Abstract
Objective:
To examine the continuity of adherence barriers across stages of development in pediatric epilepsy and to assess the differential influence of barriers on several important clinical outcomes from early childhood to young adulthood, including adherence, seizures, and health-related quality of life.
Method:
A developmentally representative sample of youth 2–25 years with epilepsy was obtained by combining data from five different studies. A total of 274 participants were included in this investigation, including 269 caregivers and 77 adolescents and young adults. Participants completed measures of adherence barriers and health-related quality of life. An electronic monitoring system was used to assess adherence to the primary antiepileptic drug over 30 days. The prevalence of individual barriers across development and their relative importance as predictors of clinical outcomes were examined.
Results:
Adherence barriers are characterized by both continuity and discontinuity from early childhood to early adulthood. Barriers such as disliking the taste of medication, parent forgetfulness and refusal to take medications were significantly more salient during certain developmental periods. No significant differences across age groups were found for other barriers, including difficulty getting to the pharmacy, embarrassment, etc. Certain adherence barriers, such as running out of medications, were more important to particular clinical outcomes despite low prevalence. Adherence barriers differentially predicted adherence, seizure control, and health-related quality of life based on developmental stage.
Conclusion:
Routine assessment of adherence barriers is imperative from toddlerhood to young adulthood given that the prevalence of barriers and their relative influence on important health outcomes varies by developmental stage. Adherence intervention efforts should be targeted, developmentally tailored, and focused on those barriers that are most predictive of poor outcomes for a given developmental period.
Keywords: adherence, barriers, development, seizures, health-related quality of life
1. Introduction
Epilepsy is a brain disorder characterized by recurrent unprovoked seizures that affects 470,000 children in the United States [1]. Antiepileptic drugs (AEDs) are the first-line treatment for most children to achieve seizure freedom, symptom management, and increased function. Nonadherence to AEDs has been associated with a variety of undesirable outcomes including limited treatment efficacy (e.g., continued seizures [1–3]), increased mortality [4], higher healthcare utilization [5, 6] and costs [6], and lower health-related quality of life (HRQOL) [7]. In youth with epilepsy, approximately 60% of patients exhibit AED nonadherence, as measured by electronic monitoring [3, 8]. Adherence has been described as a dynamic behavior, with both stable (e.g., socioeconomic status [8]) and modifiable (e.g., barriers to adherence, psychological functioning) factors that contribute to nonadherence. Given the serious and costly consequences of nonadherence, a better understanding of malleable contributing factors is critical to guide the development of evidence-based interventions.
Barriers to adherence are modifiable variables that demonstrate consistent associations with nonadherence and suboptimal clinical outcomes in pediatric populations [9, 10]. Among children with epilepsy, barriers such as difficulties swallowing medications, forgetfulness and refusing to take medications as prescribed have been longitudinally associated with electronically-monitored nonadherence [11]. The stability of barriers to adherence has also been documented in children with newly diagnosed epilepsy, suggesting that once a barrier is endorsed, it is likely to persist for a 2-year period without targeted intervention. These findings provide clinically meaningful information about barrier stability, but are limited in their ability to contextualize barriers across the lifespan. No empirical work, to date, has examined barriers from a developmental perspective, and further research is needed to fill a critical gap in the literature regarding the continuity or discontinuity of barriers across stages of development.
Child development is a complex process characterized by qualitative and quantitative changes in many domains of functioning, including biological, socioemotional, behavioral, and cognitive. As a result of these developmental changes that naturally unfold as children mature, the types of adherence barriers that children face may also change as they grow. The degree to which different barriers may be more salient at different stages of development, or the extent to which certain barriers become no longer developmentally salient, however, is unknown. For example, pill swallowing difficulties are typically more common among preschoolers compared to adolescents. Further, the relative importance of individual barriers as predictors of adherence across different stages of development has not been empirically studied, despite its critical implications for the creation of developmentally sound interventions.
