Abstract
Background:
Noise-induced hearing loss (NIHL) is a common, irreversible occupational disease. Statins have recently been proposed to prevent NIHL.
Objective:
To assess the effect of atorvastatin for the prevention of NIHL in rats.
Methods:
In this experimental study, forty 2–3-month-old Wistar male rats were divided into 5 groups of 8 animals. 3 groups of rats received atorvastatin at doses of 5, 25, and 50 mg/kg daily for 14 days. The 4th group of rats received normal saline; another group was the control group. After 2 weeks of treatment, the rats were exposed to broad-band noise (125– 20 000 Hz) at 110 dB-SPL intensity for 2 hours. Response amplitude of all ears at 5 frequencies was assessed by distortion product otoacoustic emissions (DP-OAE) at baseline, 2 hours, and 2 weeks after the exposure.
Results:
Response amplitude was significantly decreased at all frequencies immediately after exposure to noise in all studied groups. The amplitude increased after 72 hours to a level higher than temporary threshold shift (TTS); this change was only significant in the group received 5 mg/kg atorvastatin.
Conclusion:
Low dose atorvastatin (5 mg/kg) used before exposure to noise can probably prevent NIHL in rats. This effect was not observed with higher doses of the drug.
Keywords: Hearing loss, noise-induced, Otoacoustic emissions, spontaneous, Atorvastatin, Antioxidants, Occupational diseases
TAKE-HOME MESSAGE
Noise is the most frequent physical exposure in the workplace.
Noise leads to some health effects among which noise-induced hearing loss (NIHL) is the most common.
The target organ of the effect of noise is cochlear sensory hair cells that are affected by noise through mechanical, metabolic, and vascular mechanisms such as glutamate excitotoxicity, ion imbalance, production of oxygen radicals, and activation of histone deacetylase.
Statins, currently used as cholesterol-lowering agents, are among the substances being claimed as NIHL-preventing substances due to their antioxidant effects.
Atorvastatin at a dose of 5 mg/kg administered before exposure to noise can probably prevent NIHL in rats. This effect was not observed with higher doses of the drug.
Introduction
Noise is the most frequent physical exposure in the workplace. It is estimated that about 28% of workers in the Europe are exposed to noise level above 85 dBA.1 Noise leads to some health effects among which noise-induced hearing loss (NIHL) is the most common. NIHL, which is the second most common type of sensorineural hearing loss after presbycusis, is an irreversible disorder.2,3 It is one of the most common work-related diseases and is considered as an occupational injury that is not commonly self-reported.2 NIHL is typically a bilateral and symmetric sensorineural hearing loss that presents as a V-shaped notch at 3, 4, or 6 kHz, and a recovery at 8 kHz as the first sign.4,5
NIHL is a major concern for workforce health in different parts of the world even developed countries.4,6,7 It is estimated that 30 million workers are exposed to noise and about 10 million suffer from NIHL in the USA.8 According to National Institute for Occupational Safety and Health (NIOSH), about 5.7 million workers (25% of all US workers) in manufacturing industry are exposed to hazardous noise.9 In a study, the costs of NIHL in the USA have been estimated to be more than US$ 1 billion.10
Although some methods have been studied for the treatment of NIHL, we have still no acceptable treatment for the disease; however, it is preventable.11 OSHA in its hearing conservation program (HCP), presents some methods for prevention of NIHL including lowering the exposure time to noise and wearing hearing protection devices (HPDs). Currently, HPDs are used as the commonest method for prevention of NIHL, although with variable efficiency, because it may cause a considerable discomfort for the worker, which may lower the worker's compliance and impairs the communication, especially important in safety critical jobs. On the other hand, when noise level is more than 105 dBA, HPDs alone cannot attenuate the noise to the acceptable level. Therefore, some other approaches should be considered in these situations.
