ABSTRACT
Rift Valley fever virus (RVFV), a recognized category A priority pathogen, causes large outbreaks of Rift Valley fever with some fatalities in humans in humans and huge economic losses in livestock. As wild-type RVFV must be handled in BSL-3 or BSL-4 laboratories, we constructed a high-titer vesicular stomatitis virus (VSV) pseudotype bearing RVFV envelope glycoproteins to detect neutralizing antibodies in vitro under BSL-2 conditions. The neutralizing properties of 39 amino acid mutant sites that have occurred naturally over time in the RVFV envelope glycoproteins were analyzed with their corresponding pseudoviral mutants separately. Compared with the results in the primary strain, the variants showed no statistically significant differences. We next established a Balb/c mouse pseudovirus infection model for detecting neutralizing antibodies against pseudovirus. Five immunizations with pseudoviral DNA protected the mice from infection with the pseudovirus. Bioluminescence imaging, which we used to evaluate viral dissemination and distribution in the mice, showed a good relationship between the neutralizing antibodies titers in vitro. These pseudovirus methods will allow for the safe determination of neutralizing antibodies in vivo and in vitro, and will assist with studies on vaccines and drugs against RVFV with the long term objective of Rift Valley fever prevention.
KEYWORDS: Rift Valley fever virus, pseudovirus, neutralizing antibody, mouse model, site mutation, DNA vaccine
Introduction
Rift Valley fever virus (RVFV), a zoonotic arbovirus, infects ruminants and humans via the bites of infected mosquitoes percutaneously, or by exposure to diseased animals.1 In livestock animals, especially sheep and cattle, RVFV primarily causes abortions in ruminants and high mortality also in newborns with a rate approaching 100%.2 In most human disease cases, RVFV infection lacks clinical signs, but about 1% to 3% of infected individuals develop serious complications such as severe encephalitis, renal failure, retinitis, fatal hepatitis and hemorrhagic fever.3,4 Worryingly, large explosive epidemics of this viral disease sometimes occur, especially in Africa.4 In 1977, RVFV was responsible for a massive epizootic epidemic in Egypt with more than 200,000 people estimated to be infected and approximately 600 deaths occurring.5 To date, live attenuated candidate vaccines have been used to protect veterinarians and laboratory workers at high risk of exposure to RVFV, but no vaccines have been licensed for production and commercial use.
RVFV, a negative-sense, single-stranded RNA virus, contains three segments (L, M, S). The open reading frame (ORF) of the RVFV M segment encodes a long peptide that is processed into four mature proteins: the envelope glycoprotein N (Gn) and glycoprotein C (Gc), a nonstructural protein, and a 78-kDa fusion protein comprising nonstructural and Gn proteins.6 Both Gn and Gc, which are located on the virion surface, are necessary for viral assembly and maturation.7–9 Gn and Gc contain epitopes recognized by neutralizing antibodies, and these play an important role for researchers analyzing viral antigenicity.10–12 RVFV is an RNA viruses prone to mutate naturally.13 Whether such natural mutations in the envelope glycoprotein can change the antigenicity and neutralization properties of the virus is not clear. Investigating all the natural variants of RVFV by analyzing their antigenicity and neutralization properties is problematic because working with these viruses requires access to a BSL-3 or BSL-4 containment laboratory.
In this study, we constructed a pseudovirus (pRVFV) with the RVFV envelope glycoproteins encoded by the M segment of the RVFV ZH548 strain using a recombinant VSV pseudovirus (pVSVΔG).14 Mutant pseudoviruses carrying naturally occurring mutations in the M segment were also constructed using site-directed mutagenesis. The antigenic differences in the various pseudoviral strains were analyzed using anti-serum from immunized guinea pigs. The protective effects of the newly designed recombinant DNA vaccine were also evaluated in vivo using the pRVFV pseudovirus.
Results
Construction of a high-titer pRVFV packaging system
Because the RVFV envelope glycoprotein is able to recognize and bind to the cell surface receptor that mediates viral entry into cells, the coding gene was cloned into an eukaryotic expressive vector to construct the pseudovirus. To obtain high-titer pRVFV, four parameters (transfection reagents, the amount of pVSVΔG used, the time point of pVSVΔG addition, and the time point of viral harvest) were optimized (Figure 1). Finally, the pseudovirus in the cell culture medium, collected from the 293T cells cultured in a T75 tissue flask at 24h after the DNA-Lipofectamine 3000 complex being added together with a 1.6 × 106 50% tissue culture infective dose (TCID50) of pVSVΔG, could produce the highest relative light units (RLU) at 24 hours post-infection (pi).
Figure 1.
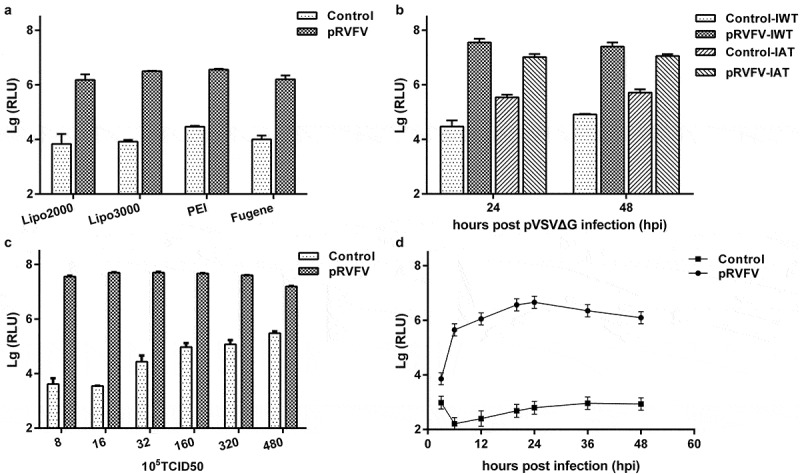
Optimization of the pRVFV packaging system. Culture medium collected from the cells transfected with empty vectors and infected with pVSVΔG was used as control. (a) Optimization of the transfection reagents including Lipofectamine 2000, Lipofectamine 3000, PEI and Fugene. (b) Identifying the appropriate time point for pVSVΔG participation. IWT (Infection together with Transfection), after transfecting the 293T cells with plasmids, pVSVΔG was added immediately and both were washed away together 6 hours later. IAT (Infection after Tansfection), pVSVΔG was added to the cell monolayer 24 h after the transfection and removed 1 hour later. (c) Optimization of the additive dose of the pVSVΔG with the same quantities of vectors encoding the envelope proteins. (d) The growth curve for pRVFV.
