According to ICD 10 classification “adjustment disorders are states of subjective distress and emotional disturbance, usually interfering with social functioning and performance, arising in the period of adaptation to a significant life change or a stressful life event.”1 The WHO’s classification (ICD 10: Chapter 5 “Mental and Behavioural disorders,” F43.2) indicates different types of stressor that may be linked to a single event or multiple events and may be recurrent events or continuous.
According to DSM-5 adjustment disorder occurs when the onset of symptoms is within three months of exposure to the stressor(s) (criterion A).2 Generally, there is no adjustment disorder without a stressor, but, usually, the stressor is a precipitating factor while the risk of occurrence and the shaping of the manifestations depend on different vulnerabilities as well as coping skills of the individual.1 Moreover, symptoms or behaviors are clinically significant because they are in excess of what would be expected by exposure to the stressor, taking into account the external context and the cultural factors that might influence symptom severity and presentation (criterion B, 1).2 In Europe, the psychosocial risks at work are one of the priorities of the Community Strategy for Health and Safety at Work, but there is not a general agreement on the question of recognition of work-related mental disorders as occupational diseases or work injuries. As a matter of fact, there are some questions concerning the causal relation between work and the disease, because (unlike the so-called “conventional occupational diseases”) a worker’s mental health can be affected not only by working conditions but also by extra-occupational stressors; moreover, there is difficulty in defining the concept of psychosocial risk and characterizing the causal relation, in order to define a framework for recognition and compensation procedures.3 In Europe, only Denmark has registered a mental disorder, ie, post-traumatic stress disorder (PTSD), on its list of occupational diseases. On the contrary, in Italy, such as other European countries (eg, Belgium, and France), such mental disorders are only mentioned in a complementary list. The complementary system requires the demonstration of a direct, decisive, essential and very probable link between the off-list disease and work performance. Generally, a mental disorder can be recognized as an accident at work (usually, with a diagnosis of PTSD) or as an occupational disease (usually, with a “chronic adjustment disorder” diagnosis). In Europe, Italy is the country that has most precisely defined the practice of recognition and compensation for mental disorders. The nosographic framework of the pathologies covered by the Italian insurance system corresponds to the two types of stress-related syndromes—(PTSD) and “chronic adjustment disorder.” Nevertheless, the Italian compensation system for occupational injuries and diseases (Decree n.38/2000) established the measure of the “biological damage” that is the basis for compensation for permanent disability, only for the PTSD but not for the “adjustment disorder” (Fig 1). In Italy, there is a mixed system (list and complementary system) for notification and recognition of occupational diseases. Although PTSD and adjustment disorders are not in the “official” list made by the Italian Workers’ Compensation Authority (INAIL) and approved by Ministerial Decree (Decree April 4, 2008) for recognition of occupational diseases, INAIL covers both PTSD and adjustment disorders caused by risks situation created by inconsistencies in the organization process. In Italy, these psychosocial risk factors are reported as “organizational constraints” in the Circular of INAIL n.71/2013 and in a Ministerial Decree of April 2004 (updated by the Decree 10th June 2014) fixing the new lists of diseases having a possible work-related origin that must be reported by law in accordance with art. 139 of Italian law n. 1124/65. Only the Circular was declared void by the Italian administrative courts because it considers mental disorders caused by a mobbing situation as real occupational diseases and because psychosocial risks covered in the INAIL’s Circular were referable to situations of mobbing and task-related bullying,4-6 and excluded organization factors related to the dynamics common to the occupational environment and the purely subjective attitudes adopted by people in their workplace.3,7
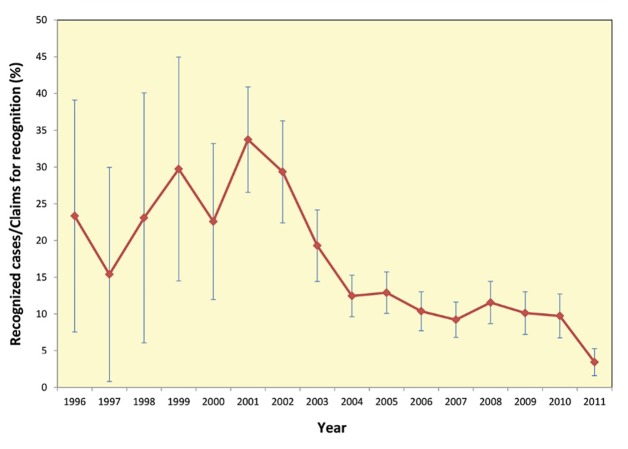
Figure 1.
The ratio of “recognized cases” to “claims cases” of mental disorders as “occupational disease” in Italy between 1996 and 2011 (data from Eurogip Report, 2013)3. Error bars represent 95% confidence interval.
