically significant (p = 0.002).
Table 3.
Mann Whitney U results. (*) = statistically significant.
| Original Analysis | ||||
|---|---|---|---|---|
| Factor | Group | Median | Range | p value |
| Number of painful patterns | Control | 0 | −1, 5 | 0.278 |
| Intervention | 0 | −3, 3 | ||
| Total number of risk factors | Control | −1 | −2, 4 | 0.002* |
| Intervention | −3 | −5, 0 | ||
| Modified Analysis | ||||
| Total number of risk factors | Control | 0 | −2,4 | 0.003* |
| Intervention | −3 | −5,0 | ||
DISCUSSION
The purpose of this study was to determine if one-on-one treatment—with interventions matched to address the specific deficits of each subject—was effective at reducing the number of risk factors for LE musculoskeletal injury. The interventions prescribed to each subject followed an algorithm consisting of soft tissue and joint mobilizations followed by corrective exercises to improve fundamental movement patterns and neuromuscular control. The results of this study indicate that one-on-one treatment with matched interventions is an effective approach to reduce the presence of risk factors in collegiate soccer players. While individualized treatment for every athlete would be ideal, most clinicians and coaching staffs have limited resources. Group injury prevention programs are used commonly to decrease injury risk due to the time and cost efficiency. Unfortunately many group programs have a limited scope of prevention, as they tend to address risk factors for only one joint or injury.23 Additionally, emerging research indicates that individuals at the highest risk for injury, or those with the greatest number of risk factors, are also less likely to respond to group injury preventions.24 Therefore, a systematic approach is needed to not only identify these high-risk individuals, but to provide targeted interventions as well. This system may provide a more economical alternative to group injury prevention programs by allocating resources to the individuals who need them most.
This individualized approach to injury prevention programs has been successful in other athletic populations. Kiesel et al utilized individualized corrective exercises in professional football players to improve fundamental movement patterns.25 Movement deficits for each player were identified using the FMSTM, and prescribed exercises included self and partner soft tissue work and stretching, followed by exercises to improve core function and movement patterns. Additionally, Bodden et al utilized a similar individualized program in mixed martial arts athletes by combining self-mobility and corrective exercises, in an intervention group and compared to controls.26 Taken collectively, programs targeting an individual's specific deficits with soft tissue and mobility interventions, followed by corrective exercises reinforcing fundamental movement patterns and neuromuscular control can be a successful approach to injury prevention.
Mean changes are often used to determine effectiveness of interventions. However, the effectiveness of the one-on-one, deficit-matched program could be lost if limited to this type of comparison. For example, in this study only two subjects in the intervention group had limitations in closed kinetic chain dorsiflexion ROM. Though both subjects experienced an increase in ROM (and an elimination of this risk factor), a significant difference in group mean change scores was not observed because so few subjects had a dorsiflexion deficit. Therefore, examining effectiveness on an individual level may provide a more useful way of measuring success than comparing mean changes.
One of the many challenges in injury prevention is the dichotomization of continuous variables. Cutoff scores for continuous variables are developed to determine presence of a risk factor. This presents a challenge for researchers and clinicians, as some athletes may score very near the cutpoint. Given the error associated with each measurement, when the value is close to the cutpoint, the true presence or absence of these risk factors is questionable. The most conservative interpretation was to consider this risk factor to be present in order to avoid underestimation of injury risk. Unfortunately, small changes in these measurements resulted in crossing of the dichotomous threshold, translating to an elimination of that risk factor without exceeding minimal detectable difference (MDD). Minimal detectable difference (also known as minimal detectable change) is the amount of change in a variable that exceeds measurement error, and represents a true change.22 This phenomenon is illustrated in Figure 5, where the control group demonstrates a reduction in the presence of the YBT-UQ risk factor. One female subject had low composite scores on the YBT-UQ on the right and left sides at pretest, with scores of 80.1 and 83.5, respectively. The cutoff for passing the YBT-UQ composite score (thereby removing this risk factor) for females was 83.9. At posttest, the right and left composite scores for this subject were 84.80 and 86.40, respectively. The MDD for the YBT-UQ composite score has been reported as 6.10-8.10.19 Though the posttest scores crossed the threshold for this risk factor, because the change scores for this subject fell below the MDD, the change observed may be due to measurement error and not a true change in the risk factor. A modified analysis was performed requiring the observed change for each risk factor to cross the operationally defined threshold as well as exceed MDD to qualify as a risk factor change. Even when a more conservative estimate was used, the Mann-Whitney U test revealed a statistically significant difference between the intervention and control groups with a p value of 0.003 (Table 3).
LIMITATIONS
Strength of Evidence
Limited consistency exists in the literature regarding which factors contribute to LE injury in soccer players. The purpose of this study was to combine risk factors common to multiple LE injuries to have a broader effect in injury reduction. The risk factors selected for the study have an association to LE injury in soccer players or other athletic populations, though the strength of evidence supporting each factor varies. For example, hip ER deficit was the most prevalent risk factor amongst both groups, with 82.6% of all subjects having at least one hip that failed to clear the 40 degree threshold. However, the strength of evidence supporting the ability of limited hip ER to predict LE injury is less robust than other factors. In 58.3% of cases, the interventions selected were successful at eliminating limited hip ER as a risk factor. Still, it is possible that elimination of this risk factor does not translate to a meaningful reduction in LE injury risk. Other studies have combined risk factors and stratified subjects using a weighted algorithm, where the most robust risk factors carry greater weight than less robust risk factors.17 Weighting risk factors would allow resources to be allocated to those individuals that need it most and injury prevention efforts to be focused on areas that would produce meaningful reductions in injury risk.