Development of the in vitro RVFV neutralization method based on pseudovirus
Two main parameters were optimized to develop the best neutralization assay in terms of its accuracy and stability. First, different cell lines were selected to study the tropism of RVFV. From them, Huh7 was chosen as the best cell line for infection because it generated higher RLU values (Figure 2(a)). Furthermore, the best viral inoculation quantity was determined by detecting anti-RVFV serum in a dose range from 50 to 6400TCID50/well. The results showed that the 50% inhibition dilution (ID50) decreased gradually when the viral inocula exceeded 1600TCID50/well, and varied greatly at less than 100TCID50/well (Figure 2(b)). Finally, 400TCID50/well was chosen as the optimal viral dose for calculating the serum titers.
Figure 2.
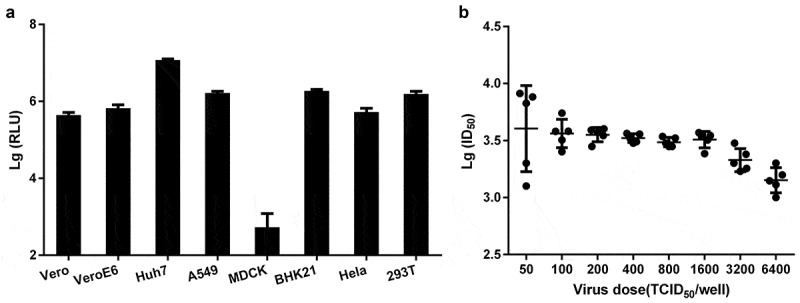
Optimization of the parameters used for the in vitro neutralization assays. (a) Selection of the sensitive cell line. For each cell line, the same number of cells was infected with equal amounts of pRVFV, and the RLU values were detected concurrently. (b) Optimization of the viral inocula. The ID50 value of the serum from an immunized guinea pig was determined using different pRVFV doses.
Neutralization sensitivities of the mutant strains against the antibodies induced by the recombinant DNA vaccine
Because the RVFV envelope glycoprotein is able to induce the production of neutralizing antibody production,15 the recombinant vector containing the entire ORF sequence was used as a candidate vaccine to obtain antibodies against it in guinea pigs. The antibodies titers in the immune sera were positively correlated with the numbers of immunization administered, but differences between individuals existed, and the ID50 value of the serum taken from guinea pig-1 was higher than those from the other animals at the same point. After five immunizations, the ID50 values were all above 3000, while that for guinea pig-1 approached 9000 (Figure 3(a)).
Figure 3.
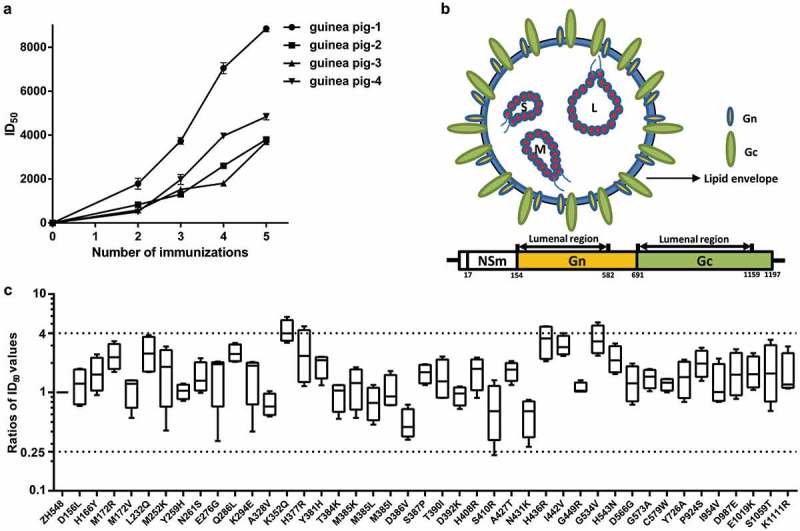
(a) Relationship between the serum titers from the guinea pigs and the number of immunizations they received. From the second immunization to the last, blood samples were taken from the heart (4 times). (b) Schematic diagram of the structure of RVFV and its M segment. Sites outside the viral membrane are from positions 154 to 582 and from 691 to 1159 (http://www.uniprot.org). (c) The ratios of the ID50 values detected using the pseudoviral variants compared with pRVFV-ZH548. Increases and decreases (4-fold) were highlighted with dashed lines.
The amino acid sequences of 117 glycoproteins were analyzed using the BioEdit software sequence alignment tool.16 Compared with the ZH548 reference sequence, 192 amino acid sites differed, the frequencies of which ranged from 0.85% to 95.73%. Theoretically, only the sites outside the viral membrane should combine with neutralizing antibodies, and 55 and 42 sites located in the lumenal regions of Gn and Gc (Figure 3(b)), respectively, were found that could potentially influence protein binding. It is generally known that most amino acid substitutions have no effect on protein binding. As mutant sites in potential binding regions with frequencies over 4.0% (high frequency mutations) were selected, we also selected promising mutations with the help of Sorting Intolerant From Tolerant software (SIFT)17–19 and Protein Variation Effect Analyzer (PROVEAN) software20 to assemble the mutant pseudoviruses. Finally, 42 naturally occurring amino acid mutations that may affect protein function and located at 39 amino acid sites (32 sites in Gn, 7 sites in Gc, Table 1) were selected to construct the pseudoviral mutants based on sequence homology and the physical properties of the amino acids, among them, two and three mutations were present at the amino acid positions 172 and 385 in Gn, respectively.
Table 1.