Therefore, mobbing-related psychosocial risk factors that are still included in the Decree June 10, 2014 are not specifically considered in the INAIL/ISPESL risk assessment methodology.7 On the other hand, the Italian protocol developed for the work-related stress risk assessment by INAIL/ISPESL,8,9 includes assessment of psychosocial risk factors based on the workers’ subjective perception of psycho-social hazards, related to both the content of and context to work described in the Cox’s research, commissioned by Eu-OSHA.10 Specifically, according to the Italian Consultative Committee’s protocol, there is a preliminary assessment to analyze the objective risk indicators related to work-related stress, in three distinct areas—sentinel events, work content factors, and contextual factors at work. If, in this phase, there is no evidence of work-related stress, the employer provides a monitoring plan. Otherwise, if some risk factors are emerged and appropriate corrective actions are ineffective, the subjective perceptions of workers are collected in an in-depth assessment perceptions of work, through questionnaires, focus group, and semi-structured interviews.8 In Italy, occupational health surveillance may be activated during the “in-depth” phase, when the risk assessment required it.11 According to the European directives, health surveillance at work is mandatory only when the risk assessment has identified a risk for workers’ health that technical, organizational, and procedural actions were not able to remove it. A significant challenging issue concerns the misdiagnosis of adjustment disorder because it is a longitudinal diagnosis based on etiology and outcome,12 and also because it has no reliable and valid diagnostic tool.13,14 In this way, occupational health surveillance is able to give an advantage to make diagnosis of chronic adjustment disorder arising from work-related stress, because an occupational medicine physician well knows both the psychosocial risk assessment of the company and the medical history of the worker affected by a mental disorder. Nevertheless, in Italy, occupational health surveillance programs for preventing occupational mental disorders might be useless. Most of the times, the agreement between employers and persons delegated by workers may stop at the first step of the work-related stress risk assessment. In this case, occupational health surveillance, as a corrective measure, is not activated and a medical examination might only be conducted at the request of the employees by the occupational physician of the company. As a consequence, it will be difficult for an occupational physician to make a diagnosis of adjustment disorder as an occupational disease. Adjustment disorders are some of the most common, yet under-researched, mental health disorders that occupational physicians might encounter. The preliminary phase of the work-related stress risk assessment, based only on the objective factors, might neglect individual predisposition or vulnerability of the worker, which plays an important role in the risk of occurrence and the shaping of the manifestations of adjustment disorders.1 For this reason, health surveillance in the workplace should be activated, even though the preliminary phase of work-related stress risk assessment did not need an in-depth evaluation. In this way, health surveillance might also be useful to check that control measures are working well by giving feedback on risk assessments, suggesting where further actions might be needed and what they might be, providing data, by means of the health records, to detect and evaluate health psychosocial risks. Moreover, a neglected issue concerns which protocol should be established by the occupational physician of the company for health surveillance of employees, when the risk assessment required it.
In my opinion, occupational medicine physicians (through occupational health surveillance), psychiatrists, psychologists, and experts in work organization should operate in strict cooperation for diagnosing chronic adjustment disorder in the workplace. As for diagnosing adjustment disorders and other mental health ailments, self-administered questionnaires such as General Heath Questionnaire (GHQ) or other screening tools for anxiety-depression, might be useful in the first step medical examination (by an occupational physician). However, it should also be necessary a second step for the organizational analysis (by an expert in work organization) and a third step for psychiatric and psychological examination (this latter phase needs both clinical examination and SCID-5).5,6,15
In a review,16 Casey has highlighted two types of tools for diagnosing adjustment disorders—the structured interviews and the screening instruments. As for the first category, he stated that the Clinical Interview Schedule (CIS)17 and the Composite International Diagnostic Interview (CIDI)18 do not incorporate adjustment disorders at all. Moreover, the Schedules for Clinical Assessment in Neuropsychiatry developed by WHO (SCAN)19 does include adjustment disorders, but only at the end of the interview. Finally, the SCID-I for DSM-IV TR20 and the Mini-International Neuropsychiatric Interview (MINI)21 also include a section dealing with adjustment disorders, but it is possible to make a diagnosis of adjustment disorder only if the criteria for any other mental disorders are excluded with the de factoeffect of relegating it to a sub-syndromal status, because major depression often supersedes adjustment disorder. According to Casey, structured interviews, having been designed for use by lay interviewers, are overly rigid and the diagnosis of adjustment disorder relies heavily on clinical judgment, context, and presumptive longitudinal course than symptoms alone. On the other hand, since there is symptom overlap with major depression, there is a possibility that instruments used for screening depression might identify people with adjustment disorder.16 Therefore, Casey16 indicates some tools such as the Zung Depression Scale22 or the Inventory of Depressive Symptomatology,23 though further investigation of these instruments is clearly required.