Subject Compliance
Three subjects received one-on-one treatment but were considered non-compliant due to poor attendance of treatment sessions. One subject attended only one treatment session and no change in risk factors was noted from pretest to posttest. The remaining non-compliant subjects attended three one-on-one sessions each, with reductions in risk factors of -1 and -5. These findings suggest that significant improvement may be possible in fewer treatments, though more than one treatment session is likely needed. Additionally, compliance with independent performance of prescribed home exercises is uncertain. Subjects in the intervention group were asked to perform prescribed exercises at least once daily and record performance in a journal supplied to them. Unfortunately only one subject returned an exercise journal one time during the intervention period. Therefore compliance with independent performance of prescribed exercises, and dosage of interventions cannot be determined.
Follow up
Long term follow up was not feasible for this study, therefore maintenance of risk factor reduction and impact on future LE risk is unknown. Most of the subjects in this study were returning home for the summer to train or compete on local travel teams. Without continued performance of corrective exercises during training, it is possible that the risk factors would return and injury risk would increase. Additionally, it is unknown if removal of these risk factors translates to a decrease in injuries. It is recommended that future studies utilize a long term follow up, preferably following players through in-season play, to determine changes in number of risk factors over time as well as translations to injury rate reduction.
CONCLUSIONS
Utilizing one-on-one interventions designed to target evidence-based injury risk factors is an effective strategy to eliminate LE musculoskeletal injury risk factors and potentially mitigate injury risk. The interventions included in the algorithm were selected based on current evidence and clinical expertise of the treating physical therapists. Clinically and pragmatically, of greatest importance is that identified deficits are matched with interventions designed to improve them. These impairments should be reassessed after the treatment to determine the effectiveness of the technique. This study may be used as a template for injury prevention efforts, allowing clinicians to allocate resources where they are needed most.
Appendix: MOBILITY INTERVENTIONS
Ankle Dorsiflexion
Half kneeling mobilization with movement
Details: The subject begins in half-kneeling, with knee and ankle flexed to 90 degrees, and ankle to be treated forward. The therapist provides a posterior force to the subject's talus as the subject shifts his or her weight forward with an upright trunk, advancing the tibia to produce closed kinetic chain dorsiflexion.
Instrument Assisted Soft Tissue Mobilization (IASTM)—Soleus
Details: An instrument was used to mobilize soft tissue trigger points or painful areas in the soleus.
Ankle Dorsiflexion Home Exercise Program (HEP) Foam rolling—Gastroc-soleus
Details: The subject places the leg to be treated on top of the foam roller, crossing the contralateral leg on top. Lifting the hips off the floor, the subject then rolls over the soft tissue of the gastroc-soleus complex to mobilize trigger points or painful areas.
Half kneeling dorsiflexion
Details: The subject begins in a half kneeling position, with knee and ankle flexed to 90 degrees, and leg to be treated forward. The subject shifts his or her weight forward with an upright trunk, advancing the tibia over the toes to produce closed kinetic chain dorsiflexion.
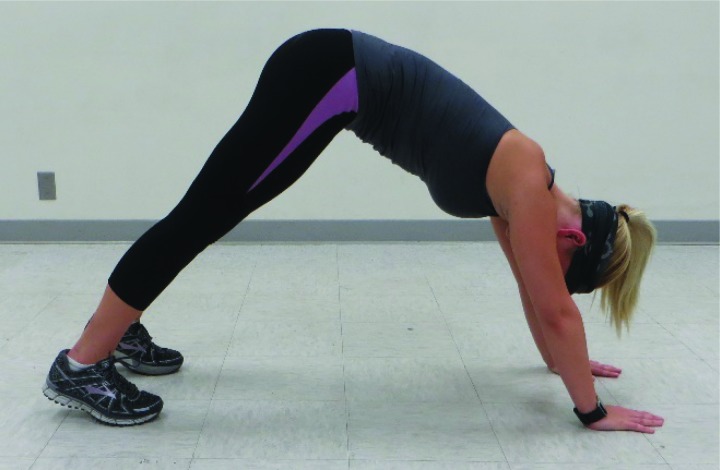
Downward dog
Details: The subject begins in a modified push up position, with hips raised toward the ceiling, bearing weight through hands and feet. The subject then pushes through the floor with his or her hands, keeping the knees extended, to produce a stretch in the gastrocnemius muscles.
Hip External Rotation
Anterior capsule mobilizations
Details: The subject lies in prone with the hip to be treated slightly abducted and knee flexed. With the subject's foot supported by a pillow, the therapist applies an anterior glide to the posterior aspect of the femoral acetabular joint.
IASTM to Rectus femoris
Details: The subject lies in supine while the therapist uses an instrument to mobilize trigger points or painful areas in the rectus femoris.
Hip External Rotation HEP Foam rolling—Rectus femoris
Details: The subjects lies prone with the leg to be treated in direct contact with the lateral edge of the foam roller, and the contralateral hip flexed and abducted off to the side. The subject then rolls over the tissue of the rectus femoris to mobilize trigger points or painful areas.