Information of amino acid substitution, including GenBank accession and mutant PCR primers.
| Number | Amino acid variation | Frequency (%) | Accession | PCR primer |
|---|---|---|---|---|
| 1 | P156L | 0.85 | AEC14288 | F:TCTGTTTCTCAGGTGAAGGTCCTCAGCGAACAC R:GTGTTCGCTGAGGACCTTCACCTGAGAAAACGA |
| 2 | H166Y | 0.85 | ABD38823 | F:CAGACCTGGCAAAGGCTACAACTACATTGACGGCATGAC R:GTCATGCCGTCAATGTAGTTGTAGCCTTTGCCAGGTCTG |
| 3 | M172R | 2.56 | AEB20472 | F:AGGCCACAACTACATTGACGGCGTGACACAGGAAGACGCCACCTG R:CAGGTGGCGTCTTCCTGTGTCACGCCGTCAATGTAGTTGTGGCCT |
| 4 | M172V | 0.85 | AOS50856 | F:AGGCCACAACTACATTGACGGCAGGACACAGGAAGACGCCACCTG R:CAGGTGGCGTCTTCCTGTGTCCTGCCGTCAATGTAGTTGTGGCCT |
| 5 | L232Q | 96.58 | ABD38827 | F:ATCCCCCTAGCTGTGATCTCCAATCCGCCCATGGCAA R:TTGCCATGGGCGGATTGGAGATCACAGCTAGGGGGAT |
| 6 | N252K | 0.85 | ABD38803 | F:GATGAAAACCCACTGCCCCAAAGACTACCAAAGCGCCCA R:TAATGGGCGCTTTGGTAGTCTTTGGGGCAGTGGGTTTTCATTTA |
| 7 | Y259H | 1.71 | AAA47449 | F: ACGACTACCAAAGCGCCCATCACCTCAACAACGA R:TCGTTGTTGAGGTGATGGGCGCTTTGGTAGTCGT |
| 8 | N261S | 0.85 | ACE78370 | F:CCAAAGCGCCCATTACCTCTCCAACGACGGCAAAATGGCTT R:AAGCCATTTTGCCGTCGTTGGAGAGGTAATGGGCGCTTTGG |
| 9 | E276G | 1.71 | ABD38801 | F:GAAGTGCCCCCCCAAATACGGGCTGACAGAAGACTGCAACT R:AGTTGCAGTCTTCTGTCAGCCCGTATTTGGGGGGGCACTTC |
| 10 | Q286L | 2.56 | ABD38830 | F:GAGGCGCCGGTCATCAGTCTACAAAAGTTGCAGT R:ACTGCAACTTTTGTAGAACTGATGACCGGCGCCTC |
| 11 | K294E | 0.85 | ABD38806 | F:ATGACCGGCGCCTCCCTCAAGGAGGGAAGCTACCCTCTGCAG R:CTGCAGAGGGTAGCTTCCCTCCTTGAGGGAGGCGCCGGTCAT |
| 12 | A328V | 0.85 | ABD38806 | F:TGTGTGAGGTCGGCGTGCAGGTCCTCAAGAAGTGTGAT R:ATCACACTTCTTGAGGACCTGCACGCCGACCTCACACA |
| 13 | K352Q | 0.85 | AEB20462 | F:TGTTTAAGAACTCCAAACAGGTCTACCTGGACAAGCTGG R:CCAGCTTGTCCAGGTAGACCTGTTTGGAGTTCTTAAACA |
| 14 | H377R | 0.85 | ABD38823 | F:ATAGCTTTGTGTGCTTCGAACGTAAGGGCCAGTATAAGGG R:CCCTTATACTGGCCCTTACGTTCGAAGCACACAAAGCTAT |
| 15 | Y381H | 0.85 | ABD38807 | F:TCGAACATAAGGGCCAGCATAAGGGCACCATGGACTC R:GAGTCCATGGTGCCCTTATGCTGGCCCTTATGTTCGA |
| 16 | T384K | 1.71 | ABD38828 | F:ATAAGGGCCAGTATAAGGGCAAGATGGACTCCGGACAAA R:TTTGTCCGGAGTCCATCTTGCCCTTATACTGGCCCTTAT |
| 17 | M385I | 0.85 | ABD38831 | F:AAGGGCCAGTATAAGGGCACCATCGACTCCGGACAAACCAA R:TTGGTTTGTCCGGAGTCGATGGTGCCCTTATACTGGCCCTT |
| 18 | M385K | 1.71 | ABD38812 | F:AAGGGCCAGTATAAGGGCACCAAGGACTCCGGACAAACCAA R:TTGGTTTGTCCGGAGTCCTTGGTGCCCTTATACTGGCCCTT |
| 19 | M385L | 0.85 | AFD98306 | F:AAGGGCCAGTATAAGGGCACCCTGGACTCCGGACAAACCAA R:TTGGTTTGTCCGGAGTCCAGGGTGCCCTTATACTGGCCCTT |
| 20 | D386V | 0.85 | AMD08950 | F:AGTATAAGGGCACCATGGTCTCCGGACAAACCAAGAGGGA R:TCCCTCTTGGTTTGTCCGGAGACCATGGTGCCCTTATACT |
| 21 | S387P | 0.85 | ABD38815 | F:TATAAGGGCACCATGGACCCTGGACAAACCAAGAGGG R:CCCTCTTGGTTTGTCCAGGGTCCATGGTGCCCTTATA |
| 22 | T390I | 2.56 | ABD38806 | F:ACCATGGACTCCGGACAAATCAAGAGGGAGCTGAAGA R:TCTTCAGCTCCCTCTTGATTTGTCCGGAGTCCATGGT |
| 23 | R392K | 0.85 | ABD38834 | F:ACTCCGGACAAACCAAGAAGGAGCTGAAGAGCTTCGA R:TCGAAGCTCTTCAGCTCCTTCTTGGTTTGTCCGGAGT |
| 24 | H408R | 0.85 | ABD38808 | F:AATGCCCCAAGATTGGCGGACGTGGTTCTAAGAAGTGTA R:TACACTTCTTAGAACCACGTCCGCCAATCTTGGGGCATT |
| 25 | S410R | 2.56 | AEB20462 | F:AAGATTGGCGGACATGGTCGTAAGAAGTGTACCGGAGA R:TCTCCGGTACACTTCTTACGACCATGTCCGCCAATCTT |
| 26 | A427T | 0.85 | ABD38823 | F:TTACGAGTGCACCACCCAGTACGCCAACGCCTATT R:AATAGGCGTTGGCGTACTGGGTGGTGCACTCGTAA |
| 27 | N431K | 0.85 | ABD38817 | F:ACCGCCCAGTACGCCAAAGCCTATTGTTCCCATGCCAA R:TTGGCATGGGAACAATAGGCTTTGGCGTACTGGGCGGT |
| 28 | H436R | 0.85 | AEB20462 | F:AGTACGCCAACGCCTATTGTTCCCGTGCCAATGGCTCCGGCA R:TGCCGGAGCCATTGGCACGGGAACAATAGGCGTTGGCGTACT |