The first aim of this study was to identify the most highly endorsed adherence barriers at different stages of development (e.g., pre-school, school-aged, adolescence, and young adulthood). Guided by developmental principles and prior literature [8, 11, 12], it was hypothesized that disliking taste, child refusal and swallowing difficulties would be the most highly endorsed barriers among pre-school children; embarrassment would emerge as a highly endorsed barrier among school-aged children; and forgetfulness and competing activities would be the most highly endorsed barriers among adolescents and young adults. A second aim of this study was to compare the frequency of individual barriers by developmental period. It was hypothesized that disliking taste, refusal and swallowing difficulties would be most prevalent in younger children compared to the other development periods, and that forgetting and competing activities would be most prevalent in adolescents compared to the other developmental periods. The final aim was to evaluate the relative importance of individual barriers as predictors of clinical outcomes (e.g., adherence, seizure control, and HRQOL) at different stages of development. Based on prior studies, we hypothesized that forgetfulness and child refusal would be the most important predictors of adherence, seizure control and HRQOL among pre-school children, and that forgetfulness and competing activities would be the most salient predictors of adherence, seizure control and HRQOL among adolescents.
2. Material and methods
2.1. Participants and Procedures
A developmentally representative sample of youth with epilepsy was obtained by combining data from five different studies examining adherence barriers in children, adolescents and young adults with epilepsy. Detailed participant and methodology information for each of these studies has been published elsewhere [11, 13–16]. A total of 274 participants were included in this investigation, including 269 caregivers of youth with epilepsy between the ages of two and 25, and 77 adolescents and young adults between the ages of 13 to 25. Exclusion criteria for all studies included developmental delay, non-English speaking, and having a comorbid medical condition requiring daily medication. Recruitment rates for the studies included in this investigation ranged from 66% to 96% [8, 13, 15, 17, 18]. Detailed sociodemographic and medical information for the combined sample is presented in Table 1.
Table 1.
Sociodemographic and Medical Information
| N = 274 | ||
|---|---|---|
| Variable | M | SD |
| Age (years) | 9.69 | 4.73 |
| Medication Adherence | 82.62 | 22.70 |
| Frequency | % | |
| Sex | ||
| Male | 148 | 54.0 |
| Female | 126 | 46.0 |
| Age group | ||
| 2–5 years | 60 | 21.9 |
| 6–12 years | 134 | 48.9 |
| 13–17 years | 69 | 25.2 |
| 18–25 years | 11 | 4.0 |
| Race | ||
| White | 215 | 78.5 |
| Black | 42 | 15.3 |
| Asian | 2 | 0.7 |
| Biracial | 11 | 4.0 |
| Other | 4 | 1.5 |
| Family income | ||
| < $10,000 | 27 | 9.9 |
| $10,000–50,000 | 104 | 38.0 |
| $50,001–75,000 | 48 | 17.5 |
| >$75,000 | 80 | 29.2 |
| Prefer not to disclose | 15 | 5.5 |
| Seizure type | ||
| Partial | 136 | 49.6 |
| Generalized | 91 | 33.2 |
| Unclassified | 47 | 17.2 |
| Seizures in last three months | ||
| Yes | 174 | 63.5 |
| No | 99 | 36.1 |
| Antiepileptic medication | ||
| Depakote | 83 | 30.3 |
| Tegretol | 109 | 39.8 |
| Keppra | 44 | 16.1 |
| Trileptal | 10 | 3.6 |
| Zarontin | 17 | 6.2 |
| Topomax | 4 | 1.5 |
| Lamictal | 5 | 1.8 |
For all studies, eligible participants were identified by trained research staff and approached for participation during routine epilepsy clinic visits in a major Midwestern tertiary pediatric hospital. Procedures for providing an overview of study goals and objectives were standardized across studies. Families were given the opportunity to ask questions, which were thoroughly answered prior to obtaining consent, assent and HIPPA release. Participants completed all measures during the study visit or sent questionnaires back to study coordinators. Only baseline questionnaires were used in this investigation, with the exception of one longitudinal study examining psychosocial functioning and adherence over a two year study period for children newly diagnosed with epilepsy (e.g., recruited on day of diagnosis [8]). For this study, both the barriers and corresponding adherence data (e.g., 30-day adherence) for each participant were randomly selected out of a total of 10 possible time points spread over a 25-month period. This approach was used to better reflect average adherence rather than initial adherence immediately after diagnosis. Thirty-day adherence data was collected following the baseline visit for the remaining studies. Compensation for all participants was provided in the form of a gift card. The Institutional Review Board approved all studies included in this investigation.