The target organ of the effect of noise is cochlea in the inner ear, where sensory hair cells are affected by noise through some possible mechanisms including mechanical, metabolic, and vascular mechanisms such as glutamate excitotoxicity, ion imbalance, production of oxygen radicals, and activation of histone deacetylase.12-15 Therefore, antioxidant mechanisms can probably prevent NIHL. There are some internal antioxidative mechanisms in the inner ear such as glutathione reductase and γ-glutamyl cycteine synthetase,13 but noise can overcome these defense systems.16
Therefore, different researchers have assessed the effect of some antioxidants for the prevention of NIHL. Antioxidants such as N-acetyl cysteine, vitamin A, C, and E, lipoic acid, resveratrol, etc, have been assessed in small animals with different efficacies.17-19 Among other antioxidants, statins have also been proposed as efficacious drugs for prevention of NIHL in small animals.16
Different kinds of statins are currently used as cholesterol-lowering agents, by inhibiting HMG-CoA reductase,20 though they have other effects on the body independent of this effect.21 Park, et al, found that pretreatment of mice with pravastatin (25 mg/kg) for five days can significantly decrease compound threshold shift and permanent threshold shift.22 Syka, et al, found that atorvastatin can slow down age-related inner ear function in mice.23
The most frequent type of statin used in Iran is atorvastatin, which is inexpensive as well. We therefore conducted this experimental study to assess the effect of atorvastatin for the prevention of NIHL in an animal model.
Materials and Methods
This experimental study was performed in the central laboratory of Medical School, Shahid Sadoughi University of Medical Sciences, Yazd, Iran in 2014. The protocol of the study was approved by the University Ethics Committee.
Animals
Forty 2–3-month-old Wistar male rats weighing 250±50 g were obtained from animal center of the international branch of Shahid Sadoughi University of Medical Sciences. The animals were housed in animal center of the Medical School in polycarbonil cages with 15×20×30 cm dimensions at a temperature of 25 °C and relative humidity of 55%. All animals were exposed to light:dark cycles of 12:12 hours. They had access to food and water ad libitum. The room was well-ventilated with noise intensity <45 dBA in 24 hours. Animals were divided into five groups (eight animals in each group).
Noise Exposure
Animals were placed in a glass cage. A broad-band noise (125–20 000 Hz) produced by an audiometer (OB922, Madsen, Denmark) at 110 dB-SPL intensity was used for two hours for each animal.
Hearing Assessment
The hearing status of each animal was assessed by distortion product otoacoustic emissions (DP-OAE) with Capella (Madsen, Denmark). Before the test, rats were anesthetized with ketamine 100 mg/kg and xylazine 10 mg/kg. Two probes designed for rat external ear canal, were placed in the ear canal and response amplitude at 2, 3, 4, 6 and 8 kHz frequencies in each ear were recorded.
Experimental Procedure
Rats were divided into five groups of eight animals. At baseline, response amplitude of all ears at five frequencies was assessed by DP-OAE. Then, three groups of rats received atorvastatin at doses of 5, 25, and 50 mg/kg via intra-gastric gavage once daily for 14 days. The fourth group of rats received 3 mL normal saline solution via intra-gastric gavage. The fifth group (control group) of rats did not receive saline or atorvastatin.
After two weeks of treatment with either atorvastatin or saline, rats were exposed to noise for two hours. Two hours after the exposure, DP-OAE was performed by the same device to find temporary threshold shift (TTS). Finally, 72 hours after exposure to noise, DP-OAE was performed to assess permanent threshold shift (PTS).
Statistical Analysis
Data were analyzed by SPSS® for Windows® ver 20. One-sample Kolmogorov-Smirnov test was used to test the normality of data. Parametric tests and non-parametric tests were used for the analysis of data with and without normal distribution, respectively. A p <0.05 was considered statistically significant.