| 29 | I442V | 6.84 | AEF79993 | F:TTCCCATGCCAATGGCTCCGGCGTAGTGCAGATCCAGGT R:ACCTGGATCTGCACTACGCCGGAGCCATTGGCATGGGAA |
| 30 | G449R | 1.71 | AEB20463 | F:ATCGTGCAGATCCAGGTGTCCCGAGTGTGGAAGAAGCCTC R:GAGGCTTCTTCCACACTCGGGACACCTGGATCTGCACGAT |
| 31 | G534V | 0.85 | AEB20472 | F:CTGGCATCTCCCAGAGCTCCGTAGGAGATATCGGCGTGCATAT R:ATATGCACGCCGATATCTCCTACGGAGCTCTGGGAGATGCCAG |
| 32 | H543N | 0.85 | ABD38800 | F:GCTCTGGTCATCGTTGGCCATATGCACGC R:GCGTGCATATGGCCAACGATGACCAGAGC |
| 33 | D566G | 95.73 | ABD38823 | F:ATCCTTGCCTGGTGCACGGCTGTATCGTCTGCGCTCAT R:ATGAGCGCAGACGATACAGCCGTGCACCAGGCAAGGAT |
| 34 | G573A | 1.71 | AEB20469 | F:ACTGTATCGTCTGCGCTCATGCCCTGATCAATTACCAGTGCCAC R:GTGGCACTGGTAATTGATCAGGGCATGAGCGCAGACGATACAGT |
| 35 | C579W | 1.71 | AEB20467 | F:TCATGGCCTGATCAATTACCAGTGGCACACCGCCCTCTCCGCC R:GGCGGAGAGGGCGGTGTGCCACTGGTAATTGATCAGGCCATGA |
| 36 | V726A | 0.85 | AEZ53085 | F:GCTTCGGCTCCGGCGCTGCCAGCTC R:GAGCTGGCAGCGCCGGAGCCGAAGC |
| 37 | P924S | 0.85 | ABD38805 | F:CAGGAAGCCCTGTCTACTGATCTCGCTGAAAGGC R:GCCTTTCAGCGAGATCAGTAGACAGGGCTTCCTG |
| 38 | I954V | 41.88 | AEB20467 | F:TCAGGGCTCCCAACCTGGTTAGCTACAAGCCCATGAT R:ATCATGGGCTTGTAGCTAACCAGGTTGGGAGCCCTGA |
| 39 | D987E | 11.11 | ABD38826 | F:CCAGACCAGGAACGAAAAGACCTTCGCCGCTTCCA R:TGGAAGCGGCGAAGGTCTTTTCGTTCCTGGTCTGG |
| 40 | E1019K | 0.85 | AEB20463 | F:ACTGATGTTCGACAACTTTAAGGTGGATTTTGTGGGAGCTGCC R:GGCAGCTCCCACAAAATCCACCTTAAAGTTGTCGAACATCAGT |
| 41 | S1059T | 87.18 | ABD38797 | F:TTACATCCACCGGAACAGGCACCCTCAGCGCCCATAAT R:ATTATGGGCGCTGAGGGTGCCTGTTCCGGTGGATGTAA |
| 42 | K1111R | 4.27 | ABD38830 | F:ATGAAAGGCCCCTGCTCGTCAGAGGCACCCTCATCGCTA R:TAGCGATGAGGGTGCCTCTGACGAGCAGGGGCCTTTCAT |
Notes: F, R presents the forward and reverse primer respectively. All mutant strains were packaged into pseudovirus.
Serum samples from the guinea pigs immunized five times were used to evaluate the neutralization sensitivity of the RVFV variants. Compared with the original pRVFV-ZH548 virus, the variation in the range of ID50 values in the serum samples that were detected by the variant pseudoviruses was within a 4-fold range. Generally, a change in antibody titer within this range is considered to be an experimental error.21 We found that almost all the single amino acid variants had neutralization sensitivities in the same range as that of the ZH548 strain (Figure 3(c)).
Establishment of a mouse infection model and evaluation of neutralizing antibodies in vivo
Bioluminescence imaging (BLI) is a powerful way to study biological processes of virus infection in live animals. In this study, mice infected with pRVFV were monitored using in vivo BLI to evaluate viral dissemination and the bodily distribution of the virus. Dissemination and distribution of pRVFV in mouse were monitored separately at different times pi using BLI, and a male Balb/c mouse infected with pRVFV was used for the anatomical observations. The results showed that the optimal observation time was 6 h pi, and the major affected organs were the liver, spleen and lungs (Figure 4(a)). To determine the optimal pseudovirus inoculation dose, mice in control group were injected intraperitoneally with DMEM, while mice in the experimental groups were intraperitoneally infected with serially diluted pseudoviruses and subjected to BLI at 6 h pi, and the 50% animal infection dose (AID50) was 275TCID50 (Figure 4(b)). Finally, to ensure that stable infections occurred in the mice, pseudoviruses with 90AID50 (about 2.5 × 104TCID50) values were used as the viral inocula in the following experiments.
Figure 4.