2.2. Measures
2.2.1. Sociodemographic and Medical Information.
Across all studies, participants were asked to complete a brief background questionnaire that assessed child age, sex, race, family income, and caregiver marital status. Research staff completed a retrospective medical chart review to extract relevant medical variables, including date of epilepsy diagnosis, epilepsy type, prescribed AEDs, and presence of seizures over the previous three months.
2.2.2. Barriers to Adherence
The Barriers subscale of the Pediatric Epilepsy Medication Self-Management Questionnaire (PEMSQ [19]) was used to assess treatment barriers that interfere with AED adherence. Caregivers, adolescents, and young adults used a 5-point Likert scale, ranging from “strongly agree - 5” to “strongly disagree - 1” to indicate the extent to which eight different barriers interfere with the AED regimen. Higher subscale scores are indicative of more barriers to adherence. Internal reliability for the self-report Barriers subscale for the current study was α = 0.79, consistent with prior studies[19].
2.2.3. Medication Adherence
An electronic monitoring system, the Medication Event Monitoring System (MEMS) TrackCaps, was used to assess adherence to the primary AED. MEMS TrackCaps document the time and date a medication vial is opened and closed. Adherence data for each patient was downloaded from the TrackCap during study visits. To facilitate comparison of baseline adherence across the studies, 30-day mean adherence was calculated by using daily adherence data. For example, if a patient took 24 of 30 prescribed doses, mean adherence would be calculated by dividing the total number of doses taken over the total number of prescribed doses and multiplying that number by 100 (i.e., [24/30]*100 = 80%).
2.2.4. Health-related Quality of Life
The Quality of Life in Childhood Epilepsy Questionnaire (QOLCE [20]) is a 79-item measure of parent-reported HRQOL for children four to 18 years of age with epilepsy. Caregivers rate how much difficulty the child had with various tasks and domains of functioning over the previous month using a Likert scale. A total of 17 subscales make up the QOLCE, including Physical Restrictions, Energy/Fatigue, Depression, Anxiety, Control/Helplessness, Self-esteem, Behavior, Attention/Concentration, Memory, Language, Other Cognitive, Social Interaction, Social Activity, and Stigma. A Total HRQOL score is obtained by averaging all subscale scores. Scores range from 0 to 100, with higher scores indicating better HRQOL. The psychometric properties of the QOLCE have been well-established in the literature [20] and internal consistency was 0.95 across several studies for the Total HRQOL score [15, 21].
2.3. Statistical Analyses
Descriptive statistics, including means, standard deviations, and percentages were calculated to characterize the demographic and medical data. Frequencies were calculated to identify the most commonly endorsed barriers across stages of development, including pre-school (2–5 years) and school (6–12 years) aged children, as well as adolescents (13–17 years) and young adults (18–25 years). χ2 tests of independence were conducted to determine differences in the proportion of participants endorsing barriers versus not by developmental level. Finally, dominance analyses (“domin” function in Stata)[22, 23] were used to evaluate the relative importance of individual barriers as predictors of outcomes (e.g., adherence, seizures, and HRQOL) by developmental stage. Statistical analyses were performed using the IBM Statistical Package for Social Sciences (SPSS), Version 23 (IBM Corp., Armonk, NY, USA) and Stata version 14.