Results
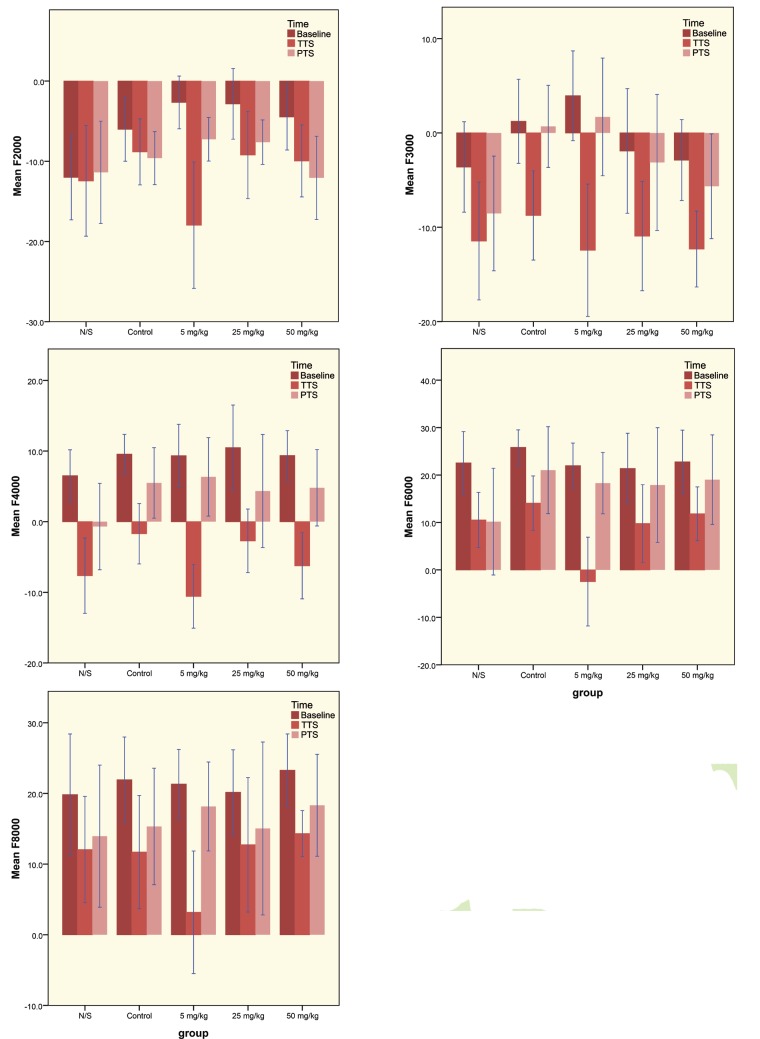
None of the studied data had normal distribution. Totally, 40 animals (80 ears) were studied. Response amplitude was significantly decreased at all frequencies immediately after exposure to noise in all five studied groups (TTS). The amplitude increased after 72 hours to a level higher than TTS, but this change was only significant in the group received 5mg/kg atorvastatin. Figure 1 compares the mean response amplitude in studied groups at baseline, immediately after noise exposure (TTS) and 72 hours after noise exposure (PTS) at different frequencies.
Figure 1.
Comparison of the response amplitude at different frequencies (2–8 kHz) in the study groups receiving various doses of atorvastatin. Error bars represent 95% CI of the mean. N/S stands for normal saline.
Discussion
Noise is one of the most hazardous factors of the modern societies.24 NIHL, as an irreversible disorder, is very frequent in most industrial settings. So far, there is no effective treatment for NIHL.25 Investigators have been seeking methods for prevention of NIHL in workers exposed to noise. Drugs from different families have been used for this purpose. Examples are N-acetyl cysteine, vitamin E, vitamin C, vitamin A, lipoic acid, corticosteroids, and calcium channel blockers.6,16-18,25,26
One of the well-known mechanisms of NIHL is oxidant injury and free radical production.24,27,28 Therefore, some substances with antioxidant properties have been tested for prevention of NIHL.22,27
Luxmore in a study examined the effect of a mixed drug regimen—T-type calcium channel blockers and synthetic glucocorticoids—for protection and treatment of NIHL in mice. He found that this combination can prevent NIHL in mice, but it was not effective for the treatment of NIHL.25 Baoa, et al, also examined a combination therapy for NIHL consisting of ethosuximide and dexamethasone, in mice and found a significant preventive and therapeutic effect for these drugs.29
Statins, currently used as cholesterol-lowering agents, are among the substances being claimed as NIHL-preventing substances due to their antioxidant effects.20,21 The effect of statins in prevention of NIHL is however, controversial.
In this study, the preventive effect of atorvastatin was evaluated in rats that were exposed to loud noise. We found that atorvastatin can prevent permanent hearing loss at a dose of 5 mg/kg in comparison to the control group; higher doses of atorvastatin, however, did not have this protective effect.
Koc, et al, found that oxidative stress can be decreased partially with rosuvastatin and that this effect was almost more prominent with a higher dose of the drug.27 Another study failed to show a statistically significant NIHL-protective effect of pravastatin in rats.30
Park, et al, used pravastatin and found that this drug reduced hair cell death in the cochlea after noise exposure and decreased threshold shifts. They also showed that this attenuation was caused by inhibition of NADPH oxidase complex formation.22 Syka, et al, found that atorvastatin can slow down age-related inner ear function in mice.23 Olzowy, et al, in a controlled clinical trial on old people with presbycusis and tinnitus found that atorvastatin though cannot change the hearing threshold, can attenuate tinnitus.31
The discrepancy between results of the studies on statins is probably due to different methods (ie, noise exposure, time to test PTS) and different animals used. In the current study, we used three doses of atorvastatin, but only 5 mg/kg had significant effect on the prevention of PTS. Liu, et al, reported a case of permanent hearing loss due to atorvastatin consumption,32 thus, higher doses of the drug may be ototoxic. It is recommended to study the effect of atorvastatin on the prevention of NIHL with doses other than the effective dose of 5 mg/kg, eg, 10 mg/kg, which may be associated with higher responses, and lower doses, which may result in the same effect.