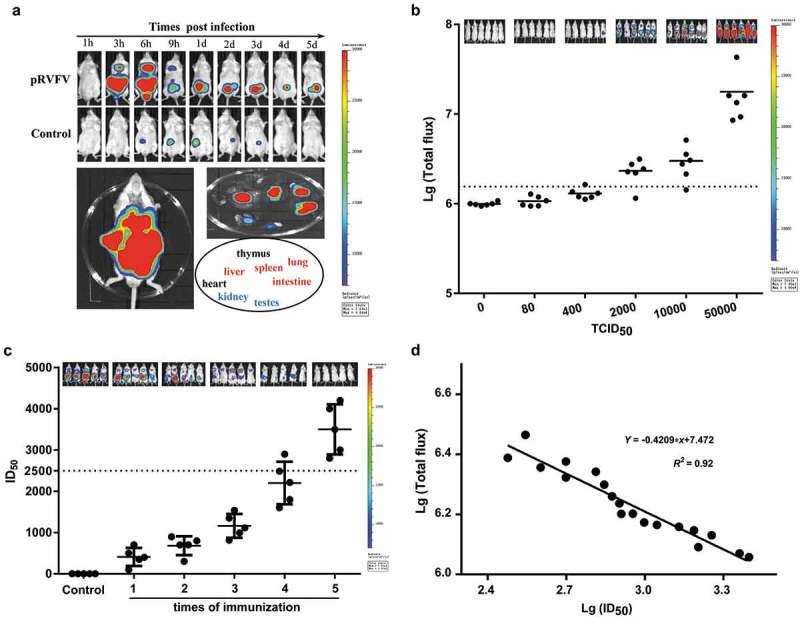
Establishment of the Balb/c mouse model and determination of neutralizing antibodies in vivo. (a) Determining the optimal detection time point post infection and the targeted organs using BLI. The mouse injected with equal volumes of culture media from the cells transfected with pcDNA3.1+ was used as the control. (b) Determination of the optimal infection dose of pRVFV in vivo. The sum of the mean values (and standard deviations) of the total flux values for the mice challenged with 400 TCID50 of pRVFV was set as the cutoff value to determine a positive or negative result, as highlighted here by dashed lines. (c) Evaluations of neutralizing antibodies in vivo and in vitro. Bioluminescence in the mice was detected by BLI at 6 h pi, and a small serum sample collected from them concurrently was detected in vitro. 2500, the lowest ID50 value for a neutralizing antibody protecting mice from pRVFV infection, as highlighted with dashed lines. (d) Correlation between the total flux values of the mice and the ID50 values of their sera.
Next, we carried out DNA vaccination experiments to evaluate the protective effect of our candidate DNA vaccine, and the mice immunized with pcDNA3.1+ were the control group. The serum ID50 values, which were measured in vitro, increased gradually after each immunization. While those from mice lacking visible bioluminescence were all above 2500 (Figure 4(c)). After five immunizations, the mice were completely protected from the infection with pRVFV (Figure 4(c)). The relative bioluminescence signals (total flux values) from the bioluminescent mice and the ID50 values of their sera were analyzed, and it showed a strong linear correlation (R2 = 0.92) (Figure 4(d)).
Discussion
To develop a safe and convenient standard laboratory method for evaluating neutralizing antibodies against RVFV, we successfully prepared a RVF pseudovirus comprising the RVFV envelope protein and VSV core. The resulting pseudoviral particle was only capable of achieving a single round of replication, and it is envisaged that the luciferase reporter gene contained within it could be used to detect the neutralizing antibodies in BSL-2 containment laboratories efficiently and accurately.
The conventional method used to construct pseudoviruses based on the recombinant VSVΔG system is to add pVSVΔG to 293T cells 24h after the plasmids expressing the viral envelope proteins are transfected.14,22–24 In contrast, by optimizing the conventional methods, we were able to prepare a higher titer pseudovirus with a lower background. Several common cell lines used for viral culturing were also selected to characterize the tropism of pRVFV, including the traditional Vero cell line used for RVFV culture,25 human adherent cell lines and non-human cell lines. Finally, the Huh7 cell line was chosen to be the model cell line for neutralizing antibodies detection in vitro, because it provided the most stable and accurate results.
Currently, vaccines against RVFV are mainly divided into three categories: inactivated, attenuated and engineered. The first candidate vaccine, NDBR-103, based on the RVFV Entebbe strain was inactivated by formalin, and its immune effect was limited.26 As the most successful live-attenuated vaccine for RVFV currently, MP-12 was obtained from the 12th passage of virulent ZH548 under the pressure of 5-fluorouracil pressure and conditionally approved as a veterinary vaccine in the USA.27 Other engineered vaccines against RVFV are still under development.28,29 In the present study, the recombinant plasmid containing the ZH548 M segment induced high titer neutralizing antibodies, suggesting that using DNA as a vaccine against RVFV is feasible. Our newly developed neutralizing antibody detection assay is based on the VSV pseudotype system. This system has also been used to develop candidate vaccines against Hantaan virus,30 Filoviruses,31 Arenaviruses31 and SARS-CoV,32 where it reportedly can induce high levels of neutralizing antibodies against these viruses. In future, RVFV vaccines may also be developed using this system.
As the neutralizing antibody titer induced by a vaccine is an important indicator of its effectiveness, we established a method to detect neutralizing antibodies against RVFV safely and accurately in vitro. Another important criterion when evaluating vaccine is whether or not the neutralizing antibodies induced by the vaccine are broad-spectrum, as this would be needed to inhibit infections with different viral strains. As RNA viruses are prone to mutate to escape from neutralization, we aligned 117 full glycoprotein sequences from RVFV to identify naturally occurring amino acid substitutions and used specialized software (SIFT and PROVEAN) to analyze the effect of amino acid substitution on protein function. Subsequently, 39 sites with 42 mutations in the outer membrane region of Gn and Gc were selected to construct the candidate pseudoviral mutants. Compared with the results for the original pseudovirus, no obvious antigenic changes in these pseudoviral mutants were observed. This observation may be related to the limited effect of single amino acid substitutions on the glycoprotein or the good broad-spectrum effect of the serum induced by the recombinant DNA vaccine; however, this finding needs to be further confirmed by constructing naturally occurring multi-point mutant strains.
In our BLI mouse model, we found that our pseudovirus engineered to undergo a single round of replication is safe for use in BSL-2 laboratories, and that the experimental mice were sensitive to the infection and easily handled, making observations on them convenient, both spatially and temporally. The administration route used for the pseudoviruses in this study was intraperitoneal, which is the classic route used for infection challenge with wild-type RVFV. The observable biodistribution of pRVFV in mice using BLI reflected the known main replication sites of wild-type RVFV, such as the liver, spleen and lungs.1,33,34 Based on this finding, an in vivo method without wild-type RVFV in the whole experimental procedure was successfully established to evaluate vaccines and antibodies. This method should provide researchers with a safe work system, a shorter experimental time period (only 6 hours), and significantly improved overall efficiency. Some studies have shown that humoral immunity can protect against infection with RVFV.35 In this study, active immunization with recombinant DNA was evaluated in vivo using BLI, and no bioluminescence was detected in the mice when the ID50 values of the neutralizing antibodies exceeded 2500 in vitro. This result directly illustrates that mice can be completely protected from the viral infection when their antibodies reached a certain level. The neutralizing antibody levels should also be apparent if BLI is used in vivo. The protective effects of the vaccine and its associated antiviral antibodies could be evaluated more accurately and clearly by combining the in vivo and in vitro tests. It has been shown that recombinant plasmids expressing the RVFV M segment can stimulate production of the neutralizing antibodies that protect mice from infections of wild-type RVFV,15,36 however in this study, we didn’t validate the in vitro or in vivo methods on the wild-type RVFV because of the limited experimental conditions available and a lack of the wild-type virus. In the future, we intend to determine whether the methods used for the pseudovirus can be used with the wild-type virus and, ideally, standardize this system further.