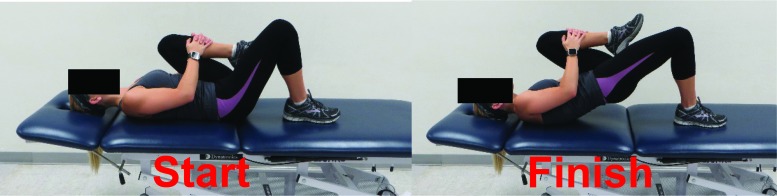
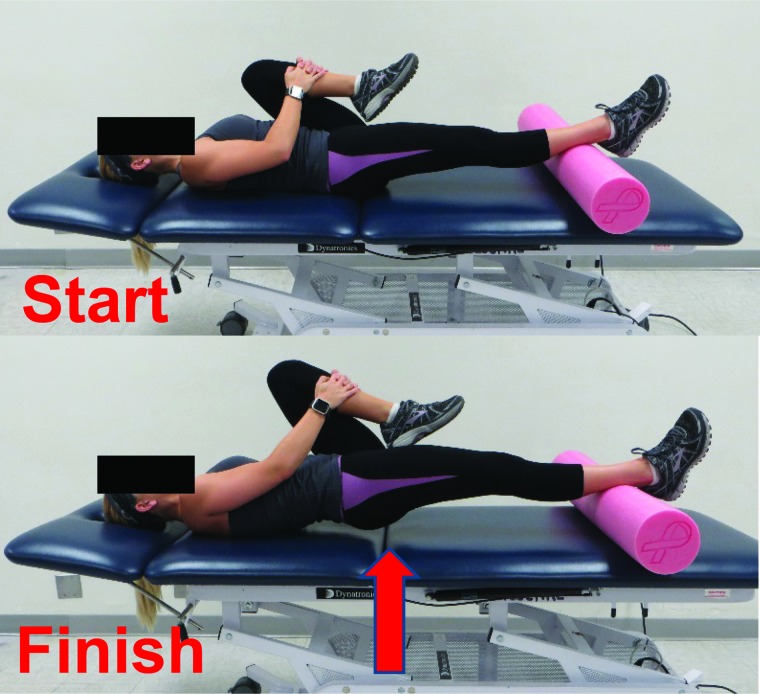
Single leg lumbar locked bridging
Details. Start: The subject begins in hooklying position with the foot of the leg to be treated flat on the table and contralateral knee flexed up toward the chest. Finish: The subject holds the knee tightly toward the chest using his or her hands, while lifting the hips toward the ceiling by pushing through the heel.
Windmill
Details. Start: The subject starts in half kneeling, with hip to be treated forward and contralateral leg externally rotated so that the feet are perpendicular to each other.
Finish: The subject shifts weight away from the forward leg, lowering contralateral hip toward contralateral heel until contralateral palm contacts the floor.
Thorax Rotation
Seated J stroke
Details: The subject is seated on the edge of a plinth with arms crossed over chest. The therapist wraps his or her arms around the subject, with hands clasped over the subject's elbows. The therapist applies a posterior and inferior force through the subject's elbows before providing a superior distraction thrust, using a “J” shaped maneuver.
IASTM to Obliques
Details: The subject is positioned in sidelying, with side to be treated toward the ceiling. A pillow or bolster was placed between the contralateral lower ribs and iliac crest. The arm of the side to be treated is abducted overhead to increase tissue stretch while the therapist mobilizes trigger points or painful areas in the obliques.
Thorax Rotation—HEP
T-spine extension over foam roller
Details: The subject is in hooklying, with the foam roller positioned at the mid-thoracic spine. After lifting the hips, the subject rolls over the foam roller and performs extension segment by segment throughout the thoracic vertebrae.
Sidelying rib grab
Details. Start: The subject starts in sidelying with the side to be treated toward the ceiling and ipsilateral hand draped over the stomach, grasping the contralateral ribs. Finish: The subject then rotates posteriorly, retracting the ipsilateral scapula toward the table.
Tall kneeling rotations with kettlebell
Details. Start: The subject begins in tall kneeling, with knees abducted slightly wider than hips and heels of both feet touching. Finish: While holding the kettlebell directly behind him or her, the subject rotates towards one side, maintaining an upright trunk and retracted scapulas before rotating toward the opposite side.
Fundamental Pattern Interventions
Active Straight Leg Raise (ASLR)
IASTM to Rectus femoris
Details: The subject lies in supine while the therapist uses an instrument to mobilize trigger points or painful areas in the rectus femoris.
IASTM to Hamstrings
Details: The subject lies prone while the therapist uses an instrument to mobilize trigger points or painful areas in the hamstring muscle group.
Proprioceptive Neuromuscular Facilitation (PNF) to Rectus femoris
Details: The subject lies in a modified prone position, with the contralateral floor flat on the floor and the leg to be stretched on the table with the knee flexed to 90 degrees. The therapist stabilizes the ipsilateral hip with one hand, while grasping the ipsilateral distal tibia with the other. The subject is asked to perform knee extension into resistance provided by the therapist, resulting in an isometric contraction. The therapist then passively flexes the knee to produce a stretch to the rectus femoris.