3. Results
3.1. Most common adherence barriers by stages of development
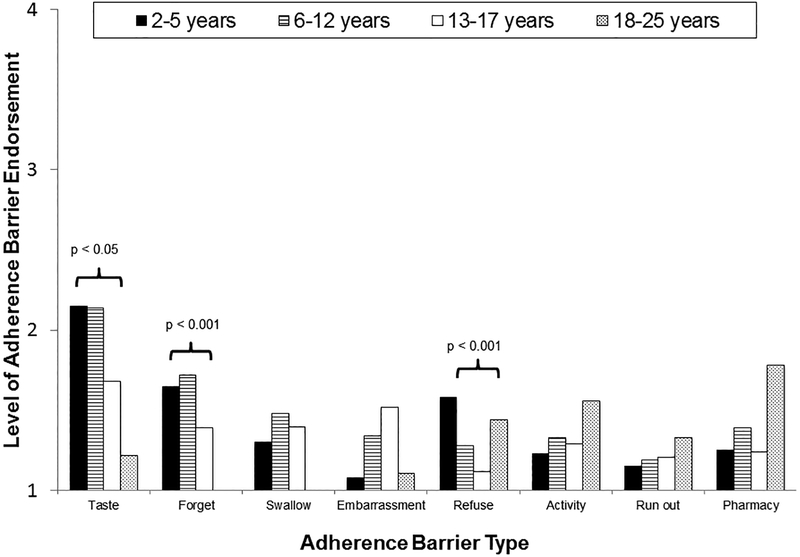
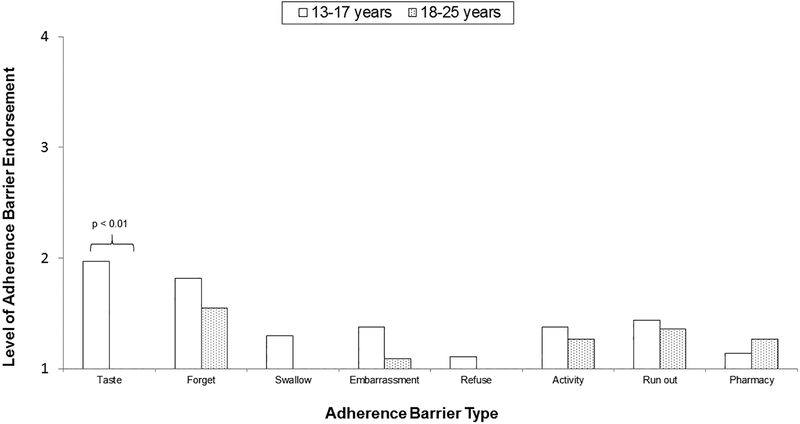
Among pre-school children, caregivers reported that disliking taste, parent forgetfulness, and child refusal were the most highly endorsed barriers to adherence (Figure 1). A total of 81.67% of pre-school children experienced at least one barrier to adherence. Among school-aged children, caregivers reported that disliking taste, parent forgetfulness, and swallowing difficulties were the most highly endorsed barriers to adherence. Approximately 80% of school-aged children experience at least one adherence barrier. Among adolescents, caregivers reported that disliking taste, embarrassment, and swallowing difficulties were the most highly endorsed barriers. Adolescents, on the other hand, endorsed disliking taste, forgetfulness, and running out of medications as their primary barriers to adherence (Figure 2). A total of 72.73% of parents and 81.81% of adolescents reported at least one barrier to adherence. Lastly, the caregivers of young adults indicated that difficulty getting to the pharmacy, activities that interfere with medication taking, and medication refusal were the most highly endorsed adherence barriers in this age group. Young adults themselves endorsed forgetfulness, running out of medications and difficulty getting to the pharmacy as their primary barriers to adherence. A total of 55.56% of parents and 72.72% of young adults endorsed at least one adherence barrier.
Figure 1.
PARENT REPORTED ADHERENCE BARRIERS ACROSS DEVELOPMENT
Figure 2.
ADOLESCENT AND YOUNG ADULT REPORTED ADHERENCE BARRIERS
3.2. Endorsement of individual barriers vary across development
Caregivers of 2–5 year olds (55%) and 6–12 year olds (46%) endorsed “dislike taste” more frequently than caregivers of 13–17 year olds (32%) and 18–25 year olds (11%), p < 0.05. Likewise, caregivers of 2–5 (52%) and 6–12 (52%) year olds endorsed “caregiver forgetfulness” more frequently than caregivers of 13–17 (32%) and 18–25 (0%) year olds, p < 0.001. A higher proportion of caregivers of 2–5 year olds (38%) and 18–25 year olds (33%), endorsed “medication refusal” compared to caregivers of 6–12 year olds (17%) and 13–17 year olds (11%), p < 0.001. Age groups did not significantly differ on any other caregiver-reported barriers. For self-report, a significantly higher proportion of 13–17 year olds (45%) endorsed “dislike taste” than 18–25 year olds (0%), p < 0.01. Adolescents and young adults did not differ on any other barriers.