To date, work-related adjustment disorders and depression are frequently work-related mental problems,13 but occupational physicians have little knowledge about the available tools for workplace health surveillance. Over years, research on work-related stress very often used self-reported instruments such as questionnaires for assessing the linkage between work stress and anxiety, depression, burnout, and other outcomes of mental health.24 The most common assessment tool for mental well-being is the GHQ. Since its development by Goldberg in the 1970s, GHQ has been extensively used in different setting and various cultures for measuring common mental health problems of depression, anxiety, somatic symptoms, and social withdrawal.25 Nevertheless, GHQ was not used in adjustment disorder’s research. Furthermore, the Maslach Burnout Inventory (MBI) is the most commonly used instrument for measuring burnout syndrome that is a chronic stress-related disorder typically and particularly found within human service professions.26
Nevertheless, adjustment disorders can often be difficult to diagnose, because burnout syndrome, depression, and adjustment disorder overlap considerably. Moreover, there is difficulty in differential diagnosis between adjustment disorder and PTSD/acute stress disorder, and symptoms of adjustment disorder can be confused with the symptoms of depressive illness, psychosis-related illness or personality disorders, because there is no clear-cut way to make this differentiation.
As for new specific tools for diagnosing adjustment disorders, Cornelius, et al, achieved, partly adjusting and operationalizing DSM-IV criteria, a new instrument called Diagnostic Interview Adjustment Disorder (DIAD). According to Cornelius’s study, DIAD is a valid instrument for diagnosing adjustment disorder, but further studies on reliability and on other aspects of validity are needed.27 Finally, the recent Structured Clinical Interview for DSM-5 (SCID-5)28 is a semi-structured interview guide for making DSM-5 diagnoses such as adjustment disorder and has replaced the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I). According to American Psychiatric Association, the latest SCID-5 is an available tool useful for a forensic diagnostic evaluation.2
In conclusion, in Europe and in Italy, implementation research is needed to establish the best available tools for recognizing adjustment disorders and other work-related mental health disorders, as occupational diseases by occupational medicine physicians of the companies. In Italy, work-related stress risk assessment is mandatory and recognition of work-related mental disorders as occupational disease by INAIL is increasing; for this reason, there is a debate about whether psychosocial risk factors related to organizational constraints which are included in the Decree June 10, 2014, should be also considered by employers when they carry out their work-related stress risk assessment. Moreover, according to the current methodology for the work-related stress risk assessment, policy makers should amend the current list of occupational diseases attached to Ministerial Decree June 10, 2014 to include also psychosocial risk factors related to the dynamics common to the occupational environment. Nevertheless, in this way, adjustment disorders as occupational diseases caused by common organizational risk factors might be included, at a later time, in the “official” list of occupational diseases attached to Decree April 4, 2008, which INAIL uses for recognizing of occupational diseases. It might be a big problem for the management of claims for compensation by INAIL. In every case, for improving the prevention and management of work-related mental disorders, I hope health surveillance in the workplace can be activated, even though the preliminary phase of work-related stress risk assessment does not need an in-depth evaluation, for reducing the misdiagnosis of adjustment disorders as occupational diseases and improving the knowledge of the work-related stress risk assessment.
Conflicts of Interest:
None declared.
Cite this article as: Chirico F. Adjustment disorder as an occupational disease: Our experience in Italy. Int J Occup Environ Med 2016;7:52-57.
References
- 1. WHO. ICD 10, Available from www.who.int/classifications/icd10/browse/2015/en#/F40-F48 (Accessed November 19,2015).
- 2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington DC, American Psychiatric Association Press, 2013.
- 3. Eurogip. What recognition of work-related mental disorders? A study on 10 European countries. Study report, February 2013. Ref. Eurogip-81/E. Paris: Eurogip, Available from www.eurogip.fr (Accessed November 19,2015).
- 4.Signorelli MS, Costanzo MC, Cinconze M, Concerto C. What kind of diagnosis in a case of mobbing: post-traumatic stress disorder or adjustment disorder? BMJ Case Reports. 2013 Jun 11 doi: 10.1136/BCR-2013-010080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sed B, Magrini A, Livigni L, et al. Evaluation approach to chronic stress, organizational constrictivity, and mobbing. G Ital Med Lav Erg 2006;28,Sup 127.