PNF to Hamstrings
Details: The subject lies in supine, both knees extended, with the leg to be stretched supported by the therapist's shoulder. The subject performs hip extension with the ipsilateral leg into resistance provided by the therapist, resulting in an isometric contraction, while the therapist provides stabilization to the contralateral leg to maintain full knee extension. The therapist then passively flexes the ipsilateral hip with the knee extended to produce a stretch to the hamstrings.
ASLR—HEP
Sidelying Brettzel
Details: The subject begins in sidelying, with the leg to be stretched down on the table. The contralateral hip is flexed toward the chest and the subject grasps it with the ipsilateral hand. The ipsilateral hip is extended, with the knee flexed, and the subjects posteriorly rotates through the thoracic spine to grasp the foot with the contralateral hand to produce a stretch through the rectus femoris and iliopsoas.
Doorway ASLR
Details. Start: The subject lies in supine with the leg to be treated supported by a door frame or table, with hips as close to the door frame as tolerated. Finish: Maintaining full knee extension on both legs, the subject then lifts and lowers the contralateral leg.
Single leg dead lift
Details: The subject begins in standing with the contralateral arm holding a kettlebell. After shifting his or her weight to the leg to be treated, the subject balances on the ipsilateral side and hinges forward to lift the contralateral leg toward the ceiling, keeping a straight line from the head to the foot. The subject then returns to standing position.
In-Line Lunge
IASTM to Rectus femoris
Details: The subject lies in supine while the therapist uses an instrument to mobilize trigger points or painful areas in the rectus femoris.
IASTM—Gastroc-soleus
Details: The subject lies in prone while an instrument was used to mobilize soft tissue trigger points or painful areas in the gastrocnemius and soleus.
PNF to Rectus femoris
Details: The subject lies in a modified prone position, with the contralateral floor flat on the floor and the leg to be stretched on the table with the knee flexed to 90 degrees. The therapist stabilizes the ipsilateral hip with one hand, while grasping the ipsilateral distal tibia with the other. The subject is asked to perform knee extension into resistance provided by the therapist, resulting in an isometric contraction. The therapist then passively flexes the knee to produce a stretch to the rectus femoris.
Half kneeling dorsiflexion
Details: The subject begins in a half kneeling position, with knee and ankle flexed to 90 degrees, and leg to be treated forward. The subject shifts weight forward with an upright trunk, advancing the tibia over the toes to produce closed kinetic chain dorsiflexion.
Sidelying Brettzel
Details: The subject begins in sidelying, with the leg to be stretched down on the table. The contralateral hip is flexed toward the chest and the subject grasps it with the ipsilateral hand. The ipsilateral hip is extended, with the knee flexed, and the subjects posteriorly rotates through the thoracic spine to grasp the foot with the contralateral hand to produce a stretch through the rectus femoris and iliopsoas.
Single leg lumbar locked bridging
Details. Start: The subject begins in hooklying position with the foot of the leg to be treated flat on the table and contralateral knee flexed up toward the chest. Finish: The subject held the knee tightly toward the chest using his or her hands, while lifting the hips toward the ceiling by pushing through the heel.
Hurdle Step
IASTM to Iliopsoas
Details: The subject lies in supine while the therapist palpates the medial surface of the pelvis, mobilizing trigger points or tender areas noted in the iliacus or psoas muscles.
IASTM to Rectus femoris
Details: The subject lies in supine while the therapist uses an instrument to mobilize trigger points or painful areas in the rectus femoris.
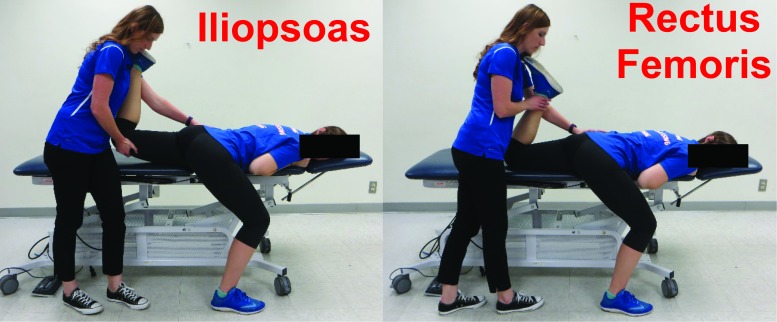
PNF to Iliopsoas and Rectus femoris
Details. Iliopsoas: The subject lies in a modified prone position, with the contralateral floor flat on the floor and the leg to be stretched on the table with the knee flexed comfortably. The therapist stabilizes the ipsilateral hip with one hand, while grasping the ipsilateral distal femur. The subject is asked to perform hip flexion into resistance provided by the therapist, resulting in an isometric contraction. The therapist then passively extends the hip to produce a stretch to the iliopsoas muscle group. Rectus Femoris: The subject and therapist positions are the same, except the therapist is grasping the distal tibia rather than distal femur. The subject is asked to perform knee extension into resistance provided by the therapist, resulting in an isometric contraction. The therapist then passively flexes the knee to produce a stretch to the rectus femoris.
Hurdle Step—HEP
Pigeon stretch
Details: The subject stands facing the end of a plinth with the leg to be treated supported by the plinth and positioned in 90 degrees of knee flexion and full hip external rotation and abduction. The subject is instructed to keep knee and tibia parallel with the plinth surface and a stretch should be felt in the posterior hip.