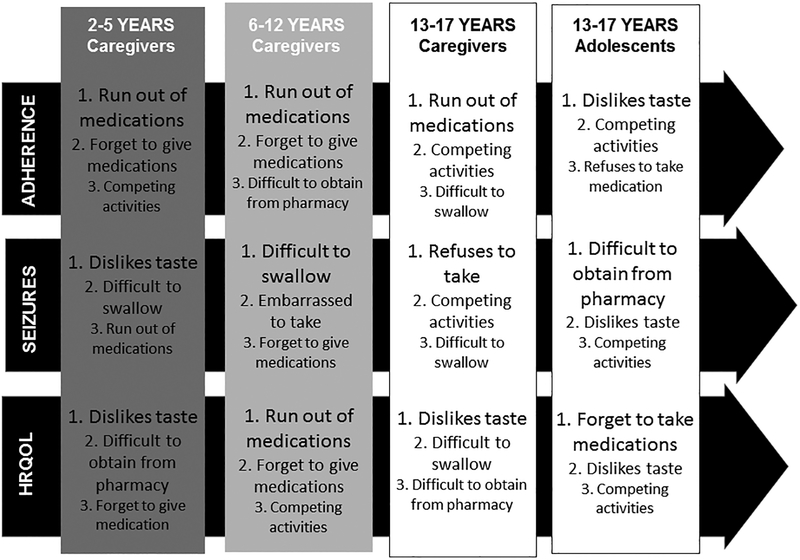
3.3. Relative importance of barriers related to outcomes
Dominance analyses were conducted to examine the relative importance of adherence barriers on clinical outcomes, including adherence, seizures, and total HRQOL across stages of development. However, the limited sample size of young adults precluded dominance analysis in this age group. Running out of medications was the single most important barrier for AED adherence across age groups (See Figure 3). Forgetting to give medications by caregivers appeared to be another important barriers for younger children (2–12 years old), while competing activities were of relative importance for adolescents, based on both caregiver and adolescent perspectives. Based on age, the most important barriers for seizure control varied by development. Specifically, disliking the taste of the medication and difficulty swallowing pills contributed to seizures in the younger cohorts. In contrast, refusal to take medications (caregiver-report) and difficulty obtaining the prescription (adolescent-report) were the most important barriers related to seizure control. Finally, caregivers reported that disliking the taste of medications was a relatively important barrier for HRQOL while forgetting to take/give medications, embarrassment of taking medications, and difficulty obtaining medications from pharmacies also played an important role in HRQOL.
Figure 3.
Dominance Analyses of Outcome Measures
4. Discussion
Adopting a developmental framework to examine adherence barriers is critical to understand the continuity and discontinuity of barriers across stages development in pediatric epilepsy. Further, the use of developmental principles to examine the influence of barriers on clinical outcomes throughout the lifespan is a necessary and important step towards creating developmentally informed adherence interventions in this population. Results of this study demonstrate that adherence barriers are characterized by both continuity and discontinuity from early childhood to early adulthood. Additionally, this study indicates that barriers have a differential impact on important outcomes of interest (e.g., adherence, seizures, and HRQOL) based on developmental stage.
Consistent with normative developmental expectations, barriers related to medication refusal were more prevalent among 2–5 year olds, but most strongly associated with poor adherence and poor seizure control outcomes among adolescents. These findings suggest that parents of younger children who refuse to take their medications have greater influence on their children’s behaviors and are potentially better equipped to address such behaviors. For example, use of parent management strategies typically used for common behavioral concerns is likely effective in regards to medication refusal among preschoolers. Conversely, parents of adolescents who demonstrate oppositional behaviors may find it significantly more challenging to encourage adherence in adolescents who actively refuse to take their medications as prescribed and are likely seeking independence and autonomy. Given that behavioral and oppositional concerns in this age group are remarkably more difficult to manage compared to preschoolers, parents of adolescents struggling with medication refusal may require additional behavioral and family support to effectively promote optimal adherence. Further, in some cases, adolescents themselves may benefit from health and psychosocial interventions targeting oppositional behaviors that are negatively impacting medication adherence, or from interventions (e.g., Motivational Interviewing) that target medication-taking ambivalence, which may be at the root of oppositional behavior.