The pseudovirus constructed with the RVFV glycoprotein in this study can only be used to determine the neutralizing antibody titers against the glycoprotein. But the antibodies against other viral proteins, especially nucleocapsid protein, could not be detected out with this system. Nevertheless, our newly established method could be a useful resource for researchers working on the development of vaccines and antiviral drugs against RVFV.
Materials and methods
Cells, viruses, plasmids and animals
The following cell types were used in this study: HEK293T (ATCC, CRL-3216), Vero (ATCC, CCL81), VeroE6 (ATCC, CRL-1586), A549 (ATCC, CCL-185), HeLa (ATCC, CCL-2), BHK21 (ATCC, CCL-10) and Huh7 (Cell Bank of Chinese Academy of Sciences, TCHu182). All cells were maintained in Dulbecco’s modified Eagle’s medium (HyClone, South Logan, UT, USA) supplemented with 10% fetal bovine serum (FBS, Gibco, Carlsbad, CA, USA), 1% penicillin-streptomycin solution (Gibco, Carlsbad, CA, USA), and 2% HEPES (Gibco, Carlsbad, CA, USA) at 37°C in a humidified incubator with 5% CO2. pVSVΔG, a recombinant VSV derived from the full-length cDNA clone from the VSV genome (Indiana serotype), in which the coding region of the G protein was replaced by the firefly luciferase (Fluc) gene and the G protein was supplied in trans, was kindly provided by Prof. Whitt at The University of Tennessee. The RVFV codons-optimized envelope glycoprotein sequences (GenBank: ABD38819) were synthesized by GENEWIZ (GENEWIZ, Suzhou, China) and then subcloned into the BamHI and XhoI sites of the pcDNA3.1+ expression vector (Invitrogen, USA) to construct the recombinant DNA (pcDNA3.1-ZH548). The guinea pigs and Balb/c mice used in this study were provided by the Institute of Experimental Animal Resources at the National Institute for Food and Drug Control (Beijing, China). All the animal studies were approved by the Institutional Animal Care and Use Committee of the National Institute of Food and Drug Control.
Preparation of sera
pcDNA3.1-ZH548, was used as the DNA vaccine, 200μg of which was inoculated into female guinea pigs by electroporation each time to prepare the anti-RVFV serum. The blood taken from the heart of each animal was incubated for 1 h at 37°C and then centrifuged to separate the serum. All the serum samples recovered from the animals were inactivated for 30 min at 56°C before their first use.
Preparation and titration of pseudovirus
293T cells were passaged at a density of about 5 × 105/mL the day before the transfections. When the cell density reached about 80%, the plasmids were transfected into the 293T cells according to the instructions for the transfection reagents and, concurrently, the cells transfected with pcDNA3.1+ were used as the negative control group. After being infected with pVSVΔG, the 293T cell monolayer was washed with DMEM containing 1% heat-inactivated FBS three times, and new complete culture medium was added. Pseudoviruses in the culture supernatants were clarified by low-speed centrifugation and stored at −80°C. For pseudovirus titration, Huh7 cells grown in 96-well plates were infected with 100μl of serially diluted virus stock. After 24h incubation at 37°C in a CO2 incubator, the RLU values were calculated as described previously.37 The TCID50 value of the pseudovirus was calculated by the Reed-Muench method.38
In vitro pseudovirus neutralization
Neutralization was measured by the reduction in RLU values as described previously.39 pRVFV was incubated with 3-fold serially diluted serum samples (30-fold in the initial dilution) from immunized guinea pigs in 96-well plates for 1 h at 37°C before adding the cells, followed by co-incubation for 24 h. The RLU values were then measured, and the reduction values calculated were compared with those for the control wells, which were then used to determine the ID50 values of the sera using the Reed-Muench method.40
Naturally occurring single amino acid substitutions and site-directed mutagenesis
RVFV glycoprotein sequences were downloaded from the National Center for Biotechnology Information Database (NCBI, https://www.ncbi.nlm.nih.gov/) and the Virus Pathogen Database and Analysis Resource (ViPR, http://www.viprbrc.org/). All sequences were aligned with the reference sequence using ClustalW multiple alignment analysis software implemented in BioEdit version 7.0.5.3. Further analysis of the amino acid mutations was performed using the SIFT and PROVEAN software, with all parameters set to the default positions. The recombinant plasmid containing the reference sequence (ZH548-M) was used as the template DNA to construct the genetic variants. DNA containing the desired mutation was synthesized by polymerase chain reaction (PCR) approaches using two complimentary oligonucleotides containing the mutation (Table 1). Subsequent digestion of the reaction mixture with DpnI was employed to remove the template DNA, leaving the intact newly synthesized double-stranded DNA, which was subsequently transformed into E. coli DH5α cells.41
In vivo bioluminescence imaging (BLI)
In the in vivo pseudovirus challenge experiments, the mice were inoculated with pseudoviruses intraperitoneally and bled from the intraocular canthus. The serum titers were determined by in vitro pseudovirus neutralization assays.
The bioluminescence emitted from each mouse was detected to evaluate the infection status of the pseudovirus in vivo. Balb/c mice (4-week old) were immunized each time with 50μg of the DNA vaccine by electroporation, and boosted every 2 weeks. The mice were challenged with pRVFV one week after the last immunization. In vivo BLI experiments were performed using the IVIS-Lumina III imaging system (PerkinElmer, Baltimore, MD, USA), as described previously.41 Mice were anaesthetized using an intraperitoneal injection of pentobarbitalum (45 mg/kg body weight) and D-luciferin (150 mg/kg body weight; PerkinElmer), and 10 min later, their bioluminescence values were measured. Image software (Caliper Life Sciences, Baltimore, MD, USA) was used to calculate the total flux values (photons/s/cm2/sr) for the mice using the photon-per-second mode described previously.39
Funding Statement
This work was supported by the National Science and Technology Major Projects of Infectious Disease funds of China (grants 2017ZX10304402).