Single leg lumbar locked straight leg bridge
Details. Start: The subject lies in supine with the leg to be treated extended and supported on a bolster, and the contralateral knee flexed to his or her chest. Finish: Keeping contralateral knee held tightly toward chest, the subject lifts the hips off the table, keeping ipsilateral knee extended.
Single leg Oscillatory Technique for Isometric Stabilization (OTIS)
Details: The subject begins standing on the leg to be treated, with the contralateral leg raised approximately 6 inches off the floor and both arms grasping a resistance band. While maintaining balance on the ipsilateral leg, the subject rapidly and repeatedly flexes and extends the arms in a limited range to provide a perturbation to single leg balance.
Motor Control Interventions
Lower Quarter Neuromuscular Training
Planks
Details. Traditional: The subject holds a “plank” position by propping up onto elbows and toes, keeping trunk and hips off the surface and maintaining a straight line from head to heels. Side: The subject holds a “side plank” position by propping up onto one elbow, keeping trunk and hips off the surface and maintaining a straight line from head to heels. This is repeated on the opposite side.
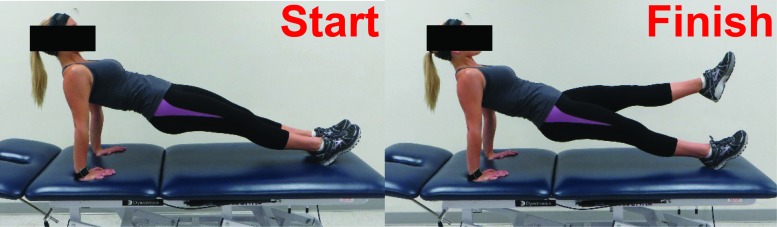
Pilates—Reverse Planks
Details. Start: The subject begins in a reverse plank position, propping up on hands and heels while lifting the hips off the plinth surface. Finish: The subject then alternates lifting one leg off the plinth surface, without dropping hips toward the plinth.
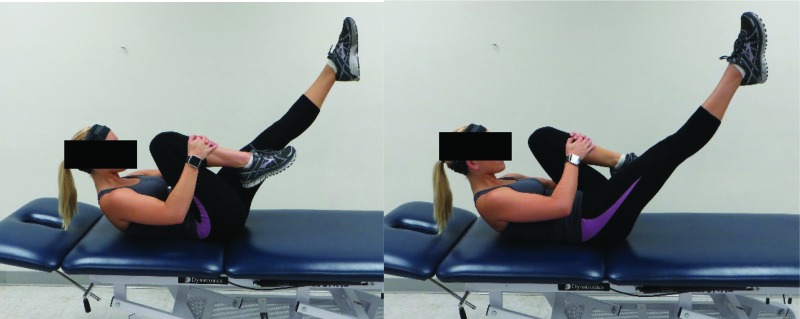
Pilates-Single leg stretch
Details: The subject lies in supine with his or her head elevated from the plinth surface. One knee is flexed toward chest while the other is extended approximately 45 degrees from the plinth surface. The subject alternates bringing one knee to chest while extending the other.
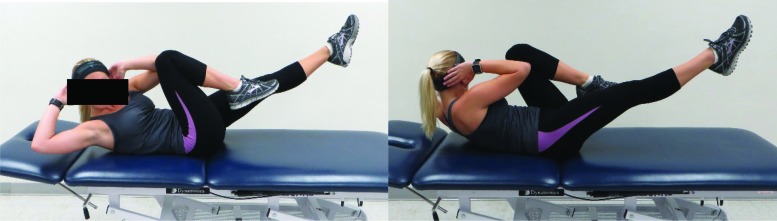
Pilates—Bicycle
Details. The patient begins with head raised slightly off the plinth surface, with one leg extended and one knee flexed to chest. The subject alternates flexing and extending legs while twisting the contralateral elbow toward the flexed knee.
Pilates—Sidelying leg lift
Details: The subject begins in sidelying with hips perpendicular to ceiling and knees extended. Anterior: The subject lifts the top leg toward the ceiling, then advances it forward before dropping toward the front edge of the table. Posterior: The subject then raises the top leg toward the ceiling again, before reaching backwards and dropping the leg toward the back edge of the table. This is repeated on the opposite leg.
Single leg dead lift
Details: The subject begins in standing with the contralateral arm holding a kettlebell. After shifting weight to the leg to be treated, the subject balances on the ipsilateral side and hinges forward to lift the contralateral leg toward the ceiling, keeping a straight line from the head to the foot. The subject then returns to standing position.