In this study, we could not use acoustic brainstem response (ABR) which is more precise than OAE for the assessment of hearing.
Acknowledgements
This study was originated from a residency thesis in occupational medicine in Shahid Sadoughi University of Medical Scienses.
Conflicts of Interest:
None declared.
Cite this article as: Jahani L, Mehrparvar AH, Esmailidehaj M, et al. The effect of Atorvastatin on preventing noise-induced hearing loss: An experimental study. Int J Occup Environ Med 2016;7:15-21. doi: 10.15171/ ijoem.2016.627
References
- 1. uropean Agency for Safety and Health at Work (EASHW). Monitoring the state of occupational safety and health in the European Union Pilot Study, 2000.
- 2. Dunn DE, Rabinowitz PM. Noise, In: Rosenstock L, ed. Textbook of clinical occupational and environmental medicine. 2nd ed. St. Louis Mo, Elsevier Saunders, 2005:893.
- 3. Rabinowitz PM, Rees TS. Occupational hearing loss, In: Rosenstock L, ed. Textbook of clinical occupational and environmental medicine. 2nd ed. St. Louis Mo, Elsevier Saunders, 2005:426-30.
- 4.Hong O. Hearing loss among operating engineers in American construction industry. Int Arch Occup Environ health. 2005;78:565–74. doi: 10.1007/s00420-005-0623-9. [DOI] [PubMed] [Google Scholar]
- 5. eyer MR. Occupational exposure to noise. Rom W, ed. Environmental and Occupational Medicine, 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 2007:1296-310.
- 6.Chen JD, Tsai JY. Hearing loss among workers at an oil refinery in Taiwan. Arch Environ Health. 2003;58:55–8. doi: 10.3200/AEOH.58.1.55-58. [DOI] [PubMed] [Google Scholar]
- 7.McBride DI, Firth HM, Herbison GP. Noise exposure and hearing loss in agriculture: a survey of farmers and farm workers in the Southland region of New Zealand. J Occup Environ Med. 2003;45:1281–8. doi: 10.1097/01.jom.0000100001.86223.20. [DOI] [PubMed] [Google Scholar]
- 8. U.S. Department of Labor, Occupational Safety and Health Administration (USDOL OSHA), Noise and Hearing Conservation, 2002.
- 9.Tak S, Davis RR, Calvert GM. Exposure to hazardous workplace noise and use of hearing protection devices among US workers: NHANES, 1999–2004. Am J Ind Med. 2009;52:358–71. doi: 10.1002/ajim.20690. [DOI] [PubMed] [Google Scholar]
- 10.Fausti SA, Wilmington DJ, Helt PV. et al. Hearing loss prevention and hearing conservation practice. J Rehabil Res Dev. 2005;42:45–62. doi: 10.1682/jrrd.2005.02.0039. [DOI] [PubMed] [Google Scholar]
- 11. Schindler DN, Robinson ST. Hearing loss. In: LaDou J, ed. Occupational and Environmental Medicine. 3rd ed. New York, McGraw-Hill, 2007:104-20.