Parent forgetfulness emerged as a particularly critical barrier among young children who rely almost exclusively on their caregivers for treatment. Consistent with developmental expectations, this barrier becomes progressively less salient as children grow into adolescence and begin to assume more responsibilities for their health care. Parent forgetfulness was the second most important predictor of medication nonadherence among 2–12 year olds, but not a predictor for 13–17 year olds, highlighting the critical importance of assessing parent barriers among preschool and school-aged children. Detailed assessment of the contributing factors to parent forgetfulness (e.g., logistical burden, psychosocial stressors, cognitive functioning) is essential in order to inform the types of supports and interventions that caregivers need. Parents with lower cognitive skills, for example, may have greater difficulty understanding treatment plans and recommendations. Because knowledge is a key predictor of epilepsy adherence [24], these caregivers may inconsistently follow treatment recommendations. In these cases, addressing health literacy and providing clarification of treatment plans would effectively address barriers related to parent forgetfulness. In contrast, visual or auditory reminders (e.g., texts, apps [25–27]) could be beneficial for caregivers who simply forget to give AEDs to their children.
Medication taste was another barrier characterized by discontinuity, in which a higher prevalence was noted for younger children compared to adolescents. While medication taste is typically less salient in adolescents and young adulthood, dominance analyses revealed that this barrier was the first or second most important predictor of nonadherence, seizure control, and HRQOL among adolescents. The consistency of these associations across clinical outcomes highlights the importance of addressing taste related barriers in teens. Among 2–5 year olds, barriers related to medication taste were the top predictor of HRQOL and seizure control but not adherence, supporting past research demonstrating nonlinear associations between seizure control and adherence [3]. These findings highlight the role that biology and behavior play in determining clinical outcomes and stress the importance of considering the dynamic relations that characterize barriers and adherence to better understand health outcomes.
There were a number of adherence barriers for which continuity was found throughout stages of development, suggesting that they may be unlikely to resolve without targeted intervention. Running out of medications, for example, emerged as a particularly influential barrier across stages of development, as it was the most important predictor of AED adherence for all age groups based on caregiver report. Although prior research has demonstrated that running out of medications is an unstable barrier over a two year period in children recently diagnosed with epilepsy,[28] our results indicate that when present, this barrier is associated with significant negative outcomes across age groups. Although this study did not examine the causal factors leading to running out of medications, it is possible that logistical (e.g., insurance, transportation), cognitive (e.g., forgetting to pick up refills), or psychosocial (e.g., caregiver depression) barriers are partially responsible. Healthcare providers play a critical role in helping families problem solve possible solutions to minimize nonadherence, including keeping extra doses of AEDs in the home, facilitating access to insurance coverage, developing reminder systems to pick up prescribed AEDs or using delivery/mail services for timely medication delivery. Multidisciplinary teams, including social workers and care coordinators, can help minimize the impact of logistical barriers, such as difficulty obtaining refills from pharmacies.
Barriers related to activities that interfere with medication taking were also similar across development but most strongly associated with lower adherence rates and poor seizure control among adolescents. Adolescence is a developmental period characterized by increasing independence, more social activities that compete with responsibilities, and fewer supervised routines. Parents are consequentially less involved in adolescents’ activities, have less access to them, and are less aware of how or where adolescents are spending their time. These changes in family dynamics and allocation of treatment responsibility as children grow older [18, 29] make it increasingly challenging for parents to provide the same level of close supervision and oversight that they once did. As a result, adolescents may lack the parental scaffolding they received when they were younger, which increases the probability of missed AED doses and nonadherence.
Other barriers such as difficulty swallowing medications, difficulty getting to the pharmacy, or embarrassment related to taking medications were also present across stages of development but differentially predicted outcomes based on the age group examined. These findings suggest that interventions should focus not simply on the most commonly endorsed barriers to adherence, but rather on the barriers that are most consistently associated with poor clinical outcomes during certain developmental periods.