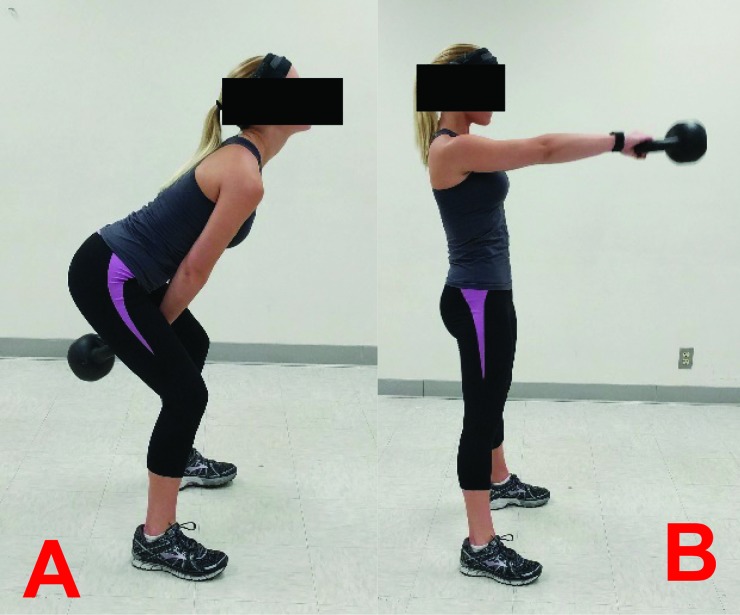
Kettlebell Swings
Details: The subject begins with feet shoulder width apart in a squat position and hands grasping the handles of the kettlebell on the floor. Keeping elbows straight, the subject pulls the kettlebell through the legs posteriorly (A), before quickly extending the hips (B) to swing the kettlebell toward the ceiling.
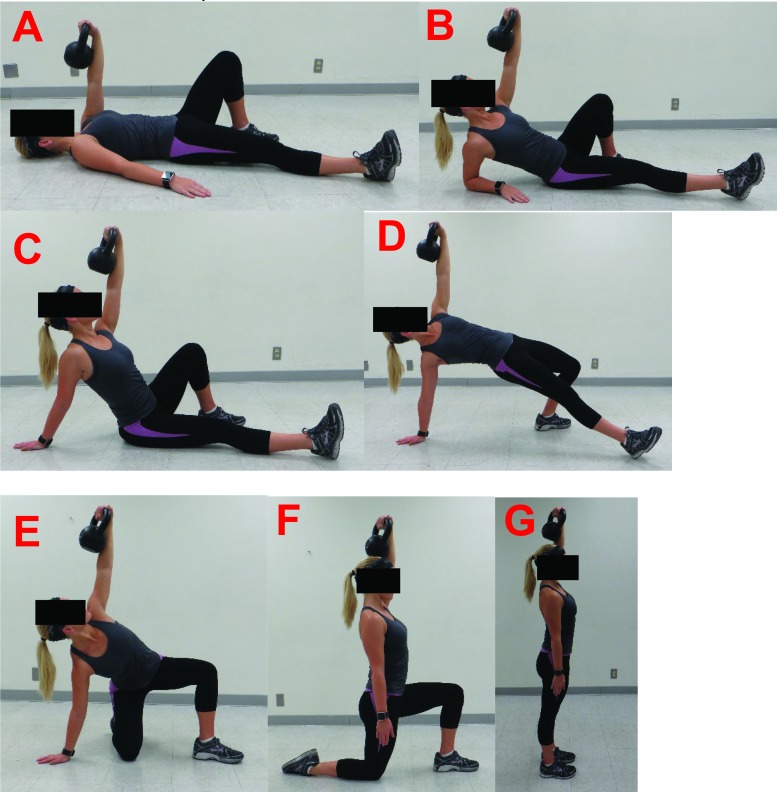
Turkish Get Ups
Details: The subject begins in supine with the ipsilateral knee bent and the ipsilateral arm is flexed to 90 degrees holding a kettlebell with a neutral wrist. The contralateral leg and arm are slightly abducted (A). The subject rolls up to the contralateral elbow (B), then extends the elbow to prop up into a modified long sitting position (C). The patient then lifts the hips toward the ceiling (D) before placing the contralateral knee under the hips (E). The subject then pushes the weight up toward the ceiling and rotates the contralateral leg so that he or she is now in a half kneeling position (F). Finally, the subject stands up (G), before reversing the sequence to return to a supine position.
Upper Quarter Neuromuscular Training
Planks
Details. Traditional: The subject holds a “plank” position by propping up onto elbows and toes, keeping trunk and hips off the surface and maintaining a straight line from head to heels. Side: The subject holds a “side plank” position by propping up onto one elbow, keeping trunk and hips off the surface and maintaining a straight line from head to heels. This is repeated on the opposite side.
Supine arm bar; (aka) Bottoms up arm bar
Details. The subject begins in hooklying with arm to be treated holding a kettlebell at 90 degrees of shoulder flexion. Supine: The bell rests against the forearm while the wrist is neutral, and the scapula is in a retracted and depressed position. Bottoms Up: The bell is facing the ceiling, balancing over the shoulder. The wrist is neutral and the scapula is retracted and depressed.
Sidelying arm bar
Details: The subject begins in sidelying with hips and knees flexed to 90 degrees and arm to be treated abducted to 90 degrees. The kettlebell is balanced directly over the shoulder, with the bell resting against the forearm. The wrist is neutral and the scapula is retracted and depressed.