- 12.Tao L, Davis R, Heyer N. et al. Effect of cigarette smoking on noise-induced hearing loss in workers exposed to occupational noise in China. Noise Health. 2013;15:67–72. doi: 10.4103/1463-1741.107159. [DOI] [PubMed] [Google Scholar]
- 13.enderson D, McFadden SL, Liu CC. et al. The role of antioxidant in protection from impulse noise. Ann N Y Acad Sci. 1999;884:368–80. doi: 10.1111/j.1749-6632.1999.tb08655.x. [DOI] [PubMed] [Google Scholar]
- 14.Mehrparvar AH, Mirmohammadi SJ, Hashemi SH. et al. Concurrent effect of noise exposure and smoking on extended high-frequency pure-tone thresholds. Int J Audiol. 2015;5:301–7. doi: 10.3109/14992027.2014.978906. [DOI] [PubMed] [Google Scholar]
- 15.Wen LT, Wang J, Wang Y, Chen F. Association between histone deacetylases and the loss of cochlear hair cells: Role of the former in noise-induced hearing loss. Int J Mol Med. 2015;36:534–40. doi: 10.3892/ijmm.2015.2236. [DOI] [PubMed] [Google Scholar]
- 16.Adams JC, Seed B, Lu N. et al. Selective activation of nuclear factor kappa B in the cochlea by sensory and inflammatory stress. Neuroscience. 2009;60:530–9. doi: 10.1016/j.neuroscience.2009.02.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oishi N, Schacht J. Emerging treatment for noise-induced hearing loss. Expert Opin Emerg Drugs. 2011;16:235–45. doi: 10.1517/14728214.2011.552427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kopke R, Slade MD, Jackson R. et al. Efficacy and safety of N-acetylcysteine in prevention of noise induced hearing loss: a randomized clinical trial. Hear Res. 2015;323:40–50. doi: 10.1016/j.heares.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 19.Chen GD, Fechter LD. The relationship between noise-induced hearing loss and hair cell loss in rats. Hear Res. 2003;177:813–20. doi: 10.1016/s0378-5955(02)00802-x. [DOI] [PubMed] [Google Scholar]
- 20.Nassief A, Marsh JD. Statin therapy for stroke prevention. Stroke. 2008;39:1042–8. doi: 10.1161/STROKEAHA.107.501361. [DOI] [PubMed] [Google Scholar]
- 21.Farmer JA. Pleiotropic effects of statins. Curr Atheroscler Rep. 2000;2:208–17. doi: 10.1007/s11883-000-0022-3. [DOI] [PubMed] [Google Scholar]
- 22.Park JS, Kim SW, Park K. et al. Pravastatin attenuates noise-induced cochlear injury in mice. Neuroscience. 2012;208:123–32. doi: 10.1016/j.neuroscience.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 23.Syka J, Ouda L, Nachtigal P. et al. Atorvastatin slows down the deterioration of inner ear function with age in mice. Neurosci Lett. 2007;411:112–6. doi: 10.1016/j.neulet.2006.10.032. [DOI] [PubMed] [Google Scholar]
- 24.Zheng KC, Ariizumi M. Modulations of immune functions and oxidative status induced by noise stress. J Occup Health. 2007;49:32–8. doi: 10.1539/joh.49.32. [DOI] [PubMed] [Google Scholar]
- 25. Luxmore RL. Efficacy of a combined drug therapy for ameliorating noise-induced hearing loss, Washington University, School of Medicine Program in Audiology and Communication Sciences, 2012.
- 26.McEwen BS. Central effects of stress hormones in health and disease. Eur J Pharm. 2008;583:174–85. doi: 10.1016/j.ejphar.2007.11.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Koc ER, Ersoy A, Ilhan A. et al. Is rosuvastatin protective against on noise-induced oxidative stress in rat serum? Noise Health. 2005;17:11–6. doi: 10.4103/1463-1741.149565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Van Campen LE, Murphy WJ, Franks JR. et al. Oxidative DNA damage is associated with intense noise exposure in the rat. Hear Res. 2002;164:29–38. doi: 10.1016/s0378-5955(01)00391-4. [DOI] [PubMed] [Google Scholar]
- 29.Baoa J, Hungerford M, Luxmore R. et al. Prophylactic and therapeutic functions of drug combinations against noise-induced hearing loss. Hearing Res. 2013;304:33e–40. doi: 10.1016/j.heares.2013.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sanders JM. Protective effect of systemic administration of pravastatin against noise-induced hearing loss In the fischer 344/nhsd rat substrain, Capstone Project, The Ohio State University, 2012.
- 31.Olzowy B, Canis M, Hempel JM. et al. Effect of Atorvastatin on progression of sensorineural hearing loss and tinnitus in the elderly: results of a prospective, randomized, double-blind clinical trial. Otol Neurotol. 2007;28:455–8. doi: 10.1097/01.mao.0000271673.33683.7b. [DOI] [PubMed] [Google Scholar]
- 32.Liu M, Alafris A, Longo AJ, Cohen H. Irreversible Atorvastatin-Associated Hearing Loss. Pharmacotherapy. 2012;32:e27–34. doi: 10.1002/PHAR.1040. [DOI] [PubMed] [Google Scholar]