Despite the novelty of these findings, this investigation has limitations. While the current study included a developmentally representative sample, it combined data from five different studies, which resulted in a cross-sectional versus longitudinal examination of development. Future studies employing longitudinal methodologies may follow a cohort of youth with epilepsy over time in order to examine whether adherence barriers change as children grow older. The small sample size of young adults limited our ability to conduct dominance analysis with this age group. As a result, our findings do not capture the relative importance of adherence barriers in the prediction of clinical outcomes during young adulthood. Having a larger cohort of young adults would enable the execution of dominance analyses in the future. To ensure consistency in objective adherence data across studies, we used one month of daily electronic adherence. In future studies, the concurrent assessment of adherence and barriers trajectories may provide unique insights into how these two constructs change and evolve throughout development.
4.1. Conclusions
Adherence barriers are characterized by both continuity and discontinuity from early childhood to early adulthood. Adherence barriers differentially predicted adherence, seizure control, and health-related quality of life based on developmental stage. Routine assessment of adherence barriers is imperative from toddlerhood to young adulthood because the nature and clinical impact of adherence barriers can change, reflecting the biological, socioemotional and cognitive changes that children experience through development. Further, because some adherence barriers are more important to certain clinical outcomes despite being low prevalence, special attention should be given to those barriers at particular developmental epochs. The use of brief and validated measures of adherence barriers may provide time-efficient, practical and empirically sound avenues for clinicians to identify adherence barriers that result in poor health outcomes. Adherence intervention efforts should be targeted, developmentally tailored, and focused on those barriers most predictive of poor outcomes for a given developmental stage.
Supplementary Material
Acknowledgements
We thank the families who participated in this study, all the CRCs that contributed to the execution of the studies included in this project, and the Comprehensive Epilepsy Center.
Funding
This work was supported by several grants from Cincinnati Children’s Hospital Medical Center (Schmidlapp Women’s Scholars Award, Endowed Scholars Award) and the National Institutes of Health (K23HD057333) to the senior author.
Footnotes
Declarations of Interest
Declarations of interest: none.
References
- [1].Kyngas H Compliance with health regimens of adolescents with epilepsy. Seizure 2000;9: 598–604. [DOI] [PubMed] [Google Scholar]
- [2].Modi AC, Rausch JR, Glauser TA. Early pediatric antiepileptic drug nonadherence is related to lower long-term seizure freedom. Neurology 2014;82: 671–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Modi AC, Wu YP, Rausch JR, Peugh JL, Glauser TA. Antiepileptic drug nonadherence predicts pediatric epilepsy seizure outcomes. Neurology 2014;83: 2085–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Sillanpaa M, Shinnar S. Long-term mortality in childhood-onset epilepsy. N Engl J Med 2010;363: 2522–9. [DOI] [PubMed] [Google Scholar]
- [5].Samsonsen C, Reimers A, Brathen G, Helde G, Brodtkorb E. Nonadherence to treatment causing acute hospitalizations in people with epilepsy: an observational, prospective study. Epilepsia 2014;55: e125–8. [DOI] [PubMed] [Google Scholar]
- [6].Faught RE, Weiner JR, Guerin A, Cunnington MC, Duh MS. Impact of nonadherence to antiepileptic drugs on health care utilization and costs: findings from the RANSOM study. Epilepsia 2009;50: 501–9. [DOI] [PubMed] [Google Scholar]
- [7].Wu YP, Follansbee-Junger K, Rausch J, Modi A. Parent and family stress factors predict health-related quality in pediatric patients with new-onset epilepsy. Epilepsia 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Modi AC, Rausch JR, Glauser TA. Patterns of non-adherence to antiepileptic drug therapy in children with newly diagnosed epilepsy. JAMA 2011;305: 1669–1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Hommel KA, Baldassano RN. Brief report: Barriers to treatment adherence in pediatric inflammatory bowel disease. J Pediatr Psychol 2010;35: 1005–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Dobbels F, Ruppar T, De Geest S, Decorte A, Van Damme-Lombaerts R, Fine RN. Adherence to the immunosuppressive regimen in pediatric kidney transplant recipients: a systematic review. Pediatr Transplant 2010;14: 603–13. [DOI] [PubMed] [Google Scholar]