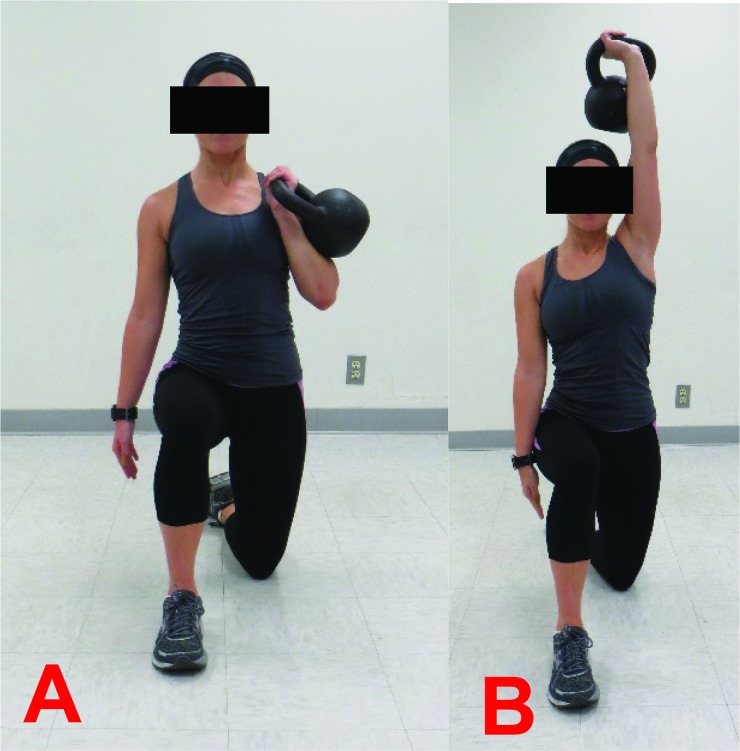
Half kneeling press up
Details: The subject begins in half kneeling with the contralateral leg forward, knee and ankle flexed to 90 degrees. The kettlebell is held in a “rack” position, held with a neutral wrist at shoulder height and resting on the forearm (A). While maintaining an upright trunk, the subject presses the weight overhead (B).
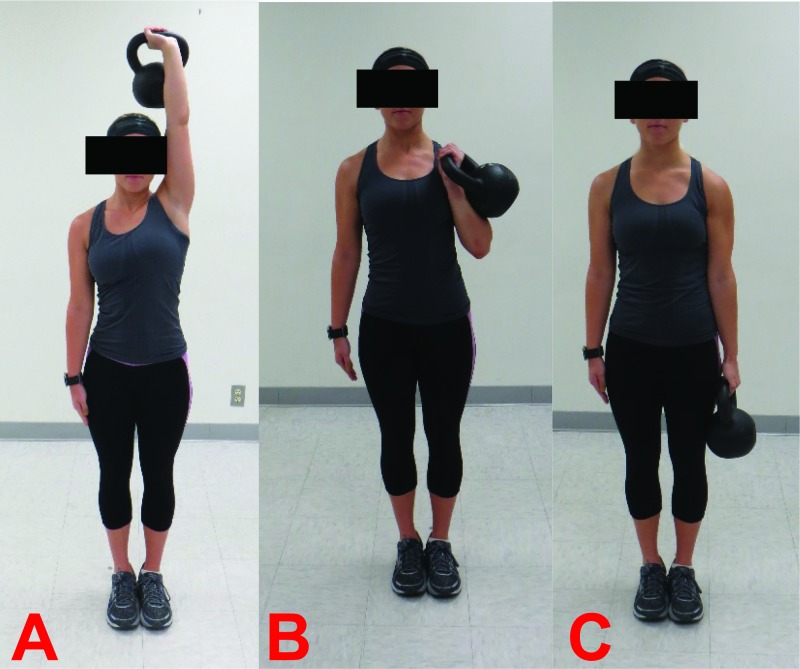
3 position kettlebell carry
Details: The subject begins in a standing position with the kettlebell held directly overhead (A). The subject walks forward in a straight path until he or she is unable to hold the kettlebell overhead, at which time it is lowered to the “rack” position (B). The subject continues to walk in a forward path until he or she is unable to hold the bell in the “rack” position, at which time the kettlebell is lowered to the side (C). The subject continues walking until he or she is unable to hold the kettlebell the side, at which time the kettlebell is lowered to the ground and the set is complete.
REFERENCES
- 1.Chandran A Barron MJ Westerman BJ, et al. Time Trends in Incidence and Severity of Injury Among Collegiate Soccer Players in the United States: NCAA Injury Surveillance System, 1990-1996 and 2004-2009. Am J Sports Med. 2016;44(12):3237-42. [DOI] [PubMed] [Google Scholar]
- 2.Effgen SK. Meeting the physical therapy needs of children. 2nd ed. Philadelphia: F.A. Davis Co. 2013.
- 3.Hewett TE Myer GD Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492-501. [DOI] [PubMed] [Google Scholar]
- 4.Padua DA DiStefano LJ Beutler AI, et al. The Landing error scoring system as a screening tool for an anterior cruciate ligament injury-prevention program in elite-youth soccer athletes. J Athl Train. 2015;50(6):589-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Verrall GM Slavotinek JP Barnes PG, et al. Hip joint range of motion restriction precedes athletic chronic groin injury. J Sci Med Sport. 2007;10(6):463-6. [DOI] [PubMed] [Google Scholar]
- 6.de Noronha M Refshauge KM Herbert RD, et al. Do voluntary strength, proprioception, range of motion, or postural sway predict occurrence of lateral ankle sprain? Br J Sports Med. 2006;40(10):824-8; discussion 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Teyhen DS Shaffer SW Butler RJ, et al. What risk factors are associated with musculoskeletal injury in US army rangersϿ. A prospective prognostic study. Clin Orthop Relat Res. 2015;473(9):2948-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perry J Burnfield JM. Gait analysis : Normal and pathological function. 2nd ed. ed. Thorofare, N.J.: SLACK 2010.