- 6.Taino G, Pizzuto C, Pucci E, Imbriani M. Reactive anxiety crisis and chronic adjustment disorder: a unique case of work injury and suspected occupational disease. G Ital Med Lav Ergon. 2014;36:118–23. [PubMed] [Google Scholar]
- 7.Chirico F. The assessment of the psycosocial risk: only work-related stress” or something else? Med Lav. 2015;106:65–6. [PubMed] [Google Scholar]
- 8.Persechino B, Valenti A, Ronchetti M. et al. Work-related stress risk assessment in Italy: a methodological proposal adapted to regulatory guidelines. Saf Health Work. 2013;4:95–9. doi: 10.1016/j.shaw.2013.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Circolare Ministero del Lavoro del 18 novembre 2010. Available from www.lavoro.gov.it/ sicurezzalavoro/MS/CommissionePermanente/(Accessed November 04,2015).
- 10. Cox T, Griffiths A, Rial-Gonzalez E. Research on work-related stress. Luxembourg: Office for Official Publications of the European Communities: European Agency for Safety & Health at Work. 2000.
- 11. Coordinamento Tecnico Interregionale della prevenzione nei luoghi di lavoro (Gennaio 2012). Stress lavoro correlato. Indicazioni per la corretta gestione del rischio e per l’attività di vigilanza alla luce della lettera circolare del 18 novembre 2010. Available from www.inail.it(Accessed November 19,2015).
- 12.Casey P. Adjustment disorder: new developments. Curr Psychiatry Rep. 2014;16:451. doi: 10.1007/s11920-014-0451-2. [DOI] [PubMed] [Google Scholar]
- 13.Nakamura J. Early detection and intervention for adjustment disorder and depression in the work place. Seishin Shinkeigaku Zasshi. 2012;114:1093–9. [PubMed] [Google Scholar]
- 14.Casey P, Doherty A. Adjustment Disorder: implications for ICD-11 and DSM-5. The British Journal of Psychiatry. 2012;201:90–92. doi: 10.1192/bjp.bp.112.110494. [DOI] [PubMed] [Google Scholar]
- 15. Chirico F. Adjustment Disorders in DSM-5: implications for occupational health surveillance. Acta Psychopathologica 2015. Available from http://psychopathology.imedpub.com/adjustment-disorders-in-dsm5-implications-for-occupationalhealth-surveillance.pdf (Accessed October 15, 2015).
- 16.Casey P, Bailey S. Adjustment disorders: the state of the art. World Psychiatry. 2011;10:11–8. doi: 10.1002/j.2051-5545.2011.tb00003.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lewis G, Pelosi AJ, Araya R. Measuring psychiatric disorders in the community: a standardised assessment for use by lay interviewers. Psychol Med. 1992;22:465–86. doi: 10.1017/s0033291700030415. [DOI] [PubMed] [Google Scholar]
- 18.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative version of the World Health Organization Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wing JK, Babor T, Brugha T. SCAN: Schedules for Clinical Assessment in Neuropsychiatry. Arch Gen Psychiatry. 1990;47:589–93. doi: 10.1001/archpsyc.1990.01810180089012. [DOI] [PubMed] [Google Scholar]
- 20. First MB, Williams JBW, Spitzer RL, Gibbon M. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Clinical Trials Version (SCID-CT). New York: Biometrics Research, New York State Psychiatric Institute, 2007.
- 21.Sheehan D, Lecrubier Y, Sheehan KH. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- 22.Zung WW. A self-rating depression scale. Arch Gen Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]
- 23.Trivedi MH, Rush AJ, Ibrahim HM. The Inventory of Depressive Symptomatology, Clinician Rating (IDS-C) and Self-Report (IDS-SR), and the Quick Inventory of Depressive Symptomatology, Clinician Rating (QIDS-C) and Self-Report (QIDS-SR) in public sector patients with mood disorders: a psychometric evaluation. Psychol Med. 2004;34:73–82. doi: 10.1017/s0033291703001107. [DOI] [PubMed] [Google Scholar]
- 24.Henderson M, Harvey SB, Øverland S. et al. Work and common psychiatric disorders. R Soc Med. 2011;104:198–207. doi: 10.1258/jrsm.2011.100231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jackson C. The General Health Questionnaire. Occup Med (Lond) 2007;57:79. [Google Scholar]
- 26.Maslach C, Schaufeli W, Leiter M. Job burnout. Annu Rev of Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 27.Cornelius LR, Brouwer S, de Boer MR. et al. Development and validation of the Diagnostic Interview Adjustment Disorder (DIAD) International Journal of Methods in Psychiatric Research. 2014;23:192–207. doi: 10.1002/mpr.1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. First MB, Williams JBW, Karg RS, Spitzer RL. Structured Clinical Interview for DSM-5—Research Version (SCID-5 for DSM-5, Research Version; SCID-5-RV). Arlington, VA, American Psychiatric Association, 2015.