- [11].Ramsey RR, Zhang N, Modi AC. The Stability and Influence of Barriers to Medication Adherence on Seizure Outcomes and Adherence in Children with Epilepsy over Two Years. Journal of Pediatric Psychology in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Cicchetti D Developmental Psychopathology, Maladaptation and Psychopathology. Hoboken, NJ; 2016. [Google Scholar]
- [13].Modi AC, Guilfoyle SM, Mann KA, Rausch JR. A Pilot Randomized Controlled Clinical Trial to Improve Antiepileptic Drug Adherence in Young Children with Epilepsy Epilepsia 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Modi AC, Guilfoyle SM, Rausch J. Preliminary Feasibility, Acceptability, and Efficacy of an Innovative Adherence Intervention for Children With Newly Diagnosed Epilepsy. J Pediatr Psychol 2013;38: 605–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Smith AW, Mara C, Ollier S, Combs A, Modi AC. Rebellious Behaviors in Adolescents With Epilepsy. J Pediatr Psychol 2017. [DOI] [PubMed] [Google Scholar]
- [16].Smith AW, Mara C, Modi AC. Self-management in adolescents with epilepsy In: 9th Annual Health Care Transition Research Consortium Symposium. Houston, TX; 2017. [Google Scholar]
- [17].Guilfoyle SM, Wagner JL, Modi AC, Junger KF, Barrett LE, Riisen AC, Schoffner KR, Smith AW, Weyand C. Pediatric Epilepsy and Behavioral Health: The State of the Literature and Directions for Evidence-Based Interprofessional Care, Training, and Research. Clinical Practice in Pediatric Psychology 2017;5: 79–90. [Google Scholar]
- [18].Ryan JL, Arnett AD, Pai AL, Modi AC. An examination of the Allocation of Treatment Responsibility scale in adolescents with epilepsy. Epilepsy Behav 2014;41: 1–5. [DOI] [PubMed] [Google Scholar]
- [19].Modi AC, Monahan S, Daniels D, Glauser TA. Development and validation of the Pediatric Epilepsy Medication Self-Management Questionnaire. Epilepsy Behav 2010;18: 94–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Sabaz M, Lawson JA, Cairns DR, Duchowny MS, Resnick TJ, Dean PM, Bye AM. Validation of the quality of life in childhood epilepsy questionnaire in American epilepsy patients. Epilepsy Behav 2003;4: 680–91. [DOI] [PubMed] [Google Scholar]
- [21].Ramsey RR, Loiselle K, Rausch JR, Harrison J, Modi AC. Predictors of trajectories of epilepsy-specific quality of life among children newly diagnosed with epilepsy. Epilepsy Behav 2016;57: 202–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Luchman JN. DOMIN: Stata module to conduct dominance analysis. In; 2013. [Google Scholar]
- [23].Johnson JW. A heuristic method for estimating the relative weight of predictor variables in multiple regression. Multivariate Behavioral Research 2000;35: 1–19. [DOI] [PubMed] [Google Scholar]
- [24].Loiselle K, Rausch JR, Modi AC. Behavioral predictors of medication adherence trajectories among youth with newly diagnosed epilepsy. Epilepsy & Behavior 2015;50: 103–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Dayer L, Heldenbrand S, Anderson P, Gubbins PO, Martin BC. Smartphone medication adherence apps: potential benefits to patients and providers. J Am Pharm Assoc (2003) 2013;53: 172–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Park LG, Howie-Esquivel J, Dracup K. A quantitative systematic review of the efficacy of mobile phone interventions to improve medication adherence. J Adv Nurs 2014;70: 1932–53. [DOI] [PubMed] [Google Scholar]
- [27].Checchi KD, Huybrechts KF, Avorn J, Kesselheim AS. Electronic medication packaging devices and medication adherence: a systematic review. JAMA 2014;312: 1237–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Ramsey RR, Zhang N, Modi AC. The Stability and Influence of Barriers to Medication Adherence on Seizure Outcomes and Adherence in Children With Epilepsy Over 2 Years. J Pediatr Psychol 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Holbein CE, Smith AW, Peugh J, Modi AC. Allocation of treatment responsibility in adolescents with epilepsy: Associations with cognitive skills and medication adherence. Journal of Pediatric Psychology under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.