- 9.de la Motte S Arnold BL Ross SE. Trunk-rotation differences at maximal reach of the star excursion balance test in participants with chronic ankle instability. J Athl Train. 2015;50(4):358-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kiesel KB Butler RJ Plisky PJ. Prediction of injury by limited and asymmetrical fundamental movement patterns in american football players. J Sport Rehabil. 2014;23(2):88-94. [DOI] [PubMed] [Google Scholar]
- 11.Mokha M Sprague PA Gatens DR. Predicting musculoskeletal injury in national collegiate athletic association Division II athletes from asymmetries and individual-test versus composite functional movement screen scores. J Athl Train. 2016;51(4):276-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bushman TT Grier TL Canham-Chervak MC, et al. Pain on Functional Movement Screen Tests and Injury Risk. J Strength Cond Res. 2015;29 Suppl 11:S65-70. [DOI] [PubMed] [Google Scholar]
- 13.Zazulak BT Hewett TE Reeves NP, et al. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Am J Sports Med. 2007;35(7):1123-30. [DOI] [PubMed] [Google Scholar]
- 14.Wilkerson GB Giles JL Seibel DK. Prediction of core and lower extremity strains and sprains in collegiate football players: a preliminary study. J Athl Train. 2012;47(3):264-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Plisky PJ Rauh MJ Kaminski TW, et al. Star excursion balance test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys The.r 2006;36(12):911-9. [DOI] [PubMed] [Google Scholar]
- 16.Gribble PA Terada M Beard MQ, et al. Prediction of lateral ankle sprains in football players based on clinical tests and body mass index. Am J Sports Med. 2016;44(2):460-7. [DOI] [PubMed] [Google Scholar]
- 17.Lehr ME Plisky PJ Butler RJ, et al. Field-expedient screening and injury risk algorithm categories as predictors of noncontact lower extremity injury. Scand J Med Sci Sports. 2013;23(4):e225-32. [DOI] [PubMed] [Google Scholar]
- 18.Plisky PJ Gorman PP Butler RJ, et al. The reliability of an instrumented device for measuring components of the star excursion balance test. N Am J Sports Phys Ther 2009;4(2):92-9. [PMC free article] [PubMed] [Google Scholar]
- 19.Gorman PP Butler RJ Plisky PJ, et al. Upper Quarter Y Balance Test: reliability and performance comparison between genders in active adults. J Strength Cond Res. 2012;26(11):3043-8. [DOI] [PubMed] [Google Scholar]
- 20.Teyhen DS Shaffer SW Lorenson CL, et al. The Functional Movement Screen: a reliability study. J Orthop Sports Phys Ther. 2012;42(6):530-40. [DOI] [PubMed] [Google Scholar]
- 21.Minick KI Kiesel KB Burton L, et al. Interrater reliability of the functional movement screen. J Strength Cond Res. 2010;24(2):479-86. [DOI] [PubMed] [Google Scholar]
- 22.Portney LG Watkins MP. Foundations of clinical research : Applications to practice. 3rd ed. Upper Saddle River, N.J.: Pearson/Prentice Hall 2009.
- 23.Noyes FR Barber Westin SD. Anterior cruciate ligament injury prevention training in female athletes: a systematic review of injury reduction and results of athletic performance tests. Sports Health. 2012;4(1):36-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heubner BJ Plisky PJ Kiesel KB Schwartzkopf-Phifer K. Can injury risk category be changed in athletesϿ. An analysis of an injury prevention system. Int J Sports Phys Ther. 2019;14(1):127-34. [PMC free article] [PubMed] [Google Scholar]
- 25.Kiesel K Plisky P Butler R. Functional movement test scores improve following a standardized off-season intervention program in professional football players. Scand J Med Sci Sports. 2011;21(2):287-92. [DOI] [PubMed] [Google Scholar]
- 26.Bodden JG Needham RA Chockalingam N. The effect of an intervention program on functional movement screen test scores in mixed martial arts athletes. J Strength Cond Res. 2015;29(1):219-25. [DOI] [PubMed] [Google Scholar]
- 27.Barengo NC Meneses-Echavez JF Ramirez-Velez R, et al. The impact of the FIFA 11 + training program on injury prevention in football players: a systematic review. Int J Environ Res Public Health. 2014;11(11):11986-12000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Johnson KD Kim KM Yu BK, et al. Reliability of thoracic spine rotation range-of-motion measurements in healthy adults. J Athl Train. 2012;47(1):52-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fullenkamp AM Campbell BM Laurent CM, et al. The Contribution of trunk axial kinematics to poststrike ball velocity during maximal instep soccer kicking. J Appl Biomech. 2015;31(5):370-6. [DOI] [PubMed] [Google Scholar]
- 30.Dutton M. Orthopaedic examination, evaluation, and intervention. New York: McGraw-Hill 2004.
- 31.Pope R Herbert R Kirwan J. Effects of ankle dorsiflexion range and pre-exercise calf muscle stretching on injury risk in Army recruits. Aust J Physiother. 1998;44(3):165-72. [DOI] [PubMed] [Google Scholar]
- 32.Malliaras P Hogan A Nawrocki A, et al. Hip flexibility and strength measures: reliability and association with athletic groin pain. Br J Sports Med. 2009;43(10):739-44. [DOI] [PubMed] [Google Scholar]