Acknowledgments
We are grateful to Michael A. Whitt for allowing us to use the VSV system and for his helpful advice in regard to it. The authors wish to thank Chunnan Liang, from the Institute for Laboratory Animal Resources, for the helping with the animal experiments. We also thank Sandra Cheesman, PhD, from Liwen Bianji, Edanz Group China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Disclosure of potential conflicts of interest
No potential conflicts of interest were reported by the authors.
References
- 1.Ikegami T, Makino S.. The pathogenesis of Rift Valley fever. Viruses. 2011;3:493–519. doi: 10.3390/v3050493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rippy MK, Topper MJ, Mebus CA, Morrill JC. Rift Valley fever virus-induced encephalomyelitis and hepatitis in calves. Vet Pathol. 1992;29:495–502. doi: 10.1177/030098589202900602. [DOI] [PubMed] [Google Scholar]
- 3.Mcintosh BM, Russell D, Dos Santos I, Gear JHS. Rift Valley fever in humans in South Africa. S Afr Med J. 1980;58:803–06. [PubMed] [Google Scholar]
- 4.Madani TA, Al-Mazrou YY, Al-Jeffri MH, Mishkhas AA, Al-Rabeah AM, Turkistani AM, Al-Sayed MO, Abodahish AA, Khan AS, Ksiazek TG, et al. Rift Valley fever epidemic in Saudi Arabia: epidemiological, clinical, and laboratory characteristics. Clin Infect Dis. 2003;37:1084–92. doi: 10.1086/378747. [DOI] [PubMed] [Google Scholar]
- 5.Meegan JM. The Rift Valley fever epizootic in Egypt 1977–78. 1. Description of the epizzotic and virological studies. Trans R Soc Trop Med Hyg. 1979;73:618–23. doi: 10.1016/0035-9203(79)90004-X. [DOI] [PubMed] [Google Scholar]
- 6.Collett MS, Purchio AF, Keegan K, Frazier S, Hays W, Anderson DK, Parker MD, Schmaljohn C, Schmidt J, Dalrymple JM. Complete nucleotide sequence of the M RNA segment of Rift Valley fever virus. Virology. 1985;144:228–45. doi: 10.1016/0042-6822(85)90320-4. [DOI] [PubMed] [Google Scholar]
- 7.Freiberg AN, Sherman MB, Morais MC, Holbrook MR, Watowich SJ. Three-dimensional organization of Rift Valley fever virus revealed by cryoelectron tomography. J Virol. 2008;82:10341–48. doi: 10.1128/jvi.01191-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gerrard SR, Nichol ST. Characterization of the Golgi retention motif of Rift Valley fever virus G(N) glycoprotein. J Virol. 2002;76:12200–10. doi: 10.1128/JVI.76.23.12200-12210.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Piper ME, Sorenson DR, Gerrard SR. Efficient cellular release of Rift Valley fever virus requires genomic RNA. PLoS One. 2011;6:e18070. doi: 10.1371/journal.pone.0018070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Papin JF, Verardi PH, Jones LA, Monge-Navarro F, Brault AC, Holbrook MR, Worthy MN, Freiberg AN, Yilma TD. Recombinant Rift Valley fever vaccines induce protective levels of antibody in baboons and resistance to lethal challenge in mice. Proc Natl Acad Sci U S A. 2011;108:14926–31. doi: 10.1073/pnas.1112149108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Besselaar TG, Blackburn NK, Meenehan GM. Antigenic analysis of Rift Valley fever virus isolates: monoclonal antibodies distinguish between wild-type and neurotropic virus strains. Res Virol. 1991;142:469–74. doi: 10.1016/0923-2516(91)90069-F. [DOI] [PubMed] [Google Scholar]
- 12.Besselaar TG, Blackburn NK. The effect of neutralizing monoclonal antibodies on early events in Rift Valley fever virus infectivity. Res Virol. 1994;145:13–19. doi: 10.1016/S0923-2516(07)80002-1. [DOI] [PubMed] [Google Scholar]
- 13.Grobbelaar AA, Weyer J, Leman PA, Kemp A, Paweska JT, Swanepoel R. Molecular epidemiology of Rift Valley fever virus. Emerg Infect Dis. 2011;17:2270–76. doi: 10.3201/eid1712.111035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Whitt MA. Generation of VSV pseudotypes using recombinant DeltaG-VSV for studies on virus entry, identification of entry inhibitors, and immune responses to vaccines. J Virol Methods. 2010;169:365–74. doi: 10.1016/j.jviromet.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spik K, Shurtleff A, McElroy AK, Guttieri MC, Hooper JW, SchmalJohn C. Immunogenicity of combination DNA vaccines for Rift Valley fever virus, tick-borne encephalitis virus, Hantaan virus, and Crimean Congo hemorrhagic fever virus. Vaccine. 2006;24:4657–66. doi: 10.1016/j.vaccine.2005.08.034. [DOI] [PubMed] [Google Scholar]
- 16.Hall TA. BioEdit: a user-friendly biological sequence alignment editor and analysis program for Windows 95/98/NT. Nucleic Acids Symp Ser. 1999;41:95–98. doi: 10.1021/bk-1999-0734.ch008. [DOI] [Google Scholar]
- 17.Ng PC, Henikoff S. SIFT: predicting amino acid changes that affect protein function. Nucleic Acids Res. 2003;31:3812–14. doi: 10.1093/nar/gkg509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sim NL, Kumar P, Hu J, Henikoff S, Schneider G, Ng PC. SIFT web server: predicting effects of amino acid substitutions on proteins. Nucleic Acids Res. 2012;40:W452–W457. doi: 10.1093/nar/gks539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prateek K, Steven H, Ng PC. Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat Protoc. 2009;4:1073–81. doi: 10.1038/nprot.2009.86. [DOI] [PubMed] [Google Scholar]
- 20.Choi Y, Chan AP. PROVEAN web server: a tool to predict the functional effect of amino acid substitutions and indels. Bioinformatics. 2015;31:2745–47. doi: 10.1093/bioinformatics/btv195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ning T, Wolfe A, Nie J, Huang W, Chen XS, Wang Y. Naturally occurring single amino acid substitution in the L1 Major capsid protein of human papillomavirus type 16: alteration of susceptibility to antibody-mediated neutralization. J Infect Dis. 2017;216:867–76. doi: 10.1093/infdis/jix274. [DOI] [PubMed] [Google Scholar]
- 22.Ogino M, Ebihara H, Lee BH, Araki K, Lundkvist A, Kawaoka Y, Yoshimatsu K, Arikawa J. Use of vesicular stomatitis virus pseudotypes bearing hantaan or seoul virus envelope proteins in a rapid and safe neutralization test. Clin Diagn Lab Immunol. 2003;10:154–60. doi: 10.1128/CDLI.10.1.154-160.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lennemann NJ, Herbert AS, Brouillette R, Rhein B, Bakken RA, Perschbacher KJ, Cooney AL, Miller-Hunt CL, Ten EP, Biggins J, et al. Vesicular stomatitis virus pseudotyped with Ebola virus glycoprotein serves as a protective, non-infectious vaccine against Ebola virus challenge in mice. J Virol. 2017. doi: 10.1128/jvi.00479-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Takada A, Robison C, Goto H, Sanchez A, Murti KG, Whitt MA, Kawaoka Y. A system for functional analysis of Ebola virus glycoprotein. Proc Natl Acad Sci USA. 1997;94:14764–69. doi: 10.1073/pnas.94.26.14764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ellis DS, Shirodaria PV, Fleming E, Simpson DI. Morphology and development of Rift Valley fever virus in Vero cell cultures. J Med Virol. 1988;24:161–74. doi: 10.1002/jmv.1890240205. [DOI] [PubMed] [Google Scholar]
- 26.Randall R, Gibbs CJ Jr., Aulisio CG, Binn LN, Harrison VR. The development of a formalin-killed Rift Valley fever virus vaccine for use in man. J Immunol. 1962;89:660–71. [PubMed] [Google Scholar]
- 27.Caplen H, Peters CJ, Bishop DH. Mutagen-directed attenuation of Rift Valley fever virus as a method for vaccine development. J Gen Virol. 1985;66(Pt 10):2271–77. doi: 10.1099/0022-1317-66-10-2271. [DOI] [PubMed] [Google Scholar]
- 28.Kortekaas J, de Boer SM, Kant J, Vloet RP, Antonis AF, Moormann RJ. Rift Valley fever virus immunity provided by a paramyxovirus vaccine vector. Vaccine. 2010;28:4394–401. doi: 10.1016/j.vaccine.2010.04.048. [DOI] [PubMed] [Google Scholar]
- 29.Lopez-Gil E, Lorenzo G, Hevia E, Borrego B, Eiden M, Groschup M, Gilbert SC, Brun A. A single immunization with MVA expressing GnGc glycoproteins promotes epitope-specific CD8+-T cell activation and protects immune-competent mice against a lethal RVFV infection. PLoS Negl Trop Dis. 2013;7:e2309. doi: 10.1371/journal.pntd.0002309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee BH, Yoshimatsu K, Araki K, Okumura M, Nakamura I, Arikawa J. A pseudotype vesicular stomatitis virus containing Hantaan virus envelope glycoproteins G1 and G2 as an alternative to hantavirus vaccine in mice. Vaccine. 2006;24:2928–34. doi: 10.1016/j.vaccine.2005.12.040. [DOI] [PubMed] [Google Scholar]
- 31.Garbutt M, Liebscher R, Wahl-Jensen V, Jones S, Moller P, Wagner R, Volchkov V, Klenk HD, Feldmann H, Stroher U. Properties of replication-competent vesicular stomatitis virus vectors expressing glycoproteins of filoviruses and arenaviruses. J Virol. 2004;78:5458–65. doi: 10.1128/jvi.78.10.5458-5465.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kapadia SU, Rose JK, Lamirande E, Vogel L, Subbarao K, Roberts A. Long-term protection from SARS coronavirus infection conferred by a single immunization with an attenuated VSV-based vaccine. Virology. 2005;340:174–82. doi: 10.1016/j.virol.2005.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smith DR, Steele KE, Shamblin J, Honko A, Johnson J, Reed C, Kennedy M, Chapman JL, Hensley LE. The pathogenesis of Rift Valley fever virus in the mouse model. Virology. 2010;407:256–67. doi: 10.1016/j.virol.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 34.Anderson GW Jr., Slone TW Jr., Peters CJ. Pathogenesis of Rift Valley fever virus (RVFV) in inbred rats. Microb Pathog. 1987;2:283–93. doi: 10.1016/0882-4010(87)90126-4. [DOI] [PubMed] [Google Scholar]
- 35.Niklasson BS, Meadors GF, Peters CJ. Active and passive immunization against Rift Valley fever virus infection in Syrian hamsters. Acta Pathol Microbiol Immunol Scand C. 1984;92:197–200. doi: 10.1111/j.1699-0463.1984.tb00074.x. [DOI] [PubMed] [Google Scholar]
- 36.Lorenzo G, Martin-Folgar R, Hevia E, Boshra H, Brun A. Protection against lethal Rift Valley fever virus (RVFV) infection in transgenic IFNAR(-/-) mice induced by different DNA vaccination regimens. Vaccine. 2010;28:2937–44. doi: 10.1016/j.vaccine.2010.02.018. [DOI] [PubMed] [Google Scholar]
- 37.Nie J, Wu X, Ma J, Cao S, Huang W, Liu Q, Li X, Li Y, Wang Y. Development of in vitro and in vivo rabies virus neutralization assays based on a high-titer pseudovirus system. Sci Rep. 2017;7:42769. doi: 10.1038/srep42769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Matumoto M. A note on some points of calculation method of LD50 by Reed and Muench. Jpn J Exp Med. 1949;20:175. [PubMed] [Google Scholar]
- 39.Liu Q, Fan C, Zhou S, Guo Y, Zuo Q, Ma J, Liu S, Wu X, Peng Z, Fan T, et al. Bioluminescent imaging of vaccinia virus infection in immunocompetent and immunodeficient rats as a model for human smallpox. Sci Rep. 2015;5:11397. doi: 10.1038/srep11397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reed LJ, Muench H. A simple method of estimating fifty percent endpoints. Am J Epidemiol. 1938;27:493–97. doi: 10.1093/oxfordjournals.aje.a118408. [DOI] [Google Scholar]
- 41.Shenoy AR, Visweswariah SS. Site-directed mutagenesis using a single mutagenic oligonucleotide and DpnI digestion of template DNA. Anal Biochem. 2003;319:335–36. doi: 10.1016/S0003-2697(03)00286-0. [DOI] [PubMed] [Google Scholar]


